Abstract
Purpose
To investigate (i) the frequency and natural evolution of meniscal ramp lesions (MRLs) on MRI in subjects with acute ACL-tear and (ii) to compare knee cartilage compositional degeneration between subjects with MRLs and subjects without meniscal pathology over 2 years.
Materials and Methods
Fifty-seven subjects with ACL tears (32 females; age 32.6±8.3y; BMI 24.5±3.5kg/m2) from a prospective study were screened for the presence of MRLs. Morphological (high-resolution 3D fast spin-echo) and compositional (T1ρ and T2-mapping) MRI was performed prior to and 2-years after ACL-reconstruction. Follow-up MR images were assessed for changes in the signal-intensity of the MRLs and the presence of meniscal tears. Differences of compositional parameters were compared between subjects with MRLs and without meniscal lesions using an Independent Samples t Tests.
Results
MRLs were found in 16% (9/56) of the subjects with ACL tears at baseline. Only one subject with MRLs developed a posterior horn meniscal tear over 2 years. In 12 knees no meniscal tears were found, which were defined as controls. Most interestingly, cartilage ΔT1ρ of the medial femur and medial tibia increased significantly more in subjects with MRLs compared to controls (mean difference, MF=6.0±0.8 vs. 2.3±0.6, p=0.004 and MT=4.4±1.4 vs. 0.4±0.6, p=0.027) and medial femur ΔT2 over 2 years increased significantly more in MRL than in control knees (5.1±2.5 ms vs. 2.2±1.9 ms, p=0.012).
Conclusion
Subjects with ACL-tear presented MRLs in 16% of cases. Compared to controls without meniscal lesions knees with MRLs demonstrated accelerated degeneration of cartilage composition in the medial knee compartment over 2-years.
Introduction
Patients with tears of the anterior cruciate ligament (ACL) have frequently concomitant intra-articular lesions (1,2) and almost 45% of all ACL-ruptured patients present with an associated meniscal injury (3). Strobel (4) described a specific type of meniscal lesion associated with ACL rupture involving the peripheral attachment of the posterior horn of the medial meniscus. Currently known as a meniscal ramp lesion (MRL), this abnormality was defined as a tear of the peripheral menisco-capsular attachment of the posterior horn of the medial meniscus (5,6) and its incidence has been reported in 16% to 40% of all knees with ACL tears (7,8).
Magnetic resonance imaging (MRI) is the diagnostic modality of choice for imaging of an ACL tears and also demonstrates MRLs preoperatively. A recent systematic review and meta-analysis demonstrated that MRI has a moderate sensitivity (0.71) and excellent specificity (0.94) for the diagnosis of MRLs in comparison with arthroscopy (9). Recently MRLs have received renewed interest in the orthopedic and radiological literature (10–13) for several reasons: (i) MRLs can cause knee instability with anterior translation and external rotational laxity (14), (ii) secondary meniscal injury may occur with progressive tearing tear and finally (iii) patients also have an increased risk for developing osteoarthritis. Although the need for surgical repair of MRLs is debatable (15,16), the identification and repair of the MRLs are important as ACL reconstructions without MRLs repair may fail to restore normal joint kinematics (14,17).
Therefore, the purpose of our study was to investigate the frequency and natural evolution of MRLs on MR imaging in patients with acute ACL tears over a period of 24 months. We also aimed to compare knee structural and cartilage degeneration over 24 months between patients with ACL-tears in combination with MRLs and controls with ACL-tears without meniscal abnormalities.
Material and Methods
Patient Cohort
Patients with complete traumatic acute ACL tear (N=57; 32 females; age 32.6±8.3y; BMI 24.5±3.5kg/m2) from a prospective study investigating the impact of ACL-tears on cartilage and joint degeneration were included in this project. Our institutional review board approved this study and all subjects gave written informed consent. We included subjects with clinically diagnosed acute ACL tear, confirmed by pre-operative MRI, who underwent ACL reconstruction as well as standard pre- and post-operative rehabilitation (18). Inclusion criteria also included availability of baseline and follow-up MRIs without artifacts or other technical deficiencies limiting image evaluation and arthroscopic surgery performed within 3 months after injury. The exclusion criteria were history of osteoarthritis, inflammatory disease, previous severe injury and surgery and additional injuries of the knee during the follow-up period. All subjects underwent knee MR imaging at baseline (prior to the surgery) and 2-years after surgery.
