Abstract
Background:
Cardiovascular disease (CVD) is the leading cause of hospitalization in the United States and patients with CVD are at a high risk of readmission after discharge. We examined whether patients’ perceived risk of readmission at discharge was associated with actual 30-day readmissions in patients hospitalized with CVD.
Methods:
We recruited 730 patients from the Duke Heart Center who were admitted for treatment of CVD between January 1, 2015 and August 31, 2017. A standardized survey was linked with electronic health records to ascertain patients’ perceived risk of readmission, and other sociodemographic, psychosocial, behavioral, and clinical data prior to discharge. All-cause readmission within 30 days after discharge was examined.
Results:
Nearly 1-in-3 patients perceived a high risk of readmission at index admission and those who perceived a high risk had significantly more readmissions within 30 days than patients who perceived low risks of readmission (23.6% vs. 15.8%, p=0.016). Among those who perceived a high risk of readmission, non-white patients (odds ratio [OR], 2.07; 95% confidence interval [CI], 1.28–3.36), those with poor self-rated health (OR, 2.30; 95% CI, 1.38–3.85), difficulty accessing care (OR, 2.72; 95% CI, 1.24–6.00), and prior hospitalizations in the past year (OR, 2.13; 95% CI, 1.21–3.74) were more likely to be readmitted. Among those who perceived a low risk of readmission, patients who were widowed (OR, 2.69; 95% CI, 1.60–4.51) and reported difficulty accessing care (OR, 1.89; 95% CI, 1.07–3.33) were more likely to be readmitted.
Conclusions:
Patients who perceived a high risk of readmission had a higher rate of 30-day readmission than patients who perceived a low risk. These findings have important implications for identifying CVD patients at a high risk of 30-day readmission and targeting the factors associated with perceived and actual risks of readmission.
INTRODUCTION
Cardiovascular disease (CVD) remains the leading cause of hospitalization in the United States and patients with CVD have an especially high risk of readmission after discharge.1 For more than a decade, clinicians, payers, and policy makers have targeted 30-day readmissions to lower healthcare costs and improve the quality of care for patients with CVD.2, 3 Despite these efforts, strategies to effectively identify patients at high risk of readmission have remained a challenge.3–6 To date, however, few approaches have considered patient-reported factors when assessing risks for 30-day readmission.7, 8
Studies have demonstrated the importance of patient-reported characteristics, perceptions, and outcomes for improving clinical practice and the provision of care.7–10 A patient’s perception of risk is an important factor that reflects the understanding and interpretation of one’s personal health, available resources, and wider socio-environmental contexts, which standard clinical measures are unable to capture.11 Indeed, studies suggest that a patient’s perceived risk of developing a disease or experiencing an adverse event is significantly related to their adherence to medical treatments and preventive behaviors.11–13 To our knowledge, no study has directly assessed whether a patient’s perception of their readmission risk at discharge is associated with actual 30-day readmission. Understanding patients’ perceptions of their risk of 30-day readmission and the factors associated with these perceptions may identify high-risk patients and promote targeted care-management strategies that prevent actual 30-day readmissions.
This study linked patient-reported data with electronic health records (EHR) to investigate the correlates and consequences of the perceived risk of readmission at the time of discharge in patients with CVD. Our overall objectives were threefold: first, to identify the sociodemographic, psychosocial, behavioral, and clinical factors associated with the perceived risk of readmission in patients hospitalized with CVD; second, to examine how patients’ perceived risk of readmission is associated with actual 30-day readmissions; and third, to evaluate the factors associated with 30-day readmissions in patients with different perceptions of readmission risk.
METHODS
Because of the sensitive nature of the data collected for this study, qualified researchers trained in human subject confidentiality protocols may send requests to access the data that support the findings of this study to the corresponding author.
Sample
Patients who were admitted for treatment of cardiovascular-related conditions between January 1, 2015 and August 31, 2017 were recruited from the Duke Heart Center at Duke University Health System. A total of 6,860 patients 18 years or older were admitted during the study period and were eligible to participate in the study. Eligible patients were randomly selected, consented, and administered a standardized survey questionnaire to collect their demographic background, socioeconomic status, psychosocial and behavioral factors, as well as patient-reported outcomes. Additional data were extracted from patients’ EHR using Duke Enterprise Data Unified Content Explorer (DEDUCE), a data extraction system that identifies patient cohorts and provides access to clinical data stored in the organizational data warehouse.14 Detailed information on subject selection, recruitment, and survey administration have been published elsewhere.15 Prior research has also demonstrated that the demographic and clinical profiles of study participants and all eligible patients at the Duke Heart Center were similar.15 A total of 860 patients were approached for inclusion and 67 refused to participate in this study (Figure 1). Among the 762 recruited patients, 32 did not answer the perceived risk of readmission question. The final analytical sample included 730 patients who were interviewed and followed after discharge. The study was approved by the Institutional Review Board at Duke University.
Figure 1.
