Abstract
The guiding principle of this synthesis is to organize research on predictors of BPD features within a developmentally specific framework (e.g. infancy, preschool, middle childhood, adolescence). In addition, studies are prioritized that have longitudinal and observational components. Based on current literature, a Developmental Cascade Model of BPD is offered in which specific difficulties during one developmental period contribute to specific difficulties in a succeeding period, resulting in increasingly broad areas of dysregulation over time. Furthermore, to address specificity, we contrast trajectories toward BPD with trajectories toward antisocial behavior, noting shared and divergent predictors. The review highlights the importance of locating research findings in relation to the competencies and challenges of particular developmental periods when modelling developmental trajectories toward BPD.
Keywords: borderline personality disorder, development, infancy, preschool, middle childhood
Theories of BPD have long conceptualized its etiology as partially rooted in family processes that affect early social-emotional regulation, rather than emerging in adolescence in response to new developmental stressors [1, 2]. Here, we will lay out a view of the tasks of each developmental period that need to be addressed in a developmentally grounded theory of BPD. Then we review and synthesize existing work within each developmental period, to build toward a Developmental Cascade Model for future work. Affirming the call by Musser et al. [3**], we emphasize research using prospective longitudinal designs and observational methods. We will not consider research on parental BPD because that literature does not yet identify which of the multiple risks associated with parental BPD might also be specific to the child’s pathway toward BPD.
1. A Developmental Psychopathology Perspective
The effective environment of an infant is vastly different from the effective environment of the same child even a few years later. To date, etiological theories of BPD have featured general factors posited to be critical to BPD across developmental periods, e.g. mentalization, invalidation, attachment, etc. However, a developmental psychopathology perspective would call for identifying the developmental transactions relevant to BPD that are being negotiated during each developmental period, as well as the period-specific deviations that might put the child on a pathway toward BPD [4]. To take account of the particular ecology of development in a given period. we will need different lenses and different methods of assessment for each period.
2. An Attachment Perspective
Given that most theories of BPD posit early deviations in the parent-child relationship as one contributor to BPD (e.g. Biosocial Developmental Model; Mentalization Model; Emotional Cascades Model; [2], observing changes in the parent-child relationship over time should play a pivotal role in our understanding of BPD. Through 40 years of observational studies, attachment research has codified risk-related profiles of parent-child interaction in the form of disorganized and controlling attachment behavior [5, 6, 7, 8]. Assessment of attachment relationships has now progressed well beyond infancy, so that changes in the quality of attachment can be tracked from infancy into early adulthood (e.g. [9, 10, 11*]).
3. Addressing Diagnostic Specificity
Stepp et al. [12] noted that “We are missing critical elements required to explain divergent trajectories for unique disorder outcomes (p. 320)”. Pathways to conduct problems and antisocial behavior have been well characterized in developmental research and include male gender, impulsivity, disorganized attachment in infancy, maltreatment, rejecting parenting, coercive parent-child interactions, negative attributions of mental states, low verbal skills, aggressive conduct problems, and increased association with antisocial peers (e.g. [13]. Thus, one useful target for specificity is to differentiate trajectories toward BPD from the already well-researched trajectories toward antisocial behavior.
4. Developmental Periods: Emerging Competencies and Deviations Predicting BPD Features
4.1. Infancy.
The overarching developmental achievement in infancy is effective emotion regulation within a secure relationship. Emotion regulation emerges when central caregivers respond sensitively and promptly to the infant’s emotional communications. A secure relationship in turn gives rise to epistemic trust in the caregiver. This early negotiation of the quality of trust and security possible in the relationship is thought to affect the infant at both behavioral and neurobiological levels, in part thorough epigenetic tuning in which the quality of care affects gene expression in the stress response pathways [14]. Disorganized attachment arises when the caregiver cannot provide minimal comfort and arousal regulation to the infant at times of stress [15].
Three prospective longitudinal studies have assessed prediction from aspects of the parent-infant relationship to BPD features in adolescence or young adulthood [16**, 17*, 18*]. All studies found some evidence of prediction from infant disorganization to later BPD features. Notably, infants who were disorganized but continued to approach the mother for care were particularly at risk for later suicidality [18*]. This specificity suggests that the infants most susceptible to later BPD may be those who have a greater need for relational soothing.
However, in all studies, parenting variables proved more predictive of BPD features than infant attachment [16**, 17*, 18*]. In infancy, maternal withdrawal was the only aspect of maternal behavior predictive of later BPD features and suicidality, while maternal negative-intrusiveness made no contribution to prediction [18*]. Notably, maternal withdrawal was predictive even after controlling for childhood maltreatment and for attachment disorganization in middle childhood [18*]. Further, the association between early maternal withdrawal and later suicidality was mediated by left hippocampal volume in adulthood [19*].