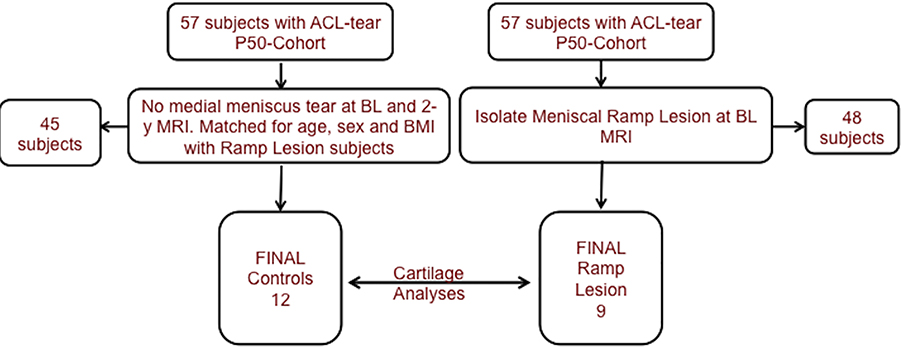
Twelve subjects frequency matched for age, sex and BMI from this cohort with ACL-tears and without medial meniscal abnormalities at baseline (confirmed by baseline MRI and during the arthroscopic surgery) and follow-up MRI were selected as controls while 9 patients with MRLs diagnosed in the baseline MRI served as case cohort. All subjects underwent arthroscopic surgery and ACL reconstruction with standard-of-care anatomic reconstruction of the ACL performed after injury. The subject selection process is shown in Figure 1.
Figure 1:
Selection of study participants. Flow chart illustrating patient selection for the present study from the overall P50 cohort. (ACL= anterior cruciate ligament; BL=baseline; BMI = body mass index; MRI=Magnetic Resonance Imaging)
MRI and Image Analysis
MRI examinations were acquired using the same 3T GE Signa MR scanner (General Electric Healthcare, Milwaukee, WI) with a 1Tx/8Rx knee coil and the imaging protocol included a high-resolution 3D fast spin-echo (CUBE) sequence and T1ρ and T2 relaxation time sequences. The detailed MR acquisition parameters are summarized in Table 1.
Table 1: Morphologic and compositional MRI pulse sequence parameters.
Morphologic and compositional MRI pulse sequence parameters. TR (repetition time); TE (echo time); BW (bandwidth) ETL (echo train length); NEX (number of excitations); FOV (field of view); Add opt (additional option); Fat Sat (fat saturation); PD (proton density); TRF (tailored radio frequency pulse); TSL (time of spin lock); FSL (frequency of spin lock).
| TR (ms) | TE (ms) | BW (kHz) | ETL | NEX | FOV (cm) | Matrix | Slice/Ga p (mm) | Add opt/parameters | |
|---|---|---|---|---|---|---|---|---|---|
| Sagittal Fat Sat 3D FSE | 1500 | 23 | 50 | 32 | 2 | 16 | 384×384 | 1/NA | Fat Sat |
| Sagittal PD | 5100 | 30 | 62.5 | 13 | 1-2 | 16 | 512×480 | 3.5/0 | TRF |
| Coronal PD | 5100 | 30 | 62.50 | 13 | 1 | 14 | 512×416 | 3.5/0 | TRF |
| 3D Tip | 9.3 | 3.7 | - | - | - | 14 | 256×192 | 4 mm | TSL (ms): 0, 10, 40 80 FSL (Hz): 500 |
| 3DT2 | 9.3 | 3.7 | - | - | - | 14 | 256x192 | 4 mm | Preparation TE (ms): 2.9, 13.6, 24.3, 45.6 |
Baseline and 2-year follow-up MRIs were available for all subjects in this study. All exams were independently evaluated for presence of MRLs by two radiologists (two board-certified radiologists with 6 years (LF) and 9 years (JG) of experience). In case of divergent findings, an adjudication reading with a senior MSK radiologist 24 years of experience (TL) was performed.
