Abstract
Introduction:
Functional models of posttraumatic stress disorder (PTSD) and alcohol use disorder (AUD) underscore the role of internally-driven negative reinforcement. However, with the focus of these models being on negative emotions broadly, there is limited understanding of the effect of alcohol use to down-regulate specific forms of negative emotions or positive emotions generally. Among populations characterized by PTSD, there is growing evidence that positive emotions may elicit aversive reactions and thus be intentionally reduced, including via alcohol use.
Objective:
The current study examined the associations among PTSD symptom severity, alcohol use to down-regulate both negative (i.e., despondency and anger) and positive emotions, and alcohol misuse.
Method:
Data were collected from 320 trauma-exposed, substance-using individuals in the community (M age = 35.78, 46.9% women).
Results:
Individuals with greater PTSD symptom severity reported significantly higher alcohol use to down-regulate despondency, anger, and positive emotions, which, in turn, were linked to greater alcohol misuse.
Conclusions:
Alcohol use may serve to down-regulate both negative (i.e., despondency and anger) and positive emotions, and these functions may help to explain the association of PTSD symptom severity to alcohol misuse. PTSD-AUD models may benefit from specifying a negatively reinforcing function of alcohol use in the context of positive emotions.
Keywords: Posttraumatic stress disorder, down-regulation, self-medication, negative reinforcement, positive emotions, despondency, anger
The co-occurrence of posttraumatic stress disorder (PTSD) and alcohol use disorder (AUD) is a public health priority. Epidemiological studies indicate that the odds of developing AUD are significantly elevated among individuals with PTSD; upwards of half of individuals with PTSD have a co-occurring AUD (Seal et al., 2011; Smith, Goldstein, & Grant, 2016; Wisco et al., 2014). Individuals with co-occurring PTSD-AUD have severe PTSD and AUD symptom profiles (Driessen et al., 2008; Saladin, Brady, Dansky, & Kilpatrick, 1995), including more hospitalizations for alcohol (Driessen et al., 2008), poorer alcohol treatment outcomes, and higher alcohol relapse rates (Mills, Lynskey, Teesson, Ross, & Darke, 2005). Moreover, individuals with PTSD-AUD report greater functional impairment (Driessen et al., 2008; Riggs, Rukstalis, Volpicelli, Kalmanson, & Foa, 2003) and more comorbidity (Driessen et al., 2008; Mills, Teesson, Ross, & Peters, 2006; Ouimette, Wolfe, & Chrestman, 1996; Saladin et al., 1995) compared to individuals with either PTSD or AUD alone. Given strong evidence for the clinical relevance of PTSD-AUD, further research is needed to clarify factors to be targeted in preventative interventions to reduce the co-occurrence of PTSD-AUD.
Theoretical models have been proposed to explain the high co-occurrence of PTSD-AUD. Negative reinforcement models (Baker et al., 2004) suggest that AUD emerges following the development of PTSD and functions to “self-medicate” (i.e., escape or avoid; Khantzian, 1997) trauma-related emotional distress. Conversely, the high-risk hypothesis suggests that AUD is associated with engagement in high-risk behaviors that subsequently increase the likelihood of traumatic exposure (Begle et al., 2011; McFarlane et al., 2009), perhaps by placing individuals in risky situations (Windle, 1994) or impairing detection of danger cues in the environment (Davis et al., 2009), and thus precedes the development of PTSD. Alternatively, the mutual maintenance model purports that there is a reflexive link between PTSD and AUD, such that PTSD symptoms lead to alcohol misuse and in turn, alcohol misuse maintains or exacerbates PTSD symptoms (Kaysen et al., 2011; McFarlane et al., 2009). Finally, non-temporal models, such as the shared vulnerability hypothesis (María-Ríos & Morrow, 2020), implicate the role of common genetic and environmental risk factors for PTSD and AUD (Sartor et al., 2011). Empirical evidence provides the greatest support for negative reinforcement models (for a systemtatic review, see Hawn et al., in press), suggesting a central function of down-regulation of trauma-related emotional distress in the prediction of alcohol misuse among individuals with PTSD.
Relatedly, contemporary models of alcohol use (Cox & Klinger, 1988, 1990, 2004) highlight internally-driven negative reinforcement as a prominent motivation underlying the development and maintenance of alcohol misuse (for reviews, see Cooper et al., 2016; Kuntsche et al., 2005; Kuntsche et al., 2006). Individuals with PTSD-AUD have been found to be more likely to drink to manage negative emotions than individuals with AUD alone (Grayson & Nolen-Hoeksema, 2005; Miranda et al., 2002; Simpson, 2003; Ullman et al., 2005); these individuals may be at particular risk for alcohol misuse if they perceive it to be an effective strategy for coping with distress. Thus, alcohol use appears to serve to not only down-regulate trauma-related emotional distress, but also negative emotions more broadly among individuals with PTSD. Further, although less studied, there is evidence that these findings extend to specific forms of negative emotions, including the experiences of despondency (Mackinnon et al., 2014; Woicik et al., 2009) and anger (Maisto et al., 2016; Rabinovitz, 2014).
Importantly, however, this research has been limited in its almost exclusive focus on alcohol use to down-regulate negative emotions, despite growing evidence that individuals—particularly those with PTSD (Weiss et al., 2020)—may also engage in efforts to reduce or diminish positive emotional experiences (Zou et al., 2019). Several explanations have been proposed to help explain why individuals with PTSD may engage in efforts to down-regulate positive emotions. Individuals with PTSD may take a judgmental and evaluative stance toward positive emotions (Weiss et al., in press-a; Weiss et al., 2018; Weiss et al., 2019). These maladaptive responses to positive emotional experiences may derive from the heightened physiological arousal elicited by positive emotions (Litz et al., 2000). Indeed, physiological arousal is characteristic of many PTSD symptoms (e.g., intrusions; American Psychiatric Association, 2013), and, as such, may result in emotional distress through stimulus generalization (Roemer et al., 2001). In this respect, heightened levels of physiological arousal, regardless of source (e.g., negative or positive emotions), may be experienced as aversive among individuals with PTSD. An alternative explanation is that individuals with PTSD experience competing negative cognitions in the context of positive emotions (Frewen et al., 2012b; Frewen et al., 2012c). For instance, trauma-exposed individuals may not believe that they deserve to experience positive emotions or interpret positive emotions as a weakness (Lawrence & Lee, 2014). Negative affect interference may drive aversive reactions to positive emotions over time. Individuals with PTSD who experience positive emotions as aversive may engage in efforts to down-regulate positive emotion states (Roemer et al., 2001), including through alcohol use (Weiss et al., 2020). These findings suggest that individuals with PTSD may also be motivated to use alcohol to down-regulate positive emotional experiences.
