Abstract
Background
A De Garengeot hernia is a femoral hernia that contains the appendix. This rare type of hernia was first described by René-Jacques Croissant De Garengeot in 1731. Numerous case reports have been published since then, yet collective analysis about the presentation, diagnosis, management, and outcomes of patients with this unique hernia is lacking.
Methods
A systematic review was performed using PubMed, Google Scholar, Embase, and Web of Science for cases of De Garengeot hernias. Keywords searched included ”De Garengeot hernia” OR “femoral appendicitis” OR “femoral hernia appendix” OR “crural hernia appendix.” To facilitate review, a classification system was created based on the gross appearance of the appendix and related structures in the femoral hernia.
Results
Two hundred and twenty-two cases were identified in 197 manuscripts. Cases most commonly came from Europe but have been reported worldwide. There was a female predominance (n = 180, 81.1%) and the mean age at presentation was 69.8 years. The most common presenting symptoms were a groin bulge and groin tenderness (82.4%, n = 183 and 79.7%, n = 177, respectively). A groin bulge was observed on physical exam in 95.0% (n = 211) of cases, and erythema over the hernia was present in 33.3% (n = 74). A pre-operative diagnosis of a De Garengeot hernia was established with imaging in only 31.5% (n = 70) of cases. The most common surgical approach was through a groin incision. Complications occurred in 9.5% (n = 21) of cases, most commonly surgical site infections. The most common condition of the appendix was congested/inflamed, found in 44.1% (n = 98) of cases and corresponding to class 2A in the classification system devised.
Conclusions
Overall, De Garengeot hernias were found to be rare and clinically heterogeneous, as highlighted by our classification system. A systematic approach to categorizing this unique hernia may improve management decisions and help avoid complications.
Keywords: De Garengeot hernia, Femoral appendicitis, Femoral hernia appendix, Crural hernia appendix
The appendix protruding through a femoral hernia was first described by the French surgeon René-Jacques Croissant De Garengeot [1]. He described a 55-year-old woman, who developed tenderness and a bulge in her right upper thigh after lifting 24 lb of bread. The bulge was unable to be reduced and over the next 4 days the overlying skin became erythematous. The patient was thought to have an abscess and after a groin incision was made, a femoral hernia was encountered which contained foul-smelling purulent fluid and a structure that resembled a “finger” near the femoral vessels. The structure was reduced back into the peritoneal cavity and the wound was allowed to heal via secondary intention, and the patient made an adequate recovery in 6 weeks. In 1735, another French surgeon, Claudius Amyand, described the first reported appendectomy where the appendix protruded through an inguinal hernia [2]. In 1785, Hévin published the first paper describing the surgical management of femoral appendicitis [3]. The term “De Garengeot hernia” was first used by Akopian et al. who gave credit to De Garengeot as the first to describe this type of hernia [4]. De Garengeot hernias are rare, with an estimated incidence ranging between 0.15 and 5% of all femoral hernias [5–11].
Since the first description, numerous reports of appendix-containing femoral hernias have been published. In 1906, Wood published a manuscript describing 100 cases of the appendix entering a femoral hernia, with a brief description of each case [12]. Watson, in 1925, reviewed the literature and reported 217 cases and provided a brief description, including distribution of age, sex, duration of symptoms, and length of the appendix [13]. Since 1925, numerous English reviews of De Garengeot hernias have been published, but their sample size remains limited with none containing more than 90 patients [14–17].
In this review, we highlight a case of De Garengeot hernia, perform a systematic review of the literature since 1925, and propose a classification system for this unusual type of hernia. A deeper understanding of the diagnosis and treatment of this unique hernia will provide guidance for clinicians who may encounter it in the future.
Case description
A 66-year-old man presented to the emergency room with a two-day history of right groin pain and bulge. The patient was not able to reduce the bulge and was having normal bowel movements. He admitted to intermittent nausea, but denied vomiting, fevers, chills, or night sweats. He had a history of bilateral inguinal hernia repairs, with the right repaired via an open approach 30 years prior and the left repaired via an open approach six years prior. He was being worked up for a recurrence of the left inguinal hernia as an outpatient. On exam, his temperature was 36.4 °C, heart rate 94, blood pressure 105/76, and respiratory rate of 16. A 3 cm right groin bulge below the inguinal ligament was observed that was tender to palpation and without any associated skin changes. His white blood cell count was 11,200 per mm3. Given his previous inguinal hernia repair, a computed tomography (CT) scan with intravenous contrast was obtained which showed a right femoral hernia that contained a portion of the appendix which appeared dilated with adjacent peri-appendiceal fat stranding (Fig. 1).
Fig. 1.
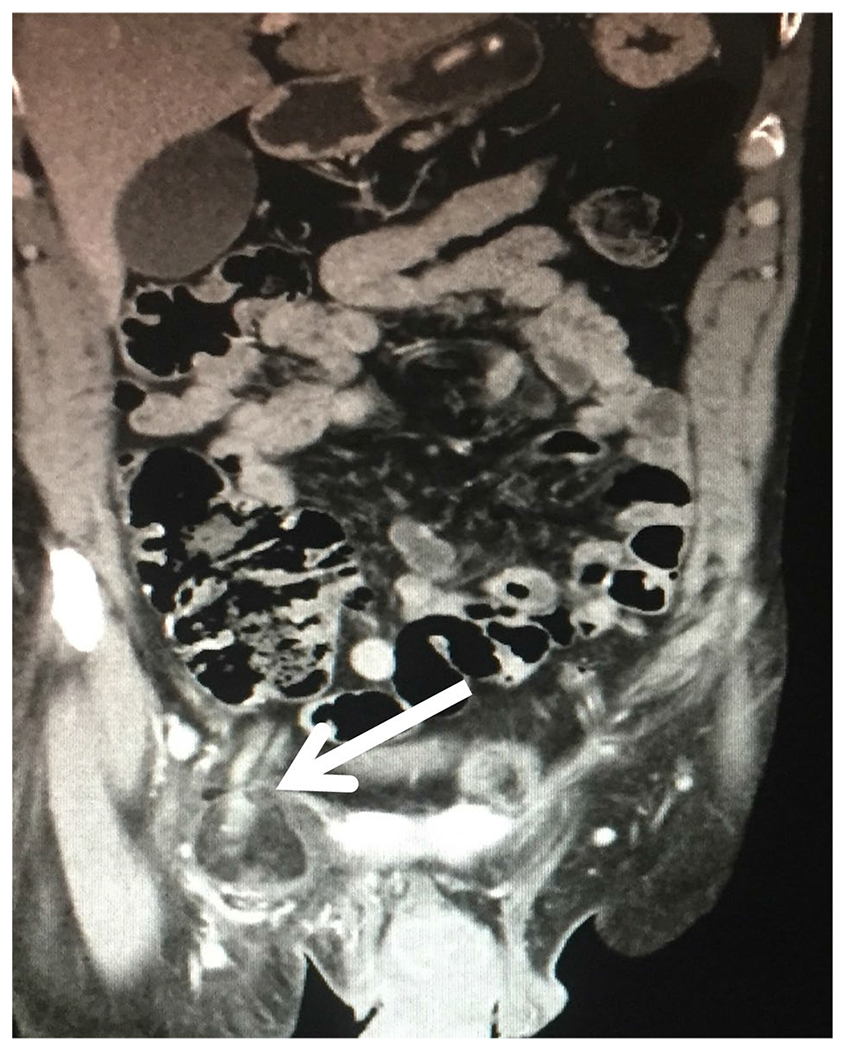
Pre-operative computed tomography showing the appendix (white arrow) within a right-sided femoral hernia
The patient was taken to the operating room for a right groin exploration. An incision was made just superior to the inguinal ligament. There was evidence of the prior inguinal repair without mesh and an infarcted appearing femoral hernia sac (Fig. 2). The sac was retracted cephalad to the inguinal ligament and opened to reveal a congested and inflamed appendix without evidence of perforation (Fig. 3). Gentle traction was applied to the appendix and the base of the cecum was easily drawn into the operative field. An appendectomy was performed, the cecum was reduced back into the peritoneal cavity, and the femoral hernia was closed using a McVay repair with interrupted 0-vicryl sutures. The skin was closed and no drains were left. The patient recovered well and was discharged on the second post-operative day. He was seen in clinic two weeks later with a well-healed wound without evidence of recurrence of the hernia. Pathologic examination of the appendix showed evidence of acute appendicitis.
