Summary Statement
Simulation played a critical role in our institution's response to the COVID-19 pandemic in New York City. With the rapid influx of critically ill patients, resource limitations, and presented safety concerns, simulation became a vital tool that provided solutions to the many challenges we faced. In this article, we describe how simulation training was deployed at our institution throughout the course of the pandemic, which included the period of our medical surge. Simulation helped refine protocols, facilitate practice changes, uncover safety gaps, and train redeployed healthcare workers in unfamiliar roles. We also discuss the obstacles we encountered with implementing simulations during the pandemic, the measures we took to adapt to our limitations, and the simulation strategies and end products that were derived from these adaptations.
Key Words: COVID-19, disaster preparedness, patient safety, simulation experience, pandemic, SARS, SARS-CoV-2, coronavirus
From March to April 2020, New York City emerged as an epicenter of the COVID-19 pandemic. In response to the exponential increase in hospitalized and critically ill patients, our institution rapidly expanded intensive care unit (ICU) and medical-surgical bed capacities, redeployed healthcare workers to provide adequate staffing, and established protocols to address clinical operational challenges such as intubations and cardiac arrests with considerations for proper infection control and mitigation.
Simulation played an integral role in our pandemic response process. Given its applications in disaster preparedness and crisis resource management, we believed that simulation would be well used to address system-based issues, such as identifying safety gaps, formulating infection control strategies, and refining clinical management protocols.1–8 In addition, simulation-based training has been consistently recognized as an asset in medical education.9–13 Therefore, it was adopted to address knowledge gaps and train redeployed clinical staff in new roles.
This article will describe in detail our simulation experience throughout the pandemic, divided into the following categories: primary system-based simulations, primary knowledge-based simulations, and the challenges encountered with our simulation implementation.
SYSTEM-BASED SIMULATIONS
The system-based simulations were developed to address clinical operational issues that came with the influx of patients. Focus was placed on optimizing infection prevention, identifying safety gaps, and refining protocols to maximize workflow efficiency as well as patient and staff safety.14–17 The simulations covered (1) personal protective equipment (PPE) training, (2) airway management, and (3) emergency code team training.
Personal Protective Equipment Training
Personal protective equipment training at our institution consisted of 3 components: an online module, in-person training, and in situ simulations. The Infection Prevention and Control (IPC) team created the online learning module, which contained educational handouts and a video reviewing the donning and doffing process. This was distributed systemwide to all employees via the institution's online learning platform as mandatory training.
To reinforce the online training, the IPC team also scheduled in-person training sessions to review PPE donning and doffing for staff in all of the first COVID-19 units. These included all emergency department bays, 6 adult ICUs, and a dedicated COVID-19 medical-surgical unit.18 The goal was for unit nursing managers and select staff to become comfortable with the donning and doffing process to guide their colleagues when needed. Each “COVID unit” received at least 1 training session, with additional sessions scheduled upon request. Participation was voluntary, and staff could either observe or practice with directive feedback for each step of the sequence. These training sessions continued with each new COVID unit or ICU that opened. However, as caseloads rapidly increased, they were reduced to mostly as-needed demonstrations because of staff shortages and the need for PPE conservation.
Despite the training provided by the IPC team, there were circulating concerns among staff regarding the impact of high-acuity situations such as cardiac arrests on the donning and doffing process (Table). To address this, PPE use was incorporated into the in situ airway management and cardiac arrest simulations (described in the next sections) to help identify any perceived latent safety threats.19,20 The following were the major PPE-specific issues identified during these simulations, along with their respective solutions:
TABLE 1.
