Abstract
Objective:
Anxiety and depression symptoms in epilepsy are common, impactful and under-recognized and undertreated. While prior survey data suggests equipoise among epileptologists for managing anxiety and/or depression via prescribing in the epilepsy clinic versus psychiatry referral, patient preferences are unknown and should potentially influence practice habits among epileptologists. Thus, the primary objective of this study was to determine patient preference for anxiety and/or depression prescribing by neurologists versus psychiatry referral among an adult epilepsy clinic sample of symptomatic patients.
Methods:
Management preferences for anxiety and/or depression were surveyed in an adult tertiary care epilepsy clinic. Individuals who screened positive for anxiety and/or depression symptoms on validated instruments during a routine care-embedded learning health system study were recruited. Demographics, social variables, psychiatric treatment history, and treatment priorities and preferences were surveyed. Preference was defined as a slightly greater than 2:1 ratio in favor neurology prescribing or psychiatry referral. The study was powered to assess this primary objective using a two-sample binomial test. Multinomial logistic regression examined an a priori multivariable model of treatment preference (secondary objective).
Results:
The study sample included N=63 symptomatic adults, with 64% women and mean age 42.2 years. Most reported past or current treatment for anxiety and/or depression, and treatment for these symptoms was a high or moderate priority among 65.1% of the sample. Neurologist prescribing was preferred in 83.0% (nearly 5:1) over psychiatry referral among those who chose neurology or psychiatry (as opposed to neither of the two; p<0.001, 95% CI 0.702–0.919). Overall, 69.8% of the total study sample preferred neurology prescribing. Multivariable modeling indicated preference for neither management option (compared with neurologist prescribing) was associated with low overall treatment prioritization and having never received neurologist medication management. None of the factors examined in the a priori multivariable model were associated with selecting psychiatry referral (compared to neurologist prescribing).
Conclusion:
In this sample, most patients indicated a preference for neurologists to prescribe for anxiety or depression symptoms in the epilepsy clinic. Care models involving neurologist prescribing for anxiety and depression symptoms merit further investigation and potential adoption in clinical practice.
Keywords: epilepsy, anxiety, depression, patient treatment preferences, neurologist, psychiatrist
1. INTRODUCTION
Anxiety and depression in epilepsy are prevalent and better predictors of poor quality of life than seizure frequency[1–3]. These symptoms are associated with increased mortality, worsened seizures, poor cognition, medication side effects, and increased healthcare utilization[4–8]. Despite this importance, anxiety and depression are under-recognized and undertreated in epilepsy, and barriers to care identified by epileptologists include poor access to mental health specialists[9–11]. Recent publications and quality improvement efforts, including the 2017 American Academy of Neurology Epilepsy Quality Measurement Set, support neurologist prescribing and screening for anxiety and depression in epilepsy clinics[12–14].
A 2016 survey of epileptologists demonstrated prescribing and psychiatry referral were the most common management approaches for anxiety and depression[11]. The epileptologists indicated slight preference for prescribing over psychiatry referral to manage depression (56% vs. 52%), while psychiatry referral was preferred over direct prescribing for anxiety (61% vs. 34%)[11]. In contrast, management preferences among people with epilepsy are largely unknown, despite general mental health research suggesting patient-preference based treatment enhances outcomes[15, 16]. Behavioral health treatment preference literature in epilepsy has examined unaffected individuals, or specifically self-management or positive psychological interventions[17–19]. Studies have not addressed preferences among individuals with active symptoms of anxiety and/or depression, nor have they compared the two most common neurology-initiated management approaches (medication prescribing, psychiatry referral). To optimize care and assess whether neurologist clinical practice habits should change, it is important to understand management preferences among symptomatic epilepsy clinic patients, and whether they differ from provider preferences.
Hence, we sought to compare preference for neurologist-prescribed medication versus psychiatry referral in an epilepsy clinic-based sample of adults who screened positive for anxiety and/or depression symptoms. Secondary objectives were to assess an a priori multivariable model of treatment preference, explore preferences for additional management options, and characterize past and current psychiatric treatments in the sample.
2. METHODS
2.1. Study overview and design
This was a prospective, cross-sectional survey of adults in a tertiary care epilepsy clinic, conducted in tandem to screening/enrollment in a learning health system pilot randomized treatment trial for anxiety and depression symptoms. The study was conducted from January to September 2019 in the practices of two adult-focused epileptologists and an epilepsy specialty physician assistant (PA) at a U.S. tertiary epilepsy center. As a combined clinical care and research screening method, patients presenting for visits completed anxiety and depression instruments after clinic check-in. Instruments were completed on a tablet in physician clinics and on paper in the PA specialty clinic. If anxiety or depression scores indicated a positive screen (defined below), a brief research screening consent was triggered on the tablet in physician clinics, followed by additional clinical questions for simultaneous clinical care and potential trial screening[20]. In the physician assistant specialty clinic, positive anxiety or depression screen was followed, among interested individuals, by the same tablet-based research screening.
