Abstract
Objective:
The mind and body function in tandem across days and development, and in unique ways for individuals, but most work on the relation between personality and physical health is cross-sectional, assuming homogeneity across time and people. For instance, although neuroticism is associated with poor health, the direction of the relation and whether it characterizes all people all of the time is unclear. The goal of this study is to fill knowledge gaps concerning the person-specific, day-to-day neuroticism-health link.
Methods:
A 75-occassion intensive longitudinal study was conducted in which 119 adults reported daily on 12 indicators of neuroticism and 3 symptoms of physical health. Person-specific network analyses, conducted using the multiple solutions version of group iterative multiple model estimation (GIMME-MS), were used to determine the presence, valence, daily lag, and direction of relations among the daily variables. Network features were compared within and between individuals.
Results:
Person-specific networks were heterogeneous. Participants were significantly more likely to have networks in which physical symptoms predicted indicators of neuroticism compared to the reverse; this was particularly true for next-day relations, and for women. Exploratory analyses suggested that participants with a disproportionate amount of these health-to-neuroticism relations scored high on conscientiousness.
Conclusions:
Person-specific network mapping of ecologically-valid intensive longitudinal data revealed heterogeneity in day-to-day relations between indicators of neuroticism and physical health, with long-term implications for personalized healthcare. There was some consistency, however, in that “body” symptoms were more likely to predict “mind” features across people.
Keywords: GIMME, intensive longitudinal study, networks, personality, somatic symptoms
Introduction
Personality and health are intricately integrated. Although high conscientiousness has been shown to predict low blood pressure (Turiano et al., 2011) and low agreeableness has been associated with worse cardiovascular health (Ozer & Benet-Martinez, 2006), the link between neuroticism and poor health is arguably the most consistent. Individuals high in neuroticism regularly report more physical health problems than those low in neuroticism (Johnson, 2003; Ozer & Benet-Martinez, 2006; Parker, Bagby, & Taylor, 1989; Suls & Martin, 2005). Unfortunately, the extant literature is cross-sectional, leaving the direction of the relation between neuroticism and physical health, and whether this direction varies across individuals, underdetermined. The aim of this paper is to address these knowledge gaps using a 75-day intensive longitudinal study and person-specific network mapping.
Neuroticism and Physical Health
Neuroticism is “a broad dimension of individual differences in the tendency to experience negative, distressing emotions and to possess associated behavioral and cognitive traits” (Costa & McCrae, 1987, p. 301). Individuals high in neuroticism use a disproportionate amount of health care resources (Lahey, 2009; ten Have, Oldehinkel, Vollebergh, & Ormel, 2005). Physical health is a broad construct, but includes symptoms of illness as well as headaches, stomach aches, fatigue, and dizziness (Kroenke, 2003) that account for millions of emergency room visits in the United States annually (Pitts, Niska, & Burt, 2008).
Research on neuroticism and physical health largely stems from a seminal paper by Costa and McCrae (1985a) suggesting that patients’ neuroticism scores predicted their reports of symptoms (e.g., chest pain). This finding has been widely replicated (Hyphantis, Goulia, & Carvalho, 2013; Rosmalen, Neeleman, Gans, & de Jonge, 2007) across cultures (e.g. Liu et al., 2018) and age groups (e.g. Jorm et al., 1993; Liu et al., 2018), and in twins (Liu et al., 2018) and the chronically ill (Hyphantis et al., 2013).
The neuroticism-health link seems to be particularly strong for women (Jorm et al., 1993; Liu et al., 2018), who generally report poorer health (Williams & Wiebe, 2000) and more frequent and intense health symptoms (Barsky, Peekna, & Borus, 2001; Hyphantis et al., 2013) than men. Additionally, there is some evidence that the relation between neuroticism and health is moderated by other personality factors: The link may only be present for those low in agreeableness because those high in agreeableness presumably have greater self-regulation of negative thoughts (Ode & Robinson, 2007).
Directionality
Regardless of moderators, the directionality of the link between neuroticism and physical health is theoretically disputed (reviewed in Rosmalen et al., 2007). The disability hypothesis suggests that the discomfort from adverse physical health causes personality changes, including increasing neuroticism, the psychosomatic hypothesis suggests that stress and negative affect from neurotic thinking cause physiological changes and can therefore cause or exacerbate health problems, and finally, the symptom perception hypothesis qualifies the psychosomatic hypothesis by claiming that neuroticism does not lead to health problems, but rather leads individuals to perceive more physical issues (Watson & Pennebaker, 1989).
These theoretical disputes likely stem from the cross-sectional nature of the empirical literature. Experimental manipulations related to health (e.g., Feldman, Cohen, Doyle, Skoner, & Gwaltney, 1999) are limited in humans, but longitudinal data provide the opportunity to make some directional inferences (Burkholder & Harlow, 2003; Selig & Little, 2012). Moreover, physical health and even personality can vary across short periods of time (Dotterer, Beltz, Foster, Simms, & Wright, 2019; Molenaar & Campbell, 2009; Wright & Simms, 2016). For instance, Fleeson (2001) demonstrated significant within-person variation in the Big Five personality traits in a study of up to 65 measurements per person. Thus, intensive longitudinal data may be best-suited to addressing directionality.
Most research on the neuroticism-health link also assumes homogeneity across people in order to average across them; even clinical and personality research, with perennial emphases on individual differences, typically rely on variability with respect to group averages. But, there is reason to think that personality and physical health are so heterogeneous that aggregations of data – although efficient in describing populations – actually misrepresent individuals, as indicated by mathematical theorem (Molenaar, 2004) and empirical evidence. For example, within-person analyses of 90-day personality assessments revealed that participants’ factor structures did not match the Big Five structure; in other words, the average personality structure did not generalize to individuals (Molenaar & Campbell, 2009). This focus on the individual is also seen in recent shifts toward personalized medicine and mental health treatment, as the underlying symptomatology and preferred intervention are often heterogeneous across individuals with the same (homogeneity-assuming) diagnosis (see Wright & Woods, 2020). This means that some features of neuroticism might be closely linked to some physical symptoms for some individuals, but that different constellations of neuroticism-health relations might characterize other individuals.
Intensive Longitudinal Research
Intensive longitudinal research would facilitate investigation into the directionality of the neuroticism-health link at the individual, or person-specific, level. This ambulatory assessment method uses smartphones, tablets and personal computers to collect many observations from the same people in ecologically valid settings (Timmers et al., 2014; Trull & Ebner-Priemer, 2013). It permits person-specific investigations that focus on intraindividual (i.e., within-person) variation, in contrast to mean-level analyses of cross-sectional data that focus on interindividual (i.e., between-person) variation. A person-specific approach assumes that individuals are unique and that their uniqueness is not a hurdle to understanding thoughts, actions, and behaviors, but rather a vehicle that drives insight (von Eye & Bogat, 2006).
