Abstract
Adverse childhood experiences (ACEs) contribute to physical, behavioral, and mental health issues throughout the lifespan and, because of their prevalence, constitute a significant public health issue. Practitioners in all health care disciplines need to be knowledgeable about ACEs and prepared to address them. ACEs can contribute to conditions that lead patients to seek rehabilitation care, and therefore a framework is needed that enables rehabilitation professionals to understand the effects of ACEs and how to discuss them with patients. This article summarizes ACE research and its clinical relevance, presents an overview of the related topic of trauma-informed care, and introduces rehabilitation professionals to practical tools for incorporating ACE- and trauma-informed care into clinical practice.
There is growing acknowledgement across all health care disciplines of the impact of ACEs. ACEs are understood as stressful, potentially traumatic events that may have lasting negative effects on health and well-being. Since the 1990s, when landmark research found striking associations between early life stress and adversity and a wide range of chronic physical, behavioral, and mental health issues, international attention to ACEs as a major public health issue has grown.1, 2 ACE-related research has identified strong correlations between chronic disease, stress, and prior experience. Eighty-six percent of health care dollars in the United States are spent on chronic diseases, and a population health strategy should include empowering, person-centered, low-risk, low-cost, self-management skill-building practices to help patients manage the stress response.3
Though a relevant consideration for all care provision, the biopsychosocial framework may be particularly important for understanding and working with chronic health conditions.4, 5, 6, 7 For example, chronic pain affects 116 million in the United States8 and may be a key force in driving patients to seek rehabilitation services. Patients need their providers to skillfully and comprehensively navigate the intersection of mental, emotional, and physical components of their healing process. Given the prevalence of ACEs and their potential contribution to chronic pain, among other conditions, rehabilitation professionals should be prepared to address ACEs in the clinical setting as a possible underlying contributor to the condition for which treatment is sought. This article provides an overview of ACEs research and the health effects that can result from ACEs and introduces a trauma-informed practical guide for rehabilitation professionals to use in clinical encounters.
Keywords: Adverse childhood experience, Chronic disease, Pain, post-traumatic, Rehabilitation, Stress disorders
List of abbreviations: ACE, adverse childhood experience; BPS, biopsychosocial; PTSD, posttraumatic stress disorder; TIC, trauma-informed care
Highlights
-
•
Adverse childhood experiences (ACEs) contribute to a broad spectrum of health challenges across the lifespan and constitute a significant public health issue.
-
•
Rehabilitation professionals routinely work with individuals experiencing health challenges that may be linked to ACEs.
-
•
Models of trauma-informed care and resilience-building approaches assist rehabilitation professionals in contributing to a solution to the prevalence of ACEs and chronic stress in the population.
-
•
A novel schema is presented to assist rehabilitation professionals in navigating the topic of ACEs in clinical care.
Adverse childhood experiences
In 1997, Kaiser Permanente and the Centers for Disease Control published a landmark adverse childhood experiences (ACEs) study examining relations between early life stress and health patterns later in life.9 The study followed more than 17,000 individuals and asked if they had experienced any of the following stressors in their childhood years (through age 18): abuse (physical, sexual, emotional), neglect (physical, emotional), or household challenges (intimate partner violence, mother treated violently, substance misuse within household, household mental illness, parental separation or divorce, incarcerated household member). Other ACE-related studies have broadened the adverse experiences content.10, 11, 12, 13
ACEs were found to be exceptionally common, with approximately two-thirds of respondents having at least one. For example, 21% reported experiencing sexual abuse and 28% reported physical abuse. Of those with at least 1 ACE, 87% had 2 or more. Of the total participants, nearly 40% reported 2 or more ACEs and 12% 4 or more. A higher ACE score was strongly related to the development and prevalence of a wide range of health issues over the course of time. A phenomenon known as clustering was also observed—a dose-response pattern where the higher the score, the greater the likelihood of complex health and behavioral issues in life, including co-occurring somatic and behavioral health disorders, even after adjustment for socioeconomic factors. Examples include stroke, cancer, heart disease, pain conditions, numerous mental health conditions such as anxiety and depression, risky health behaviors, and even unemployment.9, 14, 15 Of socioeconomic and demographic interest is that the original study participants were mostly white, middle- and upper-middle class, and college-educated, with access to high-quality health care.
To underscore the importance of the relation between ACEs and health issues, an ACE score of 4 or more increases the likelihood of hepatitis by 230%, chronic pulmonary lung disease by 390%, emphysema or chronic bronchitis by 400%, depression by 460%, and suicide by 1220%.9 Recent research demonstrates that an ACE score of 6 or more increases the odds of depression by 270%, attempted suicide by 2400%, reporting drug use by 370%, and reporting moderate to heavy drinking by 280%, after adjusting for socioeconomic and demographic factors.16 Increased rates of internalizing and externalizing forms of psychopathology,17 attention-deficit hyperactivity disorder,18 and chronic pain correlate to ACE score.19, 20, 21, 22, 23 These are just a few of the numerous associations described in the literature.
