Abstract
Background:
Structural inequities have important implications for the health of marginalized groups. Neighborhood-level redlining and lending bias represent state-sponsored systems of segregation, potential drivers of adverse health outcomes. We sought to estimate the effect of redlining and lending bias on breast cancer (BC) mortality and explore differences by race.
Methods:
Using Georgia Cancer Registry data, we included 4943 non-Hispanic White (NHW) and 3580 non-Hispanic Black (NHB) women with a first primary invasive BC diagnosis in metro-Atlanta (2010–2014). Redlining and lending bias were derived for census tracts using the Home Mortgage Disclosure Act database. We calculated hazard ratios (HRs) and 95% confidence intervals (CIs) for the associations of redlining, lending bias on BC mortality and estimated race-stratified associations.
Results:
Overall, 20% of NHW and 80% of NHB women lived in redlined census tracts, and 60% of NHW and 26% of NHB women lived in census tracts with pronounced lending bias. Living in redlined census tracts was associated with a nearly 60% increase in BC mortality (HR=1.58, 95%CI=1.37–1.82) while residing in areas with substantial lending bias reduced the hazard of BC mortality (HR=0.86, 95%CI=0.75–0.99). Among NHB women living in redlined census tracts we observed a slight increase in BC mortality (HR=1.13, 95%CI=0.90–1.42); among NHW women the association was more pronounced (HR=1.39, 95%CI=1.09–1.78).
Conclusions:
These findings underscore the role of ecologic measures of structural racism on cancer outcomes.
Impact:
Place-based measures are important contributors to health outcomes; an important unexplored area that offers potential interventions to address disparities.
Keywords: Structural Racism, Health Disparities, Breast Cancer Mortality
INTRODUCTION
Place-based socio-ecologic inequities contribute to adverse health outcomes.(1–3) Structural racism encompasses inequitable macro-level social systems—such as housing, education, employment, criminal justice, and healthcare—that interact to reinforce inequities across race and ethnic groups.(4–6) These systemic inequities can lead to limited healthcare access, inadequate transportation, and fewer community resources.(4,6) Within a metropolitan area, neighborhood composition varies substantially. The presence of disadvantaged neighborhoods often have an increased burden of adverse health outcomes, not only for the residents of those areas, but the larger metropolitan area as well.(7) A holistic approach to uncovering health inequities is an important consideration in epidemiology; it may further our understanding of the structural and policy changes that can be implemented to reduce disease burden in a population—providing a broader range of intervention targets beyond the individual.
Two neighborhood-level factors that reflect systemic inequities include redlining—defined as the systematic denial of mortgages based on place, and lending bias—the systematic denial of mortgages based on a person’s race or ethnicity. Historically, redlining emerged in the 1930’s as part of a “state-sponsored system of segregation”, inhibiting the ability of predominately African American communities to successfully apply for mortgages.(8–10) Current day redlining is a concern for disadvantaged neighborhoods because it inhibits financial security and stability for residents, which are important contributors to health and wellbeing.(4) Lending bias encompasses a similar systematic denial of mortgages; however, it is specific to the applicant rather than place.(11,12) Examining the associations between redlining and lending bias and breast cancer mortality could provide new insights into how socio-contextual factors drive cancer disparities by place and race.
Persistent inequities in breast cancer outcomes between non-Hispanic black (NHB) and non-Hispanic white (NHW) women exist in the US.(13–15) Among NHB women diagnosed with breast cancer, documented disparities include those related to the initial cancer diagnosis (i.e., stage), tumor biology (i.e., molecular subtype), and first-line therapy (i.e., delays, adherence) which impact breast cancer mortality.(13,15) While these disparities are important for understanding health outcomes, they do not fully explain inequities by race.(13,16) The recent race/ethnic disparities highlighted by the COVID-19 pandemic demonstrate that structural inequities have dire consequences for minority groups.(17–19) Ecologic measures of structural disadvantage have been limitedly explored as potential drivers of adverse outcomes among women diagnosed with breast cancer. This study sought to evaluate the role of neighborhood-level redlining and lending bias on breast cancer mortality, and whether there were differences by race/ethnicity. Building upon the foundational work of Beyer and colleagues,(20) we aimed to understand how spatial measures of structural inequity impact breast cancer mortality among women living in the metropolitan-Atlanta area—a diverse city with racial segregation, neighborhood deprivation, and pronounced race disparities in breast cancer mortality.(13,21,22)
METHODS
Study Population
The Georgia Cancer Registry (GCR) is a statewide population-based registry that has collected nearly all cancer cases diagnosed among Georgia residents since January 1, 1995. Using this registry, we identified NHB and NHW women diagnosed with a first primary stage I–IV breast cancer diagnosis (International Statistical Classification of Diseases and Related Health Problems 10th revision [ICD-10] ICD-O-3=C50) occurring between January 1, 2010 and December 31, 2014. Women were included if they resided in the metropolitan Atlanta area at the time of diagnosis, which included Cobb, Clayton, DeKalb, Fulton, and Gwinnett counties. All other diagnoses were excluded, including those among other race/ethnic groups, patients aged <18 years, male patients, patients with a previous history of cancer or any secondary tumor diagnoses, and patients with in situ disease. Patients were also excluded if diagnosed solely by death certificate or if stage was missing in the registry. The Georgia Cancer Registry captures the address at the time of diagnosis for each cancer patient and geocodes all addresses to the census tract level. Census tracts generally encompass between 3,000–8,000 individuals and were originally designed to be relatively homogeneous units with respect to population characteristics, economic status, and living conditions.(23) This study was approved by Emory IRB (#00099875) and the Georgia Department of Public Health (#190805) and was conducted in accordance of the Declaration of Helsinki.