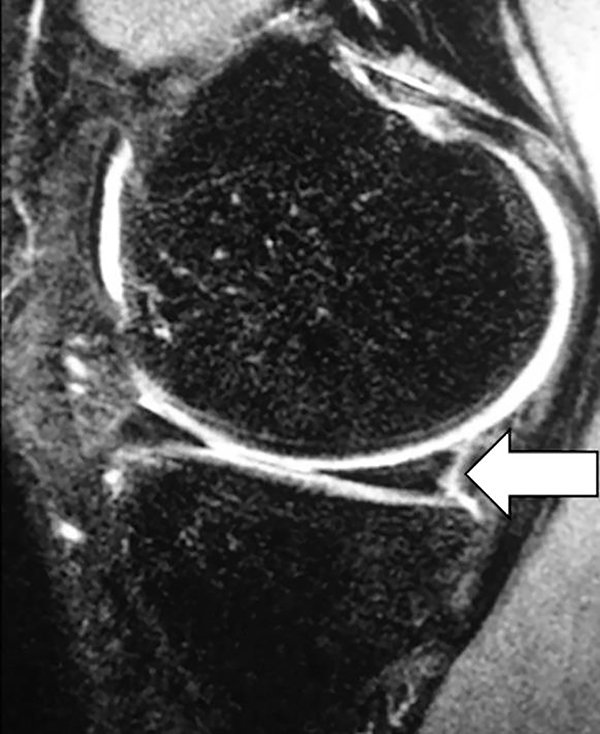
A MRL was defined on MRI (19) as a complete thin, linear lesion interposed between the posterior horn of the medial meniscus (PHMM) and the posteromedial capsule with intra-substantially located abnormally high fluid signal on fluid-sensitive sequences (posterior medial meniscocapsular separation) (Figure 1). Incomplete fluid interposition between the PHMM and the capsule was not counted as a complete MRL and not included in the case cohort.
Follow-up scans after two years in both cases and controls were assessed for longitudinal changes in signal-intensity of the MRLs and the presence / development of medial meniscal tears. The readers were blinded to baseline findings and the follow-up MRIs were read at least one month after the baseline MRI, to minimize any recall bias from previous analyses. High meniscal signal intensity was classified as a meniscal tear if it communicated with the superior, inferior or free edge of the meniscal surface on at least two consecutive images or two different planes (20).
After the meniscal abnormalities at different time points were registered, the intensities of the meniscal ramp lesion signal at the different time points were compared both at baseline and 24-month follow-up. A visual side-by-side comparison was used in order to describe whether the signal intensity decreased or remained stable (fluid-signal) over time.
Cartilage Compositional Analysis
The medial compartment cartilage was segmented on the 3D-FSE sequences using a semi-automatic Matlab-based algorithm developed at our institution (21) at baseline and 2 years after surgery in both case and control cohorts. Segmentations were registered to the T1ρ and T2 maps accounting for non-rigid movement. T1ρ and T2 maps were reconstructed by fitting the echo images pixel by pixel to the following equations: S(TSL)∞ S0exp(-TSL/T1ρ) for T1ρ and S(TE) ∞ S0exp(-TE/T2) for T2, where TSL is the time of spin lock, TE is the echo time, and S is the signal intensity. T1ρ and T2 maps at the follow-up time point were also registered to the baseline. Changes in absolute values at baseline and 2-years and mean T1ρ and T2 measurements on a compartmental level over 2-years (Δ mean T1ρ and T2) were computed by subtracting compartmental mean baseline T1ρ and T2 value measurements from mean values at 2-year follow-up.
Statistical analysis
Statistical analysis was performed with SPSS (Version 22.0. Armonk, NY: IBM Corp.) using a two-sided 0.05 level of significance. Student’s t-test (for numerical and approximately normally distributed data) and Pearson’s chi-square tests (for categorical variables) were used to evaluate differences between subjects with and without MRLs. Differences of T1ρ and T2 at baseline and 2-year follow-up and ΔT1ρ and ΔT2 subscale measurements were compared between cases and controls using Independent Samples t Tests. Statistical adjustment was not performed since there were no significant differences in age, gender, and BMI between subjects with MRLs and the control group (p > 0.05).
Reproducibility
Inter-reader reproducibility for the evaluation of the presence of MRLs was assessed between the two radiologists in all 57 cases by using the intra-class correlation coefficient (ICC).
For intra-reader reproducibility analysis, both readers repeated the readings in 25 randomly selected patients after at least two weeks.
In the pre-operative MRI analyses reader [1] identified 9 subjects (9 / 57 subjects) with meniscal ramp lesions and reader [2] identified 8 subjects (8 / 57 subjects). The images of the subject with discrepant analyses were adjudicated with a third experienced reader a final diagnosis of meniscal ramp was made.
Results
In 16% (9/57) of the screened subjects with an ACL tear MRLs were found on the preoperative MRIs. There were no significant differences between subjects with MRLs and the control group regarding age (33.6 ± 5.6 vs 36.4 ± 5.4 years, respectively; p=0.29), gender (52.8 % vs 50.1%, females p=0.24) and BMI (25.1 ± 1.5 vs 24.8 ± 2.4; p=0.91).
Inter-reader reproducibility for the evaluation of the presence of MRLs was 0.95 (95% confidence interval, 0.93–0.97) and intra-reader reproducibility for the evaluation of the presence of MRLs was 0.96 (95% confidence interval, 0.94–0.98).
