Abstract
Introduction
Temporomandibular joint (TMJ) ankylosis is an extremely disabling condition with almost complete inability to open the jaws causing difficulty in chewing, speech, poor oral hygiene and cosmetic disfigurement. Temporalis myofascial flap still remains the most common interpositional material used; however, patients usually complain of pain during movement, unesthetic bulging in the temporal region and trismus due to scar contracture. The main aim of the study was to evaluate the efficacy of abdominal dermis-fat graft and compare it with temporalis myofascial flap as to see which of the two grafts offers more advantages and provides better postoperative results following TMJ ankylosis surgery.
Materials and Methods
A total of 30 diagnosed cases of TMJ ankylosis were randomly divided into two groups of 15 patients each. All the patients underwent TMJ ankylosis release under general anesthesia followed by abdominal dermis-fat interposition in Group A and temporalis muscle in Group B. The patients were assessed for pre-operative and postoperative mouth opening (immediate and 6 month postoperative), pain during physiotherapy, donor and surgical site complications and recurrence of ankylosis.
Results
The mean maximum inter-incisal opening in dermis-fat group was significantly higher than temporalis group both at immediate and 6 month postoperative periods (p = 0.041, 0.001). Physiotherapy was less painful in dermis-fat group than in temporalis group, and the differences in VAS scores among the 2 groups showed high statistical significance (p < 0.001). Hypertrophic scar developed at the donor site in 2 patients in dermis-fat group; however, it was located below the beltline and hardly noticeable. A total of 9 patients (4 in Group A and 5 in Group B) developed temporary facial nerve weakness, and no case of re-ankylosis was noted in either group.
Conclusion
Dermis-fat graft in temporomandibular joint ankylosis showed better results than conventional temporalis myofascial flap in terms of postoperative mouth opening, physiotherapy and jaw function with esthetically acceptable results.
Keywords: Temporomandibular joint ankylosis, Temporalis myofascia, Dermis fat, Physiotherapy, Facial nerve
Introduction
Ankylosis is a Greek term meaning “stiff joint” and refers to abnormal immobility and consolidation of a joint which results in hypomobility and fixation of that joint [1]. Temporomandibular (TMJ) ankylosis is crippling condition that involves pathological fusion of articular surfaces of the TMJ as a result of which mandibular movements get restricted to a varying degrees; not only there is inability to open the mouth, forward and lateral jaw movements are also severely restricted. Apart from that, it leads to a significant facial disfigurement, impairs speech, mastication and deteriorates oral hygiene [2–5].
Numerous interpositional materials have been used as a means to prevent re-ankylosis of TMJ. However, there is no ideal interpositional graft. The common problems associated with different grafts are: muscle shrinks and fibroses, fascia lacks bulk, cartilage tends to fibrose and calcify, while alloplastic implants disintegrate under functional loads and cause foreign body giant cell reactions [6]. Temporalis myofascial flap even today is the most widely used interpositional graft in TMJ ankylosis as it is a richly vascularized (viable) local flap, provides adequate bulk and eliminates chance of any distant donor site morbidity. However, patients usually complain of pain during movement possibly due to nerve compression and unesthetic bulging in the temporal region. Also the scar contracture of the muscle may further worsen trismus in the postoperative period [6, 7].
Dermis-fat grafts are commonly employed for cosmetic restoration in anophthalmic sockets, augmentation rhinoplasties and postparotidectomy cases to eliminate concave deformity and also to prevent development of Frey’s syndrome in the postoperative period. The use of dermis-fat grafts as interpositional material in TMJ ankylosis was first described by Dimitroulis in 2004. A dermis-fat graft offers many advantages as it is easily adapted, takes any shape, provides adequate quantity, is resistant to impact, takes readily and dermis holds the fat together and prevents its fragmentation. It also stimulates neo-adipogenesis and is effective in preventing joint fibrosis and heterotrophic calcification around the bony surfaces [6, 8]. Mehrotra et al. [8] in 2008 compared dermis-fat graft with temporalis flap and found better results with dermis fat in terms of jaw function, mouth opening and recurrence. However, the study included only children with mean age of 6.5 years. Moreover, the study did not highlight the donor site complications, scar formation, esthetics, nerve function and patient acceptability among the two groups. The main purpose of this study was to see whether or not dermis-fat graft overcomes the disadvantages associated with temporalis myofascia and does it actually provide better results postoperatively when compared to temporalis?