GIMME-MS
GIMME (group iterative multiple model estimation) is a data-driven method for the person-specific analysis of intensive longitudinal data (Beltz & Gates, 2017). It implements unified structural equation models (uSEMs), which combine vector autoregression (VAR) and traditional SEMs. GIMME fits sparse networks by iteratively adding group-level relations (i.e., network connections) among variables (i.e., nodes) followed by individual-level relations. Group-level relations reflect homogeneity and are estimated in all person-specific networks if they are significant for at least 75% of the sample, while individual-level relations reflect heterogeneity and are unique to a person. The fitted relations can either be contemporaneous (reflecting prediction at the same measurement occasion) or lagged (reflecting prediction from one measurement occasion to the next). The relations do not reflect causality, but rather, statistical prediction (like independent variables in regressions, which often predict in the context of other predictors).
GIMME for multiple solutions (GIMME-MS) is ideal for detecting the direction of relations between variables (Beltz & Molenaar, 2016). A limitation of standard GIMME is that, in a given iteration (at the group- or individual-level), two relations can equally improve model fit; often these relations concern the same two variables, with contemporaneous prediction in opposite directions. Instead of arbitrarily selecting a relation, GIMME-MS generates two separate solution paths, with each relation estimated in a different path and the iterative search process continuing for both solutions (and any subsequent equivalences). Model selection is then conducted (e.g. using the Akaike Information Criterion [AIC]) to identify a single solution, which includes the statistically-optimal direction of relations between variables. Thus, GIMME-MS combines intensive longitudinal data with a (potentially) large solution space and model selection to identify a network with statistical directed predictions.
GIMME and GIMME-MS have been validated in several large-scale simulations, showing that they successfully identify the presence and direction of relations, especially when variables have over 60 observations (Beltz & Molenaar, 2016; Gates & Molenaar, 2012; Lane, Gates, Pike, Beltz, & Wright, 2019). GIMME-MS has also been used to provide insight into brain and behavioral networks, including personality (Beltz, Wright, Sprague, & Molenaar, 2016; Dotterer et al., 2019; Weigard, Beltz, Reddy, & Wilson, 2019).
Current Study
The goal of this study was to fill the knowledge gaps regarding the directionality and person-specificity of the neuroticism-health link. This was accomplished in a 75-occasion intensive longitudinal study assessing daily indicators of neuroticism and physical health combined with GIMME-MS to create person-specific networks of the relations among the indicators. We aimed to: (1) identify sample homogeneity and person-specific heterogeneity in daily relations between neuroticism and health; (2) determine the directionality of the relations between neuroticism and health; and (3) explore whether the neuroticism-health links are related to sex or other personality factors.
Methods
The data reported here are taken from a larger project concerning sex hormones and gendered cognition and behavior, with an over-representation of women. Other data from this project have already been reported (Beltz & Gates, 2017; Foster & Beltz, Under Review; Kelly & Beltz, Under Review).
Participants
The final sample consisted of 119 participants (97 female, 81.5%). Most were young adults (age: M=21.28, SD=2.94) and 69% were White. There were no sex differences in age, t(116)=−.65, p>.05, or race, χ2(3)=3.65, p>.05; age was missing for one participant.
Participants represent a subset of 175 individuals who enrolled in a 75-day diary study and were recruited from a previous laboratory-based study; some data from that study are reported here as “intake” measures. Of the 175 participants, 56 were not included in analyses for methodological reasons: To ensure validity and sufficient statistical power for person-specific network mapping, the current study focused on individuals with response rates of at least 80% with variability across the 75 days. Specifically, 32 participants with low response rates and 24 participants with neuroticism or physical health items with standard deviations of 0 were excluded.
Procedure
Participants completed a 60-minute online survey containing both cognitive tests and behavioral questionnaires, including self-reports of personality. This occurred in a research laboratory-based intake session and was supervised by a research assistant. Participants received $15 or course credit. Ethical approval was obtained for study procedures from the University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board, and all participants provided written informed consent.
Participants next completed daily 20-minute diaries for 75 days. Each day participants were emailed a unique link to an online survey that could be completed on a smartphone, tablet, computer, or other Internet-enabled device. They were asked to complete it after 8PM or at the end of their activities. Daily diaries contained the personality and physical health measures (in addition to other measures) presented in the same order every day. Due to technical difficulties, participants failed to receive their daily links 0.34% of the time. Participants were compensated up to $200. If they completed 90% of the diaries, they received $2 per diary plus a $50 bonus. If they completed between 80% (inclusive) and 90%, they received $2 per diary. If they completed less than 80%, they received $1 per diary.
Measures
The 60-item NEO Personality Inventory (Costa & McCrae, 1985b) was used to assess the Big Five personality factors in both the intake and daily diaries. In the intake, participants indicated the extent to which they generally agreed with each statement on a 5-point Likert scale (1=“Strongly disagree” to 5=“Strongly agree”). Composites for neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness were created by reverse-coding (when necessary) and averaging the relevant 12 items.
In daily diaries, participants indicated the extent to which each of the 12 neuroticism statements described them in the past 24 hours on the same 5-point Likert scale. Composites were not created; each item was used as a node in network analyses.
Three items from the Daily Inventory of Stressful Events (Almeida, 1998) were used to assess physical health. Each day participants indicated how much of the past 24 hours they experienced body aches, cold symptoms, and stomach problems (1=“None of the time”, 2=“A little of the time”, 3=“Some of the time”, 4=“Most of the time”, 5=“All of the time”). A composite was not created; each item was used as a node in network analyses.
Data Analysis
GIMME-MS (Beltz & Molenaar, 2016) was used to create sparse, person-specific networks for each participant based on their diary data (i.e., 15-variate time series consisting of up to 75 daily responses to 12 neuroticism items and 3 physical health items). All GIMME analyses were conducted using version 0.6–1 of the gimme package in R version 3.6.1.
Briefly, lagged and contemporaneous relations among the 15 items were added to a null model based on Lagrange multiplier tests, which indicate the extent to which a given relation would improve model fit if added to the network (Sörbom, 1989). Relations were added in a twotiered process. First, to prioritize sample homogeneity (if it exists), group-level relations were added to all participants’ networks if they would significantly (p<.05) improve model fit for at least 75% of the sample. Second, to capture heterogeneity, individual-level relations were added to each participant’s network if they significantly improved model fit. This search process continued until networks achieved excellent fit on at least two of four indices: comparative fit index (CFI)≥.95; non-normed fit index (NNFI)≥.95; root mean square error of approximation (RMSEA)≤.05; standardized root mean square residual (SRMR)≤.05 (Brown, 2014). If at any point in the group- or individual-level search procedure, two potential relations would equally improve model fit (i.e., had equal Lagrange multiplier tests), then each was estimated in a separate solution path; this process could occur at multiple points during model fitting, and thus, could lead to the generation of a large number of solutions per participant.