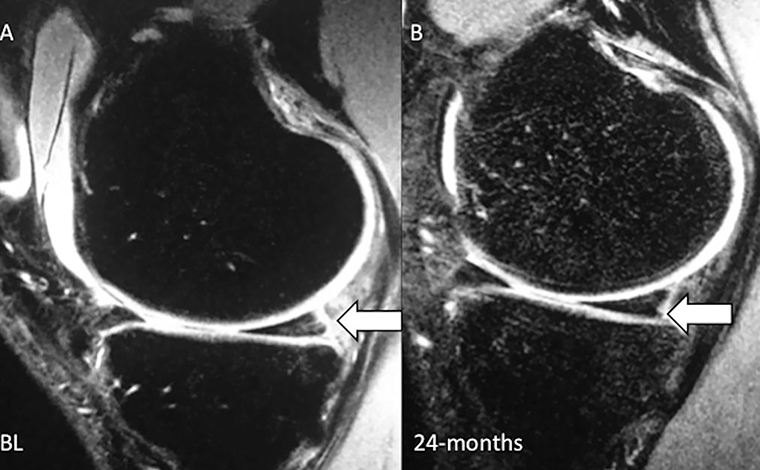
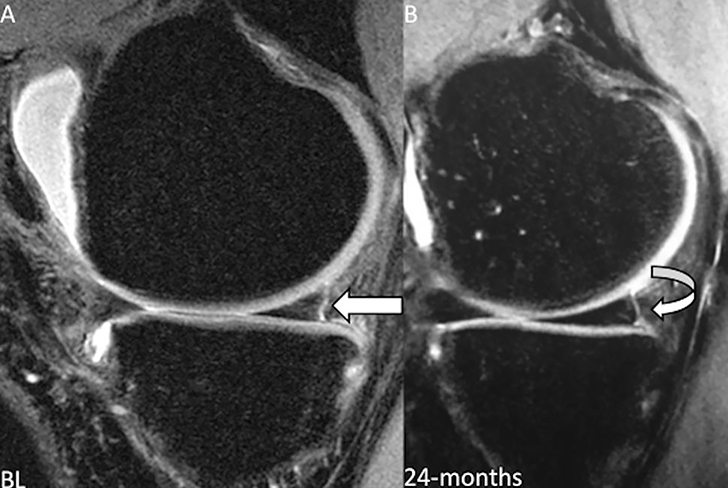
In 44% (4/9) of the cases, the MRLs morphology and linear signal abnormality (with fluid-signal) did not change over 2-years (Figure 2). In 56% (5/9) of the cases the high fluid signal-intensity interposed between the posterior horn of the medial meniscus and the posteromedial capsule decreased over 2 years (Figure 3). One (1/9) subject with MRLs developed a posterior horn meniscal horizontal tear over 2-years (Figure 4). None of the controls developed any meniscal abnormalities over 2 years.
Figure 2:
Sagittal 3D fast spin-echo sequence before surgery (baseline) of a 26 year-old man with complete ACL-tear showing the typical MRI finding of a meniscal ramp lesion (arrow) defined by a complete thin, linear lesion interposed between the posterior horn of the medial meniscus and the posteromedial capsule with fluid signal (posterior medial menisco-capsular separation).
Figure 3:
Sagittal 3D fast spin-echo sequence of a 23 year-old woman with complete ACL-tear (A) prior to surgery (baseline) and (B) 2-year follow-up MRI. Pre-operative MRI shows a meniscal ramp lesion (arrow) and follow-up MRI demonstrates persistent high fluid-signal interposed between the posterior horn of the medial meniscus and the posteromedial capsule (arrow).
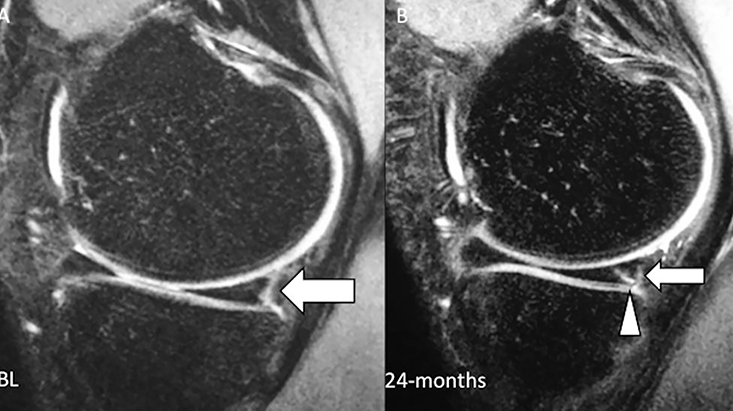
Figure 4:
Sagittal 3D fast spin-echo sequence of a 31 year-old man with complete ACL-tear (A) prior to surgery (baseline) and (B) 2-years follow-up MRI. Pre-operative MRI shows a meniscal ramp lesion (arrow) and follow-up MRI demonstrates decreased signal intensity interposed between the posterior horn of the medial meniscus and the posteromedial capsule (curved arrow), suggestive of partial healing.