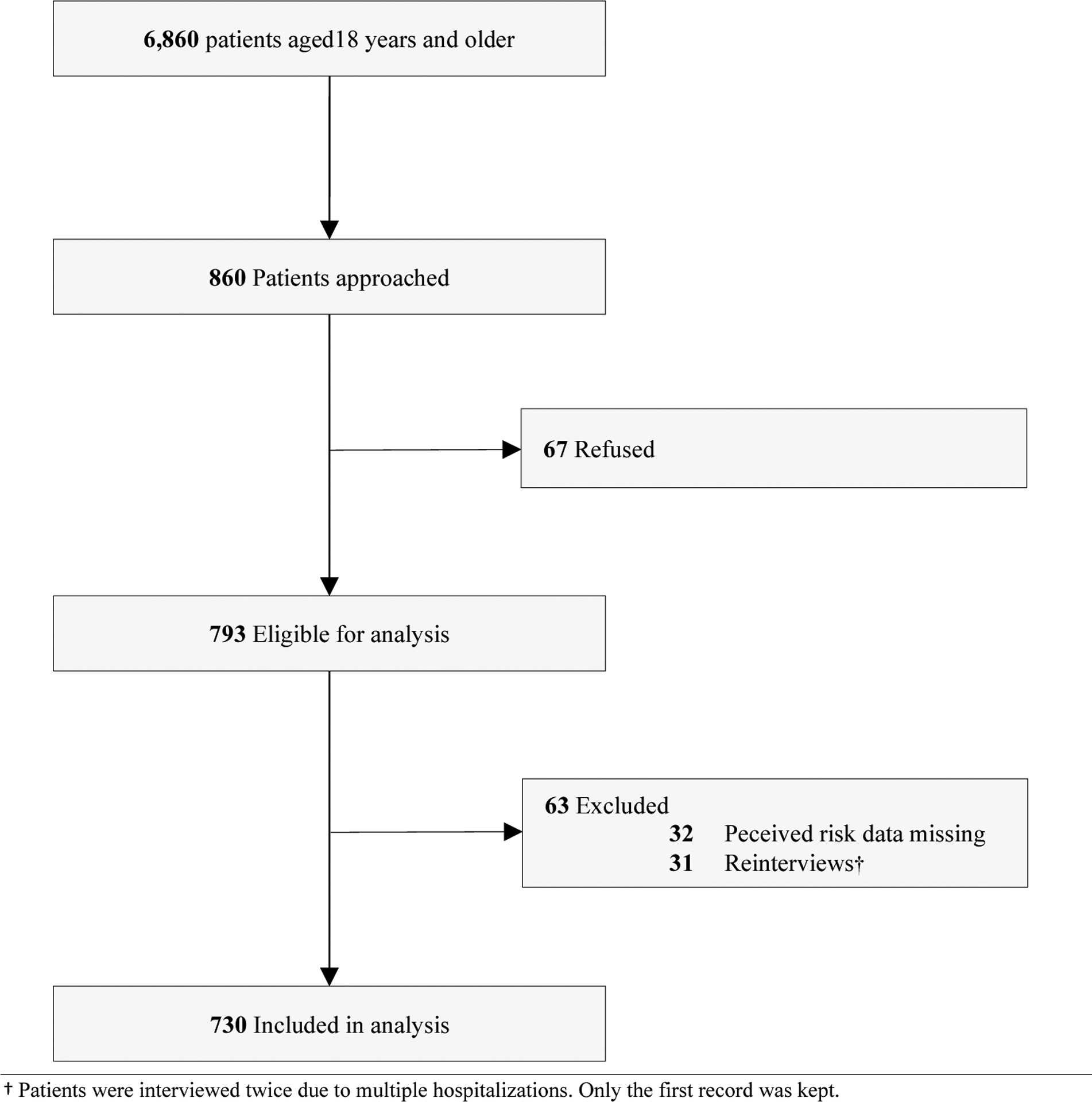
Study Participants from the Duke Heart Center
Measures
Perceived Risk of Readmission.
At the time of their index hospitalization, patients were asked how likely they thought that they would return to the hospital for an unplanned or emergency visit within the next 30 days. Possible responses included the following four categories: (1) very likely, (2) somewhat likely, (3) somewhat unlikely, and (4) not very likely. Based on the distribution of responses, and the Kaplan-Meier plots of 30-day readmissions by the responses (Supplemental Figure I), responses were dichotomized to indicate participants who perceived a high risk of readmission (categories 1 and 2) and those who perceived a low risk of readmission (categories 3 and 4).
30-Day Hospital Readmission.
Consistent with prior studies, all-cause 30-day readmissions (yes/no) were identified based on the number of days after discharge from the index admission to a subsequent hospitalization using patients’ EHRs.4, 6 Twenty-five patients died within 30 days of their discharge and five of these patients were readmitted. Another 23 patients died within 60 days of their index hospitalization. Our previous research suggests that the 30-day readmission rate in the current study was comparable to the readmission rates reported by other hospitals in North Carolina and the estimates in national reports.16 The 30-day mortality rate in this study was also similar to the mortality rate reported in prior research (3.4% in this study vs. 2.7%−5.3% in other studies).17, 18 A composite outcome of 30-day readmission or 30-day mortality was used for sensitivity analyses.19
Covariates.
Patients’ sociodemographic background, psychosocial factors, health behaviors, health-related characteristics, and healthcare utilization were collected from the surveys and EHR. Supplementary Table I presents the detailed measures for each covariate. Sociodemographic background included age, gender, race, education level, employment status, and marital status. Psychosocial factors included several previously-validated measures of social support,20, 21 life stressors,22 depressive symptoms,23, 24 self-efficacy,25, 26 and health literacy.15, 27–29 Behavioral factors included smoking history (current/past smoker or not), alcohol consumption (current drinker or not), and medication adherence.22 Health-related characteristics included poor self-rated health, a continuous measure of body mass index, any limitations in activities of daily living ([ADL], yes/no),30 and major cardiovascular related conditions that consist of hypertension, diabetes, stroke, acute myocardial infarction, atrial fibrillation, and heart failure. Measures for healthcare access and utilization included the patients’ reported difficulty accessing routine care,16, 31 length of hospital stay (in days), and having prior admissions in the past year (yes/no).
Statistical analyses
Statistical analyses were conducted in the following steps. First, we examined the differences in patients’ sociodemographic, psychosocial, behavioral, and health-related characteristics by their perceived risk of readmission using chi-square and Wilcoxon rank-sum tests (as appropriate). Next, we used Kaplan-Meier curves to demonstrate how patients’ perceived risk of readmission was associated with actual 30-day readmissions after discharge. We then conducted univariate and multivariate analyses to assess the association between perceived and actual risks of 30-day readmission accounting for all study covariates. Additionally, we used Karlson-Holm-Breen (KHB) methods to explore the extent to which these covariates contributed to the association between perceived risk of readmission and actual 30-day readmission (i.e., percentage confounding/mediating in the nested nonlinear probability models).32 In the next step, we performed bivariate and multivariate analyses using logistic regression models to identify patient characteristics that were associated with 30-day readmission (1) in patients who perceived a low risk of readmission and (2) in patients who perceived a high risk of readmission. In the final multivariate logistic regression models, backward stepwise-selection methods were used to identify the key factors significantly associated (p value <.05) with 30-day readmission in patients with different perceptions of readmission risk. Preliminary analyses showed that forward stepwise-selection methods yielded the same results on the key factors selection. Information on patient’s county of residence were extracted from the EHR and were included in all models to account for clustering and to generate robust standard errors. Tests of model discrimination and calibration were also assessed in the final models.
Preliminary analyses were also conducted to assess whether additional factors (e.g., health insurance, hyperlipidemia, chronic obstructive pulmonary disease, number of comorbidities, etc.) played a role in the associations. However, the results indicated no significant associations and were subsequently dropped in the final analyses. Sensitivity analyses also assessed alternative coding strategies for all categorical variables (e.g., different cut-points, and reference groups) and continuous variables (e.g., logged, polynomial, and grouped-ordinal scales).
The percentage of missing data among covariates ranged from 0 to 3%, with 82% of patients having complete information across all study variables. Results from Little’s MCAR test suggested that data were not missing completely at random (Chi-square = 1035.85, p < .001).33 To preserve the number of patients included in our study and to reduce the bias in estimation, we used multiple imputation methods to impute data for the missing covariates of interests.33, 34 We also performed sensitivity analyses using non-imputed data and found similar results. All analyses were performed using Stata 16.0 (StataCorp LP, College Station, TX). P values < 0.05 were considered statistically significant.