Impact of Simulation Programs on COVID-19 Patient Care
| Simulation Program | Impacts |
|---|---|
| PPE training | Rearranged physical spaces to streamline and improve the safety of the doffing process. Added new physical barriers to better isolate doffing areas. |
| Intubation and airway management | Helped familiarize staff with a new COVID-19 intubation protocol. Uncovered knowledge gaps and staff misconceptions about the new protocol. Assigned specific airway team members with a cross-monitoring task to identify protocol deviations. Consolidated airway equipment for intubation with backup equipment readily available to ensure that there are no shortages. |
| Emergency code training | Contributed to the development of a systemwide cardiac arrest protocol. Addressed safety issues such as overcrowding, environmental and staff contamination by SARS-CoV-2 virus; created new roles such as a “gate keeper” and a doffing buddy, adjusted PPE requirements to better protect staff, streamlined medication delivery. Established new communication modalities during codes; use of pregenerated signs, walkie-talkies, and speaker phones. |
| Ventilator management training | Trained noncritical care providers deployed to ICUs on ventilator management of ARDS via distance learning; participants included hospitalists, pediatricians, nurses, physician assistants, and emergency medicine physicians. |
| Proning simulation | Trained providers in the rehabilitation department, including physical and occupational therapists, in patient proning in the setting of ARDS, contributed to the creation of a proning protocol. |
Inappropriate donning and doffing: During codes, participants were observed to forget essential PPE such as face shields, googles, and even N95s; gowns would be worn inappropriately. On occasion, doffing sequences were performed incorrectly. To help reduce the frequency of these problems, a “gate-keeper” role (discussed in more detail in the emergency code team section) was used to help monitor appropriate PPE donning during codes, and a doffing buddy system was created to ensure the appropriate sequences were performed.
Environmental constraints: Participants were often doffing too close to each other, risking cross-contamination especially in the more crowded scenarios. In response, “doffing zones” were created near room exits with floor marking tapes based on participant feedback. In certain circumstances, physical barriers such as curtains were used to further separate pre- and post-doffing areas. Waste receptables and hand hygiene stations were also relocated at times to create more streamlined paths toward the doffing zones.
Airway Management
Given the known risk of aerosolization with endotracheal intubation, we sought to standardize the approach to this process, evaluating technique, equipment, medication use, and PPE to limit aerosol exposure to providers. Based on recommendations from professional society guidelines and available literature, our institution included the following policies in our intubation guidelines to minimize aerosolization21–24:
To maximize first pass success, all intubations were to be performed as rapid-sequence intubations by the most experienced person available (usually an anesthesiology attending) in dedicated negative pressure rooms when possible.
Bag-valve ventilation was prohibited after intubation, unless absolutely necessary. Endotracheal tubes were to be directly connected to a mechanical ventilator with an attached end-tidal CO2 sensor and established waveform capnography.
If bag-valve ventilation was to be performed, a high efficiency particulate air (HEPA) filter must be attached between the endotracheal tube and the bag-valve.
Seven high-fidelity in situ simulations involving an emergent intubation scenario were conducted in ICUs. The goals were to assess our staff's familiarity with the previously mentioned intubation policies, identify safety threats, and to improve the efficiency and safety of COVID-19 intubations. Thirty-five individuals participated in the airways simulations in divided groups, which included nurses, respiratory therapists, fellows, intensivists, and anesthesiologists. Debriefings were structured to discuss guideline deviations and safety issues and to collect feedback for system and process improvements. The following were the major categories of safety issues identified in the simulations, along with the respective solutions that were instituted:
Operator mistakes: On several occasions, endotracheal tubes were connected to bag valves immediately after intubation followed by manual ventilation. This behavior was observed in both the intubators and respiratory therapists. The most frequent reasons for this were habit and situational urgency. In response, a minimum 3-person airway team was reinforced, and a designated cross-monitoring role was assigned to either the respiratory therapist or the certified nurse anesthetist/critical care nurse as an additional task to ensure adherence to the practice guidelines.
Missing equipment and setup failure: In the previously mentioned situations where manual bag-valve ventilation was performed after intubation, HEPA filters were sometimes absent. End-tidal CO2 sensors would be missing on occasion as well, after endotracheal tubes were successfully connected to a mechanical ventilator. To address these issues, an intubation kit with backup equipment was made readily available and stored with unit clerks. When an intubation was anticipated, the kits would be retrieved and made available outside the intubation room by the primary medical team. When the number of intubations increased throughout the pandemic, an additional certified nurse anesthetist was added to the airway team to help coordinate peri-intubation procedures such as transporting patients, gather medications and additional equipment to ensure safety and efficiency.