Fig. 2.
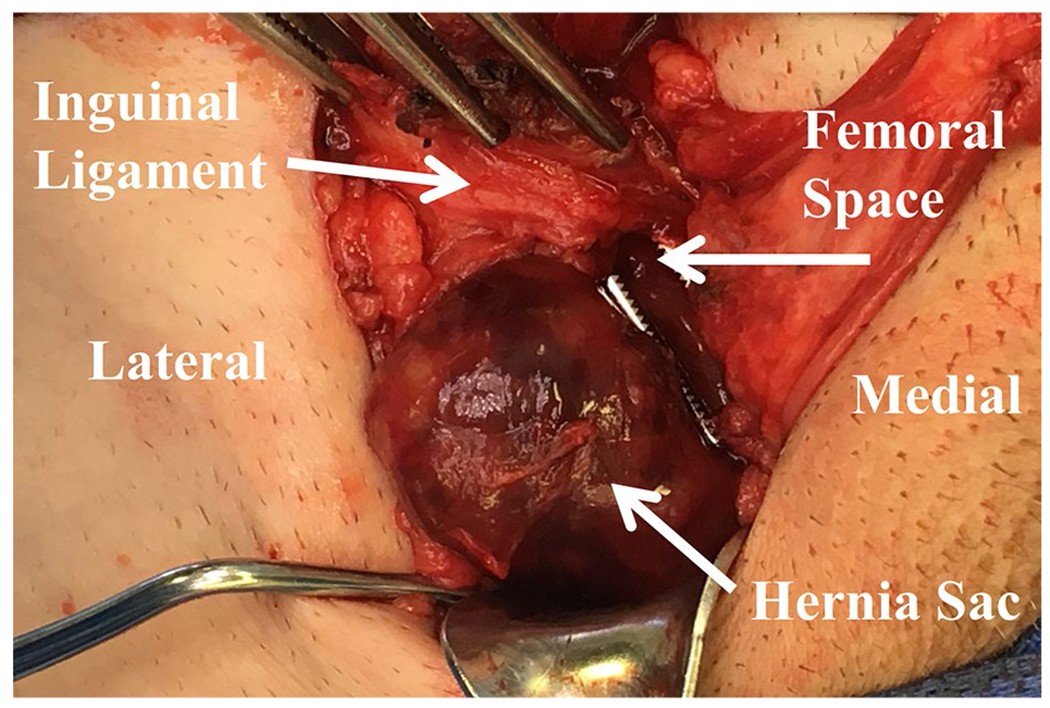
An intraoperative image showing the relationship of the incarcerated hernia sac to the inguinal ligament, thus confirming the diagnosis of a femoral hernia
Fig. 3.
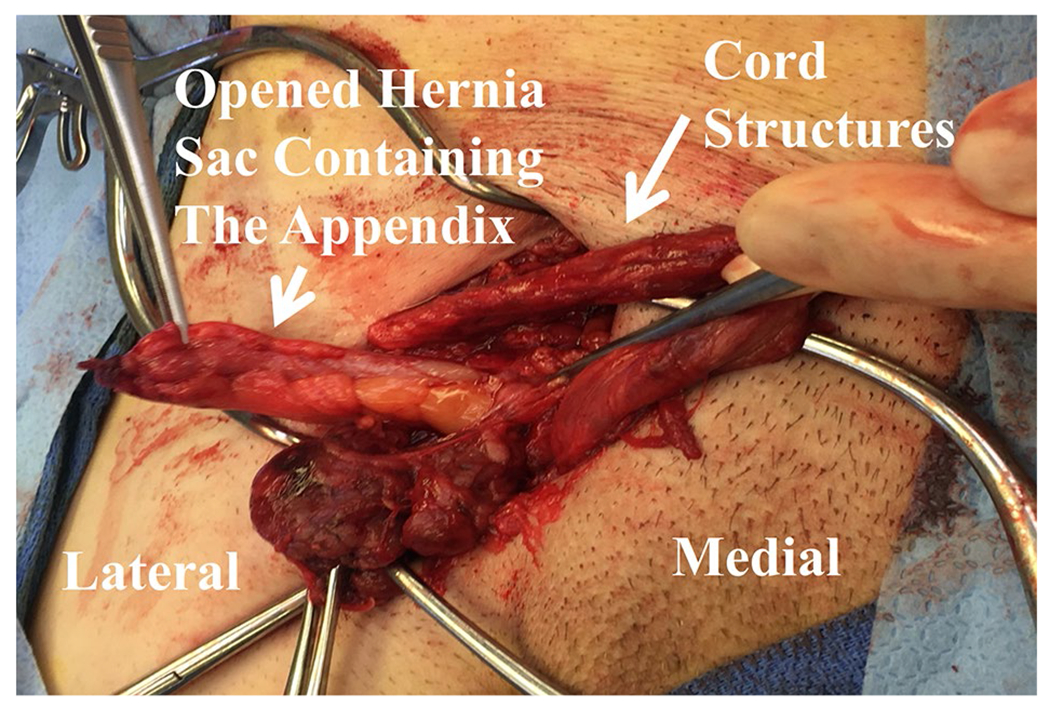
An intraoperative image showing an erythematous appendix found within the femoral hernia, thus confirming diagnosis of a De Garengeot hernia
Materials and methods
Literature search strategy
A systematic review was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) methodology for cases of De Garengeot hernias. Search engines utilized included PubMed, Google Scholar, Embase, and Web of Science. Keywords searched included “De Garengeot hernia” OR “femoral appendicitis” OR “femoral hernia appendix” OR “crural hernia appendix.” The search took place in June 2020.
