Abstract
Introduction
Maxillofacial region is one of the most complicated arrangements of bony and soft tissues in human body, superiorly bounded by cranial bones and inferiorly by the mandible with interposed dentition. This is one of the reasons which make injuries to this region difficult to manage and often controversial. The severity and patterns of these injuries have changed considerably due to the increasing reliance on fast road transportation facilities and interpersonal violence.
Materials and methods
The aim of the present study is to analyze retrospectively the changing patterns of mid-face fractures in a sample of patients reporting to Department of Oral and Maxillofacial Surgery in AIIMS Bhubaneswar, India, from April 2017 to April 2018. A performa was prepared which included age, sex, etiology of injury, alcohol influence, and treatment given during hospital stay.
Results
Road traffic accidents contributed 68.11% of zygomaticomaxillary complex (ZMC) fractures, followed by assault (18.11%) and fall from height (13.76%). RTA was the major cause of atypical ZMC fractures as compared to conventional ZMC fractures (P < 0.001).
Discussion
Due to modern lifestyle and changes in fast transportation, recent fracture patterns do not follow the tell-tale signs or patterns and often need unique and patient-specific treatment plan, making the skills of maxillofacial surgeons the pivotal factor in better prognosis.
Keywords: ZMC fractures, Atypical maxillofacial fractures, Complicated facial injuries, Complicated ZMC fractures
Introduction
Zygomaticomaxillary complex (ZMC) is one of the most critical and complex facial structures providing both vertical and horizontal strut to facial framework. Zygoma is a strong buttress of lateral portion of middle third of facial skeleton, forms the malar prominence and is an integral part of the lateral and inferior orbital rim and the orbital floor [1]. Because of its prominent position, it is more prone to fractures either alone or in combination with other structures of midface such as maxilla, nasoethmoidal and orbital area [2].
Fracture patterns commonly involve four processes of the complex resulting in distinct facial deformity. Functional impairment like paresthesia, trismus, diplopia, anti-mongoloid slant is also very much troublesome for the patient which requires surgical correction.
It is difficult to use existing classifications for ZMC fractures in few cases because of changing fracture patterns due to complex injuries. These factors in turn make the fractures difficult to manage and often require patient-specific treatment plan. The aim of the present study is to highlight the incidence of ZMC fractures in a tertiary centre and also to stress on number of cases deviating from conventional fracture lines and to uncover the underlying cause.
Materials and Method
The study was approved by institutional review board. Medical records of all the patients with maxillofacial injuries from April 2017 to April 2018 were analyzed by the same investigator. All the patients were clinically examined, and radiological investigations (CT scan with 3D reconstruction) were advised to determine the nature and extent of injury to plan for surgical treatment. Various inclusion and exclusion criteria were prepared for the study.
Inclusion criteria:
Patients between the age of 18–61 years,
Displaced and undisplaced fracture of the zygomaticomaxillary complex bone,
Fractures less than 5 weeks old [3].
Exclusion criteria:
Malunited fractures,
Previously operated.
Of 1192 patients examined, 324 patients had ZMC fractures. Various demographic data like age and sex of the patients, cause of injury, pattern of ZMC fracture were documented on a standard Performa. Neurological and ophthalmic evaluation was mandatory for all the patients before any maxillofacial intervention. All the patients included in the present study were managed by same surgical team keeping in mind standard AO principles.
Each fracture pattern was studied on 3D reconstructed images and divided into two groups: conventional fracture lines and atypical fracture lines.
Conventional Fracture Group
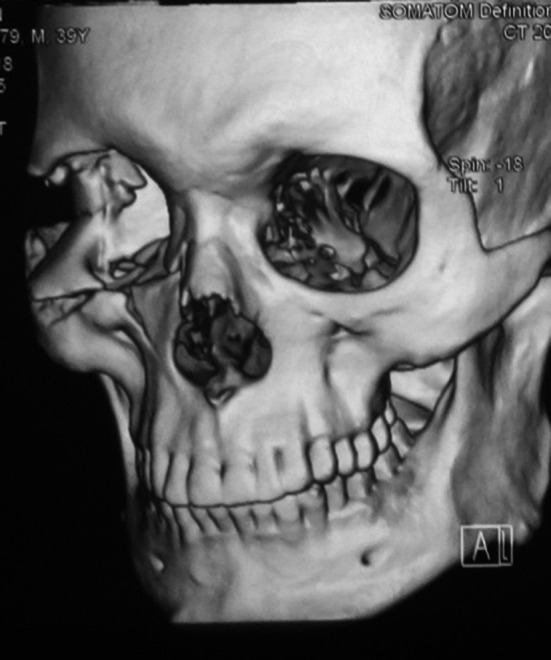
Any linear fracture which involved one or more than one processes of zygomaticomaxillary complex without any deviations was included in conventional group (Fig. 1).