Solution-reduction was implemented following procedures validated and utilized in previous work (Beltz & Molenaar, 2016; Beltz et al., 2016; Dotterer et al., 2019; Weigard et al., 2019). After discarding implausible solutions, with standardized error covariance matrix values <0 or >1 (36% of all solutions), the solution with the lowest AIC was selected. This identified plausible individual-level models for all but 5 participants.
Following GIMME-MS, inferential analyses were conducted in SPSS version 26. The density (i.e., number) of relations between the 12 neuroticism and 3 physical health nodes were of primary interest (see Rubinov & Sporns, 2010). Specifically, for each individual, the number of directional relations from neuroticism to physical health nodes (neuroticism-to-health), and the number of directional relations from physical health to neuroticism nodes (health-to-neuroticism) were calculated. The focus was on density summed across contemporaneous and lagged relations, but relation types were examined separately in follow-up sensitivity analyses.
First, the nature of the relations involving neuroticism and physical health was evaluated. A paired samples t-test was used to determine whether, proportionally, autoregressive relations (indicating that a variable predicts itself the next day) were more common for neuroticism or physical health items. To examine directionality, another paired samples t-test was conducted in which the densities of neuroticism-to-health and health-to-neuroticism relations were compared.
Second, the link between sex and network density was explored. Two separate multiple regression analyses were conducted, in which neuroticism-to-health and health-to-neuroticism densities were the dependent variables. Sex was the predictor. Mean levels of endorsement of neuroticism and physical health items across all 75 days of the study were covariates (to ensure that levels of endorsement were not driving covariation).
Third, links between individual differences in the directionality of relations between neuroticism and physical health and other features of personality were explored. Two extreme groups were created using a difference score: health-to-neuroticism density minus neuroticismto-health density. This resulted in individuals who had predominantly neuroticism-to-health relations (scores≤−2) and individuals who had predominantly health-to-neuroticism relations (scores≥2). Groups were then compared on general personality factors (from the laboratory intake) using independent t-tests; because analyses were exploratory, there were no corrections for multiple comparisons.
Results
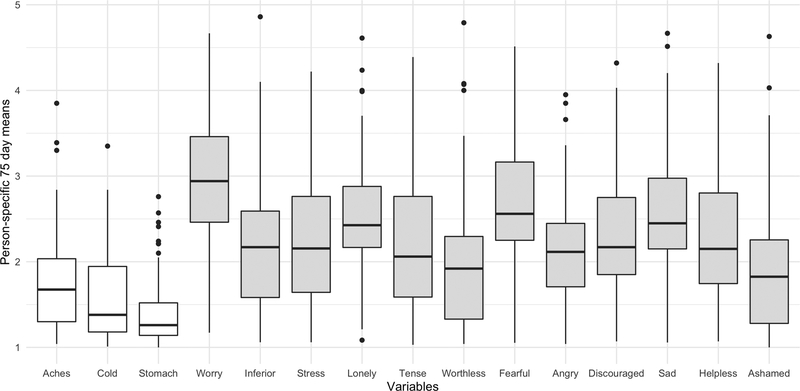
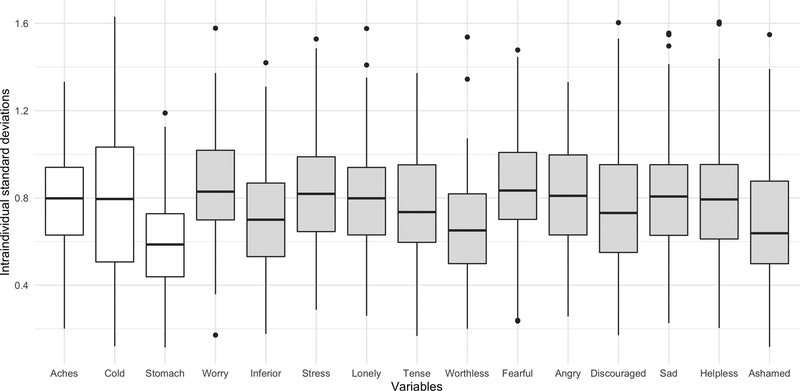
There was notable variability within and between participants in daily indicators of neuroticism and physical health. Figure 1 shows variation in participants’ mean scores across all 75 days, and Figure 2 shows participants’ intraindividual standard deviations for each variable across all 75 days. Although average endorsement of the three physical health items was generally lower than endorsement of the 12 neuroticism items (Figure 1), variability estimates were similar across variables (Figure 2).
Figure 1.
Boxplot showing the median (solid middle lines), interquartile ranges (boxes), and outliers (dots) for person-specific 75-day means of the 3 physical health indicators (white) and 12 neuroticism indicators (gray).
Figure 2.
Boxplot showing the median (solid middle lines), interquartile ranges (boxes), and outliers (dots) for intraindividual standard deviations of the 3 physical health indicators (white) and 12 neuroticism indicators (gray).
GIMME-MS
According to average indices, 112 of the 114 person-specific networks fit the data well: CFI=.96 (range: .95-.98), NNFI=.94 (range: .92-.97), RMSEA=.04 (range: .02-.06), SRMR=.08 (range: .05-.14). Two person-specific networks did not meet the criteria for excellent fit and were excluded from subsequent analyses. There were no group-level relations (i.e., relations shared by 75% of the sample), and therefore, all person-specific networks contained only individual-level relations. Of the 112 participants, 110 (98.21%) had at least 2 plausible solutions; on average participants had 25 plausible solutions (range: 1–170, SD=26). As two participants had multiple solutions with the same AIC that differed in the directionality of neuroticism-health relations, they were excluded from analyses concerning directionality. Figure 3 shows the solution generation process for one participant, demonstrating how the final solution set was created through a series of bifurcating paths. GIMME-MS produced 16 possible solutions for this participant; the 9 plausible ones are displayed, with the first solution (on the far left) selected as the final network. Figure 4A shows this network. Most relations are positive (red), there are autoregressive relations for all three physical health items but only 4 of 12 neuroticism items, and there are 7 relations between neuroticism and physical health; 2 are lagged (dashed lines) and 5 are contemporaneous (solid lines).
Figure 3.

Solution tree for a participant (whose final network is depicted in Figure 4A) showing the solution set generated by GIMME-MS. When two (or more) relations would equally improve model fit, each was freed in a separate path before iterations continued.
Figure 4.