ACEs, stress, trauma, and health
Stress and trauma science, psychoneuroimmunology, neuropsychiatry, pediatrics, midwifery and obstetrics, developmental biology, and mind-body medicine research are merging to reveal strong links between ACEs and core biological processes. Stress is an organism’s innate biological response, activated in the face of any environmental, relational, or physical demand. For people, stress can be any physical, mental, or emotional factor that challenges one’s capacity and resources. Stress ranges across a spectrum from eustress (good stress) to distress, where adverse effects may begin to occur. It has both biological and uniquely subjective components.
Although some scientific gaps in elucidating links between ACEs and health remain, the associations point to maladaptive physiological and behavioral mechanisms. Developmentally, stress is normal and even necessary. Experiences such as a skinned knee or being dropped off at daycare contribute to enhanced stress tolerance and build resilience, especially when they occur within a nurturing environment with empathetic caregivers who provide support, validation, and encouragement. But when biological systems develop under high or sustained stress, the function of the nervous, immune, endocrine, and other systems can be affected,24, 25 increasing the risk of developing numerous health problems.26 Chronic stress, independent of historical context, is implicated in illness and chronic disease,27, 28, 29 and adding subsequent stress or trauma onto an ACEs history may have cumulative effects in some individuals. The increased allostatic load that comes with unrelieved stress carries the risk of mechanisms of central sensitization.30 It also has a negative effect on inflammatory, endocrine, and immune processes, influences gene expression, and diminishes the capacity to self-regulate.31 As a result, many individuals with high ACEs may experience physical health problems and/or turn to dysfunctional behaviors and coping strategies including substance use, disordered eating, physical inactivity, violence, and promiscuity.9, 15
Trauma originates from the Greek word for wound. Although originally used solely for physical injuries, contemporary use refers to a range of distressing, disturbing, or overwhelming experiences. Biologically, trauma is rooted in the stress response including mechanisms of the autonomic nervous system. Neurophysiological models of trauma show that the individuality of response to adverse experiences should be a contextual consideration in exploring historical factors influencing a person’s present health.32, 33, 34 In an effort to develop a definition of trauma that addresses some of the numerous constructs, the Substance Abuse and Mental Health Services Administration proposed, “Individual trauma results from an event, series of events, or set of circumstances that is experienced by an individual as physically and emotionally harmful or threatening and that has lasting adverse effects on the individual’s physical, social, emotional, or spiritual well-being.”35(p.7)
ACEs can activate biological stress without being interpreted as stressful at a conscious psychological level. ACEs are potentially traumatic, though they may or may not result in a mental health diagnosis. Psychobiological factors, social support, and epigenetics are examples of factors that influence whether ACEs are experienced as traumatic or lead to the development of posttraumatic stress disorder (PTSD) or other harmful effects. Thus, the experience and expression of trauma is situation and person specific, and stressful events might be experienced as traumatic for some people and not for others. Regardless of whether or not high or unrelieved stress such as that caused by ACEs results in trauma, because of the biological effects they may remain hidden determinants of numerous health conditions and behavioral patterns.
ACEs and trauma-informed care
As the public health movement to incorporate an ACEs- and trauma-informed approach across all levels of care grows,36, 37 research emphasizing the relevance to rehabilitation practice is emerging.38, 39 The disease-focused model of care, where symptom management is the main target, has many benefits and a key role in health care; however, it often falls short in addressing root factors of chronic disease processes. Transdiagnostic approaches can be valuable in addressing these hidden determinants. This is particularly important with conditions such as chronic pain where a biopsychosocial (BPS) model increases capacity to address co-occurring problems38 and the biological underpinnings of stress, trauma, and mind-body bidirectionality.40, 41 To give an example, there is often symptom overlap in patients with chronic pain and those with PTSD, including anxiety, catastrophizing, and avoidance.38, 42, 43, 44, 45
Both integrated (physical and behavioral health care) and integrative (whole-person) models of care across professions can aid in improving existing approaches. These models are particularly relevant when considering the effect of ACEs on health. One such model is trauma-informed care (TIC), an evolving approach to recognizing and addressing the prevalence and effect of trauma within health care. A strength-based service delivery approach that is “grounded in an understanding of and responsiveness to the potential impact of trauma, TIC emphasizes physical, psychological, and emotional safety and creates opportunities for patients to rebuild a sense of control and empowerment.”46
TIC is good care even for those who have not experienced trauma. It was designed around being attuned to the needs of persons with identified trauma, but it represents a model that simply makes good sense, especially given the prevalence of ACEs and the ubiquity of stress in our lives. Raising the subject of ACEs with patients is not necessarily right for every patient or clinical situation, and the decision to proceed must be made on a case-by-case basis. But when the therapist determines the possibility of high psychosocial involvement, as is often true with chronic pain conditions,38, 47, 48, 49, 50, 51 a shift toward the BPS model, including consideration of ACEs, is warranted. Moreover, there is a need to address a continuum of interacting physical and psychosocial factors as part of standard care for all patients due to the inherent interconnectedness of body, mind, and environment. Hence, the general BPS construct combines with the frequency of ACEs and trauma in the population to support the adoption of trauma-informed care as a standard of practice in support of public health efforts. TIC and ACEs-informed care can be introduced as part of a standard BPS interview.
