Abstract
Introduction:
In the era of large-scale population genetic studies, there is an obvious need for maximally efficient measurement of neuropsychiatric phenomena. A proven method—computerized adaptive testing (CAT)—is not feasible for all types of tests, necessitating alternative methods of increasing test efficiency.
Methods:
We compared (and combined) two methods for abbreviating rapid test forms using two tests unamenable to CAT (a Continuous Performance Test [CPT] and an n-back test [NBACK]). N=9,498 participants (mean age 14.2 years; 52% female) were administered the tests, and abbreviation was accomplished using methods that answer two complementary questions: 1) what happens to standard error of measurement as items are removed, and 2) what happens to scores’ correlations with validity criteria as items are removed. The first question was investigated using quasi-CAT simulation, while the second was investigated using bootstrapped confidence intervals around full-form-short-form comparisons.
Results:
Results for the two methods overlapped, suggesting that the CPT could be abbreviated to 102 stimuli (57% of original) and NBACK could be abbreviated to 78 stimuli (87% of original) with the maximum acceptable loss of precision and minimum acceptable relationships with validity criteria.
Conclusions:
This combination of two test-abbreviation methods (a novel quasi-CAT simulation method and successive item removal) show promise for use in other types of tests, and the divergent results for the CPT and NBACK demonstrate the methods’ ability to detect when a test should not be shortened at all (or only minimally). We recommend the two methods be used in combination, because they emphasize complementary aspects of measurement quality: precision (reliability) and validity.
Keywords: Cognitive test, Item Response Theory, Test Abbreviation, CAT Simulation, Validity
Today, it is possible to learn someone’s entire genome from a single blood draw (or even less invasively), allowing collection of genetic data with almost no cost to the study participant. Thus, one of the biggest roadblocks to large-scale genomic research is not acquiring the genetic material as such, but rather the time it takes to measure everything else, including psychological traits (e.g., cognitive ability, psychopathology, etc.), demographic information, medical histories, general biometrics (blood pressure, height, weight, etc.), biological samples (hair, stool, blood, saliva, etc.), and perhaps even neuroimaging protocols. Taking cognition as an example, even the most well-established neurocognitive test batteries used in large-scale genomic studies (e.g., Penn Computerized Neurocognitive Battery, Cambridge Neuropsychological Test Automated Battery, etc.) (Gur, R. C. et al., 2001; Gur, Ruben C. et al., 2010; Robbins et al., 1994) take about one hour to complete. Combined with the need to collect demographics, clinical symptoms, neuroimaging, and countless other variables on a large number of participants (~10,000+), one hour is often too long. The result is usually a compromise whereby the researchers choose a more limited number of tests, sacrificing breadth of measurement to fit within the time constraints.
The pressure to minimize test/scale administration time is felt especially by research groups who administer collections of tests—test batteries—on a regular basis. If there is a good method for decreasing administration time, it could be applied to all tests in a battery, cumulatively resulting in large time savings. One method to decrease administration time is computerized adaptive testing (CAT) (Chang, 2015; Wainer, 2000), which incorporates methods from item response theory (IRT) (Embretson & Reise, 2009) to build item banks and administer only the most informative items to examinees. IRT allows characterization of individual test items (e.g. their difficulty), which enables a real-time testing algorithm to determine which item from an item bank will provide the most information about an examinee, given the examinee’s current estimated trait level. For example, if nothing is known about the examinee, his/her ability could be assumed to be average, and the algorithm would choose the best item for someone of average ability. Once that person responds to the item, his/her trait can be estimated based on that one response, and the next item administered will be the one that is optimal at the newly estimated trait level. This targeted item administration means fewer items must be administered to achieve any given level of measurement error than if the items were administered sequentially. This method has proven useful in saving administration time and maximizing precision1 (Gibbons et al., 2012; Mizumoto et al., 2019; Yudien et al., 2019), especially since building CATs has become more cost effective (e.g. Scalise & Allen, 2015).
However, computerized adaptive testing is not appropriate for all types of tests. For example, a test might require someone to freely recall words from a list of words just read aloud by a proctor. In this case, the test is just one item scored as a count (“Recall as many words as you can”), which is not appropriate for CAT. Another example would be a test that is not self-paced. For example, continuous performance tests (CPTs) (Riccio, Lowe, & Reynolds, 2004) and n-back tests (requiring participants to remember stimuli presented n spaces “back” in a display sequence; Owen, McMillan, Laird, & Bullmore, 2005) both present stimuli rapidly and continue presenting stimuli regardless of whether the participant responds. This presentation of stimuli independent of examinee behavior is obviously not amenable to CAT. Thus, research groups hoping to create an abbreviated version of an entire battery (collection of tests) can expect some of their tests to be unamenable to CAT. Although there are IRT models designed for signal-detection-like tests (Thomas et al., 2018), these models have not yet been linked to computerized adaptive testing or used for test abbreviation as such. An obvious question is, if we are dealing with a test for which “CAT is not an option”, why simulate CAT administrations of it (which we do below)? The answer is that CAT would be good for these tests except for their speed (~1 second or less per stimulus), which is an unalterable characteristic of the tests. However, simply because CAT is not feasible does not mean item parameters cannot be estimated and used in informative simulations.
The creation of short/abbreviated test forms has been a goal of psychometricians for decades, and there are several well-established methods for doing so. These include selecting items that correlate most strongly with the full scale (e.g. Francis et al., 1992; Geil, 1945; Straus & Douglas, 2004), selecting items that most improve relationships with external validity criteria (Bae & Cho, 2004), removing items that demonstrate bias (Bann et al., 2012), selecting items that have high factor loadings (Bagley & Mallick, 1978; Joseph et al., 2004), selecting items that have a desirable2 spread of difficulty parameters (Calamia et al., 2011; Cole et al., 2004), selecting items based on expert human input rather than quantitative analysis (e.g. Harris, 1975; Whitman et al., 2013), and, quite often, combinations of the above (Manos et al., 2011; Peters et al., 2012; Sturm et al., 2017). The two combined methods used in the present study (described below) most closely match the first, second, fourth, and fifth approaches mentioned above: correlation with full form, correlation with validity criteria, high factor loadings (IRT discrimination parameters), and desirable spread of difficulty parameters. This approach most closely matches those described by Reise and Henson (2000), Hol et al. (2007), and Choi et al. (2010). This combined approach is unique not in its coverage of so many criteria (a common approach), but in its combined treatment of item discrimination and difficulty (via CAT simulation; see below). Some existing methods account for item difficulty, but these tend to either ignore item discrimination (Calamia et al., 2011; Hibbard et al., 2005) or subjectively choose items that span the difficulty continuum without tying those parameters to any other criteria or approaches used (e.g. Colledani et al., 2019).
The aim of the present study was to use two methods—one based on score validity (first and second approaches in above paragraph) and the other based on standard error of measurement (fourth and fifth in above paragraph)—to create optimal short-forms for two rapid tests on the Penn Computerized Neurocognitive Battery, the Penn Continuous Performance Test (CPT) and NBACK test. We used data from a large neurodevelopmental cohort to compare these two methods and examine their utility to create more economical neurocognitive assessments when the tests are not amenable to CAT.