Materials and Methods
The study was carried in the Department of Oral and Maxillofacial Surgery, Government Dental College Srinagar, from June 2016 to May 2019 after obtaining clearance from the institutional ethical committee. Using GPOWER software (version 3.0.10), it was estimated that the least number of patients required in each group with 80% power and 5% significance level is 15. Since we have compared two groups in our study, a total of 30 patients were included in our study. Thirty patients with established diagnosis of TMJ ankylosis (bony or fibrous, unilateral or bilateral) were studied. Medically compromised patients, patients with history of previous TMJ surgeries and those not willing to participate in the study were excluded. Patients suitable for operation were randomly allocated using random number cards either to Group A (abdominal dermis-fat graft interposition) or to Group B (temporalis fascia and muscle interposition), each group having 15 patients. The groups were matched in terms of age and type of ankylosis. Clinical examination was mainly focused on any facial asymmetry, bird face deformity, presence of antegonial notch (unilateral/bilateral), scars or deviation of chin, midline deviation, maximal inter-incisal opening, occlusion, gingival condition, caries, any impacted or abnormally placed teeth and TMJ movements if any. Both joints were then assessed radiographically with orthopantomograms and cone beam computed tomograms (3D, sagittal, axial and coronal views) to confirm the diagnosis, and the type of ankylosis was labeled according to Sawhney’s classification of TMJ ankylosis (1986) [9]. Lateral cephalograms were also taken to assess the maxillomandibular relationship, mandibular retrognathism and pharyngeal space.
Surgical Technique
All patients were operated under general anesthesia with nasoendotracheal intubation or elective tracheostomy, and all the surgeries were performed by a single surgeon. The joints were exposed through modified pre-auricular incision, and a gap arthroplasty was done with the help of a surgical bone-cutting device to create a minimum of 0.5–1.5 cm gap. Dermis-fat graft was harvested in Group A patients through an elliptical incision measuring 6 cm × 3 cm made in the groin region on the left side. Dermis was then exposed by de-epithelializing the area meticulously leaving dermis intact, and the required volume of dermis-fat graft was harvested and stored in saline. The wound margins at the donor site were undermined, and layerwise closure was performed. The graft was folded onto itself with the dermis surfaces apposed and placed into the defect passively and secured with sutures. In Group B patients, 1.5-cm-wide temporalis myofascia-pedicle flap was obtained and rotated beneath the zygomatic arch with fascia facing the glenoid fossa and the muscle toward condylar surfaces and was secured with 3–0 resorbable suture material. Layerwise closure was done with resorbable sutures, and skin at the pre-auricular region was sutured with prolene 6–0 sub-cutaneous sutures, whereas scalp and abdominal skin were sutured with 3–0 silk. Vacuum suction drains were placed, and pressure dressings were applied. The suction drain was removed after 48 h, sutures from the pre-auricular area were removed on the 5th postoperative day, and those from the temporal region and the abdomen on the 10th day. The surgical procedure and follow-up in Group A patients are sequentially represented in Figs. 1 and 2 and that of Group B patients in Figs. 3 and 4.
Fig. 1.
Group A case; a–d CBCT showing bilateral TMJ ankylosis; e–k pre-auricular incision, exposure of both TMJs and removal of ankylotic mass; l–o dermis-fat graft harvested and secured; p-r closure of surgical and donor sites
Fig. 2.