No significant differences in T1rho and T2 values of the medial tibia and medial femur were observed between the two groups at baseline (p > 0.05). In subjects with MRL, T1rho values in the medial tibia and medial femur were significantly higher at the 24-month follow-up examination (medial femur= 43.6±0.5 ms vs. 40.2±3.2 ms, p= 0.001 and medial tibia= 38.2±3.7 ms vs. 34.5±3.3 ms, p=0.002). Analogously, in subjects with MRL, T2 values in the medial femur were significantly higher at follow-up (36.2±2.3 ms vs. 32.4±1.5 ms, p=0.001). The ΔT1rho from baseline to 2-years was significantly higher in subjects with MRLs than in controls in the medial femur (6.2±0.8 ms vs. 2.3±0.8 ms, p = 0.004) and in the medial tibia (4.4±1.4 ms vs. 0.4±1.6ms, p = 0.027). The ΔT2 was also significantly higher in subjects with MRL than in controls in the medial femur (5.1±2.5 ms vs. 2.2±1.9 ms, p = 0.012). Findings suggested accelerated progression of cartilage matrix degeneration in the medial compartment over 2 years in ACL injured patients with MRLs compared to patients without meniscal pathology. Absolute T1rho and T2 values at baseline and after 2 years and ΔT1rho and T2 values of subjects with MRLs and controls at the medial femur and medial tibia are summarized in Tables 2 and 3.
Table 2:
Summary of T1 ρ values at baseline and 2-year follow-up as well as Δ T1 ρ 2-years after anterior cruciate ligament surgery for subjects with ramp lesions and controls. MT (medial tibia) and MF (medial femur).
| T1ρ values at BL and 2 years* | |||||||
| BL | 2-years | ||||||
| Ramp Lesion | Controls | p-value | Ramp Lesion | Controls | p-value | ||
| Global MF | 37.4±3.2 | 37.8±2.9 | 0.72 | 43.6±0.5 | 40.2±3.2 | 0.001 | |
| Global MT | 33.7±3.4 | 33.6±3.1 | 0.91 | 38.2±3.7 | 34.5±3.3 | 0.002 | |
| ΔT1ρ 2-years-BL * | |||||||
| Ramp Lesion | Controls | p-value | |||||
| Global MF | 6.2±0.8 | 2.3±0.8 | 0.004 | ||||
| Global MT | 4.4±1.4 | 0.4±1.6 | 0.027 | ||||
Data expressed in ms; Mean ± Standard Deviation.
Table 3:
Summary of T2 values at baseline and 2-year follow-up and Δ T2 over 2 years after anterior cruciate ligament surgery for subjects with ramp lesions and controls. MT (medial tibia) and MF (medial femur).
| T2 values at BL and 2 years* | |||||||
| BL | 2-years | ||||||
| Ramp Lesion | Controls | p-value | Ramp Lesion | Controls | p-value | ||
| Global MF | 31.0±2.6 | 30.2±2.2 | 0.49 | 36.2±2.3 | 32.4±1.5 | 0.001 | |
| Global MT | 28.2±2.2 | 29.6±3.1 | 0.71 | 30.6±3.7 | 30.1±3.2 | 0.59 | |
| ΔT2 2-years-BL * | |||||||
| Ramp Lesion | Controls | p-value | |||||
| Global MF | 5.1±2.5 | 2.2±1.9 | 0.012 | ||||
| Global MT | 2.2±3.3 | 0.6±2.2 | 0.18 | ||||
Data expressed in ms; Mean ± Standard Deviation.
Discussion
Our study showed that meniscal ramp lesions detected by MRI are a relatively common finding in subjects with ACL tears. Progression to a meniscal tear in meniscal ramp lesions over 2-years is not frequent, however, subjects with meniscal ramp lesions demonstrated accelerated joint degeneration of cartilage composition in the medial knee compartment over 2-years compared to subjects with ACL-tear without meniscal pathology.