Exposure Assessment
Redlining and Lending Bias
We define redlining as a systematic denial of mortgage based on location. Neighborhoods are often defined based on the population characteristic or socioeconomic makeup of the geographical unit; thus, redlining is more specific to the neighborhood where the applicant intends to reside, rather than their race/ethnicity. We define lending bias as the systematic denial of mortgages to NHB applicants compared with NHW applicant in areas where they intend to reside, regardless of their current residence.
Redlining and lending bias were calculated based on a previously published methodologic approach by Beyer et al.(20) Briefly, data were abstracted from the national database established as part of the Housing Mortgage Disclosure Act (HMDA) for the years 2010–2014.(24,25) The HMDA was passed in 1975 as part of an effort to address mortgage discrimination. The database collects information on mortgage lending practices, including: location for which a mortgage was being requested (census tract); loan approval/denial; loan type (purchase/refinance) and amount; owner-occupancy; and the applicant’s race, sex, and income.
The redlining index was estimated as the odds of denial of a mortgage application for a residence inside the census tract compared to those outside of the census tract. In this way, the redlining index identifies areas that are less likely to receive mortgages compared to others within the metropolitan Atlanta area. The index centers around a value of one, which corresponds to an area that receives the same rate of mortgage approvals when compared to other areas in metropolitan Atlanta (Figure 1a). A value less than one means that applicants in the area are less likely to be denied, whereas a value greater than one means that applicants in the neighborhood are more likely to be denied mortgage applications than applicants in other areas.
Figure 1: Distribution of redlining and lending bias in the Metropolitan Atlanta area.
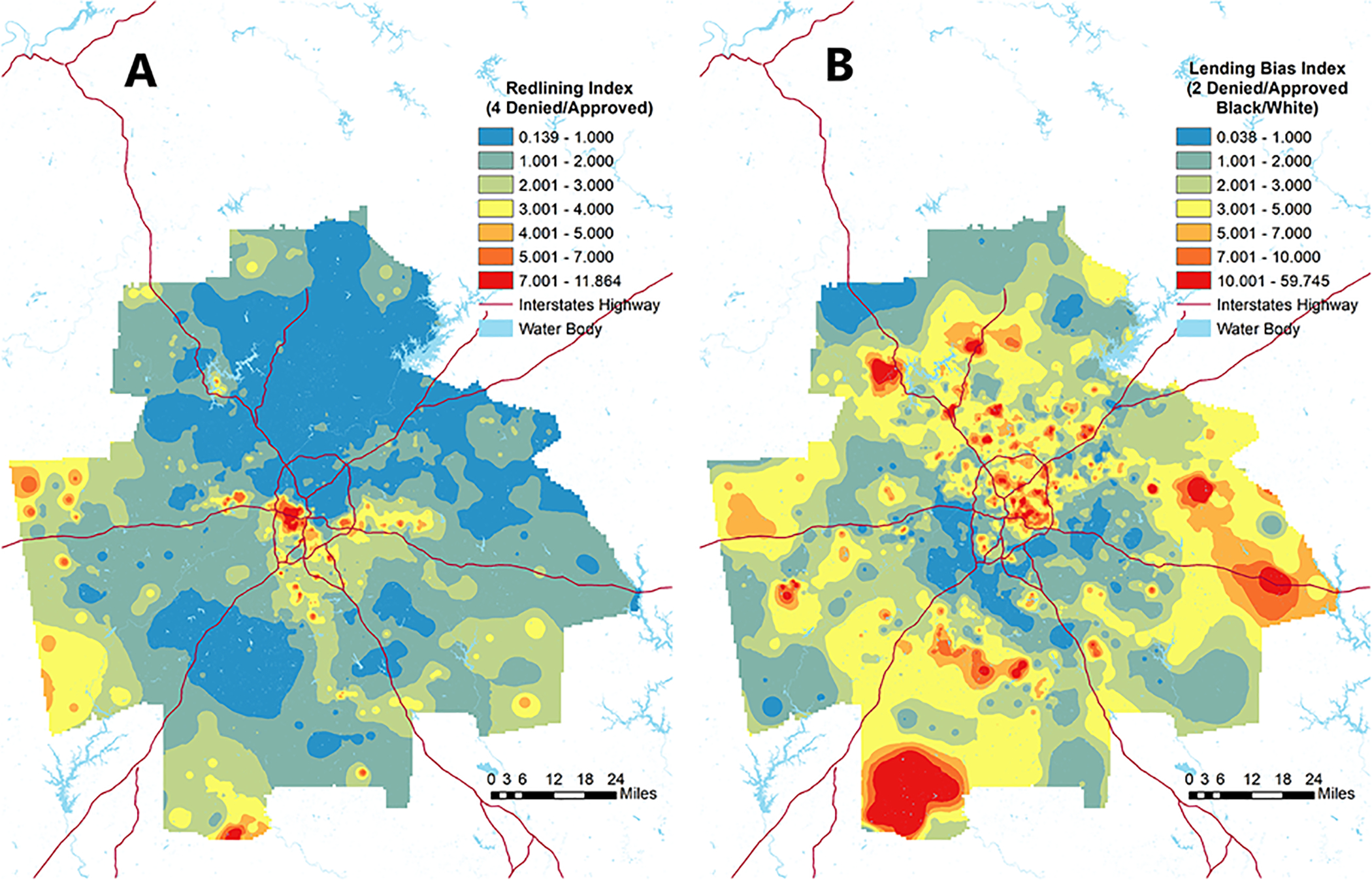
Figure 1 illustrates the distribution of (A) redlining, and (B) lending bias indices modeled using adaptive spatial filters in the Metropolitan Atlanta area (2010–2014).