Individuals who were ineligible for or declined the parent treatment study were offered cross-sectional survey participation. This study was approved by the institutional review board, with electronic informed consent for survey participation obtained from all participants. This survey was an ancillary study to the parent pragmatic treatment trial (NCT03464383). Data statement: anonymized data will be shared by request from any qualified investigator. Also, requests by qualified investigators for sharing study protocol or related documents will be considered via email inquiry to the corresponding author.
2.2. Survey study sample/setting and clinical context
Inclusion criteria for this survey were: age ≥18, positive screen for anxiety or depression (Generalized Anxiety Disorder-7, GAD-7 score≥10 or Neurological Disorders Depression Inventory-Epilepsy, NDDI-E score≥16)[21, 22], and either: 1) ineligible for treatment study (Supplementary Appendix S1) or 2) declined participation in treatment study. Eligibility for the parent treatment study, recruitment from physician or PA clinic, and reasons for treatment study ineligibility were collected to assess for confounding/bias. All participants were screened for eligibility, consented, and completed the study survey on a tablet via REDCap (Research Electronic Data Capture) immediately before or after a routine epilepsy clinic visit[23].
The study setting is a tertiary care epilepsy clinic in the southern Appalachian region of the United States, serving a multistate area. Outpatient behavioral health and psychiatry services of the parent institution are housed in a separate, local site from the epilepsy center clinic. An epilepsy monitoring unit-based social worker is utilized at times by epilepsy providers at the center to facilitate psychiatry/behavioral health referrals and for limited piloting of the UPLIFT self-management program[24]. The department of neurology also has an integrative medicine psychologist who offers relaxation training consultations. Antidepressant prescribing is routinely conducted by the epilepsy providers from whose clinics the study sample was recruited.
2.3. Measurements
Anxiety and depression screening was completed using freely available instruments validated in epilepsy: the GAD-7 and NDDI-E, with positive screen values ≥10 and ≥16, respectively, based on original validation literature for these instruments[14, 21, 22, 25]. The survey was composed of 10 treatment preference questions, 9 multipart psychiatric diagnosis and treatment history questions, demographics/social status questions, and a brief medication adherence scale for those who reported current medication treatment for anxiety and/or depression[26]. Demographic and social status variables included: age, sex, race, ethnicity, marital status, education level, employment status, and type of health insurance as a proxy for socioeconomic status. National Institute of Neurological Disorders and Stroke common data elements for epilepsy were used when possible. The following aspects of current and past psychiatric treatment were ascertained by participant report: prior and current treatment modalities (including type of physician/prescriber for medications), prior personal psychiatric diagnoses, family history of psychiatric diagnoses, past psychiatric hospitalizations, and current and past psychotropic medications. Specific psychotropic medication information collected included: number of medications tried, current and past use of individual antidepressants, anxiolytics, and atypical antipsychotics, along with prior use of mood stabilizers (if solely for mood indication). Other psychiatric symptoms were also collected: current auditory hallucinations of voices and history of manic episode (Mini-International Neuropsychiatric Interview for Diagnostic and Statistical Manual of Mental Disorders-IV, MINI-IV past manic episode module)[27]. Epilepsy diagnosis, type, and 6-month seizure freedom was determined by chart abstraction. Individuals were considered to have a diagnosis of epilepsy if there were epileptiform discharges or seizure(s) recorded on EEG, or if epilepsy was the leading clinical diagnosis documented by the managing epilepsy specialist. Epilepsy type was coded as generalized, focal, or unknown by 2017 International League Against Epilepsy Classification, using EEG findings or clinician impression and semiology description (if EEG unavailable or without epileptiform abnormalities)[28].