Inclusion criteria
English language manuscripts were included if they described a case where the appendix protruded through a femoral hernia, thus establishing the diagnosis of a De Garengeot hernia. Additionally, the case report needed basic demographic information of the patient (age and sex), presenting symptoms and/or physical exam findings, and a gross description of the appearance of the appendix or related structures within the femoral hernia. References of all eligible manuscripts were reviewed for additional cases not found on the initial database query. Complications were noted and defined as surgical site infections, prolonged ileus, pneumonia, necrotizing soft tissue infection, reintubation, prolonged drainage from the wound, fascial dehiscence, or death.
Article selection
All cases were reviewed for eligibility independently by two reviewers. Discrepancies for inclusion or exclusion were resolved by consensus agreement.
Classification system
A classification system (Table 1) was created based on the gross appearance of the appendix and any other involved structures within the femoral hernia and applied to each case.
Table 1.
Classification of De Garengeot Hernia according to gross appearance of the Appendix
| Class | Description |
|---|---|
| Class 1 | Normal appearing appendix |
| Class 2 | |
| 2A | Erythematous, inflamed, or congested appendix |
| 2B | Erythematous, inflamed, or congested appendix |
| AND | |
| Erythema of the cecum or other segment of large or small intestine | |
| Class 3 | |
| 3A | Necrosis of the appendix, isolated to the tip |
| 3B | Necrosis of the appendix, involving the entire appendix |
| Class 4 | Necrosis of the appendix |
| AND | |
| Necrosis of the cecum or other segment of large or small intestine | |
| Class 5 | Perforated appendix, abscess, or fistula |
Statistical analysis
Data from each manuscript were collected by one reviewer and tabulated into a spreadsheet. Quantitative data were analyzed as median and interquartile ranges (IQR) and qualitative data were displayed as frequencies and percentages. Quantitative data were compared by Mann–Whitney-U test and proportions were compared using a Fischer’s exact test or Chi-square test. Significance was determined based on a p value < 0.05.
Results
Literature review
Three hundred and ninety-one manuscripts were identified on the initial search (PubMed: 170, Google Scholar: 108, Embase: 83, Web of Science: 30) (Fig. 4). After manuscripts were screened, assessed for eligibility, and references screened for additional reports, 197 manuscripts met the inclusion criteria (Supplement 1). Together with the case described, 222 cases of De Garengeot hernia were identified in this cohort.
Fig. 4.
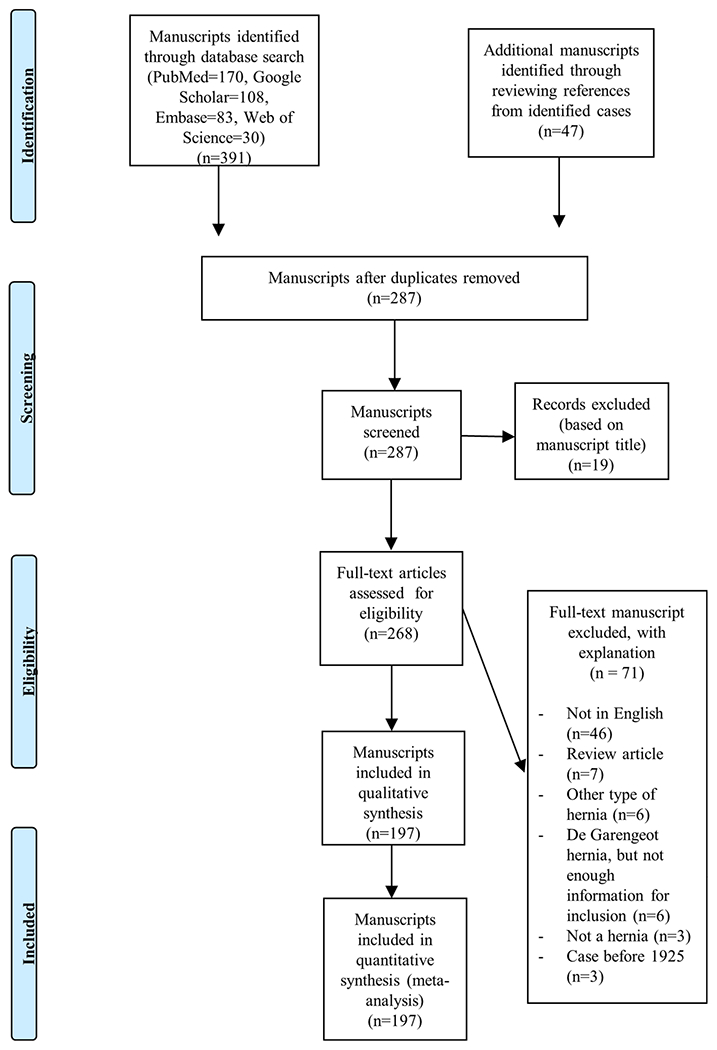
Flow diagram of systematic review for cases of De Garengeot hernias
The condition was more common in females (81.1%, n = 180) and the median age at presentation for all patients was 73 years (IQR 60–81) (Fig. 5). The median age at presentation for females was 73 (IQR 60–81) and for males was 72 years (IQR 61–83). Cases most commonly came from Europe (49.5%, n = 110), but cases were also described in North America (26.6%, n = 59), Asia (14.4%, n = 32), Australia (6.3%, n = 14), South America (2.7%, n = 6), and Africa (0.5% n = 1). The median year of publication was 2013 (IQR 2005–2016) (Fig. 6).
Fig. 5.