a, b pre- and post-op mouth openings; c, d pre- and post-op orthopantomograms; e, f post-op healing
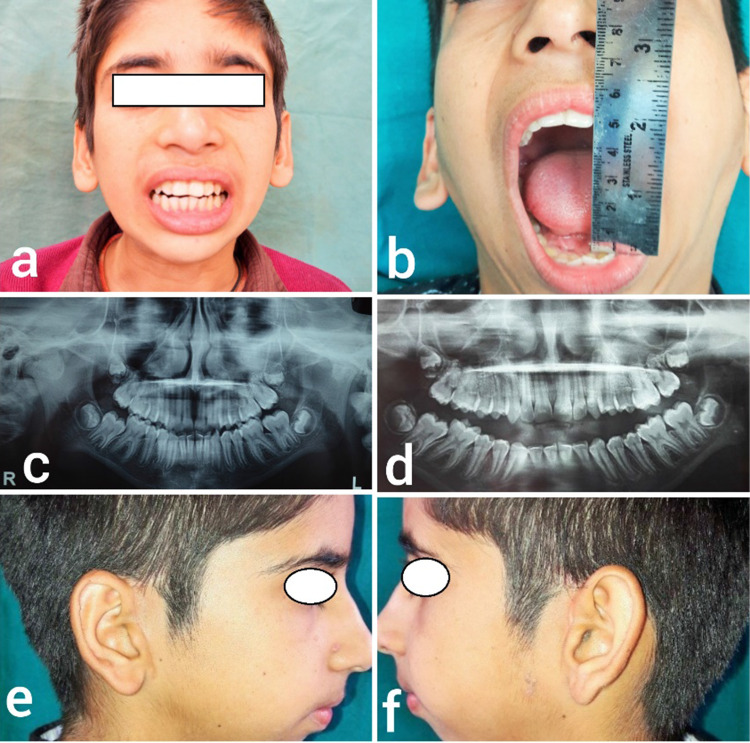
Fig. 3.
Group B patient; a pre-op mouth opening; b, c pre-op CBCT showing bilateral TMJ ankylosis; d–i incision, exposure and release of ankylosis and temporalis myofascial flap harvest
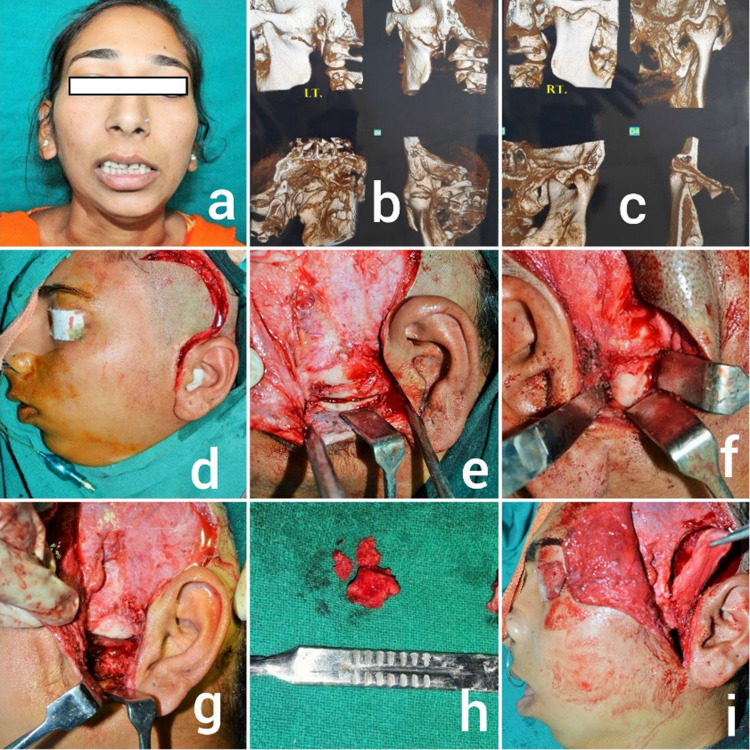
Fig. 4.
a, b closure; c, d post-op healing; e, f pre- and post-op mouth openings; g, h pre- and post-op orthopantomograms
Physiotherapy was started from the 1st postoperative day. Small wooden spatulas (each 1 mm thick) were given to the patient to be used incrementally to increase the mouth opening at the rate of 1 mm per day. Such exercises were advised about 6–8 times per day, each session lasting about 5 min, for the next 4 weeks. Physiotherapy was continued for several months if deemed necessary. Regular checkups were carried out every two weeks for 2 months and then once a month for 1 year. The patients were assessed for maximum inter-incisal opening (MIO), pain during physiotherapy, donor site complications and recurrence of ankylosis. MIO was recorded as the distance between upper and lower incisors when mouth was opened to maximum. Pain was measured by a 10-point visual analogue scale (VAS) in which a score of 0 was recorded as no pain, score 1–4 as mild pain, 5–7 as moderate pain and 8–10 as severe pain.
