Abstract
Objective:
Determine incidence and risk factors for readmissions in early infancy
Study Design:
Secondary analysis of data from the Cesarean Section Optimal Antibiotic Prophylaxis trial. All unplanned revisits (unplanned clinic, ER visits, and hospital readmissions) and hospital readmissions (initial discharge to 3-month follow-up) were analyzed.
Results:
295 (15.9%) of 1850 infants had revisits with risk factors being ethnicity (adjusted odds ratio (aOR): 0.6 for Hispanic), maternal postpartum antibiotics (1.89), azithromycin treatment (1.22), small for gestational age (1.68), apnea (3.82), and hospital stay after birth >90th percentile (0.49). 71 (3.8%) of 1850 infants were readmitted with risk factors being antenatal steroids (aOR 2.49), elective repeat C/section (0.72), postpartum maternal antibiotics (2.22), O2 requirement after delivery room (2.82), and suspected/proven neonatal sepsis (0.55).
Conclusion(s):
Multiple risk factors were identified, suggesting potential impact on the neonatal microbiome (maternal postpartum antibiotics) or issues related to access/cost of care (Hispanic ethnicity associated with fewer revisits).
Introduction:
Readmissions and emergency department visits are considered markers of the quality of health care (eg. discharge planning, transition of care between inpatient and outpatient providers), but have not been endorsed to date for neonatal care, primarily because of a lack of agreement between study teams of what constitutes “preventable” readmissions.1, 2, 3, 4, 5 Readmissions and emergency department visits of very premature, moderate preterm, late preterm, and early term infants have been studied by many investigators.6, 7, 8 However, term infants account for many readmissions, for they comprise the majority (~90%) of live births, but readmissions of term infants have not been as well studied.6 Most studies of readmissions of term infants have focused on early (≤48 hours after birth) versus later (>48 hours) discharge.9, 10, 11 Infants born by vaginal delivery are more likely to be discharged earlier, and are at higher risk of readmission12 for multiple causes such as hyperbilirubinemia, poor feeding, or other issues that are detected in infants while they are still in hospital. Infants born following cesarean delivery are usually not discharged early, as mothers are hospitalized for longer as compared to after vaginal deliveries.13 Therefore, a study of readmissions or emergency department visits of infants following cesarean delivery would exclude readmissions due to early discharges of term infants, enabling the identification of more specific risk factors for readmissions after cesarean delivery.
Readmissions of infants following cesarean delivery are not uncommon, and may potentially be influenced by interventions such as maternal antimicrobial therapy.14 Maternal antimicrobial therapy with drugs such as azithromycin (AZI) may reduce transmission of pathogens to the neonate, reducing the risk of neonatal sepsis or other morbidities.15, 16, 17 The antimicrobial therapy may also potentially influence acquisition of the postnatal microbiome, and thereby possibly alter the rate of atopic disease, gastrointestinal disorders (gut microbiome), or asthma (airway microbiome). AZI may also cause gastrointestinal side effects such as diarrhea, vomiting, or abdominal pain in pediatric patients, which may manifest as feeding issues in neonates. In a recent study of infants with gestational ages 34–42 weeks (either vaginal or cesarean delivery) discharged from well-baby nurseries18, 1.8% (5308 of 296,114 infants) were readmitted within 28 days of discharge, primarily for feeding issues (41%), jaundice (35%), or respiratory distress (33%). There is therefore a strong rationale to evaluate risk factors for readmissions following cesarean delivery, and to determine effects of maternal antimicrobial therapy on readmissions in early infancy.
In the Cesarean Section Optimal Antibiotic Prophylaxis (C/SOAP) trial,19 that evaluated the benefits and safety of azithromycin-based extended-spectrum prophylaxis in women undergoing nonelective cesarean section adjunctive AZI reduced endometritis, wound infection and other postpartum infections in mothers >24w gestational age (GA) undergoing C/section during labor or after membrane rupture (AZI 6.1% vs. Placebo 12%, p<0.001). There were no differences in neonatal death/morbidities (14.3% vs. 13.6%), NICU admission (16.8% vs. 17%), or neonatal readmissions/unscheduled visits (16.7% vs. 14.1%).19 This more recent cohort of infants had information prospectively collected regarding hospital readmissions and all unplanned revisits, and enabled us to determine the incidence, reasons and risk factors for neonatal readmissions in a cohort of infants who were not discharged early.
Methods:
Infants whose mothers were randomized in the C/SOAP trial were analyzed. The full details of this trial have been published elsewhere,19 but in brief, this trial conducted in 14 US centers studied 2013 women with a singleton pregnancy at 24 or more weeks of gestation who were undergoing cesarean delivery during labor or after membrane rupture, who were randomly assigned to receive either 500 mg of azithromycin IV or placebo in addition to standard antibiotic prophylaxis.19 Women were screened from April 2011 to November 2014, with the first delivery on 5/2/2011 and last delivery on 11/25/2014. Participants had a 6-week postpartum visit and a 3-month telephone call to identify infant deaths and adverse events. Key study outcomes were infant readmission or unplanned revisit. Two sets of analyses were completed where the primary outcome variable was first based on any type of revisit and subsequently based on hospital-only readmissions. Characteristics were compared between groups with and without the outcomes with bivariate analyses including t-tests for continuous variables and chi-square tests of association for categorical variables. Parsimonious multivariable logistic regression models were developed using backward elimination (p>0.2 for removal) for the outcomes of hospital readmissions (readmissions between initial discharge and 3-month follow-up) and all revisits (unplanned clinic or ER visits and hospital readmissions). We report the c-statistic, equivalent to the area under the curve of the receiver operating characteristic curve [AUC of ROC]), which ranges from 0.5 to 1.0, with higher values representing better predictive accuracy.