Lending bias was similarly estimated as the odds of denial of a mortgage application from a NHB applicant compared to denial of a NHW applicant desiring to move in the same census tract, controlling for applicant sex and the ratio of the loan amount to applicants reported annual income (i.e. debt to income ratio). A value of one would indicate that NHB and NHW applicant have equal probability of being denied a mortgage application in the census tract of interest. The distribution of lending bias in the metropolitan Atlanta area had a median value of 3 (used as the cut point for high vs. low lending bias), which reflects a three-fold increase in the odds of mortgage denial for NHB applicants compared with NHW applicants. The odds ratios for redlining and lending bias were calculated using logistic regression with an adaptive spatial filter based on tract level data from the HDMA (Figure 1a and 1b). The centroid of the adaptive filter was then assigned as the value of redlining and lending bias to census tracts in the metropolitan-Atlanta area. Using the patient’s address at diagnosis, we then assigned the area level measures for redlining and lending bias to the patients residing in those census tracts.
Outcome Assessment
Underlying cause of death was determined directly from death certificates using ICD-10 codes. The GCR was linked to the Georgia vital statistics registry annually to identify deaths and causes of death from the preceding year. Additionally, the GCR was also linked to the US National Death Index each year to identify deaths that occurred outside of Georgia. In this study, we included only breast cancer related deaths (ICD-10=C50) recorded through December 31, 2016.
Covariates of Interest
Neighborhood Characteristics
Neighborhood characteristics were derived using publicly available data from the American Community Survey (ACS) and calculated at the census tract level using five-year estimates centered on 2012.(26) Characteristics included: proportion of the population identified as Black, percent of the population living below the federal poverty level, percent of population age 25 and older without a high school diploma, and median household income.
Patient Characteristics
We considered different patient demographic characteristics at the time of diagnosis that may relate to redlining, lending bias, and breast cancer mortality. Race and ethnicity were obtained from documentation in medical records using classifications similar to the 2010 Decennial Census.(27) When medical record data were not available, Hispanic ethnicity was determined by the North American Association of Central Cancer Registries Hispanic Identification Algorithm,(28) which uses a combination of variables routinely captured by registries (e.g., birthplace, race, and names) in addition to Hispanic surname lists from the US Census to classify women as Hispanic or non-Hispanic. Additionally, we included type of health insurance (uninsured, private, Medicaid, and Medicare), age at diagnosis (<40, 40–49, 50–65, >65 years), and marital status (married, single, divorced/widowed/separated), which are standard variables collected by the GCR.
Tumor Characteristics
Tumor characteristics used in this analysis included: cancer stage at diagnosis; tumor grade; expression of the estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor-2 (HER2), and extrapolated molecular subtype. Cancer stage at diagnosis was a derived variable based on the American Joint Committee on Cancer (AJCC) Staging Manual Seventh Edition using combined clinical and pathologic information. Tumor grade was categorized as 1, 2 or 3+ with priority coding for Nottingham or Bloom-Richardson scores/grades. Hormone receptor (HR) expression was classified as positive or negative based on the expression of ER (≥1%), PR (≥1%),, or both. HER2 expression was similarly classified as positive or negative through standard reporting to the GCR, based on summary of results from immunohistochemistry (3+), fluorescence in situ hybridization, or chromogenic in situ hybridization test results, and has been routinely collected by the GCR since 2010. Derived molecular subtype was based on the joint expression of HR and HER2: luminal A (HR+/HER2−), luminal B (HR+/HER2+), HER2 overexpressing (HR−/HER2+), and Triple Negative (TNBC), which corresponds to a lack of expression of either tumor biomarker (HR−/HER2−).
Statistical Methods
Descriptive statistics were calculated for covariates across categorizations of redlining (≥1 vs <1) and lending bias (≥3 vs <3) as median values with interquartile rage, or frequency and proportion within categories. We categorized redlining and lending bias as the approximate mean (1 and 3, respectively) based on the distribution observed in the study population for the purposes of the analysis (Supplemental Figures 1 and 2). Follow-up was defined as time in months, from the date of diagnosis until the first of a) mortality event, b) last date of contact in the registry, or c) December 31, 2016. We used age-adjusted and multivariable-adjusted Cox proportional hazard models to calculate the hazard ratios (HR) and 95% confidence intervals (CIs) for the association between neighborhood level redlining or lending bias and breast cancer mortality. We also calculated race-specific effects to explore potential differences in these associations by race (NHB and NHW), through inclusion of an interaction term and the common referent approach to calculate the departure from additivity based on the relative excess risk due to interaction (RERI). The 95%CI for the RERI was calculated using the variance-covariance estimates and the delta method. Potential confounders were determined a priori, based on previous literature and graphical based methods.(29) Our graphical assessment of potential confounders showed that all covariates of interest were on the causal path between redlining and breast cancer mortality (Supplemental Figure 3). These models were thus adjusted for age (continuous). We additionally report model results including age and stage adjustment. Final models for the association between lending bias and breast cancer specific mortality included age and stage based on graphical assessment (Supplemental Figure 4). All analyses were carried out using R version 3.6 and SAS version 9.4 (Cary, NC).
RESULTS
We identified 8,523 (3,580 NHB and 4,943 NHW) women diagnosed with a first primary breast cancer between 2010 and 2014 in the Metropolitan-Atlanta area (Table 1). On average, women were followed for 3.5 years, ranging 0–7 years. We observed 488 breast cancer deaths among NHB women and 319 breast cancer deaths among NHW women (Supplemental Table 1). In our study population, 3,871 (45%) and 3,843 (45%) patients resided at diagnosis in areas of redlining and high lending bias, respectively.
Table 1.
