Abstract
Younger siblings of children with autism spectrum disorders (HR-Sibs) are at elevated risk for social communication deficits and language delays. One way to mitigate this risk early, before these deficits and delays become clear or impairing, may be to equip parents to use the strategies taught through the Improving Parents as Communication Teachers (ImPACT) intervention. In this randomized control trial, 97 HR-Sibs (mean age 14 mos) and their primary caregiver were randomized to either ImPACT or a business-as-usual control group. Our a priori, preregistered hypothesis was that parents’ participation in ImPACT training would indirectly attenuate younger siblings’ social communication challenges 9 months later by sequentially increasing parents’ use of ImPACT strategies immediately after the intervention phase and by improving children’s midpoint proximal skills (e.g., motor imitation or intentional communication). Results supported this prediction.
Thirty-three percent of younger siblings of children with autism spectrum disorders (high risk, or HR-Sibs) are likely to meet criteria for a language delay or autism spectrum disorder (ASD) by 36 months. Fourteen percent of HR-Sibs eventually meet criteria for a language delay, but not ASD (Messinger et al., 2013). Another 19% meet criteria for ASD (Ozonoff et al., 2011), which involves challenges with social communication (American Psychiatric Association, 2013). While ASD diagnoses can be made as early as 14 to 18 months, for many children who ultimately meet criteria for ASD, the symptom presentation manifests more slowly such that diagnosis is not possible until much later (Ozonoff et al., 2015; Pierce et al., 2019, Zwaigenbaum, & Penner, 2018). These children miss the birth-to-three eligibility window for early intervention through the IDEA Part C service system.
One way to reduce the severity of social and communication challenges in HR-Sibs may be to provide a pre-emptive intervention. Parent-implemented interventions may serve this purpose because they are less expensive than providing equivalent hours of therapist-implemented intervention, and they are better able to infuse social and communicative skill development into a variety of daily routines and play contexts throughout the day. The two studies of parent-implemented interventions for HR-Sibs that have been conducted to date found positive effects with regard to: (a) parents’ non-directiveness and synchrony (Green et al., 2017); (b) child attentiveness/ communication initiations with parents (Green et al., 2017); (c) parent-reported infant adaptive functioning (Green et al., 2015); and (d) parent-reported receptive and expressive language (Whitehouse et al., 2019). Parents cannot be blinded to treatment assignment when they are the implementers of the treatment. Thus, it is important to test the efficacy of a parent-implemented treatment on outcomes that cannot be influenced by the bias that can occur through parental knowledge of treatment group assignment.
From a developmental psychopathology perspective, parent-implemented intervention during the first few years of life is likely to have a cascading effect on children’s later social communication outcomes by first improving their “pivotal skills” (e.g., Masten & Cicchetti, 2010; Rogers & Pennington, 1991). Pivotal skills are central building blocks that enable children to learn from or recruit input from their natural social environment (Koegel, Koegel, & Carter, 1998). When pivotal skills are elicited, modeled, and rewarded in a treatment, they are proximal outcomes (Yoder, Bottema-Beutel, Woynaroski, & Sandbank, 2013). Thus, we might expect that early intervention will indirectly affect later child outcomes by promoting the development of earlier proximal skills that are pivotal in facilitating broader outcomes, such as language delay or social communication difficulties associated with ASD. For younger siblings at familial risk for ASD, these proximal skills include: (a) intentional communication (Yoder, Watson, & Lambert, 2015); (b) expressive vocabulary level; (c) motor imitation (Rogers, 1999; Ingersoll & Schreibman, 2006); and (d) object play (Lieberman & Yoder, 2012). All four proximal skills are malleable with intervention (Yoder & Stone, 2006; McDuffie, Lieberman, & Yoder, 2014; Wainer & Ingersoll, 2013), have theoretical rationale for influencing future social communication, and empirically predict later communication ability in children with ASD (Yoder et al., 2015).
In order for parent-implemented interventions to impact children’s growth, coaches must first foster parents’ ability to independently use the intervention strategies they are taught. This cascading model of intervention delivery (e.g., Kaiser & Roberts, 2013) is an underemphasized precondition of parent-implemented intervention efficacy. Only one group has demonstrated that, for older children with ASD, parent-implemented interventions affect child outcomes through parents’ use of the taught strategies (Aldred et al., 2012; Pickles et al., 2016). To date, no study has assessed the longitudinal, cascading effects of a parent-implemented intervention for HR-Sibs by using an indirect, or mediational, model to examine whether intervention training first improves parent strategy use, which then improves child proximal skills, which ultimately improves child social communication outcomes.
A promising parent-implemented intervention is Improving Parents as Communication Teachers (ImPACT; Ingersoll & Dvortcsak, 2010). ImPACT is part of a class of a naturalistic, developmental, behavioral interventions (NDBIs; Schreibman et al., 2015), which employ behavioral strategies within a naturalistic, play-based setting to address developmentally-appropriate goals. ImPACT was selected for the present study because it: (a) seeks to enhance dyadic mutuality, which has been found to predict which HR-Sibs fail to receive an ASD diagnosis (Wan et al., 2012); (b) focuses on teaching the above-mentioned proximal skills; (c) uses guided practice in every session to teach parents skills; (d) uses child teaching techniques that are evidenced-based; (e) is liked by parents when they are the implementers (Wainer & Ingersoll, 2013); and (f) has preliminary data to support its efficacy in children with ASD (Ingersoll & Wainer, 2013). A recent quasi-experiment testing the effect of parent-implemented ImPACT conducted with young children at risk for ASD found positive effects on measures from parent-child interactions (Stahmer et al., 2020). No internally-valid test of the efficacy of ImPACT on generalized skills in HR-Sibs has been conducted.
Research Aims
This study was designed to test the hypothesis that parents’ participation in ImPACT training will have cascading, indirect effects on HR-Sib’s social communication outcomes. We used serial mediation modeling to test the hypotheses that ImPACT training would: (a) increase parents’ generalized use of ImPACT strategies directly after intervention, (b) indirectly improve HR-Sibs’ proximal skills (intentional communication, expressive vocabulary level, motor imitation, and object play) by 3 months post-intervention, and (c) indirectly improve HR-Sibs’ social communication and expressive language outcomes by 6 months post-intervention. We also address limitations in the previous literature by (a) assessing children’s generalized skills by measuring behavior during their interactions with blinded examiners, rather than their interactions with parents (who also may serve as their interventionists at home); and (b) measuring behavioral outcomes using blinded coders rather than only through parent report or interactions with parents, to avoid potential bias.
Method
Participants
Ninety-seven children and their primary parent at two sites (Nashville n = 49, Seattle n = 48) participated in this study. Inclusion criteria were: (a) younger sibling age between 12–18 months at study entry; (b) at least one full sibling with diagnosed ASD in the home; and (c) English as the primary home language. Tables 1 and 2 provide descriptive statistics for the participants. None of the descriptor variables differed significantly between intervention groups, p values: range = .12 - .95, mean = .70, SD = .24. All participants were consented and the study was approved by the relevant institutional review boards.
Table 1.
Preintervention Participant Characteristics by Intervention Group for Continuous Variables
| Variable | ImPACT (n = 49) M(SD) | Control (n = 48) M(SD) | Between-group effect sizea |
|---|---|---|---|
| Age in months | 14(2) | 14(2) | 0.00 |
| Mental age in monthsb | 12(3) | 13(3) | −0.33 |
| Expressive age in monthsb | 11(4) | 12(4) | −0.25 |
| Receptive age in monthsb | 11(3) | 11(3) | 0.00 |
| Cognitive standard score (M=100, SD = 15)b | 88(16) | 91(15) | −.19 |
| Expressive T score (M=50, SD = 10)b | 41(12) | 41(12) | 0.00 |
| Receptive T score (M=50, SD = 10)b | 37(11) | 37(10) | 0.00 |
Cohen’s d.
