Abstract
African-American (AA) women are at higher risk of breast cancer mortality than women of other races. Factors influencing breast cancer risk, including exogenous environmental exposures, and debate around timing of exposure and dose-response relationship, can cause misunderstanding. Collaboration with priority populations encourages culturally relevant health messaging that imparts source reliability, influences message adoption, and improves understanding. Through six focus groups with AA individuals in rural and urban counties in the southeastern United States, this study used a community-engaged participatory approach to design an innovative visual tool for disseminating breast cancer information. Results demonstrated that participants were generally aware of environmental breast cancer risks and were willing to share new knowledge with families and community members. Recommended communication channels included pastors, healthcare providers, social media, and the Internet. Participants agreed that a collaboratively designed visual tool serves as a tangible, focused “conversation starter” to promote community prevention and education efforts.
Keywords: environmental health, breast cancer, focus groups, community engagement, health communication, visual communication
Background
In the United States, African-American (AA) women are more likely to die from breast cancer and present with later stage disease than women of other races.1–3 Many factors contribute to racial disparities in health outcomes, including social and economic injustice, health literacy, cultural norms, beliefs and perceptions about health, access to information and care, genetic predisposition, and environmental factors.4–9 AA populations have historically experienced environmental injustice, influenced by a variety of causes, including residential segregation and socioeconomic status.9–11 Nguyen et al. found significant racial disparities in chemical biomarker concentrations for a variety of environmental exposures including pesticides and personal care and consumer compounds, suggesting increased exposure to environmental breast cancer risks for minority populations.10 While, there are several known environmental risks for breast cancer, the state of the science is constantly evolving and information regarding these risks can be confusing, especially where there is debate regarding the degree and timing of exposure for environmental risks for breast cancer,2,3,10,12–23 which may result in misperception of risk within the general public.7,11–13,24
Research suggests that women perceive a variety of environmental exposures as risk factors for cancer,25 and specifically for breast cancer,24 despite uncertainty about causation. However, the literature regarding specific community-held perceptions of environmental risks for breast cancer is sparse. Additionally, information on environmental risks contains a mixture of evidenced-based facts and sensationalized details designed to sell commercial products,12 making it difficult for consumers to separate scientific evidence from hype. Environmental factors also have the advantage of being more readily modifiable compared to other breast cancer risk factors (e.g., reproductive factors). Given cancer-related health disparities and significantly higher mortality burden among AA women, understanding their perceptions of environmental risk can aid in the development of targeted prevention efforts that are both sensitive to and informed by community-held knowledge. To address this issue, we conducted focus groups with AA women in two counties in a southeastern state in the United States. For the purpose of this study, environmental risks refer to exogenous exposures to chemicals or physical agents.3
Community Co-Development of Effective Health Messaging
Where there is uncertainty in the science, the United States Interagency Breast Cancer and Environmental Research Coordinating Committee (IBCERCC) recommends a “precautionary approach” to complex risk communication that relies on the “weight of the evidence”, explores alternatives to potential harms, and employs a participatory process for community decision-making.3 Findings from an analysis of online information on environmental contaminants as risk factors for breast cancer demonstrated that the majority of Internet resources lacked cultural sensitivity26 and were written at or above a high school reading grade level, which is beyond the reading level of the general population and limits universal understanding of environmental information that enables engagement in appropriate preventive behaviors.12,27 Environmental health literacy involves a “wide range of skills and competencies that people need to seek out, comprehend, evaluate, and use environmental health information to make informed choices, reduce health risks, improve quality of life, and protect the environment”. Research suggests that environmental health literacy is a continuum that begins with individual knowledge of specific environmental exposure risks and their connection to human health, as well as the strategies to reduce or eliminate these exposures, for preventive decision making that can extend to the greater community.28 In addition, qualitative exploration of AA perceptions of environmental risks for breast cancer and related health communication demonstrates community-held cultural mistrust in medical information messages.11,13 Cancer messages co-developed with community members can improve comprehension, environmental health literacy, and cultural suitability, and promote trust between researchers and communities for the successful translation of scientific research and adoption of health messaging.2,13,29,30
Visual Storytelling and Message Adoption
Focus group findings from our larger study revealed that participants desired printed, culturally sensitive, visual breast cancer materials that they could easily reference or display at community gatherings and events.13 Research suggests that storytelling is an effective tool for health communication as it plays a role in education and modeling behavior.31,32 Visual storytelling can help familiarize complex information, which may increase audience engagement and reduce message resistance.31 Literature also indicates that graphic communication can improve efficiency in message receipt and memory through cognitive and emotional connection with the information and can increase message adoption where culturally representative images are used.33 Visual tools aim to elicit personal interpretations that prompt further discussion relative to the knowledge, beliefs, and attitudes that influence perceptions.34
Purpose of Study
Participatory development of a visual tool for topical health communication entails discussion with a community regarding needs and preferences in order to generate shared understanding and shared vision that accounts for cultural and historical influences on community perception and understanding.34 The purpose of this study was to develop a culturally relevant visual health communication tool for AA community members in South Carolina that would focus community discussions about environmental risks for breast cancer and preferred communication sources and channels.