Unfamiliarity with the new guidelines: Despite hospital-wide distribution of the guidelines via early e-mails and meetings, not all staff were familiar with them or had a chance to see them. They also reported receiving mixed messages about the recommendations from their colleagues and assumed that the guidelines had changed. This was exacerbated by the frequency of new information disseminated during the early periods of the pandemic. To resolve this, the guidelines were reviewed with the participants during debriefings, but more importantly, this was addressed with specific department leaderships to reinforce the guidelines with their staff.
Emergency Code Team Training
Code training was one of the most important simulation activities carried out during our pandemic response. Strategies for optimal workflow and team organization within our systemwide cardiac arrest protocol were primarily derived from these simulations; guidelines for approaches to cardiac arrests at the time had limited information regarding these issues for COVID-19 patients.25 Given the risk of aerosolization during cardiopulmonary resuscitation, we also sought to assess the extent to possible fluid and aerosol contamination during this process.25
A total of 8 cardiac arrest simulations were conducted in various ICUs with their respective staff. Sixty-eight participants were recorded in attendance; however, there were likely more as some staff had to leave during mid-debriefing to attend to urgent clinical duties as the simulations were in situ. The participants included nurses, physicians, physician assistants, and respiratory therapists during both day and night shifts. Each simulation was followed by a debriefing to collect feedback and discuss safety concerns. To visualize the extent of possible contaminations, we applied fluorescent dyes made of diluted powder detergent onto the mannequin's airway and face to simulate oral secretions and aerosolized fluid during chest compressions (Fig. 1). At the end of each code, participants were evaluated under a black light to determine the presence of aerosol contamination. From these experiences, the following lessons and safety gaps were identified and their associated changes implemented:
FIGURE 1.
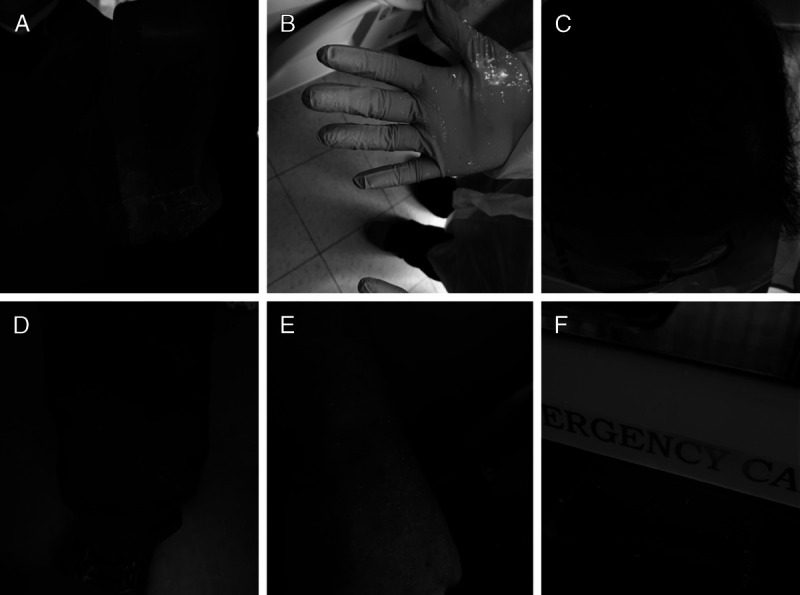
“Aerosol contamination” of surfaces as indicated by fluorescent dye. A, Contaminated gown sleeve. B, Contaminated glove. C, Contaminated hair. D, Contaminated pants. E, Contaminated wrist. F, Contaminated code cart.