2.4. Treatment preferences
At the start of the survey, a personalized popup box informed participants of their screening results: “You screened positive for Anxiety” “… Depression” or “… Anxiety and Depression.” Participants were then prompted to answer treatment preference questions specifically for these symptom type(s) with positive screen(s) (based on GAD-7 and NDDI-E scores). Questions included an overall treatment priority question with a 5-point response scale, a specific choice question to assess the primary and secondary endpoints, and a series of questions to rate each of various treatment options on a 5-point Likert scale. The specific choice question prompted participants to select one preferred choice among 3 options: psychiatry referral, neurologist-prescribed medication, or neither. The primary outcome was the ratio of participants indicating preference for “medication prescribed or adjusted by your neurologist” to those indicating preference for a “referral to see a psychiatrist.” Among those who chose psychiatry referral or neurologist-prescribed medication, strength of preference was ascertained using a 5-point scale ranging from “no preference” to “strong preference.” Treatment options examined in the subsequent series of Likert scale questions were: prescribing by neurologist, prescribing by primary care provider, prescribing by psychiatrist, counseling/psychotherapy, wellness activities, complementary/alternative treatments, and no treatment (scale and response wording shown in Figure 3).
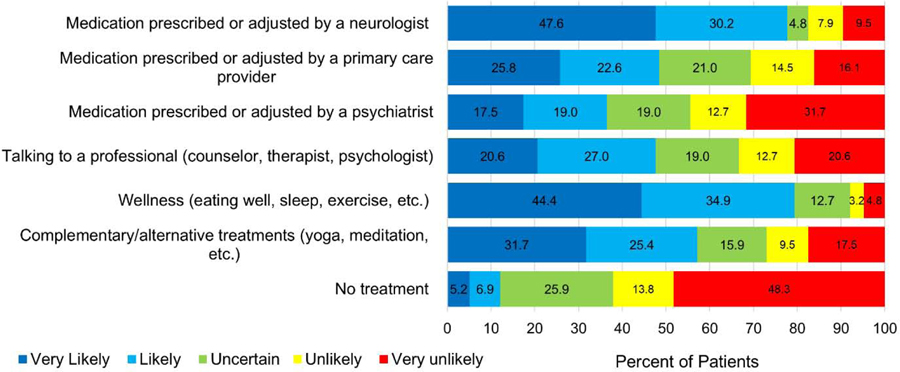
Figure 3.
Patient preferences for various treatment modalities
Figure shows treatment preference by modality. Bars indicate how likely participants reported they would be to choose the various treatment modalities.
2.5. Statistical analysis and data management
Study data were collected and managed using Research Electronic Data Capture (REDCap)[23]. Statistical analyses were conducted using SAS 9.4. We examined the distribution of data prior to additional analyses. To assess the primary objective, a one-sample binomial test with alpha=0.05 (two-sided) was conducted, comparing the proportion selecting neurologist-prescribed medication with that selecting psychiatry referral on the specific choice treatment preference question. Our null hypothesis was that there was no difference in these proportions. With target sample size of 50 individuals selecting either neurologist prescription or psychiatry referral, this study had ≥80% power to detect a difference under the alternative proportions of 0.70 or greater for either treatment preference (i.e., slightly greater than 2:1 preference ratio in favor of one of the treatments). The actual sample was 53 individuals selecting either treatment.
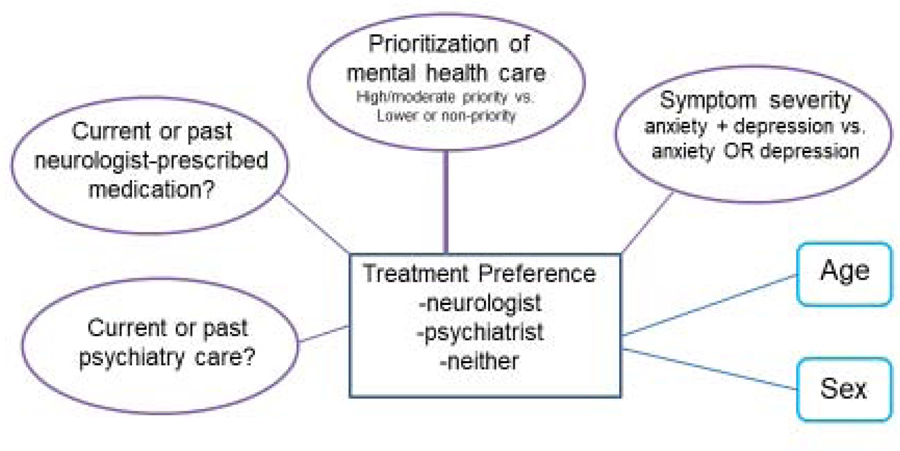
To assess the secondary objective, we used multinomial logistic regression modeling to assess the conceptual model of treatment preference depicted in Figure 1. For multivariable modeling, all 3 possible selections for the treatment preference dependent variable were included (neurologist-prescribing, psychiatry referral, neither). Neurologist prescribing was the referent group. Explanatory variables included in the modeling were selected a priori based on general population treatment preference literature and potential treatment planning relevance in a conceptual model of preference-based care for anxiety and depression symptoms in epilepsy (Figure 1)[15, 16]. We were not able to include race in the multivariable model due to insufficient variability in our study sample. For multivariable modeling, current/past neurologist-prescribed medication and current/past psychiatry care (yes/no), treatment prioritization (high/moderate priority versus lower priority/not a priority/unsure), symptom severity (screen positive for BOTH anxiety and depression versus either anxiety OR depression), sex and age (continuous) were included. Modeling with ≤6 independent variables was considered appropriate for the overall sample size of 63. P values of ≤0.05 were considered statistically significant. There was no missing data for factors included in the multivariable modeling.