RESULTS
Table 1 presents the patients’ characteristics by perceived risk of 30-day readmission. Overall, the median age was 66 (interquartile range [IQR]: 57–75), 38.2% were female, and 34.9% were non-white. Approximately 36% of the patients had an index admission for heart failure (Supplementary Table II), followed by atrial fibrillation (20.1%), angina (15.8%), and shortness of breath (15.2%). Before discharge, nearly one-third of the patients (n=229) perceived that they were at high risk of readmission (Supplementary Figure II). Patients who perceived they were at a high risk of readmission had lower levels of education, were less likely to be working, had lower levels of social support, more life stressors, and more depressive symptoms than patients who perceived a low risk. Patients with high perceived risk were also less likely to consume alcohol, were more likely to report poor self-rated health and ADL limitations, have longer hospital stays, and have a prior hospital admission in the past year. Results from the fully-adjusted model suggested that being female (OR=0.69 [95% CI 0.52–0.93]), having more life stressors (OR=1.22 [95% CI 1.11–1.34]), reported poor self-rated health (OR=1.89 [95% CI 1.13–3.16]), having any ADL limitations (OR=2.03 [95% CI 1.38–2.99]), and having at least one prior hospital admission in the past year (OR=1.40 [95% CI 1.03–1.90]) were significantly associated with perceiving a high risk of readmission (Supplementary Table III).
Table 1.
Characteristics of Study Participants by Perceived Risk of 30-Day Readmission (N = 730)
| Overall (N = 730) | Low Perceived Risk ( N = 501) | High Perceived Risk (N = 229) | P value | Missing N (%) | |
|---|---|---|---|---|---|
| Sociodemographic Characteristics | |||||
| Age, median (IQR) | 66 (18) | 66 (18) | 66 (20) | 0.354 | 10 (1.37) |
| Female | 278 (38.19) | 194 (38.88) | 84 (36.68) | 0.571 | 2 (0.27) |
| Non-white | 255 (34.93) | 173 (34.53) | 82 (35.81) | 0.737 | |
| H.S. or less education | 104 (14.31) | 61 (12.22) | 43 (18.86) | 0.018 | 3 (0.41) |
| Not currently working | 575 (79.09) | 381 (76.35) | 194 (85.09) | 0.007 | 3 (0.41) |
| Insurance status | 0.809 | 6 (0.82) | |||
| Currently insured | 662 (91.44) | 457 (91.77) | 205 (90.71) | ||
| Medicaid only | 36 (4.97) | 23 (4.62) | 13 (5.75) | ||
| Uninsured | 26h (3.59) | 18 (3.61) | 8 (3.54) | ||
| Psychosocial Factors | |||||
| Marital status | 0.975 | 4 (0.55) | |||
| Currently married | 396 (54.55) | 270 (54.22) | 126 (55.26) | ||
| Never married | 95 (13.09) | 65 (13.05) | 30 (13.16) | ||
| Divorced | 141 (19.42) | 99 (19.88) | 42 (18.42) | ||
| Widowed | 94 (12.95) | 64 (12.85) | 30 (13.16) | ||
| Social support, mean (SD) | 16.51 (3.88) | 16.66 (3.87) | 16.17 (3.90) | 0.049 | 8 (1.10) |
| Life stressors, mean (SD) | 3.00 (1.97) | 2.71 (1.84) | 3.64 (2.09) | <.001 | 11 (1.51) |
| CES-D symptoms, mean (SD) | 7.17 (4.26) | 6.71 (4.13) | 8.15 (4.37) | <.001 | 15 (2.05) |
| Self-efficacy, mean (SD) | 9.27 (1.61) | 9.35 (1.59) | 9.11 (1.65) | 0.145 | 11 (1.51) |
| Inadequate health literacy | 109 (14.99) | 65 (13.03) | 44 (19.30) | 0.028 | 3 (0.41) |
| Behavioral Factors | |||||
| Current or past smoker | 405 (56.17) | 284 (57.49) | 121 (53.30) | 0.293 | 9 (1.23) |
| Current drinker | 286 (39.23) | 211 (42.20) | 75 (32.75) | 0.015 | 1 (0.14) |
| Medication non-adherence | 158 (22.35) | 103 (21.33) | 55 (24.55) | 0.338 | 23 (3.15) |
| Health-Related Factors | |||||
| Poor self-rated health | 123 (17.13) | 58 (11.76) | 65 (28.89) | <.001 | 12 (1.64) |
| Any ADL limitations | 413 (57.60) | 252 (51.12) | 161 (71.88) | <.001 | 13 (1.78) |
| Body mass index, mean (SD) | 30.29 (7.95) | 30.37 (7.80) | 30.09 (8.27) | 0.427 | 3 (0.41) |
| Disease Diagnoses | |||||
| Hypertension | 331 (45.34) | 238 (47.50) | 93 (40.61) | 0.083 | - |
| Diabetes | 171 (23.42) | 121 (24.15) | 50 (21.83) | 0.493 | - |
| Heart failure | 346 (47.40) | 228 (45.51) | 118 (51.53) | 0.131 | - |
| Acute MI | 107 (14.66) | 76 (15.17) | 31 (13.54) | 0.563 | - |
| Atrial fibrillation | 204 (27.95) | 136 (27.15) | 68 (29.69) | 0.476 | - |
| Stroke | 121 (16.58) | 78 (15.57) | 43 (18.78) | 0.279 | - |
| Healthcare Access and Utilization | |||||
| Difficulty accessing care | 107 (14.76) | 70 (14.00) | 37 (16.44) | 0.391 | 5 (0.68) |
| Length of stay, median (IQR) | 5.19 (6.95) | 4.97 (6.70) | 5.91 (8.52) | 0.048 | - |
| Any admissions in the past year | 319 (43.70) | 201 (40.12) | 118 (51.53) | 0.004 | - |
| 30-Day readmission rate | 133 (18.22) | 79 (15.77) | 54 (23.58) | 0.011 | - |
Abbreviations: ADL: Activities of Daily Living; CES-D: Center for Epidemiologic Studies Depression; H.S.: High school; IQR: Interquartile range; MI: Myocardial infarction; SD: Standard deviation.
Note: Categorical variables reported as n (%) and continuous variables reported as mean (SD) or median (IQR)
The overall 30-day readmission rate was 18.2%. Supplementary Figure III presents the Kaplan-Meier plots demonstrating significant differences in 30-day readmission rate by patients who perceived a high vs. a low risk of readmission (23.6% vs. 15.8%, respectively; p = .016). Table 3 presents the univariate and multivariate analyses of the association between perceived and actual risks of 30-day readmission. Results from the unadjusted model suggested that patients who perceived high risk were 66% more likely to be readmitted (OR=1.66 [95% CI 1.10–2.51]). This association was attenuated after adjusting for all study covariates (OR=1.31 [95% CI 0.87–1.96]). Similar results were found in an analysis using the composite 30-day outcome (Supplementary Table IV). Additional analyses using KHB methods suggested that a combination of all study covariates contributed to 49.3% of the association between perceived and actual risks of readmission. In particular, poor self-reported health (23.6%) and prior admissions in the past year (9.4%) were the two factors contributing most to the association.
