Abstract
Anxiety and depression are common mental illness in stroke caregivers, resulting in significant stress to the emotion health of caregivers. Caregivers’ emotion can seriously affect the recovery rate of stroke patient, therefore, how to control and affect the caregivers’ anxiety and depression is of great importance. Here three multiple centers observation and validation study were performed to screen out the risk factors for development of anxiety and depression in main family caregiver, and the effect of anxiety and depression of family caregivers on 6-month mortality of patients with moderate-severe stroke. The severity of the stroke, the duration of care time and the medical payment associated with increased risk of anxiety and depression. Anxiety and depression of main family caregivers are associated with increased risk 6-month mortality of patients with moderate-severe stroke. Therefore, the support provided to the family caregivers might have positive effect on prognosis of the patients with stroke.
Subject terms: Cardiovascular diseases, Risk factors
Background
Stroke is the dominant leading cause of death and disability among Chinese adults for recent 3 decades1. Although great progress has been made in the treatment of stroke in recent years, numerous stroke patients had moderate-severe disability when discharged from the hospital2–4. Hence, the main caregivers must have to take care of the patients' physical and daily activities, including communication and emotional support. However, the long-time care process may cause great psychological pressure on the family caregivers, while it also brings a heavy burden, the anxiety and depression introduced silently5,6.
Previous studies disclosed that the high incidence rate of anxiety and depression occurred among family caregivers6–10. The prevalence of anxiety and depressive symptoms for main caregivers of patients with stroke have been reported to 30%-45% and 20–50%, respectively5,11,12. Many studies suggested that the anxiety or depressive symptoms of caregivers have a negative impact on caregivers’ socioeconomic status, physical health and quality of life13–15. When main caregivers are in a state of anxiety or depression, they may not provide valuable support for stroke survivors any more, which may reduce the efficiency of the rehabilitation of patients and cause adverse effects on the prognosis of disease16.
China is a developing country, traditionally the most stroke patients live at home after discharge. Moreover, most of family caregivers were not received any profession training to care the stroke survivor. This informal care often takes a big amount of time and effort, which might result in overwhelming feelings. Previous studies demonstrated that anxiety or depressed caregivers might impair the quality of life and associated with decreased physical function of stroke patients11,17,18. There are few studies investigated the rate of anxiety or depression in main family caregivers of patients with moderate-severe stroke, and the association with the mortality of patients.
Therefore, we are to investigate the risk factors for development of anxiety and depression among main family caregivers and the effect of anxiety or depression of family caregivers on 6-month mortality of patients with moderate-severe stroke.
Methods
Ethics approval and consent to participate
This study was approved by the Institute of Institutional Review Board and by the Ethics Committee of Xinxiang Central Hospital, The Second Affiliated Hospital of Zhengzhou University, The First Affiliated Hospital of Chengdu Medical College, and the Fengqiuxian People’s Hospital of Henan Province. All experiments were performed in accordance with relevant guidelines and regulations. All participants provided written informed consent.
Study population
This was a multicenter prospective study, the consecutive patients with neurological symptom due to cerebrovascular disease were collected within 30 days of symptom onset from January 2015 to February 2020. Cerebrovascular disease was diagnosed according to the diagnostic criteria of the 4th National Cerebrovascular Disease (The 4th National Symposium on Cardiovascular Disease of the Chinese Medical Association,1996). Classification of stroke was confirmed by brain computed tomography (CT) scan or magnetic resonance imaging (MRI). The severity of stroke was assessed by using the National Institutes of Health Stroke Scale (NIHSS). Moderate-severe stroke was defined as admission NIHSS ≥ 6. All the patients and their caregivers were paired, the caregiver group comprised family members who lived with the patient by take caring of the patients' physical and all daily activities, including communication, emotional support.
Inclusive and exclusive criteria
Paired caregivers were recruited to this study when patients were recruited. The main caregiver was defined as a family member who spent a lot of time with the patient, supported the patient physically and mentally, and helped the patient in daily activities, including assisted patient in walking, turning over in bed, feeding, defecating, and bathing. Caregivers were recruited in the study only if they fulfilled all the following criteria: (1) ≥ 18 years old; (2) The main caregivers were a family member of the patient; (3) Caregivers began to care the patients after stroke, and care time was more than 3 months, ≥ 6 h per day. Caregivers were excluded if they fulfilled the following criteria: (1) Any paid caregivers; (2)Caregivers with severe renal failure (estimated glomerular filtration rate < 30 ml/min.1.73 m2), severe pulmonary disease, active malignancies, hypoplasia; (3) incomplete investigation due to communication or reading and writing difficulties. (4) a history of mental illness, and (5) alcohol or drug abuse. The physical health status of the caregivers was obtained through the medical history. Liver and kidney function were obtained by physical examination report within the prior 3 months. Paired caregiver who could not provide the physical examination report, liver function, kidney function and blood count were measured within 48 h after patients’ admission.
Patients were recruited if they met the following criteria: (1) Admission for first-ever stroke within 1 month, and modified Rankin Scale (mRS) score was 0 before stroke; (2) NIHSS ≥ 6 and lived at home after discharge. Patients were excluded if they fulfilled the following criteria: (1) Patients with neurological symptom unrelated to cerebrovascular disease; (2)Severe atrioventricular block and supraventricular arrhythmia; (3)Active malignancies, renal failure(estimated glomerular filtration rate < 30 ml/min.1.73 m2), severe pulmonary disease, liver failure, or procedural or surgical complications.
