Abstract
Objective
This article describes survey results from child and adolescent psychiatry (CAP) fellowship program directors regarding attitudes of their programs’ capacity to effectively educate fellows on the social determinants of mental health and program directors’ perceived importance of doing so.
Methods
A survey asking about six topics within the social determinants of mental health was disseminated to all CAP program directors with email addresses found in the Fellowship and Residency Electronic Interactive Database (FREIDA) (n = 134). Data were exported using the Qualtrics survey platform.
Results
Fifty-three program directors (40%) responded to the survey. Overall, 98% of program directors felt education on the social determinants of mental health was “essential” for fellowship training, but there were significant differences in perceived relative importance and effectiveness of education provided across topics. Familial factors were rated as significantly more important than structural, historical, and economic factors. Structural and historical factors were viewed as being taught less effectively than other factors. Educational, structural, and historical factors and neighborhood factors were allotted significantly less instructional time than familial factors.
Conclusions
While there is near-universal consensus that social determinants of mental health education are critical for fellowship training, program directors feel that social determinants of mental health topics differ in importance and are taught at varying levels of effectiveness. These findings highlight the need for intra-institutional and or inter-institutional collaboration for social determinants of mental health educational content development if CAP programs are to prepare trainees to best serve their most vulnerable patients.
Keywords: Child and adolescent psychiatry, Training, Social determinants of mental health
Physicians increasingly recognize the importance of the social determinants of mental health and the causal relation between psychosocial factors and childhood mental illness [1]. In recent years, psychiatric educators have emphasized the need to improve residency training on the social determinants of mental health [2], asserting that trainees must learn to consider ways that institutions, neighborhood conditions, public policies, and health care delivery systems shape symptoms and diseases and also work to address these underlying conditions both inside and outside of the traditional clinic setting [3].
The Accreditation Council for Graduate Medical Education (ACGME) requires general psychiatry residents to demonstrate competence in knowledge of how “psychological, sociocultural, economic, [and] ethnic … factors significantly influence physical and psychological development throughout the life cycle” and “in the evaluation and treatment of patients of different ages and genders from diverse backgrounds, and from a variety of ethnic, racial, sociocultural, and economic backgrounds” [4]. Some adult psychiatry programs have developed and disseminated novel educational content on the social determinants of mental health for trainees [5, 6]. For child and adolescent psychiatry (CAP) fellowships, the ACGME also requires that CAP training addresses disparities in mental health as part of fellowship curricula [7].
Given the expanding emphasis on incorporating psychosocial factors into clinical care, we sought to better understand the attitudes of CAP program directors regarding the importance of educating fellows on the social determinants of mental health and their perceptions of their programs’ abilities to do so. Categories of social determinants of mental health for children and adolescents were drawn from a large metaanalysis of social determinants of mental health [8], the World Health Organization’s expository paper on the subject [9], and published screening tools for identifying areas of psychosocial distress that may impact child physical and behavioral health [10–12]. Through these methods, we identified the following social determinants of mental health topics: economic factors (e.g., transportation access, food scarcity), familial factors (e.g., caregiver separation, family composition), cultural factors (e.g., linguistic barriers, cultural understanding of mental illness), neighborhood factors (e.g., housing instability, community violence exposure), educational factors (e.g., unmet educational need), and structural and historical factors (e.g., institutionalized poverty and racism, community history).
Methods
The study was deemed exempt research by the Johns Hopkins Medicine Office of Human Subjects Research Institutional Review Boards. Program directors of US CAP fellowships were invited to participate in this study. Using publicly available information from the Fellowship and Residency Electronic Interactive Database (FREIDA) [13], 136 programs were identified. Of those programs, 2 (1.5%) had no functional e-mail address available, leaving 134 eligible participants. Survey invitations were sent to program directors via Qualtrics survey software.
The survey collected program demographic information and inquired about program directors’ attitudes and perceptions regarding CAP fellowship education on the social determinants of mental health. Using a four-point Likert scale, program directors were asked about their beliefs regarding the importance of teaching various social determinants topics (rated from “No Importance” to “Essential for Fellow Education”) and their perceptions of how effectively each topic was taught to fellows at their institution (rated from “Ineffectively” to “Extremely Effectively”). Program directors were also asked how much instructional time, both didactic and non-didactic non-clinical (e.g., via experiential learning), was allotted to fellow education over the course of the fellowship for each topic.