Extending existing research, the current study examined the associations among PTSD symptom severity, alcohol use to down-regulate specific forms of negative emotions (i.e., despondency and anger) and positive emotions broadly, and alcohol misuse within a sample of trauma-exposed, substance-using community individuals. Furthermore, the indirect effect of PTSD symptom severity on alcohol misuse through alcohol use to down-regulate despondency, anger, and positive emotions was explored. We hypothesized that trauma-exposed individuals with greater PTSD symptom severity would report higher levels of alcohol use to down-regulate despondency, anger, and positive emotions. Further, we hypothesized that trauma-exposed individuals who reported higher levels of alcohol use to down-regulate despondency, anger, and positive emotions would endorse significantly greater alcohol misuse. Finally, we hypothesized that PTSD symptom severity would be indirectly associated with alcohol misuse through alcohol use to down-regulate despondency, anger, and positive emotions.
Method
Participants and Procedure
Trauma-exposed community individuals were recruited from Amazon’s Mechanical Turk (MTurk), an internet based crowdsourcing platform. MTurk generates reliable data (Buhrmester et al., 2011; Shapiro et al., 2013), represents the general population in terms of prevalence of psychiatric problems (Shapiro et al., 2013), and demonstrates utility for trauma research in capturing individuals with PTSD in a cost-/time-effective manner (van Stolk-Cooke et al., 2018).
Participants were screened for the study based upon five inclusion criteria: (1) at least 18 years old, (2) living in North America, (3) working knowledge of English, (4) lifetime exposure to a traumatic event, and (5) past 30-day substance use. Participants who met eligibility criteria provided informed consent and completed the survey on Qualtrics. To improve data quality, we embedded four validity checks in the MTurk survey which assessed attentive responding and comprehension (Aust et al., 2013; Meade & Craig, 2012; Oppenheimer et al., 2009; Thomas & Clifford, 2017). Participants who failed to correctly respond to any of the four validity checks were excluded. Participants were compensated $2.50 for study participation. All procedures were approved by the Institutional Review Board at [redacted].
Exclusions and Missing Data
Of the obtained 951 responses, 392 participants were excluded for not meeting all inclusion criteria (remaining n = 559). We then excluded 172 participants who failed to pass any of the four validity questions (remaining n = 387), and 67 participants who attempted to complete the survey more than once (remaining n = 320). Thus, the final sample included 320 participants. Participants had an average age of 35.78 (SD = 10.63); 46.9% (n = 150) identified as women and 81.6% (n = 261) as White. See Table 1 for sample demographic information.
Table 1.
Sample Characteristics
| N = 320 | M (SD) | n (%) |
|---|---|---|
| Age | 35.78 (10.63) | |
| Gender | ||
| Men | 161 (50.3%) | |
| Women | 150 (46.9%) | |
| Different Gender | 9 (2.8%) | |
| Ethnicity | ||
| Hispanic/Latinx | 44 (14.3%) | |
| Not Hispanic/Latinx | 264 (85.7%) | |
| Race | ||
| White | 261 (81.6%) | |
| African American/Black | 41 (12.8%) | |
| American Indian/Alaskan Native | 14 (4.4%) | |
| Asian | 9 (2.8%) | |
| Different Race | 8 (2.6%) | |
| Employment Status | ||
| Full-time | 258 (81.6%) | |
| Part-time | 34 (10.8%) | |
| Not in Labor Force (Student, Homemaker) | 13 (4.1%) | |
| Unemployed | 11 (3.5%) | |
| Education | ||
| Less than High School | 11 (3.4%) | |
| High School Degree | 30 (9.6%) | |
| Some College | 87 (27.8%) | |
| Four-year College | 114 (36.4%) | |
| More than Four-year College | 71 (22.7%) | |
| Income | $25,847.99 ($35,576.11) |
Note: Participants could indorse more than one racial category.
Measures
Trauma Exposure.
The Life Events Checklist for DSM-5 (LEC-5; Weathers et al., 2013a) is a 17-item self-report measure designed to screen for lifetime exposure to traumatic events. The LEC-5 assesses 16 traumatic events and includes one item assessing any other stressful event not captured in the first 16 items. Participants indicate exposure to each event on a 6-point scale: happened to me, witnessed it, learned about it, part of my job, not sure, and does not apply. Endorsement of any of the first four response options is considered a positive endorsement of a trauma, consistent with DSM-5 Criterion A for PTSD (American Psychiatric Association, 2013). Additionally, using recommendations set forth by Contractor et al. (2020), we created variables to denote trauma type classifications. Specifically, we clustered LEC-5 index traumas as follows: Accidental/Injury Traumas (LEC-5 items 1, 2, 3, 4 and 12), Victimization Traumas (LEC-5 items 6, 8, and 9), and Predominant Death Threat Traumas (LEC-5 items 5, 7, 10, 11, 13–16). Frequencies of endorsement of each LEC-5 traumatic event are presented in Table 2. In this sample, there were no participants who only endorsed item 17 (“any other stressful event”).
Table 2.
Prevalence of Endorsement of LEC-5 Traumatic Events
| Trauma Types | n % |
|---|---|
| Transportation accident (e.g. car accident, boat accident, train wreck, plane crash) | 230 (74.9%) |
| Physical assault (e.g., being attacked, hit, slapped, kicked, beaten up) | 213 (69.4%) |
| Fire or explosion | 179 (58.3%) |
| Life-threatening illness or injury | 169 (55.0%) |
| Serious accident at work, home, or during recreational activity | 168 (65.7%) |
| Sexual assault (e.g., rape, attempted rape, made to perform any type of sexual act through force or threat of harm) | 166 (54.1%) |
| Other unwanted or uncomfortable sexual experience | 161 (52.4%) |
| Sudden accidental death | 150 48.9%) |
| Natural disaster (e.g., flood, hurricane, tornado, earthquake) | 144 (46.9%) |
| Sudden violent death (e.g., homicide, suicide) | 144 (46.9%) |
| Assault with a weapon (e.g., being shot, stabbed, threatened with a knife, gun, bomb) | 139 (45.3%) |
| Severe human suffering | 113 (36.8%) |
| Exposure to toxic substance (e.g., dangerous chemicals, radiation) | 103 (33.6%) |
| Combat or exposure to a war-zone (in the military or as a civilian) | 97 (31.6%) |
| Serious injury, harm, or death you caused to someone else | 83 (27.0%) |
| Captivity (e.g., being kidnapped, abducted, held hostage, prisoner of war) | 81 (26.4) |
PTSD Symptom Severity.
The PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013b) is a 20-item self-report measure designed to assess PTSD symptom severity over the past 30 days. Participants completed the PCL-5 in response to their most distressing traumatic event on the LEC-5. Participants rate each item using a 5-point Likert-type scale (0 = not at all, 4 = extremely) and item scores are summed to create a total score. Higher scores indicate greater PTSD symptom severity; a score of 33 or higher indicates a probable PTSD diagnosis (Blevins et al., 2015). The PCL-5 has demonstrated excellent psychometric properties (Bovin et al., 2016; Wortmann et al., 2016), and reliability in the current sample was excellent (Cronbach’s α = .97).