ACE screening and biopsychosocial interviewing
The way in which psychosocial factors and physical factors have been compartmentalized may create unhelpful boundaries in the provision of BPS-informed care.52, 53, 54 An important consideration for wider implementation of ACE-informed and BPS-oriented interviewing is the potential for positive public health effect. This must be weighed against barriers that may exist within individual patients, providers, and systems, in addition to the need for adequate clinician training in effective interventions, responses, and resources.37, 55, 56 Concerns that ACE-informed screening would lead to an increase in demand for services have been shown to be unfounded.57
Practicing active listening as part of cultivating patient-provider alliance is an important component of all therapeutic interactions.58 Regarding ACEs, research has shown that the act of asking about and listening to patients’ experiences is, in itself, likely to have a positive effect on health outcomes.57 A compassionate attitude toward the patient on the part of the provider is critical for the delivery of trauma-informed care.59 Furthermore, the use of an ACE-informed, BPS-oriented patient interview has been shown to significantly reduce subsequent doctor’s office visits by 35% in a large population sample of ∼130,000 patients.37 This was in the absence of any suggestion by the provider of need for psychotherapeutic resource utilization. In comparison, a similar cohort demonstrated a notably smaller 11% reduction of subsequent visits when only standard biomedical interviewing was used.60 Expanding the patient interview to an even broader strategy (supportive inquiry combined with relevant functional education) can reduce pain severity, sleep problems, and global psychological symptoms.61
ACE- and trauma-informed care treatment approaches
Even with ACE questioning as part of a BPS interview, the provider may not know the extent of possible influence or present distress from past experiences. Understanding and applying TIC is an invaluable skillset to support patient safety and enhance the patient care experience.
The implementation of TIC requires additional training for most rehabilitation professionals, because it has not been traditionally incorporated into their core studies. Materials that inform the adoption of TIC in health care practice are available. For example, Menschner and Maul delineate principles of TIC for both clinical and organizational practices. As adapted here, these principles include the following: Empowerment: using patients’ strengths, skills, and preferences in the treatment process. Choice: informing patients of all available safe and efficacious treatment options. Collaboration: maximizing teamwork among health care staff, patients, and their families in the treatment process. Safety: developing health care settings and activities that ensure physical and emotional safety.
Trustworthiness: Communicating clear expectations with patients about the evaluation and treatment process, including logistics and how and by whom care will be provided.62
We have developed a framework for integrated, ACE- and trauma-informed care that builds on these key ingredients. The goal is improved understanding on the part of the rehabilitation professional, with guidelines for how to approach the topic and navigate the patient encounter in a trauma- and ACE-informed manner.