Descriptive analyses were used to analyze the data. Differences in perceived importance across the six social determinants categories were examined using the related samples Cochran’s Q test. Post hoc pairwise comparisons were then conducted using Dunn’s test to determine which category comparisons were significant. Because perceived effectiveness of teaching each topic and time dedicated for instruction of each topic were both ordered categorical variables, Friedman’s test was conducted to determine whether there were any significant differences across the social determinants of mental health categories, and Kendall’s W was used to estimate effect size. Post hoc pairwise comparisons were then conducted using the Wilcoxon-signed rank test to determine which category comparisons were significant. To control for multiple comparisons (15 post hoc comparisons), a Bonferroni correction was made using the following formula (.05/15). Thus, the adjusted significance level of .003 was used.
Results
A total of 53 surveys were completed by the 134 surveyed program directors (40%). A majority of respondents represented programs in urban settings (55%), though 11% were situated in suburban areas, 2% in rural communities, and 32% utilized a combination of settings. The mean number of total fellows per program was 8.2 (SD = 5.2). Among participating programs, 58% required fellows to provide multiple visits over at least a six-month period in a clinical setting that primarily provides care for medically underserved populations or in medically underserved areas, while 34% did not and 8% of program directors were uncertain.
Overall, 91% of program directors rated education on the social determinants of mental health as being “Essential for Fellow Education,” 9% of program directors rated it as being of “Modest Importance,” and no respondents selected “Low Importance” or “No Importance.”
In comparing program directors’ perceptions of the relative importance of teaching each social determinants topic, the related samples Cochran’s Q test was significant (χ2 (5, N = 53) = 24.78, p < .001). Pairwise post hoc Dunn’s tests demonstrated that familial factors were rated as significantly more important than structural and historical factors (p < .001) and economic factors (p = .001). No other comparisons between social determinants topics were statistically significant. Structural and historical factors were least likely to be rated “Essential” by program directors, and 74% rated the topic as such compared with 98% for familial factors (Fig. 1, part a).
Fig. 1.
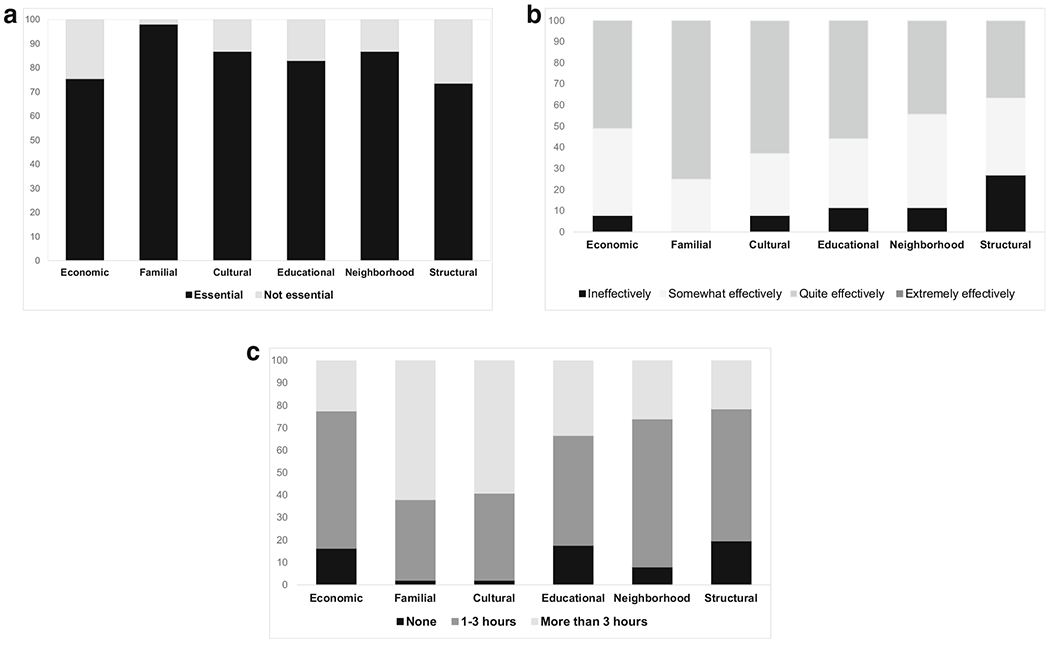
Perceived importance, perceived effectiveness, and time spent teaching fellows about the impact of key social determinants of mental health on child development and psychopathology. Notes. Social determinants of mental health content areas are listed along the x-axis. Values shown on the y-axis indicate the percentage of respondents selecting a particular response. Captions for each part of the figure are as follows: a Perceived importance of teaching social determinants, b perceived effectiveness in teaching social determinants, c amount of time spent teaching social determinants
