Abstract
Introduction
The aim of this study was to compare body weight loss between postoperative intermaxillary fixation with metal wire and elastic traction and to investigate factors related to body weight loss after orthognathic surgery.
Materials and methods
Subjects were 59 patients with dentofacial deformity, comprising 31 patients treated with intermaxillary fixation (IMF) and 28 patients treated with elastic traction without IMF (ELT) just after surgery. Body weight loss was measured at 1 week (T1) and 2 weeks (T2) after surgery. Body weight loss was compared between IMF and ELT, and factors related to body weight loss were statistically analyzed.
Results
Body weight loss ratio was significantly increased in IMF (2.6%) rather than in ELT (1.4%) at T1, but only tended to be increased in both groups at T2, showing no statistical difference. Body weight loss ratio was significantly increased at T2 compared to T1 in both groups. Body weight loss was significantly greater at T2 than at T1.
Conclusion
Both IMF and ELT cause body weight loss after orthognathic surgery, but IMF causes body weight loss earlier than ELT and increased early body weight loss increases continuous body weight loss after orthognathic surgery.
Keywords: Body weight loss, Orthognathic surgery, Intermaxillary fixation with metal wire, Elastic traction
Introduction
Nutritional management is one of the basic cornerstones to the medical treatment of all diseases. Nutrition can affect postoperative morbidity in surgical patients [1, 2], and insufficient food intake can decrease therapeutic effects. In the perioperative period, poor nutrition is thought to adversely affect wound healing [3, 4] and postoperative infections [5]. Preventing deterioration of nutritional status in the perioperative period is desirable. In particular, patients following orthognathic surgery are unable to eat a normal diet for 6–8 weeks due to trismus and postoperative occlusal management. If postoperative intermaxillary fixation with metal wire (IMF) is performed just after surgery, patients can only take food orally by liquid diet or by nasogastric tube feeding until the IMF is removed. IMF is one of the modalities used before the utilization of miniplates to stabilize and promote the healing of fractured facial bones in cases of maxilla-mandibular trauma or orthognathic surgery. Recently, elastic traction (ELT) has been mainly used for occlusal management without IMF according to development of the miniplates osteosynthesis method. No reports appear to have compared body weight loss between postoperative occlusal management with IMF or ELT, although body weight loss has been noted as one of the major side effects of IMF in patients with mandibular fractures [6] or orthognathic surgery [7]. This may eventually lead to impaired bone and wound healing and thus to a deterioration in overall functional recovery [8]. The literature lacks systematic documentation of the weight loss experienced by patients during the first few weeks or months or of the time required for postoperative recovery following orthognathic surgery. The perioperative period of orthognathic surgery is thus suboptimal for nutrition, but the details remain unclear. In addition, few reports have investigated factors related to nutritional status after orthognathic surgery. Knowledge about nutritional status and related factors in the early postoperative period following orthognathic surgery is important for perioperative management of orthognathic surgery. The aim of this study was therefore to compare body weight loss between IMF and ELT and to investigate factors related to body weight loss after orthognathic surgery.
Materials and Methods
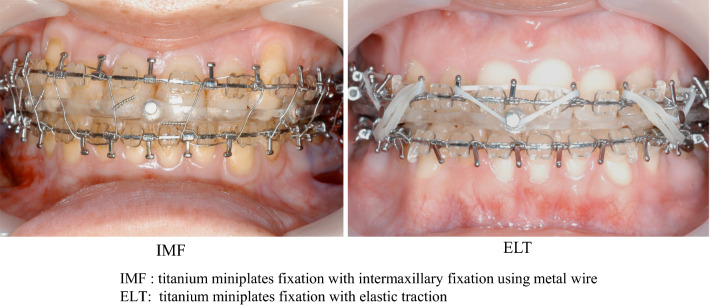
Subjects were 59 patients with dentofacial deformity who underwent bilateral sagittal splitting ramus osteotomy (BSSRO). Of these, 31 patients were treated with intermaxillary fixation using metal wire (IMF) and 28 patients were treated with elastic traction without IMF (ELT) after surgery (Fig. 1). IMF was done for 2 weeks only in IMF group. Patients were able to have food without elastics during only meal time in ELT group. This study performed retrospectively. ELT group was subsequently treated after IMF group was treated. No significant differences in clinical status were seen between the two groups (Table 1). No cases showed postoperative nausea or vomiting. All patients consumed food at nearly 35 kcal/kg body weight from 1 day after surgery. A liquid diet was ingested orally or through a nasogastric tube in IMF during 2 weeks only. In ELT, the liquid diet was ingested orally until 5 days after surgery and then paste or a soft diet was started depending on the state of elastics removal for each meal. Age and body mass index (kg/m2) were assessed as physical factors, while operation time, blood loss, and amount of mandibular movement were assessed as operative stress factors, and body weight loss, total protein, and serum albumin were assessed as nutritional state factors at 1 week postoperatively (T1) and 2 weeks postoperatively (T2).
