Abstract
Comorbid diagnoses are common in youth who are at clinical high-risk (CHR) for developing psychosis, with depression being the most common. The aim of this paper is to examine depression over two years in a large sample of CHR youth who do not make the transition to psychosis, considering both categorical and dimensional ratings of depression severity. The sample consisted of 267 CHR youth who were followed for two years. Based on DSM-IV diagnoses over this time period, 100 CHR individuals never received a diagnosis of depression, 64 individuals continuously met criteria for depression, 92 individuals received a diagnosis of depression at one or more timepoints, and 11 participants had a diagnosis of depression only at 24-months. These groupings were supported by six-monthly ratings on the Calgary Depression Scale. The majority of this sample experienced a major depressive episode on more than one occasion, suggesting that depression and depressive symptoms identify a domain of substantial unmet clinical need. Recommendations are that depression in CHR youth and young adults should be monitored more frequently and that there is a need for clinical trials to address depression systematically in this vulnerable population.
Keywords: depression, clinical high-risk, psychosis, prognosis, symptoms
1. Introduction
Typically, the goal of research into clinical high-risk (CHR) for psychosis has been to prevent the transition to psychosis. Although there have been some promising outcomes in terms of preventive treatments (Addington et al., 2020), one of the barriers to successful treatment has been the heterogeneity of CHR individuals. Several years ago, research suggested that transition to a psychotic illness occurred in approximately 25% of CHR individuals (Fusar-Poli et al., 2012) but numbers cited in more recent studies suggest that this number is dropping (Addington et al., 2020; Fusar-Poli et al., 2017; Raballo et al., 2020). Unfortunately, this likely does not reflect improved outcomes (i.e., fewer people developing psychosis due to treatment), but rather indicates a highly heterogeneous course with these young people having a range of outcomes often with unmet clinical needs (Addington et al., 2019b; Allswede et al., 2020; Healey et al., 2018; Woods et al., 2018). In addition to experiencing attenuated psychotic symptoms, a decline in functioning (Fusar-Poli et al., 2015), neurocognitive difficulties (Seidman et al., 2016), and comorbid diagnoses are prevalent in this population (Addington et al., 2017), with the most common diagnosis in CHR individuals being depression. Approximately 40-60% of CHR individuals report a current or past depressive episode (Addington et al., 2017; Fusar-Poli et al., 2014; McAusland et al., 2017; Shi et al., 2017). In addition, depression has been shown to be associated with lower quality of life (Takahashi et al., 2017), more pronounced negative and general symptoms, a decreased likelihood for remission from CHR status (Kline et al., 2018) and to predict persistent paranoia in CHR individuals (Salokangas et al., 2016).
It is still relatively unknown whether or not depression or depressive symptoms are an independent risk factor for transition to psychosis, or, what might be more likely, a marker of poor prognosis for the CHR syndrome (Kline et al., 2018). Kline and colleagues (Kline et al., 2018) further suggest that since depression accounts for much of the variation in presenting symptoms of a CHR individual, with the exception of attenuated psychotic symptoms, targeting depression may not only improve depression but other concerns such as general or disorganized symptoms or even poor social functioning. This is important as depression has not been emphasized in the literature as an independent treatment target for CHR individuals, (Addington et al., 2019a) although it is highly prevalent even amongst those who do not transition to psychosis (Addington et al., 2019b).
Finally, to date, depression has mainly been assessed at baseline and less often as a later outcome. Thus, little is known about the trajectory of depression in CHR. Therefore, in attempting to deconstruct the heterogeneity of the CHR syndrome to better predict individual clinical trajectories, examining depression over time is warranted and would be an important clinical outcome to define and address, especially since details on treatment of depression in CHR are limited.
Thus, as a first step to address the heterogeneity of outcomes of CHR youth, this paper will focus on depression as an outcome that could potentially be a marker of poor prognosis (Kline et al., 2018) and which needs to be addressed. More specifically, the paper will focus on assessing the occurrence of depression over a two-year period in those who do not transition to psychosis using both categorical and dimensional ratings of depression.