Methods
Participants
Participants were part of the Philadelphia Neurodevelopmental Cohort (PNC) (Calkins et al., 2014; Calkins et al., 2015; Moore, T. M. et al., 2016; Satterthwaite et al., 2014; Satterthwaite et al., 2016), which included youth (age 8–21) recruited through an NIMH-funded Grand Opportunity study characterizing clinical and neurobehavioral phenotypes in a genotyped, prospectively accrued community cohort. All study participants previously consented for genomic studies when they presented for pediatric services within the Children’s Hospital of Philadelphia (CHOP) health care network. At that time, they provided a blood sample for genetic studies, authorized access to Electronic Medical Records, and gave written informed consent/assent to be recontacted for future studies. Of the 50,540 genotyped subjects, 18,344 met criteria necessary to be included in the study (listed below) and were randomly selected, with stratification for age, sex, and ethnicity. A total of 9,498 enrolled in the study between 11/2009 –12/2011 and were included in this analysis.
The sample included children in stable health, proficient in English, and physically and cognitively capable of participating in an interview and performing the computerized neurocognitive testing. Youths with disorders that impaired motility or cognition (e.g., significant paresis or palsy, intellectual disability) were excluded. Notably, participants were not recruited from psychiatric clinics, and the sample is not enriched for individuals seeking psychiatric help. Participants provided informed consent/assent after receiving a complete description of the study and the Institutional Review Boards at Penn and CHOP approved the protocol. Table 1 shows the demographic characteristics of the sample, as well as rates of common mental disorders.
Table 1.
Sample Demographic and Basic Lifetime Clinical Information.
| Variable | Mean (SD) |
|---|---|
| Age, months (SD) | 170.3 (43.9) |
| Prop. Female | 0.52 |
| Prop. African American | 0.33 |
| Prop. Caucasian | 0.56 |
| Prop. Hispanic | 0.07 |
| Avg. Parent Edu., yrs. (SD) | 14.3 (2.3) |
| Prop. with Depression | 0.12 |
| Prop. with GAD | 0.03 |
| Prop. with OCD | 0.03 |
| Prop. with Psychosis | 0.04 |
| Prop. with ADD | 0.18 |
Note. Prop = proportion; yrs = years; SD = standard deviation; GAD = generalized anxiety disorder; OCD = obsessive-compulsive disorder; ADD = attention deficit disorder.
Measures
Continuous Performance Test.
The Penn CPT (Gur et al., 2010) measures vigilance and visual attention independent of working memory or perceptual factors. Vertical and horizontal lines in 7-segment displays appear on the screen at a rate of one second each. The participant is instructed to press the spacebar when the lines are configured as complete numbers (first half of task) or complete letters (second half of task) and to not press when the lines are not complete numbers or letters, respectively. Each half lasts 1.5 minutes, and during each one-second response window, the stimulus is presented for only 300 milliseconds (leaving 700 milliseconds of blank screen). If a stimulus is shown and the examinee behaves correctly (press in the case of targets, don’t press in the case of foils), that “item” is a correct response. For the validity-centered method (successive item removal; see below), the key outcome was d-prime, defined as the z-transform of the hit rate (proportion of targets for which the participant correctly pressed the space bar) minus the z-transform of the false alarm rate (proportion of foils for which the participant incorrectly pressed the space bar). For example, if someone correctly pressed the space bar on 99% of the targets and incorrectly pressed the space bar on 20% of the foils, his/her d-prime would be Z(0.99) – Z(0.20) = 2.33 – (−0.84) = 2.33 + 0.84 = 3.17. For the precision-centered method (CAT simulation), the key piece of information is the standard error of the score, which is obtained by traditional expectation-maximization (Bock & Aitkin, 1981) latent trait scoring.
n-Back.
The Penn Letter n-Back Test (NBACK) (Ragland et al., 2002) measures working memory, the ability to maintain and update goal-related information. Participants attend to a continual series of letters that flash on the screen (one at a time) and press the spacebar according to three different rules (0-back, 1-back, and 2-back). During the 0-back condition, the participant is instructed to simply respond to a currently present target (“X”). During the 1-back condition, the participant is instructed to press the spacebar when the letter on the screen is the same as the previous letter. During the 2-back condition, the participant is instructed to press the spacebar when the letter on the screen is the same as the letter before the previous letter (i.e., 2 letters back). In all trials, the inter-stimulus interval (ISI) is 2.5 seconds, and the stimuli (letters) are presented for 0.5 seconds each. The participant practices all three principles before testing. If a stimulus is shown and the examinee behaves correctly (press in the case of targets, don’t press in the case of foils), that “item” is a correct response. Scoring of the NBACK was the same as the scoring of the CPT, where the NBACK also has clear targets and foils.
Clinical Assessment.
An in-person interview based on the structured Schedule for Affective Disorders and Schizophrenia for School-Age Children (GOASSESS) evaluated lifetime history of clinical symptoms (Calkins et al., 2014; Calkins et al., 2015) across major psychopathology domains. Participants were assessed dimensionally and categorically and had to have significant symptoms associated with distress that affected functioning to score high on specific domains of mood/anxiety, fear, externalizing behavior, and psychosis. The procedures used for obtaining the dimensional clinical scores are described in Shanmugan et al. (2016, Supplement) and Moore et al. (2019)3. Briefly, item-factor analysis was performed on 112 clinical symptoms extracting four theoretical factors—three described by Krueger (1999), plus psychosis—where those factors were allowed to correlate. Of the four dimensional factors (Anxious-Misery, Fear, Externalizing, and Psychosis), only Psychosis was used here due to its unambiguous and well-established associations with cognition. The clinical assessment also included the Children’s Global Assessment Scale (CGAS) (Shaffer et al., 1983).
Approximation of Socioeconomic Status.
Socioeconomic status was approximated using neighborhood-level characteristics obtained by geocoding participants’ addresses to census and crime data in the Philadelphia area. Neighborhood characteristics were measured at the block-group level and included median family income, percent of residents who are married, percent of real estate that is vacant, and several others; see Moore et al. (2016) for further details.
Analysis
The first method of test abbreviation (Simulated Successive Item-Removal; SSIR) involved simulating test administrations as successive numbers of items were removed and examining the effect of item-removal on the criterion validity of total scores. The second method (CAT Simulation Method) involved calibrating items using IRT and simulating the number of stimuli needed to achieve various levels of precision (indicated by standard error of measurement).
Simulated Successive Item Removal (SSIR) Method.
The SSIR method focuses on what happens when test items/stimuli are removed. Specifically, what happens to the relationship between test scores and important criteria (e.g., ADHD severity) when successive items are removed? For example, if we find that scores on a 100-item test correlate −0.25 with ADHD severity, we want to know what happens to that −0.25 correlation when 1 item is removed (i.e., only 99 items are administered) compared to the full test version. Items are successively removed until the point (e.g., going from 82 items to 81 items) where removal of one additional item decreases the magnitude of the −0.25 correlation beyond what would be considered acceptable (see below for description of unacceptable levels). This point—where the score-criterion relationship is deflated to an unacceptable level—is the point at which the test is “too short.” Using this information, a short form can be constructed that comprises just enough items to achieve an acceptable relationship with ADHD score (indicating acceptable measurement precision).
The Simulated Successive Item Removal method for the CPT proceeded as follows:
Item order was scrambled (as in real administrations of the CPT), and d-prime was calculated for the full test plus each successive short form (e.g., d-prime after the last item is removed, d-prime after the last two items are removed, etc.), for a total of 89 short-form scores.
Bivariate relationships were calculated between the full-form d-prime and each of the short-form’s d-prime (full-short correlations).
Bivariate relationships were calculated between the full-form d-prime and the following validity criteria: age, global assessment of functioning (CGAS), socioeconomic status, psychosis (severity) score, and total score on a working memory test (NBACK).
The same bivariate relationships above were calculated for all short-form scores.
The above four steps were repeated 1,000 times to obtain a distribution of each bivariate relationship.
