Abstract
Introduction:
Understanding the drivers of health care utilization patterns following disasters can better support health planning. This study characterized all-cause hospitalizations among older Americans after eight large-scale hurricanes.
Study Objective:
The objective of this study was to characterize all-cause hospitalizations for any cause among older Americans in the 30 days after eight large-scale hurricanes.
Methods:
A self-controlled case series study among Medicare beneficiaries (age 65+) exposed to one of eight hurricanes was conducted. The predicted probability of sociodemographic factors associated with hospitalization using logit models was estimated.
Results:
Hurricane Sandy (2012) had the highest post-hurricane admission rate, a 23% increase (incidence rate ratio [IRR] = 1.23; 95% CI, 1.22–1.24), while Hurricane Irene in 2011 had only a 10% increase (IRR = 1.10; 95% CI, 1.09–1.11). Higher likelihood of hospitalization occurring after hurricanes included being 85 or older (36.8% probability of hospitalization; 95% CI, 34.7–39.0) and being dually eligible for Medicare and Medicaid (62.8%; 95% CI, 60.7–64.9).
Conclusion:
Planning to address the surge in hospitalization for a longer time period after hurricanes and interventions targeted to support aging Americans are needed.
Keywords: delivery of health care, disaster, disaster preparedness, older adults
Introduction
Disasters are unpredictable, chaotic events that can have a serious impact on the health of older adults. Age-related changes such as decreased mobility, cognitive deficits, frailty, limited financial resources, and the presence of chronic and comorbid disease predispose older adults to more serious health consequences during the intra-disaster period. During a disaster, there may be disruption of services at the household and community levels that complicate access to needed routine health care. Indeed, the eight recent large-scale hurricanes included in this study were each associated with loss of electricity, mass evacuations, and temporary to permanent closure of health systems which provided care for thousands of individuals. The impact of the disruption of essential services caused by these storms can be understood through the health breakdowns that occur among older adults and resultant health care costs.
After a disaster, effects on health differ depending on a number of factors, including sociodemographic characteristics (such as age, sex, race/ethnicity, the presence of co-morbidities, and poverty), and not just the disaster itself. Older adults remain affected by disaster longer than expected, beyond the immediate recovery period and beyond the period explicable by injuries and trauma from the disaster. These long-term effects include changes in health behaviors, excess hospitalizations, and in some cases, mortality.1,2 Other studies have examined the impact of diabetes-related hospital admissions after Hurricanes Katrina (2005) and Rita (2005),3 hypertension among US veterans,4 and of course, Hurricane Maria (2017) related mortality.5 Prior studies limited to examining a single disaster suggest that exposure to hurricanes may affect the health of older adults. There is a clear need to understand patterns of morbidity for older adults after large-scale disasters and emergencies. Indirect effects from disaster—loss of electricity, limited transportation, lack of access to health care, and poor nutrition—have consequences on health outcomes.
To this point, the aging population is growing exponentially,6 alongside a rapid rise in the incidence of chronic disease.7 The effects on already-strained health care systems of a combination of a rise in population of older adults, an increase in incidence of chronic disease, and more intense and severe disasters are obvious. However, there is not sufficient evidence currently of what these impacts are. Examining hospitalizations among older adults after disaster in recent, highest cost, and arguably most severe hurricane disasters can describe the extent to which older adults are affected by these events.
Therefore, all-cause hospitalizations were examined among older Americans in the 30-day period after eight of the most costly, large-scale hurricanes in recent history.
Methods
Among a large sample of older adults (age 65 and older), a self-controlled case series study was conducted using a combination of Medicare administrative claims data from eight federally declared hurricane disasters from 2004–2012. The change in all-cause hospital admissions in the 30 days after each large-scale hurricane was determined when compared to the rest of the calendar year. This study received ethical approval from the University of Michigan (Ann Arbor, Michigan USA) Health and Behavioral Sciences institutional review board (HUM00144124).