Alcohol Use to Down-Regulate Negative and Positive Emotions.
The revised Regulatory Emotional Self-Efficacy Scale (rRESE; Zou et al., 2019) is a 12-item self-report measure designed to assess one’s self-perceived ability to regulate negative and positive emotions. The rRESE contains two subscales for down-regulating negative emotions – despondency (i.e., general negative feelings) and anger – and one subscale for down-regulating positive emotions. Participants rate their self-efficacy beliefs on a 7-point Likert-type scale (1 = not at all well, 7 = extremely well) and respective item scores are summed to create subscale scores. Higher scores indicate greater down-regulation of despondency, anger, and positive emotions. The current study modified the rRESE to examine the extent to which alcohol functioned to down-regulate both negative and positive emotions. The rRESE has demonstrated good psychometric properties (Zou et al., 2019), and reliability in the current sample was good (Cronbach’s α = .85, .88, and .82 for down-regulation of despondency, anger, and positive emotions, respectively).
Alcohol Misuse.
The Alcohol Use Disorder Identification Test (AUDIT; Saunders et al., 1993) is a 10-item self-report measure designed to assess alcohol misuse. Participants rate each item using a 5-point Likert-type scale and item scores are summed to create a total score. Higher scores indicate greater likelihood of alcohol misuse, with a recommended cutoff score of ≥ 8 to identify probable AUD (Babor et al., 2001). The AUDIT has good psychometric properties (Saunders et al., 1993), and reliability in the current sample was excellent (Cronbach’s α = .90).
Data Analysis
Descriptive information was calculated to characterize the sample. Pearson correlations were conducted to examine the bivariate associations among PTSD symptom severity, alcohol use to down-regulate negative (i.e., despondency and anger) and positive emotions, and alcohol misuse. Using Model 1 of the PROCESS SPSS macro (Hayes, 2012), we tested whether alcohol use to down-regulate despondency, anger, and positive emotions, separately and simultaneously, indirectly affected the relationship between PTSD symptom severity and alcohol misuse. Gender responses were coded into ‘male’ and ‘female’ (other responses were excluded due to limited endorsement) and included as a covariate in study analyses given well-established relations with both PTSD (Kilpatrick et al., 2013) and AUD (Grant et al., 2015). The bootstrap method was used for estimating the standard errors of parameter estimates and the bias-corrected confidence intervals of the indirect effects (MacKinnon et al., 2002; Preacher & Hayes, 2004). The bias-corrected confidence interval is based on a non-parametric re-sampling procedure that has been recommended when estimating confidence intervals of the indirect effect due to the correction it applies over a large number of bootstrapped samples (Efron, 1987). The indirect effect is significant if the 95% confidence interval does not contain zero (Preacher & Hayes, 2004). In this study, 5,000 bootstrap samples were used. Standardized estimates are presented to facilitate comparison of the magnitude of change from the total to the direct effect. Sobel tests examined whether the relation between PTSD symptom severity and alcohol misuse decreased when accounting for alcohol to down-regulate despondency, anger, and positive emotions, separately. In the model testing alcohol use to down-regulate despondency, anger, and positive emotions, simultaneously, percent reduction in effect between the total and direct effect was calculated.
Results
Preliminary Analyses
One-hundred and forty-two participants (44.5%) reported PTSD symptoms consistent with a probable PTSD diagnosis, 175 participants (54.9%) reported alcohol misuse symptoms consistent with a probable AUD diagnosis, and 93 participants (29.2%) reported PTSD symptoms and alcohol misuse symptoms consistent with probable PTSD and AUD diagnoses. Descriptive data and Pearson correlations are presented in Table 3. PTSD symptom severity, alcohol use to down-regulate negative (i.e., despondency and anger) and positive emotions, and alcohol misuse were significantly positively associated with each other.
Table 3.
Descriptive Data and Bivariate Correlations for the Primary Variables of Interest
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. PCL-5 | - | .03 | .06 | .01 | .48* | .49* | .43* | .31* |
| 2. LEC-5 – Accidental/Injury Traumas | .03 | - | .54* | .67* | .03 | −.01 | .04 | .01 |
| 3. LEC-5 – Victimization Traumas | .05 | .54 | - | .60* | .03 | .05 | .03 | .03 |
| 4. LEC-5 – Predominant Death Threat Traumas | .01 | .67 | .60 | - | .03 | .07 | .05 | .04 |
| 5. rRESE – Down-regulation of Despondency | .47 | .03 | .03 | .03 | - | .69* | .62* | .57* |
| 6. rRESE – Down-regulation of Anger | .48 | −.02 | .05 | .07 | .68 | - | .77* | .43* |
| 7. rRESE – Down-regulation of Positive Emotions | .43 | .02 | .03 | .05 | .60 | .76 | - | .38 |
| 8. AUDIT | .34 | .09 | .03 | .04 | .59 | .44 | .38 | - |
| M | 28.19 | 3.43 | 1.75 | 2.96 | 7.16 | 6.25 | 5.57 | 11.11 |
| SD | 21.92 | 1.41 | 1.71 | 2.71 | 3.62 | 3.70 | 3.53 | 8.81 |
| Observed Range | 0 – 78 | 1 – 5 | 0 – 3 | 0 – 8 | 3 – 15 | 2 – 15 | 3 – 15 | 0 – 38 |
Note: PCL-5 = PTSD Symptom Checklist for DSM-V; rRESE = Revised Regulatory Emotional Self-Efficacy Scale; AUDIT = Alcohol Use Disorder Identification Test.
denotes correlations that are significant at the p < .001 level. Values to the right of the diagonal reflect zero-order correlations, while values to the left of the diagonal reflect partial correlations controlling for gender. LEC-5 – Accidental/Injury Traumas (LEC-5 items 1, 2, 3, 4 and 12). LEC-5 – Victimization Traumas (LEC-5 items 6, 8, and 9). LEC-5 – Predominant Death Threat Traumas (LEC-5 items 5, 7, 10, 11, 13–16).