Mullen Scales of Early Learning (Mullen, 1995). M = mean, SD = standard deviation. All between-group contrasts are nonsignificant.
Table 2.
Preintervention Participant Characteristics by Group for Categorical Variables
| ImPACT | Control | |||
|---|---|---|---|---|
| Variable | Levels | Percentage of group | Percentage of group | Between-group effect sizea |
| Sex | Male | 55% | 58% | 0.07 |
| Race | African American | 2% | 7% | |
| Asian | 8% | 8% | ||
| White | 79% | 76% | ||
| Mixed | 10% | 11% | 0.07 | |
| Formal education of primary parent | ||||
| 12 years or GED | 6% | 9% | ||
| 1 – 2 years of college or technical school | 16% | 13% | ||
| 3-4 years of college or technical school | 39% | 49% | ||
| 1 -2 years of graduate or professional school | 16% | 13% | ||
| 3 or more years of graduate or professional school | 22% | 17% | 0.07 | |
| Number of children with ASD in home Primary parent | 1 | 92% | 94% | 0.07 |
| Mother | 88% | 92% | ||
| Father | 10% | 8% | ||
| Other | 2% | 0.08 | ||
Effect size is Cramer’s V (sqrt(chi square/(n*df)). All between-group contrasts were nonsignificant.
Figure 1 indicates the number and dropout classification (i.e., no-shows vs discontinuers) for participants at each stage of the study using the CONSORT conventions. According to the Deke and Chiang’s (2017) guidelines and the measurement period at which attrition was at its maximum (Time 3), we judged that the overall (8%) and differential attrition (4%) were unlikely to cause bias. Sixty-five percent of eligible families chose to participate, 95% CI [57%, 73%]. As a benchmark for judging this level of self-selection, a meta-analysis of preventative parent-implemented interventions found a mean of 52%, SD = 26% (Finan, Swierzbiolek, Priest, Warren, & Yap, 2018).
Figure 1.
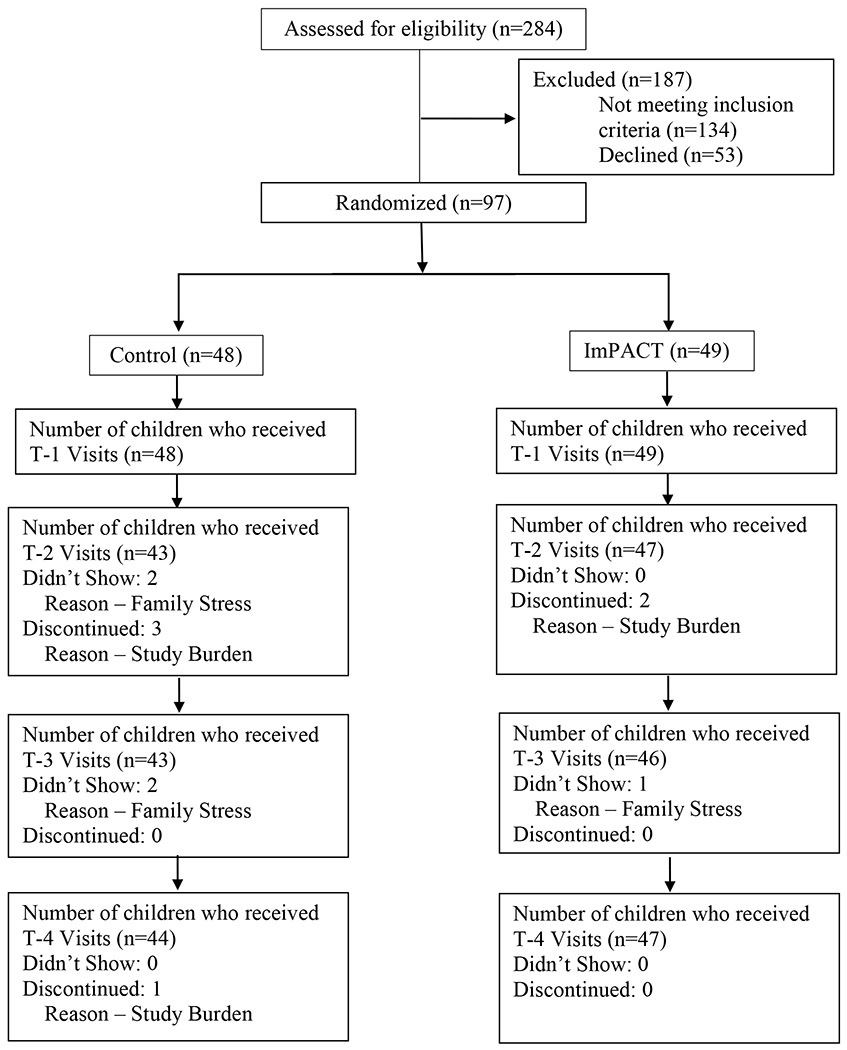
Flow diagram of the progress through the measurement periods of this 2-group randomized trial.
Research Design
This study used a randomized between-group experiment. Parent-child pairs were randomly assigned (with computerized balancing) to either ImPACT (n = 49) or control (n = 48) groups. Study assessors and coders of observational procedures were blind to intervention group assignment. Intent-to-treat analysis procedures were used (i.e., including all participants in primary analyses, regardless of attendance at intervention and assessment sessions). Full information maximum likelihood estimation was used to address missing values. This study was registered at www.clinicaltrials.gov with clinical trials registration number 140924. Hypotheses dealing with mediation are addressed in this report, while hypotheses dealing with moderation are addressed in a separate report. We combined two hypotheses initially stated as separate simple mediation models to one hypothesis stated and tested as a serially mediated model to improve parsimony and reduce the number of significance tests.
The variables in the mediated models were measured at different periods to meet the assumption of temporal precedence. The four measurement periods were: pre-intervention (Time 1); immediately after the 3-month intervention phase ended (Time 2); 6 months after study entry (Time 3); and 9 months after study entry (Time 4). Use of ImPACT strategies was measured immediately after the intervention phase ended, because parents were expected to show their strongest level of implementation at that period. In addition to Time 1, proximal skills were measured 3 months after the intervention phase ended to provide sufficient time for parents’ use of ImPACT strategies to have an effect on these skills. In addition to Time 1, social communication abilities were measured 3 months after putative proximal skills to provide sufficient time for putative proximal skills to have an effect on these outcomes.
Intervention Groups
ImPACT.
This instantiation of the ImPACT intervention involved staff offering parents 24 in-home teaching sessions over the course of 12 weeks. The ImPACT intervention is described in detail in the first edition of the comprehensive manual (Ingersoll & Dvortcsak, 2010). Examples of the ImPACT curriculum include: (a) arranging materials and furniture to encourage productive child engagement; (b) following the child’s lead; (c) using positive affect and animation; (d) modeling and expanding language and communication; (e) using communicative temptations; (f) directly teaching expressive communication, receptive language, motor imitation, and object play; and (g) integrating interactive and direct teaching methods. In general, the curriculum focuses on setting up joint-action routines around objects that enable modeling and direct teaching of play, communication, and language skills that are just beyond the child’s current production level. Child imitation of adult models is encouraged as a part of teaching all skills. Parents were asked to provide at least 1 hour of therapy per day, which could be dispersed across the day, 5 days/week for the duration of the study.