Data Source
The Medicare Provider and Analysis Review File (MedPAR), combined with Medicare beneficiary claims data, was used as the individual-level data source. The MedPAR contains final action stay records for acute in-patient hospitalizations for individuals aged 65 or older and contains information for all fee-for-service Medicare beneficiaries using hospital in-patient services,8 and those who were not fee-for-service beneficiaries were excluded. The study sample included individuals who resided in counties with a federal disaster declaration for Individual Assistance (IA) after one of eight recent, large-scale hurricanes. To reduce bias, individuals who died during the interval being examined were excluded from the study.
Identification of Hurricane Exposure
The hurricanes were selected based on National Oceanic and Atmospheric Administration (NOAA; Washington, DC USA) estimates of total cost, and were among the most costly hurricane disasters occurring from 2004 through 2012.9 These were: Frances in 2004, Ivan in 2004, Wilma in 2005, Rita in 2005, Katrina in 2005, Ike in 2008, Irene in 2011, and Sandy in 2012 (Table 1). The primary exposure variable was defined as the 30 days after exposure to one of eight hurricane disasters (Table 1). This was compared with all other days during the same calendar year as the disaster. The disaster-exposed sample included residents of any county which experienced major hurricanes with Federal Emergency Management Agency (FEMA; Washington, DC USA) disaster declarations10 requiring IA support. Individual Assistance provides support to families and individuals in counties with federal disaster declarations and is conceptualized in this study as a more-specific measure of severity of disaster exposure. An older adult was considered exposed if their ZIP code resided in an affected county.
Table 1.
Hurricane Disasters Included in Study
| Disaster | Month of Landfall | Cost | Category at Landfall | Landfall Location |
|---|---|---|---|---|
| Hurricane Katrina | August 2005 | $160.0b | 5 | Orleans Parish, Louisiana |
| Hurricane Sandy | October 2012 | $70.2b | 1 | Atlantic County, New Jersey |
| Hurricane Ike | September 2008 | $34.8b | 2 | Galveston County, Texas |
| Hurricane Ivan | September 2004 | $27.1b | 3 | Baldwin County, Alabama |
| Hurricane Wilma | October 2005 | $24.3b | 2 | Collier County, Florida |
| Hurricane Rita | September 2005 | $23.7b | 3 | Jefferson County, Texas |
| Hurricane Irene | August 2011 | $15.0b | 1 | Carteret County, North Carolina |
| Hurricane Frances | August 2004 | $13.6b | 2 | Martin County, Florida |
Note: Cost was consumer price index adjusted. Source: Billion-Dollar Weather and Climate Disasters - https://www.ncdc.noaa.gov/billions/events/US/2000-2015.
All-Cause Hospitalization
The primary outcome was all-cause hospital admission among fee-for-service Medicare beneficiaries in the 30-day period after each of the identified disasters. Hospitalizations that included an intensive care unit (ICU) admission were examined separately.
As an additional sensitivity analysis, the hypothesis was tested that immediate injuries and trauma may have accounted for the increased hospitalizations in the immediate period after the disaster. To do this, the first three days after the hurricane were excluded using two storms: Hurricane Irene, which had the lowest rate of hospital admissions; and Hurricane Sandy, which had the highest.
Statistical Analyses
In order to assess the short-term outcome on the acute exposure of a disaster, a self-controlled case series analysis was conducted, where the within-person differences in the rate of hospital admissions in the 30 days following each hurricane were estimated. Self-controlled case series methodology has been well-explained in the scientific literature,11 where analyses have been used in prior studies of disaster morbidity,2 adverse reactions to vaccines,12 and sepsis outcomes.13 This case-crossover methodology, where individuals serve as their own controls and confounders are controlled for within the modeling, is ideal for secondary data analysis in which limited information is available on potential confounders.11 As this method examines within-person differences based on an event, covariates such as functional status, income, or education are controlled for in the analysis without the need to directly measure them. One claim per hospitalization was examined in order to avoid double counting hospitalizations. Effect estimates were expressed as incidence rate ratios (IRRs).