There were significant differences in program directors’ perceptions of effectiveness of teaching psychiatry fellows about social determinants of mental health topics (Friedman’s χ2 (5, N = 51) = 45.84, p < .001, Kendall’s W = .180). Results of post hoc pairwise comparisons (Table 1) showed multiple significant differences among topics. Structural and historical factors were perceived to be taught significantly less effectively than economic factors (p = .002), educational factors (p = .005), cultural factors (p < .001), and familial factors (p < .001). Additionally, familial factors were perceived to be taught significantly more effectively than economic factors (p = .001), cultural factors (p = .002), and neighborhood factors (p < .001). No other comparisons achieved statistical significance. Overall, 27% of program directors felt their program’s instruction on structural and historical factors was “Ineffective” while 0% of program directors felt their program’s instruction on familial factors was “Ineffective.” No program directors rated instruction on any topic as “Extremely Effective,” but 75% of program directors rated their program’s instruction on familial factors as “Quite Effective.” Conversely, at least 45% of program directors rated their program’s instruction on economic factors, educational factors, and neighborhood factors as being either “Ineffective” or only “Somewhat Effective” (Fig. 1, part b).
Table 1.
Comparison of perceptions of effectiveness and time dedicated to teach psychiatry fellows about the social determinants of mental health across different social determinant content areas
| Comparison | Perceived effectiveness of teaching about social determinants |
Time dedicated to teaching about social determinants |
||
|---|---|---|---|---|
| Z-statistic | p value | Z-statistic | p value | |
| Structural vs economic | − 3.15 | .002 | − 0.24 | .808 |
| Structural vs educational | − 2.81 | .005 | − 1.13 | .258 |
| Structural vs cultural | − 3.91 | < .001 | − 4.74 | < .001 |
| Structural vs neighborhood | − 2.68 | .007 | − 1.81 | .071 |
| Structural vs familial | − 4.79 | < .001 | − 4.20 | < .001 |
| Economic vs educational | − 0.25 | .802 | − 0.80 | .425 |
| Economic vs cultural | − 1.09 | .275 | − 4.21 | < .001 |
| Economic vs neighborhood | − 1.51 | .132 | − 1.41 | .157 |
| Economic vs familial | − 3.37 | .001 | − 4.17 | < .001 |
| Educational vs cultural | − 0.93 | .354 | − 3.45 | .001 |
| Educational vs neighborhood | − 1.27 | .204 | − 0.38 | .707 |
| Educational vs familial | − 2.91 | .004 | − 4.23 | < .001 |
| Cultural vs neighborhood | − 2.12 | .034 | − 3.79 | < .001 |
| Cultural vs familial | − 3.05 | .002 | − 0.50 | .617 |
| Neighborhood vs familial | − 3.95 | < .001 | − 3.77 | < .001 |
Because this analysis involved multiple comparisons, a Bonferroni adjustment was applied such that only those differences with a p value of p ≤ .003 are considered significant
Significant differences were identified in educational time allotted for each social determinants of mental health topic (χ2 (5, N = 49) = 54.898 p < .001, Kendall’s W = .224). Post hoc pairwise comparisons (Table 1) revealed multiple significant differences among topics. Structural and historical factors were allotted significantly less instructional time than cultural factors (p < .001) and familial factors (p < .001). Economic factors were allotted significantly less time than cultural factors (p < .001) and familial factors (p < .001). Educational factors were allotted significantly less time than cultural factors (p < .001) and familial factors (p < .001). Neighborhood factors were allotted significantly less time than cultural factors (p < .001) and familial factors (p < .001). In addition, 16% of program directors shared that they allotted no time for didactic or non-didactic non-clinical instruction for economic factors, 18% shared the same for educational factors, and 20% for structural and historical factors. Only 2% of program directors shared they allotted no time for cultural factors or familial factors (Fig. 1, part c).