4.2. Preschool.
Crucial capacities relevant to BPD take shape during the preschool years. First, the capacity to mentalize unfolds over the years from two to six. By age three the child is aware that others’ feelings and desires differ from his/her own [20, 21], and by age five the child understands that others have potentially different thoughts and reasons supporting their different feelings [21, 22]. Social pretend play with peers also emerges and constitutes a particularly rich crucible for negotiating the differing perspectives of self and other in collaborative play [23]. In addition, with language emerges the capacity to attach attributes to the self, which constitutes one early foundation for a sense of personal identity [24]. Thus, the preschool period has implications for early deviations in mentalization, in emerging sense of self-identity, in attribution of negative motives to self and others, and in deficits in quality of negotiation with peers.
The parent’s sensitivity and emotional availability continue to be important, but now the parent must balance responsiveness to the child’s concerns with parental structure and limit-setting around the rights and needs of others. Parents who are more passive and withdrawn may abdicate the responsibility for structuring and guiding the child, while those who are more intrusive may interfere with the child’s developing autonomy and self-control. Given greater mentalizing capacities, some disorganized children attempt to exert control over the parent’s attention through either controlling-caregiving or controlling-punitive behavior or both [25], [26]. Abdication of a parental role is specifically predictive of the child’s attempting to maintain parental engagement through controlling-caregiving behavior [9]. Further, both maternal hostility and maternal boundary dissolution (parental abdication of a parental role) at 3 ½ were predictive of the child’s BPD features in adulthood [17*].
In path modelling using the large-sample Study of Early Child Care and Youth Development, insensitive parenting and parental depressive symptoms during the infancy/preschool period significantly predicted BPD features at age 15. However, based on a latent class analysis at age 4 ½, only the withdrawn parenting class, but not the hostile parenting class, significantly predicted BPD features. Controlling behavior at 3 ½ contributed to social/emotional dysregulation in middle childhood [16**].
4.3. Middle Childhood:
In middle childhood, children prefer peers to parents as companions [27]. Children are sensitive to being liked by others and are aware of their peers’ relative popularity [28]. They also have a number of strategies for negotiating peer conflict without resorting to aggression [23, 29]. Children in middle childhood are also aware of group and societal norms and strive to behave in accord with those norms [29]. In relation to mentalizing and emotion regulation, children are aware of multiple emotions toward the same event or person, prefer problem-solving as a coping strategy, and use volitional emotion regulation, purposefully modifying emotions using amplification, minimization, and other strategies [30, 31].
While parents are still primary sources of comfort, the attachment relationship becomes a collaborative alliance in which the child is using the parent as a resource rather than relying on the parent to solve his difficulties [27]. Parents now work with the child to solve the child’s problems, preparing the child to cope more independently in adolescence [27]. Disorganized and controlling attachment patterns continue to be salient in middle childhood, with mixed disorganized/controlling attachment behavior predictive of adult BPD features [18*]. Consistent with previous work on relational aggression [32], deviations in peer relationships in the form of bully-victimization were precursors to BPD features at age 11 and to self-harm by age 17 [33], [34]. In contrast, self-reported maternal hitting and punishing was not related to BPD features at age 11 [35*]. Similarly, relational aggression by boys and both physical and relational aggression by girls were related to BPD features at age 14 [36]. In a third sample, BPD features at 12 years were associated with lower IQs, less developed theory of mind, lack of self-control, and higher levels of impulsivity and externalizing and internalizing problems at age 5 [37]. Exposure to harsh treatment in the family through age 10 also predicted BPD features, but only when there was a family psychiatric history [37]. Also in relation to parenting, 10- to-12-year-olds were lowest in BPD features when parents were high in self-reported supportive socialization and/or low in non-supportive reactions and the child was low in emotional vulnerability [38*].
Importantly, however, social-emotional dysregulation in middle childhood (suicidality, peer conflict, bully-victim relations, intense anger) mediated the effects of earlier and concurrent insensitive parenting on BPD-related features at age 15 [16**]. In addition, self- representation at the age of 12 mediated the relation between attachment disorganization in infancy and adult BPD features [17*]. Both reports underscore the importance of middle childhood disturbance in mediating effects of earlier predictors.
4.4. Adolescence:
In adolescence, an enhanced focus on finding one’s place in relation to peers decreases the influence of parents [39]. Hormonal changes enhance interest in romantic relationships [40] and explorations of sexual and gender identity. Adolescents are also able to engage in enhanced levels of mentalizing, leading to increased self-consciousness [41, 42]. In addition, adolescents can generate increasingly differentiated strategies for regulating emotions [30], but emotion dysregulation in individuals experiencing BPD worsens in adolescence [43*]. Parenting strategies shift toward encouraging open communication with the adolescent to provide guidance, while supporting increased adolescent self-regulation and autonomy [31]. Parental emotional flexibility may be particularly relevant to managing the increased potential for parent-child conflict.
Adolescents with elevated BPD features may pose particular challenges for parents. In one noted study, time-specific elevations in BPD features predicted subsequent elevations in perceived parental harsh punishment or low warmth [44]. In addition, observed maternal psychological control was related to BPD features in adolescence (affective instability, negative relationships, and self-harm) [45]. Notably, there were no significant differences in validation or invalidation between mothers of daughters who engaged in self-injury relative to controls. However, maternal invalidation was associated with adolescent BPD features when adolescents also perceived their mothers as low in validation [46**]. Finally, both maternal insensitivity and maternal depressive symptoms at age 15 made significant contributions to age 15 BPD features, beyond the contributions of the same variables at earlier ages [16**].