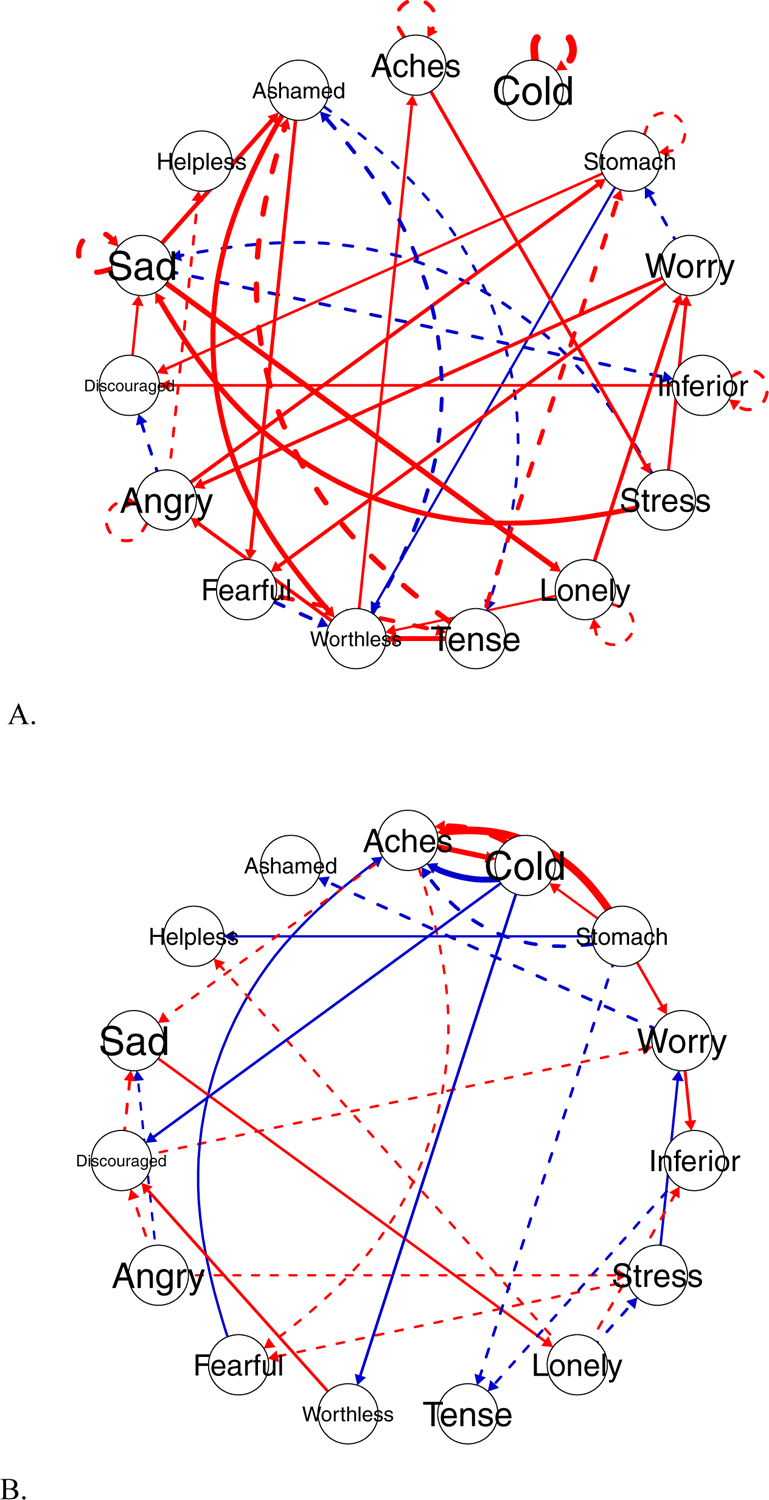

Networks for three heterogeneous participants produced by GIMME-MS. Circles are network nodes (i.e., variables in the 75-day intensive longitudinal study), and lines are directed relations reflecting prediction between nodes. Solid lines reflect same-day prediction, dashed lines reflect next-day prediction (i.e., lag 1 relations), red lines reflect positive relations, and blue lines reflect negative relations. Line thickness reflects the magnitude of the relation.
Neuroticism and Physical Health: Stability and Directionality
Across all 112 person-specific networks, there were 3942 relations. Of these, 3041 were positive (77.14%) and 901 were negative (22.86%).
Autoregressive relations were examined to provide insight into the stability of neuroticism and physical health indicators across days. Almost all participants (94.64%) had an autoregressive relation, and 95.11% were positive in magnitude. Figure 5 displays the percentage of participants who had an autoregressive coefficient for each node. Physical health autoregressions were more frequent than neuroticism autoregressions, t(111)=13.46, p<.001, with participants having autoregressive relations for 50.30% of physical health items and 12.59% of neuroticism items.
Figure 5.
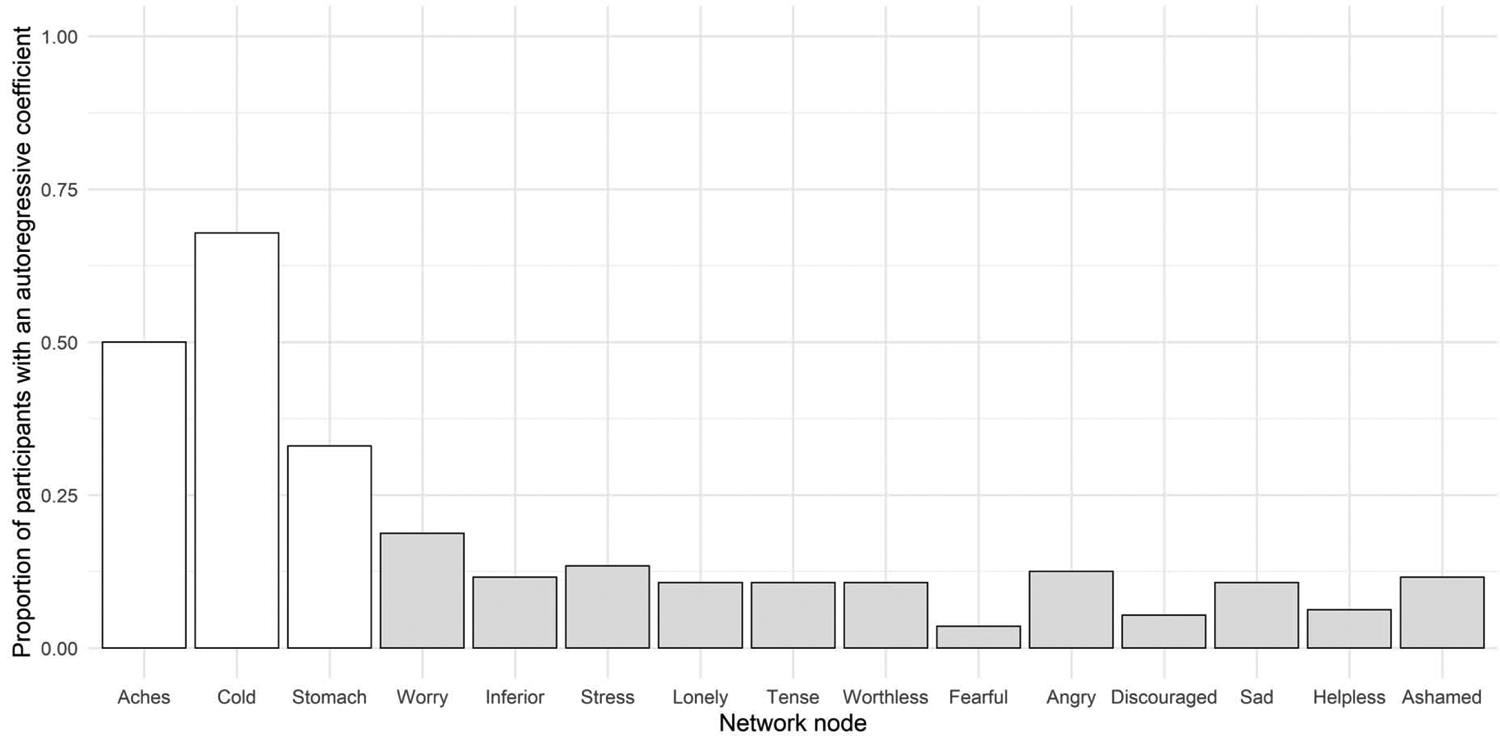
Proportion of participants (out of N=112) that had an autoregressive relation for each of the 15 nodes (i.e., variables) included in the networks produced by GIMME-MS; physical health nodes are white, and neuroticism nodes are gray.