Table 3.
Factors Associated with 30-Day Readmission in Patients Who Perceived High Risks of Readmission (N = 229)
| Variables | Unadjusted OR (95% CI) |
P value | Adjusted OR (95% CI) |
P value |
|---|---|---|---|---|
| Age | 0.99 (0.97–1.01) | 0.346 | - | - |
| Female | 1.25 (0.73–2.17) | 0.419 | - | - |
| Non-white | 1.97 (1.33–2.92) | 0.001 | 2.07 (1.28–3.36) | 0.003 |
| H.S. or less education | 0.72 (0.38–1.34) | 0.298 | - | - |
| Not currently working | 1.00 (0.56–1.79) | 0.991 | - | - |
| Insurance status (ref: currently insured) | ||||
| Medicaid only | 0.79 (0.23–2.73) | 0.711 | ||
| Uninsured | 1.49 (0.48–4.67) | 0.489 | ||
| Marital status (ref: currently married) | ||||
| Never married | 1.81 (0.98–3.33) | 0.059 | - | - |
| Divorced | 1.52 (0.55–4.17) | 0.419 | - | - |
| Widowed | 0.56 (0.22–1.42) | 0.218 | - | - |
| Social support | 0.99 (0.92–1.07) | 0.872 | - | - |
| Life stressors | 1.13 (0.96–1.33) | 0.147 | - | - |
| CES-D symptoms | 1.09 (1.02–1.17) | 0.010 | - | - |
| Self-efficacy | 0.99 (0.81–1.20) | 0.913 | - | - |
| Inadequate health literacy | 0.56 (0.25–1.25) | 0.154 | - | - |
| Current or past smoker | 0.88 (0.49–1.56) | 0.653 | - | - |
| Current drinker | 0.65 (0.36–1.19) | 0.163 | - | - |
| Medication nonadherence | 1.24 (0.61–2.51) | 0.548 | - | - |
| Poor self-rated health | 2.35 (1.45–3.80) | <0.001 | 2.30 (1.38–3.85) | 0.002 |
| Any ADL limitations | 1.28 (0.76–2.16) | 0.357 | - | - |
| Body mass index | 0.98 (0.95–1.02) | 0.423 | - | - |
| Hypertension | 0.91 (0.52–1.59) | 0.743 | - | - |
| Diabetes | 1.35 (0.72–2.55) | 0.352 | - | - |
| Heart Failure | 1.02 (0.55–1.88) | 0.957 | - | - |
| Acute MI | 0.44 (0.19–0.99) | 0.046 | - | - |
| Atrial fibrillation | 1.25 (0.68–2.28) | 0.467 | - | - |
| Stroke | 0.83 (0.35–2.02) | 0.680 | - | - |
| Difficulty in accessing to care | 2.96 (1.55–5.66) | 0.001 | 2.72 (1.24–6.00) | 0.013 |
| Length of stay | 1.01 (0.99–1.03) | 0.375 | - | - |
| Any admissions in the past year | 2.04 (1.12–3.71) | 0.019 | 2.13 (1.21–3.74) | 0.001 |
Abbreviations: ADL: Activities of Daily Living; CES-D: Center for Epidemiologic Studies Depression; CI: Confidence Interval; H.S.: High school; MI: Myocardial infarction; OR: Odds ratio; SD: Standard deviation.
Note: P values are based on logistic regression models for both unadjusted and adjusted ORs. Results from the adjusted model were derived using backward stepwise-selection procedures.
Among patients who perceived they were at a high risk of readmission prior to discharge, findings from both unadjusted and adjusted models suggest that patients who were non-white (OR=2.07 [95% CI 1.28–3.36]) and those with poor self-rated health (OR=2.30 [95% CI 1.38–3.85]), difficulty accessing care (OR=2.72 [95% CI 1.24–6.00]), and prior admissions in the past year (OR=2.13 [95% CI 1.21–3.74]) were significantly more likely to be readmitted within 30 days (Table 3). Among patients who perceived they were at a low risk of readmission, widowhood (OR=2.69 [95% CI 1.60–4.51]) and difficulty accessing care (OR=1.89 [95% CI 1.07–3.33]) were key factors significantly associated with 30-day readmission (Table 4).
Table 4.
Factors Associated with 30-Day Readmission in Patients who Perceived Low Risks of Readmission (N = 501)
| Variables | Unadjusted OR (95% CI) |
P value | Adjusted OR (95% CI) |
P value |
|---|---|---|---|---|
| Age | 0.99 (0.98–1.01) | 0.373 | - | - |
| Female | 1.46 (0.82–2.60) | 0.196 | - | - |
| Non-white | 1.36 (0.82–2.25) | 0.238 | - | - |
| H.S. or less education | 1.42 (0.74–2.72) | 0.295 | - | - |
| Not currently working | 1.68 (0.97–2.91) | 0.064 | - | - |
| Insurance status (ref: currently insured) | ||||
| Medicaid only | 1.03 (0.30–3.53) | 0.964 | ||
| Uninsured | 0.48 (0.06–4.20) | 0.508 | ||
| Marital status (ref: currently married) | ||||
| Never married | 1.88 (1.06–3.33) | 0.030 | 1.79 (0.98–3.27) | 0.060 |
| Divorced | 0.56 (0.27–1.16) | 0.119 | 0.54 (0.26–1.13) | 0.100 |
| Widowed | 2.71 (1.64–4.47) | <0.001 | 2.69 (1.60–4.51) | <0.001 |
| Social support | 0.99 (0.94–1.04) | 0.638 | - | - |
| Life stressors | 0.99 (0.89–1.11) | 0.886 | - | - |
| CES-D symptoms | 1.01 (0.96–1.07) | 0.688 | - | - |
| Self-efficacy | 1.11 (0.94–1.32) | 0.218 | - | - |
| Inadequate health literacy | 1.09 (0.57–2.08) | 0.786 | - | - |
| Current or past smoker | 0.97 (0.60–1.57) | 0.901 | - | - |
| Current drinker | 0.71 (0.48–1.05) | 0.085 | - | - |
| Medication nonadherence | 0.99 (0.59–1.68) | 0.976 | - | - |
| Poor self-rated health | 1.67 (1.01–2.78) | 0.048 | - | - |
| Any ADL limitations | 1.24 (0.75–2.05) | 0.401 | - | - |
| Body mass index | 0.97 (0.94–1.01) | 0.172 | - | - |
| Hypertension | 1.09 (0.67–1.79) | 0.726 | - | - |
| Diabetes | 0.63 (0.36–1.11) | 0.112 | - | - |
| Heart Failure | 1.13 (0.66–1.94) | 0.651 | - | - |
| Acute MI | 0.78 (0.32–1.90) | 0.587 | - | - |
| Atrial fibrillation | 0.89 (0.55–1.47) | 0.658 | - | - |
| Stroke | 1.08 (0.52–2.24) | 0.832 | - | - |
| Difficulty in accessing to care | 1.91 (1.09–3.34) | 0.023 | 1.89 (1.07–3.33) | 0.028 |
| Length of stay | 1.01 (1.00–1.02) | 0.022 | - | - |
| Any admissions in the past year | 1.47 (0.94–2.32) | 0.095 | - | - |
Abbreviations: ADL: Activities of Daily Living; CES-D: Center for Epidemiologic Studies Depression; CI: Confidence Interval; H.S.: High school; MI: Myocardial infarction; OR: Odds ratio; SD: Standard deviation.