Adolescents with BPD features exhibited more role confusion, hostility and disorientation during a conflict discussion with their mothers than did other adolescents [47]. Notably, hostility and disorientation, but not role-confusion, were also related to the severity of the adolescent’s childhood maltreatment [47]. In a second study, maternal boundary dissolution at age 13 also predicted BPD in adulthood [17*]. Finally, in young adulthood, women with a diagnosis of BPD were more likely to show disorganized attachment interactions with mothers compared to those with anxiety/depression or no diagnosis (OR = 7.80) [11**]. Regarding mentalizing, hypomentalizing in caregivers was related to adolescent BPD pathology via an effect on adolescent hypermentalizing, assessed by participants’ inferences about movie characters [48**]. Further, adolescents with BPD reported lower reflective functioning when compared to healthy adolescents [49]. Finally, identity diffusion was associated with BPD features among a sample of inpatient adolescents [50*].
5. Integration and Future Directions
5.1. Toward a Developmental Cascade Model of Pathways to BPD.
As reviewed above, developmental trajectories toward BPD are likely to involve a cascade of successive developmental deviations from infancy through adolescence. Potential contributors from each period are shown in Figure 1. Clearly, any such model remains tentative due to the sparse longitudinal data available. However, a more clearly specified period-specific developmental model can catalyze needed research to address gaps in our understanding.
Figure 1. Developmental Cascade Model of Trajectories Toward Borderline Personality Pathology.
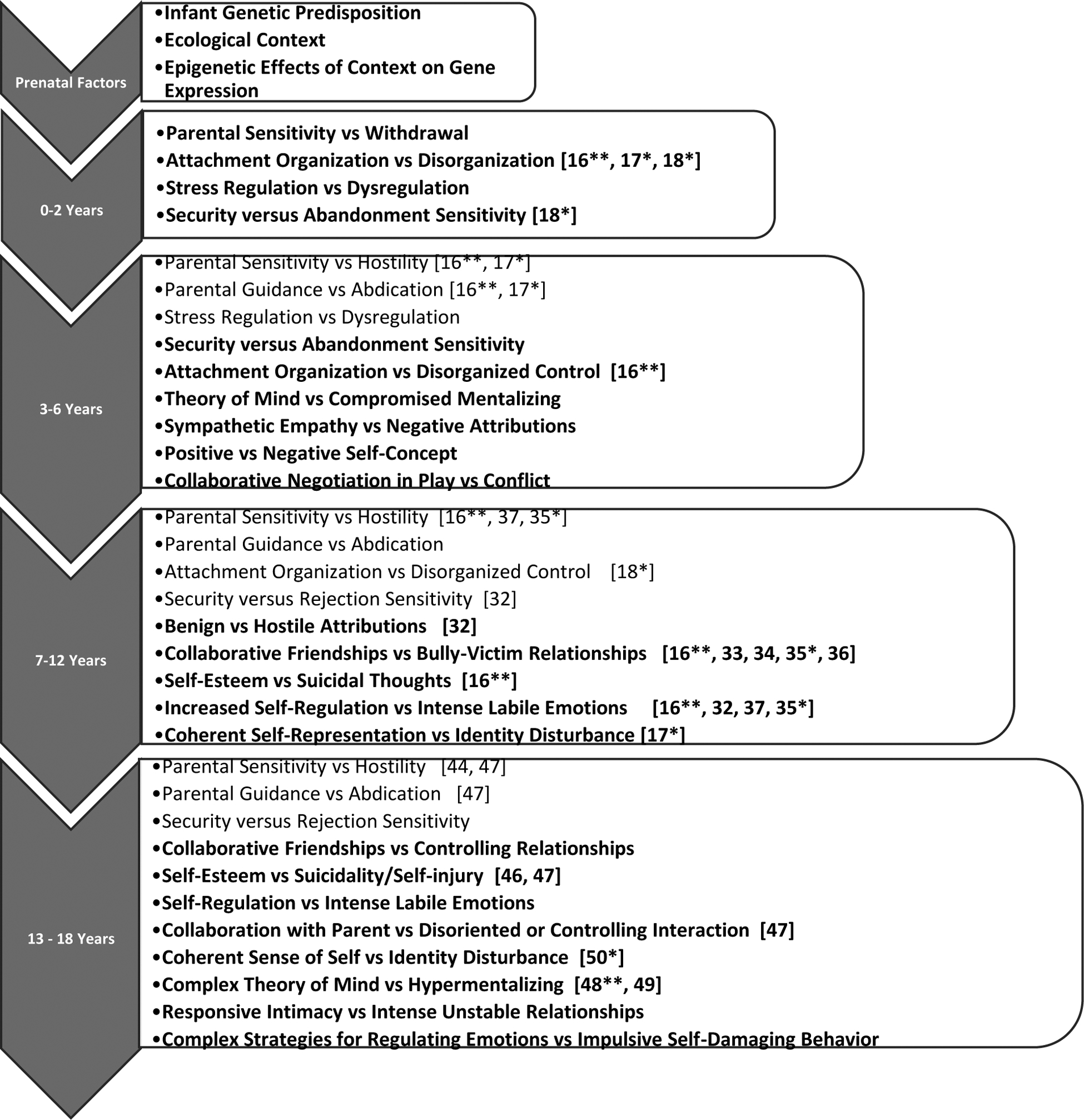
This tentative developmental cascade model summarizes the competencies and potential deviations being negotiated during particular developmental periods. As outlined above, early regulatory systems are set up in the first two years of life through transactions between the infant and the caregiving environment. Early dysregulations manifest in disorganized attachment relationships and prolonged cortisol elevations to stressors are likely to mediate the effects of prenatal factors on emerging competencies in the preschool period and compromise early mentalization, negotiation in peer play, and representations of self and others. By middle childhood, pervasive social-emotional dysregulation predicts later BPD features and mediates the effects of developmental deviations during earlier periods. Disorganized/controlling behavior toward both parents and peers is one feature of this dysregulation. By adolescence, with increased responsibility for self-directed choices, self-regulation deficits become prominent in a variety of impulsive, self-damaging behaviors, as well as suicidality, unstable relationships, and intense and labile affects. Relationships remain marked by disorganization and controlling behaviors, as well as hypermentalization and fears of abandonment, with diffusion of self-identity as one potential aspect of continued hypervigilance to the state of the other. Bolded competencies indicate new forms of functioning for each period. Citations are provided for studies addressed in this review. Earlier literature has already described impulsive self-damaging features of BPD in adolescence. However, a number of critical developmental competencies in each period have yet to be studied in relation to BPD, pointing the way to needed work.
5.2. BPD Trajectories Compared to Antisocial Pathways.