For each short-form (e.g., one item removed, two items removed, etc.), the relationships with validity criteria were compared to the same relationships using the full test by taking the ratio of the correlations. A ratio of 1.0 would mean the full-form and short-forms have exactly the same correlation with the validity criterion, and deviations (up or down) from 1.0 would suggest a difference between the correlations. Consistent with the common (albeit arbitrary) 0.90 cutoff (e.g. Baker et al., 2019; Dunkel et al., 2005; Jamison et al., 2007; Ward et al., 2018) for what is considered an acceptable correlation of a short-form with its corresponding original form (i.e. a 10% lower correlation), we used 10% as the maximum acceptable difference between short- and long-form criterion correlations. That is, if 0.90 or 1.10 fell within two standard deviations of the ratio of correlations between the full test and a validity criterion, that short form was considered too short. For each short form and for each validity criterion (completely crossed), we obtained a distribution of ratios of correlations, and if the ratio was not between > 0.90 and < 1.10 with 95% confidence, the short-form was considered an insufficient substitute for the full form.
For each short-form (e.g., one item removed, two items removed, etc.), the distribution of correlations with the full-form (short-full correlations) was examined. If 0.90 (the minimum acceptable) was contained within two SDs of the distribution, the short-form was considered too short.
For the NBACK, the steps described were the same, with two exceptions. Item order for a given form is important for the NBACK because the correctness of a response depends on previous stimuli. Therefore, the item order was preserved, and variation across simulations was produced by random row sampling (random sampling of exactly half of the response vectors). In addition, correlations with the CPT were used as validity criteria in bivariate relationships.
CAT Simulation Method.
Introduced4 by Moore et al. (2015) and building on the work of Reise and Henson (2000) and Choi et al (2010), the CAT-simulation method of short-form creation used here has shown promise in both cognitive (Bezdicek et al., 2018; Roalf et al., 2016) and non-cognitive (Lawson, Moore, Okamura, Becker-Haimes, & Beidas, 2020; Saine et al., 2020) assessments. This method uses IRT, which is the measurement theory underlying and facilitating CAT. Details of IRT (Embretson & Reise, 2009) and CAT (Wainer, 2000) are beyond the present scope. Principally, IRT takes the focus away from evaluating psychometric properties of the test as a whole (e.g. global reliability) and instead focuses on characterizing each individual item (e.g., difficulty of the item, how well the item can discriminate between test-takers with high versus low scores). These item characteristics, in combination, determine how much information an item provides about a person at any given trait level. Further details of IRT are provided in the Supplement, but a key point here is that IRT is the basis for Computerized Adaptive Testing (CAT). The item characteristics mentioned above can be estimated for multiple items (e.g., all items on a test), which composes an “item bank”, the group of items from which a CAT algorithm can choose if the test is administered adaptively. Establishing an item bank also allows one to simulate what would happen if a test were taken adaptively (as a CAT), and this simulation is the basis of the CAT-simulation method used here. After simulating CAT administrations, one can look post hoc at how often each item was administered; the items administered most often can be considered the “best” items and should be included on the short form. Here, we use a variation of the CAT-simulation method in which we determined the number of items necessary to achieve a predetermined precision goal (e.g., SEM< 0.30), rather than selecting the specific items providing the most information (on average). That is, whereas the CAT-simulation method of creating a short-form usually involves selecting items based on exposure (frequency of administrations), in this case that exposure is fixed (random exposure in the case of the CPT, and sequential exposure in the case of the N-BACK). Indeed, the only “CAT” characteristic of the simulated tests in this case is that they have a standard-error based termination criterion, which depends on IRT item parameter estimates.
In summary, the CAT-simulation method finds items that have an optimal5 combination of discrimination and difficulty—high discrimination, with difficulty within a reasonable range. Discrimination measures the differential capability of an item, such that a high discrimination value indicates that an item provides a high capability to differentiate subjects. High discrimination is desirable because it indicates that an item can distinguish among more fine-grained levels of the trait than if it had low discrimination. Having difficulty parameters within a reasonable range avoids items answered correctly/incorrectly by almost everyone (too easy or too difficult). Consider two hypothetical items: item #1 has a discrimination of 1.0 (normal) and difficulty of 0.0 (average); item #2 has a discrimination of 2.0 (high) and difficulty of 2.0 (high). So, item #2 has better discrimination than item #1, but item #1 has better difficulty (within typical range). So how do we determine which item should be selected for a short-form? The obvious problem is that researchers will usually not be able to “eyeball” a table of item parameter estimates and determine which combination is optimal, and thus a practical way is to simulate what would happen if a computer algorithm (CAT) were selecting these items based on information, which is inversely related to standard error of measurement. If the algorithm selects an item at any given time, it means that item was indeed the absolute best of all options in the item bank, so an item that is selected often is a good item. It is worth reiterating that, as with the use of the word “optimal” above, the assertion that “an item that is selected often is a good item” here depends on some assumptions. For example, in real-world CAT applications, it is sometimes advantageous to limit exposure of some items and promote exposure of others—i.e. to prevent item under- or overexposure (Eggen, 2001; Revuelta & Ponsoda, 1998).
The CAT-simulation method proceeded as follows:
Dimensionality of the test was assessed to determine whether a unidimensional IRT model can be used. Specifically, the ratio of first to second eigenvalues was examined to determine whether there was any possibility of unidimensionality; if so (e.g. eigenvalue ratio > 3.0), follow-up tests would have been performed (parallel analysis and fit of the unidimensional model) to confirm the unidimensionality (see Slocum-Gori & Zumbo, 2011). If multidimensionality was detected—i.e., a unidimensional IRT model was inappropriate—the optimal number of factors was determined in preparation for a multidimensional model. The planned tests for the number of factors included the minimum average partial method (Velicer, 1976), scree test (Cattell, 1966), and parallel analysis with Glorfeld correction (using 99th percentile) (Glorfeld, 1995). However, in the present case involving targets and foils, both theory (targets vs. foils) and the clean 2-factor solution (all targets on one factor and all foils on another factor) suggested 2-factors.
In the present data, multidimensionality was detected (ratios of 1st:2nd eigenvalues = 1.94, 1.17, 1.94, 2.11, and 2.51 for the CPT Numbers, CPT Letters, NBACK 0-back, NBACK 1-back, and NBACK 2-back, respectively), and item responses were therefore calibrated using a bifactor (Reise, 2012) IRT model, where each item loaded on its specific factor (targets or foils) and on a general factor comprising all items. Parameter estimates for the general factor are used here, and intercepts were transformed to conventional IRT difficulty parameters using Equation 9 in Cai (2010).
The parameter estimates for the general factor obtained from #2 above were input to Firestar (Choi, 2009), which simulates test administrations. Normally, CAT simulation follows some versions of the typical CAT procedure: select item based on maximum information at current trait estimate, re-estimate ability based on response, select best item based on new ability estimate, etc. Here, however, the simulated test administrations proceeded non-adaptively—i.e., item-selection was random for the CPT and sequential for the NBACK—and the administrations stopped after a predetermined number of items (depending on the simulation condition). Unlike in Moore et al. (2015), where the goal was to find which items were selected most often during the simulations, the goal here was to determine the standard error of measurement we could expect (on average) after administration of x items. It is all part of the same CAT-simulation procedure, and the focus on test precision here (rather than selecting specific items) is due to the fact that the stimuli are (by design) administered randomly in the final test. We are trying to minimize the number administered randomly.
Age Associations.