Logit models were used to estimate the predicted probability of hospitalization following exposure to explore how the risk of hospitalization differs according to specific characteristics. These factors were decided on a priori and based on literature review and clinical relevance, including age, sex, race, and ethnicity. Dual eligibility for Medicare and Medicaid was used as a proxy measure for poverty (and limited to adults aged 65 or older). A multi-level logit model conditional on hurricane-specific random effect (random intercept model) was constructed using the categorical individual level-factors. Covariates in the models used to predict hospitalization in the 30 days after the hurricane included age, sex, race and ethnicity, dual eligibility, comorbidity (using Elixhauser Comorbidity Index14), and hospitalization prior to the hurricane (12 months). Stata (version 15.1; StataCorp, College Station, Texas USA) was used for all analyses. All hypothesis tests were two-sided and used a critical alpha level of 0.05.
Results
There were 2,404,079 fee-for-service beneficiaries that met the study criteria of residing in a disaster-affected area during the study years. After excluding 273,780 beneficiaries as they died during the study period, the total number included in the study was 2,130,299 persons. The mean age was 75.6 years old, 57.4% of the sample was female, and 84.2% were White, non-Hispanic (Table 2). The majority (87.6%) lived in urban environments, 14.5 % were from rural areas, and 12.5% were dually eligible for Medicare and Medicaid.
Table 2.
Demographic Characteristics of Study Sample
| Total Sample | Frances, 2004 | Ivan, 2004 | Katrina, 2005 | Wilma, 2005 | Rita, 2005 | Ike, 2008 | Irene, 2011 | Sandy, 2012 | |
|---|---|---|---|---|---|---|---|---|---|
| Mean Age, years (SD) | 75.6 (SD = 8.0) |
75.3 (SD = 7.4) |
74.8 (SD = 7.3) |
74.9 (SD = 7.6) |
75.6 (SD = 7.6) |
74.4 (SD = 7.3) |
75.4 (SD = 7.9) |
76.4 (SD = 8.6) |
76.3 (SD = 8.6) |
| Gender | |||||||||
| Female | 6.68 (57.4) | 1.00 (56.6) | 1.35 (57.5) | 0.32 (58.9) | 0.41 (56.8) | 0.34 (57.5) | 0.35 (56.3) | 1.60 (57.7) | 1.31 (57.9) |
| Male | 4.95 (42.6) | 0.77 (43.4) | 1.00 (42.5) | 0.22 (41.1) | 0.31 (43.2) | 0.25 (42.5) | 0.27 (43.7) | 1.17 (42.3) | 0.95 (42.1) |
| Race and Ethnicity | |||||||||