The staff providing the parent teaching were a speech-language pathologist (SLP) who had been trained and certified by the originators of the ImPACT intervention at the primary site. The SLP trained and monitored a staff member at the second site, using the methods she experienced when she was trained by the originators of ImPACT. After meeting criteria for implementation fidelity, the trained staff member implemented ImPACT with participants at the sister site. Using self-administered, session-specific checklists on at least 2 sessions per parent-child pair, staff adherence to the ImPACT protocol for teaching parents was estimated to average 91% (SD = 3%). Eighty-six percent of parents assigned to the ImPACT group completed the program content.
Control.
Like the ImPACT families, families assigned to the control group were free to pursue intervention outside of the research study. As indicated by parent report administered at all measurement periods, parents reported their children received an average of one half-hour of non-project therapy per month, which was not significantly different between groups, ImPACT M(SD) = 0.6(1.6); Control M(SD) = 0.5(1.4), p > .05.
Procedures
The administration manuals and fidelity of implementation instruments are available from the first author. In all examiner-child sessions, the interaction style, location, examiner, and materials differed from those used in the intervention sessions. Examiners were blind to group status. In the parent-child sessions, the materials and location differed from intervention sessions. Parents were not explicitly told to use ImPACT strategies during parent-child assessment sessions to ensure that instructions would be consistent between groups and to test whether parents assigned to the ImPACT group would spontaneously generalize the use of ImPACT strategies when their coaches were absent.
Parent implementation of ImPACT strategies procedures.
To measure parents’ use of ImPACT strategies in both groups at Times 1 and 2, the parent-child free play (PCFP) and parent-child snack (PCS) were administered. The PCFP is a 15-minute unstructured activity for which the parent was instructed to, “Play as you would at home if you had no interruptions and had time to play with your child” (Yoder et al., 2015). A standard set of developmentally appropriate toys was made available. The PCS is a 10-minute unstructured session, for which the parent was told, “We want to see how your child communicates during snack times when you are interacting with him or her to elicit communication” (Yoder et al., 2015). Parents were given a standard set of materials, and child-preferred snacks and drinks were available.
Motor imitation procedures.
To measure motor imitation at Times 1 and 3, the Semi-Structured Imitation Scale (SSIS) and Adapted Legerstee Imitation Task (ALIT) were administered. The SSIS is an examiner-child session consisting of 10 modeled actions with no accompanying verbal instructions. It is a shortened version of a procedure designed for use with toddlers and preschoolers with ASD to measure spontaneous motor imitation in a playful context (Ingersoll & Meyer, 2011), as this type of motor imitation correlates most strongly with social reciprocity in children with ASD (McDuffie et al., 2007). The ALIT is a structured task adapted from work with 10-month-olds (Legerstee & Markova, 2008) and involves 4 items. The examiner models putting an object in or taking an object out of a container, giving the object or container to the child, and waiting for child to imitate without verbal instructions. The simple actions, structured format, and prior use with infants supported the use of this procedure to prevent a floor effect for motor imitation measurement.
Intentional communication procedures.
To measure intentional communication at Times 1 and 3, the Communication and Symbolic Behavior Scales-behavior sample (CSBS) and Brief Observation of Social Communication Change (BOSCC) were administered. The CSBS (Wetherby & Prizant, 2003) is a structured, interactive measure of communication, early language, and play for children with communication ages between 6–24 months; the 15-minute behavior sample portion was used. The BOSCC (also 15 minutes) was developed to measure change in communication over time in minimally verbal children with ASD (Grzadinski et al., 2016) and includes a standard set of materials and procedures administered by an examiner.
Object play procedures.
To measure object play at times 1 and 3, the CSBS (above) and the Developmental Play Assessment (DPA) were administered. The DPA is a prompt-free, play-based interaction using a standardized set of toys that was designed to measure exploratory to multi-schema symbolic play in children with ASD from 6–36 months (Lifter, 1988).
Expressive vocabulary level procedures.
To measure expressive vocabulary level at Times 1 and 3, the CSBS (above), BOSCC (above), andMacArthur-Bates Communicative Development Inventory (MCDI; Fenson et al., 2006) were administered. The raw score from the MCDI expressive vocabulary checklist was used. The infant version of the MCDI was used for Time 1, and the toddler version was used for Time 3.
Expressive language ability procedures.
To derive a continuous measure of expressive language ability at Times 1 and 4, the percentile ranking from the expressive vocabulary checklist on the MCDI (above), and the Mullen Scales of Early Learning (MSEL; Mullen, 1995) were administered. The MSEL is a commonly used cognitive assessment for children between birth and 68 months. It was administered by licensed psychologists or trained research staff under the psychologists’ supervision. At Time 1, the age equivalencies and T scores for all MSEL subscales except the gross motor scale were used to describe children’s mental ages and cognitive delays.
Social communication procedures.
To measure social communication at Times 1 and 4, the CSBS (above) was used at both periods and the Autism Diagnostic Observation Scale, version 2; (ADOS-2) was used at Time 4. The ADOS-2 (Lord et al., 2015) is a semi-structured measure designed to inform the diagnosis of ASD. Research-reliable licensed psychologists and supervised staff administered the ADOS-2. In the current study, either the Toddler Module or Module 1 was administered to all but one participant, who received Module 2. The social affect calibrated severity score was used to provide an interpretable index of symptom severity that is comparable across modules (Hus, Gotham, & Lord, 2014; Esler et al., 2015). For the preparatory and primary analyses, the calibrated severity score was reverse scored so that higher scores would convey more adaptive functioning.
ASD diagnosis.
The diagnosis of ASD at Time 4 was determined by a licensed clinical psychologist on the basis of information obtained from the ADOS-2, a parent interview based on the ASD criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013), and other clinical assessments (e.g., Mullen Scales) as available. This variable was used as a dependent variable in an exploratory analysis.
Coding, Coded Variables, and Their Interobserver Reliability
Overview.
All coding manuals are available from the first author. Session-level, point-by point agreement checks were conducted on at least 20% of randomly selected sessions throughout the study to reduce observer drift. Primary coders did not know which sessions would be double coded. Interobserver reliability was estimated using intraclass correlation coefficients (ICCs) using a method in which errors on unitizing and classifying are reflected in the same reliability estimate. Reliability estimates for all variables at all time points were greater than our accepted threshold of ICC > .69, with the exception of communicative temptations at Time 1, which was .60. Thus, communicative temptations was not used to measure parents’ use of ImPACT strategies at Time 1.
Parents’ use of ImPACT strategies.
Three approaches were used by trained observers to quantify parents’ use of ImPACT strategies at Times 1 and 2. First, observers used Procoder for Digital Video (ProcoderDV; Tapp, 2003) to implement a 5-second partial interval behavior sampling of parents’ use of modeling language (i.e., verbally mapping the child’s focus of attention) during the PCFP and PCS. Second, observers used ProcoderDV to implement timed-event sampling of the number of instances the parent used direct teaching techniques to elicit child communication (i.e., expressive communication teaching) from the PCS. Expressive communication teaching is a collapsed category comprising elicited production prompts, complying with child communication, and expanding child communication. Third, observers used a 5-point, likert-like rating scale adapted from Frost’s Naturalistic Developmental Behavioral Intervention code to rate behaviors from the PCFP (Frost, 2018). Some aspects of the original rating system were not used because those behaviors were not well elicited by the PCFP or PCS (e.g., direct teaching of motor imitation). The adapted Frost rating scale was used to measure aspects of the ImPACT strategies that required qualitative judgements: (a) face-to-face positioning; (b) following the child’s lead; (c) positive affect and animation; (d) response to child communication attempts; and (e) use of communication temptations.
Intentional communication and expressive vocabulary level.