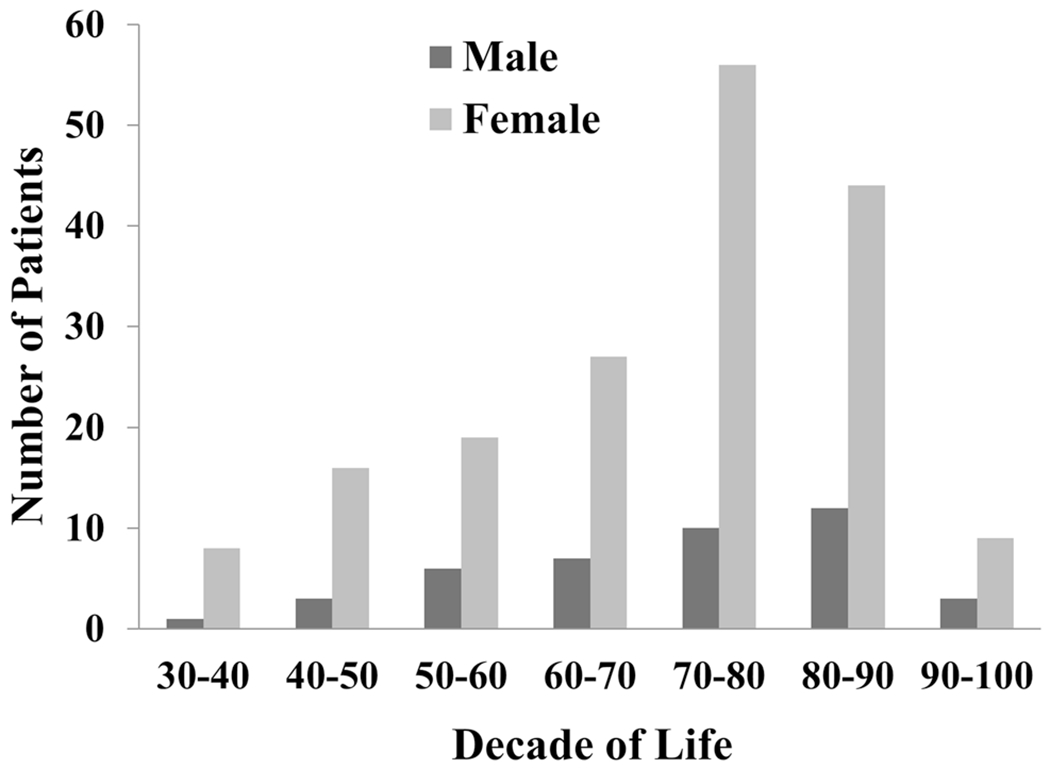
Age distribution for cases of De Garengeot hernias based on sex
Fig. 6.
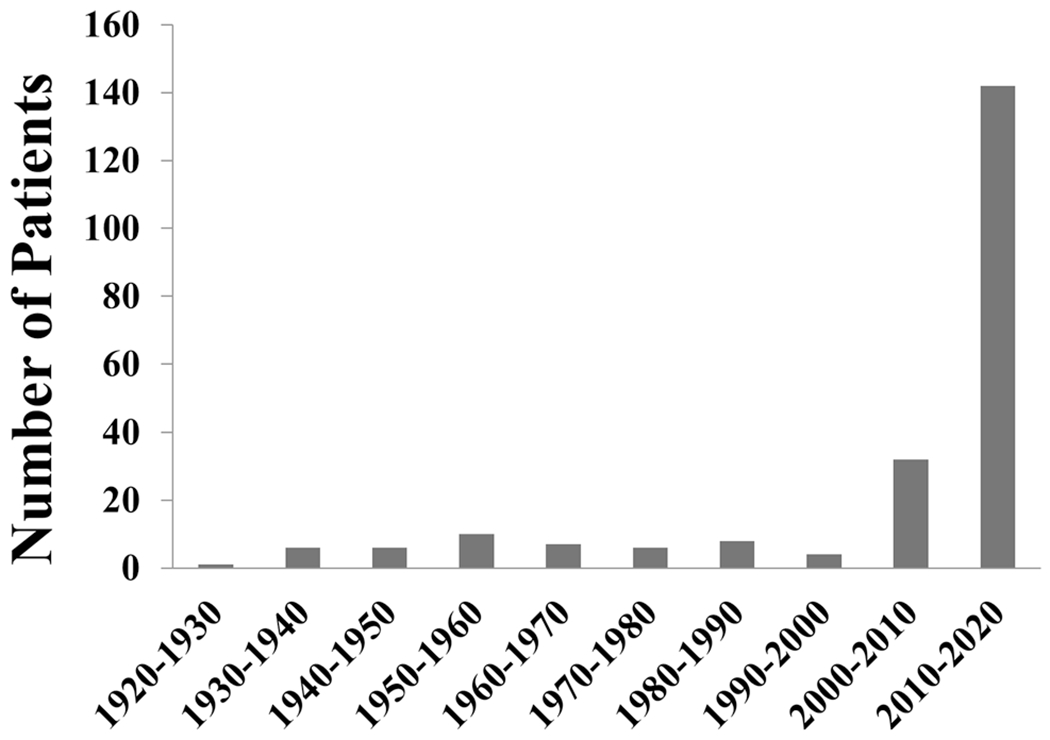
Distribution of cases of De Garengeot hernias based on decade
Symptoms and signs
The duration of symptoms was described in 80.2% (n = 178) of manuscripts with a median of 3 days (IQR 2–5). A groin bulge or groin pain were the most common presenting symptoms described by patients (82.4%, n = 183 and 79.7%, n = 177, respectively) (Table 2). A previous right-sided inguinal hernia repair was reported in 33.3% of men (n = 14) and 4.4% of women (n = 8). The median temperature on presentation was 37.4 °C (IQR 37–38.2, n = 48) and in 23 cases the patient was described as afebrile without a reported temperature reading. On physical exam, the most common findings were a groin bulge (95.0%, n = 211) and groin tenderness (86.5%, n = 192). Groin erythema was noted in 33.3% (n = 74) of cases. The white blood cell count was reported in 98 cases with a median of 11,950 per mm3 (IQR 9000–13,850).
Table 2.
Distribution of patient characteristics
| Variable | Percentage of all cases (n) |
|---|---|
| Presenting symptoms | |
| Groin bulge | 82.4% (183) |
| Groin pain | 79.8% (177) |
| Nausea/vomiting | 24.3% (54) |
| Abdominal pain | 22.5% (50) |
| Obstipation | 4.5% (10) |
| Diarrhea | 2.7% (6) |
| Abdominal distension | 2.3% (5) |
| Physical exam findings | |
| Groin bulge | 95.0% (211) |
| Groin tenderness | 86.5% (192) |
| Groin erythema | 33.3% (74) |
| Abdominal tenderness | 13.5% (30) |
| Surgical approach | |
| Isolated groin incision | 50.9% (113) |
| Combined groin incision/laparotomy | 7.7% (17) |
| Laparoscopic hernia repair with laparoscopic appendectomy | 5.9% (13) |
| Isolated McEvedy incision | 5.4% (12) |
| Groin incision and laparoscopic appendectomy | 5.4% (12) |
| Combined groin and McBurney incision | 5.4% (12) |
| Laparotomy only | 1.8% (4) |
| Complications | |
| Surgical site infection | 4.5% (10) |
| Prolonged ileus | 1.4% (3) |
| Necrotizing soft tissue infection | 1.4% (3) |
| Post-operative pneumonia | 0.9% (2) |
| Reintubation | 0.5% (1) |
| Prolonged drainage from wound | 0.5% (1) |
| Fascial dehiscence | 0.5% (1) |
| Death | 0.5% (1) |
Diagnosis
Diagnosis was most commonly made at the time of surgery (68.5%, n = 152), but 31.5% (n = 70) were diagnosed pre-operatively; most by CT scan (27.5%, n = 61), but ultrasound (2.3%, n = 5) and magnetic resonance imaging (MRI) were also used (1.8%, n = 4). The sensitivity of a CT scan to correctly diagnosis a De Garengeot hernia was 61% (61 true positive and 39 false negatives) and for MRI was 100% (4 true positives and 0 false negatives).