2. Materials and Methods
2.1. Participants
Participants in this study were from the North American Prodrome Longitudinal Study-2 (NAPLS-2). We have previously described in detail our ascertainment processes (Addington et al. 2012). There were 764 CHR participants (436 males, 328 females) in NAPLS-2, recruited from all eight NAPLS-2 sites. The Structured Interview for Psychosis-risk Syndromes (SIPS) (McGlashan et al., 2010) was used to determine if participants met the Criteria for at least one of the Psychosis-risk Syndromes (COPS), that is attenuated psychotic symptoms syndrome (APSS); brief intermittent psychotic symptoms syndrome (BIPS); or genetic risk and deterioration syndrome (GRD). From this NAPLS-2 sample of 764, there were 86 who had transitioned to psychosis, 390 dropped out before two years for various reasons and 21 who did complete two years were excluded from the analyses as they were missing the depression assessments. We have previously demonstrated that there were no clinical differences between those who completed the study and those who dropped out prior to two years (Stowkowy et al., 2018). We have also previously reported that there was minimal depression (less than 4%) reported over time in the healthy control group that was part of NAPLS-2 (Addington et al., 2012; Addington et al., 2017). Thus, the sample (n=267) described in this paper had not made the transition to psychosis and had completed two years of follow-up. Those who made a transition to psychosis were not included since 71 of them converted prior to 12-months and had only baseline DSM-IV diagnoses. Participants’ age ranged between 12 and 35 years. Exclusion criteria were meeting criteria for a current or past axis I psychotic disorder, IQ less than 70, or past or current history of a clinically significant central nervous system disorder.
2.2. Measures
Current and lifetime depression was assessed with the Structured Clinical interview for DSM-IV (SCID) (First et al., 1995) and the SIPS (McGlashan et al., 2010) to determine COPS criteria. The severity of attenuated psychotic symptoms was assessed with the Scale of Psychosis-risk Symptoms (SOPS).
The Calgary Depression Scale for Schizophrenia (CDSS) (Addington et al., 1990) was used to measure current depressive symptom severity over the past two weeks. The CDSS was originally developed for patients with schizophrenia to address the issue of the overlap between depression and negative symptoms and has become the recommended scale to assess the severity of depression in schizophrenia (Collaborative Working Group on Clinical Trial Evaluations, 1998). Over the past 20 years there has many published studies on the CDSS (www.ucalgary.ca/cdss) including its translation into more than 40 languages. Its psychometric properties are excellent and include internal consistency, inter-rater reliability, sensitivity, specificity, and discriminant and convergent validity (Addington et al., 1994; Addington et al., 1992; Bernard et al., 1998; Lancon et al., 2000; Muller et al., 1999; Sarro et al., 2004). There is little overlap with positive and negative symptoms (Addington et al., 1994; Muller, 2002). Finally, the CDSS has been shown to be superior relative to other depression rating scales, such as the Hamilton Depression Rating Scale and the Montgomery-Asberg Scale in that it differentiates between depression and negative and positive symptoms and it is short to administer (Addington et al., 1996; Collins et al., 1996). More recently the CDSS has been validated in CHR individuals (Addington et al., 2014)..
Social and role functioning were assessed with the Global Functioning-Social (GF:S) and Role (GF:R) scales which were specifically designed to measure social and role functioning in CHR individuals. They have good psychometric properties and construct validity (Cornblatt et al. 2007).
Use of anti-psychotic and anti-depressant medication was determined at each assessment. Participants acknowledged only whether they were taking either of these medications at the given assessments. Data reflecting type, dose, length of use, compliance, and reason for prescription is not available.
2.3. Procedures
This study was approved by the Institutional Review Boards of all eight NAPLS-2 sites. We obtained written informed consent, including parental consent, from all participants 18 and older and parents/guardians of minors. CDSS data were collected at five-time points: baseline, 6-, 12-, 18- and 24-month follow-ups, and SCID diagnoses were conducted annually at baseline, 12- and 24-month follow-ups.
2.4. Statistical Analysis
To accommodate missing data and account for intra-participant correlation over time, a generalized linear mixed model for repeated measures was used for the different depression groups to examine changes in CDSS over time (baseline, 6-, 12-, 18-, and 24-months) both between and within depression groups. Two assessments were missing at baseline, 29 at 6-months, 21 at 12-months, 62 at 18-months and 1 at 24-months. One-way Anovas were used to compare each of the depression groups on positive symptoms, negative symptoms and social functioning at each of the five assessment timepoints.
3. Results
Demographics are presented in Table 1. Antipsychotics were used by this sample at different times over the course of two years. Sixty-six percent never used an antipsychotic. Antipsychotics were reportedly being used at all five assessment points by 4.9%, at four assessment points by 4.9%, at three assessment points by 6.4%, at two assessment points by 6.4% and only at one assessment point by 11.2%.
Table 1.