Note: P values are based on logistic regression models for both unadjusted and adjusted OR. Results from the adjusted model were derived using backward stepwise-selection procedures.
An assessment of c-statistics for the two final models suggested better model discrimination in patients with a high perceived risk of readmission (c-statistic = 0.72, 95% CI, 0.65–0.79) than in patients with a low perceived risk of readmission (c-statistic = 0.66, 95% CI, 0.59–0.72). Non-significant results from Hosmer-Lemeshow goodness-of-fit tests also indicated good calibration in both models.
DISCUSSION
This study is the first to investigate how patient-perceived risk of readmission is associated with actual 30-day readmissions in patients with CVD. We found that approximately one-third of hospitalized patients perceived they had a high risk of readmission within 30 days after discharge. Furthermore, we found that patients who perceived they were at high risk of readmission were more likely to be readmitted compared with those who perceived a low risk. We also identified several key factors associated with risk of 30-day readmission in patients who perceived a high risk of readmission and among those who perceived a low risk of readmission. Similar to prior studies,35, 36 these models had moderate discrimination and good calibration performance.
In this study, we found that perceived risk of readmission was associated with actual 30-day readmission; and that this association was explained most by health-related factors. Specifically, self-reported health status had the largest impact on the association between perceived and actual 30-day readmission. These findings were similar to a prior study showing that poor self-rated health was associated with an increased risk of 30-day readmission in patients with acute MI.17 Our supplementary analyses further revealed that patients’ self-rated health was related to the perception of their risk of readmission. Together, this suggests that a patient’s self-awareness of their health status may not only impact how they perceive their risks of readmission, but also is an independent predictor of actual 30-day readmission. Furthermore, the association between perceived and actual risks of readmission was no longer statistically significant after adjusting for all study covariates, suggesting some degree of disconcordance between a patient’s perceived and actual risks of readmission. Therefore, to better understand this (dis)concordance, we directly examined factors associated with actual 30-day readmissions in patients who perceived a high risk of readmission and in those who perceived a low risk of readmission.
Among patients who perceived they were at a high risk of readmission, we found that non-white patients were significantly more likely to be readmitted within 30 days than their white counterparts. This finding is consistent with prior studies that have also shown higher rates of 30-day readmission in non-white patients hospitalized with CVD-related conditions.37–39 In addition, we found that adjusting for patients’ socioeconomic backgrounds and clinical characteristics did not account for racial differences in 30-day readmission. Non-white patients may be less likely to receive (or procure) the necessary support and/or care-management services to mitigate their risk of readmission. Accordingly, the American College of Cardiology (ACC) and the American Heart Association (AHA) have highlighted the need for research to identify pathways that mediate racial disparities in cardiovascular care.40, 41 Furthermore, greater efforts are needed to address potential racial disparities in CVD care, particularly among non-white patients who may be aware of their high risk of readmission and yet are readmitted within the next 30 days.
In patients who perceived they were at a high risk of readmission, we also found that those with poor self-rated health and those with prior admissions in the past year were more likely to be readmitted within 30 days after discharge. As we discussed in previous section, it can be argued that the high perceived risk in these patients may be attributable to a self-awareness of their health status and their past experiences of hospitalization; which in turn, accurately reflect their actual risk of 30-day readmission. If this is the case, providers need to consider screening patients for poor self-reported health, prior admissions, and perceptions of their risk of readmission to identify patients who may benefit from additional care-management programs to reduce their likelihood of being readmitted within 30 days after discharge.
In patients with a low perceived risk of readmission, we found that the risk of 30-day readmission were 2.7 times greater in widowed patients than in those who were currently married. These findings are sizeable and overall consistent with prior studies that have shown the associations between widowhood and other adverse cardiovascular events and mortality.42–44 Prior research has shown that HF patients who received support from their family were less likely to be readmitted than those who lacked support.19 Therefore, we speculate that patients who were widowed may be more socially isolated from the resources and support that may help them manage and monitor their disease symptoms. Therefore, these patients may not be aware of their risk of readmission but nevertheless face a high risk of being readmitted within 30 days. Although our exploratory analyses accounted for several psychosocial factors—including social support, depressive symptoms, and life stressors—possibily other and/or more detailed measures are needed to better explain the association between widowhood and the risks of readmission. Therefore, we encourage studies to further explore the potential factor(s) contributing to how the loss of a spouse can increase the risk of readmission in cardiovascular patients.
Two other notable findings warrant discussion. First, this study suggests that patients who report difficulty accessing their routine medical care have a significantly higher rate of 30-day readmission than those without difficulty accessing care. This association was observed in both the high and low-perceived risk groups and is consistent with evidence from our prior research.16 These findings contribute to the growing evidence that addressing barriers to routine medical care may be an effective approach to reducing 30-day readmissions in CVD patients.7, 9, 31 A second notable finding was that the difference in readmission rates between the high and low-perceived risk groups largely emerged 14 days after discharge (Supplementary Figure 3). This general pattern is consistent with recent evidence in support of current guidelines that recommend outpatient follow-up within 7–14 days to reduce 30-day readmissions.45, 46 Given that more than one-third of patients still do not receive timely outpatient follow-up,47, 48 our results further underscore the need to identify barriers that limit access to care and more widely recognize the importance of patient-reported evidence to develop more effective interventions to reduce 30-day readmissions.