Fig. 1.
Occlusal management after orthognathic surgery
Table 1.
Clinical status of the patients with dentofacial deformity treated by bilateral sagittal splitting ramus osteotomy
| IMF | ELT | P value | |
|---|---|---|---|
| Case (number) | 31 | 28 | |
| Age | 23 (17–33) | 24 (17–40) | 0.2947 |
| BMI | 21.0 (15.1–26.6) | 21.0 (17.7–28.0) | 0.9624 |
| Body weight (kg) | 53.0 (33–73) | 53.8 (43.5–71.5) | 0.6655 |
| Laboratory data | |||
| Total protein (g/dl) | 7.4 (6.5–8.3) | 7.2 (5.9–7.9) | 0.1691 |
| Total albumin (mm) | 4.6 (4.1–5.2) | 4.5 (3.9–4.9) | 0.0899 |
IMF titanium miniplates with 2-week intermaxillary fixation using metal wire, ELT titanium miniplates fixation with elastic traction, BMI body mass index
Mean (range) *P < 0.05 t test
Body weight loss ratio (preoperative body weight − postoperative body weight/preoperative body weight × 100 (%)) was compared between IMF and ELT, and factors related to body weight loss were statistically analyzed (Prism 7 GraphPad software, San Diego, CA). This study was approved by the Hokkaido University Research Ethics Committee (Ref. No. 010-0285).
Results
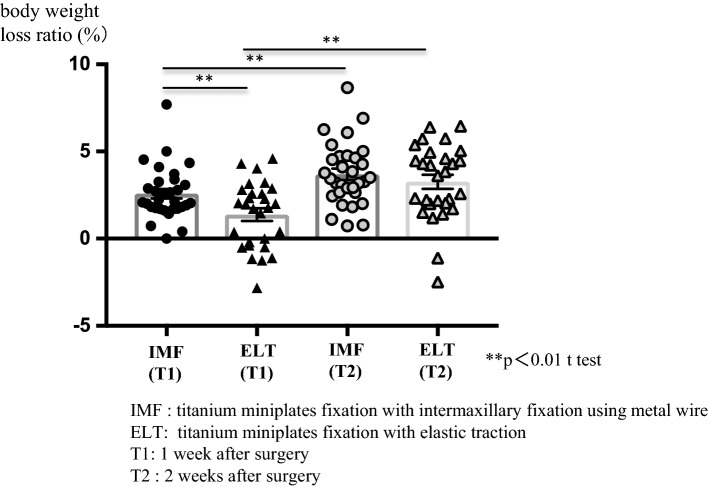
Body weight loss ratio was significantly higher in IMF (2.6%) than in ELT (1.4%) at T1, but was increased with no significant difference between groups at T2. A body weight loss ratio ≥ 5% was observed in 5 patients in both groups at T2, but in only 1 patient in IMF at T1 (Fig. 2). Body weight loss ratio was significantly increased at T2 compared to T1 in both groups (Table 2). Body weight loss ratio at T2 was compared to that at T1 (Fig. 3).
Fig. 2.
Body weight loss ratio at 1 and 2 weeks after bilateral sagittal splitting ramus osteotomy in IMF and ELT
Table 2.
Factors related to body weight loss at 2 week after bilateral sagittal splitting ramus osteotomy (n = 59)
| R square | P value | |
|---|---|---|
| Physical factors | ||
| Age | 0.0348 | 0.1570 |
| Body mass index (BMI) | 0.0001 | 0.9836 |
| Operative stress factors | ||
| Operation time (min) | 0.0003 | 0.8983 |
| Blood loss (g) | 0.0376 | 0.1408 |
| Mandibular movement (mm) | 0.0028 | 0.6924 |
| Nutritional state factors | ||
| Body weight loss (1 week after surgery) | 0.3697 | 0.0001* |
| Laboratory data (change from preoperation) | ||
| Total protein | 0.0940 | 0.0203 |
| Serum albumin | 0.0450 | 0.1273 |
*P < 0.05 Spearman’s test
Fig. 3.