Results
The recorded data were compiled and entered in a spreadsheet (Microsoft Excel) and then exported to data editor of SPSS version 20.0 (SPSS Inc., Chicago, Illinois, USA). Student’s independent t test was employed for comparing continuous variables. Chi-square test or Fisher’s exact test, whichever appropriate, was applied for comparing categorical variables. A p value of less than 0.05 was considered statistically significant. All p values were 2 tailed.
A total of 30 patients were included in the study and divided into two groups with 15 patients in each group. All the demographic details of the study groups are illustrated in Table 1. A total of 25 patients underwent fiberoptic nasotracheal intubation and 5 patients (3 from Group A and 2 from Group B, p > 0.05) required elective tracheostomy. Both the groups were comparable (p > 0.05) in terms of gender and mean age of presentation. Trauma was the cause of ankylosis in 90% (27 out of 30) of the cases, otitis media in one case (3.3%), and the cause of ankylosis was unknown in 2 patients (6.7%). In total, 17 patients had bilaterally affected joints, and 13 had unilateral ankylosis, making a total of 47 joints. Majority of the affected joints belonged to Sawhney’s Type III category followed by Type II ankylosis. The mean age of onset of ankylosis was 8.3 years with most cases predominating in first and second decades of life. Severely restricted mouth opening was the most common clinical finding followed by retruded chin, facial asymmetry and midline deviation.
Table 1.
Demographics of patients included in the study
| Characteristic | Group A | Group B | P Value | |
|---|---|---|---|---|
| Gender | Male | 10 (66.7%) | 9 (60%) | 0.705 |
| Female | 5 (33.3%) | 6 (40%) | ||
| Age distribution in years | 1–10 | 3 (20%) | 3 (20%) | 0.751 |
| 11–20 | 9 (60%) | 10 (67%) | ||
| 21–30 | 3 (20%) | 2 (13%) | ||
| Type of ankylosis | Unilateral | 6 (40%) | 7 (46.7%) | 0.713 |
| Bilateral | 9 (60%) | 8 (53.3%) | ||
| Sawhney’s grade of ankylosis (47 joints) | Type I | 3 (12.5%) | 2 (8.7%) | 0.899 |
| Type II | 8 (33.3%) | 7 (30.4%) | ||
| Type III | 9 (37.5%) | 11 (47.8%) | ||
| Type IV | 4 (16.7%) | 3 (13.1%) | ||
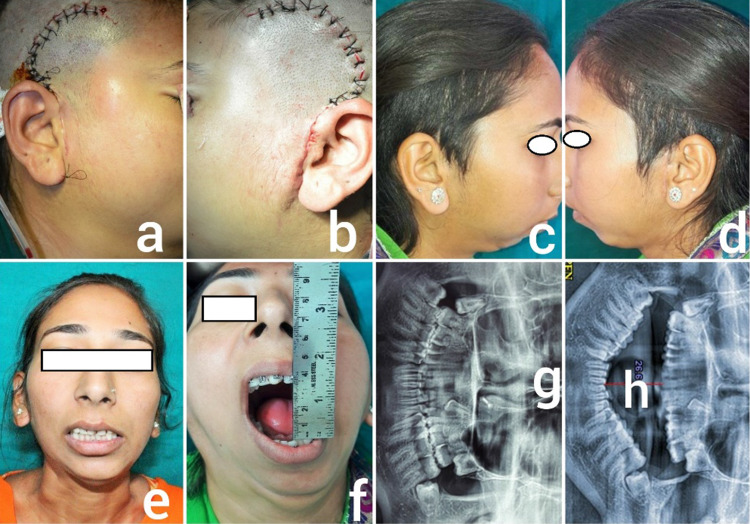