The directionality of relations between neuroticism and physical health was also examined. In general, participants had more (i.e., greater density of) health-to-neuroticism than neuroticism-to-health relations, t(109)=−3.25, p=.002, d=.34. Follow-up t-tests did not detect this difference in lagged relations, t(109)=−1.98, p=.061, d=.21, but did detect it for contemporaneous relations, t(109)=−3.04, p=.003, d=.36. The same pattern of results was observed when only the directionality of positive relations was considered.
Overall, participants’ networks contained an average of 2.99 (SD=2.36) neuroticism-to-health relations and 3.86 (SD=2.70) health-to-neuroticism relations. Figure 4B illustrates this directional effect at the individual level by showing a participant with a disproportionate amount of health-to-neuroticism relations compared to neuroticism-to-health, while Figure 4C shows a participant with the opposite pattern, indicating that directionality is heterogeneous.
Sex Differences in Relations Between Neuroticism and Physical Health
Regressions explored whether sex was linked to the density of directional relations between neuroticism and physical health, while controlling for mean daily neuroticism (M=2.32, SD=.58) and physical health (M=1.58, SD=.37); see Table 1. For neuroticism-to-health relations, the final model was not significant, F(3, 106)=.19, p=.905, R2=.005. Sex was not a significant predictor (p=.50, d=.15), nor were covariates. For health-to-neuroticism relations, the final model, F(3, 106)=2.79, p=.044, R2=.07, included a significant effect of sex (p=.005, d=.72), such that women had more health-to-neuroticism relations than men, and covariates were not significant. Follow-up analyses (see Table 1) indicated that the sex effect was significant (p=.004, d=.82), with a significant final model, F(3, 108)=3.14, p=.028, R2=.08, for lagged relations, but not for contemporaneous relations (p=.104, d=.42), with a non-significant final model, F(3, 108)=1.07, p=.367, R2=.03. The same pattern of results was observed when only positive relations were considered.
Table 1.
Coefficients from regression analyses examining sex differences in the density of neuroticism-to-health and health-to neuroticism relations, while controlling for mean neuroticism and physical health scores.
| Neuroti cism-to-Health | Health-to-N euroti cism | Health-to-N euroti cism Lagged | Health-to-N euroti cism Contemporaneous | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | B | SE | β | B | SE | β | B | SE | β | |
| Neuroticism | −.10 | .41 | −.03 | .06 | .46 | .01 | .05 | .31 | .02 | .01 | .24 | .002 |
| Health | −.07 | .66 | −.01 | −.52 | .73 | −.07 | −.66 | .49 | −.13 | .13 | .39 | .03 |
| Sex | −.39 | .58 | −.07 | −1.86 | .65 | −.28** | −1.19 | .44 | −.28** | −.57 | .35 | −.16 |
Note: Neuroticism represents mean daily neuroticism score; health represents mean daily physical health score; significant effects were followed-up with analyses examining the density of lagged and contemporaneous relations separately.
p<.05,
p<.01.
Links to General Personality
To explore links to Big Five personality traits, participants were categorized into two extreme groups based on whether they had a disproportional number of neuroticismto-health relations (n=16) or health-to-neuroticism relations (n=43). There were no group differences in agreeableness, t(57) = 1.75, p = .085, d = 0.51; extraversion, t(57) = 0.92, p = .362, d = 0.28; neuroticism, t(57) =1.21, p = .231, d = 0.38; or openness to experience, t(57) = −0.45, p = .658, d = 0.12. However, there was a group difference in conscientiousness, t(57) = 2.57, p = .013, d = 0.73, with participants who had relatively more health-to-neuroticism relations (M=3.88, SD=.47) being more conscientious than those who had relatively more neuroticism-to-health relations (M=3.51, SD=.55). When only positive relations were considered, the two groups were smaller (n=14 for disproportional neuroticism-to-health relations, and n=30 for disproportional health-to-neuroticism relations), but the same pattern of results was observed, with the effect size for the conscientiousness group difference reducing to d=.22.
Discussion
The primary goals of this study were to delineate the directionality and person-specificity of the day-to-day relations between neuroticism and physical symptoms using data from over a hundred participants in a 75-day intensive longitudinal study and a temporal network modelling approach (GIMME-MS). Sex differences and links to general personality were explored.
There were no group-level relations in the final networks produced by GIMME-MS, indicating substantial heterogeneity in the relations between neuroticism and health across participants. Heterogeneity was reflected in the individual-level relations, which were primarily positive in magnitude, yet several patterns emerged. For instance, participants had more autoregressive relations for physical symptoms than neuroticism, reflecting greater behavioral inertia (stability) for physical health. This is consistent with evidence for item-level and person-specific variation in personality (Hofmans, De Clercq, Kuppens, Verbeke, & Widiger, 2019; Molenaar & Campbell, 2009; Wright et al., 2019).
Moreover, the directionality of the individual-level relations between neuroticism and physical health was evaluated using network density (Rubinov & Sporns, 2010). On average, individuals displayed more relations from health to neuroticism than relations from neuroticism to health (even when only positive relations were considered). The vast majority of participants, however, had at least one relation in each direction. This set of findings highlights the heterogeneity among individuals and the unique constellation of neuroticism and physical health indicators for each person. Although the heterogeneity of individuals seems to be a more common assumption in clinical practice than in basic research (Millon & Grossman, 2007), the approach utilized here (i.e., merging intensive longitudinal data with person-specific analytic methods) exemplifies one way in which basic research can begin to inform personalized healthcare (Insel, 2014; Wright & Woods, 2020), that is, by showcasing how intraindividual variability provides novel information about symptomatology that is missed by averages or even individual deviations from averages. Furthermore, by operationalizing neuroticism with 12 items instead of a single score (based on a group-derived structure), this study has particular potential to provide insight into individual differences in the neuroticism-physical health link; for example, two people might have the same composite score of neuroticism for different reasons, with a score driven by “worried” for one person but “lonely” for another, and these indicators could underlie health in unique ways (see Wright & Woods, 2020).