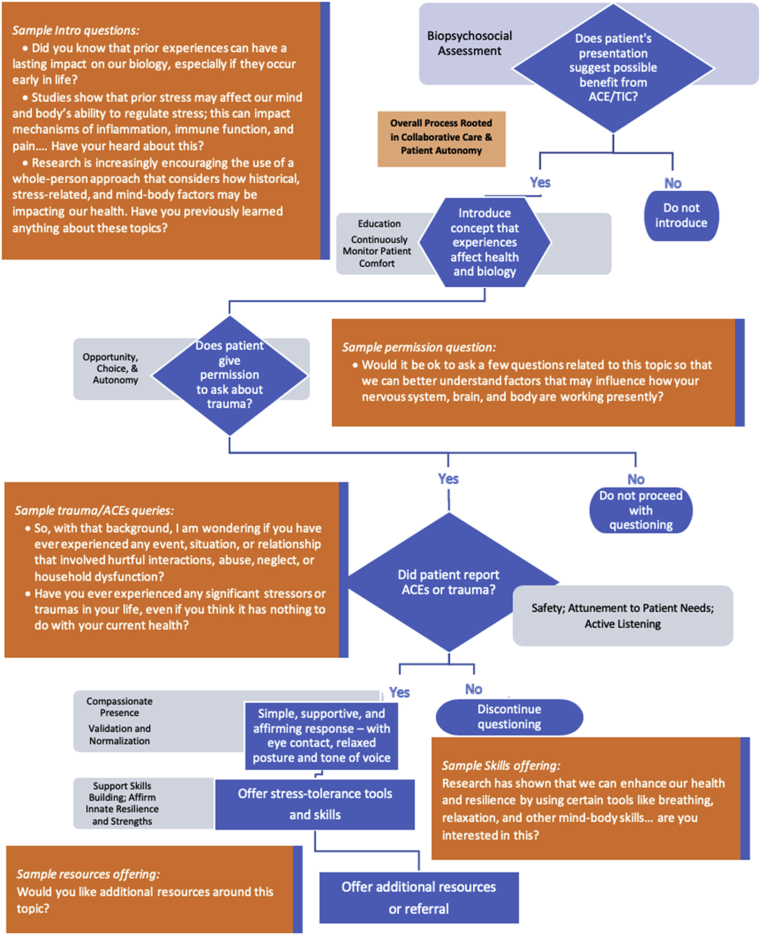
Our framework for exploring ACEs and/or TIC includes a schema with example questions or statements to use at each stage (fig 1). This is built on core principles that inform the examples and expand on Menschner and Maul’s work. It is intended to be a learning tool that combines with clinical judgment to determine if and when it is appropriate to use. The provider should inform the patient of the concept of ACEs because it relates to health and disease in simple terms, with care taken to respect the patient’s intelligence while not assuming familiarity with medical jargon. The framework outlines ways to respond to patient disclosures and prompts the offering of tools, resources, and further treatment support.
Fig 1.
A guide for navigating the process of applying ACEs- and trauma-informed care in the patient encounter in rehabilitation practice.
Opening the door to inquiry as above allows the patient to respond based on his or her individual comfort. Such an approach is sometimes referred to as the look back but don’t stare (as opposed to a probing or content-focused) strategy. The provider inquires directly, yet without judgment, about the person’s story and experiences, remaining mindful of both his or her own and the patient’s body language and tone of voice. A relaxed posture, caring facial expression, and soft tone of voice are suggested, regardless of the response. Time should be taken to give the person a few moments to respond.
Figure 1 provides examples and format for such a dialogue. This is consistent with principles of motivational interviewing and reflects a phenomenological approach that assists the process of self-discovery while respecting each patient’s unique subjective experience.63 It engages the patient’s capacity to delineate her or his own beliefs and needs and to subsequently explore healthy ways to get those needs met.
When patients disclose a history of ACEs or trauma, the provider is mindful to avoid delving into the specific psychological content or detail without specific training in trauma,64 and avoids assumptions about the potential relevance or the meaning ascribed to any such content. Instead, it is recommended to operate from a compassionate presence and subsequent inquiry into the patient’s interest for additional care and resources.
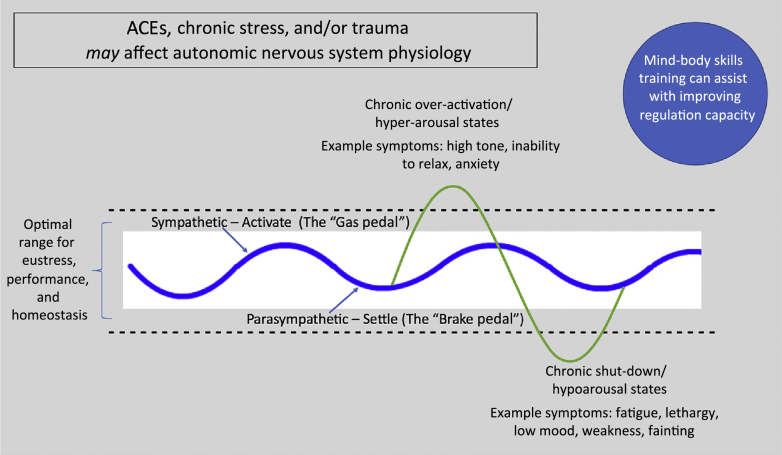
Specific to providing functional education, a short overview of the commonality of ACEs and/or a brief primer on the possible translation into biological effects such as dysregulation of the autonomic nervous system is appropriate. Figure 2 provides an example of such a simple validating education tool that simultaneously supports self-regulation skills training.65, 66 These frameworks can also help normalize the topic as applicable to all persons, regardless of ACE history or symptomatology. Extensive online resources are available to support both patients and professionals in this regard.67
Fig 2.
An example of educational information for use with the patient explaining autonomic nervous system function.