The variables that identified as statistically significantly different in bivariate analyses were considered in the multivariable models along with additional variables selected based on the existing literature and biologic plausibility. All variables considered were selected from the variables that were used for the C/SOAP trial.19 Maternal variables included age, race/ethnicity (Black vs. White vs Hispanic), marital status (married vs. not married), insurance status (private vs. none/other), prior pregnancy, any smoking history, clinical chorioamnionitis, antenatal steroids, indication for c-section (elective repeat vs. others), maternal endometritis, or wound infection or sepsis or other (abdominal/pelvic abscess/pelvic thrombophlebitis), postpartum readmission/unplanned visit, and postpartum antibiotics. Neonatal variables included birth weight, gestational age, sex, type of feeding, NICU admission, Respiratory Distress Syndrome (RDS), phototherapy, apnea (treated by mechanical ventilation or medication), intubation or chest compression in delivery room (not for meconium), oxygen requirement after delivery room, newborn sepsis suspected or proven, and duration of stay in hospital (neonatal discharge date-birth date).
All statistical tests were two-sided and evaluated at a 0.05 level of statistical significance. No adjustment was made for multiple comparisons for this exploratory analysis. SAS version 9.4 was used for all statistical analyses.
Results:
Among 2013 women who were randomized in the primary trial, 1850 were analyzed. A total of 163 infants were excluded: 109 with no follow up, 6 who were transferred to chronic care, 1 death before discharge, and 47 in hospital for ≥ 4 weeks (Figure 1). The delivery gestational range for the total population of infants studied was 31–42 weeks with 169 preterm deliveries.
Figure 1:
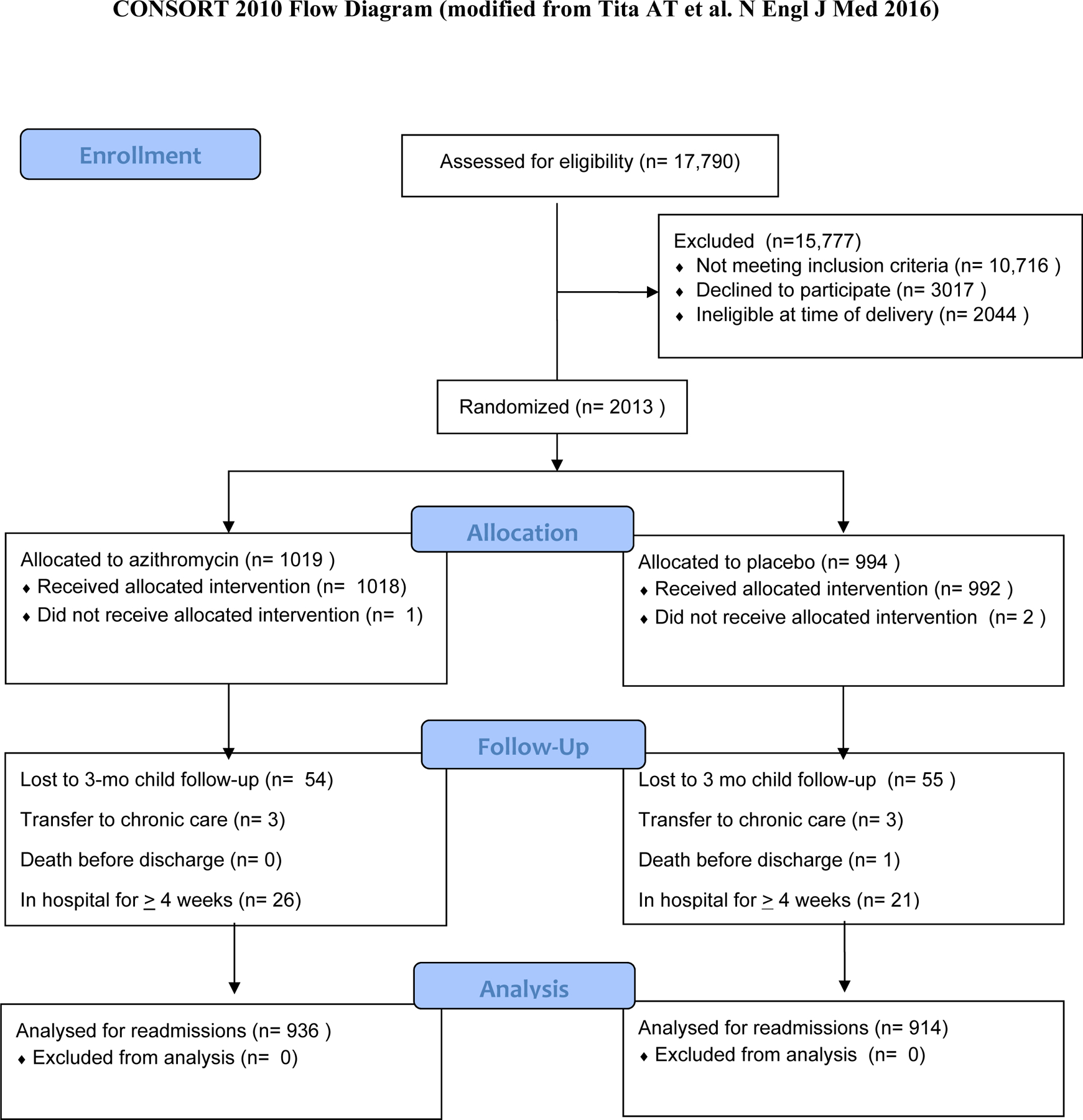
Flow diagram of patient enrollment
All visits/readmissions:
Of 1850 infants, 295 (15.9%; 14.3%−17.6%) had unplanned clinic or ER visits and hospital readmissions.