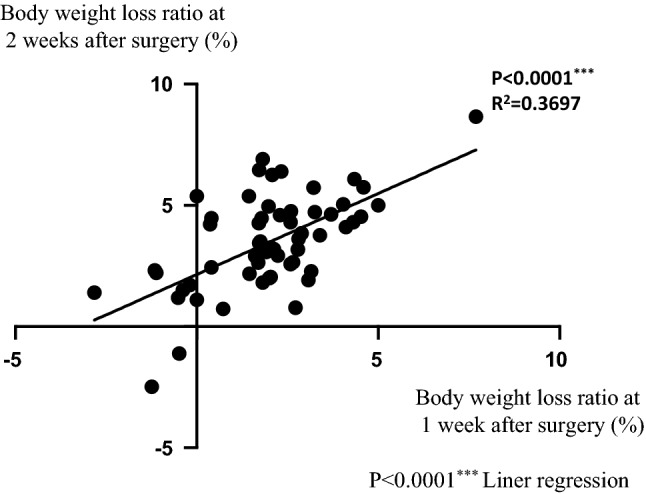
Relationship between body weight loss ratio at 2 weeks after surgery and 1 week after surgery
Discussion
The evidence for nutritional support during the perioperative period has been reviewed, and recommendations have been made regarding when nutritional support is most useful and when it may be counterproductive [7]. Past studies have focused on the relationship between the preoperative nutritional state and postoperative complications. The importance of postoperative nutritional changes has rarely been discussed, particularly in oral and maxillofacial surgery. Nutrition affects the defense systems of the body in many ways. More than 60 years ago, Studley [9] reported that postoperative infection-related morbidity and mortality increased when patients lost ≥ 20% of their preoperative body weight. When 35–40% of body weight is lost, death is generally inevitable [10]. Recent studies on nutrition and wound healing have focused on the relationship between specific nutrients and wound healing [4]. Nutrition directly influences the wound-healing process, since malnutrition decreases anabolism and depresses immunity [11]. Animal studies have shown that 6 weeks of nutritional deficiency reduces wound strength and depresses both cellular and humoral immunity [12, 13]. Clinically, these deficits manifest as delayed healing, wound infection, and prolonged rehabilitation [14]. These indicate that nutrition is a key factor in the development of postoperative complications. Tadano [15] reported that administration of non-nutrient solutions via gastrostomy under TPN accelerated jejunal anastomotic healing in comparison with TPN alone with a fasting period and provided comparable effects to early enteral feeding. The mechanical loading under such stretch conditions contributed to the upregulation of de novo type I and type III collagen synthesis by rat fibroblasts derived from the gastrointestinal tract. These results indicate that nutrition is important for immunity and wound healing in animal models.
Body weight offers a simple, easily measured, and important index of nutrition. Nutrition affects the defense systems of the body in many ways. Body weight was reduced by a mean of 3.5 kg in patients with complications and 2.1 kg in patients with no complications following oral and maxillofacial malignancy [16]. This indicates that nutrition is a key factor in the development of postoperative complications. Intermaxillary fixation with metal wire is used for reliable occlusal management just after orthognathic surgery or maxilla-mandibular fracture reduction. Long-term trismus due to this method often causes body weight loss. Worral [17] reported no significant difference in weight loss or body composition changes between plated and non-plated groups at 1 week postoperatively, but the IMF group had lost significantly more weight (mean, 4.5 kg) than the plated group (mean, 1.1 kg) by 6 weeks postoperatively. Cawood [18] reported that patients whose mandibular fractures were treated by internal fixation without IMF lost less weight and regained their preoperative weight faster than those with fractures treated by IMF alone. In a series of 100 cases, the plated group lost less weight (mean, 3 kg) in the first postoperative week than the IMF group (mean, 5 kg) and had regained their preoperative weight within 4 weeks. In these studies, intermaxillary fixation was shown to cause an undernourished state. However, no mention was made of the quantity of nutrient intake in the intermaxillary fixation and non-intermaxillary fixation groups in either study. Generally, fewer calories are present in fluid food than in solid food, because fluid food includes more water. Fluid food with a higher caloric content is needed to provide the same content as solid food. For the purpose of preventing marked differences in nutritional intake, 35 kcal/kg was provided to both groups in our study. No significant difference in body weight loss ratio was evident between groups at 2 weeks after surgery, suggesting the effectiveness of this approach. The stress of IMF in the initial stage up to 1 week may have been greater than that of ELT, because body weight loss at 1 week was significantly large in IMF than in ELT. In addition, body weight loss ratio ≥ 5% was observed in 5 patients in both groups at 2 weeks after surgery, but only 1 patient with IMF at 1 week after surgery. This indicates that elastic traction carries similar levels of nutritional stress to IMF by 2 weeks, whereas ELT offers advantages over IMF by 1 week after surgery. Both diet and conversation are difficult due to trismus for a certain period of time after orthognathic surgery, and this is thought to be a strong stressor. These factors should therefore be taken into account when determining the nutrient dose. In recent years, the need for intermaxillary fixation has decreased with miniplate fixation, but undernutrition appears avoidable by providing sufficient nutrients when intermaxillary fixation is needed for abnormal fractures. Many hospitals maintain a close relationship with dietetics departments, whose staff provide invaluable support and advice both before and after surgery. However, despite dietary advice and support, many patients continue to lose weight during the 6- to 8-week period with jaws immobilized by intermaxillary fixation or while eating a soft diet to protect the internal titanium mini plates.