Data collection
Patients’ demographics and clinical characteristics including vascular risk factors (e.g., hypertension, diabetes mellitus, hyperlipidemia, and smoking history) were collected. While, the caregivers’ demographics included age, sex, duration of care time, education level, care time per day > 8 h(h), and patients’ medical payment method were collected as well. All patients’ and caregivers’ the baseline characteristics were collected within 48 h after admission.
The severity of anxiety was assessed by the 14-item Chinese version of Hamilton Anxiety Rating Scale (HARS)18–20 in main family caregivers at 1 month after stroke. Each item is scored from 0 to 4 points, the total score is 0–56, and the anxiety level can be divided as follows: < 7 means no anxiety, 7–14 means possible anxiety, 15–21 means certain anxiety, 21–29 means obvious anxiety and > 29 means severe anxiety. Certain anxiety symptoms were defined by a HARS score > 1420.
Meanwhile, the severity of depression was assessed by the 17-item Chinese Hamilton Depression Rating Scale (HDRS)21,22,each item is scored on a 2 or 4 point scale, and the depression level can be divided as follows: 0–6 points considered no depression, 7–16 as mild depression,17–24 as moderate depression, and > 24 means severe depression. Certain depressive symptoms were defined by a HDRS score > 17.
The Chinese version of the 14-item HARS has been widely used in the Chinese population, indicating good reliability and validity (20). The validity and reliability of the 17-item Chinese HRSD had been proven in previous studies22, and interrater reliability was excellent, the item total score correlations were good, and the internal reliability was satisfactory. A neurologist was trained by psychiatrist with certification qualification of China’s National Health Commission in HARS and HDRS assessment in each hospital, who performed HARS and HDRS assessment of caregivers. The interobserver data differences were resolved by consensus.
The patients lived at home on discharge. All patients and caregivers were followed up once a month for a total of 6 months. All patients were followed up by face-to-face or telephone interview, and patient’s information was obtained from hospital medical records.
Statistical analysis
The data were presented as median values (interquartile range [IQR]), numbers (%), or mean values (± standard deviation). To distinguish the subgroup difference, the Pearson χ2 test was used to categorical variables. Besides, student’s test was used to compare normally distributed variables. Mann–Whitney analysis was used to compare the nonnormal distributed variables. Logistic regression analysis was used to determine the association between anxiety or depression of caregivers and 6-month mortality of patients with stroke. The results were expressed as adjusted odds ratios (aOR) with their corresponding 95% confidence intervals (CI). The data was analyzed using SPSS 22 software. P < 0.05 was considered statistically significant.
Results
Characteristics of the main caregivers
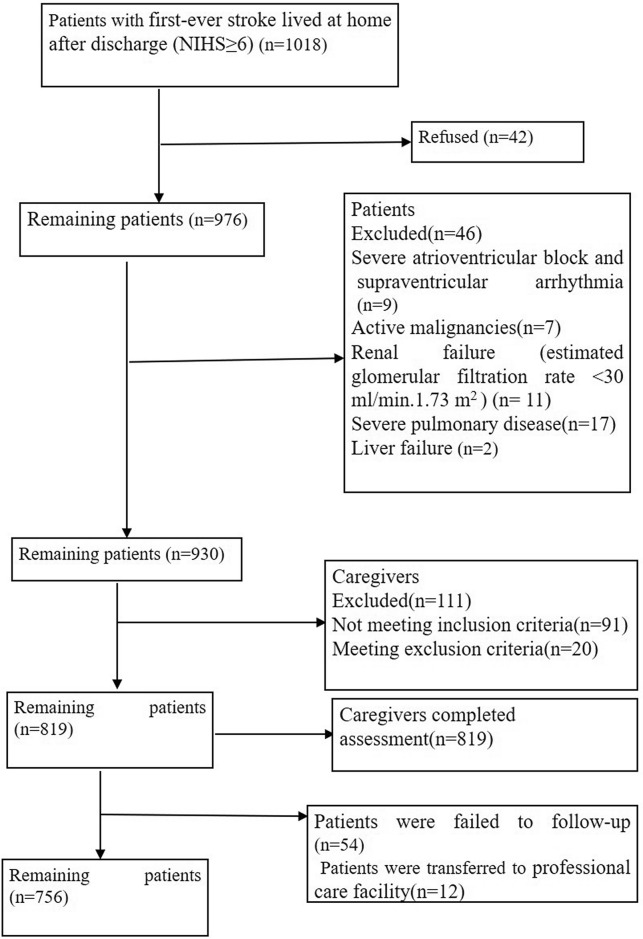
A total of 1018 patients with first-ever stroke lived at home after discharge (NIHS ≥ 6) were included from four multicenter, 42 patients refused to participate in the study, 46 patients met exclusion criteria, 111 paired caregivers were excluded because they met 1 or more of the other exclusion criteria (Fig. 1), the remaining 819 caregivers (249 male; 570 female) were recruited in this study, and the mean age was 55.64 ± 10.09 years (18–88 years). All the main family caregivers were relatives, 512 (62.52%) were spouse of the patients, 290(35.41%) were offspring, and 17(2.08%) were parents. The average care duration was 138.3 ± 28.7 days (93–183 days), caregivers with care time per day > 8 h were 477 (58.2%). The detail basic characteristics of the main family caregivers were shown in Table 1.