Methods
Data Collection
Data were collected through six audio-recorded focus groups with AA community members in both an urban and a rural county in a southeastern state in the United States. Focus groups lasted 45–90 minutes and were conducted in a round-table format. Session attendance ranged from 6–15 participants, 2–3 researchers, and 1–2 community partners. These semi-structured sessions utilized open-ended questions to allow participants to share their perceptions of environmental risks for breast cancer. Participant recruitment was conducted in close collaboration with community and faith-based partners using purposive and convenience sampling techniques.35 Recruitment methods included distribution of flyers and printed posters in public spaces, local radio advertisements, and in-person or phone contact with participants referred directly by partners or other participants via word-of-mouth. More detailed methodology as part of our larger qualitative study is published elsewhere.13 This study was approved by the University’s institutional review board.
Prototype Development
A visual tool was developed to communicate environmental risk factors for breast cancer based on the findings from the initial set of focus group discussions in both counties.13 Thematic analysis identified commonly discussed, perceived environmental risks for breast cancer as well as preferred communication sources and channels for health messaging. A draft of the visual was presented to participants during the second set of focus group sessions, in which researchers elicited feedback on the prototype imagery as well as the language and format. The final version was distributed to individuals attending the third focus group session, and copies were provided in bulk to key community members for distribution at local events such as health fairs. Both draft and final version are presented in Figures 1 and 2.
Figure 1.
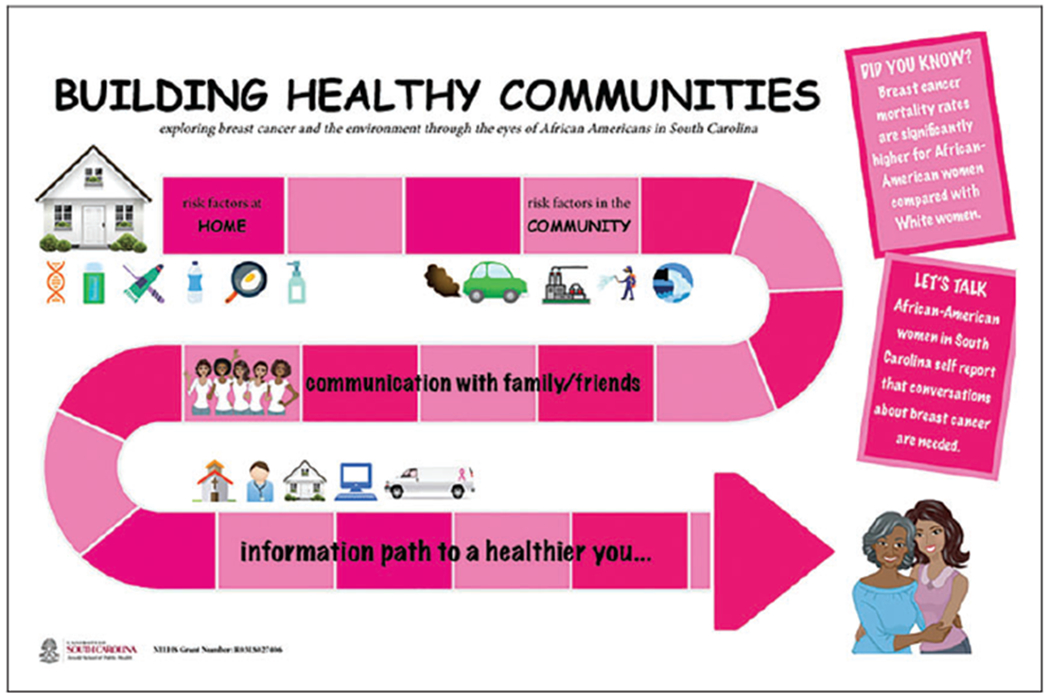
Draft of Visual Tool, “Building Healthy Communities.”