To explore predictors of network characteristics, sex differences in both neuroticism-to-health and health-to-neuroticism relations were examined. Women were more likely than men to have health-to-neuroticism relations (even when only positive relations were considered), suggesting that their physical health had greater consequences for their neuroticism. This extends the extant literature (Barsky et al., 2001; Hyphantis et al., 2013) with respect to the direction of neuroticism and health and with respect to temporal variation, as the sex difference was particularly true for lagged relations (i.e., women’s physical health today predicts their negative feelings tomorrow). This is consistent with other work indicating that there is temporal carryover associated with emotion in girls and women more than boys and men (Beltz, Beekman, Molenaar, & Buss, 2013; Johnson & Whisman, 2013). It is important to note that sex differences in these patterns of relations (i.e., covariation) were not confounded by overall levels of physical health and neuroticism, which were non-significant covariates in the analyses.
Finally, exploratory analyses were conducted to examine whether the direction of relations between neuroticism and health characterized different “types” of participants. Participants were differentiated into two “extreme” groups depending on whether they had a disproportional number of neuroticism-to-health or health-to-neuroticism relations. Individuals with more health-to-neuroticism relations had greater conscientiousness, which aligns with meta-analytic work showing that neuroticism and conscientiousness are the Big Five factors with the strongest correlations with health (Strickhouser, Zell, & Krizan, 2017). The size of this finding was attenuated when only positive relations were considered, though, so it requires replication. Nonetheless, the exploratory sex and personality findings illustrate how analysis of within-person variation can be used to investigate research questions about between-person variation by classifying individuals based on their demographic or network features and examining group differences in cross-sectional measures.
Study Considerations
Findings should be interpreted with respect to study methods. First, this study focused on physical health symptoms in generally healthy adults without chronic illness. Future work should examine whether findings generalize to a patient population or to symptoms beyond colds, aches, and stomach pains; for example, there is evidence that neuroticism is uniquely correlated with tension (e.g., neck pain, migraine), but not colds (Johnson, 2003).
Second, results of temporal network mapping are likely dependent upon the measurement interval of 24 hours. It has been argued that the relation between neuroticism and physical health is weaker when reports are made daily versus across weeks (Larsen, 1992) or with an event-sampling approach (Brown & Moskowitz, 1997). Nonetheless, there is evidence for the importance of daily personality in the literature (Borkenau & Ostendorf, 1998; Wright & Simms, 2016). Moreover, the proportions of contemporaneous and lagged as well as positive and negative relations are likely related to the length of the measurement interval. For instance, there is reason to expect an increased number of lagged and negative relations when measurement intervals are small, reflecting the nature of both temporally dense time series and model fitting (Lütkepohl, 2005). Thus, researchers should strive to use the measurement interval that best captures the psychological process in question; future work is needed to determine what that interval is in the relation between neuroticism and health.
Third, there were more women than men in this sample, potentially raising concerns about the robustness of preliminary findings concerning sex differences. Although results are congruent with past research, it will be important for future work with balanced groups to examine the directionality of the neuroticism-health link.
Fourth, single items were used to index physical health and neuroticism. Although this may lead to concerns about reliability, it was done in an attempt to balance the pulls of an entirely idiographic (with personalized items, factors, and analyses) and entirely nomothetic (with common items, between-person factors, and group-level inferences) approach; specifically, it was nomothetic in that common items were used and group-level network relations were possible, but it was idiographic in that common factors were avoided and person-specific networks were generated. Thus, future studies might complement this one by taking either a more idiographic or a more nomothetic approach. For instance, researchers might employ the new latent variable version of GIMME (Gates, Fisher & Bollen, 2020) that allows for personalized variation in factor structures that undergo network mapping. This approach also has the potential to indicate whether some neuroticism and health items are best characterized as part of the same latent construct. Researchers might also employ the hybrid version of GIMME (based on Molenaar & Lo, 2016) that allows for exogenous bidirectional correlations among study variables.
Fifth, GIMME-MS is only one person-specific temporal network approach that could be used to address the question of directionality. There are others (e.g., graphical and multi-level VAR), but most do not consider the directionality of contemporaneous relations, arguing that links between concurrent measurements must be bidirectional (Epskamp et al., 2018). Because GIMME-MS simultaneously fits lagged and contemporaneous relations, though, it is possible to leverage the time-indexed nature of the data to at least identify the model (if a solution space is generated) that explains the most information (using the AIC). Simulations suggest this works well (Beltz & Molenaar, 2016), but inferences from GIMME-MS might change if other selection criteria were used.
Conclusion
This 75-day intensive longitudinal study and temporal network analyses conducted with GIMME-MS revealed that there is person-specific heterogeneity in the relations between aspects of neuroticism and physical health, but that physical health is more likely to influence neuroticism than neuroticism is to influence physical health, especially for next-day (i.e., lagged) effects in women. This work inspires future intensive longitudinal investigations of the person-specificity of personality and health and has downstream implications for personalized healthcare.
Highlights.
Over 100 person-specific networks were created from 75-day diary data
There was substantial heterogeneity in relations between neuroticism and health
Relations were in both directions, but health-to-neuroticism links were more common
Women had more health-to-neuroticism relations than men, predicting across days
Acknowledgments
Portions of this work were presented at the LIFE Academy in Zurich, Switzerland in October 2019. Adriene Beltz was supported by the Jacobs Foundation. Alexander Weigard was supported by NIAAA T32 AA007477 (to Frederic Blow). The authors thank the study participants and several people for their contributions to this project. Amy Loviska and members of the Methods, Sex differences, and Development - M(SD) - Lab at the University of Michigan helped with recruitment, testing, and data management. Zachary Fisher and Cara Arizmendi implemented GIMME-MS in R and assisted with the generation of Figure 3.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no competing interests to report.