Primary Analyses1,2
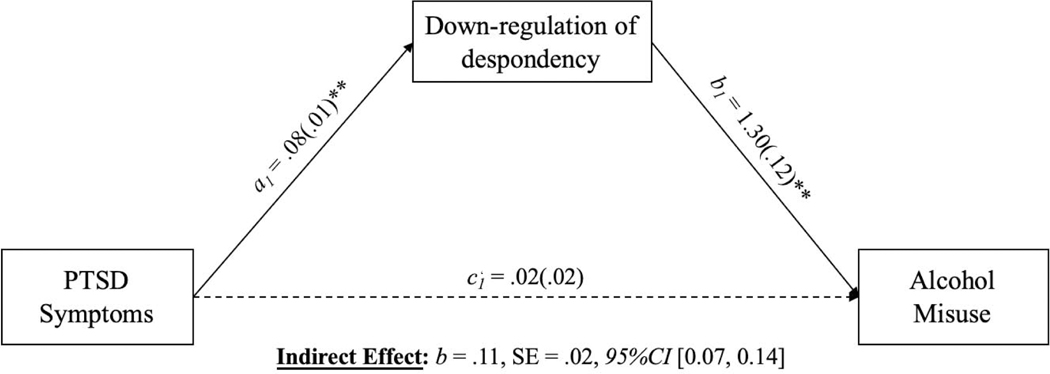
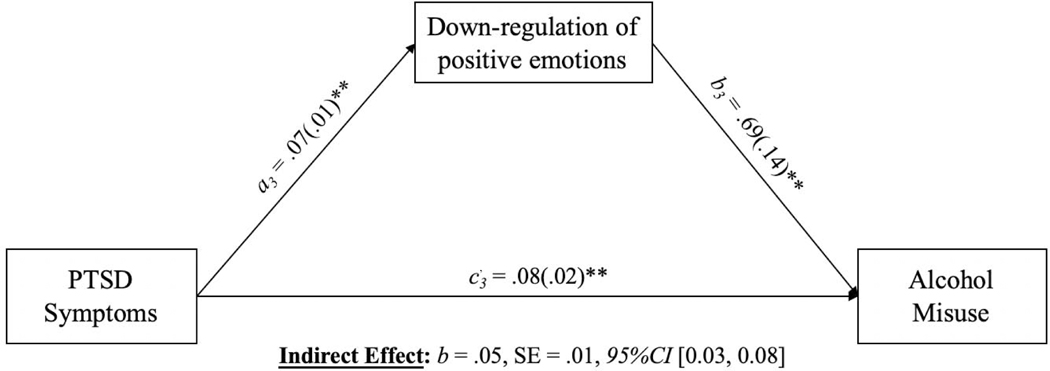
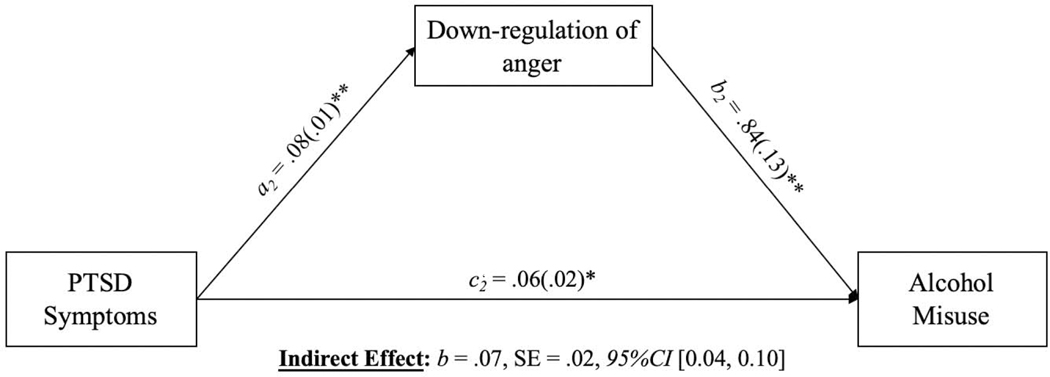
Models explicating the indirect effects of alcohol use to down-regulate despondency, anger, and positive emotions, separately, on the association between PTSD symptom severity and alcohol misuse (adjusting for gender) are depicted in Figures 1–3.
Figure 1.
Indirect effect of alcohol use to down-regulate despondency in the relation between PTSD symptoms and alcohol misuse adjusting for gender
Note. **p < .01. Solid lines represent significant associations at the level p < .05. Dashed lines represent non-significant associations.
Figure 3.
Indirect effect of alcohol use to down-regulate positive emotion in the relation between PTSD symptoms and alcohol misuse adjusting for gender
Note. **p < .01. Solid lines represent significant associations at the level p < .05.
In the model examining alcohol use to down-regulate despondency (see Figure 1), the association between PTSD symptom severity and alcohol use to down-regulate despondency was significant, b = .08, SE = .01, t = 9.90, p < .001, 95%CI [0.06, 0.10], as was the association between alcohol use to down-regulate despondency and alcohol misuse, b = 1.31, SE = .13, t = 10.16, p < .001, 95%CI [1.05, 1.56]. Further, the indirect effect of PTSD symptom severity on alcohol misuse through the pathway of alcohol use to down-regulate despondency was significant, completely standardized b = .26, SE = .04, 95%CI [0.18, 0.34]. Notably, the direct effect linking PTSD symptom severity to alcohol misuse was non-significant after controlling for alcohol use to down-regulate despondency, completely standardized b = .06, SE = .02, t = 1.13, p = .26, 95%CI [−0.02, 0.07]. The Sobel test indicated that the effect of PTSD symptom severity on alcohol misuse significantly decreased when controlling for alcohol use to down-regulate despondency, and was found to be significant (z = 7.10, p < .001).
In the model examining alcohol use to down-regulate anger (see Figure 2), the association between PTSD symptom severity and alcohol use to down-regulate anger was significant, b = .08, SE = .01, t = 10.37, p < .001, 95%CI [0.07, 0.10], as was the association between alcohol use to down-regulate anger and alcohol misuse, b = .84, SE = .14, t = 6.04, p < .001, 95%CI [0.57, 1.12]. Further, the indirect effect of PTSD symptom severity on alcohol misuse through the pathway of alcohol use to down-regulate anger was significant, completely standardized b = .18, SE = .04, 95%CI [0.11, 0.26]. However, the direct effect linking PTSD symptom severity to alcohol misuse remained significant after controlling for alcohol use to down-regulate anger, completely standardized b = .14, SE = .02, t = 2.46, p = .01, 95%CI [0.01, 0.10]. The Sobel test indicated that the effect of PTSD symptom severity on alcohol misuse significantly decreased when controlling for alcohol use to down-regulate anger (z = 4.80, p < .001).
Figure 2.
Indirect effect of alcohol use to down-regulate anger in the relation between PTSD symptoms and alcohol misuse adjusting for gender
Note. *p < .05, **p < .01. Solid lines represent significant associations at the level p < .05.