The sample used here had a fairly wide age range (8 – 21 years), and most importantly, this age range is one of rapid and complex neurodevelopment. Theoretically, the only effect of age is to improve or worsen performance (in this sample, improve), which would have no effect on the metrics used here (measurement precision and correlations with criteria). However, age could have other effects as well—e.g. the relationship between cognitive performance and a given criterion might be weaker/stronger in older participants than in younger participants. This age effect would affect our outcome metrics. For thoroughness, we therefore performed the SSIR method described above after splitting the sample into younger (8 – 14 years) and older (15 – 21 years) groups.
Results
SSIR Method
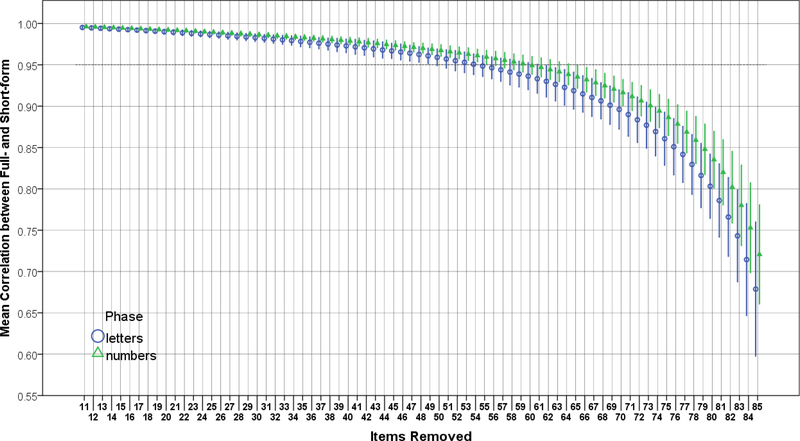
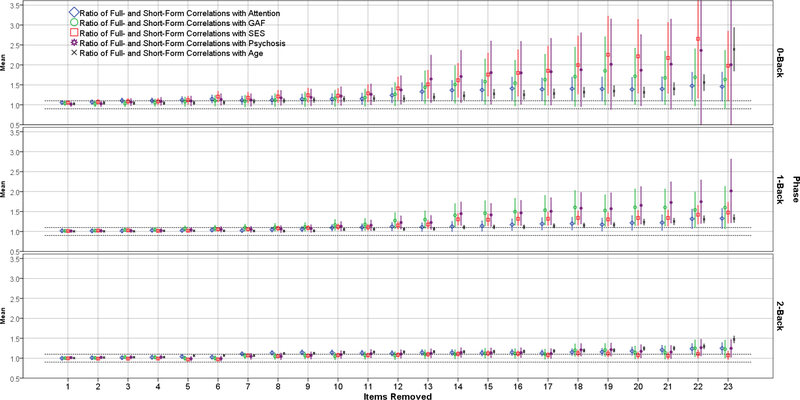
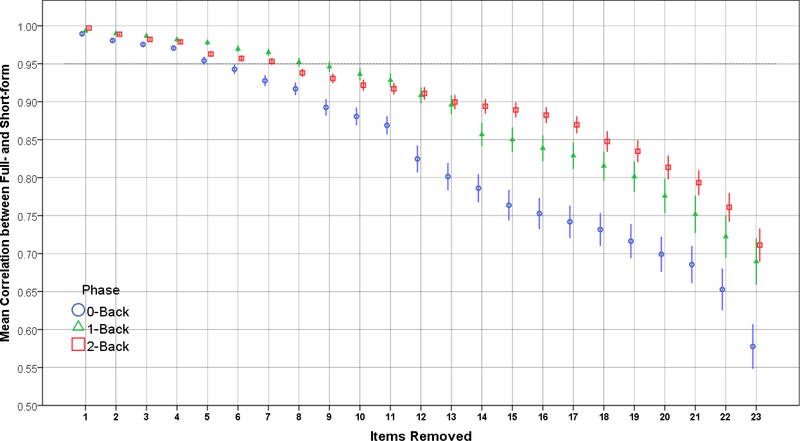
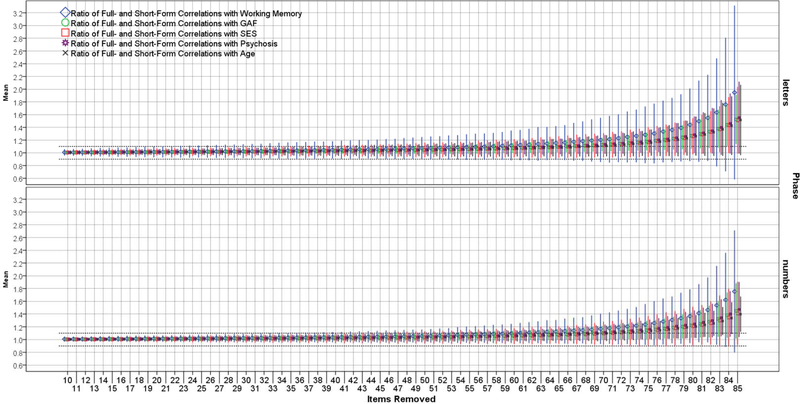
Figures 1–4 show the results of the SSIR method for the CPT and NBACK. Figures 1 and 2 show changes to correlations between full- and short-forms as items are removed. For the CPT (Figure 1), the correlation stays fairly steady until >55 items are removed, at which point the correlation plummets. Thus, the optimal number of items (point where the correlation 95% CI first includes 0.95) for the CPT letters and numbers, respectively, were 41 (46% of original) and 35 (39%). For the NBACK (Figure 2), there is a more uniform decline in full-short correlations as items are removed, such that the short forms quickly become too short as items are removed. The optimal number of items for the NBACK 0-back, 1-back, and 2-back, respectively, were 26 (87% of original), 23 (77%), and 24 (80%). Figures 3 and 4 show what happens to short-form correlations with validity criteria (compared to full-form) as items are removed. For both tests, the ratio of full-form to short-form correlations increases as items are removed. That is, the full form shows stronger correlations with validity criteria, and this difference (reflected in a ratio) increases as items are removed. The focal points on Figures 3 and 4 are the places where the 2SD error bars touch the dotted lines at 1.10 and 0.90, because these points indicate the limit of shortening for the test.
Figure 1.
Mean Correlation between Short-Form and Full-Form Versions of the CPT, by Phase.
Figure 4.
Ratios of Criterion Validity Correlations Using the Full-Form and Short-Forms of the NBACK, by Phase.
Figure 2.
Mean Correlation between Short-Form and Full-Form Versions of the NBACK, by Phase.
Figure 3.
Ratios of Criterion Validity Correlations Using the Full-Form and Short-Forms of the CPT, by Phase.
Table 2 shows the results of these analyses—i.e., the recommended number of items for a short-form—corresponding to Figures 1–4. Two overall patterns are apparent. First, the suggested CPT length (mean across phases = 53% of original) is much shorter than the suggested NBACK length (mean 83% of original). Second, the suggested test length does not differ substantially across validity criteria. The lowest average suggested length (64.4%) comes from analyses using Age, while the highest average suggested length (78.2%) comes from analyses using the convergent validity criterion (working memory predicting attention, and vice versa). Based on the results in Table 2 and using the 10% rule described in Methods (point where CI of correlation ratio includes 0.90 or 1.10), we suggest that the minimum acceptable lengths of CPT letters phase, CPT numbers phase, NBACK 0-back, NBACK 1-back, and NBACK 2-back, are 51 (57%), 43 (48%), 28 (93%), 23 (77%), and 24 (80%) items, respectively.
Table 2.