In bivariate analyses, revisits were significantly associated with maternal characteristics of race/ethnicity (less for Hispanic) and receipt of postpartum maternal antibiotics (Table 1), and with neonatal characteristics of RDS, apnea, and intubation/chest compression in delivery room (Table 1).
Table 1:
All revisits
| Maternal Characteristics | |||
|---|---|---|---|
|
All Revisits (n = 295) |
No Revisits (n = 1555) |
P value | |
| Years of Age, mean ± SD | 28.3 ± 6.3 | 28.4 ± 6.4 | 0.66 |
| Race/Ethnicity, n (%) | 0.003 | ||
| Black, non-Hispanic | 115 (39.0%) | 505 (32.5%) | |
| Hispanic/Other | 68 (23.1%) | 509 (32.7%) | |
| White, non-Hispanic | 112 (38.0%) | 541 (34.8%) | |
| Married, n (%) | 122 (42.4%) | 709 (46.0%) | 0.25 |
| Private insurance, n (%) | 99 (34.4%) | 497 (32.2%) | 0.48 |
| Prior pregnancy, n (%) | 160 (52.2%) | 863 (55.5%) | 0.69 |
| Any smoking, n (%) | 25 (8.5%) | 164 (10.6%) | 0.28 |
| Chorioamnionitis, n (%) | 7 (2.4%) | 16 (1.0%) | 0.07 |
| Antenatal steroids for lung maturity, n (%) | 10 (3.4%) | 46 (3.0%) | 0.69 |
| Primary indications for cesarean delivery, n (%) | 0.78 | ||
| Elective repeat | 133 (45.1%) | 715 (46.0%) | |
| Other | 162 (54.9%) | 840 (54.0%) | |
| Composite wound infection, n (%) | 15 (5.1%) | 64 (4.1%) | 0.45 |
| Postpartum readmission/unplanned visits, n (%) | 36 (12.2%) | 153 (9.8%) | 0.22 |
| Postpartum antibiotics, n (%) | 39 (13.2%) | 121 (7.8%) | 0.002 |
| Azithromycin dose, n (%) | 163 (55.3%) | 773 (49.7%) | 0.08 |
| Neonatal Characteristics | |||
|
All Revisits (n = 295) |
No Revisits (n = 1555) |
P value | |
| Birthweight, g | 3311 ± 646 | 3334 ± 574 | 0.58 |
| Gestational age at birth, wks | 39.1 ± 1.8 | 39.2 ± 1.7 | 0.75 |
| Feeding type, n (%) | 0.92 | ||
| Bottle | 76 (25.8%) | 386 (24.8%) | |
| Breast | 118 (40.0%) | 621 (39.9%) | |
| Both | 101 (34.2%) | 548 (35.2%) | |
| NICU admission, n (%) | 45 (15.3%) | 221 (14.2%) | 0.64 |
| RDS, n (%) | 14 (4.8%) | 34 (2.2%) | 0.011 |
| Phototherapy, n (%) | 11 (3.7%) | 77 (5.0%) | 0.67 |
| Apnea (treated by ventilator or medication), n (%) | 8 (2.7%) | 13 (0.8%) | 0.012 |
| Intubation or chest compression in delivery room, n (%)* | 7 (2.4%) | 12 (0.8%) | 0.022 |
| Oxygen requirement after delivery room, n (%) | 26 (8.8%) | 107 (6.9%) | 0.24 |
| Newborn sepsis suspected or proven, n (%) | 32 (10.9%) | 164 (10.6%) | 0.88 |
| Duration of hospital stay, days | 3 (3–4) | 3 (3–4) | 0.56 |
Does not include meconium
In the final multivariable logistic regression model for all visits/readmissions, selected maternal characteristics included race/ethnicity (aOR 0.6; 95% CI: 0.43–0.83 for Hispanic vs White Non-Hispanic), smoking (0.72;0.46–1.13), postpartum antibiotics (1.89;1.27–2.82) and AZI (1.22;0.95–1.59), while neonatal characteristics included SGA (1.68;1.1–2.5), apnea (3.82;1.48–9.86), and hospital stay>90th percentile (0.49;0.3–0.82) (Table 2). The c statistic for the final regression model was 0.60.