Unlike prior research, results from this study show that insurance status and comorbidities were not significant predictors of 30-day readmission.17, 35, 36 The reasons are potentially twofold. First, most patients (96%) in our study were insured and there were no overall differences in insurance status or comorbidities by perceived risks of readmission. Second, the heterogeneity among our study patients may partially explain the non-significant finding of comorbidities. Because we recruited patients who were admitted for treatment of any cardiovascular-related conditions, the number and type of comorbidities may not be a good indicator of the patient’s severity of disease. Additional research is needed to further assess the relationship between perceived and actual risks of 30-day readmission in patients with specific cardiovascular conditions (e.g. acute myocardial infarction, heart failure, and atrial fibrillation, etc.). Relatedly, given that all study covariates accounted for only about 50% of the relationship between perceived and actual risks of 30-day readmission, we recognize that there are other unmeasured factors—patient-reported factors in particular—contributing to the association. Indeed, prior studies have found that factors such as frailty, anxiety, and cognitive impairment were also strong predictors of rehospitalizations in heart failure patients.19, 49 Additional research is needed to further assess whether and how patient-reported factors may influence perceived and actual risks of 30-day readmission. These findings may shed light on specific areas for improvement to promote high quality care as the U.S. healthcare system transitions from fee-for-service to value-based care.
Limitations
Our study has several limitations. First, this study was an observational study so that no causality can be assessed. We also recognize that the study only included CVD patients who were admitted at Duke Heart Center, which limits the generalizability of our findings. Relatedly, because we were only able to identify hospitalizations within the Duke University Healthcare System, we may not have captured readmissions that occurred outside of this health system. Nevertheless, as previously noted, the rates of 30-day readmission in the current study were comparable to the readmission rates reported by other hospitals in North Carolina. We also acknowledge that other factors—such as medications prescribed at discharge—may be related to 30-day readmissions but were not available in the current data sources. Lastly, we acknowledge the heterogeneity among patients with regard to their primary diagnosis for index admissions.
Conclusion
Nearly one-third of CVD patients perceived that they were at a high risk of readmission in this study. Patients who perceived a high risk of readmission had a significantly higher rate of 30-day readmission than those who perceived a low risk of readmission. These findings provide strong evidence for the clinical utility of assessing patients’ perceived risk of readmission prior to discharge to better identify those who may be readmitted within 30 days. Our study also identifies important non-clinical factors that are associated with 30-day readmission in patients with different perceptions of their risk. These findings have important implications for targeting CVD patients at high risk of 30-day readmission and for developing interventions that are responsive to patient-reported needs and perceptions.
Supplementary Material
Table 2.
Unadjusted and Adjusted Associations between Perceived and Actual Risks of 30-day Readmission (N = 730)
| Variables | Unadjusted OR (95% CI) |
P value | Adjusted OR (95% CI) |
P value |
|---|---|---|---|---|
| Perceived high risk | 1.66 (1.10–2.51) | 0.015 | 1.31(0.87–1.96) | 0.200 |
| Age (years) | 0.99 (0.98–1.01) | 0.267 | 0.99 (0.98–1.01) | 0.235 |
| Female | 1.30 (0.87–1.93) | 0.200 | 1.11 (0.64–1.94) | 0.704 |
| Non-white | 1.50 (1.12–2.02) | 0.006 | 1.53 (1.03–2.28) | 0.036 |
| H.S. or less education | 1.30 (0.78–2.16) | 0.310 | 1.23 (0.66–2.29) | 0.517 |
| Not currently working | 0.62 (0.43–0.91) | 0.014 | 0.74 (0.42–1.31) | 0.305 |
| Insurance status (ref: currently insured) | ||||
| Medicaid only | 1.09 (0.54–2.21) | 0.803 | 0.50 (0.18–1.34) | 0.166 |
| Uninsured | 1.00 (0.50–2.01) | 0.997 | 0.79 (0.31–2.05) | 0.630 |
| Marital status (ref: currently married) | ||||
| Never married | 1.90 (1.29–2.81) | 0.001 | 1.61 (0.96–2.71) | 0.069 |
| Divorced | 0.88 (0.41–1.87) | 0.735 | 0.78 (0.33–1.81) | 0.557 |
| Widowed | 1.86 (1.16–2.98) | 0.010 | 1.55 (0.80–3.01) | 0.191 |
| Social support | 0.98 (0.93–1.02) | 0.278 | 1.00 (0.94–1.06) | 0.949 |
| Life stressors | 1.07 (0.99–1.15) | 0.097 | 0.97 (0.86–1.09) | 0.574 |
| CES-D symptoms | 1.05 (1.01–1.09) | 0.018 | 1.03 (0.97–1.09) | 0.300 |
| Self-efficacy | 1.06 (0.93–1.20) | 0.387 | 1.08 (0.95–1.23) | 0.258 |
| Inadequate health literacy | 0.94 (0.56–1.58) | 0.817 | 0.72 (0.43–1.20) | 0.207 |
| Current or past smoker | 0.95 (0.67–1.35) | 0.783 | 1.02 (0.66–1.56) | 0.940 |
| Current drinker | 0.67 (0.50–0.89) | 0.006 | 0.75 (0.55–1.03) | 0.071 |
| Medication non-adherence | 1.06 (0.67–1.68) | 0.803 | 1.04 (0.67–1.61) | 0.870 |
| Poor self-rated health | 2.27 (1.59–3.25) | 0.000 | 2.04 (1.33–3.14) | 0.001 |
| Any ADL limitations | 1.34 (0.92–1.94) | 0.127 | 1.04 (0.67–1.60) | 0.867 |
| Body mass index | 0.98 (0.95–1.00) | 0.099 | 0.97 (0.94–1.00) | 0.030 |
| Hypertension | 0.98 (0.70–1.37) | 0.906 | 1.08 (0.73–1.58) | 0.701 |
| Diabetes | 0.86 (0.57–1.30) | 0.469 | 0.81 (0.48–1.38) | 0.437 |
| Heart Failure | 1.14 (0.76–1.71) | 0.537 | 0.86 (0.51–1.46) | 0.589 |
| Acute MI | 0.67 (0.40–1.14) | 0.138 | 0.67 (0.37–1.24) | 0.207 |
| Atrial fibrillation | 1.00 (0.71–1.42) | 0.990 | 1.15 (0.72–1.82) | 0.566 |
| Stroke | 0.95 (0.53–1.70) | 0.864 | 0.89 (0.53–1.50) | 0.661 |
| Difficulty in accessing to care | 2.12 (1.39–3.22) | <0.001 | 2.06 (1.32–3.23) | 0.002 |
| Length of stay | 1.01 (1.00–1.02) | 0.010 | 1.00 (0.99–1.01) | 0.374 |
| Any admissions in the past year | 1.70 (1.10–2.62) | 0.017 | 1.55 (1.02–2.34) | 0.040 |
Abbreviations: ADL: Activities of Daily Living; CES-D: Center for Epidemiologic Studies Depression; CI: Confidence Interval; H.S.: High school; MI: Myocardial infarction; OR: Odds ratio; SD: Standard deviation
Note: P values are based on logistic regression models for both unadjusted and adjusted ORs
What is Known.