Two variables were derived from the CSBS and BOSCC procedures to measure intentional communication and expressive vocabulary levels. Each communication act was classified as non-symbolic (i.e., imitated words or phrases, non-word vocalizations, and gestures; for a weight of 1 point), single non-imitated word utterances (2 points), or multiple non-imitated word utterances (3 points). The weighted sum of instances of intentional communication was the metric used to quantify maturity of the form and frequency of communication, which we referred to as weighted frequency of intentional communication. Our past research with HR-sibs has shown that weighted intentional communication is a more construct valid measure (i.e., more predictive of later social impairment) than unweighted intentional communication (Yoder, Stone, Walden, & Malesa, 2009). The original CSBS coding system does not make the needed distinctions nor weight scores in the manner suggested by our past research. We used the same scoring for the BOSCC as the CSBS because we wanted to measure weighted intentional communication from different procedures for our composite intentional communication variable. Additionally, we were unable to attain sufficient reliability with the rating system recommended by the BOSCC originator. Using our own coding increased the reliability of the resulting scores. When a communication act was judged to include a non-imitated word approximation, the word was orthographically transcribed. Systematic Analysis of Language Transcripts (SALT; Miller & Chapman, 1985) software was used to count unique word roots (e.g., “ball” and “balls” are considered the same word root). We derived the number of different words from the BOSCC and CSBS because we wanted to measure expressive vocabulary from these procedures. Neither the CSBS nor the BOSCC coding recommended by the originators of those procedures derives this variable.
Motor imitation.
Motor imitation was coded at Times 1 and 3. For the SSIS and ALIT, coders rated the presence and extent to which the child accurately imitated the adult’s action on a 0–2 scale. The total raw score was the metric used for each motor imitation variable.
Object play.
Object play was coded at Times 1 and 3. Using the event behavior sampling method, observers coded play behaviors from the CSBS using the instructions in the CSBS manual for the play subscale (Wetherby & Prizant, 2003). On the DPA, timed event sampling was used to code the number of different toys touched and the number of unique differentiated play actions.
Social communication.
The social communication behaviors coded were those that tend to be most difficult for children with ASD (Wetherby et al., 2004). Trained observers identified the instances of four non-mutually-exclusive categories using a timed event sampling method from the CSBS at Times 1 and 4: (a) coordinated cues (the combined use of at least 3 of the following behaviors: smiles, word/vocalization, gesture, and eye gaze within 3 seconds); (b) positive affect sharing (i.e., smile with a gaze); (c) showing or pointing; and (d) sharing interest (use of gesture or vocalization for apparent declarative pragmatic function).
Results
Preparatory Analyses
Data reduction.
To improve validity and reduce the number of significance tests (Yoder, Symons, & Lloyd, 2018), equally weighted composite variables were computed by averaging z-converted scores when component variables posited to measure the same construct at the same period were sufficiently associated with each other (i.e., correlation or factor loading of > .39). If the results of factor analyses indicated that two composite variables were needed to quantify a construct and the two composite variables correlated > .39, we computed a 2nd-order composite. If component variables posited to measure the same construct were not sufficiently associated, a single component variable was selected to measure this construct based on relative convergent construct validity evidence or internal validity issues. With regard to internal validity issues, if preparatory analyses indicated the need to statistically control one Time 1 measure of a construct but not another measure of the same construct, the component variable needing statistical control was selected in tests of research aims. For example, the motor imitation estimate from the SSIS was selected over that of the ALIT because motor imitation at Time 1 differed between groups only for the SSIS (see next section for details). Using these criteria, the variables selected for the analyses that follow are indicated in Table 3.
Table 3.
Constructs, Procedures, Measurement Periods, and Variables
| Constructs | Procedures | Measurement Periods | Variables |
|---|---|---|---|
| Parent’s use of ImPACT strategies | PCFP, PCS | 1 | 2nd order composite of two 1st order composites: (a) positive affect and animation rating, modeling language count, and expressive language teaching count; and (b) face-to-face rating, following the child’s lead rating, and response to child rating |
| Parent’s use of ImPACT strategies | PCFP, PCS | 2 | 2nd order composite of two 1st order composites: (a) response to child rating, use of communication temptation rating, modeling language count, and expressive language teaching count; and (b) face-to-face rating, following the child’s lead rating, and positive affect and animation rating |
| Intentional communication | CSBS, BOSCC | 1, 3 | Composite of weighted frequency of intentional communication across procedures |
| Expressive vocabulary level | CSBS, BOSCC, MCDI | 1, 3 | Composite of number of different words said across procedures |
| Motor imitation | SSIS | 1, 3 | Total raw score |
| Object Play | CSBS, DPA | 1 | Composite of CSBS play raw score, DPA number of different toys, and DPA number of unique differentiated play actions |
| Object Play | DPA | 3 | Composite of number of different toys and number of unique differentiated play actions |
| Expressive language ability | MCDI, MSEL expressive | 1, 4 | Composite of percentile rankings across procedures |
| Social communication | CSBS | 1 | 2nd order composite of two 1st order composites: (a) sharing interests, show, and point counts; and (b) coordinating cues and positive affect sharing counts |
| Social communication | CSBS ADOS-2 | 4 | 2nd order composite of two 1st order composites: (a) sharing interests, show, and point counts, the reflected social affect calibrated severity score; and (b) coordinating cues and positive affect sharing counts |
PCFP = Parent-child free play and PCS = Parent-child snack (Yoder, Watson, & Lambert, 2015); CSBS = Communication and Symbolic Behavior Scale (Wetherby & Prizant 2003), BOSCC = Brief Observation of Social Communication Change (Grzadzinski et al., 2016); MCDI = MacArthur-Bates Communicative Development Inventory (Fenson, et al., 2006); SSIS = Semi-structured imitation scale (Ingersoll and Meyer 2011); DPA = Developmental Play Assessment (Lifter 1988); MSEL = Mullen Scales of Early Learning (Mullen, 1995); and ADOS-2 = Autism Diagnostic Observation Scale- Version 2 (Lord, Rutter, DiLavore, Risi, Gotham, Bishop, & Schedule, 2015).
Testing the need for and assumptions of pretest covariates.
The only Time 1 measure of a dependent variable that differed significantly between groups was motor imitation from the SSIS, t(92) = 3.7, p < .001, favoring the control group. Additionally, motor imitation at Time 1 significantly and positively predicted all four proximal skills at Time 3 and the two communication challenge variables at Time 4. Finally, the data fit the assumption of homogeneity of slopes for models predicting all putative proximal skills at Time 3 and both communication challenges outcomes at Time 4. All other pretests were nonsignificantly different between groups, p values: range .06 - .70, M = .40, SD = .21, Cohen’s d range = −.21 to .39. Thus, motor imitation at Time 1 was partialed out of the proximal skills at Time 3 and communication ability at Time 4.
Intervention effects did not vary by site.
No significant effects occurred for site x intervention predicting: (a) parents’ use of ImPACT strategies at Time 2; (b) putative proximal skills at Time 3; or (c) communication ability at Time 4. The p values range from .36 - .80, M = .60, SD = .13.
Primary Analyses
ImPACT teaching’s total effects.
The total effects of ImPACT (i.e., not considering mediators) were tested controlling for Time 1 measures of the dependent variables to increase the precision of effect size estimates. Table 4 provides the adjusted means, SDs, and between-group effect sizes for the ImPACT intervention’s total effects. The only significant total effect of ImPACT teaching was a very large effect on parents’ use of ImPACT strategies, Wald χ2(1) = 37, p < .001, favoring the ImPACT group.
Table 4.