Figure 1.
Conceptual model of factors potentially associated with treatment preference
3. RESULTS
3.1. Recruitment and participant characteristics
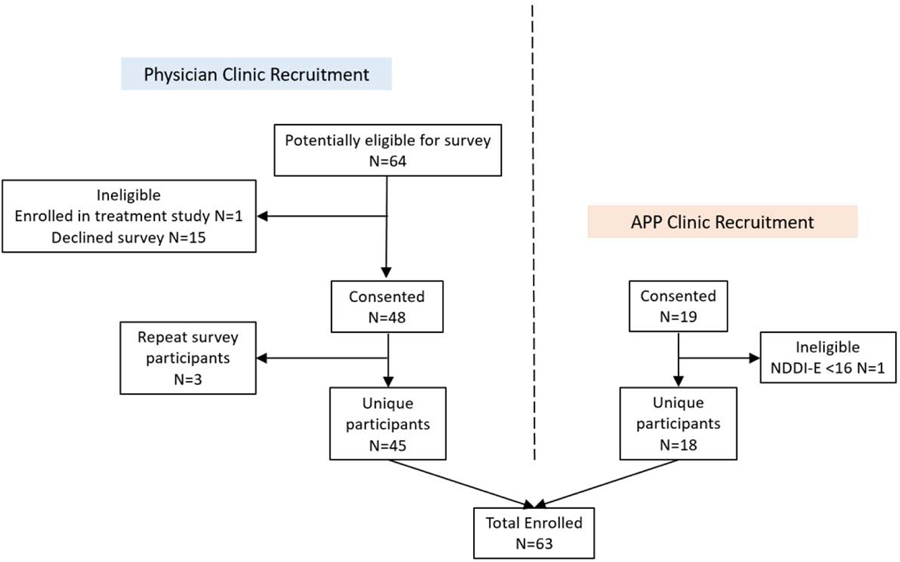
A total of N=63 unique adults were included in this analysis (Figure 2). Table 1 demonstrates demographic and epilepsy characteristics of the sample, which included mostly women. Ages ranged 19–67 years, and 9 of the 11 non-Caucasians were Black/African American, with one Asian and one American Indian/Alaska Native. Among those with education beyond high school, 17 (27%) had some college, 9 (14.3%) earned associates or bachelor degrees, and 7 (11.1%) had at least some graduate or professional school. The demographic and clinical factors in Table 1 did not differ by preference group (neurologist prescribing, psychiatry referral, neither).
Figure 2.
Enrollment flow diagram
Flow diagram details numbers of participants enrolled from each recruitment pathway (physician clinics vs. APP clinics), and reasons for exclusion.
Table 1.
Sample demographics, social and epilepsy characteristics
| N=63 unless otherwise noted below | N (%) |
|---|---|
| Age (yr.) (mean ± SD) | 42.2 ± 13.5 |
| Female | 40 (63.5%) |
| Race | |
| Black/African American, American Indian or Alaska Native, Asian | 11 (17.4%) |
| White or Caucasian | 48 (76.2%) |
| Unknown/ prefer not to answer | 4 (6.3%) |
| Ethnicity | |
| Hispanic or Latino | 4 (6.3%) |
| Not Hispanic or Latino | 47 (74.6%) |
| Prefer not to answer/unknown | 12 (19.0%) |
| Marital status | |
| Single | 29 (46.0%) |
| Married or domestic partner | 26 (41.3%) |
| Divorced/separated/widowed | 8 (12.7%) |
| Employment status | |
| Employed | 16 (25.4%) |
| Unemployed | 9 (14.3%) |
| Disabled | 33 (52.4%) |
| Retired or other | 5 (7.9%) |
| Education | |
| High school/GED or less | 30 (47.6%) |
| Some college or post-secondary degree | 33 (52.4%) |
| Primary health insurance | |
| Private/commercial | 20 (31.7%) |
| Medicaid | 19 (30.2%) |
| Medicare | 15 (23.8%) |
| None or other | 9 (14.3%) |
| Leading diagnosis of epilepsyb | 57 (90.5%) |
| Epilepsy type (N=57) | |
| Focal | 35 (61.4%) |
| Generalized | 18 (31.6%) |
| Unknown | 4 (7.0%) |
| Seizure free 6 months – epileptic seizures (N=57) | 19 (33.3%) |
One individual did NOT have a diagnosis of epilepsy. For five others, it was uncertain whether epilepsy or another condition was the primary diagnosis.