Table 2:
Regression analysis – All revisits
| Maternal data | ||
|---|---|---|
| Unadjusted RR | Adjusted OR | |
| Years of Age | 1.00 (0.98–1.02) | x |
| Race/Ethnicity | ||
| Black, non-Hispanic | 1.10 (0.83–1.47) | 0.97 (0.72–1.30) |
| Hispanic/Other | 0.65 (0.47–0.89) | 0.60 (0.43–0.83) |
| White, non-Hispanic | Ref | Ref |
| Married | 0.92 (0.80–10.6) | x |
| Private insurance | 1.07 (0.90–1.27) | x |
| Prior pregnancy | 0.98 (0.87–1.10) | x |
| Any smoking | 0.80 (0.54–1.20) | 0.72 (0.46–1.13) |
| Chorioamnionitis | 2.31 (0.96–5.56) | x |
| Antenatal steroids for lung maturity | 1.15 (0.58–2.24) | x |
| Primary indications for cesarean delivery | ||
| Elective repeat | 0.98 (0.86–1.12) | x |
| Other | Ref | x |
| Composite wound infection | 1.24 (0.71–2.14) | x |
| Postpartum readmission/unplanned visits | 1.24 (0.88–1.74) | x |
| Postpartum antibiotics | 1.70 (1.21–2.38) | 1.89 (1.27–2.82) |
| Azithromycin dose | 1.11 (0.99–1.25) | 1.22 (0.95–1.59) |
| Neonatal Data | ||
| Birthweight ≤ 10th percentile (2622.5g) | 1.47 (1.008–2.15) | 1.68 (1.10–2.55) |
| Gestational age at birth | 0.99 (0.92–1.06) | x |
| Feeding type | ||
| Bottle | 1.03 (0.77–1.38) | x |
| Breast | 1.07 (0.77–1.49) | x |
| Both | Ref | x |
| Nicu admission | 1.07 (0.80–1.44) | x |
| RDS* | 2.17 (1.18–3.99) | x |
| Phototherapy | 0.75 (0.41–1.40) | x |
| Apnea (treated by ventilator or medication)* | 3.24 (1.36–7.76) | 3.82 (1.49–9.86) |
| Intubation or chest compression in delivery room* | 3.07 (1.22–7.75) | x |
| Oxygen requirement after delivery room | 1.28 (0.85–1.93) | x |
| Newborn sepsis suspected or proven | 1.03 (0.72–1.47) | x |
| Hospital stay ≥ 90th percentile (5 days) | 0.81 (0.54–1.19) | 0.49 (0.30–0.82) |
These three variables were highly correlated so we only included Apnea in the model
Hospital readmissions:
Seventy-one (3.8%; 3.0%−4.7%) of 1850 infants were readmitted.
In bivariate analyses, readmissions were significantly associated with maternal characteristics of antenatal steroids and maternal postpartum antibiotics, and with neonatal characteristics of respiratory distress syndrome (RDS), and O2 requirement after delivery room (Table 3).
Table 3:
Hospital readmissions
| Maternal characteristics | |||
|---|---|---|---|
| Hospital Readmission (n = 71) |
No Hosp Readmission (n = 1779) |
P value | |
| Years of Age, mean ± SD | 28.0 ± 6.4 | 28.4 ± 6.3 | 0.60 |
| Race/Ethnicity, n (%) | |||
| Black, non-Hispanic | 23 (32.4%) | 597 (33.6%) | 0.74 |
| Hispanic/Other | 20 (28.2%) | 557 (31.3%) | |
| White, non-Hispanic | 28 (39.4%) | 625 (35.1%) | |
| Married, n (%) | 27 (38.6%) | 804 (45.7%) | 0.24 |
| Private insurance, n (%) | 21 (30.0%) | 575 (32.7%) | 0.64 |
| Prior pregnancy, n (%) | 39 (54.9%) | 984 (55.3%) | 0.95 |
| Any smoking, n (%) | 7 (9.9%) | 182 (10.2%) | 0.92 |
| Chorioamnionitis, n (%) | 2 (2.8%) | 21 (1.2%) | 0.22 |
| Antenatal steroids for lung maturity, n (%) | 6 (8.5%) | 50 (2.8%) | 0.018 |
| Primary indications for cesarean delivery, n (%) | 0.18 | ||
| Elective repeat | 27 (38.0%) | 821 (46.2%) | |
| Other | 44 (62.0%) | 958 (53.9%) | |
| Composite wound infection, n (%) | 4 (5.6%) | 75 (4.2%) | 0.54 |
| Postpartum readmission/unplanned visits, n (%) | 10 (14.1%) | 179 (10.1%) | 0.27 |
| Postpartum antibiotics, n (%) | 11 (15.5%) | 149 (8.4%) | 0.036 |
| Azithromycin dose, n (%) | 35 (49.3%) | 901 (50.7%) | 0.82 |
| Neonatal Characteristics | |||
|
Hospital Readmission (n = 71) |
No Hosp Readmission (n = 1779) |
P value | |
| Birthweight, g | 3299 ± 710 | 3331 ± 581 | 0.70 |
| Gestational age at birth, wks | 38.8 ± 1.8 | 39.2 ± 1.7 | 0.08 |
| Feeding type, n (%) | 0.19 | ||
| Bottle | 21 (29.6%) | 441 (24.8%) | |
| Breast | 21 (29.6%) | 718 (40.4%) | |
| Both | 29 (40.9%) | 620 (34.9%) | |
| NICU admission, n (%) | 15 (21.1%) | 251 (14.1%) | 0.10 |
| RDS, n (%) | 5 (7.0%) | 43 (2.4%) | 0.034 |
| Phototherapy, n (%) | 6 (8.5%) | 82 (4.6%) | 0.15 |
| Apnea (treated by ventilator or medication), n (%) | 2 (2.8%) | 19 (1.1%) | 0.19 |
| Intubation or chest compression in delivery room, n (%)* | 2 (2.8%) | 17 (1.0%) | 0.16 |
| Oxygen requirement after delivery room, n (%) | 12 (16.9%) | 121 (6.8%) | 0.001 |
| Newborn sepsis suspected or proven, n (%) | 8 (11.3%) | 188 (10.6%) | 0.85 |
| Duration of hospital stay, days | 3 (3–4) | 3 (3–4) | 0.38 |
Does not include meconium
Maternal characteristics presented in the final multivariable logistic regression model included antenatal steroids (aOR 2.49; 95% CI 0.95–6.6), anticipated elective repeat C/section (0.72; 0.44–1.18), and postpartum maternal antibiotics (2.22; 1.13–4.4), while neonatal characteristics included O2 requirement after delivery room (2.82; 1.3–6), and suspected or proven neonatal sepsis (0.55; 0.24–1.29) (Table 4). The c statistic for the final regression model was 0.62.