Figure 1.
Patient’s and caregiver’s flowchart.
Table 1.
Comparison of baseline characteristics between caregivers with no anxiety and anxiety groups.
| No anxiety group (522) | Anxiety group (297) | OR (95% CI) | P* | |
|---|---|---|---|---|
| Caregivers’ age, y (Mean SD) | 54.97±10.09 | 56.81±10.00 | 0.014 | |
| NIHSS of patients, median (IQR) | 8 [6–12] | 10 [7–13] | < 0.001 | |
| Duration of care time, d (Mean SD) | 130.46±25.78 | 152.08±28.54 | < 0.001 | |
| Females, n (%) | 359 (68.77) | 210 (70.71) | 1.10 (0.80–1.50) | 0.564 |
| Men, n (%) | 163 (31.23) | 87 (29.29) | 1.10 (0.80–1.50) | 0.564 |
| Education (high school and above), n (%) | 209 (40.04) | 123 (41.41) | 1.06 (0.79–1.41) | 0.700 |
| Care time per day >8 h, n (%) | 270 (51.72) | 207 (69.70) | 2.15 (1.59–2.90) | < 0.001 |
| Relationship to the patients | ||||
| Spouse, n (%) | 320 (61.30) | 192 (64.65) | 1.15 (0.86–1.55) | 0.342 |
| Other family member, n (%) | 202 (38.70) | 105 (35.35) | 1.15 (0.86–1.55) | 0.342 |
| Self–finance, n (%) | 122 (23.37) | 142 (47.81) | 3.00 (2.321–4.07) | < 0.001 |
| Household income, Chinese Yuan (CNY) <5000/month, n (%) | 237 (45.40) | 144 (48.48) | 0.88 (0.66–1.18) | 0.395 |
The risk factors for anxiety
According to the result of HARS, 297 (36.26%) main family caregivers had anxiety. The average HARS of main family caregivers with anxiety was 21.41 ± 7.80, the average HARS of main family caregivers with no anxiety was 9.18 ± 3.27. Baseline characteristics of caregivers in the no anxiety and anxiety groups were compared (Table 1). The results uncovered that caregivers’ age, NIHSS of patients, duration of care time, care time per day > 8 h and self-finance had effects on the anxiety of main family caregivers, and they presented significant difference (P < 0.05).
The anxiety level of caregivers of medical insurance group was lower than that of self-financed group (12.54 ± 7.31 vs 15.88 ± 8.77, P < 0.001), and the anxiety level of caregivers with care time per day > 8 h was higher than that of care time per day ≤ 8 h (14.83 ± 8.79 vs 11.91 ± 6.26, P < 0.001).Caregivers in anxiety group had older age, higher NIHSS of patients, longer duration of care time, higher percentage of care time per day > 8 h and self-finance than caregivers in no anxiety group(both P < 0.05).
To further analyze the risk factors for the anxiety of main family caregivers, multivariable logistic regression was performed, after adjusting for caregivers’ age, NIHSS, duration of care time, sex, education, care time per day > 8 h, self-finance, relationship to the patients, household income, the results showed that NIHSS (aOR, 1.08; 95% CI, 1.04–1.12; P = 0.001), duration of care time(aOR, 1.03; 95% CI, 1.02–1.04; < 0.001),care time per day > 8 h (aOR, 1.50; 95% CI, 1.08–2.10; P = 0.016), self-finance (aOR, 2.52; 95% CI, 1.80–3.52 P < 0.001) were associated with increased risk of anxiety. Among them, self-finance and care time per day > 8 h were the major risk factors for anxiety (Table 2).
Table 2.
Multivariable Models Showing Association Between baseline risk factors and anxiety.
| OR (95% CI) | P* | |
|---|---|---|
| NIHSS | 1.08 (1.04–1.12) | 0.001 |
| Duration of care time | 1.03 (1.02–1.04) | < 0.001 |
| Care time (> 8 h) | 1.50 (1.08–2.10) | 0.016 |
| Self-finance | 2.52 (1.80–3.52) | < 0.001 |
*Multivariable adjusted for caregiver’s age, NIHSS, duration of care time, sex, education, care time per day > 8 h, self-finance, relationship to the patients, household income.
The risk factors of depression
According to the result of HDRS, 192(23.44%) main family caregivers had depression. The average HDRS of main family caregivers with depression was 23.11 ± 6.64, the average HDRS of main family caregivers with no depression was 8.57 ± 5.03. Baseline characteristics of caregivers in the no depression and depression groups were compared (Table 3). The results showed that caregivers’ age, NIHSS of patients, duration of care time, care time per day > 8 h and self-finance had effects on the depression, and the difference among two groups was statistically significant (P < 0.05). The depression level of caregivers of medical insurance group was lower than that of self-financed group (11.48 ± 7.89 vs 13.03 ± 8.81, P = 0.012), and the depression level of caregivers with care time per day > 8 h was higher than that of care time per day ≤ 8 h (13.04 ± 8.92 vs 10.51 ± 6.88, P < 0.001).Caregivers in depression group had older caregivers’ age, higher NIHSS, longer duration care time, higher percentage of care time per day > 8 h and self-finance than caregivers in no depression group (both P < 0.05).