Overcrowding during cardiac arrest codes. This was a consistent observation across many scenarios, and a major concern given the infectious nature of Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2). From our debriefings, many participants expressed that this behavior was done out of habit, resulting from a natural instinct to help during a code. In response, we established a “gate-keeper” role during codes to help disperse crowds, monitor for cross contaminations, and limit the number of people who were necessary for patient care to 6 people maximum (usually included a code leader, a nurse, an intubator, a respiratory therapist, and 2 compressors). The gate keeper also prevented anyone without appropriate PPE from entering the rooms. By proactively limiting personnel during these emergency situations, we were reducing not only exposure but also PPE usage. From debriefings in both simulations and true cardiac arrests, participants consistently expressed that the limited number of members responding to a code improved team communication compared with prepandemic times, and they hoped to maintain this structure going forward.
The extent of aerosol contamination. Contamination data were collected from 6 of the total 8 simulations, which included 44 participants divided into 6 groups. Each group was evaluated for the percentage of participants with any contaminated PPE, and any presence of contamination on body surfaces not covered by PPE. We found that every participant in each group had gown and glove contaminations, including code leaders who usually had minimal patient contact standing at the foot of the bed. We observed, on multiple occasions, contamination of uncovered body surfaces. These included hair (if not covered by head protection), exposed wrists and necks, pants, and shoes. As a response to these findings, we recommended that staff involved in codes should wear more extensive and impermeable PPE that covers the hair, face, and neck.
Environmental contamination. Fluorescent “aerosol” dye was found on the surfaces of code carts that were placed even outside the patient care room. We observed that members of the cardiac arrest teams were unintentionally coming in and out of the room to access the code cart, unfortunately contaminating it. As a response, we created a specialty code bag dedicated to COVID-19 cardiac arrests. We also implemented a policy where 1 nurse would remain outside the room to prepare medications that a dedicated person from inside of the room would collect in a plastic bin. The “gate keeper” would monitor for cross contamination between these 2 individuals, and if that were to happen, hand washing with hand sanitizer would be reminded.
Communication. A new layer of complexity involving cardiac arrests during COVID-19 patients was the challenge of communicating needs from the cardiac arrest team to team members outside enclosed patient rooms. Doors were kept closed to prevent aerosol spread. Our simulation training allowed staff members to generate several creative ideas. These included the use of pregenerated signs, walkie-talkies, or speaker phones when available, and bundling of medications and equipment for periodic delivery into the rooms during the arrest.
The identification of all the gaps resulted in formulation of an organization-wide cardiac arrest protocol that incorporated the lessons learned to streamline the code team to key roles, minimizing exposure as well as cross contamination of staff and equipment.
KNOWLEDGE-BASED SIMULATION
Because of the rapid expansion of our ICUs and COVID units, many clinical staff were redeployed to serve new roles. Examples included redeploying hospitalists to manage ventilated patients and recruiting physical therapists to serve as a “proning team.” These changes brought us the unique challenge of providing adequate training in a short period to fill knowledge gaps that could impact patient care. Our institution used simulation-based training to meet these specific education needs. The programs included (1) ventilator management training and (2) patient pronation training.
Ventilator Management Training
Because many non-ICU providers, including some pediatric providers, were redeployed to adult ICUs, there was a need to review respiratory physiology and basics of ventilator management in patients with acute respiratory distress syndrome (ARDS). To accomplish this, we created and widely distributed several videos to providers in the various ICUs. These videos reviewed basic physiology as well as principles of ventilator management in ARDS.
Our simulation group created a telesimulation session that allowed learners to use the Zoom platform to join a virtual meeting from their home via invitation. The learners were connected to the simulation center where a high-fidelity manikin simulator with test lungs was used alongside an LTV 1200 ventilator to walk the learners through a case of a patient with hypoxemic respiratory failure in a COVID-19 setting.