Table 4:
Regression Analysis: Hospital readmissions
| Maternal data | ||
|---|---|---|
| Unadjusted RR | Adjusted OR | |
| Years of Age | 0.99 (0.95–1.03) | x |
| Race/Ethnicity | ||
| Black, non-Hispanic | 0.86 (0.49–1.51) | x |
| Hispanic/Other | 0.80 (0.45–1.44) | x |
| White, non-Hispanic | Ref | |
| Married | 0.84 (0.63–1.14) | x |
| Private insurance | 0.92 (0.64–1.32) | x |
| Prior pregnancy | 0.99 (0.80–1.23) | x |
| Any smoking | 0.96 (0.47–1.97) | x |
| Chorioamnionitis | 2.39 (0.57–9.98) | x |
| Antenatal steroids for lung maturity | 3.01 (1.33–6.78) | 2.49 (0.95–6.55) |
| Primary indications for cesarean delivery | ||
| Elective repeat | 0.82 (0.61–1.11) | 0.72 (0.44–1.18) |
| Other | Ref | Ref |
| Composite wound infection | 1.34 (0.50–3.55) | x |
| Postpartum readmission/unplanned visits | 1.40 (0.78–2.53) | x |
| Postpartum antibiotics | 1.85 (1.05–3.25) | 2.22 (1.13–4.40) |
| Azithromycin dose | 0.97 (0.77–1.24) | x |
| Neonatal Data | ||
| Unadjusted RR | Adjusted OR | |
| Birthweight ≤ 10th percentile (2622.5g) | 1.89 (1.14–3.16) | x |
| Gestational age at birth | 0.90 (0.79–1.01) | x |
| Feeding type | ||
| Bottle | 0.63 (0.35–1.11) | x |
| Breast | 1.02 (0.57–1.81) | x |
| Both | Ref | x |
| NICU admission | 1.50 (0.94–2.38) | x |
| RDS | 2.91 (1.19–7.13) | x |
| Phototherapy | 1.83 (0.83–4.06) | x |
| Apnea (treated by ventilator or medication) | 2.64 (0.63–11.11) | x |
| Intubation or chest compression in delivery room* | 2.95 (0.69–12.51) | x |
| Oxygen requirement after delivery room | 2.48 (1.44–4.28) | 2.82 (1.33 (5.99) |
| Newborn sepsis suspected or proven | 1.07 (0.55–2.08) | 0.55 (0.24–1.29) |
| Hospital stay ≤ 90th percentile (5 days) | 1.49 (0.85–2.61) | x |
Reasons for readmissions
The most common diagnosis for both all visits/readmissions and hospital readmissions was respiratory illness, followed by fever/infection (Table 5). Other conditions such as vomiting, diarrhea, and fall/trauma, etc were less common. Hospital readmissions occurred slightly earlier (median day 36, 25th-75th percentiles: 14–55 days) as compared to all visits/readmissions (45.5, 23–75). Most infants were admitted just once, and only a few received more than two revisits/admissions (Table 5).