In the model examine alcohol use to down-regulate positive emotions (see Figure 3), the association between PTSD symptom severity and alcohol use to down-regulate positive emotions was significant, b = .07, SE = .01, t = 8.87, p < .001, 95%CI [0.06, 0.09], as was the association between alcohol use to down-regulate positive emotions and alcohol misuse, b = .69, SE = .15, t = 4.79, p < .001, 95%CI [0.41, 0.98]. Further, the indirect effect of PTSD symptom severity on alcohol misuse through the pathway of alcohol use to down-regulate positive emotions was significant, completely standardized b = .12, SE = .03, 95%CI [0.07, 0.19]. However, the direct effect linking PTSD symptom severity and alcohol misuse remained significant after controlling for alcohol use to down-regulate positive emotions, completely standardized b = .20, SE = .02, t = 3.45, p = .001, 95%CI [0.03, 0.13]. The Sobel test indicated that the effect of PTSD symptom severity on alcohol misuse significantly decreased when controlling for alcohol use to down-regulate positive emotions (z = 3.84, p < .001).
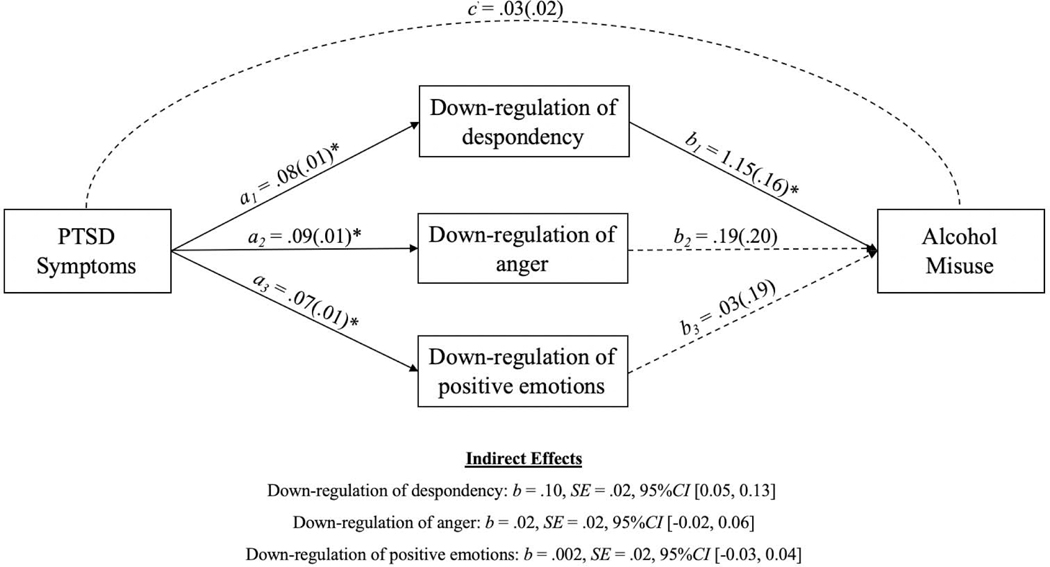
Supplemental Analyses
A fourth model examining the indirect effects of alcohol use to down-regulate despondency, anger, and positive emotions, simultaneously, on the association between PTSD symptom severity and alcohol misuse (adjusting for gender) is depicted in Figure 4. The association between PTSD symptom severity and alcohol use to down-regulate despondency was significant, b = .08, SE = .01, t = 9.64, p < .001, 95%CI [0.06, 0.10], as was the association between alcohol use to down-regulate despondency and alcohol misuse, b = 1.15, SE = .16, t = 7.11, p < .001, 95%CI [0.83, 1.47]. Further, the indirect effect of PTSD symptom severity on alcohol misuse through the pathway of alcohol use to down-regulate despondency was significant, completely standardized b = −.004, SE = .02, 95%CI [0.05, 0.13]. Conversely, while the association between PTSD symptom severity and alcohol use to down-regulate anger was significant, b = .09, SE = .01, t = 10.37, p < .001, 95%CI [0.07, 0.10], the association between alcohol use to down-regulate anger and alcohol misuse was not significant, b = .19, SE = .20, t = 0.99, p = .33, 95%CI [−0.19, 0.59]. Further, the indirect effect of PTSD symptom severity on alcohol misuse through the pathway of alcohol use to down-regulate anger was not significant, completely standardized b = −.001 , SE = .02, 95%CI [−0.02, 0.06]. Similarly, while the association between PTSD symptom severity and alcohol use to down-regulate positive emotions was significant, b = .07, SE = .01, t = 8.70, p < .001, 95%CI [0.06, 0.09], the association between alcohol use to down-regulate positive emotions and alcohol misuse was not significant, b = .03, SE = .19, t = 0.19, p = .90, 95%CI [−0.34, 0.40]. Further, the indirect effect of PTSD symptom severity on alcohol misuse through the pathway of alcohol use to down-regulate positive emotions was not significant, completely standardized b = .007, SE = .02, 95%CI [−0.03, 0.04]. The direct effect of PTSD symptom severity to alcohol use was not significant, completely standardized b = .31, SE = .02, t = 1.05, p = .30, 95%CI [−0.02, 0.07]. There was a 12.7% reduction in the effect of PTSD symptom severity on alcohol misuse when controlling for down-regulation of despondency, anger, and positive emotions in this combined model.
Figure 4.
Indirect effects of alcohol use to down-regulate despondency, anger, and positive emotions, simultaneously, in the relation between PTSD symptoms and alcohol misuse adjusting for gender
Note. *p < .001. Solid lines represent significant associations at the level p < .001.
Discussion
The goal of the current study was to advance functional models linking co-occurring PTSD-AUD. Specifically, we explored whether alcohol use to down-regulate both negative and positive emotions contributed to the relation between PTSD symptom severity and alcohol misuse in a sample of trauma-exposed, substance-using community individuals. Results indicated that PTSD symptom severity was indirectly associated with alcohol misuse through alcohol use to down-regulate negative and positive emotions. Specifically, individuals with greater PTSD symptom severity reported significantly higher levels of alcohol use to down-regulate despondency, anger, and positive emotions, which, in turn, were linked to greater alcohol misuse. Findings extend understanding of the role of emotional processes (and uniquely for positive emotions) in the PTSD-AUD relationship, highlighting important avenues for future research and practice. Of note, when interpreting the study findings, it is important to consider the high extent to which the current sample needed to be truncated (57%). While using validity checks and excluding individuals who take the survey more than once improves MTurk data quality (Oppenheimer et al., 2009; Buhrmester et al., 2011; Aust et al., 2013) and the extent of our sample truncation is comparable to other MTurk trauma studies (57%; van Stolk-Cooke et al., 2018), a potential selection bias in our study may limit generalizability of study findings.