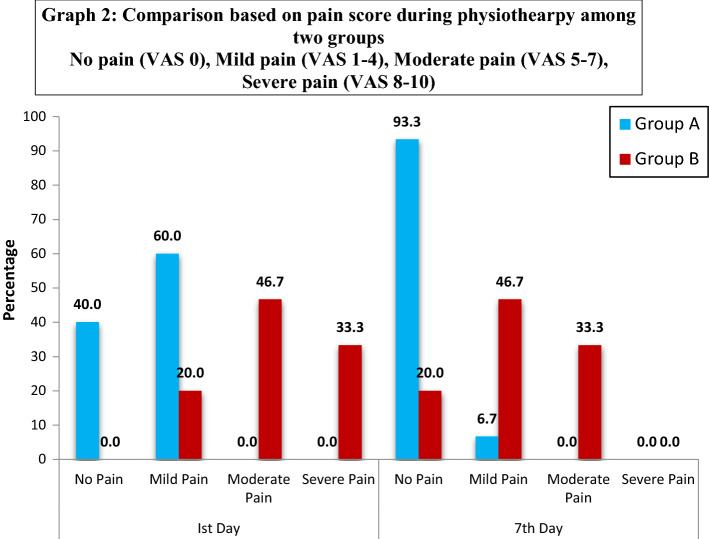
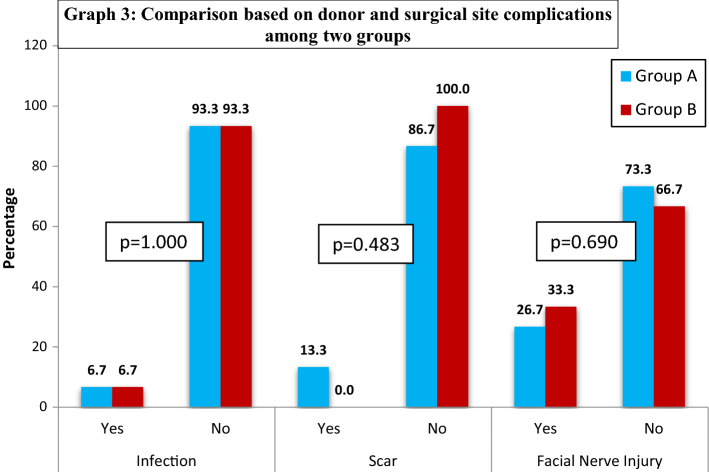
Mean pre-operative MIO was comparable between the two groups (p = 0.573). However, statistically significant differences were noted when mouth opening was compared between the two groups immediately after surgery and 6 months postoperatively (p = 0.041, 0.001) where in Group A displayed a better outcome (Fig. 5) Pain on physiotherapy was evaluated in both groups at 1st and 7th postoperative days. In Group A, pain was usually mild at 1st postoperative day and most of the patients were free of pain on seventh day making physiotherapy relatively easy. In contrast, Group B patients usually exhibited moderate to severe pain during physiotherapy on 1st day and physiotherapy again was relatively painful on 7th day as compared to Group A. There was a significant difference between the pain scores of Group A and Group B both on first and seventh postoperative days, and the differences were statistically significant (p < 0.001) (Fig. 6). Postoperative donor site infection was observed in one case in each group. Hypertrophic scars were appreciated in 2 patients of Group A in the groin region but of little significance as these rested below the belt line.
Fig. 5.
Comparison based on maximum mouth opening (mm) among 2 groups
Fig. 6.
Comparison based on pain score during physiotherapy among 2 groups. No pain (VAS 0), mild pain (VAS 1–4), moderate pain (VAS 5–7), severe pain (VAS 8–10)
Assessment of facial nerve function was done pre- and postoperatively at 24 h, 1 week, 1 and 6 months using House–Brackmann Facial Nerve Grading System [10]. A total of 4 patients in Group A had temporary facial nerve weakness (temporal and/or zygomatic branch), 2 patients had Grade II (mild dysfunction) facial nerve injury, and 2 patients had Grade III (moderate dysfunction) injury at 24 h. In Group B, 5 patients developed temporary facial nerve weakness out of which 2 patients had Grade II nerve injury and 3 patients had Grade III injury. The difference between the two groups was statistically insignificant (p > 0.05). No case of re-ankylosis was reported in either group during the follow-up period (Fig. 7).
Fig. 7.