Number of Items Necessary to Achieve Satisfactory Levels of Criterion Validity (Relative to Full-Form) and Short-Full Correlation.
| Criterion Validity | ||||||
|---|---|---|---|---|---|---|
| Test & Phase | Convergent | CGAS | SES | Psychosis | Age | Full-Short Correlation |
| CPT letters | 69 (77%) | 42 (47%) | 55 (61%) | 48 (53%) | 53 (59%) | 41 (46%) |
| CPT numbers | 55 (61%) | 40 (44%) | 48 (53%) | 43 (48%) | 39 (43%) | 35 (39%) |
| NBACK 0-back | 29 (97%) | 28 (93%) | 29 (97%) | 28 (93%) | 25 (83%) | 26 (87%) |
| NBACK 1-back | 23 (77%) | 27 (90%) | 24 (80%) | 25 (83%) | 18 (60%) | 23 (77%) |
| NBACK 2-back | 24 (80%) | 24 (80%) | 24 (80%) | 24 (80%) | 23 (77%) | 24 (80%) |
Note. CGAS = Children’s Global Assessment Scale; SES = socio-economic status; CPT = Continuous Performance Task.
Age Associations.
Supplementary Figure S2 shows the same analyses as presented in Figure 3 but split by age. Two points are worth noting. First, the functions for older and younger participants are mostly overlapping until the midpoint (~40 items removed). However—and this is the second point—there does appear to be some consistent separation between the older and younger participants in the Letters portion (blue curve slightly above red curve). Supplementary Figure S3 shows the same analyses as above, but for the NBACK. As for the CPT, there is very little separation between the older and younger groups (red and blue curves) until the midpoint (~11 items removed). Notably, some of the differences become quite large after this midpoint. However, unlike for the CPT, there is no consistent difference between the curves—i.e. red appears above blue about as often as the opposite.
CAT Simulation Method
Supplementary Tables S1 and S2 show the item parameter estimates (normal metric; D = 1.702) for the NBACK (mean discrimination = 0.80; mean difficulty = −1.96) and CPT (mean discrimination = 0.48; mean difficulty = −1.22). Of note for the NBACK, discrimination parameters were substantially higher for the targets (mean = 1.35) than for the foils (mean = 0.53), which was also true for the difficulty parameters (mean for targets = −1.52; mean for foils = −2.18). Differences for the CPT were similar but subtler (mean target & foil discrimination = 0.55 & 0.44; mean target & foil difficulty = −1.07 & −1.29). One noticeable difference between the parameter estimates of the NBACK and CPT is that the former appear to depend on a stimulus’ position in the sequence (i.e. which stimulus was displayed immediately before) while the latter appear to depend more on characteristics of the stimulus itself. The stimuli in Table S2 are “blocked” into sets of 5, such that the first five rows are the same stimulus presented at successively later (though random) times; for example, items 1, 2, 3, 4, and 5 are the same stimulus and could be administered, for example, in random positions 3, 10, 55, 56, 81, and 90, respectively. To take an extreme example, items 121 through 125 all have near-zero discrimination parameters, indicating that this specific stimulus is a poor indicator of the ability to correctly reject the non-target. (Indeed, the stimulus is a non-letter that looks very much like a letter.) When this stimulus was administered during the simulations, it left the standard error of measurement essentially unchanged, meaning it is a “dead weight” item that takes up time but adds nothing6.
Table 3 shows the item exposure results using the CAT-simulation method of test abbreviation. The numbers of items necessary to achieve six levels of precision (from very high precision to minimum acceptable) are shown for each test and phase. Taking the fourth row (Max. SEM = 0.45) as an example, the second column gives the equivalent test-level reliability7 (0.80) followed by (going from left to right) the recommended lengths of the CPT Numbers phase (can be shortened to 69% of original), CPT letters phase (76% of original), NBACK 0-back (97%), NBACK 1-back (92%), and NBACK 2-back (92%). Across the six levels of precision, going from extreme to minimum acceptable (top to bottom of Table 3), the mean recommended short-form lengths were 98%, 95%, 90%, 85%, 80%, and 73% of the original test, a relatively linear decrease. Consistent with the results from the SSIR method reported above, the results in Table 3 suggest that the CPT can be shortened substantially, whereas the NBACK cannot. Using “moderate” precision as the cutoff for an acceptable short form, the suggested test lengths of CPT letters phase, CPT numbers phase, NBACK 0-back, NBACK 1-back, and NBACK 2-back are 62, 69, 29, 28, and 28, respectively. Taken together, these results, combined with the SSIR method, suggest that we can create a CPT that is 57% of its original length and an NBACK that is 87% of its original length.
Table 3.
Number of Stimuli Necessary to Reach Six Levels of Measurement Precision for the CPT and NBACK.
| Items Needed | ||||||
|---|---|---|---|---|---|---|
| Precision | CPT | NBACK | ||||
| Max. SEM | α Equivalent† | Numbers | Letters | 0-back | 1-back | 2-back |
| 0.30 | 0.91 (extreme) | 84.4 (94%) | 88.8 (99%) | 29.6 (99%) | 29.6 (99%) | 30.0 (100%) |
| 0.35 | 0.88 (high) | 78.4 (87%) | 83.7 (93%) | 29.4 (98%) | 29.0 (97%) | 29.6 (99%) |
| 0.40 | 0.84 | 71.0 (79%) | 76.9 (85%) | 29.1 (97%) | 28.4 (95%) | 28.8 (96%) |
| 0.45 | 0.80 (moderate) | 62.0 (69%) | 68.6 (76%) | 29.0 (97%) | 27.7 (92%) | 27.7 (92%) |
| 0.50 | 0.75 | 52.1 (58%) | 59.4 (66%) | 28.9 (96%) | 27.1 (90%) | 26.5 (88%) |
| 0.55 | 0.70 (min. acceptable) | 41.1 (46%) | 49.4 (55%) | 28.9 (96%) | 25.9 (86%) | 24.9 (83%) |
Note. CPT = Continuous Performance Task; SEM = standard error of measurement; max = maximum;
standard error of measurement and internal consistency reliability (here, Cronbach’s α) are related by the equation SEM = SDscores × sqrt(1 − α), which can be reduced to SEM = sqrt(1 − α) in the normal IRT metric in which SDscores is assumed to be 1.0 without further information (SD = standard deviation).
Discussion
In this study, we compared a method of test abbreviation using correlations with full forms and validity criteria to a precision-based method using CAT simulation. Results from the validity-based method were largely consistent with those from the CAT-simulation method using the lowest reliability cutoff (SEM < 0.55). For the CPT, the validity-based method suggested that the test could be shortened by about half of its original length for letters and numbers, respectively, while the CAT-simulation method suggested almost identical percentages. Both offer substantial savings in administration time. For the NBACK, results were not as consistent, with the CAT-simulation results being more conservative. For the 0-, 1-, and 2-back, the validity-based method suggested almost no abbreviation; the CAT-simulation method suggested the same. Both methods indicate that the time savings are negligible, and if this test is used, it should be administered in its entirety. Further research is needed to determine the cause of the discrepancy for the NBACK, as it could be related to the fixed order of the task, difficulty of the task, or other factors.