Beyond the introduction of ACEs and general stress education as part of a trauma-informed BPS interview, mind-body skills practices such as breath and body awareness, neuromuscular relaxation training, cognitive behavioral integration, mindfulness and meditation training, biofeedback, guided imagery, Qi Gong, or yoga provide physiological mechanisms of regulation and resilience without a need to directly address specific psychological content.41, 68 Such approaches, which support stress tolerance and resilience, are within the scope of practice of all health care professionals and may require accessing available continuing education programs, contributing to a healing process without crossing the boundaries of professional competence.
Of particular importance in this discussion is the understanding that the psychosocial history of each patient must never be equated with the presence of psychopathology; similarly, ACEs- and trauma-informed practice does not imply mental health practice.48, 49, 52 Rehabilitation professionals using ACEs- and trauma-informed practice constructs can and must respect professional scope of practice by avoiding analysis of psychological content and deferring the diagnosis, assessment, and treatment of psychopathology to mental health professionals. Suicidal ideation with intent is a clear case in which crisis services need to be used, while report of self-harm or other significant mental health need warrants referral to a mental health provider. In other instances, such as relationship distress or an emotional state that interferes with rehabilitation progress, the patient should be asked whether they would like additional support.
TIC also implies a need to be prepared for the presence of comorbidity, such as PTSD in a patient referred for a somatic concern.69 Concurrent mental health services are recommended as appropriate and accessible. Stigma around seeking mental health care can be both individual and culture specific and may prohibit some patients from pursuing further services; this reality reinforces clinical guidelines for cross-disciplinary training to reduce the effect of psychological comorbidity across the health care system.70
Referral to other practitioners is inherent to all professions when the patient’s presentation falls outside a provider’s skill base, comfort level, and/or scope of practice. Simultaneously, rehabilitation professionals can embrace a trauma-informed, BPS model as evidence-based practice to contribute to addressing comorbidity and whole-person care within the scope of practice.71, 72
Conclusion
ACEs are common. Research is uncovering more and more links between ACEs and altered physiological responses that influence stress-management capacity. Safely exploring the topic of ACEs contributes to public health outcomes. Knowledge gained from ACE research assists in breaking down long-standing barriers between mental and physical health care. Raising the issue of ACEs in a skilled, gentle, and compassionate way, while conducting listening-focused inquiry, providing education, and, when appropriate, resources, can enhance clinical care. The topic of ACEs intersects with trauma-informed care. For patient and provider alike, a trauma-informed care model can contribute to better understanding of hidden determinants of health and disease; the utilization of tools such as mind-body skills training that assist with healthy coping; and promoting resiliency by actively and compassionately enlisting the biological substrates of safety, nurturance, and empowerment.
Acknowledgments
We thank Andra DeVoght, PT, MPH, and Matthew J. Taylor, PT, PhD, C-IAYT, who contributed valuable feedback on this article, and Karen Alexander, PhD, for writing assistance.
Footnotes
Disclosures: none.
References
- 1.Garner A.S., Shonkoff J.P., Siegel B.S. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012;129:e224. doi: 10.1542/peds.2011-2662. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Adverse childhood experiences International Questionnaire (ACE-IQ) http://www.who.int/violence_injury_prevention/violence/activities/adverse_childhood_experiences/en/ Available at:
- 3.Multiple Chronic Conditions Chartbook Agency for Healthcare Research & Quality. https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/prevention-chronic-care/decision/mcc/mccchartbook.pdf Available at:
- 4.Engel G.L. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 5.Sulmasy D.P. A biopsychosocial-spiritual model for the care of patients at the end of life. Gerontologist. 2002;42:24–33. doi: 10.1093/geront/42.suppl_3.24. [DOI] [PubMed] [Google Scholar]
- 6.Vancouver J.B. Living systems theory as a paradigm for organizational behavior: understanding humans, organizations, and social processes. Behav Sci. 1996;41:165–204. doi: 10.1002/bs.3830410301. [DOI] [PubMed] [Google Scholar]