Comparison based on donor and surgical site complications among 2 groups
Discussion
Temporomandibular joint ankylosis is a debilitating condition that impairs mastication, speech, deteriorates oral hygiene and gives rise to psychological problems. TMJ ankylosis during growth period can lead to varying degrees of facial deformity mainly involving the mandible [11]. The goals of treatment for TMJ ankylosis include improving the range of mouth opening and jaw function, minimizing disability and discomfort, preventing re-ankylosis and allowing for possible growth of the jaw in young patients [12].
Various interpositional materials have been used which include alloplastic materials like silastic, silicone, proplast, Teflon, acrylic, metals, etc., autogenous materials like muscle, fascia, cartilage, fat, costochondral grafts, metatarsals, metacarpophalangeal joint transfer, sternoclavicular joint transfer, full thickness skin graft, temporalis myofascia flap and dermis fat, each having its own advantages and disadvantages [13–18]. Temporalis myofascial flap still remains the most widely used interpositional graft in TMJ ankylosis. However, problems like restricted jaw movements and esthetic concerns cannot be ignored. Dermis-fat graft offers many advantages as it is easily adapted, takes any shape, provides adequate quantity and is resistant to impact. Dermis holds the fat together and prevents its fragmentation. It also prevents joint fibrosis and heterotrophic calcification, thereby preventing re-ankylosis [6–8, 19].
In our study, mean age of onset of TMJ ankylosis was below 10 years of age, and mean age of presentation was between 11 and 20 years of age with majority of the patients being males with a previous history of trauma. The results were consistent with other similar studies [12, 13, 20–26]. Mean MIO in Group A patients was considerably higher than Group B patients both at immediate post-op and 6 month post-op periods. This significant difference in MIO at immediate post-op period can be attributed to more surgical trauma with extensive temporalis muscle dissection in temporalis group, thereby causing more restriction in movements and also because of pain during movement due to compression of the nerves, while at later stages lesser MIO values in Group B patients could possibly be due to more muscle scarring as the graft was harvested from the same surgical site. The resultant scar contracture at the donor site might further decrease the mouth opening in these patients. Dermis fat on the other hand allows smoother movement of the condylar stump owing to the flexible nature of the graft. This is the reason why some patients in the temporalis myofascial flap group experienced a slight decrease in mouth opening within few months postoperatively, while as postoperative mouth opening was maintained in dermis-fat group patients even after 6 months and never decreased with time. Similar results are reported in a study carried out by Mehrotra et al. [8]. A significantly higher pain score during physiotherapy was observed in Group B patients as compared to Group A patients on first and 7th postoperative days. Lower pain scores in dermis-fat group can be explained by the fact that dermis-fat graft quickly adapts to any surface and adjusts easily, provides a cushion effect and is resistant to impact and pressure [8]. Recent studies have shown that dermis fat remains viable with good volume retention and does not fibrose [27]. Moreover, dermis-fat group did not require any unnecessary extension of the pre-auricular incision toward temporal area as was required in temporalis group. Therefore, it was more pleasing to the patient with no risk of alopecia along the incision line in the scalp which otherwise is common with temporalis harvesting procedure.
In our study, donor site in the dermis-fat group was infected in one patient. The infected site was managed with serial debridement and antibiotic dressings till a healthy granulation tissue was formed. It was supported with systemic antibiotics, and finally, the wound was closed layer wise. Infection rates were similar as seen with any other surgical procedure [28]. No case of seroma was seen. However, two patients developed hypertrophic scars at the donor site in the groin region. Since the scar was well below the belt line, the patients felt no need to go for scar revision (Fig. 8). In the temporalis group, there was one case of postoperative infection at the donor site which was managed conservatively. Some patients from this group complained of hollowing in the temporal region which was partially masked by hair at later stages. No appreciable scar was seen at the surgical site in both the groups, and there was no need for scar revision in any patient. Two patients, one from each group developed unilateral pneumothorax in the immediate postoperative period; one possibly due to barotrauma during general anesthesia and other due to infection. Both cases were managed by placing chest tubes along with antibiotic support.
Fig. 8.