Table 5:
Reasons for revisits/readmissions (numbers of infants with diagnosis)
| All visits/readmissions | Hospital readmissions | |
|---|---|---|
| Diagnosis at first visit/ readmission | Vomiting: 21 | Vomiting: 4 |
| Diarrhea: 7 | Diarrhea: 1 | |
| Respiratory illness:95 | Respiratory illness: 20 | |
| Fever/infection: 40 | Fever/infection: 10 | |
| Fall/Trauma:5 | Fall/Trauma: 1 | |
| Other: 127 | Other 24 | |
| Age at first visit/readmission Days (Median; 25–75th centiles) | 45.5 (23–75) | 36 (14–55) |
| Diagnosis at second visit/readmission | Vomiting: 6 | Vomiting: |
| Diarrhea: 4 | Diarrhea: | |
| Respiratory illness: 22 | Respiratory illness: 6 | |
| Fever/infection: 12 | Fever/infection: 1 | |
| Fall/Trauma: 2 | Fall/Trauma: | |
| Other: 41 | Other 3 | |
| Age at second visit/readmission (Median; 25–75th centiles) | 57 (37–83) | 54 (47–76) |
| Diagnosis at third visit/readmission | Vomiting: 2 | Vomiting: |
| Diarrhea: 3 | Diarrhea: | |
| Respiratory illness: 9 | Respiratory illness: 2 | |
| Fever/infection: 3 | Fever/infection: 1 | |
| Fall/Trauma: 1 | Fall/Trauma: | |
| Other: 14 | Other 2 | |
| Age at third visit/readmission (Median; 25–75th centiles) | 78 (56–85) | 81.5 (74–88) |
| Diagnosis at fourth visit/readmission | Vomiting:1 | Vomiting: |
| Diarrhea: | Diarrhea: | |
| Respiratory illness: 1 | Respiratory illness: | |
| Fever/infection: 1 | Fever/infection: | |
| Fall/Trauma: | Fall/Trauma: | |
| Other: 8 | Other: 1 | |
| Age at Fourth visit/readmission (Median; 25–75th centiles) | 84 (77–99) | 83 (83–83) |
Discussion:
In this study of a well-characterized cohort of mothers and infants, a relatively large number of infants (15.9% or approximately 1 in 8) had unplanned clinic, ER visits, or hospital readmissions within the first three months of age, while a substantial proportion (3.8% or approximately 1 in 25) were readmitted to the hospital during the same time period. Multiple risk factors for unplanned clinic or ER visits and hospitalization were identified. Although many can be considered anticipated (e.g. antenatal steroids, apnea, SGA etc), others suggest potential impact on the neonatal microbiome (maternal postpartum antibiotics) or issues related to access/cost of care (Hispanic ethnicity associated with fewer revisits) that require further study.
Strengths of our study include the prospective and highly detailed data collection, and the multicenter nature of the randomized trial of which this study was a secondary analysis, which increases the generalizability of the results. Another strength is the follow-up to three months of age, as most previous studies have evaluated only early (<1 month) re-admissions. As can be seen in our results, the median day of both readmissions to hospital or all revisits was at more than a month of age. Our focus on infants delivered by cesarean section also avoids readmissions associated with early discharge, for these infants are usually discharged after 48 hours of age. A limitation is that this study was focused on the risk factors for revisits and readmissions, but not specifically upon the details of revisits or readmissions, other than broad diagnostic categories. More recently, with the current opioid crisis in the United States, it has been noted that infants with Neonatal Abstinence Syndrome (NAS) are at higher risk of readmissions.20 However, we do not have sufficient information to define the incidence of NAS in our cohort, and it is unlikely that readmissions beyond a month of age are attributable directly to NAS. It is important to note that overall, the c-statistic of the models (equivalent to the area under the curve of the receiver operating characteristic curve [AUC of ROC]) was only 0.60–0.62, indicating that the models have much room for improvement. As early discharges were not included due to the inclusion of only cesarean deliveries, some of the predictability was removed due to absence of early discharged infants at higher risk of poor feeding and jaundice. Also, it is possible that many revisits/readmissions cannot be predicted, because we lack sufficient resolution in data collection (e.g. many readmissions were due to respiratory illness, which may be associated with number of siblings, daycare attendance, or seasonal variation etc). It is also likely that illness in young children is stochastic in nature i.e., it is randomly determined and can be statistically analyzed as a probability but cannot be precisely predicted due to uncertainty.
Early readmissions may indicate an inadequate assessment of the newborn’s readiness for discharge, as more immature infants and infants with feeding problems, jaundice, or respiratory distress are at higher risk for readmission.18 Results from our analysis are consistent with such findings from the literature, as low birth weight and apnea (often indicators of prematurity) were associated with any revisits, and antenatal steroid administration and oxygen requirement after the delivery room (also indicators of prematurity) were associated with hospital readmissions. However, given that many readmissions were after a month of age, and were associated with respiratory illness or fever/infection, it is likely that these later readmissions and subsequent visits in our cohort were evidence of increased susceptibility of infants (especially preterm infants) to respiratory viruses such as respiratory syncytial virus (RSV; most infants did not qualify for RSV prophylaxis), adenovirus, rhinovirus, metapneumovirus, and other agents.21, 22, 23
Certain risk factors identified by our analysis are novel. Hispanic ethnicity was associated with a lower odds ratio of revisit, but not hospital readmission. Pediatric studies in the past found that more readmissions and ER visits were associated with Hispanic ethnicity,24, 25, 26, 27, 28, 29 but our results indicate the converse may be true for newborn infants. Simon et al.30 found that irrespective of insurance status, Latino children have lower rates of ER injury visits, perhaps due to different healthcare seeking behavior, and it is possible that similar differences in healthcare seeking behavior, cost, or access to care account for lower revisits but similar hospitalization rates in Hispanics. However, Lee et al.31 found that in the United States, ER visits in the neonatal period are highest among non-Hispanic blacks, with 14.4% of newborns having an ER visit in the neonatal period, compared to 6.7% for whites and 7.7% for Hispanics. It is possible that increasing immigration legislation and fear of deportation in recent years reduces ER visits of less sick infants but not hospitalization of sicker infants.32 Postpartum maternal antibiotics were associated with a higher odds ratio of neonatal revisits as well as readmissions. It is not clear if confounding factors (e.g. intrauterine infection or inflammation or both – triple I33 or clinical chorioamnionitis) were antecedent to both postpartum antibiotic use and neonatal signs of illness, or if maternal infection or antibiotic use affected neonates directly (e.g. by reducing breast feeding or by causing diarrhea, or by effects on the neonatal microbiome) thereby increasing the probability of revisit or readmission.34 In the C/SOAP trial, chorioamnionitis in the mother was an exclusion criterion for enrollment, which limited the number of infants with antenatal exposure to chorioamnionitis in this study. A prolonged hospital admission (>90th percentile or 5 days) was associated with a lower odds ratio, perhaps because the longer hospital stay eliminated the early readmissions.