Table 3.
Comparison of baseline characteristics between caregivers with no depression and depression groups.
| No depression group (627) | depression group (192) | OR (95% CI) | P* | |
|---|---|---|---|---|
| Caregivers’ age, y (Mean SD) | 54.40 ± 9.97 | 59.70 ± 9.44 | < 0.001 | |
| NIHSS of patients, median (IQR) | 97–12 | 107–14 | < 0.001 | |
| Duration of care time, d (Mean SD) | 133.49 ± 26.66 | 154.03 ± 29.74 | < 0.001 | |
| Females, n (%) | 439 (70.02) | 130 (67.71) | 0.90 (0.63–1.27) | 0.544 |
| Men, n (%) | 188 (29.98) | 62 (32.29) | 0.90 (0.63–1.27) | 0.544 |
| Education (high school and above), n (%) | 256 (40.83) | 76 (39.58) | 0.95 (0.68–1.32) | 0.758 |
| Care time per day > 8 h, n (%) | 338 (53.91) | 139 (72.40) | 2.24 (1.58–3.19) | < 0.001 |
| Relationship to the patient | ||||
| Spouse, n (%) | 397 (63.32) | 115 (59.90%) | 0.87 (0.62–1.21) | 0.391 |
| Other family member, n (%) | 230 (36.68) | 77 (40.10) | 0.87 (0.62–1.21) | 0.391 |
| Self-finance, n (%) | 175 (27.91) | 89 (46.35) | 2.23 (1.60–3.11) | < 0.001 |
| Household income, Chinese Yuan (CNY) < 5000/month | 299 (47.69) | 82 (42.71) | 1.26 (0.91–1.74) | 0.226 |
In order to further analyze the risk factors for depression. Multivariate logistic regression was performed (Table 4). The results showed that patient’s NIHSS (aOR, 1.06; 95% CI, 1.02–1.11; P = 0.012), duration of care time(aOR, 1.02; 95% CI, 1.02–1.04; P < 0.001), caregivers’ age (aOR, 1.06; 95% CI, 1.04–1.08; P < 0.001), care time per day > 8 h(aOR, 1.50; 95% CI, 1.02–2.22; P = 0.039),self-finance (aOR, 1.98; 95% CI, 1.39–2.81; P = 0.001) were associated with increased risk of depression.
Table 4.
Multivariable Models Showing Association Between baseline risk factors and depression.
| OR (95% CI) | P* | |
|---|---|---|
| NIHSS of patients | 1.06 (1.02–1.11) | 0.012 |
| Duration of care time | 1.02 (1.02–1.04) | < 0.001 |
| Caregivers’ age | 1.06 (1.04–1.08) | < 0.001 |
| Care time per day > 8 h | 1.50 (1.02–2.22) | 0.039 |
| Self-finance | 1.98 (1.39–2.81) | 0.001 |
*Multivariable adjusted for caregiver’s age, NIHSS, duration of care time, sex, education, care time per day > 8 h, self-finance, relationship to the patients, household income.
Characteristics of the patients
During the 6-month follow-up period, 54 patients were failed to follow-up, a total of 765 patients were finally analyzed, comprised 50.98% (390/765) women and 49.02% (375/765) men. The mean age was 67.33 ± 10.62 years (40–96 years). Among 765 main family caregivers, 290(37.91%) had anxiety symptoms, 182(23.79%) had depressive symptoms,81 caregivers had anxiety and depressive symptoms. In the study population, 480 patients had a history of hypertension, 310 had a history of diabetes, 458 had a history of hyperlipidemia, 210 patients smoke, 442 patients had current alcohol drinking.
Univariable models for predictors of death
During the 6-month follow-up period, 77 out of 765(10.07%) patients had died. Baseline characteristics of patients in the survivor and dead groups were compared (Table 5). At baseline, dead group showed significantly older age (70.78 ± 10.88 vs 66.94 ± 10.53, P < 0.001), higher NIHSS (12.96 ± 5.18 vs 9.71 ± 4.00, P < 0.001), higher percentage of caregivers with anxiety (70.13% vs 34.30%;OR,4.50;95% CI,2.69–7.51; P < 0.001) and caregivers with depression (44.16% vs 21.51%;OR,2.89;95% CI, 1.78–4.69; P < 0.001), and higher percentage of caregivers with anxiety + depression (24.68% vs 9.01%;OR,3.31;95% CI,1.85–5.91; P < 0.001) than patients with survivor group. Compared with survivor group, dead group had a significantly higher HADS score of caregivers (25.97 ± 12.88 vs 12.38 ± 5.91, P < 0.001), and higher HRDS score of caregivers (17.86 ± 13.14 vs 11.37 ± 7.38, P < 0.001).
Table 5.