Figure 2.
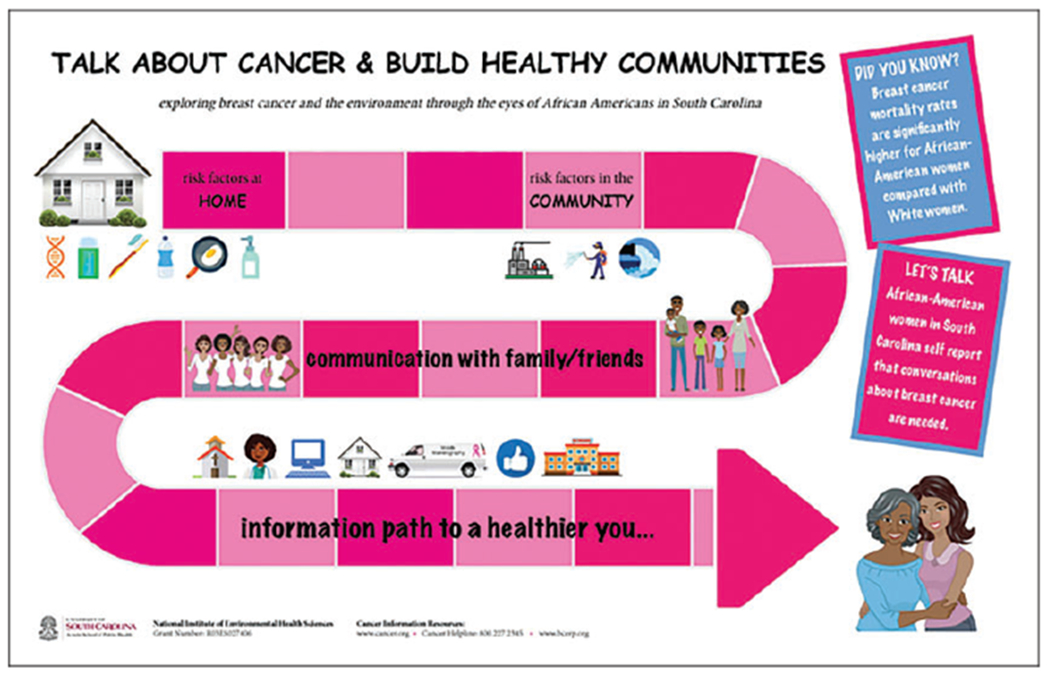
Final Visual Tool, “Talk About Cancer and Build Healthy Communities.”
Participant Survey
Participants were administered a survey at the end of the third focus group to determine their intention to communicate more with others regarding environmental risks for breast cancer. Participants were asked how likely they were to: 1) communicate more with friends and family about breast cancer and the environment; 2) communicate more with the broader community about breast cancer and the environment; 3) access community resources (churches, schools, health fairs, etc.) to obtain breast cancer information; 4) encourage others to learn about breast cancer and the environment; 5) share the visual tool as a way to communicate about environmental risks of breast cancer. Likert-scale responses ranged from 1 (not at all likely) to 5 (greatest extent likely).
Results
To better understand community specific needs, we conducted multiple focus groups with members of our priority population in both an urban and a rural county in South Carolina. Participants (n=50) were 98% AA (n=49) and female (n=49), with a mean age of 49.4 years old (±13.8). All participants were residents of the counties where the focus groups took place, and thus did not commute from elsewhere. Of the study population, 16% reported an annual household income of $50,000 or more, with 32% reporting earnings of less than $10,000 per year. Regarding education level, 8% of participants had an advanced degree, 14% had an undergraduate degree, 38% had some college experience, 28% had a high school diploma or GED, and 6% had less than a high school level of education.