Adjusteda Means, SDs, and Between-group Effect Sizes for ImPACT’s Total Effects
| ImPACT | Control | ||||
|---|---|---|---|---|---|
| Adjusted | Adjusted | Cohen’s | |||
| M | SD | M | SD | d | |
| Parents’ use of ImPACT strategies at Time 2 | .28 | .61 | −.33 | .51 | 1.09*** |
| Children’s object play at Time 3 | −.03 | .77 | .03 | .82 | −.07 |
| Children’s expressive vocabulary at Time 3 | .18 | 1.0 | −.19 | .58 | .45 |
| Children’s intentional communication at Time 3 | .05 | 3.4 | −.06 | 3.1 | .38 |
| Children’s motor imitation at Time 3 | 6.2 | 3.7 | 6.1 | 3.2 | .03 |
| Children’s expressive language ability at Time 4 | .09 | 1.0 | −.1 | .72 | .22 |
| Children’s social communication at Time 4 | −.03 | .77 | .03 | .63 | −.08 |
Means are adjusted for their Time 1 measures (and for motor imitation at Time 1 if correlated).
p < .001.
ImPACT teaching’s indirect effects on children’s communication challenges.
MPlus (Muthen & Muthen, 2019) was selected to test indirect effects because it allows FIML estimation and bias-corrected bootstrapping to estimate confidence intervals around indirect effect coefficients (Enders, 2010; Hayes, 2017). Table 5 provides the significant serially-mediated effects. ImPACT’s effect on children’s expressive ability at Time 4 and children’s social communication at Time 4 were both serially mediated by parents’ use of ImPACT strategies at Time 2 and then through HR-Sibs’ motor imitation at Time 3 (see Figure 2 for an example illustration). Finally, ImPACT’s effect on social communication at Time 4 was serially-mediated through parents’ use of ImPACT strategies and then through HR-Sibs’s intentional communication at Time 3. All other serially-mediated effects involving other putative proximal skills were nonsignificant (i.e., the confidence intervals around the indirect effect coefficients were inclusive of zero).
Table 5.
ImPACT’s Effects on Children’s Communication Abilities Occurs Through Parents’ Use of ImPACT Strategies and Children’s Proximal Skills
| M1 | M2a | Outcome a | Unstandardized coefficient [95% CI] |
|---|---|---|---|
| Parents’ use of ImPACT strategies at Time 2 | Motor Imitation at Time 3 | Expressive language ability at Time 4 | .05 [.01, .16] |
| Parents’ use of ImPACT strategies at Time 2 | Motor Imitation at Time 3 | Social communication at Time 4 | .06 [.01, .17] |
| Parents’ use of ImPACT strategies at Time 2 | Intentional communication at Time 3 | Social communication at Time 4 | .06 [.01,.18] |
M1 = first mediator; M2 = second mediator;
Controlling for Time 1 motor imitation.
Figure 2.
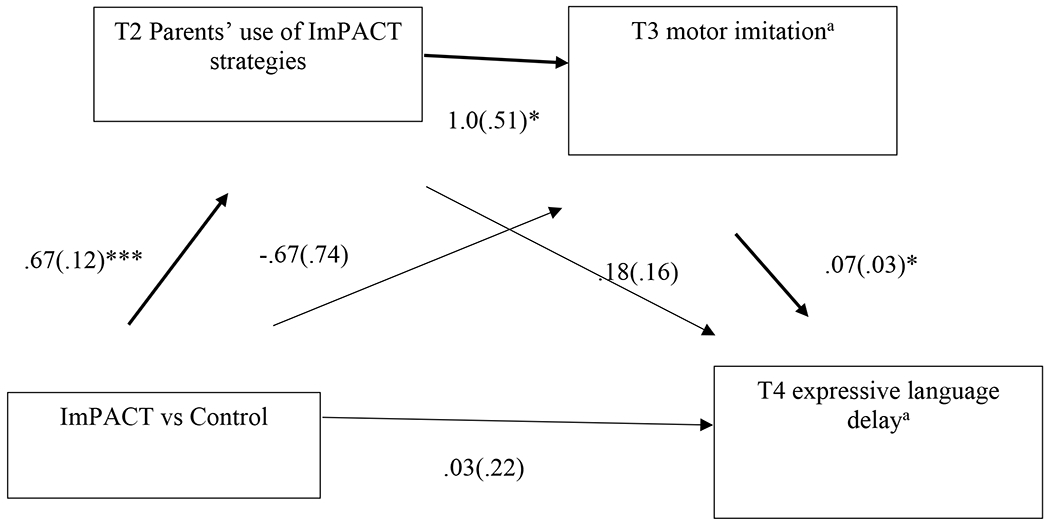
Path diagram of the ImPACT teaching’s indirect effect on expressive language ability at Time 4 through parents’ use of ImPACT strategies at Time 2 and HR-Sibs’ motor imitation at Time 3. Unstandardized coefficients (and their standard errors) are shown; *, *** = p < .05, and .001, respectively. aResiduals after controlling for motor imitation at Time 1.
Post-hoc Analyses for Clinical Significance
Given the significant indirect effect of ImPACT on continuously measured communication abilities, we next assessed the clinical importance of these indirect effects for language delay and ASD diagnosis through parents’ use of ImPACT strategies (i.e., ImPACT teaching). “Expressive language delay” was operationalized as a score at or below the 10th percentile ranking on the MSEL expressive language scale. ImPACT teaching had a statistically significant simple indirect effect on Time 4 expressive language delay subgroup membership through parents’ use of ImPACT strategies at Time 2, indirect effect’s unstandardized coefficient = −.13, 95% CI [−.26, −.003] (see Figure 3). ImPACT teaching also had a significant indirect effect through parents’ use of ImPACT strategies at Time 2 on Time 4 ASD diagnostic status, indirect coefficient = −.10, SE = .06, 95% CI [−.21, −.01].
Figure 3.
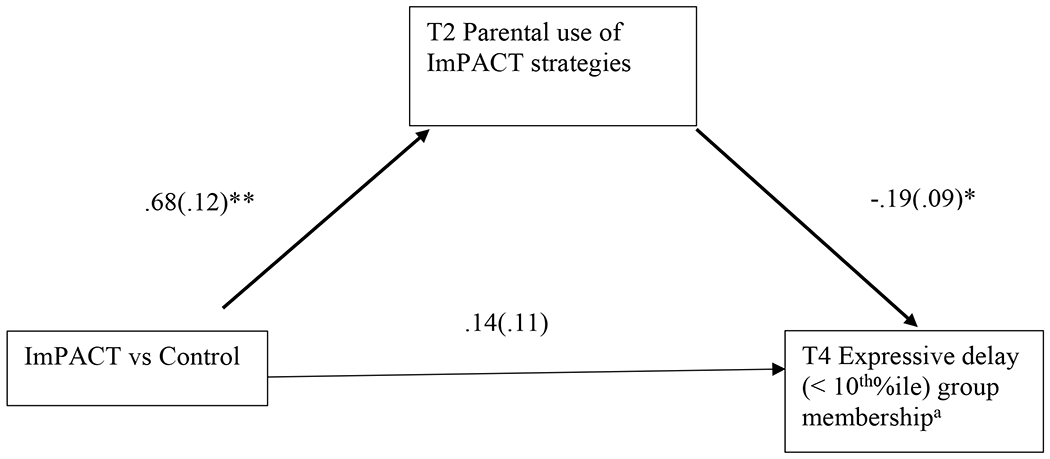
Path diagram of the ImPACT intervention’s indirect effect on expressive language delay group membership at Time 4 through parents’ use of ImPACT strategies at Time 2. Unstandardized coefficients (and their standard errors) are shown; *, ** = p < .05, .01, respectively. aResidual after controlling for motor imitation at Time 1
Discussion
Summary of the Research Findings
The current study examined ImPACT’s intervention effects on children’s early communication abilities. Our pregistered, a priori hypotheses were partially confirmed. Parents’ participation in ImPACT had: (a) a large total effect on parents’ use of ImPACT strategies; and (b) an indirect effect on continuous measures of HR-Sibs’ communication challenges through parents’ use of ImPACT strategies and on HR-Sibs’ subsequent motor imitation or HR-Sibs’ subsequent intentional communication. Although total effects of participating in ImPACT training were nonsignificant on child outcomes, indirect effects are interpretable without significant total effect (Hayes, 2013). In addition, we found that the ImPACT intervention had an indirect effect on HR-Sibs’ categorical expressive delay group membership and diagnostic status through parents’ use of ImPACT strategies. The latter analyses were exploratory because it is very difficult to detect effects of relatively short-term, low-intensity interventions on categorical outcomes due to the loss of information that occurs when continuous variables are dichotomized. However, the indirect effects on the categorical outcomes provide evidence that parents’ use of ImPACT strategies leads to clinically important language and diagnostic outcomes.