Baseline demographic characteristics
| Variable | Total n = 267 |
|---|---|
| Mean (SD) | |
| Age (years) | 18.87 (4.37) |
| Years of education | 11.48 (2.74) |
| Frequency (%) | |
| Sex | |
| Female | 116 (43.4) |
| Male | 151 (56.6) |
| Race | |
| Caucasian | 154 (57.7) |
| Black | 53 (19.9) |
| Interracial | 35 (13.1) |
| Asian | 19 (7.1) |
| Other b | 6 (2.2) |
| Marital status | |
| Single, never married | 257 (96.3) |
| Other | 10 (3.7) |
| Current living arrangement | |
| Living with family | 196 (73.4) |
| Living with others a | 41 (15.4) |
| Living on own | 19 (7.1) |
| Living with spouse/partner | 11 (4.1) |
| Current employment | |
| Not worked in the past year | 131 (49.1) |
| Currently working | 73 (27.3) |
| Worked in the past year | 61 (22.8) |
| Full time parent | 2 (0.7) |
Abbreviations: SD, standard deviation
Includes living with friends (excluding spouse/partners), in a boarding/group home, or academic residence.
includes, First Nations, Native Hawaiian or Pacific Islander.
Using the Structured Clinical interview for DSM-IV (SCID) diagnoses of depression (i.e., major depressive disorder, dysthymia and depression NOS) conducted at baseline, 12- and 24-months, four different depression groups were created. No participant had bipolar depression or a mood disorder with psychotic features. These groups were based on the number of assessments at which participants had received a mood diagnosis and considered whether they had received a mood diagnosis at the final assessment at 24-months. Group one consisted of 100 individuals who never received a diagnosis of depression at any of the three SCID assessments called NON-DEP. Group two, CON-DEP, consisted of 64 individuals who had a mood diagnosis at 24-months plus a diagnosis of depression at least one other assessment. The majority had received a mood diagnosis on at least 2 occasions prior to 24-months. Group three consisted of 92 individuals who received a diagnosis of depression, at least once, although approximately 50% had a diagnosis at more than one assessment, but had no diagnosis of depression at 24-months called INT-DEP. There were 11 participants who had a diagnosis of depression only at 24-months. We created a separate group for them called 24-DEP as it was unclear in which of the other two groups, they would best fit.
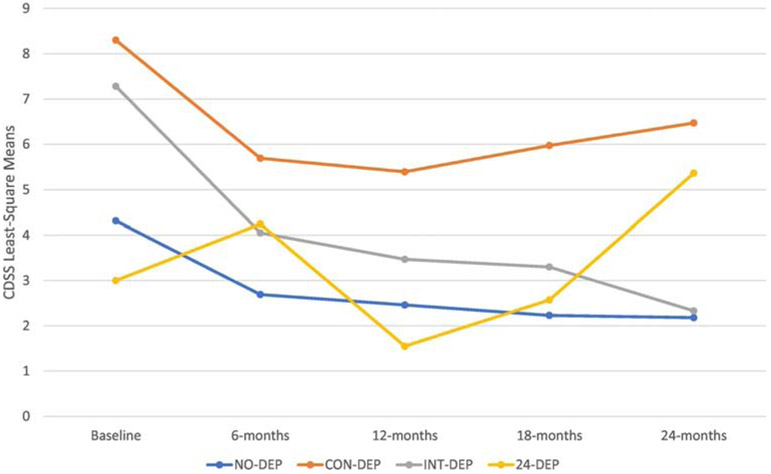
Results of the generalized linear model for changes in CDSS over time and within and between the four depression groups are presented in Table 2 and Figure 1. For the NO-DEP group, there was significant improvement at 18- and 24-months relative to their baseline scores, although the mean score at baseline was relatively low. For the CON-DEP group, their 6-, 12- and 18- month follow-up scores were significantly decreased with average scores in the moderate range. For those in the INT-DEP group, scores were significantly improved at all follow-up assessments compared to baseline. For the participants in the 24-DEP group there was no statistically significant changes over time in their CDSS scores although there was a notable clinical increase from 12 months to 24 months. With respect to the between group differences it was observed that at each timepoint ratings were significantly higher for the CON-DEP group compared to the NON-DEP group. At baseline, the INT-DEP group also had significantly more severe ratings than the NON-DEP group. Those in the INT-DEP group at both 18-and 24-month follow-up had significantly lower ratings than the CON-DEP group.
Table 2.