References
- Almeida D (1998). Daily Inventory of Stressful Events (DISE) Expert Coding Manual. Tuscon, AZ: University of Arizona, Division of Family Studies and Human Development. [Google Scholar]
- Barsky AJ, Peekna HM, & Borus JF (2001). Somatic symptom reporting in women and men. Journal of General Internal Medicine, 16(4), 266–275. doi: 10.1046/j.1525-1497.2001.016004266.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beltz AM, Beekman C, Molenaar PC, & Buss KA (2013). Mapping temporal dynamics in social interactions with unified structural equation modeling: A description and demonstration revealing time-dependent sex differences in play behavior. Applied Developmental Science, 17(3), 152–168. doi: 10.1080/10888691.2013.805953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beltz AM, & Gates KM (2017). Network Mapping with GIMME. Multivariate Behavioral Research, 52(6), 789–804. doi: 10.1080/00273171.2017.1373014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beltz AM, & Molenaar PC (2016). Dealing with Multiple Solutions in Structural Vector Autoregressive Models. Multivariate Behavioral Research, 51(2–3), 357–373. doi: 10.1080/00273171.2016.1151333 [DOI] [PubMed] [Google Scholar]
- Beltz AM, Wright AG, Sprague BN, & Molenaar PC (2016). Bridging the Nomothetic and Idiographic Approaches to the Analysis of Clinical Data. Assessment, 23(4), 447–458. doi: 10.1177/1073191116648209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkenau P, & Ostendorf F (1998). The Big Five as states: How useful is the five-factor model to describe intraindividual variations over time? Journal of Research in Personality, 32(2), 202–221. doi: 10.1006/jrpe.1997.2206 [DOI] [Google Scholar]
- Brown KW, & Moskowitz DS (1997). Does unhappiness make you sick? The role of affect and neuroticism in the experience of common physical symptoms. Journal of Personality and Social Psychology, 72(4), 907. doi: 10.1037/0022-3514.72.4.907 [DOI] [PubMed] [Google Scholar]
- Brown TA (2014). Confirmatory Factor Analysis for Applied Research: Guilford Publications. [Google Scholar]
- Burkholder GJ, & Harlow LL (2003). An illustration of a longitudinal cross-lagged design for larger structural equation models. Structural Equation Modeling- A Multidisciplinary Journal, 10(3), 465–486. doi: 10.1207/S15328007sem1003_8 [DOI] [Google Scholar]
- Costa PT, & McCrae RR (1985a). Hypochondriasis, neuroticism, and aging: When are somatic complaints unfounded? American Psychologist, 40(1), 19. doi: 10.1037/0003-066x.40.1.19 [DOI] [PubMed] [Google Scholar]
- Costa PT, & McCrae RR (1985b). The NEO Personality Inventory. [Google Scholar]
- Costa PT, & McCrae RR (1987). Neuroticism, Somatic Complaints, and Disease: Is the Bark Worse than the Bite? Journal of Personality, 55(2), 299–316. doi: 10.1111/j.1467-6494.1987.tb00438.x [DOI] [PubMed] [Google Scholar]
- Dotterer HL, Beltz AM, Foster KT, Simms LJ, & Wright AG (2019). Personalized models of personality disorders: Using a temporal network method to understand symptomatology and daily functioning in a clinical sample. Psychological Medicine, 1–9. doi: 10.017/s0033291719002563 [DOI] [PubMed] [Google Scholar]
- Epskamp S, van Borkulo CD, van der Veen DC, Servaas MN, Isvoranu AM, Riese H, & Cramer AOJ (2018). Personalized Network Modeling in Psychopathology: The Importance of Contemporaneous and Temporal Connections. Clinical Psychological Science, 6(3), 416–427. doi: 10.1177/2167702617744325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman PJ, Cohen S, Doyle WJ, Skoner DP, & Gwaltney JM Jr. (1999). The impact of personality on the reporting of unfounded symptoms and illness. Journal of Personality and Social Psychology, 77(2), 370–378. doi: 10.1037//0022-3514.77.2.370 [DOI] [PubMed] [Google Scholar]
- Fleeson W (2001). Toward a structure- and process-integrated view of personality: Traits as density distributions of states. Journal of Personality and Social Psychology, 80(6), 1011–1027. doi: 10.1037/0022-3514.80.6.1011 [DOI] [PubMed] [Google Scholar]
- Foster KT, & Beltz AM (Under Review). Affective heterogeneity in men and women: Basic science and clinical implications for precision health.
- Gates K, Fisher ZF, & Bollen K (2020). Latent variable GIMME using model implied instrumental variables (MIIVs). Psychological Methods, 25(2), 227–242. doi: 10.1037/met0000229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates KM, & Molenaar PCM (2012). Group search algorithm recovers effective connectivity maps for individuals in homogeneous and heterogeneous samples. Neuroimage, 63(1), 310–319. doi: 10.1016/j.neuroimage.2012.06.026 [DOI] [PubMed] [Google Scholar]
- Hofmans J, De Clercq B, Kuppens P, Verbeke L, & Widiger TA (2019). Testing the Structure and Process of Personality Using Ambulatory Assessment Data: An Overview of Within-Person and Person-Specific Techniques. Psychological Assessment, 31(4), 432–443. doi: 10.1037/pas0000562 [DOI] [PubMed] [Google Scholar]
- Hyphantis T, Goulia P, & Carvalho AF (2013). Personality traits, defense mechanisms and hostility features associated with somatic symptom severity in both health and disease. Journal of Psychosomatic Research, 75(4), 362–369. doi: 10.1016/j.jpsychores.2013.08.014 [DOI] [PubMed] [Google Scholar]
- Insel TR (2014). The NIMH Research Domain Criteria (RDoC) Project: precision medicine for psychiatry. American Journal of Psychiatry, 171(4), 395–397. doi: 10.1176/appi.ajp.2014.14020138 [DOI] [PubMed] [Google Scholar]
- Johnson DP, & Whisman MA (2013). Gender differences in rumination: A meta-analysis. Personality and Individual Differences, 55(4), 367–374. doi: 10.1016/j.paid.2013.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M (2003). The vulnerability status of neuroticism: over-reporting or genuine complaints? Personality and Individual Differences, 35(4), 877–887. doi: 10.1016/s0191-8869(02)00303-3 [DOI] [Google Scholar]
- Jorm AF, Christensen H, Henderson S, Korten AE, MacKinnon AJ, & Scott R (1993). Neuroticism and Self-Reported Health in an Elderly Community Sample. Personality and Individual Differences, 15(5), 515–521. doi: 10.1016/0191-8869(93)90334-y [DOI] [Google Scholar]
- Kelly D, & Beltz AM (Under Review). Capturing fluctuations in gendred cognition with novel intensive longitudinal measures. [DOI] [PubMed] [Google Scholar]