Theoretical models of PTSD-AUD purport that alcohol use is often developed, maintained, and exacerbated by negative reinforcement processes (Brady et al., 2004). Consistent with this assertion, existing empirical work in this area indicates that alcohol use among individuals with PTSD reduces or diminishes trauma-related distress and negative affect more broadly (Hawn et al., 2020; Hawn et al., in press-b). However, with the focus of this research being on negative emotions generally, there is limited understanding of the effect of alcohol use to down-regulate specific forms of negative emotions or positive emotions broadly. Greater specificity of the functional role of alcohol use in the context of negative and positive emotions is necessary to inform targeted assessment and intervention efforts for alcohol misuse. In this vein, results of the current study extend past research by suggesting that efforts to down-regulate specific negative emotions (i.e., despondency and anger) and positive emotions broadly may play an important role in PTSD-AUD. Specifically, our findings indicated that individuals with greater PTSD symptom severity engaged in more efforts to down-regulate despondency, anger, and positive emotions, which, in turn, were associated with greater alcohol misuse.
While alcohol use to down-regulate negative emotions, such as despondency (Mackinnon et al., 2014; Woicik et al., 2009) and anger (Maisto et al., 2016; Rabinovitz, 2014), is well-understood in the context of existing research, less obvious are the conceptual underpinnings explaining alcohol use to down-regulate positive emotions. Positive emotions are generally a desired outcome (Bastian et al., 2014), and often serve as a protective function post-trauma (Folkman, 2008), such as by counteracting negative emotions (Tugade & Fredrickson, 2004) and restoring physiological, psychological, and social resources (Fredrickson, 1998, 2001). Counterintuitively, however, there is growing evidence to suggest that positive emotions have the potential to elicit aversive reactions (Frewen et al., 2012a; Weiss et al., 2015) and thus may be intentionally suppressed (Beblo et al., 2013; Roemer et al., 2001), including via alcohol use (Weiss et al., 2020). This tendency to negatively evaluate positive emotions—and subsequently down-regulate them through alcohol use—may be especially pronounced in PTSD. Individuals with PTSD exhibit greater non-acceptance of positive emotions, frequently exhibiting secondary emotional responding, such as fear or shame, in their context (Weiss et al., in press-a; Weiss et al., 2018; Weiss et al., 2019). Aversive responses to positive emotions may result from negative affect interference (i.e., negative emotions in the context of positive emotional stimuli; Frewen et al., 2012a) or stimulus generalization (e.g., fear of physiological arousal linked to positive emotions due to pairing with trauma cues; Roemer et al., 2001). Notably, individuals with PTSD have been found to be more likely to use alcohol in contexts that signal negative reinforcement (Sharkansky et al., 1999; Stewart et al., 2000). Evidence suggests that this finding may extend to positive emotions: individuals with PTSD are more likely to engage in efforts to down-regulate positive emotions (Roemer et al., 2001) through means such as alcohol use (Weiss et al., 2020). Our findings here provide additional support for this hypothesis, suggesting the need for more rigorous examination of the down-regulatory function of positive emotions in PTSD-AUD.
Of note, while alcohol use to down-regulate despondency, anger, and positive emotions, separately, accounted for the relation of PTSD symptom severity to alcohol misuse, in a model that simultaneously examined these factors, only alcohol use to down-regulate despondency made a significant and unique contribution to this association. Thus, while trauma-exposed, substance-using community individual’s use of alcohol to down-regulate despondency, anger, and positive emotions may help explain the relation of PTSD symptom severity to alcohol misuse, and thus be important factors to consider, alcohol use to down-regulate despondency may be particularly relevant to our understanding and treatment of PTSD-AUD. These findings are not surprising given the extensive literature linking despondency to alcohol misuse (for reviews, see Boden & Fergusson, 2011; Foulds et al., 2015). Future research would benefit from further explicating of the relative and unique roles of alcohol use to down-regulate despondency, anger, and positive emotions in PTSD-AUD. For instance, person-centered approaches may clarify whether there subgroups (i.e., classes) of individuals that are differentiated by levels of alcohol use to down-regulate despondency, anger, and positive emotions, and whether PTSD symptom severity and alcohol misuse differ across these classes.
Results should be considered within the context of study limitations. First, the cross-sectional and correlational nature of the data precludes causal determination of examined associations. Future research is needed to investigate the nature and direction of these relations through prospective, longitudinal investigations. Second, this study relied exclusively on self-report measures. Future investigations should include objective measures shown to demonstrate concordance with emotional responding (Gratz et al., 2006). Third, although MTurk is a cost- and time-effective approach for conducting research with individuals with PTSD (van Stolk-Cooke et al., 2018), collecting data through the internet has some disadvantages that may limit generalizability of results, such as sample biases and lack of control over the research setting (Kraut et al., 2004). Fourth, the measure of down-regulation utilized here assessed positive emotions broadly. Theoretical accounts suggest that individuals with PTSD may be particularly motivated to down-regulate high arousal positive emotions (e.g., excitement); future work is needed to parse the down-regulation of the specific types of positive emotions in relation to PTSD and alcohol misuse. Fifth, although we were able to consider the influence of type of trauma in our study analyses, our measure of traumatic exposure did not allow us to test the influence of other important trauma-related characteristics, such as time passed since the traumatic event, age at which the traumatic event was experienced, and perpetrator type in the case of interpersonal trauma. Future investigations in this area should assess for and explore these trauma characteristics. Lastly, we examined relations among PTSD symptom severity, down-regulation of negative and positive emotions, and alcohol misuse in a community sample. Replication among other trauma-exposed populations (e.g., treatment-seeking) is warranted.
Despite these limitations, the results of the current study advance our understanding of the functional association between PTSD and AUD. Specifically, our findings suggest that trauma-exposed, substance-using individuals in the community with greater severity of PTSD symptoms report higher levels of alcohol use to down-regulate negative (i.e., despondency and anger) and positive emotions, which, in turn, are associated with greater alcohol misuse. These findings suggest that theoretical models explaining PTSD-AUD may benefit from consideration of the potential negatively reinforcing function of alcohol use in the context of positive emotions. Moreover, if replicated, the results of the current study may suggest the need for modification of current PTSD-AUD treatments to address the down-regulation of positive emotions. Most PTSD-AUD treatments uniformly target an increase in positive emotions among patients. Our findings converge with mounting research to suggest that high levels of positive emotions may, at times, confer maladaptive outcomes (e.g., positive emotion dysregulation, positive urgency, positive emotion persistence; Cyders et al., 2007; Gruber, 2011; Weiss et al., 2015). As such, clinicians treating individuals with PTSD-AUD may first want to assess maladaptive responses to positive emotions, and, when indicated, address these areas of concern.
Highlights.
PTSD was linked to alcohol misuse via down-regulation of negative/positive emotions
Extends current models by supporting a down-regulation function for positive emotions
PTSD-AUD interventions may target down-regulation of positive emotions
Acknowlegdements
Role of Funding Sources
Work on this paper by the first author (NHW) was supported by National Institutes of Health Grants K23DA039327 and P20GM125507. The opinions, findings, and conclusions or recommendations in this manuscript are those of the authors and do not necessarily reflect those of the National Institutes of Health.
Contributors: NHW designed the study and wrote the majority of the paper. SG conducted statistical analyses. AMR, MRS, and AAC provided feedback on all drafts.