- 7.Bell I.R., Caspi O., Schwartz G.E. Integrative medicine and systemic outcomes research: issues in the emergence of a new model for primary health care. Arch Intern Med. 2002;162:133–140. doi: 10.1001/archinte.162.2.133. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education . National Academies Press; Washington (DC): 2011. Relieving pain in America: a blueprint for transforming prevention, care, education, and research.http://www.ncbi.nlm.nih.gov/books/NBK91497/ Available at: [PubMed] [Google Scholar]
- 9.Felitti V.J., Anda R.F., Nordenberg D. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 10.Finkelhor D., Shattuck A., Turner H., Hamby S. Improving the adverse childhood experiences study scale. JAMA Pediatr. 2013;167:70–75. doi: 10.1001/jamapediatrics.2013.420. [DOI] [PubMed] [Google Scholar]
- 11.Cronholm P.F., Forke C.M., Wade R. Adverse childhood experiences: expanding the concept of adversity. Am J Prev Med. 2015;49:354–361. doi: 10.1016/j.amepre.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Marsac M.L., Kassam-Adams N., Delahanty D.L., Widaman K., Barakat L.P. Posttraumatic stress following acute medical trauma in children: a proposed model of bio-psycho-social processes during the peri-trauma period. Clin Child Fam Psychol Rev. 2014;17:399–411. doi: 10.1007/s10567-014-0174-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Afifi T.O., Ford D., Gershoff E.T. Spanking and adult mental health impairment: the case for the designation of spanking as an adverse childhood experience. Child Abuse Negl. 2017;71:24–31. doi: 10.1016/j.chiabu.2017.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu Y., Croft J.B., Chapman D.P. Relationship between adverse childhood experiences and unemployment among adults from five US states. Soc Psychiatry Psychiatr Epidemiol. 2013;48:357–369. doi: 10.1007/s00127-012-0554-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anda R.F., Felitti V.J., Bremner J.D. The enduring effects of abuse and related adverse experiences in childhood: a convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256:174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merrick M.T., Ports K.A., Ford D.C., Afifi T.O., Gershoff E.T., Grogan-Kaylor A. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse Negl. 2017;69:10–19. doi: 10.1016/j.chiabu.2017.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barch D.M., Belden A.C., Tillman R., Whalen D., Luby J.L. Early childhood adverse experiences, inferior frontal gyrus connectivity, and the trajectory of externalizing psychopathology. J Am Acad Child Adolesc Psychiatry. 2018;57:183–190. doi: 10.1016/j.jaac.2017.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jimenez M.E., Wade R., Jr., Schwartz-Soicher O., Lin Y., Reichman N.E. Adverse childhood experiences and ADHD diagnosis at age 9 years in a national urban sample. Acad Pediatr. 2017;17:356–361. doi: 10.1016/j.acap.2016.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davis D.A., Luecken L.J., Zautra A.J. Are reports of childhood abuse related to the experience of chronic pain in adulthood? A meta-analytic review of the literature. Clin J Pain. 2005;21:398–405. doi: 10.1097/01.ajp.0000149795.08746.31. [DOI] [PubMed] [Google Scholar]
- 20.Nelson S., Simons L.E., Logan D. The incidence of adverse childhood experiences (ACEs) and their association with pain-related and psychosocial impairment in youth with chronic pain. Clin J Pain. 2018;34:402–408. doi: 10.1097/AJP.0000000000000549. [DOI] [PubMed] [Google Scholar]
- 21.Sachs-Ericsson N., Kendall-Tackett K., Hernandez A. Childhood abuse, chronic pain, and depression in the National Comorbidity Survey. Child Abuse Negl. 2007;31:531–547. doi: 10.1016/j.chiabu.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 22.Kopec J.A., Sayre E.C. Stressful experiences in childhood and chronic back pain in the general population. Clin J Pain. 2005;21:478–483. doi: 10.1097/01.ajp.0000139909.97211.e1. [DOI] [PubMed] [Google Scholar]
- 23.Imbierowicz K., Egle U.T. Childhood adversities in patients with fibromyalgia and somatoform pain disorder. Eur J Pain. 2012;7:113–119. doi: 10.1016/S1090-3801(02)00072-1. [DOI] [PubMed] [Google Scholar]