Scar in donor groin region
Facial nerve weakness is commonly observed in patients operated for TMJ ankylosis, most common reason being excessive retraction and manipulation of tissues during TMJ surgery causing neuropraxia. Permanent facial nerve injury is rare if proper surgical technique is followed [29]. We observed facial nerve weakness in some patients and the condition improved slowly with physiotherapy. Full recovery of the nerve was attained in all the patients at 6–12 months. Similar results were seen by Malhotra et al. [30] who assessed facial nerve injury in patients of temporomandibular joint ankylosis using deep subfascial approach. The mean follow-up period was 2.3 years and 2.1 years in Group A and Group B, respectively, and no case of re-ankylosis was reported from either group.
Conclusion
Dermis-fat graft in temporomandibular joint ankylosis showed better results than conventional temporalis myofascial flap in terms of postoperative mouth opening, physiotherapy and jaw function. Graft is quick and easy to harvest with minimal morbidity. There is no ugly bulging in the temporal region and the scar even if present is hardly noticeable below the belt line and is esthetically acceptable. Dermis-fat graft is also effective in preventing re-ankylosis by inhibiting joint fibrosis and heterotrophic bone formation around the bony surfaces.
Acknowledgements
The authors declare that they have not received any funding from any source.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Haidar Z. Ankylosis of the temporomandibular joint. J Oral Med. 1986;41:246–249. [PubMed] [Google Scholar]
- 2.Row NL. Ankylosis of the temporomandibular joint. J R Coll Surg Edinb. 1982;27:67–69. [PubMed] [Google Scholar]
- 3.Row NL. Ankylosis of the temporomandibular joint. J R Coll Surg Edinb. 1982;27:167–173. [PubMed] [Google Scholar]
- 4.Row NL. Ankylosis of the temporomandibular joint. J R Coll Surg Edinb. 1982;27:209–218. [PubMed] [Google Scholar]
- 5.El Sheikh MM. Temporomandibular joint ankylosis: the Egyptian experience. Ann R Coll Surg Engl. 1999;81:12–18. [PMC free article] [PubMed] [Google Scholar]
- 6.Dimitroulis G. The interpositional dermis-fat graft in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 2004;33:755–760. doi: 10.1016/j.ijom.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 7.Su-Gwan K. Treatment of temporomandibular joint ankylosis with temporalis muscle and fascia flap. Int J Oral Maxillofac Surg. 2001;30:189–193. doi: 10.1054/ijom.2001.0047. [DOI] [PubMed] [Google Scholar]
- 8.Mehrotra D, Pradhan R, Mohammad S, Jaiswara C. Random control trial of dermis-fat graft and interposition of temporalis fascia in the management of temporomandibular ankylosis in children. Br J Oral Maxillofac Surg. 2008;46:521–526. doi: 10.1016/j.bjoms.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Sawhney CP. Bony ankylosis of the temporomandibular joint: follow-up of 70 patients treated with arthroplasty and acrylic spacer interposition. Plast Reconstr Surg. 1986;77(1):29–40. doi: 10.1097/00006534-198601000-00006. [DOI] [PubMed] [Google Scholar]
- 10.House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93(2):146–147. doi: 10.1177/019459988509300202. [DOI] [PubMed] [Google Scholar]
- 11.Moorthy AP, Finch LD. Interpositional arthroplasty for ankylosis of the temporomandibular joint. Oral surg Oral Med Oral pathol. 1983;55:545–552. doi: 10.1016/0030-4220(83)90366-3. [DOI] [PubMed] [Google Scholar]
- 12.Huang IY, Lai ST, Shen YH, Worthington P. Interpositional arthroplasty using autogenous costal cartilage graft for Temporomandibular joint ankylosis in adults. Int J Oral Maxillofac Surg. 2007;36:909–915. doi: 10.1016/j.ijom.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 13.Chorsegross C, Guyot L, Cheynet F, Blanc JL, Cannoni P. Full thickness skin graft interposition after TMJ ankylosis surgery: a study of 31 cases. Int J Oral Maxillofac Surg. 1999;28:330–334. doi: 10.1016/S0901-5027(99)80075-7. [DOI] [PubMed] [Google Scholar]