Footnotes
NHW: Conceptualization, Writing - Original Draft, Methodology
SG: Formal analysis
AMR: Writing - Review & Editing
MRS: Writing - Review & Editing
AAC: Writing - Review & Editing
Conflict of Interest: None.
Conflict of Interest
None to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Study analyses were reran excluding 13 participants who did not endorse any past 30-day alcohol use. The strength and direction of the study findings remained the same.
Study analyses were reran controlling for the trauma type classifications described by Contractor et al. (2020; i.e., Accidental/Injury Traumas, Victimization Traumas, and Predominant Death Threat Traumas). The strength and direction of the findings remained the same. As such, for the sake of parsimony, we decided to retain our initial analyses.
References
- American Psychiatric Association; (2013). Diagnostic and statistical manual of mental disorders (5th ed.). [Google Scholar]
- Aust F, Diedenhofen B, Ullrich S, & Musch J. (2013). Seriousness checks are useful to improve data validity in online research. Behavior Research Methods, 45, 527–535. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Bibble JC, Saunders JB, & Monteiro MG (2001). The alcohol use disorder identification test. World Health Organization. [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111, 33–51. [DOI] [PubMed] [Google Scholar]
- Bastian B, Kuppens P, De Roover K, & Diener E. (2014). Is valuing positive emotion associated with life satisfaction? Emotion, 14, 639–645. [DOI] [PubMed] [Google Scholar]
- Beblo T, Fernando S, Kamper P, Griepenstroh J, Aschenbrenner S, Pastuszak A, Schlosser N, & Driessen M. (2013). Increased attempts to suppress negative and positive emotions in borderline personality disorder. Psychiatry Research, 210, 505–509. [DOI] [PubMed] [Google Scholar]
- Begle AM, Hanson RF, Danielson CK, McCart MR, Ruggiero KJ, Amstadter AB, Resnick HS, Saunders BE, & Kilpatrick DG (2011). Longitudinal pathways of victimization, substance use, and delinquency: Findings from the national survey of adolescents. Addictive Behaviors, 36, 682–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28, 489–498. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychological Assessment, 28, 1379–1391. [DOI] [PubMed] [Google Scholar]
- Brady KT, Back SE, & Coffey SF (2004). Substance abuse and posttraumatic stress disorder. Current Directions in Psychological Science, 13, 206–209. [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon’s mechanical turk: A new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science, 6, 3–5. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Kuntsche E, Levitt A, Barber LL, & Wolf S. (2016). Motivational models of substance use: A review of theory and research on motives for using alcohol, marijuana, and tobacco In Sher KJ, (Ed.), The Oxford Handhood of Substance Use Disorders (Vol. 1). Oxford University Press. [Google Scholar]
- Cox WM, & Klinger E. (1988). A motivational model of alcohol use. Journal of Abnormal Psychology, 97, 168–180. [DOI] [PubMed] [Google Scholar]
- Cox WM, & Klinger E. (1990). Incentive motivation, affective change, and alcohol use: A model In Cox WM (Ed.), Why people drink (pp. 291–311). Gardner Press. [Google Scholar]
- Cox WM, & Klinger E. (2004). A motivational model of alcohol use: Determinants of use and change In Cox WM & Klinger E. (Eds.), Handbook of motivational counseling: Concepts, approaches, and assessment (pp. 121–138). John Wiley & Sons. [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, & Peterson C. (2007). Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychological Assessment, 19, 107–118. [DOI] [PubMed] [Google Scholar]
- Davis KC, Stoner SA, Norris J, George WH, & Masters NT (2009). Women’s awareness of and discomfort with sexual assault cues: Effects of alcohol consumption and relationship type. Violence Against Women, 15, 1106–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efron B. (1987). Better bootstrap confidence intervals. Journal of the American Statistical Association, 82, 171–185. [Google Scholar]
- Folkman S. (2008). The case for positive emotions in the stress process. Anxiety, Stress & Coping, 21, 3–14. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL (1998). What good are positive emotions? Review of General Psychology, 2, 300–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56, 218–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen PA, Dean JA, & Lanius RA (2012a). Assessment of anhedonia in psychological trauma: Development of the hedonic deficit and interference scale. European Journal of Psychotraumatology, 3, 8585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen PA, Dozois DJA, & Lanius RA (2012b). Assessment of anhedonia in psychological trauma: Psychometric and neuroimaging perspectives. European Journal of Psychotraumatology, 3, 8587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen PA, Dozois DJA, Neufeld RWJ, & Lanius RA (2012c). Disturbances of emotional awareness and expression in posttraumatic stress disorder: Meta-mood, emotion regulation, mindfulness, and interference of emotional expressiveness. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 152–161. [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, & Huang B. (2015). Epidemiology of DSM-5 alcohol use disorder: Results from the national epidemiologic survey on alcohol and related conditions-iii. JAMA psychiatry, 72, 757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, & Gunderson JG (2006). An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology, 115, 850–855. [DOI] [PubMed] [Google Scholar]
- Grayson CE, & Nolen-Hoeksema S. (2005). Motives to drink as mediators between childhood sexual assault and alcohol problems in adult women. Journal of Traumatic Stress, 18, 137–145. [DOI] [PubMed] [Google Scholar]
- Gruber J. (2011). Can feeling too good be bad? Positive emotion persistence (pep) in bipolar disorder. Current Directions in Psychological Science, 20, 217–221. [Google Scholar]
- Hawn SE, Bountress KE, Sheerin CM, Dick DM, & Amstadter AB (2020). Trauma-related drinking to cope: A novel approach to the self-medication model. Psychology of Addictive Behaviors, 34(3), 465–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawn SE, Cusack SE, & Amstadter AB (in press). A systematic review of the self-medication hypothesis in the context of posttraumatic stress disorder and comorbid problematic alcohol use. Journal of Traumatic Stress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2012). Process: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. University of Kansas, KS. [Google Scholar]
- Kaysen D, Atkins DC, Moore SA, Lindgren KP, Dillworth T, & Simpson T. (2011). Alcohol use, problems, and the course of posttraumatic stress disorder: A prospective study of female crime victims. Journal of Dual Diagnosis, 7, 262–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4, 231–244. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26, 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraut R, Olson J, Banaji M, Bruckman A, Cohen J, & Couper M. (2004). Psychological research online: Report of board of scientific affairs’ advisory group on the conduct of research on the internet. American Psychologist, 59, 105–117. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, & Engels R. (2005). Why do young people drink? A review of drinking motives. Clinical Psychology Review, 25, 841–861. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, & Engels R. (2006). Who drinks and why? A review of socio-demographic, personality, and contextual issues behind the drinking motives in young people. Addictive Behaviors, 31, 1844–1857. [DOI] [PubMed] [Google Scholar]