Patient demographic and clinicopathological characteristics among 8523 non-Hispanic White (NHW) and Black (NHB) women diagnosed with stage I-IV breast cancer in the metropolitan Atlanta area between 2010–2014 and registered with the Georgia Cancer Registry.
| Redlining | Lending Bias | |||||||
|---|---|---|---|---|---|---|---|---|
| <1 | ≥1 | <3 | ≥3 | |||||
| Neighborhood Characteristics | N | % | N | % | N | % | N | % |
| Percent Black | ||||||||
| ≥50% | 99 | 2.1 | 2948 | 76 | 2574 | 55 | 473 | 12 |
| <50% | 4553 | 98 | 923 | 24 | 2106 | 45 | 3370 | 88 |
| Percent Poverty | ||||||||
| ≥20% | 369 | 7.9 | 1957 | 49 | 1672 | 36 | 693 | 18 |
| <20% | 4283 | 92 | 1914 | 51 | 2969 | 64 | 3189 | 82 |
| Percent less than Highschool Education | ||||||||
| ≥20% | 124 | 2.7 | 911 | 26 | 1323 | 29 | 530 | 14 |
| <20% | 4528 | 97 | 2960 | 74 | 3318 | 71 | 3352 | 86 |
| Medium Household Income | ||||||||
| <$44,311 | 213 | 4.6 | 1915 | 49 | 1502 | 32 | 587 | 15 |
| $44,311- < $61,403 | 774 | 17 | 1355 | 35 | 1424 | 30 | 705 | 18 |
| $61,403 - <$84,497 | 1578 | 34 | 544 | 14 | 1157 | 25 | 1004 | 26 |
| ≥ $84,497 | 2087 | 45 | 57 | 1.5 | 597 | 13 | 1547 | 40 |
| Patient Characteristics | ||||||||
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | |
| Age at Diagnosis (years) | 58 | 49, 68 | 58 | 49, 67 | 58 | 49, 66 | 59 | 49, 68 |
| Length of Follow-up (months) | 44 | 30, 62 | 43 | 28, 61 | 44 | 28, 61 | 44 | 29, 62 |
| Time to event (months) | 23 | 12, 37 | 21 | 11, 33 | 21 | 12, 33 | 23 | 10, 36 |
| N | % | N | % | N | % | N | % | |
| Breast Cancer-Specific Death | 314 | 3.7 | 493 | 5.8 | 486 | 5.7 | 321 | 3.8 |
| Race/Ethnicity | ||||||||
| Non-Hispanic Black | 721 | 16 | 2859 | 75 | 2668 | 57 | 912 | 24 |
| Non-Hispanic White | 3931 | 85 | 1012 | 26 | 2012 | 43 | 2931 | 76 |
| Stage | ||||||||
| I | 2496 | 54 | 1628 | 42 | 2093 | 45 | 2031 | 53 |
| II | 1483 | 32 | 1395 | 36 | 1654 | 35 | 1224 | 32 |
| III | 427 | 9.2 | 522 | 13 | 586 | 13 | 363 | 9.4 |
| IV | 246 | 5.3 | 326 | 8.4 | 347 | 7.4 | 225 | 5.9 |
| Molecular Subtype | ||||||||
| HR+/HER2− (Luminal A) | 3260 | 75 | 2325 | 64 | 2936 | 67 | 2649 | 74 |
| HR+/HER2+ (Luminal B) | 496 | 11 | 461 | 13 | 553 | 13 | 404 | 11 |
| HR−/HER2+ (HER2 Overexpressing) | 175 | 4.1 | 182 | 5.0 | 205 | 4.7 | 152 | 4.3 |
| HR−/HER2− (Triple Negative) | 395 | 9.1 | 652 | 18 | 683 | 16 | 364 | 10 |
| Unknown | 326 | 251 | 303 | 274 | ||||
| Insurance Type | ||||||||
| Uninsured | 70 | 1.5 | 131 | 3.4 | 126 | 2.7 | 75 | 2.0 |
| Private | 3004 | 65 | 2050 | 53 | 2686 | 57 | 2368 | 62 |
| Medicaid | 186 | 4 | 469 | 12 | 453 | 9.7 | 202 | 5.3 |
| Medicare | 1295 | 28 | 1094 | 28 | 1266 | 27 | 1123 | 29 |
| Military/Other/Unknown** | 97 | 2.5 | 127 | 3.3 | 149 | 3.1 | 75 | 1.9 |
Mostly military; N=8 Other among NHB; N=0 Other among NHW
The spatial pattern of redlining and lending bias in Atlanta are illustrated in Figures 1a and 1b. Redlining is most prevalent in the southwest portion of the city inside the perimeter highway. On the other hand, racial lending bias is more prevalent in the northern and eastern parts of the metro area both inside and outside the perimeter highway as well as in the far southwestern and eastern regions of the metro area. Areas of redlining were more likely to be predominately Black neighborhoods (76% vs 2.1%), with a larger percent poverty (49% vs 7.9%), and a larger portion of the population without high school education (25% vs 2.7%) [Table 1]. Conversely, areas of high lending bias were more likely to have a low percent Black population (12% vs 55%), low poverty (18% vs. 36%), and low proportion of the population without a high school level educational achievement (14% vs. 28%).
Breast cancer characteristics also varied within neighborhood-level redlining and lending bias measures. Breast cancer patients residing in areas of high redlining at the time of diagnosis were more likely to have a stage IV diagnosis (8.4% vs. 5.3%), and TNBC (18% vs. 9.1%) compared with women residing in areas with low redlining (Table 1). In contrast, women residing in communities with high lending bias were more likely to have a stage I diagnosis (53% vs. 45%), and luminal A subtype (74% vs. 67%) compared with women living in neighborhoods with low lending bias.