Patients with cardiovascular disease (CVD) have a high risk of readmission after discharge.
Patients’ perception of risk is associated with their adherence to medical treatments and preventive behaviors.
What the Study Adds.
Patients who perceived high risks of readmission were more likely to be readmitted within 30 days than those who perceived low risks of readmission, suggesting its clinical utility to identify CVD patients at a high risk of readmission.
Future studies are need to identify strategies to target the factors associated with perceived and actual risks of readmission.
Acknowledgments
Special thanks to our colleagues from the Duke Office of Clinical Research for assistance with data management. Results from this study were presented at the 2019 Gerontological Society of America Annual Scientific Meeting in Austin, TX.
Funding/Support
This research was supported by a Duke REACH Equity Center (U54MD012530). This study was also funded in part by the National Institute on Aging (NIA; R21AG061142) and an NIA Training Grant (T32AG000029) for Dr. Farmer.
Non-standard Abbreviations and Acronyms
- ADL
Activities of daily living
- CES-D
Center for Epidemiologic Studies Depression
- CI
Confidence Interval
- CVD
Cardiovascular disease
- DEDUCE
Duke Enterprise Data Unified Content Explorer
- EHR
Electronic health records
- HF
Heart failure
- H.S.
High school
- IQR
Interquartile range
- KHB
Karlson-Holm-Breen
- MI
Myocardial infarction
- OR
Odds ratio
Footnotes
Disclosures
None.
Reference
- 1.Benjamin EJ, Muntner P, Bittencourt MS. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 2.Ibrahim AM, Dimick JB, Sinha SS, Hollingsworth JM, Nuliyalu U, Ryan AM. Association of Coded Severity With Readmission Reduction After the Hospital Readmissions Reduction Program. JAMA internal medicine. 2018;178:290–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. New England Journal of Medicine. 2009;360:1418–1428. [DOI] [PubMed] [Google Scholar]
- 4.Curtis LH, Greiner MA, Hammill BG, Kramer JM, Whellan DJ, Schulman KA, Hernandez AF. Early and long-term outcomes of heart failure in elderly persons, 2001–2005. Archives of Internal Medicine. 2008;168:2481–2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta A, Allen LA, Bhatt DL, Cox M, DeVore AD, Heidenreich PA, Hernandez AF, Peterson ED, Matsouaka RA, Yancy CW, et al. Association of the Hospital Readmissions Reduction Program Implementation With Readmission and Mortality Outcomes in Heart Failure. JAMA cardiology. 2018;3:44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krumholz HM, Normand SLT, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke: 1999–2011. Circulation. 2014;130:966–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132:873–898. [DOI] [PubMed] [Google Scholar]
- 8.Meddings J, Reichert H, Smith SN, Iwashyna TJ, Langa KM, Hofer TP, McMahon LF Jr. The Impact of Disability and Social Determinants of Health on Condition-Specific Readmissions beyond Medicare Risk Adjustments: A Cohort Study. Journal of general internal medicine. 2017;32:71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carter J, Ward C, Thorndike A, Donelan K, Wexler DJ. Social Factors and Patient Perceptions Associated With Preventable Hospital Readmissions. Journal of Patient Experience. 2 2020;7:19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rumsfeld JS, Alexander KP, Goff DC Jr, Graham MM, Ho PM, Masoudi FA, Moser DK, Roger VL, Slaughter MS, Smolderen KG. Cardiovascular health: the importance of measuring patient-reported health status: a scientific statement from the American Heart Association. Circulation. 2013;127:2233–2249. [DOI] [PubMed] [Google Scholar]
- 11.Brawarsky P, Eibensteiner K, Klinger EV, Baer HJ, Getty G, Orav EJ, Colditz G, Haas JS. Accuracy of self-perceived risk for common conditions. Cogent medicine. 2018;5:1463894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alwan H, William J, Viswanathan B, Paccaud F, Bovet P. Perception of cardiovascular risk and comparison with actual cardiovascular risk. Eur J Cardiovasc Prev Rehabil. 2009;16:556–561. [DOI] [PubMed] [Google Scholar]
- 13.Boggan AMN, Wang T, Li S, Pencina M, Stafford J, Goldberg A, Robinson J, Roger V, Virani S, Wilson P. Patients’ Perceived Versus Predicted Cardiovascular Disease Risk: Challenges For Shared Decision-Making In Cholesterol Management. Journal of the American College of Cardiology. 2016;67:1929. [Google Scholar]
- 14.Horvath MM, Winfield S, Evans S, Slopek S, Shang H, Ferranti J. The DEDUCE Guided Query tool: providing simplified access to clinical data for research and quality improvement. Journal of biomedical informatics. 2011;44:266–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dupre ME, Nelson A, Lynch SM, Granger BB, Xu H, Willis JM, Curtis LH, Peterson ED. Identifying Nonclinical Factors Associated With 30-Day Readmission in Patients with Cardiovascular Disease: Protocol for an Observational Study. JMIR research protocols. 2017;6:e118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dupre ME, Xu H, Granger BB, Lynch SM, Nelson A, Churchill E, Willis JM, Curtis LH, Peterson ED. Access to routine care and risks for 30-day readmission in patients with cardiovascular disease. American heart journal. 2018;196:9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dodson JA, Hajduk AM, Murphy TE, Geda M, Krumholz HM, Tsang S, Nanna MG, Tinetti ME, Goldstein D, Forman DE, et al. Thirty-Day Readmission Risk Model for Older Adults Hospitalized With Acute Myocardial Infarction. Circulation Cardiovascular quality and outcomes. 2019;12:e005320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horwitz L, Partovian C, Lin Z, Herrin J, Grady J, Conover M, Montague J, Dillaway C, Bartczak K, Ross J. Hospital-Wide (All-Condition) 30-Day Risk-Standardized Readmission Measure DRAFT Measure Methodology Report. Baltimore, MD: Centers for Medicare and Medicaid Services; 2011. [Google Scholar]
- 19.Sokoreli I, Cleland JG, Pauws SC, Steyerberg EW, de Vries JJG, Riistama JM, Dobbs K, Bulemfu J, Clark AL. Added value of frailty and social support in predicting risk of 30-day unplanned re-admission or death for patients with heart failure: An analysis from OPERA-HF. Int J Cardiol. 2019;278:167–172. [DOI] [PubMed] [Google Scholar]