Although first described decades ago, there continues to be a lack of an established arthroscopic definition (4,22,23), and no consensus exists on the definition of a meniscal ramp lesion, other than encompassing a tear of the far periphery of the posterior horn of the medial meniscus. Arner et al (24) defined a ramp lesion as findings of posterior medial meniscocapsular separation. Keyhani et al (11) DePhillipo et al (25) defined it as a longitudinal tear / detachment of the peripheral rim around the posterior horn of the medial meniscus. On the other hand, Liu et al (26) chose to include peripheral intrasubstance tears of the meniscus, limiting their size and thus defining a MRLs as a complete tear of the peripheral anchorage of the posterior horn of the medial meniscus, a longitudinal tear less than 2.5 cm in length. Finally, Thaunat et al (27) suggested a classification system subdividing MRL of the peripheral meniscocapsular junction and red-red zone based on tear pattern and also its location. All these different definitions could be the reason why the prevalence of ramp lesions was different in several previous studies, ranging from 9.3% and 40% in patients with ACL-tears (7,8). Also, these studies often failed to distinguish stable lesions from unstable lesions, which displace the meniscus into the joint with anterior probing during the arthroscopic surgery — this could be clinically relevant, as there is evidence that stable tears of the posterior horn may heal in the setting of ACL traumatic tears without formal repair (28,29).
The definition of MRLs on MRI is also variable in the literature, but the most commonly cited definition is fluid-like high signal intensity / separation between the medial meniscus posterior horn and the capsule margin (9). This was the definition that we used in our study, which represents a complete ramp lesion (complete posterior medial meniscocapsular separation). We did not include subjects with partial separation or with no fluid-like high signal abnormality at the medial meniscocapsular junction. These partial lesions do not fulfill the meniscal ramp lesion definition used in this study and the literature supports that these incomplete / partial lesions could represent stable lesions (28,29). Our study showed that MRLs detected by MRI are a relatively common finding in subjects with ACL tears, similar to a study published in 2017 by Arner et all (24).
Interestingly, over 2 years the signal intensity abnormality and configuration of the MRLs did not change in 44% of the cases, a finding that may represent lesions that did not heal over time. In 56% of the cases, the signal-intensity decreased over 2 years and the high fluid signal interposed between the posterior horn of the medial meniscus and the posteromedial capsule could not be identified anymore, a finding that may represent fibrous tissue. However, based on our data we cannot assess the stability and clinical significance of these lesions.
One of the potential problems related to this type of lesion is the increased risk of requiring further surgery to address meniscal injury: If the diagnosis of MRLs is not made at the time of ACL reconstruction, secondary meniscal injury may be required if tears progress. Extension of the lesion towards the middle third could easily destabilize the entire posterior meniscus or result in a bucket handle tear. This could result in additional surgery for meniscal repair, meniscal resection, or meniscectomy. However, our longitudinal data showed that only one of the MRLs progressed to a meniscal tear over 2 years.
Another important potential problem related to this type of lesion is the increased risk of developing osteoarthritis: If neglected or misdiagnosed, ramp lesions can lead to instability or injury of the body of the medial meniscus which is a significant precursor to osteoarthritis of the knee. The literature reports that the risk of osteoarthritis in patients with an ACL and without a meniscal tear is between 0 and 13 %, but the risk increases to 21–48 % with meniscal tears. Thus, meniscal injuries that accompany ACL tears are relevant for the long-term prognosis, especially for OA after ACL reconstruction (2,30,31). To the best of our knowledge, no studies have yet been published on the association of MRLs and joint cartilage degeneration. Our results suggest that subjects with meniscal ramp lesions have accelerated cartilage degeneration in the medial knee compartment over 2 years compared to subjects with ACL-tears without meniscal abnormalities, demonstrating the impact of this specific pattern of meniscal lesion on joint cartilage.
No consensus exists regarding the appropriate management of ramp lesions (5). Despite being in the red-red zone, an area with a rich vascular supply, questions have been raised on whether ramp lesions can heal without repair. The subjects selected in our study participated in an ongoing prospective study, and by the time the data was collected this specific type of lesion was recommended to be treated conservatively. Therefore, our results describe the natural history of conservatively managed meniscal ramps lesions and the effect on joint cartilage longitudinally over 2 years.
This study has several limitations: First, it is based on a relatively small cohort as MRLs were found in 9 subjects or 16% of subjects with ACL tears, which probably represents the normal prevalence of this finding after ACL tears. Also, in our study only 1 subject out 9 with meniscal ramp lesion progressed to a meniscal tear over 2-years, and this finding need to be reproduced in larger cohorts. However, we followed these patients over 2 years, which is the first longitudinal investigation of this specific pattern of meniscal lesion.