Redlining and breast cancer mortality
In the age-adjusted model, for each 1-unit increase in the redlining metric we observed a 19% increase in the estimated mortality rate (HR=1.19, 95%CI 1.15, 1.24) [Table 2]. Comparing patients who resided in areas of redlining with those who did not (≥1 vs. <1) we observed a two-fold increase in the estimated breast cancer mortality rate (HR=1.97, 95%CI 1.71, 2.27). In models that additionally adjusted for stage, we observed similar, although attenuated, estimates of association (HR=1.58, 95%CI 1.37, 1.82). The association between redlining and breast cancer mortality differed by race/ethnicity. Among NHB women, each 1-unit increase in the redlining metric did not increase the estimated breast cancer mortality rate (HR=1.03, 95%CI 0.97, 1.08). Results were similar using a dichotomous classification of redlining (HR=1.08, 95%CI 0.86, 1.36) (Table 3). However, among NHW women, each 1-unit increase in the redlining metric was associated with a 28% increase in the estimated breast cancer mortality rate (HR=1.28, 95%CI 1.14, 1.44). Among NHW women, those who resided in areas of redlining had 1.6 times the estimated rate of breast cancer mortality (HR=1.60, 95%CI, 1.26, 2.04) compared with women who did not reside in redlined areas (≥1 vs. <1).
Table 2.
Hazard ratios (HR) and 95% confidence intervals (95% CI) for breast cancer-specific death according to census tract redlining and lending bias indices among non-Hispanic White (NHW) and non-Hispanic Black (NHB) women diagnosed with breast cancer in the metropolitan Atlanta area 2010–2014 and registered with the Georgia Cancer Registry.
| No. Deaths | Adjusted* | Adjusted** | |
|---|---|---|---|
| N | HR (95% CI) | HR (95% CI) | |
| Redlining Index | |||
| Continuous | |||
| Overall | 807 | 1.19 (1.15, 1.24) | 1.13 (1.08, 1.17) |
| NHB | 488 | 1.03 (0.97, 1.08) | 1.03 (0.97, 1.08) |
| NHW | 319 | 1.28 (1.14, 1.44) | 1.23 (1.08, 1.41) |
| Dichotomous | |||
| ≥1 | 493 | 1.97 (1.71, 2.27) | 1.58 (1.37, 1.82) |
| <1 | 314 | Referent | Referent |
| Lending Bias Index | |||
| Continuous | |||
| Overall | 807 | 0.93 (0.90, 0.97) | 0.95 (0.92, 0.99) |
| NHB | 488 | 1.03 (0.99, 1.07) | 1.00 (0.96, 1.04) |
| NHW | 319 | 0.93 (0.88, 0.99) | 0.96 (0.90, 1.02) |
| Dichotomous | |||
| ≥3 | 476 | 0.77 (0.66, 0.88) | 0.86 (0.75, 0.99) |
| <3 | 331 | Referent | Referent |
Age-adjusted
Age and stage adjusted
Table 3.
Hazard ratios (HR) and 95% confidence intervals (95% CI) for breast cancer-specific death according to census tract redlining and lending bias indices by non-Hispanic White (NHW) and non-Hispanic Black (NHB) women diagnosed with breast cancer in the metropolitan Atlanta area 2010–2014 and registered with the Georgia Cancer Registry.
| No. Deaths | Common Referent | RERI | Stratified Effects1 | Stratified Effects2 | |||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | (95% CI) | HR (95% CI) | HR (95% CI) | ||||
| Redlining Index | <1 | ≥1 | |||||
| NHB | 89 | 399 | 2.48 (1.93, 3.17) | 2.68 (2.28, 3.16) | −0.40 (−1.08, 0.29) | 1.08 (0.86, 1.36) | 1.13 (0.90, 1.42) |
| NHW | 225 | 94 | Reference | 1.60 (1.26, 2.04) | Reference | 1.60 (1.26, 2.04) | 1.39 (1.09, 1.78) |
| Lending Bias | <3 | ≥3 | |||||
| NHB | 141 | 178 | 1.62 (1.33, 1.97) | 1.75 (1.39, 2.22) | 0.21 (−0.82, 1.24) | 1.18 (0.97, 1.43) | 1.08 (0.89, 1.32) |
| NHW | 345 | 143 | Reference | 0.93 (0.74, 1.16) | Reference | 0.86 (0.69, 1.07) | 0.93 (0.74, 1.16) |
Age-adjusted
Age and stage-adjusted
Lending bias and breast cancer mortality
In the age-adjusted models, for each additional increase in unit of the lending bias metric, we observed a slight decrease in the estimated rate of breast cancer morality (HR=0.93, 95%CI 0.90, 0.97), which was similar to the multivariable-adjusted model (HR=0.95, 95%CI 0.92, 0.99) [Table 2]. Women who lived in neighborhoods of high lending bias (≥3 vs. <3) had 0.86 times the estimated rate of breast cancer mortality compared with those who did not (HR=0.86, 95%CI 0.75, 0.99). In the race-stratified models, there was no association between neighborhood lending bias and breast cancer mortality among NHB women (HR=1.00, 95%CI 0.96, 1.04) [Table 3]. Similarly, among NHW women, we observed a near null association for each unit increase in lending bias measure on breast cancer mortality (HR=0.96, 95%CI 0.90, 1.02).
DISCUSSION
This study reiterates established racial disparities in neighborhood measures of structural inequity, and relates these measures of structural inequities to their impact to breast cancer mortality. In our study, we observed that areas with current redlining had increased rates of breast cancer mortality, and areas with lending bias was associated with a decrease in the estimated rate of breast cancer mortality.