Comparison of baseline characteristics between survival and dead groups.
| Survivor group (688) | Dead group (77) | OR (95% CI) | P* | |
|---|---|---|---|---|
| Age, y (Mean SD) | 66.94 ± 10.53 | 70.78 ± 10.88 | 0.002 | |
| HADS score, (Mean SD) | 12.38 ± 5.91 | 25.97 ± 12.88 | < 0.001 | |
| HRDS score, (Mean SD) | 11.37 ± 7.38 | 17.86 ± 13.14 | < 0.001 | |
| NIHSS, median (IQR) | 97–12 | 129–16 | < 0.001 | |
| Female, n (%) | 354 (51.45) | 36 (46.75) | 0.83 (0.52–1.33) | 0.434 |
| Male, n (%) | 334 (48.55) | 41 (53.25) | 0.83 (0.52–1.33) | 0.434 |
| BMI ≥ 24 kg/m, n (%) | 199 (28.92) | 25 (32.47) | 1.18 (0.71–1.96) | 0.517 |
| Hypertension, patients, n (%) | 430 (62.50) | 50 (64.94) | 1.11 (0.68–1.82) | 0.675 |
| Current Smoking, n (%) | 190 (27.62) | 20 (25.97) | 1.06 (0.63–1.79) | 0.759 |
| Current alcohol drinking, n (%) | 224 (32.56) | 18 (23.38) | 0.62 (0.36–1.10) | 0.100 |
| Diabetes, n (%) | 282 (40.99) | 28 (36.36) | 0.82 (0.51–1.34) | 0.433 |
| Hyperlipidemia, n (%) | 410 (59.59) | 48 (62.34) | 1.12 (0.69–1.82) | 0.641 |
| Ischemic stroke, n (%) | 545 (79.22) | 62 (80.52) | 0.92 (0.51–1.67) | 0.789 |
| Hemorrhagic stroke, n (%) | 143 (20.78) | 15 (19.48) | 0.92 (0.51–1.67) | 0.789 |
| Family history of stroke, n (%) | 146 (21.22) | 18 (23.38) | 1.13 (0.65–1.98) | 0.662 |
| Nasogastric tube feeding, n (%) | 86 (1.25) | 12 (15.58) | 1.29 (0.67–2.49) | 0.442 |
| Indwelling urinary catheter, n (%) | 108 (15.70) | 16 (20.78) | 1.41 (0.78–2.54) | 0.251 |
| Anxiety, n (%) | 236 (34.30) | 54 (70.13) | 4.50 (2.69–7.51) | < 0.001 |
| Depression, n (%) | 148 (21.51) | 34 (44.16) | 2.89 (1.78–4.69) | < 0.001 |
| Anxiety + depression, n (%) | 62 (9.01) | 19 (24.68) | 3.31 (1.85–5.91) | < 0.001 |
| Medication use | ||||
| Statin, n (%) | 321 (46.66) | 43 (55.84) | 1.45 (0.90–2.32) | 0.126 |
| Antihypertensive, n (%) | 346 (50.29) | 39 (50.65) | 1.01 (0.63–1.63) | 0.952 |
Multivariable Models on the Association between dead and anxiety/depression of caregivers
In unadjusted models, there was an association between the percentage of caregivers with anxiety or depression and 6-month mortality of patients with moderate-severe stroke. In the study, the results showed that 54 (54/290, 19.66%) patients had died in caregivers with anxiety group, which was higher percentage than that in caregivers with no anxiety group (23/475, 4.84%) (P < 0.001); and 34(34/182,) patients died in caregivers with depression group, which was higher percentage than that in caregivers with no depression group(43/583, 4.84%) (P < 0.001).
To further analyze the association between anxiety and depression of caregivers and 6-month mortality of patients with moderate-severe stroke, the factors associated with 6-month mortality in the univariate analyses (P < 0.20) were entered into the multivariate logistic regression analysis[adjusted for age, baseline NIHSS, current alcohol drinking, the percentage of caregivers with anxiety and depressive symptoms/the percentage of caregivers with anxiety + depressive symptoms (or HADS score and HRDS score of caregivers), statin use], the results showed that older age (aOR,1.03;95% CI, 1.01–1.06; P = 0.010), higher NIHSS (aOR,1.12;95% CI, 1.06–1.18; P < 0.001), the percentage of caregivers with anxiety (aOR,3.57;95% CI, 2.09–6.11; P < 0.001), and the percentage of caregivers with depression (aOR,2.20;95% CI, 1.30–3.72; P = 0.003) were associated with increased risk of 6-month mortality of patients with moderate-severe stroke (Table 6), when HADS and HRDS score of caregivers were entered into multivariate logistic regression (Model 2), HADS score(aOR,1.19;95% CI, 1.15–1.24; P < 0.001) and HRDS score(aOR,1.10;95% CI, 1.07–1.41; P < 0.001) of caregivers resulted to be associated with increased risk of 6-month mortality of patients with moderate-severe stroke, and higher NIHSS (aOR,1.12;95% CI, 1.05–1.19; P = 0.001) were associated with increased risk of 6-month mortality, when the percentage of caregivers with anxiety + depression were entered into multivariate logistic regression (Model 3), the results showed that older age (aOR,1.04;95% CI, 1.01–1.06; P = 0.003), higher NIHSS (aOR,1.16;95% CI, 1.08–1.20; P < 0.001), the percentage of caregivers with anxiety (aOR,2.29;95% CI, 1.21–4.33; P = 0.011).