Importantly, this study examined parents’ generalized use of ImPACT strategies (i.e., use of the ImPACT strategies outside of the coaching contexts in which they were taught), which may explain in part why we found indirect effects on children’s later social communication. That is, ImPACT training appeared to be beneficial for children’s later social communication for those children whose parents demonstrated relatively frequent use of the strategies beyond the original treatment context. While this explanation might seem obvious, we could find no other studies of parent-implemented interventions in the HR-Sibs literature that had the required research design elements and statistical evidence to demonstrate this type of effect. Mediation models using a design that provides the temporal precedence of causal variables prior to affected variables collected in the context of RCT designs provide the evidence needed to test whether parents’ use of taught strategies is partly responsible for intervention effects on children.
The next question is why parents’ use of ImPACT strategies would specifically aid motor imitation and intentional communication. ImPACT strategies are designed to help parents interact with their children in sustained turn-taking interactions around objects. Such repetitive turn-taking interactions are thought to reduce the information processing load of interactions, which may in turn make it easier for HR-Sibs to participate in exchanges using cutting edge skills, such as imitating adult models or intentionally communicating. As children become more fluent with using new motor imitation and communication skills in highly familiar interactions, parents are taught to introduce novelty into their turn-taking interactions. By practicing these new skills in a number of interactive contexts, some of which are less routinized than others, children may develop a broader understanding of the contexts in which their new skills are functional, which may lead to generalization to activities not used in treatment and to examiners with whom the children are less familiar. Generalized motor imitation is a learning strategy that children may use to learn many new skills (Ingersoll and Schreibman 2006). Preverbal intentional communication enables children to actively convey messages to others, which will later will be conveyed by words, and elicits responses from parents and others that teach children new words for the meanings they convey (Yoder et al., 2015).
Most previous efficacy studies on ImPACT have used less rigorous research designs (e.g., multiple-baseline across participants, non-randomized group comparisons). That said, these past studies have: (a) demonstrated that parents of children with ASD learned to use the ImPACT methods (Wainer & Ingersoll, 2013); (b) demonstrated that ImPACT use is associated with prompted and spontaneous language use and joint engagement episodes with interventionists (Ingersoll, 2012; Ingersoll & Wainer, 2013; Stahmer et al., 2020); and (c) provided preliminary evidence that greater gains in child communication skills occurred for children with ASD in an ImPACT group than in a nonrandomized control group (Stadnick, Stahmer, and Brookman-Frazee, 2015; Stahmer et al., 2020).
The current study used a more internally-valid research design to replicate past study findings that ImPACT teaching had a total effect on parents’ use of ImPACT strategies in parents of children with ASD. By increasing parents’ generalized use of ImPACT strategy use, parents’ participation in teaching had an indirect effect on HR-Sibs’ generalized (a) motor imitation, (b) intentional communication, (c) expressive language ability (continuously and categorically measured), (d) continuously measured social communication abilities, and (e) ASD diagnosis.
Limitations
The most important limitation of the current study is that we could not measure actual frequency or duration of bouts of ImPACT parent’s use of ImPACT strategies throughout the intervention period. In our opinion, the field has not yet determined how to measure parents’ use of intervention strategies when research staff are absent. With NDBIs such as ImPACT, intervention use is ideally embedded in routines and short interactions throughout the day, making representative sampling of intervention use difficult. Methodology to capture day-long intervention use raises privacy concerns as well as concerns about parent reactivity (e.g., having staff visit to record interactions) and bias (e.g., self-reports of use). The lack of such measures limits our understanding of the daily or cumulative intervention intensity necessary for positive child outcomes. In addition, our sample lacked diversity. Most of our participants were Non-Hispanic White and well educated. Although many HR-Sibs studies suffer from the same issues, the racial and educational homogeneity restricts external validity.
While our study found a total effect of ImPACT intervention on parent strategy use, we found no total effects on proximal or distal child outcomes. This is may be because an insufficient proportion of parents generalized their use of ImPACT strategies to enable detection of a total effect on child outcomes. However, when parents’ generalized use of ImPACT strategies was included in the model, we found that ImPACT does affect child outcomes, albeit indirectly. Additionally, ImPACT intervention may be more effective for some parent-child dyads than others. In other words, in a heterogeneous population such as HR-Sibs, there are likely characteristics that moderate intervention efficacy. This question is addressed in a separate report. Finally, total effects of ImPACT may be detectable when parents use the strategies for longer than 6 months. Future study is required to test this hypothesis.
Although composites were used to reduce the number of significance tests, no familywise alpha adjustment was made for the multiple mediation models fitted to answer this study’s research questions. This study assessed significance of each model using M Plus, which does not provide the exact p value for each test of indirect effects, thus preventing alpha adjustment methods. However, each model fitted addressed an a priori prediction, which, when confirmed, reduces the likelihood that our results are sample-specific.
Strengths
This study has several strengths that increase its internal and external validity. In addition to the research design strengths enumerated in the design section, low attrition (overall and differential) and low participation in nonproject treatments contribute to the strong internal validity of the current study. In addition, confirmation of a preregistered hypothesis increases the likelihood of replicability. Possible concern that the difference between groups could be due to differential staff attention to parents in the two groups is addressed by showing that effects of participating in ImPACT staff-led sessions on child dependent variables are in part due to ImPACT parents’ greater use of ImPACT strategies. Because blind raters and nonintervention contexts were used to measure ImPACT strategy use, this study constitutes an advance toward determining whether parents’ increased use of pre-emptive intervention strategies generalizes outside of formal intervention sessions and improves generalized proximal skills (motor imitation and intentional communication), which have effects on clinically-important child outcomes.
Practical Implications and Conclusions
ImPACT is an intervention that can be implemented by parents during a period when it is not yet clear which particular HR-Sibs will develop a social communication-related disorder. Knowing that parents’ use of ImPACT strategies is partly responsible for effects on reduction of HR-Sibs’ communication challenges improves the basis for concluding the results are really due to ImPACT teaching. Future research might emphasize parents’ use of ImPACT strategies in more interactive contexts or activities, or provide more parent teaching sessions than those in the current study to increase the number of parents who show generalized ImPACT strategy use. Knowing that motor imitation and intentional communication are partly responsible for the reduction of communication challenges strengthens the rationale for targeting these skills.