In the race-stratified models, the association between redlining and breast cancer mortality was more pronounced among NHW women compared with NHB women, and both estimates were lower than the estimate observed among all breast cancer patients. This is likely due to a combination of two factors. First, NHB women represent approximately 42% of the study population, yet of the 3,871 women who resided in redlined neighborhoods 2,859 (74%) were NHB women (Supplemental Table 1). Similarly, there were proportionately fewer NHW women living in redlined census tracts compared with NHB women (20% vs, 80%, respectively). As such, redlining is a common exposure among NHB women, but a rare exposure among NHW. Additionally, breast cancer deaths are more common among NHB women. The combination of these two prevalence estimates for exposure and outcome leads to ratios that are lower than the combined, but a higher estimated rate ratio among NHW women Among the total study population, lending bias was associated with a slight reduction in breast cancer mortality; however, in the race-stratified models, this association did not persist among women living in areas with high lending bias. This again may reflect the large proportion of NHW women living in areas with high lending bias (60%) compared with NHB women (40%).
Previous research suggests that discriminatory practices, such as racial bias by financial institutions, manifest biologically through stress pathways.(1) This stress may lead to epigenetic perturbations that adversely impact health outcomes, representing one mechanism via which structural inequities above the skin translate below.(30,31) In addition, residential segregation limits access to educational opportunities, greenspace,(32) healthy foods,(33) and healthcare, while increasing exposure to violence(34) and environmental injustice,(35) potentially augmenting differences by SES.(36) We observed differences in the role of redlining on breast cancer mortality between NHB and NHW women. The more pronounced association between redlining and breast cancer mortality among NHW women may be suggestive of resilience among NHB women,(37) or a protective community effect.(38,39) Importantly, it reiterates that race is a social construct, as NHW women exposed to equivalent economic, spatial, and social deprivation experience similarly poor outcomes. We observed lower estimated rates of breast cancer mortality with an increase in the lending bias metric. Communities with high lending bias are likely to have greater economic advantage, robust education and healthcare infrastructures, which would improve health outcomes for the women residing in those communities. Collectively, these factors influence discriminatory housing practices—facilitating residential segregation, a concentration of people of color in disadvantaged neighborhoods, and the eventual downstream adverse breast cancer outcomes among women residing in those areas.(40,41) These discriminatory housing practices do not exist only at the individual level and place, but are also built into institution mortgage lending practices. For example, documentation of biases in algorithms used to determine an applicant’s mortgage eligibility and interest rate have been widely reported, although there are efforts to ameliorate their use.(42,43)
In this study, a disproportionate number of NHB women lived in neighborhoods with high levels of structural racism. Descriptively, neighborhoods with higher redlining indices and lower lending bias tended to also be those with a larger proportion of the population living in poverty and with lower rates of high school level education. The confluence of these attributes contributes to adverse health outcomes. Neighborhood not only influences mortality but can also influence access to primary care, which increases the chance of early detection of a breast cancer via screening. We examined the stage distribution among census tracts contributing NHB vs. NHW cases only to explore if differences in breast cancer mortality were driven by stage at diagnosis, which would reflect barriers in access to screening rather than a direct association with breast cancer mortality. The stage distribution of census tracts where only NHB breast cancer cases were diagnosed had nearly the same stage distribution as NHB women from the larger cohort (Supplemental Table 2). However, the stage distribution among census tracts with only NHW breast cancer diagnoses had a slightly higher percentage of stage I diagnoses than from the larger cohort (58% vs. 55%). The similar stage distributions suggest that the associations observed in the current study are not due to differential screening access leading to later stage diagnoses among women residing in segregated census tracts. Future studies may benefit from further exploration of the neighborhood attributes to identify modifiable targets for intervention to improve breast cancer outcomes.
This study has numerous strengths. Namely, it employs an innovative application of a method to measure redlining and lending bias measures over space and time using publicly available data from the HDMA. This study expands on the previously reported study from Milwaukee, to a new region with a large, socioeconomically diverse population. Importantly, this study measures the impact of structural racism on overall health outcomes in both NHW and NHB breast cancer patients.
We acknowledge some important limitations of this study. First, the derived measures for redlining and lending bias were at the neighborhood-level census tract of the location where the mortgage was being sought, which we generalized to the individual. Given that we aimed to explore the role of neighborhood context on breast cancer outcomes, our approach was consistent with the study aims; although it does not account for patient mobility. Residential history may provide further insight as neighborhood-level effects can contribute to various health outcomes over the life course.(22) The metropolitan Atlanta area was ranked as one of the fastest growing cities in the US in 2016, resulting in a surge in housing cost,(44) which may disproportionally impact mobility by race and SES.(45) We also applied the measures to women residing in the census tracts, which implies that they either represent those who applied for and were approved for the mortgages, or that they rent in those neighborhoods. However, this does not change how the systemic denial of mortgages shapes these neighborhoods. Additionally, the metropolitan Atlanta area is quickly changing. Like other city centers, people are moving away from the suburbs, closer to the city center. This leads to rapidly changing neighborhoods and gentrification. For the redlining and lending bias indices, we used HDMA data centered on the breast cancer diagnostic years (2010–2014), which is most relevant to our study population, but may not capture changes leading up to that time period, or neighborhood changes after diagnosis. We did not have information on creditworthiness, which is likely an important indicator for mortgage denial in both the redlining and lending bias measures. Creditworthiness also has racial biases, which is separate from redlining and lending bias.(46) We also did not have individual measures of SES, comorbidities at diagnosis, or menopausal status which may be contribute to adverse outcomes; however, these are likely downstream of neighborhood characteristics and would not affect our reported results. Finally, the results presented in this study are from one metropolitan area, which may not generalize to other regions. However, Atlanta is a diverse city with structural inequities that are similar to those observed in other regions throughout the US.(4,21)
This study underscores the role of structural racism in adverse health outcomes, which are amenable to intervention. Specifically, it highlights how persistent structural biases, including those perpetuated by financial institutions, impact spatial patterns of concentrated poverty and neighborhood segregation; and how the construct of place filtered through those structural biases impacts individual and population health outcomes. Racial disparities in breast cancer mortality are often framed as an issue of race; yet, as recently highlighted through the COVID-19 pandemic, race simply reflects the systemic inequities experienced by a person across the life course.(17–19) Similarly, place-based disparities are a reflection of the unequal distribution of interpersonal and structural biases that are potentially modifiable through system- and policy-change. Thus, future research in this area should not only consider person-level determinants of adverse health outcomes, but additionally characterize the social contexts in which person-level factors are experienced—facilitating interventions across levels.