The learners functioned as a virtual care team, directing the facilitator in the simulation center—acting as the respiratory therapist—to set up and adjust the ventilator based on vital signs, arterial blood gases, and parameters measured on the ventilator. Learners then participated in a debriefing to review their decisions. This setup allowed learners to review key concepts on ventilator management while maintaining social distancing. A total of 51 multidisciplinary and interprofessional learners that included hospitalists, emergency medicine physicians, physician assistants, residents, nurses, and a nurse educator participated in the ventilator telesimulation. Feedback collected at the end of the course was overwhelmingly positive and participants indicated an increase in their confidence of ventilator management.26
Patient Pronation
One of the key aspects of managing patients with severe ARDS involves using prone ventilation. The PROSEVA trial found that early prone-positioning sessions decreased mortality.27 With the significant rise of intubated patients meeting criteria for prone ventilation, the demand for more providers trained to undertake these maneuvers grew. Prone positioning is labor intensive and not without its dangers. With several hundreds of intubated patients throughout the hospital and non-ICU providers redeployed to existing and newly created ICUs, a standardized approach to identify appropriate candidates to execute daily pronation and supination had to be developed.
To accomplish this, we partnered with our rehabilitation department to form proning teams and created a document that summarized indications, contraindications, equipment and personnel needs, and postpronation management. We hosted six 30-minute simulations over 2 weeks and trained 60 physical and occupational therapists in patient proning. All participants wore masks throughout the session. We distributed the checklist and used a full body manikin and the Tortoise turning and positioning system to train all the participants. Directive feedback was used to debrief learners in this short session. The rehabilitation department also created a video that reviewed all the preproning steps and demonstrated each step of the pronation and supination process. The video was widely disseminated to providers of various disciplines taking care of critically ill COVID patients.
The prone teams were rapidly deployed to all the ICUs and worked with primary nurses, respiratory therapists, and members of the medical team to provide daily supination and pronation to all patients who met the criteria. By standardizing care, the proning team also created a specific protocol to reduce pressure injury by using specific dressings and positioning pillows. This initiative received positive feedback immediately from the learners as well as from leadership in the various units where proning was implemented. The rehabilitation group continued to improve the technique and has taken the lead in continued training and implementation of the protocol.
CHALLENGES AND ADAPTATIONS IN IMPLEMENTING SIMULATIONS FOR COVID-19
Several obstacles were identified in implementing simulations during the COVID-19 pandemic. Most significant were learner safety concerns and staff shortage due to lack of available simulation faculty and personnel.
Learner Safety Concerns
The need to socially distance, and the risk of infection in close gatherings of learners, was a major area of concern that led us to consider a halt on simulation activities. This was amplified by a looming shortage of PPE as our institution embraced the rapid influx of patients. However, we also recognized that in high-risk situations such as cardiac arrests, infection risks among Health Care Workers (HCW) could potentially be worse in a chaotic scenario with overcrowding and underprepared staff.19,28 Therefore, we decided that the benefit of being prepared greatly outweighed the risks of the former if done with careful consideration. To address learner safety concerns, the following strategies were implemented:
Crowding: A limit was placed on the number of learners that could participate in simulations. As an example, with our emergency code team simulations, we allowed no more than 6 individuals in a room. In our in situ simulations, the previously mentioned “gate keeper” was used to prevent additional people from entering rooms and to dismiss crowds. Although cardiac arrest management with a limited number of staff proved to be difficult at first, our learners took this opportunity to adapt and improve teamwork and communication among each other, such as learning to change roles more readily when necessary during a code.
PPE shortage: The use of PPE was incorporated into our scenarios to reduce the potential risk of infection between learners. This was done with the understanding that PPE were in short supply; therefore, we held the use of N95 masks (but verbally reminded staff regarding their use in clinical scenarios), merged multiple simulation scenarios (such as cardiac arrest and airway training) into single sessions, and asked learners to keep their PPE on and to doff only at the end of all simulation activity. Whenever possible, we used any old PPE from our simulation center or other donor sources. In addition to the PPE's original intended purposes, this also presented an opportunity to simulate and practice proper donning and doffing techniques in high-acuity situations as previously mentioned.
Distance learning: Finally, telesimulation was implemented to train non-ICU physicians in ventilator management. These scenarios helped us greatly in terms of PPE conservation and allowed for appropriate social distancing while maintaining a high degree of fidelity in our cases.