3.2. Psychiatric characteristics
The mean NDDI-E score was 15.4 (SD 3.0, range 8–22), while the mean GAD-7 score was 12.3 (SD 3.8, range 4–21). Nearly half of participants screened positive for depression alone (N=29; 46%), 31.8% (N=20) screened positive for depression and anxiety, and 22.2% (N=14) screened positive for anxiety alone. Two-thirds (42/62, 67.7%) self-reported a prior Diagnostic and Statistical Manual of Mental Disorder (DSM) Axis 1 diagnosis, including 20 individuals (32.3%) reporting Major Depressive Disorder with or without other diagnoses and 31 individuals (50%) reporting anxiety (Generalized Anxiety Disorder, Panic Disorder, or Social Phobia). More than half of participants indicated family history of an Axis 1 DSM disorder (33/61; 54.1%). Table 2 outlines current and past psychiatric treatments used by participants, demonstrating extensive treatment with various modalities. Among those with a past psychiatric hospitalization, nearly half reported more than one hospitalization (42%; N=8/19). While over 20% had tried 5 or more psychotropic medications (N=13, 20.6%), one quarter had never tried an antidepressant (22.6%, N=14/62). Of the 42 individuals taking a current psychotropic medication who completed a Morisky medication adherence scale [26] focused on psychotropic medication, most indicated high adherence (no response to all four questions; N=27; 64%). Table 2 shows adherence questions and response frequencies for each individual question. Thirteen individuals had moderate adherence (31.0%; yes to one or two questions), and only two individuals had low adherence (4.8%, both with yes to three of four questions; none responded yes to all four questions).
Table 2.
Current and past psychiatric treatment in the sample
| Treatment Modality/Agent (N=63 unless otherwise noted) | Current N (%) | Past N (%) |
|---|---|---|
| Psychiatrist visits | 10 (15.9%) | 31 (49.2%) |
| Counseling/psychotherapy | 10 (15.9%) | 33 (52.4%) |
| Medication prescribed by primary care physician (PCP) | 23 (36.5%) | 23 (36.5%) |
| Medication prescribed by neurologist | 35 (55.6%) | 11 (17.5%) |
| Medication prescribed by other physician specialty | 10 (15.9%) | 14 (22.2%) |
| Treatment by a nurse practitioner or physician assistant | 7 (11.1%) | 14 (22.2%) |
| Complementary/alternative therapies (eg. yoga, relaxation) | 10 (15.9%) | 18 (28.6%) |
| Other treatmentsa | 3 (4.8%) | 7 (11.1%) |
| Psychiatric hospitalization | N/A | 19 (30.2%) |
| Psychotropic medications overall | 44 (69.8%) | 55 (87.3%) |
| Antidepressants | 36 (57.1%) | 48/62 (77.4%) |
| sertraline | 7 (11.1%) | 19/62 (30.6%) |
| escitalopram | 11 (17.5%) | 16/62 (25.8%) |
| citalopram | 5 (7.9%) | 12/62 (19.4%) |
| fluoxetine | 4 (6.3%) | 20/62 (32.3%) |
| Other anxiolytics for anxiety symptoms | 21 (33.3%) | 27 (42.9%) |
| alprazolam | 3 (4.8%) | 15 (23.8%) |
| clonazepam | 10 (15.9%) | 16 (25.4%) |
| lorazepam | 4 (6.3%) | 9 (14.3%) |
| hydroxyzine | 4 (6.3%) | 5 (7.9%) |
| Atypical antipsychotics | 9 (14.3%) | 11 (17.5%) |
| Lithium | 0 (0.0%) | 2 (3.2%) |
| Mood stabilizing antiseizure medication solely for mood | N/A | 17/ 61 (27.9%) |
| Psychotropic medication adherence (Morisky Scale) N=42 | N/A | |
| forget to take it | 13/ 42 (31.0%) | |
| careless about taking it | 5/ 42 (11.9%) | |
| stop it when feeling better | 3/ 42 (7.1%) | |
| stop it if feel worse when taking it | 2/ 42 (4.8%) |
other treatments reported by participants included: work and soccer, though most who reported “other” treatment type did not respond to the question about the specific type of other treatment.