| White, non-Hispanic | 9.79 (84.2) | 1.58 (89.8) | 2.07 (87.7) | 0.42 (77.3) | 0.62 (87.1) | 0.48 (80.9) | 0.50 (81.3) | 2.29 (82.5) | 1.83 (80.9) |
| Black, non-Hispanic | 1.20 (10.3) | 0.10 (5.7) | 0.25 (10.6) | 0.12 (21.6) | 0.04 (5.10) | 0.08 (14.0) | 0.08 (13.6) | 0.29 (10.6) | 0.23 (10.2) |
| Hispanic | 0.26 (2.20) | 0.06 (3.2) | 0.015 (0.7) | 0.001 (0.2) | 0.04 (6.30) | 0.01 (2.1) | 0.01 (1.90) | 0.06 (2.10) | 0.06 (2.5) |
| Other/Multiple | 0.38 (3.30) | 0.024 (1.3) | 0.025 (1.0) | 0.005 (0.9) | 0.01 (1.50) | 0.02 (3.0) | 0.02 (3.20) | 0.13 (4.80) | 0.14 (6.4) |
| Rurality | |||||||||
| Urban | 10.2 (87.7) | 1.63 (92.3) | 1.91 (81.2) | 0.32 (59.2) | 0.69 (96.6) | 0.46 (76.6) | 0.45 (72.8) | 2.50 (90.4) | 2.22 (98.3) |
| Rural | 1.40 (12.3) | 0.14 (7.70) | 0.44 (18.8) | 0.22 (40.8) | 0.024 (3.40) | 0.14 (23.4) | 0.17 (27.2) | 0.27 (9.60) | 0.04 (1.70) |
| Dual Medicare/Medicaid Eligibility | |||||||||
| No | 10.17 (87.5) | 1.57 (88.9) | 2.08 (88.1) | 0.44 (81.5) | 0.61 (85.5) | 0.51 (86.1) | 0.54 (87.7) | 2.45 (88.4) | 1.96 (86.9) |
| Yes | 1.46 (12.5) | 0.20 (11.1) | 0.28 (11.9) | 0.10 (18.5) | 0.10 (14.5) | 0.08 (13.9) | 0.08 (12.3) | 0.32 (11.6) | 0.30 (13.1) |
| Number of Elixhauser Comorbidities | |||||||||
| 0 | 10.1 (86.6) | 1.51 (85.8) | 2.02 (85.5) | 0.46 (85.2) | 0.63 (87.9) | 0.52 (87.6) | 0.53 (86.3) | 2.41 (87.0) | 1.98 (87.6) |
| 1 to 3 | 1.2 0 (10.4) | 0.20 (11.2) | 0.27 (11.5) | 0.06 (11.9) | 0.07 (9.8) | 0.06 (9.8) | 0.06 (10.4) | 0.28 (10.2) | 0.20 (8.7) |
| More than 3 | 0.35 (3.0) | 0.05 (3.0) | 0.07 (3.0) | 0.01 (2.9) | 0.02 (2.3) | 0.01 (2.6) | 0.02 (3.3) | 0.08 (2.8) | 0.08 (3.7) |
| Hospitalization in Prior Month of Year Before | |||||||||
| No | 9.94 (85.5) | 1.51 (85.5) | 1.99 (84.5) | 0.46 (83.9) | 0.60 (83.6) | 0.50 (84.0) | 0.53 (85.4) | 2.42 (87.2) | 1.94 (86.0) |
| Yes | 1.68 (14.5) | 0.26 (14.5) | 0.37 (15.5) | 0.09 (16.1) | 0.12 (16.4) | 0.09 (16.0) | 0.09 (14.6) | 0.35 (12.8) | 0.32 (14.0) |
Note: Numbers in mean (SD) or number in millions (%).
All-Cause Hospitalizations
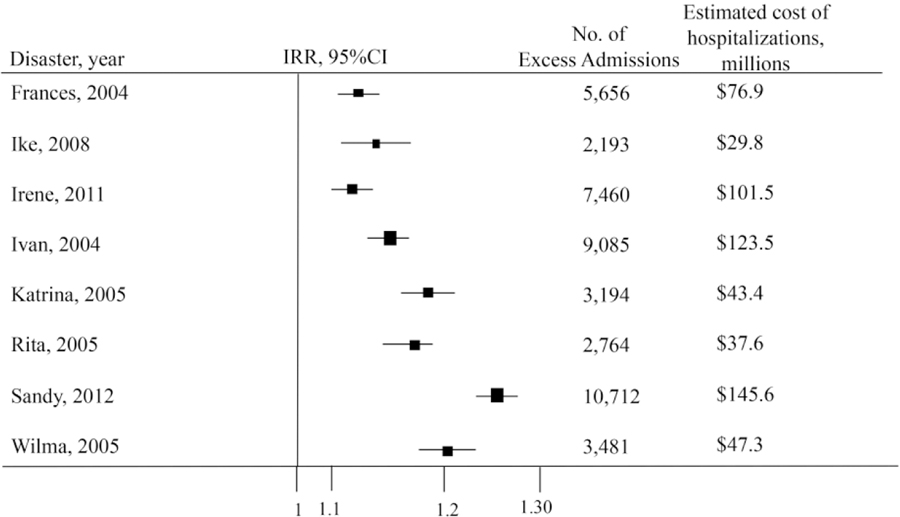
All-cause hospitalizations increased in the 30 days after exposure for all eight hurricanes studied. Hospitalizations varied between 10% to 23% higher in the 30 days after the event when compared to the other 11 months of the year.