Another limitation is that in the arthroscopic baseline data, no detailed surgical imaging correlates of MRLs were recorded. However, we could access arthroscopic information about overall meniscal abnormalities (e.g. meniscal tears, meniscal morphology and meniscal mobility) in all subjects. Finally, by excluding partial MRLs, we could potentially have underestimated their prevalence; however, the focus of our study was the complete meniscal ramp lesion (complete meniscal-capsular disjunction), which is most frequently associated with instability and clinical symptoms.
In summary, we found that meniscal ramp lesions detected by MRI are a relatively common finding in subjects with ACL tears. Progression to a meniscal tear in meniscal ramp lesions over 2-years is not frequent, however, subjects with meniscal ramp lesions demonstrated accelerated degeneration of cartilage composition in the medial knee compartment over 2-years compared to subjects with ACL-tears without meniscal pathology.
Figure 5:
Sagittal 3D fast spin-echo sequence of a 21 year-old man with complete ACL-tear (A) prior to surgery (baseline) and (B) 2-years follow-up MRI. Pre-operative MRI shows a meniscal ramp lesion (arrow) and follow-up MRI demonstrates high-fluid signal interposed between the posterior horn of the medial meniscus and the posteromedial capsule (arrow). Also in (B) a longitudinal oblique tear in posterior horn of medial meniscus was identified (arrow head).
Acknowledgments
This study has received funding by NIH/NIAMS P50 AR060752.
Footnotes
The authors declare that they have no conflict of interest
This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Bisson LJ, Kluczynski MA, Hagstrom LS, Marzo JM. A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. Am J Sports Med. 2013;41(8):1801–1807. [DOI] [PubMed] [Google Scholar]
- 2.Borchers JR, Kaeding CC, Pedroza AD, et al. Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med. 2011;39(9):1889–1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keene GC, Bickerstaff D, Rae PJ, Paterson RS. The natural history of meniscal tears in anterior cruciate ligament insufficiency. Am J Sports Med. 1993;21(5):672–679. [DOI] [PubMed] [Google Scholar]
- 4.Strobel MJ. Manual of Arthroscopic Surgery. Berlin Heidelberg: Springer-Verlag; 2002https://www.springer.com/gp/book/9783540874102 Accessed May 18, 2020.
- 5.Chahla J, Dean CS, Moatshe G, et al. Meniscal Ramp Lesions: Anatomy, Incidence, Diagnosis, and Treatment. Orthop J Sports Med. 2016;4(7):2325967116657815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lecouvet F, Van Haver T, Acid S, et al. Magnetic resonance imaging (MRI) of the knee: Identification of difficult-to-diagnose meniscal lesions. Diagn Interv Imaging. 2018;99(2):55–64. [DOI] [PubMed] [Google Scholar]
- 7.DePhillipo NN, Moatshe G, Chahla J, et al. Quantitative and Qualitative Assessment of the Posterior Medial Meniscus Anatomy: Defining Meniscal Ramp Lesions. Am J Sports Med. 2019;47(2):372–378. [DOI] [PubMed] [Google Scholar]
- 8.Balazs GC, Greditzer HG, Wang D, et al. Ramp Lesions of the Medial Meniscus in Patients Undergoing Primary and Revision ACL Reconstruction: Prevalence and Risk Factors. Orthopaedic Journal of Sports Medicine. 2019;7(5):232596711984350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koo B, Lee SH, Yun SJ, Song JG. Diagnostic Performance of Magnetic Resonance Imaging for Detecting Meniscal Ramp Lesions in Patients With Anterior Cruciate Ligament Tears: A Systematic Review and Meta-analysis. The American Journal of Sports Medicine. 2019;036354651988052. [DOI] [PubMed] [Google Scholar]
- 10.Hetsroni I, Lillemoe K, Marx RG. Small medial meniscocapsular separations: a potential cause of chronic medial-side knee pain. Arthroscopy. 2011;27(11):1536–1542. [DOI] [PubMed] [Google Scholar]
- 11.Keyhani S, Ahn JH, Verdonk R, Soleymanha M, Abbasian M. Arthroscopic all-inside ramp lesion repair using the posterolateral transseptal portal view. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):454–458. [DOI] [PubMed] [Google Scholar]
- 12.Kim SH, Lee SH, Kim K-I, Yang JW. Diagnostic Accuracy of Sequential Arthroscopic Approach for Ramp Lesions of the Posterior Horn of the Medial Meniscus in Anterior Cruciate Ligament-Deficient Knee. Arthroscopy. 2018;34(5):1582–1589. [DOI] [PubMed] [Google Scholar]