Generalized linear models for changes in Calgary Depression Scale over time between and within groups
| CDSS assessment |
No Depression NO-DEP |
Depression at each assessment CON-DEP |
1-2 episodes of depression INT-DEP |
Depression only at 24 months 24-DEP |
|---|---|---|---|---|
| M (SE) | M (SE) | M (SE) | M (SE) | |
| Baseline | 4.31 (0.47) | 8.30 (0.59)a*** | 7.28 (0.49)a** | 3.00 (1.42) |
| 6-months | 2.69 (0.39) | 5.69 (0.49)b***,h** | 4.05 (0.41)h*** | 4.24 (1.22) |
| 12-months | 2.46 (0.37) | 5.39 (0.47)c***,h** | 3.47 (0.38)h*** | 1.55 (1.08) |
| 18-months | 2.23 (0.40)h* | 5.97 (0.51)d***,h* | 3.30 (0.41)f**,h*** | 2.57 (1.14) |
| 24-months | 2.18 (0.36)h** | 6.47 (0.45)e*** | 2.33 (0.38)g***,i* | 5.36 (1.10) |
M* represents the least squares means estimated by the Generalized linear models
SE represents the standard error of the mean
significantly different from no depression group at baseline
significantly different from no depression group at 6-months
significantly different from no depression group at 12-months
significantly different from no depression group at 18-months
significantly different from no depression group at 24-months
significantly different from depression group at 18-months
significantly different from depression group at 24-months
significantly different within group change from baseline
significantly different within group change from 6-months
p<0.05
p<0.01
p<0.001
Figure 1.
CDSS scores by depression groups over time.
The four groups were compared on positive and negative symptoms and social and role functioning at each of the five assessment timepoints (see Table 3). There were no differences between the groups in positive symptoms and role functioning. The CON-DEP group had significantly more severe negative symptoms compared to the NO-DEP group at four of the assessments including 24-months, and to the INT-DEP group at 24-months. There were a couple of differences in social functioning in that the INT-DEP group at baseline and the CON-DEP group at 24 months had significantly poorer social functioning than the NO-DEP group.
Table 3.
Symptomatic and functional differences over time for the four depression groups
| Measure | No Depression NO-DEP |
Depression at each assessment CON-DEP |
1-2 episodes of depression INT-DEP |
Depression only at 24 months 24-DEP |
Test Statistic F |
|---|---|---|---|---|---|
| SOPS Positive | |||||
| Baseline | 11.96 (0.42) | 11.55 (0.52) | 11.70 (0.44) | 11.55 (1.26) | 0.148 |
| 6-months | 8.19 (0.46) | 8.48 (0.58) | 7.86 (0.49) | 10.38 (1.39) | 1.084 |
| 12-months | 7.72 (0.49) | 7.95 (0.61) | 7.26 (0.50) | 8.52 (1.46) | 0.468 |
| 18-months | 6.37 (0.48) | 7.15 (0.60) | 6.14 (0.49) | 7.92 (1.40) | 0.924 |
| 24-months | 6.40 (0.46) | 7.70 (0.58) | 6.12 (0.48) | 7.64 (1.39) | 1.781 |
| SOPS Negative | |||||
| Baseline | 10.29 (0.59) | 14.20 (0.74)a | 12.35 (0.61) | 11.00 (1.77) | 5.741** |
| 6-months | 7.89 (0.59) | 10.64 (0.75)a | 9.13 (0.63) | 11.28 (1.8) | 3.691* |
| 12-months | 7.43 (0.57) | 10.66 (0.72)a | 8.35 (0.59) | 8.61 (1.73) | 2.992* |
| 18-months | 7.06 (0.61) | 9.89 (0.77) | 7.93 (0.63) | 8.17 (1.79) | 1.878 |
| 24-months | 7.08 (0.57) | 9.98 (0.72)a | 7.25 (0.6)b | 9.09 (1.73) | 4.048** |
| GF:S | |||||
| Baseline | 6.50 (0.16) | 5.95 (0.2) | 5.9 (0.16)a | 6.45 (0.47) | 2.920* |
| 6-months | 6.81 (0.16) | 6.33 (0.2) | 6.37 (0.16) | 6.43 (0.47) | 1.455 |
| 12-months | 7.03 (0.16) | 6.32 (0.2) | 6.39 (0.16) | 7.01 (0.47) | 2.363 |
| 18-months | 7.14 (0.16) | 6.35 (0.2) | 6.52 (0.17) | 6.73 (0.47) | 2.513 |
| 24-months | 7.07 (0.15) | 6.34 (0.19) a | 6.93 (0.15) | 6.18 (0.45) | 3.934** |
| GF:R | |||||
| Baseline | 6.47 (0.22) | 5.91 (0.27) | 6.06 (0.23) | 6.09 (0.66) | 1.027 |
| 6-months | 6.59 (0.22) | 6.01 (0.28) | 6.94 (0.23) | 6.09 (0.66) | 1.757 |
| 12-months | 6.72 (0.22) | 6.33 (0.27) | 6.77 (0.22) | 6.60 (0.65) | 0.155 |
| 18-months | 6.49 (0.25) | 6.18 (0.32) | 6.63 (0.26) | 6.32 (0.72) | 0.213 |
| 24-months | 6.32 (0.25) | 6.09 (0.31) | 6.63 (0.25) | 6.82 (0.74) | 0.666 |
Abbreviations: GF:S, Global Functioning: Social Scale; GF:R, Global Functioning: Role Scale; SOPS, Scale of Psychosis risk
p<0.05
p<0.01
Significantly different from No Depression group
Significantly different from Depression at Each Episode group