Starting the Conversation
A common theme that emerged during the first set of focus groups was that conversations about breast cancer should begin at home and should involve multiple generations of women. As one participant stated, “… I say it’s lack of education cause I mean, you know, you’re gonna take the time to do certain things and breast cancer you’re not gonna talk about cause it hasn’t hit home yet. You’re not gonna talk about something that’s not close to home.” Other participants added that discussion about breast cancer risk is not a conversation that is typically had within the AA community. This important concept prompted the development of the title for the visual: “Talk About Cancer and Build Healthy Communities”.
Community Perceptions of Environmental Risk Factors
Perceptions of environmental risks for breast cancer were elicited via open-eneded questions and furthering prompts, as detailed in our larger study.13 The most commonly identified risks mentioned by focus group participants were aluminum (as found in deodorant) and plastics, with specific emphasis on bisphenol A (BPA). Exposure to pesticides, air, and water pollution were each mentioned, but with lesser frequency.13 Perceptions of breast cancer risks from exposure to plastics, pesticides, and water pollution were congruent with the current state of the science.14–21 There are currently no confirmed associations with aluminum in deodorant and breast cancer23; however, findings related to air pollution demonstrate a potential correlation, but evidence is limited.17–20 In addition, our focus group findings showed that participants held similar perceptions regarding types of environmental risks, but there was little to no discussion regarding the degree to which each factor posed a risk for breast cancer. Identified sites of exposure included the household (genetics, plastic products, cookware, personal care products) and the broader community (outdoor pollution, pesticides). Congruent with the literature, study participants reported preference for printed, culturally sensitive plain language materials with graphics that they could display or keep for future reference.13 Preferred messaging sources included friends, family, health care providers, pastors, and other community members. Additional resources for messaging included the church, schools, the Internet, and social media. Based on these findings a visual prototype was developed.
Community Review of Visual Prototype
During the second set of focus group sessions, participants reviewed the prototype and provided feedback. General feedback from both counties included using pink as the dominant color, as it is symbolic for breast cancer awareness, but to also add blue to appeal to a wider audience. They also suggested inclusion of web addresses and contact information for national and partner breast cancer information sources (such as the American Cancer Society, the Breast Cancer and the Environment Research Program, and the National Institute for Environmental Health Sciences). Participants indicated that the final version of the visual captured the content from the first round of discussions, and they noted that it was simple and easy to understand. They felt that some of the icons relating to household products could be made more clear and relevant (toothbrush/toothpaste), and they suggested that men’s pictures should also be included to represent the importance of including all family members in discussions about cancer. Participants asked to see representation of BPA in the icons, which was later included as a water bottle graphic, and they suggested inclusion of images of survivors. Regarding communication, images of phones and social media were recommended, and participants agreed to use the social media symbol to represent both. Several participants actively use the Internet and acknowledged that depicting social media and the Internet is important in order to reach more members of the community, including a younger generation, who are more likely to use these resources for information exchange. They also recommended a prominent image that highlighted free mammograms (mobile mammography units), as several women mentioned that they would actively seek these mobile services for ease of access to screening. It was also noted that the physician graphic should be culturally appropriate.