Hurricane Sandy had the highest post-hurricane admission rate increase, an increase of 23% (IRR = 1.23; 95% CI, 1.22–1.24), resulting in 10,712 additional admissions; whereas Hurricane Irene in 2011 resulted in an increase of only 10% (IRR = 1.10; 95% CI, 1.09–1.11). All other hurricanes included in the analysis showed significant increases in hospital admissions. Specifically, the other hurricanes were: Hurricane Wilma (IRR = 1.20; 95% CI, 1.18–1.22); Hurricane Rita (IRR = 1.15; 95% CI, 1.14–1.17); Hurricane Ivan (IRR = 1.14; 95% CI, 1.13–1.15); Hurricane Frances (IRR = 1.12; 95% CI, 1.11–1.13); and Hurricane Ike (IRR = 1.11; 95% CI, 1.11–1.13). Intensive care unit admissions were also elevated across all eight disasters, ranging from a 37% increase after Hurricane Sandy (IRR = 1.37; 95% CI, 1.34–1.39) to a 15% increase after Hurricane Frances (IRR = 1.15; 95% CI, 1.13–1.17; Table 3).
Table 3.
Hospital Admissions Including ICU Stay Among FFS Medicare Beneficiaries after Large-Scale Disaster
| Hospitalization | |||||
|---|---|---|---|---|---|
| Disaster, Year | Total in Study Period | Disaster-Exposure Period | Non-Exposure Period | IRR | 95% CI |
| Frances, 2004 | 577,792 | 52,601 | 525,191 | 1.15 | (1.13–1.17) |
| Ivan, 2004 | 789,152 | 73,104 | 716,048 | 1.20 | (1.18–1.22) |
| Katrina, 2005 | 212,310 | 20,349 | 191,961 | 1.20 | (1.16–1.24) |
| Wilma, 2005 | 226,877 | 21,819 | 205,058 | 1.25 | (1.22–1.28) |
| Rita, 2005 | 218,507 | 20,489 | 198,018 | 1.16 | (1.14–1.17) |
| Ike, 2008 | 208,120 | 19,075 | 189,045 | 1.22 | (1.19–1.26) |
| Irene, 2011 | 799,853 | 72,225 | 727,628 | 1.15 | (1.13–1.17) |
| Sandy, 2012 | 597,026 | 58,655 | 538,371 | 1.37 | (1.34–1.39) |
Abbreviations: FFS, fee-for-service; ICU, intensive care unit; IRR, incidence rate ratio.
Two separate sensitivity analyses were conducted. First, the first three days were removed from two selected hurricane disasters, hypothesizing that this time period would account for injuries or immediate trauma. When removing these first three days after Hurricane Sandy, which had the highest admission IRR, and Hurricane Irene, which had the lowest, hospital admissions remained elevated: Hurricane Sandy (IRR = 1.21; 95% CI, 1.20–1.22 versus IRR = 1.23; 95% CI, 1.22–1.24) and Irene (IRR = 1.11; 95% CI, 1.10–1.11 versus IRR = 1.10; 95% CI, 1.09–1.11).
Post-Estimation Analyses
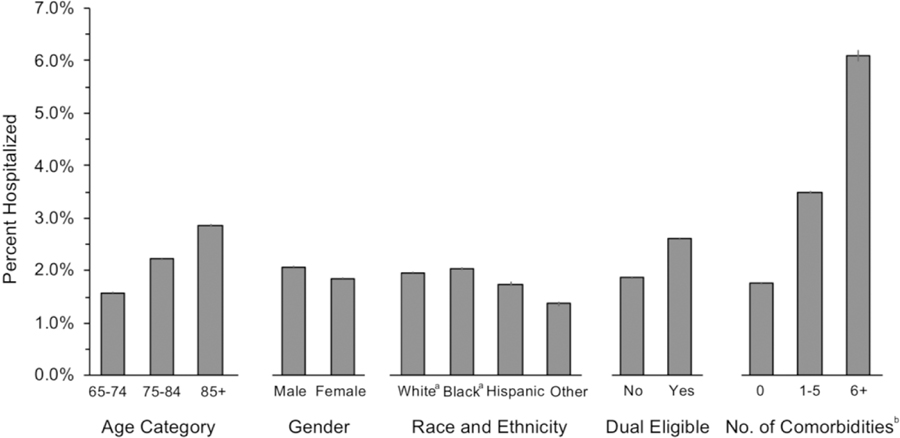
The predicted probability of hospitalization in the 30 days after disaster was examined for the total sample, controlling for multiple covariates. The oldest (85 or greater years) had the highest predictive probability of post-disaster hospitalization (36.8%; 95% CI, 34.7%–39.0%) compared to the other two categories of age: 65 to 74 (29.9%; 95% CI, 28.0%–31.7%) and 75–84 (33.3%; 95% CI, 31.4%–35.3%). Men had a higher predicted probability than women: 38.4% (95% CI, 36.8%–40.1%) compared to 27.5% (95% CI, 25.3%–29.5%). Race/ethnicity was also a factor, where Whites (27.8%; 95% CI, 26.1%–29.4%) had the lowest predicted probability of hospitalization after disaster compared with Blacks, Hispanics, and other races. Those who were dually eligible for Medicare and Medicaid, the proxy for poverty, had a 62.8% (95% CI, 60.7%–64.9%) higher predicted probability of hospitalization than those who had Medicaid only (27.7%; 95% CI, 25.9%–29.6%). Finally, using the Elixhauser co-morbidity index, the predicted probability for those with three or greater co-morbidities was 49.9% (95% CI, 49.3%–50.4%; Figure 1).