Table 6.
Multivariable Models Showing Association Between risk factors and 6-month mortality.
| OR (95% CI) | P* | |
|---|---|---|
| Model 1 (the percentage of caregivers with anxiety and depressive symptoms) | ||
| Age | 1.03 (1.01–1.06) | 0.010 |
| NIHSS | 1.12 (1.06–1.18) | < 0.001 |
| Caregivers with anxiety symptoms | 3.57 (2.09–6.11) | < 0.001 |
| Caregivers with depressive symptoms | 2.20 (1.30–3.72) | 0.003 |
| Model 2 (HADS and HRDS score) | ||
| NIHSS | 1.12 (1.05–1.19) | 0.001 |
| HADS score of caregivers | 1.19 (1.15–1.24) | < 0.001 |
| HRDS score of caregivers | 1.10 (1.07–1.41) | < 0.001 |
| Model 3 (the percentage of caregivers with anxiety + depressive symptoms) | ||
| Age | 1.04 (1.01–1.06) | 0.003 |
| NIHSS | 1.14 (1.08–1.20) | < 0.001 |
| Caregivers with anxiety + depression symptoms | 2.29 (1.21–4.33) | 0.011 |
*Multivariable adjusted for age, baseline NIHSS, current alcohol drinking, the percentage of caregivers with anxiety and depressive symptoms/the percentage of caregivers with anxiety + depressive symptoms (or HADS score and HRDS score of caregivers), statin use.
Discussion
Based on these results we found that high incidence of anxiety and depression of main family caregivers of patients with moderate-severe stroke, which were consistent with previous studies, the data showed that 297 (36.26%) main family caregivers had anxiety, and 192(23.44%) main family caregivers had depression5,23,24, furthermore, we found that anxiety and depression of caregivers were associated with increased risk of 6-month mortality of patients with moderate-severe stroke.
Stroke is leading reason to cause the disability25–27. Previous studies revealed that most stroke survivors’ leave hospital with varying degrees of disability, they are often accompanied by limb hemiplegia and other dysfunctions28–30. In China, the most of stroke survivors lived at home after discharge, obviously, the huge and invisible mental pression transfer to the caregivers. In this study, the results disclosed that the higher ratio of caregivers was female, they were the spouse of the patients, which was consistent with previous studies31, this may be due to the social and cultural lifestyles in China. In past studies showed that there was no difference in physiological distress between female and male caregivers32,33, whereas some studies reported higher rates of psychological distress in females34,35.
Meanwhile, our resulted demonstrated that the percentage of anxiety and depression was respectively 36.26% and 23.32% in main family caregivers, which was consistent with others5,11,12. The results showed that NIHSS, duration of care time, care time per day > 8 h and self-finance had significant predictive effects on the anxiety and depression of main family caregivers, and older caregivers’ age was a risk factor of depression symptoms. It can be considered that the emotional status of the main family caregivers is related to the level of dependence of the patients on assistance and the economic burden. Stroke treatment and rehabilitation costs are very high. Family economic burden is related with the medical payment method36. In our study, we also found that the percentage of main family caregivers with anxiety and depression in self-finance families were higher than those of in medical insurance payment families, which suggested that the economic burden of illness is an important risk factor of anxiety and depression for caregivers. The length of care time is a risk factor for development of anxiety and depression in main family caregiver. In this study, duration of care time and care time per day > 8 h were positively correlated with HARS and HDRS scores. Past study also showed that anxiety and depression were more likely to appear with longer care time37,38. This could be because the care time are too long every day, occupied too much of the caregivers' personal time and reducing their work, social and entertainment time in largest degree. On the other hand, the caregivers' age is related to depression, the older the caregiver, the higher the risk of depression, this may be because that elder caregivers had limited energy, which may be more likely to lead to fatigue.
There are few studies on the effect of anxiety and depression on mortality of patients with moderate-severe stroke. In our study, we investigated the association between the anxiety and depression of the main family caregivers and the 6-month mortality of patients with moderate-severe stroke. The results demonstrated that anxiety and depression of caregivers were associated with increased risk of 6-month mortality of patients with moderate-severe stroke. Therefore, it may be suggested that any support such as social and psychological leading to relieve anxiety or depression of the caregivers will be helpful to improve the recovery of the patients.
Conclusions
In conclusion, caregivers’ age, NIHSS of patients, duration of care time, care time per day > 8 h and self-finance are major risk factors for development of anxiety and depression in main family caregiver. The anxiety and depression of main family caregivers have a negative impact on 6-month mortality of patients with moderate-severe stroke. These results indicate that clinical nurses should provide home care guidance, psychological counseling and social support to family caregivers to improve their mental health.
Limitation
We selected the patients with moderate-severe stroke, while the follow up of their rehabilitation of patients post discharge were failed. Moreover, we did not collect data on caregivers' use of antidepressants and anxiety and depression in patients with stroke, 14-item Chinese HARS and HDRS score are just screening tools, we used HARS and HDRS to assess whether the caregiver had symptoms of anxiety or depression, and should not be used to diagnosis anxiety and depression, we did not analyze the effect of different levels of caregivers’ anxiety or depression on patients' mortality which might have influenced the results.