Supplementary Material
Acknowledgements
The authors acknowledge the contribution of Dr. Kevin Matthews for his support in the development and analysis of this project and manuscript.
Financial Support: This this work was supported, in part, by the Cancer Prevention and Control Research program, the Winship Research Informatics shared resources, a core supported by the Winship Cancer Institute of Emory University, and the Komen Foundation (CCR19608510) awarded to Lauren E McCullough. Lindsay J. Collin was supported by an award from the US National Cancer Institute (F31CA239566). This research was also supported by the National Cancer Institute R01CA214805 awarded to Kristen M Beyer. The collection of cancer incidence data used in this study was supported by contract HHSN261201800003I, Task Order HHSN26100001 from the NCI and cooperative agreement 5NU58DP003875-04 from the U.S. Centers for Disease Control and Prevention.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest.
References
- 1.Krieger N Discrimination and Health Inequities. Int J Health Serv 2014. October 1;44(4):643–710. [DOI] [PubMed] [Google Scholar]
- 2.Krieger N A glossary for social epidemiology. J Epidemiol Community Health. 2001. October;55(10):693–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carmona M Place value: place quality and its impact on health, social, economic and environmental outcomes. J Urban Des. 2019. January 2;24(1):1–48. [Google Scholar]
- 4.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017. April 8;389(10077):1453–63. [DOI] [PubMed] [Google Scholar]
- 5.Powell JA. Structural Racism: Building upon the Insights of John Calmore. N C Law Rev. 2007 2008;86:791. [Google Scholar]
- 6.Gee GC, Ford CL. STRUCTURAL RACISM AND HEALTH INEQUITIES. Bois Rev Soc Sci Res Race. 2011. April;8(1):115–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riley AR. Neighborhood Disadvantage, Residential Segregation, and Beyond—Lessons for Studying Structural Racism and Health. J Racial Ethn Health Disparities. 2018. April 1;5(2):357–65. [DOI] [PubMed] [Google Scholar]
- 8.Zenou Y, Boccard N. Racial Discrimination and Redlining in Cities. J Urban Econ. 2000. September 1;48(2):260–85. [Google Scholar]
- 9.Hillier AE. Redlining and the Home Owners’ Loan Corporation. J Urban Hist. 2003. May 1;29(4):394–420. [Google Scholar]
- 10.Wisniewski RE. Mortgage Redlining (Disinvestment): The Parameters of Federal, State, and Municipal Regulation. Univ Detroit J Urban Law. 1976 1977;54(2):367–430. [Google Scholar]
- 11.Kim S, Squires GD. Lender Characteristics and Racial Disparities in Mortgage Lending. J Hous Res. 1995;6(1):99–113. [Google Scholar]
- 12.Hubbard RG, Palia D, Yu W. Analysis of Discrimination in Prime and Subprime Mortgage Markets [Internet]. Rochester, NY: Social Science Research Network; 2011. November [cited 2020 Jun 24]. Report No.: ID 1975789. Available from: http://papers.ssrn.com/abstract=1975789 [Google Scholar]
- 13.Collin LJ, Jiang R, Ward KC, Gogineni K, Subhedar PD, Sherman ME, et al. Racial Disparities in Breast Cancer Outcomes in the Metropolitan Atlanta Area: New Insights and Approaches for Health Equity. JNCI Cancer Spectr [Internet]. 2019. September 1 [cited 2020 Apr 25];3(3). Available from: https://academic.oup.com/jncics/article/3/3/pkz053/5544721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeSantis CE, Ma J, Sauer AG, Newman LA, Jemal A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J Clin. 2017;67(6):439–48. [DOI] [PubMed] [Google Scholar]
- 15.DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, et al. Cancer statistics for African Americans, 2016: Progress and opportunities in reducing racial disparities. CA Cancer J Clin. 2016;66(4):290–308. [DOI] [PubMed] [Google Scholar]
- 16.Collin LJ, Yan M, Jiang R, Ward KC, Crawford B, Torres MA, et al. Oncotype DX recurrence score implications for disparities in chemotherapy and breast cancer mortality in Georgia. Npj Breast Cancer. 2019. September 26;5(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dorn A van Cooney RE, Sabin ML. COVID-19 exacerbating inequalities in the US. Lancet Lond Engl. 2020;395(10232):1243–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yaya S, Yeboah H, Charles CH, Otu A, Labonte R. Ethnic and racial disparities in COVID-19-related deaths: counting the trees, hiding the forest. BMJ Glob Health. 2020. June 1;5(6):e002913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anyane‐Yeboa A, Sato T, Sakuraba A. Racial disparities in COVID-19 deaths reveal harsh truths about structural inequality in America. J Intern Med [Internet]. [cited 2020 Jun 24];n/a(n/a). Available from: http://onlinelibrary.wiley.com/doi/abs/10.1111/joim.13117 [DOI] [PubMed] [Google Scholar]
- 20.Beyer KMM, Zhou Y, Matthews K, Bemanian A, Laud PW, Nattinger AB. New spatially continuous indices of redlining and racial bias in mortgage lending: links to survival after breast cancer diagnosis and implications for health disparities research. Health Place. 2016. July 1;40:34–43. [DOI] [PubMed] [Google Scholar]
- 21.Hayes MM. The Building Blocks of Atlanta: Racial Residential Segregation and Neighborhood Inequity. :93. [Google Scholar]
- 22.Kramer MR, Dunlop AL, Hogue CJR. Measuring Women’s Cumulative Neighborhood Deprivation Exposure Using Longitudinally Linked Vital Records: A Method for Life Course MCH Research. Matern Child Health J. 2014. February 1;18(2):478–87. [DOI] [PubMed] [Google Scholar]
- 23.Krieger N A Century of Census Tracts: Health & the Body Politic (1906–2006). J Urban Health. 2006. June 1;83(3):355–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhutta N, Popper J, Ringo D. The 2014 Home Mortgage Disclosure Act Data [Internet]. Rochester, NY: Social Science Research Network; 2015. November [cited 2020 Apr 26]. Report No.: ID 2975511. Available from: https://papers.ssrn.com/abstract=2975511 [Google Scholar]
- 25.Canner GB, Smith DS, Bowen NE, Benkoivic FM. Home Mortgage Disclosure Act: Expanded Data on Residential Lending. Fed Reserve Bull. 1991;77:859. [Google Scholar]
- 26.Survey P on the F and U of D from the AC, Statistics C on N, Education D of B and SS and, Council NR. Using the American Community Survey: Benefits and Challenges. National Academies Press; 2007. 355 p. [Google Scholar]
- 27.Humes K, Jones N, Ramirez R. Overview of race and Hispanic origin: 2010. US Census Bureau; 2011; [Google Scholar]
- 28.Howe HL. NAACCR Guideline for Enhancing Hispanic-Latino Identification: Revised NAACCR Hispanic/Latino Identification Algorithm [NHIA v2]. 2005.