Patients who undergo orthognathic surgery should be counseled on the importance of maintaining an adequate diet throughout the healing period, regardless of intermaxillary fixation.
Funding
There was no source of funding for this research.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
Approval was given by Hokkaido University Hospital Ethics Committee (Ref. No 010-0285).
Patient Consent
Not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Guo CB, Ma DQ, Zhang KH. Applicability of general nutritional status score to patients with oral and maxillofacial malignancies. Int J Oral Maxillofac Surg. 1994;23:167–169. doi: 10.1016/S0901-5027(05)80294-2. [DOI] [PubMed] [Google Scholar]
- 2.Howard L, Ashley C. Nutrition in the perioperative patient. Annu Rev Nutr. 2003;23:263–282. doi: 10.1146/annurev.nutr.23.011702.073353. [DOI] [PubMed] [Google Scholar]
- 3.Albina JE. Nutrition and wound healing. J Parenter Enteral Nutr. 1994;18:367–376. doi: 10.1177/014860719401800417. [DOI] [PubMed] [Google Scholar]
- 4.Williams JZ, Barbul A. Nutrition and wound healing. Surg Clin North Am. 2003;83:571–596. doi: 10.1016/S0039-6109(02)00193-7. [DOI] [PubMed] [Google Scholar]
- 5.Felblinger DM. Malnutrition, infection, and sepsis in acute and chronic illness. Crit Care Nurs Clin North Am. 2003;15:71–78. doi: 10.1016/S0899-5885(02)00040-0. [DOI] [PubMed] [Google Scholar]
- 6.Hayter JP, Cawood JI. The functional case for miniplates in maxillofacial surgery. Int J Oral Maxillofac Surg. 1993;22:91–96. doi: 10.1016/S0901-5027(05)80810-0. [DOI] [PubMed] [Google Scholar]
- 7.Behbehani F, Al-Aryan H, Al-Attar A, Al-Hamad N. Perceived effectiveness and side effects of intermaxillary fixation for diet control. Int J Oral Maxillofac Surg. 2006;35:618–623. doi: 10.1016/j.ijom.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Kuvat SV, Güven E, Hocaoqlu E, Basaran K, Marsan G, Cura N, Emekli U. Body fat composition and weight changes after double-jaw osteotomy. J Craniofac Surg. 2010;21:1516–1518. doi: 10.1097/SCS.0b013e3181f03fb3. [DOI] [PubMed] [Google Scholar]
- 9.Studley HD. Percentage of weight loss: basic indicator of surgical risk in patients with chronic peptic ulcer. JAMA. 1936;106:458–460. doi: 10.1001/jama.1936.02770060032009. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Obesity (1998) Preventing and managing the global epidemic. Report of a WHO consultation on obesity. World Health Organization: Geneva [PubMed]
- 11.Chandra RK. Nutrition and immunity in elderly in the elderly: clinical significance. Nutr Rev. 1995;53:S80–S83. doi: 10.1111/j.1753-4887.1995.tb01522.x. [DOI] [PubMed] [Google Scholar]
- 12.Rubcrg I. Role of nutrition in wound healing. Surg Clin Korth Am. 1984;64:721. doi: 10.1016/S0039-6109(16)43388-8. [DOI] [PubMed] [Google Scholar]
- 13.Law DK, Dudrick SJ, Abdou XI. The eflects of dietary protein depletion on immunocompetence. Ann Surg. 1974;179:168. doi: 10.1097/00000658-197402000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leigh J. Postoperative cart III. In: Rowe KL, Williams JL, editors. Maxillofacial injuries. Edinburgh: Churchill Livingstonc; 1986. p. 701. [Google Scholar]
- 15.Tadano S, Terashima H, Fukuzawa J, Mastuo R, Ikeda O, Ohkohchi N. Early postoperative oral intake accelerates upper gastrointestinal anastomotic healing in the rat model. J Surg Res. 2011;169:202–208. doi: 10.1016/j.jss.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Bozzetti F. Effects of artificial nutrition on the nutritional status of cancer patients. J Parenter Enteral Nutr. 1989;13:406–420. doi: 10.1177/0148607189013004406. [DOI] [PubMed] [Google Scholar]
- 17.Worrall SF. Changes in weight and body composition after orthognathic surgery and jaw fractures: a comparison of miniplates and intermaxillary fixation. Br J Oral Maxillofac Surg. 1994;32:289–292. doi: 10.1016/0266-4356(94)90048-5. [DOI] [PubMed] [Google Scholar]
- 18.Cawood JI. Small plate osteosvnthesis of mandibular fractures. Br J Oral Maxillofac Surg. 1985;23:77. doi: 10.1016/0266-4356(85)90057-9. [DOI] [PubMed] [Google Scholar]