Talking About Breast Cancer With the Broader Community
Results from the intention survey indicated that close to 90% of participants planned to communicate more with friends and family about breast cancer and the environment to a great extent or to the greatest extent. Regarding intention to communicate more with the broader community about breast cancer and the environment, close to 85% agreed to a great extent or to the greatest extent. Similarly, close to 90% agreed that they planned to access community resources (churches, schools, health fairs, etc.) to obtain breast cancer information. When asked if they planned to encourage others to learn about breast cancer and the environment, close to 94% agreed to a great or to the greatest extent, and close to 85% agreed that they would utilize the visual tool as a way to communicate about environmental risks of breast cancer. Participants offered to share the tool at health fairs, public libraries, and at local events during Breast Cancer Awareness Month. These findings suggest that participants are willing to communicate with friends, family, and members of their communities and churches about environmental risks for breast cancer, and that they are willing to share and use the visual tool as the conversation starter. The preference for communication through faith-based communities mirrors findings from other participatory cancer research with the AA community.6,36
Discussion
Sharing research findings with communities is both ethical and necessary,3,29,30 and thus the research process must include partnership in the development and dissemination of health messaging to ensure cultural relevance and sensitivity, encourage message adoption, and impart source reliability.2,8,13,30,36 Collaborative development of health communication materials also has the potential to better engage and inform the priority population by increasing community buy-in, situating new material within cultural and historical narratives, and improving efficiency and reach of message dissemination.13,26
Encouraging Conversation and Increasing Knowledge
As evidenced by participants’ responses regarding a lack of discussion about breast cancer within their communities, limited knowledge about genetic predisposition and elevated risk, coupled with community norms, may serve to limit conversation that could increase prevention efforts.13 Our study indicated that dissemination of the finalized visual tool with participants both helped to solidify their knowledge and acknowledge their contributions, and provided them with a tool to facilitate communication with other family and community members. Through the use of visual storytelling and collaborative development of a narrative that represents the knowledge, shared values, and preferences of the community, this tool can serve as an effective means of increasing knowledge of breast cancer risk across generations. The use of this visual also considers the health literacy spectrum and preexisting knowledge regarding breast cancer, enabling all members of the community to join the conversation and contribute to community-wide movement along the environmental health literacy continuum.28
Recommendations for a Community-Engaged Approach
Designing materials for communicating environmental breast cancer risk with specific populations should also incorporate community-held perceptions, visual and formatting preferences, appropriate graphic representations, and referral to reliable information sources.13,26,33,34,36 Our study demonstrated that community-engaged research strategies are effective means of gauging community perspectives, preferences, and knowledge of breast cancer risk within a priority demographic.13 Focus group responses indicated that community members shared perceptions of similar environmental risks for breast cancer and highlighted gaps in knowledge regarding degree of risk and timing of exposure. Identification of these gaps provides critical insight into the education needs of this population and informs health promotion efforts where community understanding is sufficient.
Study Limitations
This study has some limitations in that only AA community members from two counties were recruited. Generalizability to the AA population or to other demographics is not guaranteed. In addition, this visual tool combined perspectives from two geographic populations, so specificity was somewhat limited. While many participants attended all three sessions, there were new members in attendance during the third session. It is important to note that new members also found the visual compelling. Regarding specific imagery, there were some graphic suggestions that were not incorporated, such as coffins to represent cancer mortality, as this tool was focused on prevention messaging. We did not measure intention to communicate with others about environmental risks for breast cancer prior to the focus groups, thus our findings rely on participants’ self-reported intentions to “communicate more” with others via the follow-up survey. Despite these limitations, our study suggests that collaborative development of a novel, visual narrative tool can help improve education and increase community awareness and participation in breast cancer prevention efforts.
Implications for Practice and Research
As environmental exposures can differ based on geographic location, future participatory research with AA communities may warrant development of location specific visual scenarios. These can also include more specific communication channels, local historical or cultural iconography, and visual representation of specific solutions or replacement behaviors that may reduce individual exposures to environmental breast cancer risk factors. In addition, participants reported preference for receiving health messages from family, friends, pastors and other community members and resources, which reflects similar research demonstrating a preference for interpersonal and faith-based sources within the AA community.6,7 Future study of the accuracy of information received from these identified sources is warranted, and it is important to continue to engage these sources in education about environmental risks of breast cancer so that communities are receiving accurate and reliable messages. Similar to previous research with our priority population regarding communication of environmental health messaging, our study demonstrated that knowledge of community-specific message delivery and communication source/channel preferences can greatly improve prevention and education efforts by reducing barriers to message receipt and utilizing the existing pillars of the community for promoting trust and increasing health message adoption.2,13,30
Acknowledgment
We are grateful to our community partners and focus group participants.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Breast Cancer and the Environment Research Program (BCERP) through the National Institute of Environmental Health Sciences [grant number RO3ES027406]; and the South Carolina Cancer Prevention and Control Research Network (SC-CPCRN) [Cooperative Agreement Number U48/DP005000-01S2] from the Centers for Disease Control and Prevention (Prevention Research Centers) and the National Cancer Institute.
Biographies
Author Biographies
Brooks Yelton, MA, MSW, is a graduate of the College of Social Work and served as a Graduate Research Assistant for the South Carolina Cancer Prevention and Control Research Network at the University of South Carolina in Columbia, SC.
Heather M. Brandt, PhD, CHES, is a Professor in the Department of Health Promotion, Education, and Behavior, core faculty of the Statewide Cancer Prevention and Control Program, and Associate Dean in The Graduate School at the University of South Carolina in Columbia, SC.