Data on whether an individual was taking an antidepressant or not at any assessment was collected. We do not know the reason for the prescription, the type, dose or compliance. However in the NO-DEP group on average 20% reported taking an antidepressant at any one time, for the INT-DEP on average 36% reported taking an antidepressant at each of the assessments and for the CON-DEP approximately 44% were reportedly taking an antidepressant at each time period. For the 24-DEP only a couple were taking an antidepressant prior to 24 months at which time 5 were on an antidepressant. These data are presented in Supplementary Table 1.
4. Discussion
The purpose of this paper was to show that in attempting to deconstruct the heterogeneity of CHR outcome that depression is an important outcome that needs to be assessed and treated. To do this we examined depression over the course of two years in a sample of CHR individuals who had not transitioned to psychosis. Based on DSM-IV diagnoses that were conducted at baseline, 12- and 24- month follow-up assessments, we found four distinct depression groups. One group that presented with a diagnosis of depression at 24-months as well as at prior assessments (CON-DEP, n=64), a second group had intermittent periods of depression but were not depressed at the 24-month follow-up (INT-DEP, n=92), a small group who had never previously been depressed but met criteria for depression at the 24-month follow-up (24-DEP, n=11) and those who never met criteria for current depression during the study (NO-DEP, n=100). Thus, there is evidence of a high prevalence of depression over a two-year period with approximately one-third of those who had not transitioned to psychosis having no evidence of depression. The remainder of the sample reported at least one episode of an MDD. What is interesting is that if these young people had been in one of the newer transdiagnostic studies examining risk for a serious mental illness, approximately 50% of this sample would be considered to have made the transition to a serious mental illness.
We used the CDSS ratings to monitor depression at six-monthly intervals. Results of these ratings offer some support to the allocation of participants to the different depression groups. Both the NO-DEP and CON-DEP groups demonstrated statistically, but not clinically significant improvement over time. The INT-DEP group demonstrated both statistically and clinically significant improvement at each follow-up assessment compared to baseline. The between group differences are also what would be expected at each follow-up.
Interestingly the four groups did not differ on role functioning, nor on positive symptoms at any of the assessment points. There were differences between the NO-DEP and CON-DEP groups at four of the five assessments with the CON-DEP group having more severe negative symptoms. The CON-DEP group also had more severe negative symptoms than the INT-DEP group at 24-months. There were a couple of significant differences in social functioning in that the NO-DEP group had improved social functioning compared to the INT-DEP group at baseline and to the CON-DEP group at 24 months, although these differences could be attributed to type II error. The lack of difference between the groups in positive symptoms suggest that the presence of positive symptoms is unrelated to depression and that they are potentially independent an issue that has long been debated in the schizophrenia field. The only notable significant difference in social functioning was that the CON-DEP had lower ratings than the NO-DEP at 24 months. These differences may just be by chance or it may be that those with more depression do have poorer functioning but there is a possible floor effect since it has been established even when CHR participants are in remission and have improved functioning relative to those who remain symptomatic, their functioning is still poorer than healthy controls (Addington et al., 2019b). Thus, poor functioning would be expected in all groups. It is possible that many with more frequent depression are having difficulty in functioning, and in fact at 24 months there is a small but statistically significant correlation between ratings on the CDSS and the GF:S (r=−0.36, p<0.01). This suggests that our trajectory groupings are too broad to capture the specific association between functioning and depression.