Relationship seeking and relationship reactivity are notable features of borderline psychopathology. In contrast, pathways to antisocial behavior feature impulsivity, disorganized attachment in infancy, maltreatment, rejecting parenting, coercive parent-child interactions, negative attributions of mental states, low verbal skills, aggressive conduct problems, and increased association with antisocial peers (e.g. [13]). The proposed developmental model for BPD differs in several ways that point to a more relationship-seeking stance across development. Early caregivers are likely to be more unavailable than hostile, and the infant more relationship-seeking than other disorganized infants. Early threats of abandonment (e.g. early caregiver withdrawal) may increase relationship-seeking to the caregiver (seek or squeak responses), while threats of attack (abuse) during later developmental periods may increase fight, flight, or freeze responses, possibly based on differential involvement of left versus right limbic structures [19*, 51, 52]. Thus, the balance of caregiver withdrawal versus hostility in early life may contribute to the child’s balance of continued care-seeking versus hostility and avoidance.
By preschool age, the caregiver may become increasingly hostile to the child’s developing autonomy but is also needy (boundary violating), in ways that may inhibit early coercive cycles with parents and draw the child into hypervigilance and attempts to care for the parent. By middle childhood, the tendency to become involved in controlling forms of relationship that are submissive or dominating now includes both parents (controlling-caregiving or controlling-punitive relationships) and peers (bully-victim relationships). These disorganized/controlling relationships with parents may also contribute to hypermentalizing (i.e. hypervigilance to the needs of the parent). Notably, child punitive control alone was not predictive of BPD [16**, 18*]. Thus, by middle childhood, those who will develop BPD may differ from those on pathways to antisocial behavior marked by coercive cycles with parents. Emotional dysregulation in the form of intense anger and suicidality also becomes more evident in middle childhood and may be reactive to peer relational conflicts.
In adolescence, the self-regulation deficits associated with early parental abdication of a regulating role become prominent due to the adolescent’s increased responsibility for self-directed choices. In addition, the tendency to engage in self-damaging behavior, rather than other-damaging, behavior, can be viewed, in part, as an attempt to both protect and engage the parent. Thus, we propose that one productive approach to diagnostic specificity may be to examine where pathways to BPD and to antisocial behavior diverge in the course of development.
5.3. Future Directions.
Metaanalysis has resoundingly confirmed the association between childhood maltreatment and BPD, with emotional abuse and overall neglect particularly relevant [53*]. In addition, type and timing of maltreatment, although challenging to assess accurately, are likely to make developmentally specific contributions to BPD that need to be modelled in future work. Finally, developmental models have most often featured behavioral/psychological outcomes. However, difficulties in navigating a particular developmental period will also have neurobiological effects, e.g. altered stress hormone regulation, altered immune function, alterations in brain white matter connectivity, grey matter volumes, synaptic pruning, etc., as captured most dramatically in current epigenetic work (e.g. [14]. Future work integrating neurobiological markers is needed to better model this complexity.
Highlights.
We discuss the tasks of each developmental period that need to be addressed in a developmentally grounded theory of BPD.