This study had some notable limitations. First, there are many test types not amenable to CAT, and we only examined two relatively similar, rapid, signal-detection-like tests. It is unknown whether applying these methods will be as effective or feasible for other types of tests not amenable to CAT, such as the trail-making tests (Reitan, 1955), tests that change answer key logic mid-test (e.g., Penn Conditional Exclusion Test; Kurtz, Ragland, Moberg, & Gur, 2004), or list-learning tests involving free recall (Claparède, 1918). A second limitation is that the methods presented here do not obviate the need to make subjective decisions when building a short-form. Any decision to use a specific precision level cutoff (e.g., SEM < 0.40) or validity criterion cutoff will be at least partly subjective and based on the specific needs of the study. A third limitation is that the age range used here (8 – 21) is a unique period of human development (including puberty). It is possible that some of the effects, especially the relationships among scores and validity criteria, tend to be higher or lower for this age group (or a sub-group within this one) compared to the general population. Indeed, our analyses separating the age groups (Supplementary Figures S2 and S3) confirmed some of the above. Specifically, for the CPT Letters portion, the test forms (full versus long) tend to diverge more quickly in the older than in the younger group, such that application of the present method in a younger group would suggest the test can be shortened more than if it were done in an older group. For the NBACK, while there was no systematic difference between the older and younger groups, the differences became large and unpredictable after ~10 items were removed (right sides of panels in Figure S2). We therefore urge researchers to apply this method in the full age range for which the short-form is intended. Otherwise, the inevitable (and unmodeled) effects of age could have unintended consequences. A fourth limitation is that, while the abbreviated test forms used here save considerable time in aggregate, the time savings on an individual level is negligible (1–2 minutes). A fifth limitation is that the assumptions are made throughout that: 1) higher discrimination is always better, and 2) the trait will always be normally distributed with mean=0 and standard deviation=1. However, violations of #2 are so common in nature as to need no further explanation, and counterexamples of #1 were suggested and demonstrated by Chang & Ying (1999) and Hua & Chang (2001). Finally, it is both a potential limitation and a cautionary note that some tests (especially neurocognitive) are designed with examinee fatigue in mind; abbreviating the test might change the nature of what is being measured. For example, one aspect of the original version of the Continuous Performance Test used here is that it was quite long and therefore measured some aspect of examinee stamina for sustained attention. If the test was intentionally designed that way (to measure stamina as well as attention), careful thought needs to be given to whether it is necessary to maintain the same measurement properties as the original. If so, abbreviation might not be an option.
In sum, overall results provide some evidence in favor of using dual test-abbreviation methods for certain tests that are not amenable to traditional CAT, especially if those tests are rapid and include signal-detection-like properties (i.e., detecting and reacting to targets versus foils). Here, these novel methods were able to shorten the length of a continuous performance test by approximately half, while the time savings on an n-back measure were minimal. Future studies should examine the utility of these methods in additional computerized neurocognitive measures given in large studies. Given the scale of many current genomic and international studies, the total time savings from creation of short-forms is potentially vast. For example, the Penn Continuous Performance Test used here takes 5.3 minutes to administer. If we abbreviate it to 3.3 minutes (2 minutes saved, a conservative estimate by the present results), administration to ~500,000 people (e.g., in the UK Biobank) (Sudlow et al., 2015) would mean ~16,667 hours (1.9 years) of examinee time saved from abbreviating just one test. This consideration highlights the tremendous potential for increasing assessment efficiency, which could free up time and resources for more impactful uses or for gathering data on a broader range of behavioral domains.
Supplementary Material
Acknowledgments
This work was supported by the Lifespan Brain Institute (LiBI); NIMH grants MH089983, MH117014, and MH096891; and the Dowshen Program for Neuroscience.
Footnotes
Disclosure of Interest
The authors report no conflict of interest.
Note that the benefits of CAT depend on how it is applied. One way (variable-length) is to allow tests to proceed until some precision criterion is satisfied. This ensures that each examinee has a comparable (and acceptable) level of precision (see Babcock & Weiss, 2009; Paap et al., 2019). An alternative (fixed-length) is to administer a specific number of items to all examinees, where examinees can finish the test with varying levels of precision, yet the length of the test is predictable. Importantly, a fixed-length adaptive form will still usually produce results superior to a fixed-length short-form because the items administered in the fixed-length CAT will be selected to maximize information. An obvious problem with variable-length CATs for large-scale studies is that the varying length makes them difficult to fit in the tight participant schedules (measure after measure after measure) common in large scale studies.
“Desirable” in this case depends on the goals of the test. For example, if the test were designed to detect cognitive impairment in an elderly population, the desirable range of difficulty parameters would be toward the low end of the continuum, because the goal is to distinguish those with versus without impairment (implying low), not with versus without high-level abilities. Likewise, if there is no specific target population, then the desirable range of difficulties would roughly match what one expects in the general population: a normal curve (most difficulty parameters near the mean, with fewer and fewer as one moves away from the mean).
In both Shanmugan et al. (2016) and Moore et al. (2019), the model described here was used as an intermediate step in the process of obtaining orthogonal bifactor (Reise, Moore, & Haviland, 2010) scores. While the goal in those earlier studies was to obtain orthogonal scores (or a “p” factor in the case of Moore et al.), the present study does not need orthogonal scores, and therefore the correlated scores from the “middle step” correlated-traits model were used here.
Note that the idea of judging the “quality” of items based on exposure (frequency of administration) in CAT simulation is not new, and it is certainly possible that the methods demonstrated in Reise and Henson (2000) and Choi et al. (2010) would produce results identical to those seen here. However, Moore et al. (2015) differs from the above approaches in that the above emphasize administration rank (an item is good if it is administered early), whereas Moore et al. (2015) emphasize total item administrations. The two approaches can produce different results if, for example, there is an item with very high administration frequency that tends to be administered late. This can happen if several CAT item-administration “chains” converge on the item later in the administration sequence.
Two assumptions here are that, 1) the distribution of the trait is normal (Gaussian), such that an optimal distribution of difficulties would reflect the high proportion of examinees around the mean, and 2) each item’s characteristics can be assessed “in a vacuum”, independent of administration order or which items it ends up combining with. Accordingly, an “optimal” difficulty is one close to the mean, and higher discrimination is always better. In reality, the “optimal” workings of CAT are more complex, such that this phrase “optimal combination of discrimination and difficulty” could not be asserted without more qualifications. For example, it is not necessarily true that higher discrimination parameters are always better, as this will depend on when the items are administered during the test (Chang & Ying, 1999). See Chang (2015) for summary.
In a typical test/scale revision pipeline (see, e.g., Reise et al., 2000), an item/stimulus with such poor item qualities would be removed from future versions. For this specific application, however, we are treating the test as a fixed program that can be only shortened, not altered at the source code (stimulus presentation) level. If the task were reprogrammed from the beginning, it might be advisable to remove the problematic stimuli.
Note that Cronbach’s alpha is given here only as additional information. It is not used in the simulations.