Operative approach
The most common approach for operative repair was an open surgery via isolated groin incision. Sixty nine percent of cases reported on the method of femoral hernia repair; primary suture closure was used in 47.3% (n = 105) of all cases and mesh repair in 21.6% (n = 48). A laparoscopic approach to the femoral hernia repair was performed in 11.3% (n = 25) of cases. In 200 (90.1%) cases, management of the appendix was described; an appendectomy performed in 98.5% (n = 197) of these cases. The most common route of appendectomy was through a groin incision (n = 128), and less commonly via laparotomy (n = 31), laparoscopy (n = 25), McBurney incision (n = 8), or undescribed route (n = 5).
Outcomes
The median hospital length of stay was 3 days (IQR 2–7), reported in 64.4% of cases (n = 143). The follow-up time interval was reported in 20.7% (n = 46) of cases (median 60 days, IQR 28–180). A complication was reported in 9.9% (n = 22) of cases. Cases with pre-operative diagnoses were more common in recent years (median year of publication 2016) than cases without pre-operative diagnoses (median year of publication 2011, p < 0.001). Patients with pre-operative diagnoses had a lower complication rate than patients diagnosed at surgery (2.9% vs. 13.2%, p = 0.016). The median hospital length of stay was also shorter in patients diagnosed pre-operatively (2 days (IQR 2–5) versus 3 days (IQR 2.8–7), p = 0.004). On subgroup analysis of manuscripts published after the year 2000 the mean hospital length of stay was 2 days (IQR 2–5) for patients with a pre-operative diagnosis and 3 days (IQR 2–6.5) for patients without a pre-operative diagnosis (p = 0.061).
On subgroup analysis of manuscripts published after the year 2000, the median hospital length of stay for patients undergoing a totally laparoscopic repair was 3 days (IQR 2–5.3, n = 10) and in those undergoing an isolated open groin incision was 3 days (IQR 2–5.8, n = 78) (p = 0.9). In that same cohort published after the year 2000, the complication rate in those undergoing totally laparoscopic repair was 0% (n = 13) compared to 12.1% (n = 107) with an isolated open groin incision (p = 0.36). In all patients, a neoplasm was reported in 5 cases (2.3%); one case of a low grade mucinous neoplasm [18], two cases of appendiceal adenoma [19, 20], one case of a malignant mucocele [21], and one case of appendiceal adenocarcinoma [22].
Classification system
The most common class of De Garengeot hernia based on our classification system was 2A (44.1%, n = 98) (Table 3). There was no association between patient sex and class of De Garengeot hernia based on our classification system (p = 0.88). The observed rate of erythema was significantly different between classes of the classification system (p < 0.001), with this finding present in 68.9% (n = 31) cases of patients with class 5 De Garengeot hernia compared to 6.3% of patients with class 1 (p < 0.001), 22.5% of class 2A (p < 0.001), 13.3% of class 2B (p < 0.001), 40% of class 3A (p = 0.02), 31.3% of class 3B (p = 0.016), and 42.9% of class 4 (p = 0.2). Mesh was used in varying rates in classes 1–3 (6.3–43.4% of cases) but was not used in any patients with class 4 or 5 hernias. Complications were most common in class 5 (22.2%).
Table 3.
Patient characteristics based on class of De Garengeot hernia
| Classification |
|||||||
|---|---|---|---|---|---|---|---|
| 1 | 2A | 2B | 3A | 3B | 4 | 5 | |
| Number of patients: n (% all patients) | 16 (7.2) | 98 (44.1) | 15 (6.8) | 25 (11.3) | 16 (7.2) | 7 (3.2) | 45 (20.3) |
| Male: n (% males) | 1 (2.3) | 23 (54.8) | 4 (9.5) | 1 (2.4) | 3 (7.1) | 1 (2.7) | 9 (21.4) |
| Female: n (% females) | 15 (8.3) | 75 (41.7) | 11 (6.1) | 24 (13.3) | 13 (7.2) | 6 (3.3) | 36 (20) |
| Age of patient, years: median (IQR) | 80.5 (74.3–84.0) | 71.5 (58.5–78.0) | 70.0 (61.0–82.5) | 66.0 (56.0–81.0) | 70.5 (59.8–81.5) | 73.0 (67.5–77.5) | 76.0 (67.0–83.0) |
| Duration of symptoms, days: median (IQR) | 3.5 (1.3–13.0) | 3.0 (2.0–5.0) | 3.0 (3.0–7.0) | 2.5 (1.0–4.0) | 3.0 (2.0–4.3) | 3.0 (1.8–6.5) | 4.0 (3.0–6.5) |
| Erythema: n (% patients in each class) | 1 (6.3) | 22 (22.4) | 2 (13.3) | 10 (40.0) | 5 (31.3) | 3 (42.9) | 31 (68.9) |
| WBC count (K/mm3): median (IQR) | 10.5 (9.8–11.3) | 11.0 (7.8–13.4) | 13.0 (10.0–15.3) | 12.6 (11.3–13.7) | 11.6 (8.8–13.5) | 22.3 (22.0–22.7) | 12.0 (11.0–19.5) |
| Use of mesh: n (% patients in each class) | 7 (43.8) | 32 (32.7) | 2 (13.3) | 6 (24.0) | 1 (6.3) | 0 (0) | 0 (0) |
| Any complication: n (% patients in each class) | 2 (12.5) | 7 (7.1) | 1 (6.7) | 0 (0) | 2 (12.5) | 0 (0) | 10 (22.2) |
| SSI: n (% patients in each class) | 1 (6.3) | 4 (4.1) | 0 (0) | 0 (0) | 1 (6.3) | 0 (0) | 4 (8.9) |
| LOS, days: median (IQR) | 2.0 (1.5–3.0) | 3.0 (2.0–5.5) | 4.0 (3.0–7.5) | 3.0 (2.0–4.0) | 3.0 (2.3–6.5) | 8.0 (5.5–15) | 7.0 (5.0–14.0) |
IQR interquartile range, WBC white blood cell, SSI surgical site infection, LOS length of stay
Discussion
A total of 222 cases of De Garengeot hernia were included in this systematic review, making it the largest review of this topic to date. Taken with the 217 patients identified by Wood in 1925, there are 439 cases of De Garengeot hernia in the English language literature. The number of publications reporting cases of De Garengeot hernias has risen considerably in recent years. We found that these hernias are most common in women, and patients most commonly present with a groin bulge or tenderness. Additionally, nearly 10% of patients in this series reported a prior right-sided inguinal hernia repair. De Garengeot hernias are less commonly diagnosed pre-operatively, only 31.5% in this review. The rate of pre-operative diagnosis may increase with more frequent use of imaging, but surprisingly the sensitivity of pre-operative CT scan in diagnosing a De Garengeot hernia was only 61% in this review. We present a classification scheme for De Garengeot hernias, based upon the appearance of the appendix at the time of operative repair, which can be used to systematically describe cases and understand the outcomes associated with each class of hernia.