- 20.Lett HS, Blumenthal JA, Babyak MA, Catellier DJ, Carney RM, Berkman LF, Burg MM, Mitchell P, Jaffe AS, Schneiderman N. Dimensions of social support and depression in patients at increased psychosocial risk recovering from myocardial infarction. International journal of behavioral medicine. 2009;16:248–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mitchell PH, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, Froelicher ES, Czajkowski S, Youngblood M, Huber M. A short social support measure for patients recovering from myocardial infarction: the ENRICHD Social Support Inventory. Journal of Cardiopulmonary Rehabilitation and Prevention. 2003;23:398–403. [DOI] [PubMed] [Google Scholar]
- 22.Rahimi AR, Spertus JA, Reid KJ, Bernheim SM, Krumholz HM. Financial barriers to health care and outcomes after acute myocardial infarction. JAMA. 2007;297:1063–1072. [DOI] [PubMed] [Google Scholar]
- 23.Karim J, Weisz R, Bibi Z, ur Rehman S. Validation of the eight-item center for epidemiologic studies depression scale (CES-D) among older adults. Current Psychology. 2015;34:681–692. [Google Scholar]
- 24.Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics. 1999;11:139–148. [DOI] [PubMed] [Google Scholar]
- 25.Lachman ME, Firth KMP. The adaptive value of feeling in control during midlife In: Brim O, Ryff C and Kessler R, eds. How Healthy Are We? A National Study of Well-Being at Midlife Chicago, IL: University of Chicago Press; 2004. [Google Scholar]
- 26.Lachman ME, Weaver SL. Sociodemographic variations in the sense of control by domain: findings from the MacArthur studies of midlife. Psychology and aging. 1998;13:553–562. [DOI] [PubMed] [Google Scholar]
- 27.Levy H, Janke AT, Langa KM. Health literacy and the digital divide among older Americans. Journal of general internal medicine. 2015;30:284–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Powers BJ, Trinh JV, Bosworth HB. Can this patient read and understand written health information? JAMA. 2010;304:76–84. [DOI] [PubMed] [Google Scholar]
- 29.Stagliano V, Wallace LS. Brief health literacy screening items predict newest vital sign scores. Journal of the American Board of Family Medicine : JABFM. 2013;26:558–565. [DOI] [PubMed] [Google Scholar]
- 30.Katz S Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. Journal of the American Geriatrics Society. 1983;31:721–727. [DOI] [PubMed] [Google Scholar]
- 31.Bindman AB, Grumbach K, Osmond D, Komaromy M, Vranizan K, Lurie N, Billings J, Stewart A. Preventable hospitalizations and access to health care. JAMA. 1995;274:305–311. [PubMed] [Google Scholar]
- 32.Karlson KB, Holm A, Breen R. Comparing Regression Coefficients Between Same-sample Nested Models Using Logit and Probit:A New Method. Sociological Methodology. 2012;42:286–313. [Google Scholar]
- 33.Little RJ, Rubin DB. Statistical analysis with missing data: John Wiley & Sons; 2019. [Google Scholar]
- 34.Li P, Stuart EA, Allison DB. Multiple Imputation: A Flexible Tool for Handling Missing Data. JAMA. 2015;314:1966–1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Barreto-Filho JA, Kim N, Suter LG, Bernheim SM, et al. Hospital readmission performance and patterns of readmission: retrospective cohort study of Medicare admissions. BMJ. 2013;347:f6571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kini V, Peterson PN, Spertus JA, Kennedy KF, Arnold SV, Wasfy JH, Curtis JP, Bradley SM, Amin AP, Ho PM, et al. Clinical Model to Predict 90-Day Risk of Readmission After Acute Myocardial Infarction. Circulation Cardiovascular quality and outcomes. 2018;11:e004788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Damiani G, Salvatori E, Silvestrini G, Ivanova I, Bojovic L, Iodice L, Ricciardi W. Influence of socioeconomic factors on hospital readmissions for heart failure and acute myocardial infarction in patients 65 years and older: evidence from a systematic review. Clin Interv Aging. 2015;10:237–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rathore SS, Foody JM, Wang Y, Smith GL, Herrin J, Masoudi FA, Wolfe P, Havranek EP, Ordin DL, Krumholz HM. Race, quality of care, and outcomes of elderly patients hospitalized with heart failure. JAMA. 2003;289:2517–2524. [DOI] [PubMed] [Google Scholar]
- 39.Rodriguez-Gutierrez R, Herrin J, Lipska KJ, Montori VM, Shah ND, McCoy RG. Racial and Ethnic Differences in 30-Day Hospital Readmissions Among US Adults With Diabetes. JAMA network open. 2019;2:e1913249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cruz-Flores S, Rabinstein A, Biller J, Elkind MS, Griffith P, Gorelick PB, Howard G, Leira EC, Morgenstern LB, Ovbiagele B, et al. Racial-ethnic disparities in stroke care: the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2091–2116. [DOI] [PubMed] [Google Scholar]
- 41.Yancy CW, Wang TY, Ventura HO, Pina IL, Vijayaraghavan K, Ferdinand KC, Hall LL. The coalition to reduce racial and ethnic disparities in cardiovascular disease outcomes (credo): why credo matters to cardiologists. J Am Coll Cardiol. 2011;57:245–252. [DOI] [PubMed] [Google Scholar]
- 42.Dupre ME, Lopes RD. Marital History and Survival After Stroke. Journal of the American Heart Association. 2016;5:e004647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dupre ME, Nelson A. Marital history and survival after a heart attack. Social science & medicine (1982). 2016;170:114–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schultz WM, Hayek SS, Samman Tahhan A, Ko YA, Sandesara P, Awad M, Mohammed KH, Patel K, Yuan M, Zheng S, et al. Marital Status and Outcomes in Patients With Cardiovascular Disease. Journal of the American Heart Association. 2017;6: e005890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Albert NM, Barnason S, Deswal A, Hernandez A, Kociol R, Lee E, Paul S, Ryan CJ and White-Williams C. Transitions of care in heart failure: a scientific statement from the American Heart Association. Circulation Heart failure. 2015;8:384–409. [DOI] [PubMed] [Google Scholar]
- 46.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr., Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136:e137–e161. [DOI] [PubMed] [Google Scholar]
- 47.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, Peterson ED, Curtis LH. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–1722. [DOI] [PubMed] [Google Scholar]
- 48.Misky GJ, Wald HL, Coleman EA. Post-hospitalization transitions: Examining the effects of timing of primary care provider follow-up. Journal of hospital medicine. 2010;5:392–397. [DOI] [PubMed] [Google Scholar]
- 49.Sokoreli I, Pauws SC, Steyerberg EW, de Vries GJ, Riistama JM, Tesanovic A, Kazmi S, Pellicori P, Cleland JG, Clark AL. Prognostic value of psychosocial factors for first and recurrent hospitalizations and mortality in heart failure patients: insights from the OPERA-HF study. Eur J Heart Fail. 2018;20:689–696. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