Figure 1.
Percent Hospitalized in 30 Days Following Hurricane Landfall According to Characteristics among Older Adults.
Note: All analyses adjusted for prior hospitalization and all other characteristics shown error bars represent 95% confidence intervals.
a Non-Hispanic.
b Number of comorbidities based on the Elixhauser comorbidity index in year prior to hurricane.
Discussion
This is one of relatively few studies to characterize all-cause hospitalizations among older adults across multiple, large-scale hurricanes that occurred in recent history. This study found, regardless of the population and across different hurricanes, hospitalizations increased for the 30 days following the hurricane (even after removing the acute phase of a few days following the storm). However, there was variability in the extent to which hospitalizations increased following storms – for instance, the largest changes in hospitalizations occurred following Hurricane Sandy, whereas smaller changes were observed for Hurricane Irene. Vulnerable and at-risk groups had the highest probability of hospitalization after disaster: the oldest (85+), those living in poverty (ie, dual eligible), and those with multiple co-morbidities. This study demonstrates that the effects of disasters extend beyond the initial period following these events and underscores the need for long-term community recovery that takes into account the needs of structurally marginalized populations.
The sizeable increase in hospitalizations identified across the eight separate hurricanes calls attention to the need for an understanding of the factors specific to the disaster and subsequent community disruption associated with this increase. The results align with previous work. Previous studies have found that hospital admissions after one tornado-related disaster were associated with an increase in the month after the disaster.2 Elevations in post-disaster geriatric emergency department visits15 and cardiac events16 were seen after Hurricane Sandy, and also in a combined study looking at Hurricanes Rita and Katrina.3,17
This study also found significant increases in all-cause hospital admissions when examining eight separate, large-scale hurricanes. Prior research has described surges in hospitalization after hurricanes, however most of these reports have been limited to one disaster18 or the immediate period after a disaster. The findings of this study, using one of the largest sources of health data on older adults, studying hospitalizations in the 30 days after eight separate disasters advances the understanding of the health effects of disaster on older adults. Pre-disaster ZIP codes were used as the baseline for analyses, thereby allowing for inclusion of individuals who left the area after the hurricanes—provided that they received care somewhere in the US that was covered by Medicare. This is an important strength of this study as it considers the migration of disaster-displaced populations,19–21 a key limitation in other studies where the disaster-displaced are often lost to follow-up. Further, the time of the year the hurricanes occurred (Table 1) suggests that the increase in admission was not related to seasonal variation.