The sex breakdown of De Garengeot hernias is similar to that reported in prior studies, and to published rates of femoral hernias in general [23]. In this series, we found that 81.1% of cases were female, which differs from the 1925 review which showed a female predominance of 97.8%. The reason for this change in distribution is unclear, but could be related to a bias towards publication of less common cases. Though these hernias are rare, they have been reported worldwide. Notably, 64% of cases were reported in the decade since 2010. The increased prevalence of cases of De Garengeot hernia in the medical literature in the past 10 years is likely multifactorial but could be related to increased awareness of the disease, improved diagnostic modalities, and an increase in the available journals for publication of such case reports.
Tenderness in the groin and a groin bulge were the most common presenting symptoms. These symptoms correlated well with exam findings, as groin tenderness or a groin bulge were seen in 86.5% and 95.0% of cases, respectively. These findings were consistent with previously published analysis of the presenting symptoms of a De Garengeot hernia [15, 16]. Groin erythema was seen in 33% of all cases and in 68.9% of patients with class 5 De Garengeot hernias, which contained a perforated appendix or abscess. This makes sense clinically, as a perforated appendix or abscess in or near the hernia sac will cause a more robust inflammatory response and can lead to the skin erythema. Abdominal pain was reported by 22.5% of patients and only 13.5% of patients had tenderness on abdominal palpation. An overall lack of abdominal symptoms, especially in some cases where the appendix was perforated, can likely be explained by the constrictive and narrow diameter of the femoral canal, which may prevent the spread of inflammation into the abdominal cavity [24–29].
This review found that 33.3% of males and 4.4% of females had undergone a previous right-sided inguinal hernia repair prior to the development of their De Garengeot hernia. This observation is consistent with a study that found a 15-fold higher incidence of femoral hernias in patients that had a prior inguinal hernia repair compared to patients without prior inguinal hernia repairs [30]. Interestingly, the occurrence of a femoral hernia after an inguinal hernia repair was found to be higher in males compared to females, which again parallels our findings. The mechanism of why a previous inguinal hernia repair would lead to an increased rate of femoral hernias is thought to be due to either (1) an underlying undiagnosed or misdiagnosed femoral hernia that was initially present or (2) a result of the repair of the inguinal hernia causing the femoral canal to widen, thus increasing the risk of femoral hernia development. In this cohort, a neoplasm was reported in 2.3% of appendiceal specimens removed. This appears to be similar to previously established incidences of appendiceal tumors in patients with appendicitis, and did not seem to be related to the occurrence of a De Garengeot hernia [31].
The pre-operative diagnosis of a De Garengeot hernia was established in 31.5% of cases, most commonly by a CT scan. CT was found to have a sensitivity of 61.0% in diagnosing De Garengeot hernia. This is much lower than the sensitivity of CT to diagnose routine abdominal appendicitis [32]. Many of the 222 patients presented with what appeared to be an incarcerated groin hernia and were urgently taken to the operating room without additional imaging. It has been postulated that in these cases, imaging delays operative intervention and isn’t warranted if strangulation or incarceration are suspected [33]. Surprisingly, pre-operative diagnosis of a De Garengeot hernia was associated with an overall lower complication rate and shorter hospital length of stay. It is possible that a pre-operative diagnosis may have affected the urgency of operative intervention, choice of peri-operative antibiotics, or the surgical management which may have led to improved outcomes. The association between a pre-operative diagnosis and shorter length of hospital stay also held true when excluding patients prior to the year 2000, when Takemura et al. described the first pre-operative diagnosis of a De Garengeot using CT [34].
Many theories regarding the pathophysiology of De Garengeot hernias have been postulated. The first is that the cecum in these patients is located low in the pelvis secondary to a form of intestinal malrotation, increasing the likelihood of the appendix entering the femoral canal [14, 35]. Second, a large mobile cecum can push the appendix into the pelvis, again increasing the chance of the appendix entering the femoral canal [14, 26, 36]. Third, a longer appendix has been postulated as a risk factor for a femoral appendix [37]. Priego et al. suggested that if the appendix incidentally entered a femoral hernia sac, it would be subject to trauma that could lead to adhesion formation and cause the appendix to remain stuck in the hernia sac [9]. De Garengeot hernias additionally represent a unique scenario where appendicitis can develop from extra-luminal compression from the narrow femoral canal, as opposed to the much more common etiology of routine abdominal appendicitis, whereby intraluminal obstruction from lymphoid proliferation or a fecalith leads to appendicitis [38].
Our proposed classification system listed in Table 1 is the first described classification system for De Garengeot hernias. A classification system exists for Amyand hernias (appendix within an inguinal hernia), but is based on the presence of appendicitis and abdominal sepsis [39]. The Amyand classification system may not be as clinically useful for De Garengeot hernias as the femoral hernia orifice may be smaller than the inguinal hernia orifice and thus prevent the development of abdominal symptoms. The distribution of cases based on our classification system was broad, but class 2A was found to be the most common. This class encompassed appendices which appeared erythematous from venous congestion due to either compression in a tight femoral canal or acute non-perforated appendicitis. The decision was made to group these two conditions together, as it is difficult to grossly distinguish the two at the time of surgery and definitive pathologic examination occurs well after surgical decisions are typically made.
A prior review of treatment strategies in 90 patients with De Garengeot hernias concluded that a standardized treatment approach was not feasible and each surgeon should choose the surgical technique that corresponded to their comfort level [17]. Given the rarity of the condition, no randomized control trial has occurred or will likely ever occur exploring treatment strategies and outcomes. Furthermore, the pre-operative diagnosis was only established in 31.5% of cases and most cases proceeded to the operating room with a presumptive diagnosis of an incarcerated femoral hernia. This makes precise treatment algorithms, even based on our proposed classification system, not practical for every possible clinical scenario. Formation of a classification system aids in establishing general guidelines that may aid surgeons diagnosing and treating rare types of hernias, and provides insight into the expected post-operative course, including hospital lengths of stay and post-operative complications. Although our analysis does not establish clear evidence for a superior method of repair, the following four items of consideration are meant to aid in the operative management of De Garengeot hernias.