Discussion
Based on survey response, there is near-universal agreement that education on the social determinants of mental health should be an essential part of CAP training. By breaking down the social determinants into six distinct topic areas, we learned more specifically about child psychiatry education on this subject. Program directors rated familial factors as being the most important social determinants topic and the topic most effectively taught to fellows. This finding may not be surprising considering that the impact of family issues on child mental health is connected to five of the six ACGME CAP milestone categories [14]. Instruction not directly related to the social determinants of mental health, such as attachment and family therapy, may also be a part of fellowship training curricula. Additionally, familial and cultural factors may seem to require more immediate attention when evaluating and treating children and adolescents, as parent-child relational problems may be why a child presents to treatment, whereas structural and economic factors may be assumed to have a more indirect role in presentation. As 62% of program directors stated that their programs allot more than three hours to teaching familial factors, the highest of any social determinants topic, higher perceived effectiveness of teaching this topic in CAP programs may be explained in part by having more instructional time. Social determinants of mental health education relating to cultural factors is also an area of relative strength, with 63% of program directors rating the quality of their institution’s instruction as “Quite Effective.” Like familial factors, education related to cultural factors was allotted significantly more instructional time than economic factors, educational factors, and structural and historical factors. Similar to familial factors, cultural factors are highly represented in the ACGME milestones [14] and incorporated into four of six milestone categories. Cultural factors are also paid specific and special attention with their own section on cultural formulation in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [15].
While program directors rated structural and historical factors as least critical to CAP education among social determinants of mental health topics, the vast majority still rated it as “Essential.” Notably, 27% of program directors rated it as ineffectively taught at their institution and 20% of program directors devoted no didactic or non-didactic non-clinical instructional time to this topic. Program directors also rated economic and neighborhood factors as being less effectively taught at their institutions and in 16% of programs, no didactic or non-didactic non-clinical instructional time was devoted to economic factors.
While instructional time serves as a limiting factor given programs’ competing educational priorities, relative educational deficiencies in structural and historical, neighborhood, and economic factors found by this survey may have additional explanations. Despite the role of poverty and neighborhood conditions in child psychopathology, there may be few CAP faculty members at many institutions with this particular area of expertise. Furthermore, in their program requirements and milestones documentation, the ACGME provides little guidance regarding instruction of specific content related to psychosocial factors [7, 14]. Simply adding time for these social determinants topics may not be sufficient to improve the quality of instruction. However, there may be several ways to overcome these challenges. Child psychiatry fellowships could partner with other academic departments within their institutions, such as departments of pediatrics as well as history, education, or sociology to create educational content related to child mental health. CAP programs might also collaborate with one another to generate educational content, combining expertise, resources, and data from multiple sites. In addition, CAP programs could jointly develop educational content and experiences with local community organizations whose work centers around issues like housing or parents returning from incarceration, highlighting in a more personal way the overlap between mental health and social issues. As another example, CAP faculty can partner with departments of sociology in their own institutions and teach fellows to conduct “community assessments” as a means of identifying potential protective and risk factors for children that live in specific neighborhoods, exploring the community in person and via publicly available data. To reinforce integrating these concepts into clinical care, existing areas of instruction can be modified as well. For instance, fellows can be taught to incorporate the social determinants of health into clinical formulations, ensuring that trainees illustrate how psychosocial factors generate, exacerbate, or obfuscate psychopathology. Programs can also work with fellows to expand treatment plans to address children and families’ psychosocial needs as well.