Swann Arp Adams, PhD, is a Professor in the Department of Epidemiology and Biostatistics and College of Nursing and core faculty of the Statewide Cancer Prevention and Control Program at the University of South Carolina in Columbia, SC.
John R. Ureda, DrPH, is CEO of Insights Consulting, Inc. in Columbia, SC.
Jamie R. Lead, PhD, is a Professor in the Department of Environmental Health Sciences and Director of the Center for Environmental Nanoscience and Risk at the University of South Carolina, in Columbia, SC.
Delores Fedrick, BS, is a retired pharmacist and Director of the Chester County Literacy Council in Chester, SC.
Kaleea Lewis, PhD, is a Postdoctoral Fellow in the Department of Health Sciences at the University of Missouri in Columbia, MO.
Shibani Kulkarni, PhD, is a Doctoral Graduate of the Department of Health Promotion, Education, and Behavior at the University of South Carolina in Columbia, SC.
Daniela B. Friedman, PhD, is Professor and Chair in the Department of Health Promotion, Education, and Behavior and core faculty member of the Statewide Cancer Prevention and Control Program at the University of South Carolina in Columbia, SC.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Siegel RL, Miller KD and Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019; 69: 7–34. [DOI] [PubMed] [Google Scholar]
- 2.Williams DR, Mohammed SA and Shields AE. Understanding and effectively addressing breast cancer in African American women: unpacking the social context. Cancer 2016; 122: 2138–2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Interagency Breast Cancer and Environmental Research Coordinating Committee. Breast cancer and the environment prioritizing prevention, www.niehs.nih.gov/about/assets/docs/ibcercc_full_508.pdf (2013, accessed 27 June 2020).
- 4.Rodgers KM, Udesky JO, Rudel RA, et al. Environmental chemicals and breast cancer: an updated review of epidemiological literature informed by biological mechanisms. Environ Res 2018; 160: 152–182. [DOI] [PubMed] [Google Scholar]
- 5.Dean LT, Gehlert S, Neuhouser ML, et al. Social factors matter in cancer risk and survivorship. Cancer Causes Control 2018; 29: 611–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harmon BE, Kim SH, Blake CE, et al. Health care information in African American churches. J Health Care Poor Underserv 2014; 25: 242–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hempstead B, Green C, Briant KJ, et al. Community empowerment partners (CEPs): a breast health education program for African-American women. J Commun Health 2018; 43: 833–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farr DE, Brandt HM, Comer KD, et al. Cancer research participation beliefs and behaviors of a southern Black population: a quantitative analysis of the role of structural factors in cancer research participation. J Cancer Educ 2015; 30: 522–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coughlin SS. Social determinants of breast cancer risk, stage, and survival. Breast Cancer Res Treat 2019; 177: 537–548. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen VK, Kahana A, Heidt J, et al. A comprehensive analysis of racial disparities in chemical biomarker concentrations in United States women, 1999–2014. Environ Int 2020; 137: 105496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrera MJ, Feinstein RT, Walker WJ, et al. Embedded mistrust then and now: findings of a focus group study on African American perspectives on breast cancer and its treatment. Crit Public Health 2016; 26: 455–465. [Google Scholar]
- 12.Kulkarni S, Lewis K, Adams SA, et al. A comprehensive analysis of how environmental risks of breast cancer are portrayed on the internet. Am J Health Educ 2018; 49: 222–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lewis K, Adams SA, Brandt HM, et al. “For lack of knowledge, our people will perish”: using focus group methodology to explore African-American communities’ perceptions of breast cancer and the environment. Environ Int 2018; 121: 111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seachrist DD, Bonk KW, Ho SM, et al. A review of the carcinogenic potential of bisphenol A. Reprod Toxicol 2016; 59: 167–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Romagnolo DF, Daniels KD, Grunwald JT, et al. Epigenetics of breast cancer: modifying role of environmental and bioactive food compounds. Mol Nutr Food Res 2016; 60: 1310–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gray JM, Rasanayagam S, Engel C, et al. State of the evidence 2017: an update on the connection between breast cancer and the environment. Environ Health 2017; 16: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brody JG, Moysich KB, Humblet O, et al. Environmental pollutants and breast cancer: epidemiologic studies. Cancer 2007; 109: 2667–2711. [DOI] [PubMed] [Google Scholar]