Laparoscopic repair of a De Garengeot hernia should be considered, especially when the diagnosis is known pre-operatively in a clinically stable patient [40, 41]. However, laparoscopic repair of a De Garengeot hernia was not associated with a shorter hospital length of stay or decreased complication rates as is seen with laparoscopic techniques for abdominal appendicitis, but this may be due to the low numbers of laparoscopic repairs in this series. Laparoscopic repair should especially be used with caution if signs of appendiceal perforation or abscess formation are seen on CT scan (class 5) or skin erythema is present, as a total abdominal approach may not obtain complete source control in the groin if a localized abscess is present. The laparoscopic approach does provide the advantage of being able to evaluate the rest of the abdomen including the entire cecum and may also come with the other known benefits of laparoscopic surgery not assessed in this review, such as decreased post-operative pain and faster return to normal activities [42].
We recommend appendectomy for any case classified as Class 2 or higher; that is, for any non-normal appearing appendix. With a normal appearing appendix, one must take into consideration the patient’s age, co-morbidities, and potential need for future abdominal surgeries when deciding whether to perform an appendectomy [7]. An appendectomy was performed in 98.5% of cases in this review. Some advocate removing the appendix in all cases since microscopic ischemia cannot be detected at the time of surgery [9], however, transection of the appendix during a surgical operation has been associated with increase rates of non-fatal complications, such as wound infections [43].
When open repair is used, if the base of the appendix can be safely drawn into the operative field, entry into the abdomen may not be necessary. However, when the presenting clinical picture is suggestive of obstruction, pre-operative imaging demonstrates other contents besides the appendix within the femoral canal, or when the patient’s body habitus makes assurance of complete reduction of the femoral hernia uncertain, diagnostic laparoscopy can be performed to completely evaluate the remainder of the bowel and ensure full reduction of the femoral hernia into the peritoneal cavity.
If the clinical suspicion is low for a contaminated field, we advocate for placement of mesh, since mesh repair of a femoral hernia is associated with a lower hernia recurrence rate [23]. A feared complication of mesh placement is a mesh infection, but a surgical site infection was only seen in 3 patients that had surgical mesh placed [9, 44, 45], all of which were class 2A, and only one required explantation of the mesh [44]. The overall low rate of mesh infection can likely be attributed to clinician tendency for a tissue repair over placement of mesh in fields containing excessive inflammation or signs of active infection.
Limitations
There are several limitations of this review. First, all cases came from published case reports which introduces bias in two ways: (1) aspects reported in each case report are not standardized and (2) clinicians may be less likely to publish unfavorable outcomes, thereby skewing our results to reflect cases with positive outcomes. However, analysis of case reports represents the only current method to better understand the pathophysiology and management of rare conditions such as De Garengeot hernias [46]. Second, given the nearly 100 year inclusion period of cases since 1925, there have been great advances in aseptic technique, surgical technique, and the peri-operative care of patients that make collective analysis difficult. An attempt was made to account for this by taking the year of publication into consideration when analyzing aspects such as hospital length of stay, complication rate, and the effects of laparoscopic repair. Lastly, limiting our search to only English manuscripts both decreased the number of cases included, but also altered the geographic distribution of cases identified in this cohort.
Conclusions
De Garengeot hernias are a unique hernia with increasing prevalence in the English language literature. They most commonly affect females and patients between 60 and 90 years of age. A pre-operative diagnosis is made in one third of patients and is associated with a decreased complication rate and shorter length of hospital stay. The most common route of surgical management was through a groin incision, and an appendectomy was performed in 98.5% of patients. A classification system based on the gross appearance of the appendix and related structures within the femoral hernia was devised to help analyze outcomes and guide future operative decision-making. Lastly, management considerations for De Garengeot hernias are discussed based on this classification system.
Supplementary Material
Acknowledgments
Funding The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1 TR001860 for author CMT.
Footnotes
The work was presented at the 2019 Military Surgical Symposium, a break-out session of the Annual Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Meeting.
The title of the podium presentation was “De Garengeots Hernia: A Report of Two Cases, Analysis of 177 Published Cases, and Proposed Classification System”
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s00464-020-07934-5) contains supplementary material, which is available to authorized users.
Disclosures The views expressed in this material are those of the authors and do not reflect the official policy or opinion of the U.S. Government, Department of Veteran Affairs, the Department of Defense, or the Department of the Air Force. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Drs Guenther, Theodorou, Grace, Rinderknecht, and Wiedeman have no conflicts of interest or financial ties to disclose.
References
- 1.De Garengeot RJC (1731) Traité des operations de chirurgie 1edn
- 2.Amyand C (1735) VIII. Of an inguinal rupture, with a pin in the appendix coeci, incrusted with stone; and some observations on wounds in the guts. Philos Trans 39:329–342 [Google Scholar]
- 3.Hévin P, Simon J-F (1793) Cours de pathologie et de thérapeutique chirurgicales, chez Méquignon l’aîné [Google Scholar]
- 4.Akopian G, Alexander M (2005) De Garengeot hernia: Appendicitis within a femoral hernia. Am Surg 71:526–527 [PubMed] [Google Scholar]
- 5.Carey LC (1967) Acute appendicitis occurring in hernias: a report of 10 cases. Surgery 61:236–238 [PubMed] [Google Scholar]
- 6.Watkins RM (1981) Appendix abscess in a femoral hernial sac: case report and review of the literature. Postgrad Med J 57:306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hayakawa E, Hackett T (2015) Incidental finding of incarcerated De Garengeot hernia during laparoscopic cholecystectomy. Case Stud Surg 1:26 [Google Scholar]
- 8.Sharma H, Jha P, Shekhawat N, Memon B, Memon M (2007) De Garengeot hernia: an analysis of our experience. Hernia 11:235. [DOI] [PubMed] [Google Scholar]