There are several limitations in this paper. First, assessments were limited. DSM-IV diagnoses were only conducted at annual visits and depression ratings at six-monthly interviews. More frequent assessment of depression is needed to truly mark its course over time. Ideally depression with for example the CDSS should be being monitored every 2-4 weeks. However, this study supports a combination of conducting both a DSM diagnostic interview in conjunction with more frequent ratings on a scale such as the CDSS which has been identified as valid for this population and one of the most widely used depression scales in clinical trials. Secondly, a major limitation in this paper, is treatment for depression. This was a naturalistic study, and although participants did receive antidepressants at various times over the 24-months, they were not routinely prescribed in a systematic way, but rather such treatments were left to the discretion of their physicians in the community. It is unknown the reasons why they might be taking an antidepressant or the type and dose. It is possible that they may even have been given an antipsychotic for depression. The same is true for psychological therapies in that even if participants received, for example CBT, it is unknown for what problems the treating clinician was offering CBT. Even if treatment was being offered it may be that some participants were receiving inadequate treatment for their depression. Finally, it is impossible to tell over the course of the 24-month follow-up whether presenting attenuated psychotic symptoms may be due to a mood diagnosis and would possibly remit with adequate treatment, or whether the mood disorder was comorbid to the attenuated psychotic symptoms. This limitation underscores the need for proper trials to address depression in CHR.
In conclusion, this paper supports that depression is a major concern for youth at CHR for psychosis and that it needs to be addressed as a significant outcome in CHR. Depressive diagnoses are common, and a pattern of consistent depression diagnoses over time may be associated with an unfavorable outcome at 24 months. Recommendations for future studies are that depression must be monitored more closely with far more frequent assessments than occurred in this study. This would allow for a clearer determination of different trajectories which ought to be data driven. Treatment should be offered as part of a controlled trial so that improvements in depression can be accounted for. At the very least careful and frequent monitoring of treatments need to occur. Recent innovations from the National Institute of Mental Health (NIMH) offer promise for the future. Finding preventive treatments for psychosis is an aim of the NIMH Accelerating Medicine Partnership between industry, investigators and government which may include addressing serious mood disorders. Secondly, recent funding opportunities from NIMH that propose to establish large research networks encompassing many international sites that will rapidly recruit large numbers of CHR individuals in order to dissect the heterogeneity and predict differential outcomes to inform future treatment development, offers hope that serious depression in these young people can be assessed, monitored and eventually treated effectively.
Supplementary Material
Acknowledgement
This study was supported by the National Institute of Mental Health (grant U01 MH081984 to Dr. Addington; grants U01 MH081928; P50 MH080272; Commonwealth of Massachusetts SCDMH82101008006 to Dr. Seidman; grants R01 MH60720, U01 MH082022 and K24 MH76191 to Dr. Cadenhead; grant U01 MH081902 to Dr. Cannon; P50 MH066286 (Prodromal Core), the Staglin Family Music Festival for Mental Health and the Joseph Levin Trust to Dr. Bearden; grant U01 MH082004 to Dr. Perkins; grant U01 MH081988 to Dr. Walker; grant U01 MH082022 to Dr. Woods; and U01 MH081857-05 grant to Dr. Cornblatt).
Financial Support
This study was supported by the National Institute of Mental Health (grantU01MH081984 to Dr Addington; grants U01 MH081928; P50 MH080272; Commonwealth of Massachusetts SCDMH82101008006 to Dr Seidman; grants R01 MH60720, U01 MH082022, and K24 MH76191 to Dr Cadenhead; grantU01MH081902 to Dr Cannon; P50MH066286 (Prodromal Core) to Dr Bearden; grant U01MH082004 to Dr Perkins; grant U01MH081988 to Dr Walker; grant U01MH082022 to Dr Woods; and UO1MH081857-05 grant to Dr Cornblatt. The NIMH had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication
Role of funding source
The NIMH had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors have declared that there are no conflicts of interest with respect to this paper.