Staff Shortage
Many simulation staff were employees not in direct patient care and were subsequently asked to work from home to prevent unnecessary travel. Our educators and debriefers were primarily composed of intensivists, emergency medicine physicians, and anesthesiologists, all of whom were used to staff the ICUs and emergency departments with increased clinical demands. As a result, they were not readily available to facilitate simulations on a routine schedule. These factors contributed to an overall shortage of simulation support staff and limited functioning of our on-site simulation facility.
In response to these shortcomings, many of our high-fidelity simulations were carried out in situ, with the help and cooperation of many clinical hospital staff and learners. As an example, nursing teams would help with setup, scheduling, and facilitation of simulation activities for colleagues, while also participating as confederates and debriefers as needed. In addition, in situ simulation allowed faculty to participate in debriefings and facilitate sessions while still being able to attend to patients on service. This new workflow allowed flexibility to carry out simulations during both the daytime and nighttime to increase outreach to as many learners as possible.
Many of our faculty spent their time off from clinical duty working tirelessly to develop simulation training programs; they recruited faculty and fellows with appropriate clinical backgrounds but limited simulation education experience to help facilitate sessions and debrief in a “train-the-trainer” model. This was demonstrated in our ventilator telesimulations where facilitators with mechanical ventilation experience, but limited simulation experience, participated. The trainees would be oriented on the case scenario and provided a standardized script for debriefing that covered major learning points. They would subsequently attend a session and observe a debriefing, followed by independent practice and training of an additional colleague. The telesimulation model also allowed simulation support staff to participate from any location and assist in the flow of the simulation by controlling equipment such as cameras and manage the web video conferencing software (Zoom Video Communications, Inc, San Jose, CA) so the facilitator can focus directly on the learners.
CONCLUSIONS
Healthcare simulation proved to be vitally important in our response to COVID-19 and could even be used during a medical surge within the pandemic. Despite the difficulties and limitations in resources and personnel, as well as the need for social distancing and infection prevention, we were able to successfully carry out high-impact multidisciplinary simulations throughout our institution. We identified and addressed safety concerns, improved and streamlined protocols, trained learners in unfamiliar skills through innovative means, and created specialized self-sustaining teams who responded to novel demands such as high-volume patient pronation. These developments not only helped carry our institution through the peak of patient surge during the pandemic, but left us with lasting improvements in the function of our organization and crisis resource management.
Footnotes
The authors declare no conflict of interest.
This work is attributed to the Division of Pulmonary and Critical Care Medicine at the New York Presbyterian Hospital/Weill Cornell Medical Center.
REFERENCES
- 1.Mundell WC, Kennedy CC, Szostek JH, Cook DA. Simulation technology for resuscitation training: a systematic review and meta-analysis. Resuscitation 2013;84(9):1174–1183. [DOI] [PubMed] [Google Scholar]
- 2.Boet S Bould MD Fung L, et al. . Transfer of learning and patient outcome in simulated crisis resource management: a systematic review. Can J Anaesth 2014;61(6):571–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marlow R Singleton S Campeau D, et al. . The evolution of healthcare disaster preparedness and response training at the FEMA Center for domestic preparedness. Am J Disaster Med 2019;14(1):5–8. [DOI] [PubMed] [Google Scholar]
- 4.Rega PP, Fink BN. Immersive simulation education: a novel approach to pandemic preparedness and response. Public Health Nurs 2014;31(2):167–174. [DOI] [PubMed] [Google Scholar]
- 5.Wadman MC Schwedhelm SS Watson S, et al. . Emergency department processes for the evaluation and management of persons under investigation for Ebola virus disease. Ann Emerg Med 2015;66(3):306–314. [DOI] [PubMed] [Google Scholar]