- 13.Malatray M, Raux S, Peltier A, Pfirrmann C, Seil R, Chotel F. Ramp lesions in ACL deficient knees in children and adolescent population: a high prevalence confirmed in intercondylar and posteromedial exploration. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1074–1079. [DOI] [PubMed] [Google Scholar]
- 14.Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial Meniscocapsular Lesions Increase Tibiofemoral Joint Laxity With Anterior Cruciate Ligament Deficiency, and Their Repair Reduces Laxity. Am J Sports Med. 2016;44(2):400–408. [DOI] [PubMed] [Google Scholar]
- 15.Naendrup JH, Pfeiffer TR, Chan C, Nagai K, Novaretti JV, Sheean AJ, et al. Effect of Meniscal Ramp Lesion Repair on Knee Kinematics, Bony Contact Forces, and In Situ Forces in the Anterior Cruciate Ligament. The American journal of sports medicine. 2019;47(13):3195–202. [DOI] [PubMed] [Google Scholar]
- 16.Vieira TD, Blakeney WG, Canuto S, Cavaignac E, Claes S, Daggett M, et al. Effect of Meniscal Ramp Lesion Repair on Knee Kinematics, Bony Contact Forces, and In Situ Forces in the Anterior Cruciate Ligament: Letter to Editor. The American journal of sports medicine. 2020;48(2):Np23–np5. [DOI] [PubMed] [Google Scholar]
- 17.DePhillipo NN, Moatshe G, Brady A, et al. Effect of Meniscocapsular and Meniscotibial Lesions in ACL-Deficient and ACL-Reconstructed Knees: A Biomechanical Study. Am J Sports Med. 2018;46(10):2422–2431. [DOI] [PubMed] [Google Scholar]
- 18.Wright RW, Haas AK, Anderson J, Calabrese G, Cavanaugh J, Hewett TE, et al. Anterior Cruciate Ligament Reconstruction Rehabilitation: MOON Guidelines. Sports health. 2015;7(3):239–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hash TW. Magnetic resonance imaging of the knee. Sports Health. 2013;5(1):78–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hajek PC, Gylys-Morin VM, Baker LL, Sartoris DJ, Haghighi P, Resnick D. The high signal intensity meniscus of the knee. Magnetic resonance evaluation and in vivo correlation. Invest Radiol. 1987;22(11):883–890. [DOI] [PubMed] [Google Scholar]
- 21.Li X, Kuo D, Theologis A, et al. Cartilage in anterior cruciate ligament-reconstructed knees: MR imaging T1{rho} and T2--initial experience with 1-year follow-up. Radiology. 2011;258(2):505–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peltier A, Lording T, Maubisson L, Ballis R, Neyret P, Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2967–2973. [DOI] [PubMed] [Google Scholar]
- 23.Bumberger A, Koller U, Hofbauer M, et al. Ramp lesions are frequently missed in ACL-deficient knees and should be repaired in case of instability. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):840–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arner JW, Herbst E, Burnham JM, et al. MRI can accurately detect meniscal ramp lesions of the knee. Knee Surg Sports Traumatol Arthrosc. 2017;25(12):3955–3960. [DOI] [PubMed] [Google Scholar]
- 25.DePhillipo NN, Cinque ME, Chahla J, Geeslin AG, Engebretsen L, LaPrade RF. incidence and Detection of Meniscal Ramp Lesions on Magnetic Resonance Imaging in Patients With Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2017;45(10):2233–2237. [DOI] [PubMed] [Google Scholar]
- 26.Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39(4):832–837. [DOI] [PubMed] [Google Scholar]
- 27.Thaunat M, Fayard JM, Guimaraes TM, Jan N, Murphy CG, Sonnery-Cottet B. Classification and Surgical Repair of Ramp Lesions of the Medial Meniscus. Arthrosc Tech. 2016;5(4):e871–e875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu X, Zhang H, Feng H, Hong L, Wang X-S, Song G-Y. Is It Necessary to Repair Stable Ramp Lesions of the Medial Meniscus During Anterior Cruciate Ligament Reconstruction? A Prospective Randomized Controlled Trial. Am J Sports Med. 2017;45(5):1004–1011. [DOI] [PubMed] [Google Scholar]
- 29.Yeo Y, Ahn JM, Kim H, et al. MR evaluation of the meniscal ramp lesion in patients with anterior cruciate ligament tear. Skeletal Radiol. 2018;47(12):1683–1689. [DOI] [PubMed] [Google Scholar]
- 30.Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40(10):2342–2347. [DOI] [PubMed] [Google Scholar]
- 31.Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–1443. [DOI] [PubMed] [Google Scholar]