- 18.Maqbool F, Mostafalou S, Bahadar H, et al. Review of endocrine disorders associated with environmental toxicants and possible involved mechanisms. Life Sci 2016; 145: 265–273. [DOI] [PubMed] [Google Scholar]
- 19.Keramatinia A, Hassanipour S, Nazarzadeh M, et al. Correlation between nitrogen dioxide as an air pollution indicator and breast cancer: a systematic review and meta-analysis. Asian Pac J Cancer Prev 2016; 17: 419–424. [DOI] [PubMed] [Google Scholar]
- 20.White AJ, Bradshaw PT and Hamra GB. Air pollution and breast cancer: a review. Curr Epidemiol Rep 2018; 5: 92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu H-C, Cohn BA, Cirillo PM, et al. DDT exposure during pregnancy and DNA methylation alterations in female offspring in the child health and development study. Reproductive Toxicology. Epub ahead of print 26 February 2019. DOI: 10.1016/j.reprotox.2019.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allam MF. Breast cancer and deodorants/antiperspirants: a systematic review. Central Eur J Public Health 2016; 24: 245–247. [DOI] [PubMed] [Google Scholar]
- 23.Willhite CC, Karyakina NA, Yokel RA, et al. Systematic review of potential health risks posed by pharmaceutical, occupational and consumer exposures to metallic and nanoscale aluminum, aluminum oxides, aluminum hydroxide and its soluble salts. Crit Rev Toxicol 2014; 44: 1–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spector D, Mishel M, Skinner CS, et al. Breast cancer risk perception and lifestyle behaviors among White and Black women with a family history of the disease. Cancer Nurs 2009; 32: 299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Molina Y, Zimmermann K, Carnahan LR, et al. Rural women’s perceptions about cancer disparities and contributing factors: a call to communication. J Cancer Educ 2018; 33: 749–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Resnicow K, Baranowski T, Ahluwalia JS, et al. Cultural sensitivity in public health: defined and demystified. Ethnicity Dis 1999; 9: 10–21. [PubMed] [Google Scholar]
- 27.Cohen DJ, White S and Cohen SB. Mind the gap: the Black-White literacy gap in the national assessment of adult literacy and its implications. J Lit Res 2012; 44: 123–148. [Google Scholar]
- 28.Gray KM. From content knowledge to community change: a review of representations of environmental health literacy. Int J Environ Res Public Health 2018; 15: 466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Claudio L, Gilmore J, Roy M, et al. Communicating environmental exposure results and health information in a community-based participatory research study. BMC Public Health 2018; 18: 784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Friedman DB, Toumey C, Porter DE, et al. Communicating with the public about environmental health risks: a community-engaged approach to dialogue about metal speciation and toxicity. Environ Int 2015; 74: 9–12. [DOI] [PubMed] [Google Scholar]
- 31.Krakow M Graphic narratives and cancer prevention: a case study of an American Cancer Society comic book. Health Commun 2017; 32: 525–528. [DOI] [PubMed] [Google Scholar]
- 32.Kreuter MW, Skinner CS, Steger-May K, et al. Responses to behaviorally vs culturally tailored cancer communication among African American women. Am J Health Behav 2004; 28: 195–207. [DOI] [PubMed] [Google Scholar]
- 33.King AJ. A content analysis of visual cancer information: prevalence and use of photographs and illustrations in printed health materials. Health Commun 2015; 30: 722–731. [DOI] [PubMed] [Google Scholar]
- 34.Ureda JR, Byrd TL, Calderón-Mora JA, et al. The use of illustrated story mapping to enhance focus group discussion. Health Promot Pract 2011; 12: 74–78. [DOI] [PubMed] [Google Scholar]
- 35.Corbin J and Strauss A (2008). Basics of qualitative research (3rd ed.): techniques and procedures for developing grounded theory. Thousand Oaks, CA: SAGE Publications Inc. [Google Scholar]
- 36.Jackson DD, Owens OL, Friedman DB, et al. Innovative and community-guided evaluation and dissemination of a prostate cancer education program for African-American men and women. J Cancer Educ 2015; 30: 779–785. [DOI] [PMC free article] [PubMed] [Google Scholar]