The results of this study might generalize to other naturalistic developmental behavioral interventions (NDBIs; Schreibman et al., 2015). The ImPACT strategies that were partly responsible for effects on motor imitation and intentional communication are used in virtually all NDBIs. These strategies include expressive communication teaching, face-to-face positioning, following the child’s lead, positive affect and animation, response to child communication attempts, and use of communication temptations. Future research will be needed to verify whether other NDBIs produce indirect effects on HR-Sibs’ communication challenges through increasing the use of these strategies.
In addition, future research is needed to evaluate the scalability of ImPACT. Despite having a relatively low delivery burden (i.e., two coaching sessions per week), Part C early interventionists rarely have this amount of time to spend with families or have training in interventions such as ImPACT. As clinicians and families continue to use evidence-based NDBIs such as ImPACT, future research should focus on ways to better facilitate integration of NDBI strategies into community-based settings and for underserved families, such as by training Part C early interventionists, addressing systemic barriers, and providing telehealth access.
Acknowledgments
This work was supported by a grant to the lead author from NIDCD (R01DC013767), the National Institute for Child Health and Disorders (NICHD; P30HD15052), and a grant to S.E. from NIDCD (F31DC015696), but it does not necessarily express the views of employees of these agencies. We are grateful to the skillful and conscientious work of our staff: Catherine Bush, Elizabeth Gardner, Cassandra Newsom, Amy Nicholson, Jessica Buenahora, Heather Redix, Katherine Ragsdale, Kathryn Coddington, Danielle Trzil, Sonja Kottke, Karen Bearss, Courtney Froehlig, Veronica Kang, Shanni Geller, Allycen Kurup, Hailee Hannah, Rachel Hantman, Colleen Harker, Elizabeth Karp, & Catherine Dick. We are also grateful to the families who participated in this research.
References
- Aldred C, Green J, Emsley R, & McConachie H (2012). Brief report: Mediation of treatment effect in a communication intervention for pre-school children with autism. Journal of Autism and Developmental Disorders, 42(3), 447–454. 10.1007/s10803-011-1248-3 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: APA. [Google Scholar]
- Cohen J (1988). Statistical power analysis for the social sciences. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Deke J, & Chiang H (2017). The WWC attrition standard: Sensitivity to assumptions and opportunities for refining and adapting to new contexts. Evaluation Review, 41(2), 130–154. doi: 10.1177/0193841X16670047 [DOI] [PubMed] [Google Scholar]
- Enders CK (2010). Applied missing data analysis. New York, NY: Guildford Press. [Google Scholar]
- Esler AN, Bal VH, Guthrie W, Wetherby A, Weismer SE, & Lord C (2015). The Autism Diagnostic Observation Schedule, Toddler Module: Standardized severity scores. Journal of Autism and Developmental Disorders, 45(9), 2704–2720. doi: 10.1007/s10803-015-2432-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenson L, Marchman V, Thal D, Dale P, Reznick S & Bates E (2006). The MacArthur-Bates Communicative Development Inventories, user’s guide and technical manual (2nd Ed.). Baltimore, MD: Brookes Publishing Group. [Google Scholar]
- Finan SJ, Swierzbiolek B, Priest N, Warren N, & Yap M (2018). Parental engagement in preventive parenting programs for child mental health: A systematic review of predictors and strategies to increase engagement. PeerJ, 6, e4676. doi: 10.7717/peerj.4676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost KM (2018). Identifying and measuring common elements of naturalistic developmental behavioral interventions (Unpublished master’s thesis). Michigan State University, East Lansing, Michigan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham K, Pickles A, & Lord C (2009). Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders, 39(5), 693–705. doi: 10.1007/s10803-008-0674-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J, Charman T, Pickles A, Wan MW, Elsabbagh M, Slonims V, … & Jones EJ (2015). Parent-mediated intervention versus no intervention for infants at high risk of autism: A parallel, single-blind, randomised trial. The Lancet Psychiatry, 2(2), 133–140. doi: 10.1016/s2215-0366(14)00091-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J, Pickles A, Pasco G, Bedford R, Wan MW, Elsabbagh M, … & Charman T (2017). Randomised trial of a parent-mediated intervention for infants at high risk for autism: Longitudinal outcomes to age 3 years. Journal of Child Psychology and Psychiatry, 58(12), 1330–1340. doi: 10.1111/jcpp.12728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grzadzinski R, Carr T, Colombi C, McGuire K, Dufek S, Pickles A, & Lord C (2016). Measuring changes in social communication behaviors: Preliminary development of the Brief Observation of Social Communication Change (BOSCC). Journal of Autism and Developmental Disorders, 46, 2464–2479. 10.1007/s10803-016-2782-9 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford. [Google Scholar]
- Hus V, Gotham K, & Lord C (2014). Standardizing ADOS domain scores: Separating severity of social affect and restricted and repetitive behaviors. Journal of Autism and Developmental Disorders, 44(10), 2400–2412. doi: 10.1007/s10803-012-1719-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll B (2012). Brief report: Effect of a focused imitation intervention on social functioning in children with autism. Journal of Autism and Developmental Disorders, 42(8), 1768–1773. doi: 10.1007/s10803-011-1423-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingersoll B, & Dvortcsak A (2010). Teaching social communication to children with autism: A practitioner’s guide to parent training and a manual for parents. New York, NY: Guilford Press. [Google Scholar]
- Ingersoll B, & Meyer K (2011). Examination of correlates of different imitative functions in young children with autism spectrum disorders. Research in Autism Spectrum Disorders 5(3): 1078–1085. doi: 10.1016/j.rasd.2010.12.001 [DOI] [Google Scholar]
- Ingersoll B, & Schreibman L (2006). Teaching reciprocal imitation skills to young children with autism using a naturalistic behavioral approach: Effects on language, pretend play, and joint attention. Journal of Autism and Developmental Disorders 36: 487–505. doi: 10.1007/s10803-006-0089-y [DOI] [PubMed] [Google Scholar]
- Ingersoll B, & Wainer A (2013). Initial efficacy of Project ImPACT: A parent-mediated social communication intervention for young children with ASD. Journal of Autism and Developmental Disorders, 43, 2943–2952. doi: 10.1007/s10803-013-1840-9 [DOI] [PubMed] [Google Scholar]
- Kaiser AP, & Roberts MY (2013). Parents as communication partners: An evidence-based strategy for improving parent support for language and communication in everyday settings. Perspectives on Language Learning and Education, 20(3), 96–111. 10.1044/lle20.3.96 [DOI] [Google Scholar]
- Koegel LK, Koegel RL, & Carter CM (1998). Pivotal responses and the natural language teaching paradigm. Seminars in Speech and Language, 19(4), 355–372. doi: 10.1055/s-2008-1064054 [DOI] [PubMed] [Google Scholar]
- Legerstee M & Markova G (2008). Variations in 10-month-old infant imitation of people and things. Infant Behavior and Development 31(1): 81–91. doi: 10.1016/j.infbeh.2007.07.006 [DOI] [PubMed] [Google Scholar]
- Lieberman RG, & Yoder PJ (2012). Play and communication in children with autism spectrum disorder: A framework for early intervention. Journal of Early Intervention 34(2): 82–103. doi: 10.1177/1053815112453766 [DOI] [Google Scholar]