In summary, in this secondary analysis of a multicenter randomized trial of azithromycin prophylaxis for non-elective cesarean section,19 we identified multiple risk factors for unplanned clinic or ER visits and hospitalization in newborn infants. Although many risk factors were associated with immaturity (e.g. antenatal steroids, apnea, SGA), others suggested potential impact on the neonatal microbiome (maternal postpartum antibiotics) or issues related to access/cost of care (Hispanic ethnicity associated with fewer revisits) that require additional investigation. Many revisits and hospitalizations occurred after a month of age, indicating that the duration of monitoring needs to be extended to at least three months to capture most revisits. Our data also indicate the rate of hospital readmissions is not an appropriate quality metric for newborn infants, as risk factors alone do not contribute to a good predictive model, and the reasons for most readmissions (respiratory illness and fever/infection) are not directly attributable to the initial hospitalization.
Funding:
NIH R01 HD064729
Footnotes
Conflict of interest: The authors have no financial relationships or conflicts of interest relevant to this article to disclose.
References:
- 1.Lorch SA. National Quality Measures in Perinatal Medicine. Clin Perinatol 2017, 44(3): 485–509. [DOI] [PubMed] [Google Scholar]
- 2.Toomey SL, Peltz A, Loren S, Tracy M, Williams K, Pengeroth L, et al. Potentially Preventable 30-Day Hospital Readmissions at a Children’s Hospital. Pediatrics 2016, 138(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jonas JA, Devon EP, Ronan JC, Ng SC, Owusu-McKenzie JY, Strausbaugh JT, et al. Determining preventability of pediatric readmissions using fault tree analysis. J Hosp Med 2016, 11(5): 329–335. [DOI] [PubMed] [Google Scholar]
- 4.Hain PD, Gay JC, Berutti TW, Whitney GM, Wang W, Saville BR. Preventability of early readmissions at a children’s hospital. Pediatrics 2013, 131(1): e171–181. [DOI] [PubMed] [Google Scholar]
- 5.Zhou H, Roberts PA, Dhaliwal SS, Della PR. Risk factors associated with paediatric unplanned hospital readmissions: a systematic review. BMJ Open 2019, 9(1): e020554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuzniewicz MW, Parker SJ, Schnake-Mahl A, Escobar GJ. Hospital readmissions and emergency department visits in moderate preterm, late preterm, and early term infants. Clin Perinatol 2013, 40(4): 753–775. [DOI] [PubMed] [Google Scholar]
- 7.Underwood MA, Danielsen B, Gilbert WM. Cost, causes and rates of rehospitalization of preterm infants. J Perinatol 2007, 27(10): 614–619. [DOI] [PubMed] [Google Scholar]
- 8.Dietz PM, Rizzo JH, England LJ, Callaghan WM, Vesco KK, Bruce FC, et al. Early term delivery and health care utilization in the first year of life. J Pediatr 2012, 161(2): 234–239 e231. [DOI] [PubMed] [Google Scholar]
- 9.Radmacher P, Massey C, Adamkin D. Hidden morbidity with “successful” early discharge. J Perinatol 2002, 22(1): 15–20. [DOI] [PubMed] [Google Scholar]
- 10.Tomashek KM, Shapiro-Mendoza CK, Weiss J, Kotelchuck M, Barfield W, Evans S, et al. Early discharge among late preterm and term newborns and risk of neonatal morbidity. Semin Perinatol 2006, 30(2): 61–68. [DOI] [PubMed] [Google Scholar]
- 11.Maisels MJ, Kring E. Length of stay, jaundice, and hospital readmission. Pediatrics 1998, 101(6): 995–998. [DOI] [PubMed] [Google Scholar]
- 12.Soskolne EI, Schumacher R, Fyock C, Young ML, Schork A. The effect of early discharge and other factors on readmission rates of newborns. Arch Pediatr Adolesc Med 1996, 150(4): 373–379. [DOI] [PubMed] [Google Scholar]
- 13.Metcalfe A, Mathai M, Liu S, Leon JA, Joseph KS. Proportion of neonatal readmission attributed to length of stay for childbirth: a population-based cohort study. BMJ Open 2016, 6(9): e012007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hensman AM, Erickson-Owens DA, Sullivan MC, Quilliam BJ. Determinants of Neonatal Readmission in Healthy Term Infants: Results from a Nested Case-Control Study. Am J Perinatol 2020. [DOI] [PubMed] [Google Scholar]