- 24.Danese A., Lewis J.S. Psychoneuroimmunology of early-life stress: the hidden wounds of childhood trauma? Neuropsychopharmacology. 2017;42:99–114. doi: 10.1038/npp.2016.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Broyles S.T., Staiano A.E., Drazba K.T., Gupta A.K., Sothern M., Katzmarzyk P.T. Elevated C-reactive protein in children from risky neighborhoods: evidence for a stress pathway linking neighborhoods and inflammation in children. PLoS One. 2012;7:e45419. doi: 10.1371/journal.pone.0045419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shonkoff J.P., Garner A.S., Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 27.Miller G.E., Chen E., Zhou E.S. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychol Bull. 2007;133:25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- 28.Cohen S., Janicki-Deverts D., Miller G.E. Psychological stress and disease. JAMA. 2007;298:1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 29.Aschbacher K., Kornfeld S., Picard M. Chronic stress increases vulnerability to diet-related abdominal fat, oxidative stress, and metabolic risk. Psychoneuroendocrinology. 2014;46:14–22. doi: 10.1016/j.psyneuen.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Radley J., Morilak D., Viau V., Campeau S. Chronic stress and brain plasticity: mechanisms underlying adaptive and maladaptive changes and implications for stress-related CNS disorders. Neurosci Biobehav Rev. 2015;58:79–91. doi: 10.1016/j.neubiorev.2015.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Danese A., McEwen B.S. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav. 2012;106:29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 32.Scaer R.C. The neurophysiology of dissociation and chronic disease. Appl Psychophysiol Biofeedback. 2001;26:73–91. doi: 10.1023/a:1009571806136. [DOI] [PubMed] [Google Scholar]
- 33.Scaer R.C. Routledge; New York: 2014. The body bears the burden: trauma, dissociation, and disease. [Google Scholar]
- 34.Nestler E.J. Epigenetics: stress makes its molecular mark. Nature. 2012;490:171–172. doi: 10.1038/490171a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Substance Abuse Mental Health Services Administration (SAMHSA) A treatment improvement protocol: trauma-informed care in behavioral health services. https://www.integration.samhsa.gov/clinical-practice/SAMSA_TIP_Trauma.pdf Available at: [PubMed]
- 36.Davis M., Costigan T., Schubert K. Promoting lifelong health and well-being: staying the course to promote health and prevent the effects of adverse childhood and community experiences. Acad Pediatr. 2017;17:S4–S6. doi: 10.1016/j.acap.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 37.Felitti V.J. Future applications of the adverse childhood experiences research. J Child Adolesc Trauma. 2017;10:205–206. [Google Scholar]
- 38.Linton S.J., Flink I.K., Vlaeyen J.W. Understanding the etiology of chronic pain from a psychological perspective. Phys Ther. 2018;98:315–324. doi: 10.1093/ptj/pzy027. [DOI] [PubMed] [Google Scholar]
- 39.Wenger S., Drott J., Fillipo R. Reducing opioid use for patients with chronic pain: an evidence-based perspective. Phys Ther. 2018;98:424–433. doi: 10.1093/ptj/pzy025. [DOI] [PubMed] [Google Scholar]
- 40.Muehsam D., Lutgendorf S., Mills P.J. The embodied mind: a review on functional genomic and neurological correlates of mind-body therapies. Neurosci Biobehav Rev. 2017;73:165–181. doi: 10.1016/j.neubiorev.2016.12.027. [DOI] [PubMed] [Google Scholar]
- 41.Taylor A.G., Goehler L.E., Galper D.I., Innes K.E., Bourguignon C. Top-down and bottom-up mechanisms in mind-body medicine: development of an integrative framework for psychophysiological research. Explore (NY) 2010;6:29. doi: 10.1016/j.explore.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Linton S.J. A transdiagnostic approach to pain and emotion. J Appl Biobehav Res. 2013;18:82–103. doi: 10.1111/jabr.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Siqveland J., Ruud T., Hauff E. Post-traumatic stress disorder moderates the relationship between trauma exposure and chronic pain. Eur J Psychotraumatol. 2017;8:1375337. doi: 10.1080/20008198.2017.1375337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Siqveland J., Hussain A., Lindstrøm J.C., Ruud T., Hauff E. Prevalence of posttraumatic stress disorder in persons with chronic pain: a meta-analysis. Front Psychiatry. 2017;8:164. doi: 10.3389/fpsyt.2017.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Asmundson G.J., Coons M.J., Taylor S., Katz J. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry. 2002;47:930–937. doi: 10.1177/070674370204701004. [DOI] [PubMed] [Google Scholar]
- 46.Hopper E.K., Bassuk E., Olivet J. Shelter from the storm: trauma-informed care in homelessness services settings. Open Health Serv Policy J. 2010;3:80–100. [Google Scholar]
- 47.Keefe F.J., Main C.J., George S.Z. Advancing psychologically informed practice for patients with persistent musculoskeletal pain: promise, pitfalls, and solutions. Phys Ther. 2018;98:398–407. doi: 10.1093/ptj/pzy024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Main C.J., George S.Z. Psychologically informed practice for management of low back pain: future directions in practice and research. Phys Ther. 2011;91:820–824. doi: 10.2522/ptj.20110060. [DOI] [PubMed] [Google Scholar]
- 49.Main C.J., George S.Z. Psychosocial influences on low back pain: why should you care? Phys Ther. 2011;91:609–613. doi: 10.2522/ptj.2011.91.5.609. [DOI] [PubMed] [Google Scholar]