Disasters and their associated costs have been estimated through the NOAA’s widely-cited billion-dollar consumer price index (CPI)-adjusted estimates.9 However, the methods used to estimate these costs explicitly exclude “health care related losses, or values associated with loss of life.”22 These costs are currently unknown and unestimated. This study attempted to do this by using the 2016 estimates of cost of average hospital stay from the Healthcare Cost and Utilization Project (HCUP)23 where average hospital stay costs for Medicare beneficiaries were estimated at $13,600 and $14,500 for adults aged 65–84. In this study, 44,265 excess hospital admissions were found across the eight hurricanes studied. Applying this to the HCUP estimates, excess costs for older adults in sum were $641,842,500. Excess costs for Medicare beneficiaries were $602,004,000 (Figure 2). Patients sent to the ICU are among the most vulnerable and resource-intensive patients. Hospital stays that include ICU services have been estimated to be two-and-one-half-times more costly than other hospital stays.24 The large cost associated with increases in hospitalizations following hurricanes underscores the importance of policy implications of cost for disaster-related admissions.
Figure 2.
All-Cause Hospital Admissions in 30 Days After Hurricane, Compared to the Rest of the Same Year.
Abbreviation: IRR, incidence rate ratio.
Tracking the health effects of disaster on older adults is critical at all levels of disaster response, which can significantly inform disaster planning, but also planning for health care systems and those focused on healthy aging. Understanding the individual characteristics of those who are more likely to be admitted to the hospital after a disaster can help guide decision making on resource allocation and preparedness for older adults. Finally, future research should explore the impact of local and state variation in both emergency management and in aging policy and services surrounding disasters.
Policy Implications
This study highlights an important gap in policy related to disasters and health care: that health needs, and health care utilization, remain elevated far after the immediate impact—which is where the policy focus currently lies. Further, this study points to the considerable health care cost implications associated with disaster among older Americans. Finally, the results reported here address a gap in understanding of health care utilization patterns after disasters, which can support policymakers to anticipate long-term population health needs by coordinating resource sharing and strengthening regional planning among hospitals in disaster-affected areas. Future research to explain the differences in rates of hospitalizations after different hurricane disasters, as found in this study, can further support health systems and emergency planners to plan for needed health care services after a hurricane.
Limitations
This study was not without several limitations. Firstly, this study design does not directly adjust for confounders such as age, sex, income, education, or race and ethnicity. However, in the within-person design of this study, participants serve as their own control (before versus after), which is a strength. Second, the study was limited to fee-for-service Medicare beneficiaries aged 65 years and older that may affect the generalizability of the findings. Results may differ among older Americans enrolled in Medicare Advantage plans that are typically healthier. Finally, the possibility of misclassification of hurricane exposure cannot completely be ruled out. Disaster declarations are at the county level, and do not allow for measurement of the differential effects of the hurricanes within these counties, where community-wide damages may have differed greatly.
Conclusion
Disasters are increasing in frequency and severity across the United States. Understanding the extent to which the health of older adults is affected by disasters is critically important. This self-controlled case series study using administrative claims data found significant increases in all-cause hospital admissions across all eight hurricanes. Using data-driven evidence, as provided in this study, can guide federal, state, and local planning and the deployment of resources to support older adults and the health care systems that serve them in the event of a disaster.
Abbreviations:
- HCUP
Healthcare Cost and Utilization Project
- IRR
incidence rate ratio
- IA
Individual Assistance
- ICU
intensive care unit
- MedPAR
Medicare Provider and Analysis Review File
- NOAA
National Oceanic and Atmospheric Administration
Footnotes
Conflict of interest: All authors that have contributed significantly to this research have been listed. To the best of their knowledge, no conflict of interest, financial or other, exists. None of the authors have published, posted, or submitted any related papers from the same study.