- Lieberman R, Yoder P, Reichow B, & Wolery M (2010). Expert visual analysis of multiple-baseline across participant data showing delayed changes in the dependent variable. School Psychology Quarterly, 25, 28–44. doi: 10.1037/a0018600 [DOI] [Google Scholar]
- Lifter K (1988). Developmental Play Assessment. Boston, MA: Northeastern University. [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, & Bishop SL (2015). ADOS-2. Manual (Part I): Modules, 1-4 New York, NY: Pearson. [Google Scholar]
- Masten AS, & Cicchetti D (2010). Developmental cascades. Development and Psychopathology, 22, 491–495. doi: 10.1017/S0954579410000222 [DOI] [PubMed] [Google Scholar]
- McDuffie AS, Lieberman RG, & Yoder PJ (2012). Object interest in autism spectrum disorder: A treatment comparison. Autism, 16(4), 398–405. doi: 10.1177/1362361309360983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDuffie A, Turner L, Stone W, Yoder P, Wolery M, & Ulman T (2007). Developmental correlates of different types of motor imitation in young children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 37(3), 401–412. doi: 10.1007/s10803-006-0175-1 [DOI] [PubMed] [Google Scholar]
- Messinger D, Young GS, Ozonoff S, Dobkins K, Carter A, Zwaigenbaum L, … & Sigman M (2013). Beyond autism: A Baby Sibling Research Consortium study of high-risk children at three years of age. Journal of the American Academy of Child and Adolescent Psychiatry, 52(3), 300–308. doi: 10.1016/j.jaac.2012.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller J, & Chapman R (1985). Systematic analysis of language transcripts. Madison, WI: Language Analysis Laboratory. [Google Scholar]
- Mullen EM (1995). Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Service Inc. [Google Scholar]
- Muthén LK, & Muthén B (2019). Mplus. The comprehensive modelling program for applied researchers: User’s guide, 5. [Google Scholar]
- Ozonoff S, Young GS, Carter A, Messinger D, Yirmiya N, Zwaigenbaum L, … & Hutman T (2011). Recurrence risk for autism spectrum disorders: A Baby Siblings Research Consortium study. Pediatrics, 128(3), e488–e495. doi: 10.1542/peds.2010-2825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozonoff S, Young GS, Landa RJ, Brian J, Bryson S, Charman T, Chawarska K, Macari SL, Messinger D, Stone WL, Zwaigenbaum, & Iosif A (2015). Diagnostic stability in young children at risk for autism spectrum disorder: A Baby Siblings Research Consortium study. Journal of Child Psychology and Psychiatry, 56, 988–998. doi: 10.1111/jcpp.12421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickard KE, Wainer AL, Bailey KM, & Ingersoll BR (2016). A mixed-method evaluation of the feasibility and acceptability of a telehealth-based parent-mediated intervention for children with autism spectrum disorder. Autism, 20(7), 845–55. doi: 10.1177/1362361315614496 [DOI] [PubMed] [Google Scholar]
- Pickles A, Harris V, Green J, Aldred C, McConachie H, Slonims V, … Charman T (2015). Treatment mechanism in the MRC preschool autism communication trial: Implications for study design and parent-focused therapy for children. Journal of Child Psychology and Psychiatry, 56(2), 162–170. doi : 10.1111/jcpp.12291 [DOI] [PubMed] [Google Scholar]
- Pierce K, Gazestani VH, Bacon E, Barnes CC, Cha D, Nalabolu S, … Courchesne E (2019). Evaluation of the diagnostic stability of the early autism spectrum disorder phenotype in the general population starting at 12 months. JAMA Pediatrics, 173(6), 578–587. doi: 10.1001/jamapediatrics.2019.0624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers SJ (1999). An examination of the imitation deficit in autism In Nadel J and Butterworth G (Eds.), Imitation in infancy, 254–283. New York, NY: Cambridge University Press. [Google Scholar]
- Rogers SJ, & Pennington BF (1991). A theoretical approach to the deficits in infantile autism. Development and Psychopathology, 3, 137–162. [Google Scholar]
- Schreibman L, Dawson G, Stahmer AC, Landa R, Rogers SJ, McGee GG, … & McNerney E (2015). Naturalistic developmental behavioral interventions: Empirically validated treatments for autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(8), 2411–2428. doi: 10.1007/s10803-015-2407-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadnick NA, Stahmer A, & Brookman-Frazee L (2015). Preliminary effectiveness of Project ImPACT: A parent-mediated intervention for children with autism spectrum disorder delivered in a community program. Journal of Autism and Developmental Disorders, 45(7), 2092–2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahmer AC, Rieth SR, Dickson KS, Feder J, Burgeson M, Searcy K, & Brookman-Frazee L (2020). Project ImPACT for toddlers: pilot outcomes of a community adaptation of an intervention for autism risk. Autism, 24(3), 617–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapp J (2003). ProcoderDV (Computer software). Nashville, TN: Vanderbilt Kennedy Center. [Google Scholar]
- Wainer AL, & Ingersoll BR (2013). Disseminating ASD interventions: A pilot study of a distance learning program for parents and professionals. Journal of Autism and Developmental Disorders, 43(1), 11–24. doi: 10.1007/s10803-012-1538-4 [DOI] [PubMed] [Google Scholar]
- Wan MW, Green J, Elsabbagh M, Johnson M, Charman T, Plummer F, & Basis Team. (2013). Quality of interaction between at-risk infants and caregiver at 12–15 months is associated with 3-year autism outcome. Journal of Child Psychology and Psychiatry, 54(7), 763–771. doi: 10.1111/jcpp.12032 [DOI] [PubMed] [Google Scholar]
- Wetherby AM, & Prizant BM (2003). Communication and Symbolic Behavior Scales Developmental Profile (1st ed.). Baltimore, MD: Brookes. doi: 10.1037/t11529-000 [DOI] [Google Scholar]
- Wetherby AM, Woods J, Allen L, Cleary J, Dickinson H, & Lord C (2004). Early indicators of autism spectrum disorders in the second year of life. Journal of Autism and Developmental Disorders, 34(5), 473–493. doi: 10.1007/s10803-004-2544-y [DOI] [PubMed] [Google Scholar]
- Whitehouse AJO, Varcin KJ, Alvares GA, Barbara J, Bent C, Boutrus M, … Hudry K (2019). Pre-emptive intervention versus intervention as usual for infants showing early behavioural risk signs of autism spectrum disorder: A single-blind, randomised controlled trial. The Lancet Child & Adolescent Health, 3(9), 605–615. doi: 10.1016/s2352-4642(19)30184-1 [DOI] [PubMed] [Google Scholar]
- Yoder PJ, Bottema-Beutel K, Woynaroski T, Chandrasekhar R, & Sandbank M (2013). Social communication intervention effects vary by dependent variable type in preschoolers with autism spectrum disorders. Evidence-Based Communication Assessment and Intervention, 7(4), 150–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoder PJ, Symons F, & Lloyd B (2018). Observational measurement of behavior (2nd ed). Baltimore, MD: Brookes. [Google Scholar]
- Yoder P, & Stone WL (2006). Randomized comparison of two communication interventions for preschoolers with autism spectrum disorders. Journal of Consulting and Clinical Psychology, 74(3), 426. doi: 10.1037/0022-006X.74.3.426 [DOI] [PubMed] [Google Scholar]
- Yoder P, Stone W, Walden T, Malesa E (2009). Predicting social impairment in younger siblings of children with ASD. Journal of Autism and Developmental Disorders, 39, 1381–1391. doi: 10.1007/s10803-009-0753-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoder P, Watson LR, & Lambert W (2015). Value-added predictors of expressive and receptive language growth in initially nonverbal preschoolers with autism spectrum disorders. Journal of Autism and Developmental Disorders, 45(5), 1254–1270. doi: 10.1007/s10803-014-2286-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwaigenbaum L, & Penner M (2018). Autism spectrum disorder: advances in diagnosis and evaluation. British Medical Journal, 361, k1674. doi: 10.1136/bmj.k1674 [DOI] [PubMed] [Google Scholar]