References
- Babcock B & Weiss DJ (2009). Termination criteria in computerized adaptive tests: Variable length CATs are not biased. In Weiss DJ (Ed.), Proceedings of the 2009 GMAC Conference on Computerized Adaptive Testing Retrieved 25 September 2020 from www.psych.umn.edu/psylabs/CATCentral/ [Google Scholar]
- Bae JN, & Cho MJ (2004). Development of the Korean version of the Geriatric Depression Scale and its short form among elderly psychiatric patients. Journal of psychosomatic research, 57(3), 297–305. [DOI] [PubMed] [Google Scholar]
- Bagley C, & Mallick K (1978). Development of a Short Form of the Piers‐‐Harris Self‐Concept Scale. Educational Review, 30(3), 265–268. [Google Scholar]
- Baker RT, Burton D, Pickering MA, & Start A (2019). Confirmatory Factor Analysis of the Disablement in the Physically Active Scale and Preliminary Testing of Short-Form Versions: A Calibration and Validation Study. Journal of athletic training, 54(3), 302–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bann CM, McCormack LA, Berkman ND, & Squiers LB (2012). The health literacy skills instrument: a 10-item short form. Journal of health communication, 17(sup3), 191–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezdicek O, Červenková M, Moore TM, Stepankova Georgi H, Sulc Z, Wolk DA, … Roalf DR (2018). Determining a short form montreal cognitive assessment (s-MoCA) czech version: Validity in mild cognitive impairment parkinson’s disease and cross-cultural comparison. Assessment,, doi: 10.1177/1073191118778896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bock RD, & Aitkin M (1981). Marginal maximum likelihood estimation of item parameters: Application of an EM algorithm. Psychometrika, 46(4), 443–459. [Google Scholar]
- Cai L (2010). High-dimensional exploratory item factor analysis by A Metropolis–Hastings Robbins–Monro algorithm. Psychometrika, 75(1), 33–57. doi: 10.1007/s11336-009-9136-x [DOI] [Google Scholar]
- Calamia M, Markon K, Denburg NL, & Tranel D (2011). Developing a short form of Benton’s Judgment of Line Orientation Test: An item response theory approach. The Clinical Neuropsychologist, 25(4), 670–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkins ME, Merikangas KR, Moore TM, Burstein M, Behr MA, Satterthwaite TD, … Gur RE (2015). The philadelphia neurodevelopmental cohort: Constructing a deep phenotyping collaborative. Journal of Child Psychology and Psychiatry, 56(12), 1356–1369. doi: 10.1111/jcpp.12416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkins ME, Moore TM, Merikangas KR, Burstein M, Satterthwaite TD, Bilker WB, … Gur RE (2014). The psychosis spectrum in a young U.S. community sample: Findings from the philadelphia neurodevelopmental cohort. World Psychiatry, 13(3), 296–305. doi: 10.1002/wps.20152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattell RB (1966). The scree test for the number of factors. Multivariate behavioral research, 1(2), 245–276. [DOI] [PubMed] [Google Scholar]
- Chang H-H (2015). Psychometrics behind computerized adaptive testing. Psychometrika, 80(1), 1–20. [DOI] [PubMed] [Google Scholar]
- Chang H-H, & Ying Z (1999). a-stratified multistage computerized adaptive testing. Applied Psychological Measurement, 23(3), 211–222. [Google Scholar]
- Choi SW (2009). Firestar: Computerized adaptive testing simulation program for polytomous item response theory models. Applied Psychological Measurement, 33(8), 644–645. doi: 10.1177/0146621608329892. [DOI] [Google Scholar]
- Choi SW, Reise SP, Pilkonis PA, Hays RD, & Cella D (2010). Efficiency of static and computer adaptive short forms compared to full-length measures of depressive symptoms. Quality of Life Research, 19(1), 125–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claparède E (1918). Percentilage de quelques tests d’aptitude. Archives de Psychologie, 17, 313 Retrieved from https://search.proquest.com/docview/1305203685 [Google Scholar]
- Cole JC, Rabin AS, Smith TL, & Kaufman AS (2004). Development and validation of a Rasch-derived CES-D short form. Psychological assessment, 16(4), 360. [DOI] [PubMed] [Google Scholar]
- Colledani D, Anselmi P, & Robusto E (2019). Development of a new abbreviated form of the Eysenck personality questionnaire-revised with multidimensional item response theory. Personality and Individual Differences, 149, 108–117. [Google Scholar]
- Dunkel D, Antretter E, Fröhlich-Walser S, & Haring C (2005). Evaluation of the short-form social support questionnaire (SOZU-K-22) in clinical and non-clinical samples. Psychotherapie, Psychosomatik, Medizinische Psychologie, 55(5), 266–277. [DOI] [PubMed] [Google Scholar]
- Eggen TJHM (2001). Overexposure and underexposure of items in computerized adaptive testing. Measurement and Research Department Reports, 1. [Google Scholar]
- Embretson SE, & Reise SP (2009). Item response theory for psychologists (Repr. ed.). Mahwah, NJ: [u.a.]: Erlbaum. [Google Scholar]
- Francis LJ, Brown LB, & Philipchalk R (1992). The development of an abbreviated form of the Revised Eysenck Personality Questionnaire (EPQR-A): Its use among students in England, Canada, the USA and Australia. Personality and individual differences, 13(4), 443–449. [Google Scholar]
- Geil GA (1945). A clinically useful abbreviated Wechsler-Bellevue Scale. The Journal of Psychology, 20(1), 101–108. [Google Scholar]
- Glorfeld LW (1995). An improvement on Horn’s parallel analysis methodology for selecting the correct number of factors to retain. Educational and psychological measurement, 55(3), 377–393. [Google Scholar]
- Gur RC, Ragland JD, Moberg PJ, Turner TH, Bilker WB, Kohler C, … Gur RE (2001). Computerized neurocognitive scanning: I. methodology and validation in healthy people. Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology, 25(5), 766–776. doi: 10.1016/S0893-133X(01)00278-0 [DOI] [PubMed] [Google Scholar]
- Gur RC, Richard J, Hughett P, Calkins ME, Macy L, Bilker WB, … Gur RE (2010). A cognitive neuroscience-based computerized battery for efficient measurement of individual differences: Standardization and initial construct validation. Journal of Neuroscience Methods, 187(2), 254–262. doi: 10.1016/j.jneumeth.2009.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hau K, & Chang H-H (2001). Item selection in computerized adaptive testing: should more discriminating items be used first? Journal of Educational Measurement, 38(3), 249–266. [Google Scholar]
- Hibbard JH, Mahoney ER, Stockard J, & Tusler M (2005). Development and testing of a short form of the patient activation measure. Health services research, 40(6p1), 1918–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hol AM, Vorst HCM, & Mellenbergh GJ (2007). Computerized adaptive testing for polytomous motivation items: administration mode effects and a comparison with short forms. Applied Psychological Measurement, 31(5), 412–429. [Google Scholar]
- Jamison RN, Fanciullo GJ, McHugo GJ, & Baird JC (2007). Validation of the short-form interactive computerized quality of life scale (ICQOL-SF). Pain Medicine, 8(3), 243–250. [DOI] [PubMed] [Google Scholar]
- Joseph S, Linley PA, Harwood J, Lewis CA, & McCollam P (2004). Rapid assessment of well‐being: The short depression‐happiness scale (SDHS). Psychology and psychotherapy: Theory, research and practice, 77(4), 463–478. [DOI] [PubMed] [Google Scholar]
- Krueger RF (1999). The structure of common mental disorders. Archives of general psychiatry, 56(10), 921–926. [DOI] [PubMed] [Google Scholar]
- Kurtz MM, Ragland JD, Moberg PJ, & Gur RC (2004). The penn conditional exclusion test: A new measure of executive-function with alternate forms for repeat administration. Archives of Clinical Neuropsychology, 19(2), 191–201. doi: 10.1016/S0887-6177(03)00003-9 [DOI] [PubMed] [Google Scholar]
- Lawson GM, Moore TM, Okamura KH, Becker-Haimes EM, & Beidas RS (2020). Knowledge of Evidence-Based Services Questionnaire: Development and Validation of a Short Form. Administration and Policy in Mental Health and Mental Health Services Research, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manos RC, Kanter JW, & Luo W (2011). The behavioral activation for depression scale–short form: development and validation. Behavior therapy, 42(4), 726–739. [DOI] [PubMed] [Google Scholar]