3.3. Treatment priority and preferences: various modalities
The vast majority of participants rated treatment of anxiety and/or depression symptoms a priority (84.1%, N=53), with 65.1% indicating high or moderate priority (39.7% and 25.4%, N=25 and 16, respectively). Figure 3 shows preferences across various treatment modalities. Overall, wellness (eating well, sleep, exercise…) and neurologist-prescribed medication were most preferred (79.3% and 77.8% likely or very likely to choose these, respectively). Least preferred modalities were medication prescribed by a psychiatrist and no treatment (36.5% and 12.1% likely or very likely respectively). Complementary/alternative therapies, medication prescribed by a primary care physician and counseling/therapy were slightly more preferred than medication prescribed by a psychiatrist (47.6% to 57.1% likely or very likely to choose for these modalities; Figure 3).
3.4. Primary Outcome: Preference for neurologist prescribing versus psychiatry referral
When prompted to select between neurologist prescribing and psychiatry referral, participants indicated a nearly 5:1 ratio of preference for neurologist prescribing over psychiatry referral (N=44 vs. 9) This was statistically significant on the two-sample binomial test (Z=4.8076, p<0.001, 95% Confidence Interval(CI) 0.702–0.919; proportion selecting neurologist prescribing among those indicating either neurologist prescribing or psychiatry referral). These 53 individuals who selected neurologist prescribing or psychiatry referral reported clear preference for the modality selected, with 75.5% (N=40) indicating moderate, somewhat strong, or strong preference for their selection. There was no significant difference in strength of preference indicated between those who chose psychiatry referral or neurologist management (p=0.94, Fisher’s exact test). Figure 4 demonstrates treatment preference in the entire sample, including selection of neither neurologist prescribing nor psychiatry referral.
Figure 4.
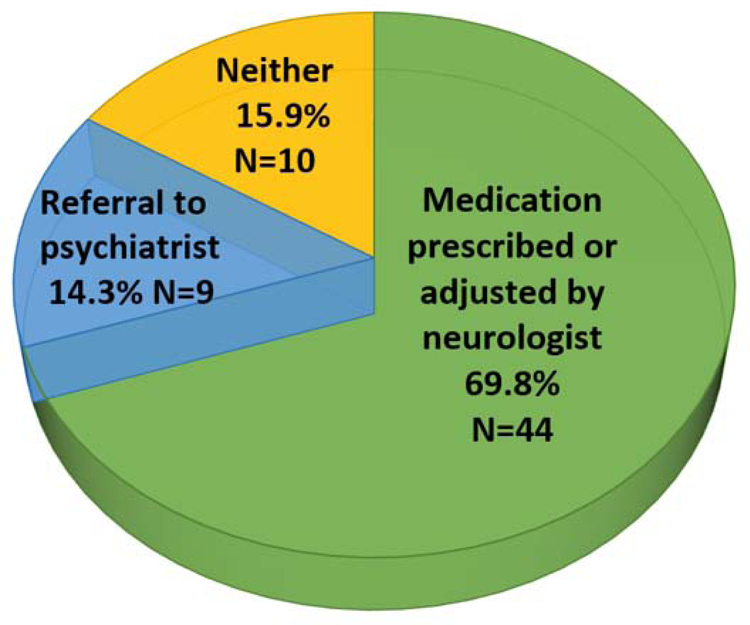
Preferred treatment modalities for anxiety and/or depression based on a specific choice question
Sections represent the proportion of total study sample selecting neurologist prescribing, psychiatry referral, or neither of these two options, when prompted to select one of these three options.
3.5. Psychiatric characteristics, treatment history and preference for other modalities by primary outcome preference group
Table 3 demonstrates psychiatric characteristics and treatment history among the 3 preference groups: neurology prescribing, psychiatry referral, and neither. Many characteristics were similar across the 3 groups. In both those preferring psychiatry referral and those preferring neurologist prescribing, approximately half had received psychiatric care in the past, and fewer still were receiving current psychiatric care. Participants who preferred neither neurologist prescribing nor psychiatry referral were prompted to indicate the reason for this selection. Half (5 of 10) indicated ongoing care of some type (2 from primary care, 1 from psychiatry, 1 therapist, 1 “doctors”). The others provided no response (3), indicated a referral was in process (1), and indicated “I can handle it myself” (1). Among these individuals who selected neither treatment on the specific choice question, for most treatment modalities listed in figure 3, the most common response was very unlikely (except counseling/therapy and complementary/alternative therapy, with most common response being likely). Among those who chose referral to a psychiatrist on the specific choice question, 66% indicated they were likely or very likely to consider medication prescribed by a neurologist, whereas only 32% of those who chose medication prescribed by a neurologist indicated they were likely or very likely to choose medication prescribed by a psychiatrist. Most who preferred psychiatry referral were likely or very likely to choose counseling/therapy (78%), compared to 39% who preferred neurology prescribing. The psychiatry referral and neurology prescribing groups were similarly likely or very likely to choose medication prescribed by primary care (55% and 51% respectively).