- 50.Nicholas M.K., Linton S.J., Watson P.J., Main C.J., “Decade of the Flags” Working Group Early identification and management of psychological risk factors (“yellow flags”) in patients with low back pain: a reappraisal. Phys Ther. 2011;91:737–753. doi: 10.2522/ptj.20100224. [DOI] [PubMed] [Google Scholar]
- 51.Linton S.J., Shaw W.S. Impact of psychological factors in the experience of pain. Phys Ther. 2011;91:700–711. doi: 10.2522/ptj.20100330. [DOI] [PubMed] [Google Scholar]
- 52.O’Keeffe M., George S.Z., O’Sullivan P.B., O’Sullivan K. Psychosocial factors in low back pain: letting go of our misconceptions can help management. Br J Sports Med. 2018 doi: 10.1136/bjsports-2018-099816. [DOI] [PubMed] [Google Scholar]
- 53.Lewis J., O'Sullivan P. Is it time to reframe how we care for people with non-traumatic musculoskeletal pain? Br J Sports Med. 2018;52:154. doi: 10.1136/bjsports-2018-099198. [DOI] [PubMed] [Google Scholar]
- 54.Craik R.L. A convincing case—for the psychologically informed physical therapist. Phys Ther. 2011;91:606–608. doi: 10.2522/ptj.2011.91.5.606. [DOI] [PubMed] [Google Scholar]
- 55.Finkelhor D. Screening for adverse childhood experiences (ACEs): cautions and suggestions. Child Abuse Negl. 2018;85:174–179. doi: 10.1016/j.chiabu.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 56.Anda R.F., Brown D.W. Root causes and organic budgeting: funding health from conception to the grave. Pediatr Health. 2007;1:141–143. [Google Scholar]
- 57.McGee C., Hughes K., Quigg Z., Bellis M., Larkin W., Lowey H. A scoping study of the implementation of Routine Enquiry about Childhood Adversity (REACh) http://www.cph.org.uk/wp-content/uploads/2015/07/REACh-Scoping-Study-BwD.pdf Available at:
- 58.Diener I., Kargela M., Louw A. Listening is therapy: patient interviewing from a pain science perspective. Physiother Theory Pract. 2016;32:356–367. doi: 10.1080/09593985.2016.1194648. [DOI] [PubMed] [Google Scholar]
- 59.Brown J.D., King M.A., Wissow L.S. The central role of relationships with trauma-informed integrated care for children and youth. Acad Pediatr. 2017;17:S94–S101. doi: 10.1016/j.acap.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 60.Felitti V.J., Anda R.F. The lifelong effects of adverse childhood experiences. In: Alexander R., Esernio-Jenssen D., editors. 4th ed. Vol 2. STM Learning, Inc; St. Louis: 2014. (Chadwick’s child maltreatment: sexual abuse and psychological maltreatment, encyclopedic). [Google Scholar]
- 61.Ziadni M.S., Carty J.N., Doherty H.K. A life-stress, emotional awareness, and expression interview for primary care patients with medically unexplained symptoms: a randomized controlled trial. Health Psychol. 2018;37:282–290. doi: 10.1037/hea0000566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Menschner C., Maul A. Key Ingredients for successful trauma-informed care implementation. http://www.chcs.org/media/ATC_whitepaper_040616.pdf Available at:
- 63.Miller W., Rollnick S. 3rd ed. Guilford; New York: 2013. Motivational interviewing: helping people change. [Google Scholar]
- 64.Raja S., Hasnain M., Hoersch M., Gove-Yin S., Rajagopalan C. Trauma informed care in medicine: current knowledge and future research directions. Fam Community Health. 2015;38:216–226. doi: 10.1097/FCH.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 65.Corrigan F., Fisher J., Nutt D. Autonomic dysregulation and the Window of Tolerance model of the effects of complex emotional trauma. J Psychopharmacol. 2010;25:17–25. doi: 10.1177/0269881109354930. [DOI] [PubMed] [Google Scholar]
- 66.Ogden P., Minton K., Pain C. 1st ed. W.W. Norton; New York: 2006. Trauma and the body: a sensorimotor approach to psychotherapy. [Google Scholar]
- 67.ACEs Connection Resource Center ACEsConnection. https://www.acesconnection.com/g/resource-center Available at:
- 68.Gard T., Noggle J.J., Park C.L., Vago D.R., Wilson A. Potential self-regulatory mechanisms of yoga for psychological health. Front Hum Neurosci. 2014;8:770. doi: 10.3389/fnhum.2014.00770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dunleavy K., Kubo Slowik A. Emergence of delayed posttraumatic stress disorder symptoms related to sexual trauma: patient-centered and trauma-cognizant management by physical therapists. Phys Ther. 2012;92:339–351. doi: 10.2522/ptj.20100344. [DOI] [PubMed] [Google Scholar]
- 70.Institute for Clinical Systems Improvement (ICSI) Pain: assessment, non-opioid treatment approaches and opioid. www.icsi.org/_asset/bw798b/ChronicPain.pdf Available at:
- 71.Russek L., McManus C. A practical guide to integrating behavioral and psychologically informed approaches into physical therapist management of patients with chronic pain. Orthopaedic Practice. 2015;27:8–16. [Google Scholar]
- 72.Occupational therapy services in the promotion of psychological and social aspects of mental health. Am J Occup Ther. 2010;64(Suppl):S78–S91. [Google Scholar]