We synthesize existing longitudinal and observational work within each developmental period, to build toward a Developmental Cascade Model for future work.
We contrast trajectories toward BPD with trajectories toward antisocial behavior, noting shared and divergent predictors, to address specificity.
We note important future directions, including the need to assess type and timing of maltreatment and to integrate neurobiological markers in developmental models of BPD.
Acknowledgements
This work was funded by Grants MH035122 and MH062030 from the National Institute of Mental Health to K. Lyons-Ruth.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References and recommended reading
Papers of particular interest, published within the period of review, have been highlighted as:
* of special interest
** of outstanding interest
- [1].Linehan MM. Skills training manual for treating borderline personality disorder. : Guilford Press; 1993. [Google Scholar]
- [2].Winsper C The aetiology of borderline personality disorder (BPD): contemporary theories and putative mechanisms. Curr Opin Psychol. 2018;21:105–110. doi: 10.1016/j.copsyc.2017.10.005. [DOI] [PubMed] [Google Scholar]
- [3**].Musser N, Zalewski M, Stepp S, Lewis J. A systematic review of negative parenting practices predicting borderline personality disorder: Are we measuring biosocial theory’s ‘invalidating environment’? Clin Psychol Rev. 2018;65:1–16. doi: 10.1016/j.cpr.2018.06.003. [DOI] [PubMed] [Google Scholar]; A systematic review examining how closely parenting assessments predicting BPD align with Linehan’s theory of invalidation. The authors found that only two self-report instruments for invalidating parenting were closely aligned with Linehan’s definition.
- [4].Cicchetti D, Cohen DJ. Perspectives on developmental psychopathology. Oxford, England: John Wiley & Sons; 1995. p. 3–20. [Google Scholar]
- [5].Van IJzendoorn MH, Schuengel C, Bakermans-Kranenburg MJ. Disorganized attachment in early childhood: Meta-analysis of precursors, concomitants, and sequelae. Dev Psychopathol. 1999;11(2):225–250. doi: 10.1017/S0954579499002035. [DOI] [PubMed] [Google Scholar]
- [6].Cyr C, Euser EM, Bakermans-Kranenburg MJ, Van IJzendoorn MH. Attachment security and disorganization in maltreating and high-risk families: A series of meta-analyses. Dev Psychopathol. 2010;22(1):87–108. doi: 10.1017/S0954579409990289. [DOI] [PubMed] [Google Scholar]
- [7].Fearon RP, Bakermans-Kranenburg MJ, Van IJzendoorn MH, Lapsley A, Roisman GI. The significance of insecure attachment and disorganization in the development of children’s externalizing behavior: a meta-analytic study. Child Dev. 2010;81(2):435–456. doi: 10.1111/j.1467-8624.2009.01405.x. [DOI] [PubMed] [Google Scholar]
- [8].Madigan S, Brumariu LE, Villani V, Atkinson L, Lyons-Ruth K. Representational and questionnaire measures of attachment: A meta-analysis of relations to child internalizing and externalizing problems. Psychol Bull. 2016;142(4):367–399. doi: 10.1037/bul0000029. [DOI] [PubMed] [Google Scholar]
- [9].Bureau JF, Easterbrooks MA, Lyons-Ruth K. Attachment disorganization and controlling behavior in middle childhood: Maternal and child precursors and correlates. Attach Hum Dev. 2009;11(3):265–284. doi: 10.1080/14616730902814788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Obsuth I, Hennighausen K, Brumariu LE, Lyons-Ruth K. Disorganized behavior in adolescent–parent interaction: Relations to attachment state of mind, partner abuse, and psychopathology. Child Dev. 2014;85(1):370–387. doi: 10.1111/cdev.12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11**].Khoury JE, Zona K, Bertha E, Choi-Kain L, Hennighausen K, Lyons-Ruth K. Disorganized attachment interactions among young adults with borderline personality disorder, other diagnoses, and no diagnosis. J Personal Disord. 2019:1–21. doi: 10.1521/pedi_2019_33_408. [DOI] [PubMed] [Google Scholar]; Using observed conflict discussions, overall attachment disorganization (punitive control, role-confusion, and disorientation) was assessed among young adults with BPD diagnoses, with other diagnoses (anxiety/depression/substance use), and with no diagnosis. The odds ratio for disorganized attachment among BPD participants was almost 8 times that of participants without BPD.