- Mizumoto A, Sasao Y, & Webb SA (2019). Developing and evaluating a computerized adaptive testing version of the Word Part Levels Test. Language Testing, 36(1), 101–123. [Google Scholar]
- Moore TM, Martin IK, Gur OM, Jackson CT, Scott JC, Calkins ME, … Gur RC (2016). Characterizing social environment’s association with neurocognition using census and crime data linked to the Philadelphia neurodevelopmental cohort. Psychological Medicine, 46(3), 599–610. doi: 10.1017/S0033291715002111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore TM, Calkins ME, Satterthwaite TD, Roalf DR, Rosen AFG, Gur RC, & Gur RE (2019). Development of a computerized adaptive screening tool for overall psychopathology (“p”). Journal of Psychiatric Research, 116, 26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore TM, Scott JC, Reise SP, Port AM, Jackson CT, Ruparel K, … Gur RC (2015). Development of an abbreviated form of the Penn Line Orientation Test using large samples and computerized adaptive test simulation. Psychological Assessment, 27(3), 955–964. doi: 10.1037/pas0000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen AM, McMillan KM, Laird AR, & Bullmore E (2005). N-back working memory paradigm: A meta-analysis of normative functional neuroimaging studies. Human Brain Mapping, 25(1), 46–59. doi: 10.1002/hbm.20131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paap MC, Born S, & Braeken J (2019). Measurement efficiency for fixed-precision multidimensional computerized adaptive tests: Comparing health measurement and educational testing using example banks. Applied Psychological Measurement, 43(1), 68–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters L, Sunderland M, Andrews G, Rapee RM, & Mattick RP (2012). Development of a short form Social Interaction Anxiety (SIAS) and Social Phobia Scale (SPS) using nonparametric item response theory: The SIAS-6 and the SPS-6. Psychological assessment, 24(1), 66. [DOI] [PubMed] [Google Scholar]
- Ragland JD, Turetsky BI, Gur RC, Gunning-Dixon F, Turner T, Schroeder L, … Gur RE (2002). Working memory for complex figures: An fMRI comparison of letter and fractal n-back tasks. Neuropsychology, 16(3), 370–379. doi: 10.1037//0894-4105.16.3.370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reise SP (2012). The rediscovery of bifactor measurement models. Multivariate behavioral research, 47(5), 667–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reise SP, & Henson JM (2000). Computerization and adaptive administration of the NEO PIR. Assessment, 7, 347–364. [DOI] [PubMed] [Google Scholar]
- Reise SP, Moore TM, & Haviland MG (2010). Bifactor models and rotations: Exploring the extent to which multidimensional data yield univocal scale scores. Journal of personality assessment, 92(6), 544–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reise SP, Waller NG, & Comrey AL (2000). Factor analysis and scale revision. Psychological assessment, 12(3), 287. [DOI] [PubMed] [Google Scholar]
- Reitan RM (1955). The relation of the trail making test to organic brain damage. Journal of Consulting Psychology, 19(5), 393. [DOI] [PubMed] [Google Scholar]
- Revuelta J & Ponsoda V (1998). A comparison of item exposure control methods in computerized adaptive testing. Journal of Educational Measurement, 35(4), 311–327. [Google Scholar]
- Riccio CA, Lowe PA, & Reynolds CR (2004). Clinical applications of continuous performance tests (1 Aufl. ed.). Hoboken: Wiley; Retrieved from http://ebooks.ciando.com/book/index.cfm/bok_id/493195 [Google Scholar]
- Roalf DR, Moore TM, Wolk DA, Arnold SE, Mechanic-Hamilton D, Rick J, … Moberg PJ (2016). Defining and validating a short form montreal cognitive assessment (s-MoCA) for use in neurodegenerative disease. Journal of Neurology, Neurosurgery & Psychiatry, 87(12), 1303–1310. doi: 10.1136/jnnp-2015-312723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robbins TW, James M, Owen AM, Sahakian BJ, McInnes L, & Rabbitt P (1994). Cambridge neuropsychological test automated battery (CANTAB): A factor analytic study of a large sample of normal elderly volunteers. Dementia (Basel, Switzerland), 5(5), 266 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/7951684 [DOI] [PubMed] [Google Scholar]
- Saine ME, Moore TM, Szymczak JE, Bamford LP, Barg FK, Mitra N, … & Lo Re V III. (2020). Validation of a modified Berger HIV stigma scale for use among patients with hepatitis C virus (HCV) infection. Plos one, 15(2), e0228471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satterthwaite TD, Connolly JJ, Ruparel K, Calkins ME, Jackson C, Elliott MA, … Hakonarson H (2016). The philadelphia neurodevelopmental cohort: A publicly available resource for the study of normal and abnormal brain development in youth. NeuroImage, 124(Pt B), 1115–1119. doi: 10.1016/j.neuroimage.2015.03.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satterthwaite TD, Elliott MA, Ruparel K, Loughead J, Prabhakaran K, Calkins ME, … Gur RC (2014). Neuroimaging of the philadelphia neurodevelopmental cohort. NeuroImage, 86, 544–553. doi: 10.1016/j.neuroimage.2013.07.064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scalise K, & Allen DD (2015). Use of open-source software for adaptive measurement: Concerto as an R-based computer adaptive development and delivery platform. British Journal of Mathematical and Statistical Psychology, 68(3), 478–496. doi: 10.1111/bmsp.12057 [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, & Aluwahlia S (1983). A children’s global assessment scale (CGAS). Archives of General Psychiatry, 40(11), 1228–1231. Retrieved from 10.1001/archpsyc.1983.01790100074010 [DOI] [PubMed] [Google Scholar]
- Shanmugan S, Wolf DH, Calkins ME, Moore TM, Ruparel K, Hopson RD, … & Satterthwaite TD (2016). Common and dissociable mechanisms of executive system dysfunction across psychiatric disorders in youth. American journal of psychiatry, 173(5), 517–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slocum-Gori SL, & Zumbo BD (2011). Assessing the unidimensionality of psychological scales: Using multiple criteria from factor analysis. Social Indicators Research, 102(3), 443–461. [Google Scholar]
- Straus MA, & Douglas EM (2004). A short form of the Revised Conflict Tactics Scales, and typologies for severity and mutuality. Violence and victims, 19(5), 507–520. [DOI] [PubMed] [Google Scholar]
- Sturm A, Kuhfeld M, Kasari C, & McCracken JT (2017). Development and validation of an item response theory‐based Social Responsiveness Scale short form. Journal of Child Psychology and Psychiatry, 58(9), 1053–1061. [DOI] [PubMed] [Google Scholar]
- Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, … Landray M (2015). UK biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Medicine, 12(3), e1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas ML, Brown GG, Gur RC, Moore TM, Patt VM, Risbrough VB, & Baker DG (2018). A signal detection–item response theory model for evaluating neuropsychological measures. Journal of Clinical and Experimental Neuropsychology, 40(8), 745–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velicer WF (1976). Determining the number of components from the matrix of partial correlations. Psychometrika, 41(3), 321–327. [Google Scholar]
- Wainer H (2000). Computerized adaptive testing (2 ed. ed.). Mahwah, NJ: Erlbaum. [Google Scholar]
- Ward T, Arnold K, Cunningham MC, & Liljequist L (2018). Three validation studies of the personality assessment inventory short form. Journal of Clinical Psychology, 74(12), 2264–2275. [DOI] [PubMed] [Google Scholar]
- Whitman ZR, Kachali H, Roger D, Vargo J, & Seville E (2013). Short-form version of the Benchmark Resilience Tool (BRT-53). Measuring Business Excellence. [Google Scholar]
- Yudien MA, Moore TM, Port AM, Ruparel K, Gur RE, & Gur RC (2019). Development and public release of the Penn reading assessment computerized adaptive test (PRA-CAT) for premorbid IQ. Psychological Assessment, 31(9), 1168–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.