Fig. 1.

Conventional fracture
Atypical Fracture Group
Fracture lines those were severely comminuted (Figs. 2, 3 and 4), sagittal fractures (Fig. 5), involving orbital complex, orbital floor fractures (n = 20) (Fig. 6), fractures associated with globe injuries and fracture lines characteristically involving the body of zygoma but not the processes were included in atypical group (Fig. 5).
Fig. 2.

Comminuted fractures
Fig. 3.
Comminuted fractures
Fig. 4.
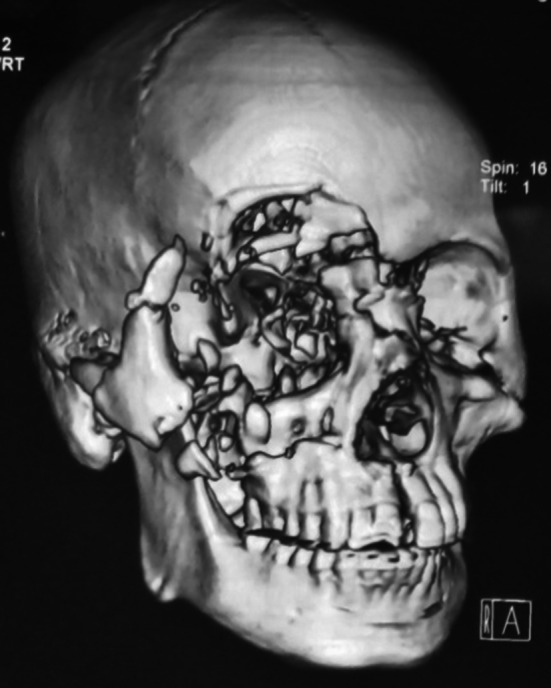
Comminuted fractures
Fig. 5.

Sagittal fractures
Fig. 6.

Orbital fractures
Statistical Analysis
Statistical analysis was done using Chi-square test and SPSS version 22.
Results
Of 1192 records evaluation, 324 patients sustained ZMC injuries. Thus, overall frequency of ZMC fractures was found to be 27.18%. Of 324 patients with ZMC fractures, 276 patients fulfilled our inclusion and exclusion criteria and only these patients were included in the present study.
On demographic analysis, it was noted that majority of cases were in the age group of 19–39 years (68.5%). Also major proportion of the study population (72.1%) was comprised of males (Table 1).
Table 1.
Distribution of demographic variable among cases
| Variable | Categories | Frequency (%) |
|---|---|---|
| Age (years) | 19–39 | 189 (68.5) |
| 40–61 | 87 (31.5) | |
| Gender | Male | 199 (72.1) |
| Female | 77 (27.9) |
Table shows the distribution of demographic variables among the cases. The distribution revealed majority of cases in the age group of 19–39 years (68.5%). An evaluation of gender in the present study revealed majority of male cases (72.1)
The etiology of ZMC fracture is summarized in Table 2. The road traffic accident contributed 68.11% for ZMC fractures, followed by assault (18.11%) and fall from height (13.76%).
Table 2.
Total number of cases according to etiology
| Fracture etiology | Number | Percentage (%) |
|---|---|---|
| RTA | 188/276 | 68.11 |
| Fall | 38/276 | 13.76 |
| Violence | 50/276 | 18.11 |
Out of these 276 ZMC fractures, 78 patients (28.26%) had atypical ZMC fracture and 198 patients (71.73%) had conventional ZMC fractures (Table 3). Each group was studied further, and more data were collected on their etiology. The correlation between the type of ZMC fractures and their etiology is mentioned in Table 4. The RTA was the major cause of atypical ZMC fractures as compared to conventional ZMC fracture (P < 0.001). The injury due to fall was least commonly associated with atypical ZMC fractures as compared to conventional fractures (P < 0.001). No significant difference was noted between the two groups when compared in terms of assault.
Table 3.
Group division
| Fracture type | Number | Percentage (%) |
|---|---|---|
| Conventional | 198 | 71.73% |
| Atypical | 78 | 28.26% |
| Total | 276 |
Table 4.