Table 3:
Psychiatric characteristics and treatments by preference groupa
| N (%) unless otherwise indicated below | Overall (N=63) | Neurology Prescribing (N=44) | Psychiatry Referral (N=9) | Neither (N=10) | Pd |
|---|---|---|---|---|---|
| NDDI-E score; mean ± SD | 15.4 ± 3.0 | 15.7 ± 3.2 | 15.0 ± 2.6 | 14.5 ± 2.5 | 0.49 |
| GAD-7 score; mean ± SD | 12.3 ± 3.8 | 12.1 ± 3.8 | 12.7 ± 3.6 | 12.8 ± 4.2 | 0.85 |
| Past manic episode (MINI module) | 0.021 | ||||
| Yes | 12 (19) | 6 (14) | 2 (22) | 4 (40) | |
| No | 50 (79) | 37 (84) | 7 (78) | 6 (60) | |
| Unknown/incomplete | 1 (2) | 1 (2) | 0 | 0 | |
| Auditory hallucinations (voices) (N=62, 43, 9, 10)b | 11 (18) | 7 (16) | 2 (22) | 2 (20) | 0.10 |
| Positive passive suicidality screenc | 4 (6) | 3 (7) | 0 | 1 (10) | 0.22 |
| Past psychiatric hospitalization | 19 (30) | 13 (30) | 3 (33) | 3 (30) | 0.085 |
| Psychiatry care: past | 31 (49) | 23 (52) | 5 (56) | 3 (30) | 0.033 |
| Psychiatry care: current | 10 (16) | 5 (11) | 3 (33) | 2 (20) | 0.032 |
| Counseling/Therapy: past | 33 (52) | 23 (52) | 4 (44) | 6 (60) | 0.062 |
| Counseling/Therapy: current | 10 (16) | 7 (16) | 2 (22) | 1 (10) | 0.11 |
| Neurology prescribed med: past | 11 (17) | 9 (20) | 2 (22) | 0 | 0.041 |
| Neurology prescribed med: current | 35 (56) | 26 (59) | 5 (56) | 4 (40) | 0.043 |
| Primary care prescribed med: past | 23 (37) | 17 (39) | 3 (33) | 3 (30) | 0.074 |
| Primary care prescribed med: current | 23 (37) | 14 (32) | 4 (44) | 5 (50) | 0.039 |
| Complementary/alternative therapy: past | 18 (29) | 13 (30) | 4 (44) | 1 (10) | 0.025 |
| Complementary/alternative therapy: current | 10 (16) | 6 (14) | 2 (22) | 2 (20) | 0.090 |
| Psychotropic medication: current | 42 (67) | 32 (73) | 4 (44) | 6 (60) | 0.020 |
| Number of prior psychotropic medications (N=61, 43, 8, 10)b | 0.0078e | ||||
| 0 | 13 (21) | 6 (14) | 4 (50) | 3 (30) | |
| 1 | 15 (25) | 14 (33) | 0 | 1 (10) | |
| 2 | 9 (15) | 7 (16) | 1 (13) | 1 (10) | |
| 3 | 7 (11) | 4 (9) | 2 (25) | 1 (10) | |
| 4 | 4 (7) | 3 (7) | 0 | 1 (10) | |
| 5+ | 13 (21) | 9 (21) | 1 (13) | 3 (30) | |
| Morisky score (N=42, 32, 4, 6)b | 0.023 | ||||
| 0, good adherence) | 27 (64) | 23 (72) | 1 (25) | 3 (50) | |
| 1+, moderate to low) | 15 (36) | 9 (28) | 3 (75) | 3 (50) |
All results are based on N=63 subjects in total, unless otherwise indicated above.
(N order: overall, neurology prescribing, psychiatry referral, neither)
Score of “sometimes” or “always” on item 4 of the NDDI-E [44]
Overall p value for association between preference and psychiatric or treatment characteristic were calculated by Fisher exact test (discrete characteristics) or analysis of variance (continuous characteristics);
number of prior psychotropic medications were categorized as none (0) versus any (1+).