Acknowledgements
We thank all patients and their families for generously consenting to use the data of patients and caregivers in this research.
Abbreviations
- HARS
14-Item Chinese Hamilton Anxiety Rating Scale
- HDRS
17-Item Chinese Hamilton Depression Rating Scale
- NIHSS
National Institutes of Health Stroke Scale
- CI
Confidence interval
- M
Mean
- OR
Odds ratio
- SD
Standard deviation
- IQR
Interquartile range
Author contributions
J.Z. was responsible for the concept and design of the study, data analysis and the first draft of the paper and final manuscript. J.L. and Y.M. were responsible for the concept and design of the study, the data analysis and interpretation. J.X. and Y.C. was responsible for overseeing the concept and design of the study, the data analysis and interpretation, and writing the paper. Z.Z., J.Y., J.X. and P.C. were responsible for data collection. All authors read and approved the final manuscript for publication.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wang W, Jiang B, Sun H, et al. Prevalence, incidence, and mortality of stroke in China: results from a Nationwide Population-Based Survey of 480 687 adults. Circulation. 2017;135(8):759–771. doi: 10.1161/CIRCULATIONAHA.116.025250. [DOI] [PubMed] [Google Scholar]
- 2.Martín-Martín L, Membrilla-Mesa MD, Lozano-Lozano M, et al. Association between physiological and subjective aspects of pain and disability in post-stroke patients with shoulder pain: a cross-sectional study. J. Clin. Med. 2019;8(8):1093. doi: 10.3390/jcm8081093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cantone L, Tobaldini E, Favero C, et al. Particulate air pollution, clock gene methylation, and stroke: effects on stroke severity and disability. Int. J. Mol. Sci. 2020;21(9):3090. doi: 10.3390/ijms21093090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cucchiara B, George DK, Kasner SE, et al. Disability after minor stroke and TIA: a secondary analysis of the SOCRATES trial. Neurology. 2019;93(7):e708–e716. doi: 10.1212/WNL.0000000000007936. [DOI] [PubMed] [Google Scholar]
- 5.Kruithof WJ, Post MW, van Mierlo ML, et al. Caregiver burden and emotional problems in partners of stroke patients at two months and one year post-stroke: determinants and prediction. Patient Educ. Couns. 2016;99(10):1632–1640. doi: 10.1016/j.pec.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 6.Forster A, Dickerson J, Young J, et al. A cluster randomised controlled trial and economic evaluation of a structured training programme for caregivers of inpatients after stroke: the TRACS trial. Health Technol. Assess. 2013;17(46):1–216. doi: 10.3310/hta17460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ohman M, Söderberg S. The experiences of close relatives living with a person with serious chronic illness. Qual. Health Res. 2004;14(3):396–410. doi: 10.1177/1049732303261692. [DOI] [PubMed] [Google Scholar]
- 8.Godwin KM, Swank PR, Vaeth P, et al. The longitudinal and dyadic effects of mutuality on perceived stress for stroke survivors and their spousal caregivers. Aging Ment. Health. 2013;17(4):423–431. doi: 10.1080/13607863.2012.756457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loh AZ, Tan JS, Zhang MW, et al. The global prevalence of anxiety and depressive symptoms among caregivers of stroke survivors. J. Am. Med. Dir. Assoc. 2017;18(2):111–116. doi: 10.1016/j.jamda.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Zorowitz RD, Gillard PJ, Brainin M. Poststroke spasticity: sequelae and burden on stroke survivors and caregivers. Neurology. 2013;80(3 Suppl 2):S45–52. doi: 10.1212/WNL.0b013e3182764c86. [DOI] [PubMed] [Google Scholar]
- 11.Cameron JI, Cheung AM, Streiner DL, et al. Stroke survivors' behavioral and psychologic symptoms are associated with informal caregivers' experiences of depression. Arch. Phys. Med. Rehabil. 2006;87(2):177–183. doi: 10.1016/j.apmr.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 12.McCullagh E, Brigstocke G, Donaldson N, et al. Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke. 2005;36(10):2181–2186. doi: 10.1161/01.STR.0000181755.23914.53. [DOI] [PubMed] [Google Scholar]
- 13.Anderson CS, Linto J, Stewart-Wynne EG. A population-based assessment of the impact and burden of caregiving for long-term stroke survivors. Stroke. 1995;26(5):843–849. doi: 10.1161/01.STR.26.5.843. [DOI] [PubMed] [Google Scholar]
- 14.Oliva-Moreno J, Peña-Longobardo LM, Mar J, et al. Determinants of informal care, burden, and risk of burnout in caregivers of stroke survivors: the CONOCES study. Stroke. 2018;49(1):140–146. doi: 10.1161/STROKEAHA.117.017575. [DOI] [PubMed] [Google Scholar]
- 15.Savini S, Buck HG, Dickson VV, et al. Quality of life in stroke survivor-caregiver dyads: a new conceptual framework and longitudinal study protocol. J. Adv. Nurs. 2015;71(3):676–687. doi: 10.1111/jan.12524. [DOI] [PubMed] [Google Scholar]