- 14.Karaca C, Barutcu A, Menderes A. Inverted, T-shaped silicone implant for the treatment of temporomandibular joint ankylosis. J Craniofac Surg. 1998;9:539–542. doi: 10.1097/00001665-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Matukas VJ, Lachner J. The use of autologous auricular cartilage for temporomandibular joint disc replacement: a preliminary report. J Oral Maxillofac Surg. 1990;48:348–353. doi: 10.1016/0278-2391(90)90429-6. [DOI] [PubMed] [Google Scholar]
- 16.Paterson AW, Shepherd JP. Fascia lata interpositional arthroplasty in the treatment of temporomandibular joint ankylosis caused by psoriatic arthritis. Int J Oral Maxillofac Surg. 1992;21:137–139. doi: 10.1016/S0901-5027(05)80779-9. [DOI] [PubMed] [Google Scholar]
- 17.Pogrel MA, Kaban LB. The role of a temporalis fascia and muscle flap in temporomandibular joint surgery. J Oral Maxillofac Surg. 1990;48:14–19. doi: 10.1016/0278-2391(90)90173-Y. [DOI] [PubMed] [Google Scholar]
- 18.Mac Intosh RB. The use of autogenous tissue for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2000;58:63–69. doi: 10.1016/S0278-2391(00)80019-1. [DOI] [PubMed] [Google Scholar]
- 19.Dimitroulis G, Trost N, Morrison W. The radiological fate of dermis-fat grafts in the human temporomandibular joint using magnetic resonance imaging. Int J Oral Maxillofac Surg. 2008;37:249–254. doi: 10.1016/j.ijom.2007.11.017. [DOI] [PubMed] [Google Scholar]
- 20.EL-Mofty S. Ankylosis of the temporomandibular joint. Oral Surg. 1972;33:650–660. doi: 10.1016/0030-4220(72)90375-1. [DOI] [PubMed] [Google Scholar]
- 21.Adekeye EO. Ankylosis of mandible: analysis of 76 cases. J Oral Maxillofac Surg. 1983;41:442–449. doi: 10.1016/0278-2391(83)90129-5. [DOI] [PubMed] [Google Scholar]
- 22.Chidzonga MM. Temporomandibular joint ankylosis review of thirty two cases. Br J Oral Maxillofac Surg. 1999;37:123–126. doi: 10.1054/bjom.1997.0089. [DOI] [PubMed] [Google Scholar]
- 23.Topazian RG. Etiology of ankylosis of temporomandibular joint: analysis of 44 cases. J Oral Surg Anesth Hosp Dent Serv. 1964;22:227–233. [PubMed] [Google Scholar]
- 24.Topazian RG. Comparison of gap and interpositional arthroplasty. J Oral Surg. 1966;1966(24):405. [PubMed] [Google Scholar]
- 25.Braithwaite F, Hopper F. Ankylosis of temporomandibular joint. Br J Plastic Surg. 1952;5:105. doi: 10.1016/S0007-1226(49)80019-1. [DOI] [PubMed] [Google Scholar]
- 26.Straith CL, Lewis JR. Ankylosis of the TMJ. Plastic Reconstr Surg. 1948;3:464. doi: 10.1097/00006534-194807000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Younis M, Shah A, Ahmed I. Viability and volumetric analysis of free autogenous dermis fat graft as interpositional material in TMJ ankylosis: a long-term MRI study. J Maxillofac Oral Surg. 2020 doi: 10.1007/s12663-020-01413-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sushmita M, Sagar J, Kalyani B, Santhosh K. Role of interpositional dermal graft in management of recurrent temporomandibular joint ankylosis: a case series of three patients. Int J Med Pharm Case Rep. 2016;6(5):1–5. [Google Scholar]
- 29.Gokkulakrishnan S, Singh S, Sharma A, Singh AK, Borah R. Facial nerve injury following surgery for temporomandibular joint ankylosis: a prospective clinical study. Indian J Dent Res. 2013;24(4):521. doi: 10.4103/0970-9290.118365. [DOI] [PubMed] [Google Scholar]
- 30.Malhotra V, Dayashankara Rao JK, Arya V, Sharma S, Kataria Y, Luthra P. Assessment of facial nerve injury with “house and brackmann facial nerve grading system” in patients of temporomandibular joint ankylosis operated using deep subfascial approach. Natl J Maxillofac Surg. 2015;6:194–199. doi: 10.4103/0975-5950.183876. [DOI] [PMC free article] [PubMed] [Google Scholar]