- [12].Stepp SD, Lazarus SA, Byrd AL. A systematic review of risk factors prospectively associated with borderline personality disorder: Taking stock and moving forward. Pers Disord : Theory Res Treat. 2016;7(4):316. doi: 10.1037/per0000186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Dodge KA, Greenberg MT, Malone PS, Conduct Problems Prevention Research Group. Testing an idealized dynamic cascade model of the development of serious violence in adolescence. Child Dev. 2008;79(6):1907–1927. doi: 10.1111/j.1467-8624.2008.01233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Turecki G, Meaney MJ. Effects of the social environment and stress on glucocorticoid receptor gene methylation: A systematic review. Biol Psychiatry. 2016;79(2):87–96. doi: 10.1016/j.biopsych.2014.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lyons-Ruth K, Jacobvitz D. Attachment disorganization from infancy to adulthood: Neurobiological correlates, parenting contexts, and pathways to disorder. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. 3rd ed. New York, NY: Guilford; 2016. p. 667–695. [Google Scholar]
- [16**].Brumariu LE, Owen MT, Dyer N, Lyons-Ruth K. Developmental pathways to BPD-related features in adolescence: Infancy to age 15. J Personal Disord 2020. ;34(480):1–26. [DOI] [PubMed] [Google Scholar]; In a large-sample path model (N = 1364), parent and child relationship contributors to BPD features at age 15 were assessed in infancy/preschool, middle childhood, and adolescence. Parenting sensitivity was assessed from videotaped observations at all ages. Maternal insensitivity and maternal depression in all developmental periods influenced age 15 BPD features. However, the influence of early insensitivity was mediated through the child’s social-emotional dysregulation in middle childhood (intense anger, peer conflict, bully/victim relations, suicidal thoughts). Person-centered profiles revealed that early withdrawn parenting, but not hostile parenting, was predictive of BPD features at age 15. Child attachment was less influential than quality of parenting.
- [17*].Carlson EA, Egeland B, Sroufe LA. A prospective investigation of the development of borderline personality symptoms. Dev Psychopathol. 2009;21(4):1311–1334. doi: 10.1017/S0954579409990174. [DOI] [PMC free article] [PubMed] [Google Scholar]; In the pioneering Minnesota Longitudinal Study, relationship variables assessed for prediction of adult BPD features included infant attachment disorganization, infant maltreatment, maternal hostility (age 3 1/2), maternal boundary dissolution (role confusion; age 3 1/2), self-representation (age 12), sexualized maternal boundary dissolution (age 13), and maltreatment from ages 4 to 18. All variables were significant predictors. In addition, Teacher Report Form items at age 12 indexing attentional problems, impulsivity, emotional reactivity, and peer aggression were predictive. However, only self-representation at age 12 made a unique contribution to prediction and mediated the effect of attachment disorganization on adult BPD features.
- [18*].Lyons-Ruth K, Bureau JF, Holmes B, Easterbrooks A, Brooks NH. Borderline symptoms and suicidality/self-injury in late adolescence: prospectively observed relationship correlates in infancy and childhood. Psychiatry Res. 2013;206(2–3):273–281. doi: 10.1016/j.psychres.2012.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this 20-year prospective observational study, maternal withdrawal in infancy, but not other aspects of mothering, was a significant predictor of both borderline features and suicidality/self-injury in late adolescence. Disorganized-controlling child behavior in middle childhood added to the prediction of borderline features. The effect of maternal withdrawal was independent of variability explained by severity of childhood abuse. Notably, suicidality/self-injury was specifically predicted by infant disorganized-approach behavior toward mother.
- [19*].Khoury JE, Pechtel P, Andersen CM, Teicher MH, Lyons-Ruth K. Relations among maternal withdrawal in infancy, borderline features, suicidality/self-injury, and adult hippocampal volume: A 30-year longitudinal study. Behav Brain Res. 2019;374:112139. doi: 10.1016/j.bbr.2019.112139. [DOI] [PMC free article] [PubMed] [Google Scholar]; In a subsample of the Lyons-Ruth et al. (2013) participants, left hippocampal volume in adulthood was predicted by maternal withdrawal in infancy but not by other dimensions of disrupted parenting. Left hippocampal volume was also associated with increased BPD features and suicidality/self-injury. Severity of childhood maltreatment was not related to left hippocampal volume.