- Kroenke K (2003). Patients presenting with somatic complaints: epidemiology, psychiatric co-morbidity and management. International Journal of Methods in Psychiatric Research, 12(1), 34–43. doi: 10.1002/mpr.140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB (2009). Public health significance of neuroticism. American Psychologist, 64(4), 241–256. doi: 10.1037/a0015309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane ST, Gates KM, Pike HK, Beltz AM, & Wright AGC (2019). Uncovering general, shared, and unique temporal patterns in ambulatory assessment data. Psychological Methods, 24(1), 480–488. doi: 10.1037/met0000192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Gillespie NA, Ye L, Zhu G, Duffy DL, & Martin NG (2018). The relationship between personality and somatic and psychological distress: A comparison of Chinese and Australian adolescents. Behavior Genetics, 48(4), 315–322. doi: 10.1007/s10519-018-9905-3 [DOI] [PubMed] [Google Scholar]
- Lütkepohl H (2005). New Introduction to Multiple Time Series Analysis. Berlin, Germany: Springer Science & Business Media. [Google Scholar]
- Millon T, & Grossman S (2007). Overcoming Resistant Personality Disorders. Wiley Online Library. [Google Scholar]
- Molenaar PCM (2004). A manifesto on psychology as idiographic science: Bringing the person back into scientific psychology, this time forever. Measurement: Interdisciplinary Research & Perspective, 2(4), 201–218. doi: 10.1207/s15366359mea0204_1 [DOI] [Google Scholar]
- Molenaar PCM, & Campbell CG (2009). The new person-specific paradigm in psychology. Current Directions in Psychological Science, 18(2), 112–117. doi: 10.1111/j.1467-8721.2009.01619.x [DOI] [Google Scholar]
- Molenaar PCM, & Lo LL (2016). Alternative forms of Granger causality, heterogeneity, and nonstationarity In Wiedermann W & von Eye A (Eds.), Statistics and Causality: Methods for Applied Empirical Research (pp. 205–230). Hoboken, NJ: John Wiley & Sons. doi: 10.1002/9781118947074.ch9 [DOI] [Google Scholar]
- Ode S, & Robinson MD (2007). Agreeableness and the self-regulation of negative affect: Findings involving the neuroticism/somatic distress relationship. Personality and Individual Differences, 43(8), 2137–2148. doi: 10.1016/j.paid.2007.06.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer DJ, & Benet-Martinez V (2006). Personality and the prediction of consequential outcomes. Annual Review of Psychology, 57, 401–421. doi: 10.1146/annurev.psych.57.102904.190127 [DOI] [PubMed] [Google Scholar]
- Parker JDA, Bagby RM, & Taylor GJ (1989). Toronto alexithymia scale, EPQ and self-report measures of somatic complaints. Personality and Individual Differences, 10(6), 599–604. doi: 10.1016/0191-8869(89)90219-5 [DOI] [Google Scholar]
- Pitts SR, Niska W, & Burt CW (2008). National hospital ambulatory medical care survey: 2006 emergency department summary. National Health Statistics Reports; No 7. [PubMed] [Google Scholar]
- Rosmalen JG, Neeleman J, Gans RO, & de Jonge P (2007). The association between neuroticism and self-reported common somatic symptoms in a population cohort. Journal of Psychosomatic Research, 62(3), 305–311. doi: 10.1016/j.jpsychores.2006.10.014 [DOI] [PubMed] [Google Scholar]
- Rubinov M, & Sporns O (2010). Complex network measures of brain connectivity: uses and interpretations. Neuroimage, 52(3), 1059–1069. doi: 10.1016/j.neuroimage.2009.10.003 [DOI] [PubMed] [Google Scholar]
- Selig JP, & Little TD (2012). Autoregressive and cross-lagged panel analysis for longitudinal data In Laursen B, Little TD, & Card NA (Eds.), Handbook of Developmental Research Methods (pp. 265–278). New York, NY: The Guilford Press. [Google Scholar]
- Sörbom D (1989). Model modification. Psychometrika, 54(3), 371–384. doi: 10.1007/Bf02294623 [DOI] [Google Scholar]
- Strickhouser JE, Zell E, & Krizan Z (2017). Does personality predict health and well-being? A metasynthesis. Health Psychology, 36(8), 797. doi: 10.1037/hea0000475.supp [DOI] [PubMed] [Google Scholar]
- Suls J, & Martin R (2005). The daily life of the garden-variety neurotic: reactivity, stressor exposure, mood spillover, and maladaptive coping. Journal of Personality, 73(6), 1485–1509. doi: 10.1111/j.1467-6494.2005.00356.x [DOI] [PubMed] [Google Scholar]
- ten Have M, Oldehinkel A, Vollebergh W, & Ormel J (2005). Does neuroticism explain variations in care service use for mental health problems in the general population? Social Psychiatry and Psychiatric Epidemiology, 40(6), 425–431. doi: 10.1007/s00127-005-0916-z [DOI] [PubMed] [Google Scholar]
- Timmers C, Maeghs A, Vestjens M, Bonnemayer C, Hamers H, & Blokland A (2014). Ambulant cognitive assessment using a smartphone. Applied Neuropsychology: Adult, 21(2), 136–142. doi: 10.1080/09084282.2013.778261 [DOI] [PubMed] [Google Scholar]
- Trull TJ, & Ebner-Priemer U (2013). Ambulatory assessment. Annual Review of Clinical Psychology, 9, 151–176. doi: 10.1146/annurev-clinpsy-050212-185510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano NA, Pitzer L, Armour C, Karlamangla A, Ryff CD, & Mroczek DK (2011). Personality trait level and change as predictors of health outcomes: Findings from a national study of Americans (MIDUS). Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 67(1), 4–12. doi: 10.1093/geronb/gbr072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Eye A, & Bogat GA (2006). Person-oriented and variable-oriented research: Concepts, results, and development. Merrill-Palmer Quarterly, 52(3), 390–420. doi: 10.1353/mpq.2006.0032 [DOI] [Google Scholar]
- Watson D, & Pennebaker JW (1989). Health complaints, stress, and distress: Exploring the central role of negative affectivity. Psychological Review, 96(2), 234–254. doi: 10.1037//0033-295x.96.2.234 [DOI] [PubMed] [Google Scholar]
- Weigard A, Beltz AM, Reddy SN, & Wilson SJ (2019). Characterizing the role of the pre-SMA in the control of speed/accuracy trade-off with directed functional connectivity mapping and multiple solution reduction. Human Brain Mapping, 40(6), 1829–1843. doi: 10.1002/hbm.24493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams PG, & Wiebe DJ (2000). Individual differences in self-assessed health: gender, neuroticism and physical symptom reports. Personality and Individual Differences, 28(5), 823–835. doi: 10.1016/s0191-8869(99)00140-3 [DOI] [Google Scholar]
- Wright AGC, & Simms LJ (2016). Stability and fluctuation of personality disorder features in daily life. Journal of Abnormal Psychology, 125(5), 641–656. doi: 10.1037/abn0000169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Gates KM, Arizmendi C, Lane ST, Woods WC, & Edershile EA (2019). Focusing personality assessment on the person: Modeling general, shared, and person specific processes in personality and psychopathology. Psychological Assessment, 31(4), 502–515. doi: 10.1037/pas0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, & Woods WC (2020). Personalized models of psychopathology. Annual Review of Clinical Psychology, 16(1). doi: 10.1146/annurev-clinpsy-102419-125032 [DOI] [PubMed] [Google Scholar]