References
- Addington D, Addington J, Atkinson M, 1996. A psychometric comparison of the Calgary Depression Scale for Schizophrenia and the Hamilton Depression Rating Scale. Schizophr Res 19(2-3), 205–212. [DOI] [PubMed] [Google Scholar]
- Addington D, Addington J, Maticka-Tyndale E, 1994. Specificity of the Calgary Depression Scale for schizophrenics. Schizophr Res 11(3), 239–244. [DOI] [PubMed] [Google Scholar]
- Addington D, Addington J, Maticka-Tyndale E, Joyce J, 1992. Reliability and validity of a depression rating scale for schizophrenics. Schizophr Res 6(3), 201–208. [DOI] [PubMed] [Google Scholar]
- Addington D, Addington J, Schissel B, 1990. A depression rating scale for schizophrenics. Schizophr Res 3(4), 247–251. [DOI] [PubMed] [Google Scholar]
- Addington J, Cadenhead KS, Cornblatt BA, Mathalon DH, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Addington JA, Cannon TD, 2012. North American Prodrome Longitudinal Study (NAPLS 2): Overview and recruitment. Schizophr Res 142(1-3), 77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Devoe DJ, Santesteban-Echarri O, 2019a. Multidisciplinary Treatment for Individuals at Clinical High Risk of Developing Psychosis. Curr Treat Options Psychiatry 6(1), 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Farris M, Devoe D, Metzak P, 2020. Progression from Being At-Risk To Psychosis: Next Step. NPJ Schizophrenia. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Piskulic D, Liu L, Lockwood J, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Bearden CE, Mathalon DH, Woods SW, 2017. Comorbid diagnoses for youth at clinical high risk of psychosis. Schizophr Res 190, 90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Shah H, Liu L, Addington D, 2014. Reliability and validity of the Calgary Depression Scale for Schizophrenia (CDSS) in youth at clinical high risk for psychosis. Schizophr Res 153(1-3), 64–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Stowkowy J, Liu L, Cadenhead KS, Cannon TD, Cornblatt BA, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Bearden CE, Mathalon DH, Santesteban-Echarri O, Woods SW, 2019b. Clinical and functional characteristics of youth at clinical high-risk for psychosis who do not transition to psychosis. Psychol Med 49(10), 1670–1677. [DOI] [PubMed] [Google Scholar]
- Allswede DM, Addington J, Bearden CE, Cadenhead KS, Cornblatt BA, Mathalon DH, McGlashan T, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Cannon TD, 2020. Characterizing Covariant Trajectories of Individuals at Clinical High Risk for Psychosis Across Symptomatic and Functional Domains. Am J Psychiatry 177(2), 164–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard D, Lancon C, Auquier P, Reine G, Addington D, 1998. Calgary Depression Scale for Schizophrenia: a study of the validity of a French-language version in a population of schizophrenic patients. Acta Psychiatr Scand 97(1), 36–41. [DOI] [PubMed] [Google Scholar]
- Collaborative Working Group on Clinical Trial Evaluations, 1998. Atypical antipsychotics for treatment of depression in schizophrenia and affective disorders. Collaborative Working Group on Clinical Trial Evaluations. J Clin Psychiatry 59 Suppl 12, 41–45. [PubMed] [Google Scholar]
- Collins AA, Remington G, Coulter K, Birkett K, 1996. Depression in schizophrenia: a comparison of three measures. Schizophr Res 20(1-2), 205–209. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams B, Williams J, 1995. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition. New York State Psychiatric Institute, New York. [Google Scholar]
- Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, Barale F, Caverzasi E, McGuire P, 2012. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry 69(3), 220–229. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Nelson B, Valmaggia L, Yung AR, McGuire PK, 2014. Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: impact on psychopathology and transition to psychosis. Schizophr Bull 40(1), 120–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Rocchetti M, Sardella A, Avila A, Brandizzi M, Caverzasi E, Politi P, Ruhrmann S, McGuire P, 2015. Disorder, not just state of risk: meta-analysis of functioning and quality of life in people at high risk of psychosis. Br J Psychiatry 207(3), 198–206. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Tantardini M, De Simone S, Ramella-Cravaro V, Oliver D, Kingdon J, Kotlicka-Antczak M, Valmaggia L, Lee J, Millan MJ, Galderisi S, Balottin U, Ricca V, McGuire P, 2017. Deconstructing vulnerability for psychosis: Meta-analysis of environmental risk factors for psychosis in subjects at ultra high-risk. Eur Psychiatry 40, 65–75. [DOI] [PubMed] [Google Scholar]