- 6.O'Keeffe DA Bradley D Evans L, et al. . Ebola emergency preparedness: simulation training for frontline health care professionals. MedEdPORTAL 2016;12:10433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clay KA O'Shea MK Fletcher T, et al. . Use of an ultraviolet tracer in simulation training for the clinical management of Ebola virus disease. J Hosp Infect 2015;91(3):275–277. [DOI] [PubMed] [Google Scholar]
- 8.Abrahamson SD, Canzian S, Brunet F. Using simulation for training and to change protocol during the outbreak of severe acute respiratory syndrome. Crit Care 2006;10(1):R3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bearman M, Greenhill J, Nestel D. The power of simulation: a large-scale narrative analysis of learners' experiences. Med Educ 2019;53(4):369–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cook DA, Andersen DK, Combes JR, Feldman DL, Sachdeva AK. The value proposition of simulation-based education. Surgery 2018;163(4):944–949. [DOI] [PubMed] [Google Scholar]
- 11.Kalaniti K, Campbell DM. Simulation-based medical education: time for a pedagogical shift. Indian Pediatr 2015;52(1):41–45. [DOI] [PubMed] [Google Scholar]
- 12.Sakakushev BE, Marinov BI, Stefanova PP, Kostianev SS, Georgiou EK. Striving for better medical education: the simulation approach. Folia Med (Plovdiv) 2017;59(2):123–131. [DOI] [PubMed] [Google Scholar]
- 13.Reedy GB. Using cognitive load theory to inform simulation design and practice. Clin Simul Nurs 2015;11(8):355–360. [Google Scholar]
- 14.Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis 2020;26:1470–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anelli F Leoni G Monaco R, et al. . Italian doctors call for protecting healthcare workers and boosting community surveillance during covid-19 outbreak. BMJ 2020;368:m1254. [DOI] [PubMed] [Google Scholar]
- 16.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323(13):1239–1242. [DOI] [PubMed] [Google Scholar]
- 17.Zhan M, Qin Y, Xue X, Zhu S. Death from Covid-19 of 23 health care workers in China. N Engl J Med 2020;382(23):2267–2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Griffin KM, Karas MG, Ivascu NS, Lief L. Hospital preparedness for COVID-19: a practical guide from a critical care perspective. Am J Respir Crit Care Med 2020;201(11):1337–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patterson MD, Geis GL, Falcone RA, LeMaster T, Wears RL. In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ Qual Saf 2013;22(6):468–477. [DOI] [PubMed] [Google Scholar]
- 20.Lamberta M, Aghera A. Latent Safety Threat Identification via Medical Simulation. In: StatPearls. StatPearls Publishing; 2020. Available at: http://www.ncbi.nlm.nih.gov/books/NBK549909/. Accessed October 11, 2020. [PubMed] [Google Scholar]
- 21.Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID-19: guidelines from the difficult airway society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia 2020;75(6):785–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan MTV Chow BK Lo T, et al. . Exhaled air dispersion during bag-mask ventilation and sputum suctioning - implications for infection control. Sci Rep 2018;8(1):198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Orser BA. Recommendations for endotracheal intubation of COVID-19 patients. Anesth Analg 2020;130(5):1109–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zuo M-Z Huang Y-G Ma W-H, et al. . Expert recommendations for tracheal intubation in critically ill patients with noval coronavirus disease 2019. Chin Med Sci J 2020;35:105–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Edelson DP Sasson C Chan PS, et al. . Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation 2020;141(25):e933–e943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Naik N, Finkelstein RA, Howell J, Rajwani K, Ching K. Telesimulation for COVID-19 ventilator management training with social-distancing restrictions during the coronavirus pandemic. Simul Gaming 2020;51(4):571–577. [Google Scholar]
- 27.Guérin C Reignier J Richard J-C, et al. . Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013;368(23):2159–2168. [DOI] [PubMed] [Google Scholar]
- 28.Chaplin T, McColl T, Petrosoniak A, Hall AK. “Building the plane as you fly”: simulation during the COVID-19 pandemic. CJEM 2020;22:576–578. [DOI] [PMC free article] [PubMed] [Google Scholar]