Statistical analysis using Chi-square test
| Conventional | Atypical | Total | P value | |
|---|---|---|---|---|
| RTA | 121 | 67 | 188 | 0.00006933 |
| Fall | 37 | 1 | 38 | 0.0001578 |
| Violence | 40 | 10 | 50 | 0.1518 |
| Overall group | 198 | 78 | 276 | 0.00007331 |
P value significant if ≤ 0.05
Discussion
The maxillofacial region is one of the most vulnerable parts of the body exposed to injury, and among the face ZMC is the subunit that is an integral part of facial esthetics and functions [4]. A study done by Singaram et al. [4] suggested that incidence of fractures involving malar bone was around 41.9% among all the maxillofacial fractures. Another study reported incidence of 24.36% from north India [5]. Rajanikanth et al. [6] also reported incidence of 30.92% in ZMC group from central India. These findings were similar to our study group with incidence of 27.18% in ZMC group. We carefully analyzed our subjects and further divided the group to atypical and conventional type according to our previously mentioned criteria.
The main objective of this study is to highlight the new patterns of ZMC fractures which cannot be classified using existing classifications, thus creating a surgical dilemma for the attending surgeon in formulating a treatment plan. Various treatment methods are used for ZMC fractures, and Ellis et al. [7] reported that 23% of their 2067 ZMC fractures did not receive surgical intervention. In our conventional fracture group out of 198 patients, 19% (n = 36) were managed conservatively without any surgical intervention while all the patients in atypical group required surgical intervention with three point fixation and orbital floor reconstruction (n = 20) (Table 5).
Table 5.
Distribution of cases according to orbital floor reconstruction
| Orbital floor reconstruction | Frequency | Percentage (%) |
|---|---|---|
| Present | 20 | 7.2 |
| Absent | 256 | 92.8 |
Table shows the distribution of cases according to the orbital floor reconstruction. An evaluation of the cases in the present study revealed that orbital floor reconstruction was present in 20 cases, whereas it was absent in majority of cases (256)
This contrasting difference in treatment needs among the two groups was not a coincidence. On statistical analysis, we noted that there was significant difference between the two groups in terms of their alleged etiology. Number of RTA cases was significantly higher in atypical group as compared to conventional group, whereas number of patients was significantly higher with alleged history of fall in conventional group. No significant difference was noted among the patient with history of violence between the two groups.
These findings suggested that RTA will mostly result in atypical fractures which in turn require greater amount of fixation due to complexity of injury. The reason behind this finding is that RTA often involves collision between two moving vehicles with resultant high relative velocity. Therefore, more number of force vectors acts from different directions over the facial framework which result in fractures involving natural lines of weakness as well as areas of natural strength presenting as atypical fractures.
While in cases of falls, since only one body (patient) is moving with the ground being static, there is a single vector of force that results in fractures involving natural lines of weakness as seen in conventional group. This situation is same as was done by Rene le fort in 1901 during his famous experiment which forms the basis of midface fractures even today [8]. But due to changing patterns of injuries nowadays, most of the surgeons rarely encounter the classic Lefort lines. Instead, patients present with hybrid and atypical fracture lines. But our studies suggest that injuries due to fall will most commonly result in conventional fracture lines.
Although violence can produce multiple force vectors thus predisposing the face to atypical fracture lines, our statistical analysis revealed contradictory results. There was no significant statistical difference between the two groups. This was the most interesting finding as opposed to our expectations. The reason behind this scenario is that although violence does involve multiple vectors, there are other factors which determine the type of injury like amount of force applied, use of dominant or nondominant hand by assailant, any defensive position acquired by the patient, etc. All these details were not collected in the present study.
On statistical comparison of the population in terms of age and sex (Tables 6 and 7), we noted a difference among the two groups, with significantly more number of patients in 19–39-year age group as compared to older age groups which was similar to other studies too [5, 6]. This indicated the fact that younger age groups, and especially males, are much more involved in injuries due to affinity toward high-velocity vehicles and interpersonal altercations.
Table 6.
Comparison between demographic variable age with cases of fracture, fracture etiology and orbital reconstruction
| Age (years) | Fracture | P value | |
|---|---|---|---|
| Conventional | Atypical | ||
| 19–39 | 60 | 129 |
0.05* (S) |
| 40–61 | 18 | 69 | |
| Age (years) | Etiology | P value | ||
|---|---|---|---|---|
| RTA | Fall | Violence | ||
| 19–39 | 137 | 23 | 29 | 0.06 |
| 40–61 | 51 | 15 | 21 | |
| Age (years) | Orbital reconstruction | P value | |
|---|---|---|---|
| Present | Absent | ||
| 19–39 | 13 | 176 | 0.73 |
| 40–61 | 7 | 80 | |
Table shows the comparison between age with cases of fracture, fracture etiology and orbital reconstruction. A comparative evaluation revealed significant difference between conventional and atypical fracture and age groups with majority of cases in the age group between 19 and 39 years showing fractures when compared to the other age group
Statistical test employed: Chi-square test statistically significant (s) P value ≤ 0.05
Table 7.