- Lawrence VA, & Lee D. (2014). An exploration of people’s experiences of compassion-focused therapy for trauma, using interpretative phenomenological analysis. Clinical Psychology & Psychotherapy, 21, 495–507. [DOI] [PubMed] [Google Scholar]
- Litz BT, Orsillo SM, Kaloupek D, & Weathers F. (2000). Emotional processing in posttraumatic stress disorder. Journa of Abnormal Psychology, 109, 26–39. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V. (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon SP, Kehayes I-LL, Clark R, Sherry SB, & Stewart SH (2014). Testing the four-factor model of personality vulnerability to alcohol misuse: A three-wave, one-year longitudinal study. Psychology of Addictive Behaviors, 28, 1000–1012. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Ewart CK, Witkiewitz K, Connors GJ, Elder G, Krenek M, & Ditmar M. (2016). Predicting drinking lapses in alcohol use disorder: The toxic combination of agonistic striving and poor anger regulation. Journal of Social and Clinical Psychology, 35, 235–254. [Google Scholar]
- María-Ríos CE, & Morrow JD (2020). Mechanisms of shared vulnerability to post-traumatic stress disorder and substance use disorders. Frontiers in Behavioral Neuroscience, 14, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane AC, Browne D, Bryant R, O’Donnell M, Silove D, Creamer M, & Horsley K. (2009). A longitudinal analysis of alcohol consumption and the risk of posttraumatic symptoms. Journal of Affective Disorders, 118, 166–172. [DOI] [PubMed] [Google Scholar]
- Meade AW, & Craig SB (2012). Identifying careless responses in survey data. Psychological Methods, 17, 437–455. [DOI] [PubMed] [Google Scholar]
- Miranda R, Meyerson LA, Long PJ, Marx BP, & Simpson SM (2002). Sexual assault and alcohol use: Exploring the self-medication hypothesis. Violence and Victims, 17, 205–217. [DOI] [PubMed] [Google Scholar]
- Oppenheimer DM, Meyvis T, & Davidenko N. (2009). Instructional manipulation checks: Detecting satisficing to increase statistical power. Journal of Experimental Social Psychology, 45, 867–872. [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36, 717–731. [DOI] [PubMed] [Google Scholar]
- Rabinovitz S. (2014). Drowning your sorrows? Social exclusion and anger effects on alcohol drinking. Addiction Research & Theory, 22, 363–370. [Google Scholar]
- Roemer L, Litz BT, Orsillo SM, & Wagner AW (2001). A preliminary investigation of the role of strategic withholding of emotions in ptsd. Journal of Traumatic Stress, 14, 149–156. [Google Scholar]
- Sartor CE, McCutcheon V, Pommer N, Nelson E, Grant J, Duncan A, Waldron M, Bucholz K, Madden P, & Heath A. (2011). Common genetic and environmental contributions to post-traumatic stress disorder and alcohol dependence in young women. Psychological Medicine, 41, 1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M. (1993). Development of the alcohol use disorders identification test (audit): WHO collaborative project on early detection of persons with harmful alcohol consumption-ii. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Shapiro DN, Chandler J, & Mueller PA (2013). Using mechanical turk to study clinical populations. Clinical Psychological Science 1(2), 213–220. [Google Scholar]
- Sharkansky EJ, Brief DJ, Peirce JM, Meehan JC, & Mannix LM (1999). Substance abuse patients with posttraumatic stress disorder (PTSD): Identifying specific triggers of substance use and their associations with ptsd symptoms. Psychology of Addictive Behaviors, 13, 89. [Google Scholar]
- Simpson TL (2003). Childhood sexual abuse, PTSD, and the functional roles of alcohol use among women drinkers. Substance Use & Misuse, 38(2), 249–270. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Conrod PJ, Samoluk SB, Pihl RO, & Dongier M. (2000). Posttraumatic stress disorder symptoms and situation-specific drinking in women substance abusers. Alcoholism Treatment Quarterly, 18(3), 31–47. [Google Scholar]
- Thomas KA, & Clifford S. (2017). Validity and mechanical turk: An assessment of exclusion methods and interactive experiments. Computers in Human Behavior, 77, 184–197. [Google Scholar]
- Tugade MM, & Fredrickson BL (2004). Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology, 86, 320–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, Filipas HH, Townsend SM, & Starzynski LL (2005). Trauma exposure, posttraumatic stress disorder and problem drinking in sexual assault survivors. Journal of Studies on Alcohol, 66, 610–619. [DOI] [PubMed] [Google Scholar]
- van Stolk-Cooke K, Brown A, Maheux A, Parent J, Forehand R, & Price M. (2018). Crowdsourcing trauma: Psychopathology in a trauma-eposed sample recruited via mechanical turk. Journal of Traumatic Stress, 31, 549–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013a). The life events checklist for DSM-5 (LEC-5). [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013b). The PTSD checklist for DSM-5 (PCL-5). [Google Scholar]
- Weiss NH, Contractor AA, Forkus SR, Goncharenko S, & Raudales AM (in press-a). Positive emotion dysregulation among community individuals: The role of traumatic exposure and posttraumatic stress disorder. Journal of Traumatic Stress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Dixon-Gordon KL, Peasant C, & Sullivan TP (2018). An examination of the role of difficulties regulating positive emotions in posttraumatic stress disorder. Journal of Traumatic Stress, 31, 775–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Forkus SR, Raudales AM, Schick MR, & Contractor AA (2020). Alcohol misuse to down-regulate positive emotions: A cross-sectional multiple mediator analysis among us military veterans. Addictive Behaviors, 105, 106322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Gratz KL, & Lavender J. (2015). Factor structure and initial validation of a multidimensional measure of difficulties in the regulation of positive emotions: The ders-positive. Behavior Modification, 39, 431–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Nelson R, Contractor AA, & Sullivan TP (2019). Emotion dysregulation and posttraumatic stress disorder: A test of the incremental role of difficulties regulating positive emotions Anxiety, Stress, & Coping, 32(4), 443–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M. (1994). Substance use, risky behaviors, and victimization among a U.S. national adolescent sample. Addiction, 89, 175–182. [DOI] [PubMed] [Google Scholar]
- Woicik PA, Stewart SH, Pihl RO, & Conrod PJ (2009). The substance use risk profile scale: A scale measuring traits linked to reinforcement-specific substance use profiles. Addictive Behaviors, 34(12), 1042–1055. [DOI] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, Foa EB, Young-McCaughan S, Yarvis JS, & Hembree EA (2016). Psychometric analysis of the PTSD checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28, 1392–1403. [DOI] [PubMed] [Google Scholar]
- Zou C, Plaks JE, & Peterson JB (2019). Don’t get too excited: Assessing individual differences in the down-regulation of positive emotions. Journal of Personality Assessment, 101, 73–83. [DOI] [PubMed] [Google Scholar]