- [20].Tomasello M The cultural origins of human cognition. : Harvard University Press; 1999. [Google Scholar]
- [21].Wellman HM, Liu D. Scaling of theory-of-mind tasks. Child Dev. 2004;75(2):523–541. doi: 10.1111/j.1467-8624.2004.00691.x. [DOI] [PubMed] [Google Scholar]
- [22].Gopnik A & Slaughter V Young children’s understanding of changes in their mental states. Child Dev. 1991;62(1):98–110. doi: 10.2307/1130707. [DOI] [Google Scholar]
- [23].Howes C The Collaborative Construction of Pretend. NY: SUNY Press; 1995. [Google Scholar]
- [24].Calverley RM, Fischer KW, Ayoub C. Complex splitting of self-representations in sexually abused adolescent girls. Dev Psychopathol. 1994;6(1):195–213. doi: 10.1017/S0954579400005952. [DOI] [Google Scholar]
- [25].Main M, Cassidy J. Categories of response to reunion with the parent at age 6: Predictable from infant attachment classifications and stable over a 1-month period. Dev Psychol. 1988;24(3):415–426. doi: 10.1037/0012-1649.24.3.415. [DOI] [Google Scholar]
- [26].Moss E, Cyr C, Dubois-Comtois K. Attachment at early school age and developmental risk: Examining family contexts and behavior problems of controlling-caregiving, controlling-punitive, and behaviorally disorganized children. Dev Psychol. 2004;40(4):519–532. doi: 10.1037/0012-1649.40.4.519. [DOI] [PubMed] [Google Scholar]
- [27].Kerns KA, Brumariu LE. Attachment in middle childhood. In: Cassidy JA, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications New York, NY: Guilford Press; 2016. p. 349–365. [Google Scholar]
- [28].LaFontana KM, Cillessen AHN. Children’s perceptions of popular and unpopular peers: A multimethod assessment. Dev Psychol. 2002;38(5):635. doi: 10.1037/0012-1649.38.5.635. [DOI] [PubMed] [Google Scholar]
- [29].Rubin KH, Coplan R, Chen X, Bowker JC, McDonald K, Heverly-Fitt S. Peer relationships in childhood. In: Bornstein MH, Lamb ME, editors. Developmental science: An advanced textbook. 7th ed. New York: Psychology Press; 2015. p. 591–649. [Google Scholar]
- [30].Saarni C The development of emotional competence. : Guilford Press; 1999. [Google Scholar]
- [31].Denham SA. Emotional Competence During Childhood and Adolescence. Handbook of Emotional Development: Springer; 2019. p. 493–541. [Google Scholar]
- [32].Crick NR, Murray–Close D, Woods K. Borderline personality features in childhood: A short-term longitudinal study. Dev Psychopathol. 2005;17(4):1051–1070. doi: 10.1017/S0954579405050492. [DOI] [PubMed] [Google Scholar]
- [33].Lereya ST, Winsper C, Heron J, Lewis G, Gunnell D, Fisher H, et al. Being bullied during childhood and the prospective pathways to self-harm in late adolescence. J Am Acad Child Adolesc Psychiatry. 2013;52(6):608–618.e2. doi: 10.1016/j.jaac.2013.03.012. [DOI] [PubMed] [Google Scholar]
- [34].Wolke D, Schreier A, Zanarini MC, Winsper C. Bullied by peers in childhood and borderline personality symptoms at 11 years of age: a prospective study. J Child Psychol Psychiatry. 2012;53(8):846–855. doi: 10.1111/j.1469-7610.2012.02542.x. [DOI] [PubMed] [Google Scholar]
- [35*].Winsper C, Hall J, Strauss VY, Wolke D. Aetiological pathways to Borderline Personality Disorder symptoms in early adolescence: childhood dysregulated behaviour, maladaptive parenting and bully victimisation. Borderline Personal Disord Emot Dysregulation. 2017;4(1):10–10. doi: 10.1186/s40479-017-0060-x. [DOI] [PMC free article] [PubMed] [Google Scholar]; In addition, in the ALSPAC sample, negative emotionality, externalizing problems, and hyperactivity between 4 and 8 years also predicted age 11 BPD features, but this relation was mediated via an increased risk of middle childhood bully-victimization. Self-reported maternal parenting behaviors such as hitting and punishing at ages 8 and 9 were not related to BPD features.
- [36].Vaillancourt T, Brittain HL, McDougall P, Krygsman A, Boylan K, Duku E, et al. Predicting borderline personality disorder symptoms in adolescents from childhood physical and relational aggression, depression, and attention-deficit/hyperactivity disorder. Dev Psychopathol. 2014;26(3):817–830. doi: 10.1017/S0954579414000418. [DOI] [PubMed] [Google Scholar]
- [37].Belsky D, Caspi A, Arseneault L, Bleidorn W, Fonagy P, Goodman M, et al. Etiological features of borderline personality related characteristics in a birth cohort of 12 year old children. Dev Psychopathol. 2012;24(1):251–265. doi: 10.1017/S0954579411000812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38*].Dixon-Gordon KL, Marsh NP, Balda KE, McQuade JD. Parent emotion socialization and child emotional vulnerability as predictors of borderline personality features. J Abnorm Child Psychol. 2020;48(1):135–147. doi: 10.1007/s10802-019-00579-6. [DOI] [PubMed] [Google Scholar]; Among 10- to 12-year-olds, children were lowest in BPD features when parents were high in self-reported supportive emotion socialization reactions and/or low in non-supportive reactions and the child was low in emotional vulnerability (e.g., low negativity/lability and good emotion regulation skills reported by parents, or low skin conductance reactivity to stress during a simulated peer rejection task).