Comparison between demographic variable gender with cases of fracture, fracture etiology and orbital reconstruction
| Gender | Fracture | P value | |
|---|---|---|---|
| Conventional | Atypical | ||
| Male | 56 | 143 | 0.943 |
| Female | 22 | 55 | |
| Gender | Etiology | P value | ||
|---|---|---|---|---|
| RTA | Fall | Violence | ||
| Male | 137 | 26 | 36 | 0.856 |
| Female | 51 | 12 | 14 | |
| Gender | Orbital reconstruction | P value | |
|---|---|---|---|
| Present | Absent | ||
| Male | 16 | 183 | 0.413 |
| Female | 4 | 73 | |
Table shows the comparison between age with cases of fracture, fracture etiology and orbital reconstruction. A comparative evaluation revealed no significant difference between gender and other parameters
Statistical test employed: Chi-square test statistically significant (s) P value ≤ 0.05
Careful history taking, clinical evaluation still forms an important part of treatment planning. Although the treatment of ZMC fractures has been improved since last decades due to advent of miniplates and improved surgical approaches [1, 8], still the treatment of ZMC fractures with atypical fracture lines creates a tight spot for the treating surgeon.
Conclusion
ZMC injuries often require interdisciplinary approach for treatment and patient-specific treatment plan. By this study, we have tried to give an insight about new patterns of ZMC fractures in our centre and statistically correlated their etiology. RTAs are mostly associated with complex ZMC injuries requiring more number of fixation points and often floor repair. Thus, planning should start from the moment patient gives the cause of injury simultaneously combined with clinical, radiological findings.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Punit S. Dikhit, Email: dikhit.punit@gmail.com
Mounabati Mohapatra, Email: mounabatimohapatra@gmail.com.
Ashok Kumar Jena, Email: ashokkjena@yahoo.co.in.
Ankita Srivastava, Email: anksri1012@gmail.com.
References
- 1.Sharma R. Re: Retroseptal transconjunctival approach for fractures of the zygomaticomaxillary complex: a retrospective study. Br J Oral Maxillofac Surg. 2018;56:435–436. doi: 10.1016/j.bjoms.2018.03.017. [DOI] [PubMed] [Google Scholar]
- 2.Yamsani B, Gaddipati R, Vura N, Ramisetti S, Yamsani R. Zygomaticomaxillary complex fractures: a review of 101 cases. J Maxillofac Oral Surg. 2015;15:417–424. doi: 10.1007/s12663-015-0851-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ashwin DP, Rohit, Rajkumar GC. A study on assessing the etiology and different treatment modalities of zygomaticomaxillary complex fracture. Int J Contemp Med Res. 2017;4:1423–1430. [Google Scholar]
- 4.Singaram M, Vijaybala GS, Udhayakumar RK. Prevalence, pattern, etiology, and management of maxillofacial trauma in a developing country: a retrospective study. J Korean Assoc Oral Maxillofac Surg. 2016;42:174–181. doi: 10.5125/jkaoms.2016.42.4.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pandey S, Roychoudhury A, Bhutia O, Singhal M, Sagar S, Pandey RM. Study of the pattern of maxillofacial fractures seen at a tertiary care hospital in North India. J Maxillofac Oral Surg. 2013;14:32–39. doi: 10.1007/s12663-013-0578-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajanikanth K, Borle D, Bhola D, Shivam D. The pattern of maxillofacial fractures in central India A Unicentric retrospective study. IOSR J Dent Med Sci. 2014;13:28–31. doi: 10.9790/0853-131102831. [DOI] [Google Scholar]
- 7.Ellis E, El-Attar A, Moos KF. An analysis of 2,067 cases of zygomatico-orbital fracture. J Oral Maxillofac Surg. 1985;43:417–428. doi: 10.1016/s0278-2391(85)80049-5. [DOI] [PubMed] [Google Scholar]
- 8.Dyer PV. Experimental study of fractures of the upper jaw: a critique of the original papers published by René Le Fort. Trauma. 1999;1:81–84. doi: 10.1177/146040869900100110. [DOI] [Google Scholar]