References
- 1.Bell SA, Choi H, Langa KM, Iwashyna TJ. Health risk behaviors after disaster exposure among older adults. Prehosp Disaster Med. 2019;34(1):95–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bell SA, Abir M, Choi H, Cooke C, Iwashyna TJ. All-cause hospital admissions among older adults after a natural disaster. Ann Emerg Med. 2017;71(6):746–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Quast T, Andel R, Sadhu AR. Long-term effects of disasters on seniors with diabetes: evidence from Hurricanes Katrina and Rita. Diabetes Care. 2019;42(11):2090–2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baum A, Barnett M, Wisnivesky J, Schwartz M. Association between a temporary reduction in access to health care and long-term changes in hypertension control among veterans after a natural disaster. JAMA Network Open. 2019;2(11):e1915111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kishore N, Marqués D, Mahmud A, et al. Mortality in Puerto Rico after Hurricane Maria. N Eng J Med. 2018;379(2):162–170. [DOI] [PubMed] [Google Scholar]
- 6.He W, Goodkind D, Kowal P. An Aging World: 2015. Washington, DC USA: US Census Bureau; 2016. [Google Scholar]
- 7.National Institutes of Health. Supporting Older Patients with Chronic Conditions: National Institutes of Health. https://www.nia.nih.gov/health/supporting-older-patients-chronic-conditions. Accessed June 2020.
- 8.Centers for Medicare & Medicaid Services. MEDPAR 2017. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/MedicareFeeforSvcPartsAB/MEDPAR.html. Accessed June 2020. [PubMed]
- 9.National Centers for Environmental Information. Billion-Dollar Weather and Climate Disasters: National Oceanic and Atmospheric Administration. https://www.ncdc.noaa.gov/billions/. Accessed June 2020.
- 10.Federal Emergency Management Agency. Disaster Declarations 2019. https://www.fema.gov/disasters. Accessed June 2020.
- 11.Petersen I Self-controlled case series methods: an alternative to standard epidemiological study designs. BMJ. 2016;354(i4515). [DOI] [PubMed] [Google Scholar]
- 12.Cohet C, Haguinet F, Dos Santos G, et al. Effect of the adjuvanted (AS03) A/H1N1 2009 pandemic influenza vaccine on the risk of rejection in solid organ transplant recipients in England: a self-controlled case series. BMJ Open. 2016;6(1):e009264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prescott HC, Dickson RP, Rogers MA, Langa KM, Iwashyna TJ. Hospitalization type and subsequent severe sepsis. Am J Respir Crit Care Med. 2015;192(5):581–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 15.Malik S, Lee DC, Doran KM, et al. Vulnerability of older adults in disasters: emergency department utilization by geriatric patients after Hurricane Sandy. Disaster Med Public Health Prep. 2018;12(2):184–193. [DOI] [PubMed] [Google Scholar]
- 16.Swerdel JN, Janevic TM, Cosgrove NM, Kostis JB. The effect of Hurricane Sandy on cardiovascular events in New Jersey. J Am Heart Assoc. 2014;3(6):e001354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quast T Emergency department visits by and hospitalizations of senior diabetics in the three years following Hurricanes Katrina and Rita. Econ Disasters Climate Change. 2019;3(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stephens W, Wilt GE, Lehnert EA, Molinari NM, LeBlanc TT. A spatial and temporal investigation of medical surge in Dallas-Fort Worth during Hurricane Harvey, Texas; 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Groen J, Polivka A. Hurricane Katrina evacuees: who they are, where they are, and how they are faring. Monthly Labor Review. 2008;32. [Google Scholar]
- 20.Sastry N, Gregory J. The location of displaced New Orleans residents in the year after Hurricane Katrina. Demography. 2014;51(3):753–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ridenour ML, Cummings KJ, Sinclair JR, Bixler D. Displacement of the underserved: medical needs of Hurricane Katrina evacuees in West Virginia. J Health Care Poor Underserved. 2007;18(2):369–381. [DOI] [PubMed] [Google Scholar]
- 22.Smith A, Katz R. US billion-dollar weather and climate disasters: data sources, trends, accuracy and biases. Natural Hazards. 2013;67:387–410. [Google Scholar]
- 23.Freeman WA, Weiss AIWH, Heslin KA. Overview of US hospital stays in 2016: variation by geographic region. HCUP Statistical Brief #246. Rockville, Maryland USA: Agency for Healthcare Research and Quality; 2018. [PubMed] [Google Scholar]
- 24.Barrett ML, Smith MW, Elixhauser A, Honigman LS, Pines JM. Utilization of intensive care services, 2011: Statistical Brief #185. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, Maryland USA: Agency for Healthcare Research and Quality; 2006. [PubMed] [Google Scholar]