- 15.Roca A, Oluwalana C, Bojang A, Camara B, Kampmann B, Bailey R, et al. Oral azithromycin given during labour decreases bacterial carriage in the mothers and their offspring: a double-blind randomized trial. Clin Microbiol Infect 2016, 22(6): 565 e561–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan GJ, Stuart EA, Zaman M, Mahmud AA, Baqui AH, Black RE. The effect of intrapartum antibiotics on early-onset neonatal sepsis in Dhaka, Bangladesh: a propensity score matched analysis. BMC pediatrics 2014, 14: 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reed BD, Schibler KR, Deshmukh H, Ambalavanan N, Morrow AL. The Impact of Maternal Antibiotics on Neonatal Disease. J Pediatr 2018, 197: 97–103 e103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Young PC, Korgenski K, Buchi KF. Early readmission of newborns in a large health care system. Pediatrics 2013, 131(5): e1538–1544. [DOI] [PubMed] [Google Scholar]
- 19.Tita AT, Szychowski JM, Boggess K, Saade G, Longo S, Clark E, et al. Adjunctive Azithromycin Prophylaxis for Cesarean Delivery. N Engl J Med 2016, 375(13): 1231–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patrick SW, Burke JF, Biel TJ, Auger KA, Goyal NK, Cooper WO. Risk of Hospital Readmission Among Infants With Neonatal Abstinence Syndrome. Hosp Pediatr 2015, 5(10): 513–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turi KN, Wu P, Escobar GJ, Gebretsadik T, Ding T, Walsh EM, et al. Prevalence of infant bronchiolitis-coded healthcare encounters attributable to RSV. Health Sci Rep 2018, 1(12): e91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Toizumi M, Suzuki M, Nguyen HAT, Le MN, Ariyoshi K, Moriuchi H, et al. Viral Acute Respiratory Illnesses in Young Infants Increase the Risk of Respiratory Readmission. Pediatr Infect Dis J 2018, 37(12): 1217–1222. [DOI] [PubMed] [Google Scholar]
- 23.Cox DW, Khoo SK, Zhang G, Lindsay K, Keil AD, Knight G, et al. Rhinovirus is the most common virus and rhinovirus-C is the most common species in paediatric intensive care respiratory admissions. Eur Respir J 2018, 52(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodriguez VA, Goodman DM, Bayldon B, Budin L, Michelson KN, Garfield CF, et al. Pediatric Readmissions Within 3 Days of Discharge: Preventability, Contributing Factors, and Necessity. Hosp Pediatr 2019, 9(4): 241–248. [DOI] [PubMed] [Google Scholar]
- 25.Kogon BE, Oster ME, Wallace A, Chiswell K, Hill KD, Cox ML, et al. Readmission After Pediatric Cardiothoracic Surgery: An Analysis of The Society of Thoracic Surgeons Database. The Annals of thoracic surgery 2019, 107(6): 1816–1823. [DOI] [PubMed] [Google Scholar]
- 26.Zook HG, Payne NR, Puumala SE, Ziegler KM, Kharbanda AB. Racial/Ethnic Variation in Emergency Department Care for Children With Asthma. Pediatr Emerg Care 2019, 35(3): 209–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ju M, Luna N, Park KT. The Effect of Limited English Proficiency on Pediatric Hospital Readmissions. Hosp Pediatr 2017, 7(1): 1–8. [DOI] [PubMed] [Google Scholar]
- 28.Samuels-Kalow ME, Stack AM, Amico K, Porter SC. Parental Language and Return Visits to the Emergency Department After Discharge. Pediatr Emerg Care 2017, 33(6): 402–404. [DOI] [PubMed] [Google Scholar]
- 29.Alpern ER, Clark AE, Alessandrini EA, Gorelick MH, Kittick M, Stanley RM, et al. Recurrent and high-frequency use of the emergency department by pediatric patients. Acad Emerg Med 2014, 21(4): 365–373. [DOI] [PubMed] [Google Scholar]
- 30.Simon TD, Bublitz Emsermann C, Dickinson LM, Hambidge SJ. Lower rates of emergency department injury visits among Latino children in the USA: no association with health insurance. Inj Prev 2006, 12(4): 248–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee HC, Bardach NS, Maselli JH, Gonzales R. Emergency department visits in the neonatal period in the United States. Pediatr Emerg Care 2014, 30(5): 315–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beniflah JD, Little WK, Simon HK, Sturm J. Effects of immigration enforcement legislation on Hispanic pediatric patient visits to the pediatric emergency department. Clin Pediatr (Phila) 2013, 52(12): 1122–1126. [DOI] [PubMed] [Google Scholar]
- 33.Higgins RD, Saade G, Polin RA, Grobman WA, Buhimschi IA, Watterberg K, et al. Evaluation and Management of Women and Newborns With a Maternal Diagnosis of Chorioamnionitis: Summary of a Workshop. Obstet Gynecol 2016, 127(3): 426–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mathew JL. Effect of maternal antibiotics on breast feeding infants. Postgrad Med J 2004, 80(942): 196–200. [DOI] [PMC free article] [PubMed] [Google Scholar]