- 29.Howards PP, Schisterman EF, Poole C, Kaufman JS, Weinberg CR. “Toward a Clearer Definition of Confounding” Revisited With Directed Acyclic Graphs. Am J Epidemiol. 2012. September 15;176(6):506–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dunkel Schetter C, Schafer P, Lanzi RG, Clark-Kauffman E, Raju TNK, Hillemeier MM. Shedding Light on the Mechanisms Underlying Health Disparities Through Community Participatory Methods: The Stress Pathway. Perspect Psychol Sci. 2013. November 1;8(6):613–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Szanton SL, Rifkind JM, Mohanty JG, Miller ER, Thorpe RJ, Nagababu E, et al. Racial Discrimination Is Associated with a Measure of Red Blood Cell Oxidative Stress: A Potential Pathway for Racial Health Disparities. Int J Behav Med. 2012. December 1;19(4):489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saporito S, Casey D. Are There Relationships Among Racial Segregation, Economic Isolation, and Proximity to Green Space? Hum Ecol Rev. 2015;21(2):113–32. [Google Scholar]
- 33.Goodman M, Lyons S, Dean LT, Arroyo C, Hipp JA. How Segregation Makes Us Fat: Food Behaviors and Food Environment as Mediators of the Relationship Between Residential Segregation and Individual Body Mass Index. Front Public Health [Internet]. 2018. [cited 2020 Jun 24];6 Available from: https://www.frontiersin.org/articles/10.3389/fpubh.2018.00092/full?report=reader [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krivo LJ, Peterson RD, Kuhl DC. Segregation, Racial Structure, and Neighborhood Violent Crime. Am J Sociol. 2009. May 1;114(6):1765–802. [DOI] [PubMed] [Google Scholar]
- 35.Russ Lopez. Segregation and black/white differences in exposure to air toxics in 1990. Environ Health Perspect. 2002. April 1;110(suppl 2):289–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep Wash DC 1974. 2001. October;116(5):404–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.RESISTANCE AND RESILIENCE: THE SOJOURNER SYNDROME AND THE SOCIAL CONTEXT OF REPRODUCTION IN CENTRAL HARLEM - ProQuest [Internet]. [cited 2020 Apr 26]. Available from: https://search.proquest.com/docview/205522361?pq-origsite=gscholar
- 38.Thorpe RJ, Brandon DT, LaVeist TA. Social context as an explanation for race disparities in hypertension: Findings from the Exploring Health Disparities in Integrated Communities (EHDIC) Study. Soc Sci Med 2008. November 1;67(10):1604–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davis R, Cook D, Cohen L. A Community Resilience Approach to Reducing Ethnic and Racial Disparities in Health. Am J Public Health. 2005. December 1;95(12):2168–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Braveman P, Gottlieb L. The Social Determinants of Health: It’s Time to Consider the Causes of the Causes. Public Health Rep. 2014;129(Suppl 2):19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic Disparities in Health in the United States: What the Patterns Tell Us. Am J Public Health. 2010. April;100(Suppl 1):S186–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bartlett R, Morse A, Stanton R, Wallace N. Consumer-Lending Discrimination in the FinTech Era [Internet]. National Bureau of Economic Research; 2019. June [cited 2020 Apr 26]. (Working Paper Series). Report No.: 25943. Available from: http://www.nber.org/papers/w25943 [Google Scholar]
- 43.Obermeyer Z, Powers B, Vogeli C, Mullainathan S. Dissecting racial bias in an algorithm used to manage the health of populations. Science. 2019. October 25;366(6464):447–53. [DOI] [PubMed] [Google Scholar]
- 44.Bureau UC. Census Bureau Reveals Fastest-Growing Large Cities [Internet]. The United States Census Bureau. [cited 2020 Jun 24]. Available from: https://www.census.gov/newsroom/press-releases/2018/estimates-cities.html [Google Scholar]
- 45.Hankins K, Puckett M, Oakley D, Ruel E. Forced Mobility: The Relocation of Public-Housing Residents in Atlanta. Environ Plan Econ Space. 2014. December 1;46(12):2932–49. [Google Scholar]
- 46.Faber JW. Segregation and the Geography of Creditworthiness: Racial Inequality in a Recovered Mortgage Market. Hous Policy Debate. 2018. March 4;28(2):215–47. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