- 9.Priego P, Lobo E, Moreno I, Sánchez-Picot S, Olarte MAG, Alonso N, Fresneda V (2005) Acute appendicitis in an incarcerated crural hernia: analysis of our experience Apendicitis aguda en una hernia crural incarcerada: análisis de nuestra experiencia. Rev Esp Enferm Dig 97:707–715 [DOI] [PubMed] [Google Scholar]
- 10.Wise L, Tanner N (1963) Strangulated Femoral Hernia appendix with perforated sigmoid diverticulitis. Proc R Soc Med 56:1105–1106 [PMC free article] [PubMed] [Google Scholar]
- 11.Ryan WJ (1937) Brief communications and case reports. Ann Surg 106:135–146 [PMC free article] [PubMed] [Google Scholar]
- 12.Wood AC (1906) IV Appendicular Femoral Hernia, with notes of 100 cases. Ann Surg 43:668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Watson LS (1924) Hernia, its anatomy, etiology, symptoms, diagnosis, differential diagnosis, prognosis, and operative treatment. Kimpton, London [Google Scholar]
- 14.Garcia-Amador C, De La Plaza R, Arteaga V, Lopez-Marcano A, Ramia J (2016) Garengeot’s Hernia: two case reports with CT diagnosis and literature review. Open Med 11:343–349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalles V, Mekras A, Mekras D, Papapanagiotou I, Al-Harethee W, Sotiropoulos G, Liakou P, Kastania A, Piperos T, Mariolis-Sapsakos T (2013) De Garengeot’s hernia: a comprehensive review. Hernia 17:177–182 [DOI] [PubMed] [Google Scholar]
- 16.Evangelos PM, Anna P, Anastasia P, Nikolaos M, Vasileia D, Nikolaos K, Theodore K, Nick Z, Anastasios M (2018) De Garengeot’s Hernia: report of a rare surgical emergency and review of the literature. Front Surg 5:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Linder S, Linder G, Mansson C (2019) Treatment of de Garengeot’s hernia: a meta-analysis. Hernia 23:131–141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ryan JW, Riordan I, Gorey T, Geoghegan T (2017) de Garengeot hernia with a mucinous neoplasm of the appendix, two clinical rarities combine to yield a first for the literature. BMJ Case Rep. 10.1136/bcr-2017-220830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yeh D, Abeysinghe J (2014) Rare case of a de Garengeot’s hernia. Eur J Surg Sci 5:77–80 [Google Scholar]
- 20.Suppiah A, Barandiaran J, Morgan R, Perry E (2008) First case of villous adenoma of the appendix leading to acute appendicitis presenting as strangulated femoral hernia: changes in management owing to concurrent adenoma. Hernia 12:95–98 [DOI] [PubMed] [Google Scholar]
- 21.Nayak IN (1974) Malignant mucocele of the appendix in a femoral hernia. Postgrad Med J 50:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spencer RF, Livingstone PD (1984) Unusual combined pathology in a femoral hernia. J R Coll Surg Edinb 29:255. [PubMed] [Google Scholar]
- 23.Hachisuka T (2003) Femoral hernia repair. Surg Clin N Am 83:1189–1205 [DOI] [PubMed] [Google Scholar]
- 24.Jin Z, Imtiaz MR, Nnajiuba H, Samlalsingh S, Ojo A (2016) De Garengeot’s hernia: two case reports with correct preoperative identification of the vermiform appendix in the hernia. Case Rep Surg 2016:2424657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Voitk JA, Macfarlane KJ, Estrada LR (1974) Ruptured appendicitis in femoral hernias: report of two cases and review of the literature. Ann Surg 179:24–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fukukura Y, Chang S (2005) Acute appendicitis within a femoral hernia: multidetector CT findings. Abdom Imaging 30:620–622 [DOI] [PubMed] [Google Scholar]
- 27.Grgić T, Šuvak I (2011) De Garengeot hernia- case report. Acta Chirurg 8:17–19 [Google Scholar]
- 28.Cutolo CL, Wasserman LI, Pinck AR, Mainzer AR (1978) Acute suppurative appendicitis occurring within a femoral hernia: report of a case. Dis Colon Rectum 21:203–204 [DOI] [PubMed] [Google Scholar]
- 29.Rose RH, Cosgrove JM (1988) Perforated appendix in the incarcerated femoral hernia. A place for preperitoneal repair. N Y State J Med 88:600. [PubMed] [Google Scholar]
- 30.Mikkelsen T, Bay-Nielsen M, Kehlet H (2002) Risk of femoral hernia after inguinal herniorrhaphy. Br J Surg 89:486–488 [DOI] [PubMed] [Google Scholar]
- 31.Connor SJ, Hanna GB, Frizelle FA (1998) Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum 41:75–80 [DOI] [PubMed] [Google Scholar]
- 32.Mun S, Ernst RD, Chen K, Oto A, Shah S, Mileski WJ (2006) Rapid CT diagnosis of acute appendicitis with IV contrast material. Emerg Radiol 12:99–102 [DOI] [PubMed] [Google Scholar]
- 33.Doddi S, Sagar V, Singhal T, Balakrishnan S, Smedley F, Sinha P (2010) Femoral hernia with a twist. Case Rep Med 2010:650829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Takemura M, Iwamoto K, Goshi S, Osugi H, Kinoshita H (2000) Strangulated femoral hernia containing gangrenous appendicitis: report of a case. Nihon Gekakei Rengo Gakkaishi 25:789–791 [Google Scholar]
- 35.Caygill P, Nair R, Sajjanshetty M, Francis D (2011) An unusual groin exploration: De Garengeot’s hernia. Int J Surg Case Rep 2:74–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kagan Coskun A, Kilbas Z, Yigit T, Simsek A, Harlak A (2012) De Garengeot’s hernia: the importance of early diagnosis and its complications. Hernia 16:731–733 [DOI] [PubMed] [Google Scholar]
- 37.Hao J, Yao J, Guo D, Sun W, Liang J, Jiang X (2014) De Garengeot hernia: the ultrasound and computed tomographic findings in an 81-year-old woman. Am J Emerg Med 32:486 e485–e486 [DOI] [PubMed] [Google Scholar]
- 38.Barbaros U, Asoglu O, Seven R, Kalayci M (2004) Appendicitis in incarcerated femoral hernia. Hernia 8:281–282 [DOI] [PubMed] [Google Scholar]
- 39.Losanoff JE, Basson MD (2007) Amyand hernia: what lies beneath—a proposed classification scheme to determine management. Am Surg 73:1288–1290 [PubMed] [Google Scholar]
- 40.Comman A, Gaetzschmann P, Hanner T, Behrend M (2007) DeGarengeot hernia: transabdominal preperitoneal hernia repair and appendectomy. JSLS 11:496–501 [PMC free article] [PubMed] [Google Scholar]
- 41.Beysens M, Haeck L, Vindevoghel K (2013) Laparoscopic appendectomy combined with TEP for de Garengeot hernia: case report. Acta Chirurg 113:468–470 [PubMed] [Google Scholar]
- 42.Biondi A, Di Stefano C, Ferrara F, Bellia A, Vacante M, Piazza L (2016) Laparoscopic versus open appendectomy: a retrospective cohort study assessing outcomes and cost-effectiveness. World J Emerg Surg 11:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wen SW, Hernandez R, Naylor CD (1995) Pitfalls in nonrandomized outcomes studies: the case of incidental appendectomy with open cholecystectomy. JAMA 274:1687–1691 [DOI] [PubMed] [Google Scholar]
- 44.Cordera F, Sarr M (2003) Incarcerated appendix in a femoral hernia sac. Contemp Surg 59:35–37 [Google Scholar]
- 45.Sinraj AP, Anekal N, Rathnakar SK (2016) De Garengeot’s hernia – A diagnostic and therapeutic challenge. J Clin Diagn Res 10:PD19–PD20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nakamura T, Igarashi H, Ito T, Jensen RT (2014) Important of case-reports/series, in rare diseases: using neuroendocrine tumors as an example. World J Clin Cases 2:608. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