- 16.Hunt D, Smith JA. The personal experience of carers of stroke survivors: an interpretative phenomenological analysis. Disabil. Rehabil. 2004;26(16):1000–1011. doi: 10.1080/09638280410001702423. [DOI] [PubMed] [Google Scholar]
- 17.Forsberg-Wärleby G, Möller A, Blomstrand C. Spouses of first-ever stroke patients: psychological well-being in the first phase after stroke. Stroke. 2001;32(7):1646–1651. doi: 10.1161/01.STR.32.7.1646. [DOI] [PubMed] [Google Scholar]
- 18.Roth DL, Haley WE, Sheehan OC, et al. Depressive symptoms after ischemic stroke: population-based comparisons of patients and caregivers with matched controls. Stroke. 2020;51(1):54–60. doi: 10.1161/STROKEAHA.119.027039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamilton M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959;32(1):50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 20.Zhang M. Depression and Anxiety. Changsha: Hunan Science and Technology Press; 1998. pp. 30–32. [Google Scholar]
- 21.Hamilton M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry. 1960;23(1):56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zheng YP, Zhao JP, Phillips M, et al. Validity and reliability of the Chinese Hamilton Depression Rating Scale. Br. J. Psychiatry. 1988;152:660–664. doi: 10.1192/bjp.152.5.660. [DOI] [PubMed] [Google Scholar]
- 23.Sennfält S, Ullberg T. Informal caregivers in stroke: Life impact, support, and psychological well-being—a Swedish Stroke Register (Riksstroke) study. Int. J. Stroke. 2020;15(2):197–205. doi: 10.1177/1747493019858776. [DOI] [PubMed] [Google Scholar]
- 24.Byun E, Evans L, Sommers M, et al. Depressive symptoms in caregivers immediately after stroke. Top Stroke Rehabil. 2019;26(3):187–194. doi: 10.1080/10749357.2019.1590950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feigin VL, Roth GA, Naghavi M, et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016;15(9):913–924. doi: 10.1016/S1474-4422(16)30073-4. [DOI] [PubMed] [Google Scholar]
- 26.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feigin VL, Norrving B, Mensah GA. Global burden of stroke. Circ. Res. 2017;120(3):439–448. doi: 10.1161/CIRCRESAHA.116.308413. [DOI] [PubMed] [Google Scholar]
- 28.Hallevi H, Barreto AD, Liebeskind DS, et al. Identifying patients at high risk for poor outcome after intra-arterial therapy for acute ischemic stroke. Stroke. 2009;40(5):1780–1785. doi: 10.1161/STROKEAHA.108.535146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Flint AC, Xiang B, Gupta R, et al. THRIVE score predicts outcomes with a third-generation endovascular stroke treatment device in the TREVO-2 trial. Stroke. 2013;44(12):3370–3375. doi: 10.1161/STROKEAHA.113.002796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saposnik G, Guzik AK, Reeves M, et al. Stroke prognostication using age and NIH Stroke Scale: SPAN-100. Neurology. 2013;80(1):21–28. doi: 10.1212/WNL.0b013e31827b1ace. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Greenwood N, Mackenzie A, Cloud GC, et al. Informal carers of stroke survivors–factors influencing carers: a systematic review of quantitative studies. Disabil. Rehabil. 2008;30(18):1329–1349. doi: 10.1080/09638280701602178. [DOI] [PubMed] [Google Scholar]
- 32.Tompkins CA, Schulz R, Rau MT. Post-stroke depression in primary support persons: predicting those at risk. J. Consult. Clin. Psychol. 1988;56(4):502–508. doi: 10.1037/0022-006X.56.4.502. [DOI] [PubMed] [Google Scholar]
- 33.Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist. 1986;26(3):260–266. doi: 10.1093/geront/26.3.260. [DOI] [PubMed] [Google Scholar]
- 34.Em S, Bozkurt M, Caglayan M, et al. Psychological health of caregivers and association with functional status of stroke patients. Top Stroke Rehabil. 2017;24(5):323–329. doi: 10.1080/10749357.2017.1280901. [DOI] [PubMed] [Google Scholar]
- 35.Simon C, Kumar S, Kendrick T. Cohort study of informal carers of first-time stroke survivors: profile of health and social changes in the first year of caregiving. Soc. Sci. Med. 2009;69(3):404–410. doi: 10.1016/j.socscimed.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 36.Familiar I, Murray S, Ruisenor-Escudero H, et al. Socio-demographic correlates of depression and anxiety among female caregivers living with HIV in rural Uganda. AIDS Care. 2016;28(12):1541–1545. doi: 10.1080/09540121.2016.1191609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bugge C, Alexander H, Hagen S. Stroke patients' informal caregivers. Patient, caregiver, and service factors that affect caregiver strain. Stroke. 1999;30(8):1517–1523. doi: 10.1161/01.STR.30.8.1517. [DOI] [PubMed] [Google Scholar]
- 38.Bakas T, Clark PC, Kelly-Hayes M, et al. Evidence for stroke family caregiver and dyad interventions. Stroke. 2014;45(9):2836–2852. doi: 10.1161/STR.0000000000000033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.