- [39].Allen J, Tan J. The multiple facets of attachment in adolescence. Handbook of attachment: Theory, research, and clinical applications. 2016:399–415. [Google Scholar]
- [40].Peper JS, Dahl RE. Surging hormones: Brain-behavior interactions during puberty. Curr Dir Psychol Sci. 2013;22(2):134–139. doi: 10.1177/0963721412473755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Fonagy P, Luyten P, Allison E. Epistemic petrification and the restoration of epistemic trust: A new conceptualization of borderline personality disorder and its psychosocial treatment. J Personal Disord. 2015;29(5):575–609. [DOI] [PubMed] [Google Scholar]
- [42].Selman RL. The development of interpersonal competence: The role of understanding in conduct. Dev Rev. 1981;1(4):401–422. doi: 10.1016/0273-2297(81)90034-4. [DOI] [Google Scholar]
- [43*].Chapman AL. Borderline personality disorder and emotion dysregulation. Dev Psychopathol. 2019;31(3):1143–1156. doi: 10.1017/S0954579419000658. [DOI] [PubMed] [Google Scholar]; This conceptual review explored the hypothesis that early impulse control problems are key indicators of a developmental trajectory toward emotional dysregulation (ED) and BPD. An invalidating environment may socialize the vulnerable child’s emotion regulation tendencies, shaping increasing emotional lability and dysregulation, and culminating in maladaptive coping behaviors in adolescence. The authors note that “one challenge moving forward is to assess where ED stops and BPD begins ”, given that aspects of ED are built into the criteria for BPD. Is ED a causal contributor or is it best characterized as a core feature of BPD?
- [44].Stepp SD, Whalen DJ, Scott LN, Zalewski M, Loeber R, Hipwell AE. Reciprocal effects of parenting and borderline personality disorder symptoms in adolescent girls. Dev Psychopathol. 2014;26(2):361–378. doi: 10.1017/S0954579413001041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Mahan RM, Kors SB, Simmons ML, Macfie J. Maternal psychological control, maternal borderline personality disorder, and adolescent borderline features. Pers Disord : Theory Res Treat. 2018;9(4):297. doi: 10.1037/per0000269. [DOI] [PubMed] [Google Scholar]
- [46**].McCallum M, Goodman SH. A multimethod, multi-informant investigation of maternal validation and invalidation of female adolescents who engage in self-inflicted injury. J Consult Clin Psychol. 2019;87(6):563. doi: 10.1037/ccp0000411. [DOI] [PubMed] [Google Scholar]; Although caregiver invalidation is a prominent candidate for contributing to BPD in offspring, mothers of adolescent daughters who engaged in self-injury did not engage in elevated levels of invalidation relative to controls, based on maternal and adolescent reports and observer ratings. However, for adolescent self-reported BPD features, adolescent perceptions of maternal invalidation were associated with BPD features when adolescents also perceived their mothers as low in validation, but not in the context of high maternal validation.
- [47].Lyons-Ruth K, Brumariu LE, Bureau JF, Hennighausen K, Holmes B. Role confusion and disorientation in young adult-parent interaction among individuals with borderline symptomatology. J Personal Disord. 2015;29(5):641–662. doi: 10.1521/pedi_2014_28_165. [DOI] [PubMed] [Google Scholar]
- [48**].Quek J, Bennett C, Melvin GA, Saeedi N, Gordon MS, Newman LK. An investigation of the mentalization-based model of borderline pathology in adolescents. Compr Psychiatry. 2018;84:87–94. doi: 10.1016/j.comppsych.2018.04.005. [DOI] [PubMed] [Google Scholar]; Among a sample of adolescents with BPD and a sample of non-clinical adolescents (14 to 17 years), hypomentalizing in caregivers was related to adolescent borderline pathology via an effect on adolescent hypermentalizing. Mentalization was assessed by inferences of mental states of characters in a 15-minute film (the MASC).
- [49].Quek J, Melvin GA, Bennett C, Gordon MS, Saeedi N, Newman LK. Mentalization in adolescents with borderline personality disorder: a comparison with healthy controls. J Personal Disord. 2019;33(2):145–163. doi: 10.1521/pedi_2018_32_336. [DOI] [PubMed] [Google Scholar]
- [50*].Lind M, Vanwoerden S, Penner F, Sharp C. Inpatient adolescents with borderline personality disorder features: Identity diffusion and narrative incoherence. Pers Disord : Theory Res Treat. 2019;10(4):389–393. doi: 10.1037/per0000338. [DOI] [PubMed] [Google Scholar]; Narrative coherence measured with the Child Attachment Interview and self-reported identity diffusion predicted BPD features in a sample of 70 inpatient adolescents. However, only the latter remained significant when considering covariance between them.
- [51].Lyons-Ruth K, Pechtel P, Yoon SA, Anderson CM, Teicher MH. Disorganized attachment in infancy predicts greater amygdala volume in adulthood. Behav Brain Res. 2016;308:83–93. doi: 10.1016/j.bbr.2016.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Pechtel P, Lyons-Ruth K, Anderson CM, Teicher MH. Sensitive periods of amygdala development: the role of maltreatment in preadolescence. Neuroimage. 2014;97:236–244. doi: 10.1016/j.neuroimage.2014.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53*].Porter C, Palmier-Claus J, Branitsky A, Mansell W, Warwick H, Varese F. Childhood adversity and borderline personality disorder: a meta-analysis. Acta Psychiatr Scand. 2020;141(1):6–20. doi: 10.1111/acps.13118. [DOI] [PubMed] [Google Scholar]; This metaanalysis resoundingly confirmed an association between childhood adversity and BPD, with OR’s of 13.91 compared to non-clinical controls and of 3.15 in relation to other psychiatric groups, with emotional abuse and neglect particularly relevant to BPD.