Limitations of this study include the relatively modest level of survey completion (40%) and the possibility of selection bias among respondents. However, even among a sample that may be especially interested in the subject, we found broad discrepancies between program directors’ perceptions of the importance of educating fellows on the social determinants of mental health and how effectively CAP programs educate on those social determinants. Given this, the ACGME may consider updating requirements and milestones for CAP programs to both reflect the necessity of social determinants of mental health education and related skills and provide more specific guidance regarding social determinants of mental health content. Furthermore, the findings of this survey support the need for a comprehensive curricular social determinants of mental health framework that could be disseminated to and used by various child psychiatry programs that emphasizes structural and historical, economic, educational, and neighborhood factors in particular. This critical educational content would help support child psychiatry’s mission to provide excellent care for the most vulnerable.
Footnotes
Disclosure On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- 1.Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, et al. Adolescence and the social determinants of health. Lancet. 2012;379:1641–52. [DOI] [PubMed] [Google Scholar]
- 2.Hansen H, Braslow J, Rohrbaugh RM. From cultural to structural competency-training psychiatry residents to act on social determinants of health and institutional racism. JAMA Psychiatry. 2018;75:117–8. [DOI] [PubMed] [Google Scholar]
- 3.Metzl JM, Hansen H. Structural competency and psychiatry. JAMA Psychiatry. 2018;75:115–6. [DOI] [PubMed] [Google Scholar]
- 4.Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in psychiatry 2017, https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/400_psychiatry_2017-07-01.pdf Accessed 20 Dec 2018.
- 5.Bromage B, Encandela JA, Cranford M, Diaz E, Williamson B, Spell VT, et al. Understanding health disparities through the eyes of community members: a structural competency education intervention. Acad Psychiatry. 2019;43:244–7. [DOI] [PubMed] [Google Scholar]
- 6.Mathis W, Cyrus K, Jordan A, Rohrbaugh R. Introducing a structural competency framework for psychiatry residents: drawing your neighborhood. Acad Psychiatry. 2019;43:635–8. [DOI] [PubMed] [Google Scholar]
- 7.Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in child and adolescent psychiatry, 2019. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/405_ChildAdolescentPsychiatry_2019.pdf?ver=2019-06-19-091518-287 Accessed 2 Jan 2020.
- 8.Lund C, Brooke-Sumner C, Baingana F, Baron EC, Breuer E, Chandra P, et al. Social determinants of mental disorders and the sustainable development goals: a systematic review of reviews. Lancet Psychiatry. 2018;5:357–69. [DOI] [PubMed] [Google Scholar]
- 9.Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26:392–407. [DOI] [PubMed] [Google Scholar]
- 10.Morone J An integrative review of social determinants of health assessment and screening tools used in pediatrics. J Pediatr Nurs. 2017;37:22–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Billioux A, Verlander K, Anthony S, Alley D. Standardized screening for health-related social needs in clinical settings: the accountable health communities screening tool. Discussion Paper, National Academy of Medicine. 2017. https://nam.edu/wp-content/uploads/2017/05/Standardized-Screening-for-Health-Related-Social-Needs-in-Clinical-Settings.pdf Accessed 17 Sep 2018. [Google Scholar]
- 12.Chung EK, Siegel BS, Garg A, Conroy K, Gross RS, Long DA, et al. Screening for social determinants of health among children and families living in poverty: a guide for clinicians. Curr Probl Pediatr Adolesc Health Care. 2016;46:135–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The American Medical Association. The AMA Residency & Fellowship Database https://freida.ama-assn.org/Freida/#/programs?specialtiesToSearch=405 Accessed 12 Mar 2019.
- 14.Hunt J, DeJong S, Edgar L, Liu H, Santos C. The Child & Adolescent Psychiatry Milestone Project, 2015. https://www.acgme.org/Portals/0/PDFs/Milestones/ChildandAdolescentPsychiatryMilestones.pdf Accessed 20 Dec 2018.
- 15.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). Arlington: American Psychiatric Publishing, Inc.; 2013. [Google Scholar]