- Healey KM, Penn DL, Perkins D, Woods SW, Keefe RSE, Addington J, 2018. Latent Profile Analysis and Conversion to Psychosis: Characterizing Subgroups to Enhance Risk Prediction. Schizophr Bull 44(2), 286–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline ER, Seidman LJ, Cornblatt BA, Woodberry KA, Bryant C, Bearden CE, Cadenhead KS, Cannon TD, Mathalon DH, McGlashan TH, Perkins DO, Tsuang MT, Walker EF, Woods SW, Addington J, 2018. Depression and clinical high-risk states: Baseline presentation of depressed vs. non-depressed participants in the NAPLS-2 cohort. Schizophr Res 192, 357–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancon C, Auquier P, Reine G, Bernard D, Toumi M, 2000. Study of the concurrent validity of the Calgary Depression Scale for Schizophrenics (CDSS). J Affect Disord 58(2), 107–115. [DOI] [PubMed] [Google Scholar]
- McAusland L, Buchy L, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, McGlashan TH, Perkins DO, Seidman LJ, Tsuang MT, Walker EF, Woods SW, Bearden CE, Mathalon DH, Addington J, 2017. Anxiety in youth at clinical high risk for psychosis. Early Interv Psychiatry 11(6), 480–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlashan T, Walsh B, Woods S, 2010. The Psychosis-Risk Syndrome: Handbook for Diagnosis and Follow-up. Oxford University Press, New York. [Google Scholar]
- Muller M, 2002. Overlap between emotional blunting, depression, and extrapyramidal symptoms in schizophrenia. Schizophr Res 57(2-3), 307. [DOI] [PubMed] [Google Scholar]
- Muller MJ, Marx-Dannigkeit P, Schlosser R, Wetzel H, Addington D, Benkert O, 1999. The Calgary Depression Rating Scale for Schizophrenia: development and interrater reliability of a German version (CDSS-G). J Psychiatr Res 33(5), 433–443. [DOI] [PubMed] [Google Scholar]
- Raballo A, Poletti M, Preti A, McGorry P, 2020. Clinical high risk for psychosis in children and adolescents: A meta-analysis of transition prevalences. Schizophr Res. [DOI] [PubMed] [Google Scholar]
- Salokangas RK, Schultze-Lutter F, Hietala J, Heinimaa M, From T, Ilonen T, Loyttyniemi E, von Reventlow HG, Juckel G, Linszen D, Dingemans P, Birchwood M, Patterson P, Klosterkotter J, Ruhrmann S, 2016. Depression predicts persistence of paranoia in clinical high-risk patients to psychosis: results of the EPOS project. Soc Psychiatry Psychiatr Epidemiol 51(2), 247–257. [DOI] [PubMed] [Google Scholar]
- Sarro S, Duenas RM, Ramirez N, Arranz B, Martinez R, Sanchez JM, Gonzalez JM, Salo L, Miralles L, San L, 2004. Cross-cultural adaptation and validation of the Spanish version of the Calgary Depression Scale for Schizophrenia. Schizophr Res 68(2-3), 349–356. [DOI] [PubMed] [Google Scholar]
- Seidman LJ, Shapiro DI, Stone WS, Woodberry KA, Ronzio A, Cornblatt BA, Addington J, Bearden CE, Cadenhead KS, Cannon TD, Mathalon DH, McGlashan TH, Perkins DO, Tsuang MT, Walker EF, Woods SW, 2016. Association of Neurocognition With Transition to Psychosis: Baseline Functioning in the Second Phase of the North American Prodrome Longitudinal Study. JAMA Psychiatry 73(12), 1239–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi J, Wang L, Yao Y, Su N, Zhan C, Mao Z, Zhao X, 2017. Comorbid Mental Disorders and 6-Month Symptomatic and Functioning Outcomes in Chinese University Students at Clinical High Risk for Psychosis. Front Psychiatry 8, 209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stowkowy J, Liu L, Cadenhead KS, Tsuang MT, Cannon TD, Cornblatt BA, McGlashan TH, Woods SW, Perkins DO, Seidman LJ, Walker EF, Bearden CE, Mathalon DH, Addington J, 2018. Exploration of clinical high-risk dropouts. Schizophr Res 195, 579–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi T, Higuchi Y, Komori Y, Nishiyama S, Nakamura M, Sasabayashi D, Nishikawa Y, Sumiyoshi T, Suzuki M, 2017. Quality of life in individuals with attenuated psychotic symptoms: Possible role of anxiety, depressive symptoms, and socio-cognitive impairments. Psychiatry Res 257, 431–437. [DOI] [PubMed] [Google Scholar]
- Woods SW, Powers AR 3rd, Taylor JH, Davidson CA, Johannesen JK, Addington J, Perkins DO, Bearden CE, Cadenhead KS, Cannon TD, Cornblatt BA, Seidman LJ, Tsuang MT, Walker EF, McGlashan TH, 2018. Lack of Diagnostic Pluripotentiality in Patients at Clinical High Risk for Psychosis: Specificity of Comorbidity Persistence and Search for Pluripotential Subgroups. Schizophr Bull 44(2), 254–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.