3.6. Multivariable analyses
Table 4 shows results of multinomial logistic regression modeling using the conceptual model from Figure 1. Compared to those who preferred neurologist prescribing, participants with lower prioritization of symptom treatment had nearly 12-fold greater odds of selecting neither treatment, while those with no past or current prescribing by a neurologist had 9-fold greater odds of selecting neither treatment. These odds ratios were somewhat higher in multivariable modeling than unadjusted models (unadjusted odds 6.2, p=0.017, CI 1.4–28.1 for lower priority; 5.1, p=0.028, CI 1.2–21.7 for no prescribing by neurologist). Other factors examined were not associated with treatment preference. Further, no factors were significantly associated with choosing psychiatry referral over neurologist prescribed medication, though a potential trend toward men preferring psychiatry over neurologist treatment was observed (Table 4; unadjusted odds 4.3, p=0.061, CI 0.93–19.7).
Table 4.
Association of pre-specified multivariable model with treatment preference: multinomial logistic regression modeling
| Psychiatry referral preferred vs. neurologist | Neither option preferred vs. neurologist | |||||
|---|---|---|---|---|---|---|
| Factor | Odds ratio | 95% Confidence Interval | p | Odds ratio | 95% Confidence Interval | p |
| Depression & anxiety (vs. anxiety or depression alone) | 0.53 | 0.085–3.3 | 0.50 | 1.4 | 0.20–9.8 | 0.74 |
| Age (per 10 years) | 0.96 | 0.55–1.7 | 0.87 | 0.86 | 0.44–1.7 | 0.65 |
| Gender (male) | 4.6 | 0.90–23.2 | 0.068 | 0.78 | 0.13–4.7 | 0.79 |
| Treatment priority: low vs. high | 1.9 | 0.34–10.6 | 0.46 | 11.9 | 1.5–91.7 | 0.018 |
| No current or past medication treatment by neurologist | 3.2 | 0.47–22.4 | 0.24 | 9.3 | 1.4–64.4 | 0.023 |
| No current or past psychiatry treatment | 0.21 | 0.022–2.0 | 0.17 | 0.26 | 0.031–2.2 | 0.22 |
3.7. Assessment for confounding by recruitment characteristics
There was no association between preference for psychiatry referral, neurologist medication treatment, or neither and MD versus PA recruitment clinic (p=0.76, Fisher’s exact test). Similarly, there was no association between treatment preference and reason for recruitment (ineligible vs. declined treatment study, p=0.88; opted in vs. opted out of screening for treatment study in MD clinics, p=0.57; Fisher’s exact test). Only one individual was ineligible for survey participation due to treatment study enrollment.
4. DISCUSSION
4.1. Treatment preferences observed
In this survey of mental health treatment preferences among a symptomatic adult epilepsy clinic sample, most patients preferred neurologist prescribing for anxiety and/or depression symptoms over psychiatry referral, with nearly 5:1 ratio of preference for neurologist prescribing versus psychiatry referral. The majority of participants indicated strong preference in favor of their selected option. This result contrasts with survey data on epileptologists’ treatment practice indicating relative equipoise among these options, in which neurologist prescribing and psychiatry referral were the most preferred treatment choices for anxiety and depression, with psychiatry preferred over prescribing for anxiety[11]. In this patient preference study, not only was neurologist prescribing preferred over psychiatry referral when participants were prompted to select between the two options, but neurologist prescribing was one of the most preferred options overall (only wellness slightly more preferred), while psychiatry prescribing was the least preferred (besides no treatment; Figure 3). The study sample had extensive experience with multiple treatment modalities for anxiety and/or depression overall, though multivariable analyses demonstrated no independent association of preference for psychiatry referral vs. neurologist prescribing with past or current psychiatry care or neurologist prescribing. In contrast to most of the study sample, the subset of individuals (15.9%) who selected neither neurologist prescribing nor psychiatry referral when prompted to select among these specific options may represent a distinct group, requiring a different clinical approach. Selection of neither option was associated with nearly 10-fold greater odds of having never been prescribed medication for anxiety or depression by a neurologist and with low treatment prioritization for anxiety and/or depression symptoms. This group may include those for whom anxiety or depression symptoms are less impactful, overall mental health treatment refusers, and potentially some individuals with false positive symptom screens. It is also worth note that some individuals did prefer psychiatry referral over neurologist prescribing, and with strong preference (similar to strong preference reported by many of those who preferred neurology prescribing). These findings suggest the need for an individualized approach/shared decision-making in management.
4.2. Potential contributors to treatment preference
While we did not find an association of past or current psychiatry referral or neurologist prescribing with patient preference for neurologist prescribing versus psychiatry referral, other factors may potentially contribute to the observed preferences. Poor access to mental health care may partially explain low patient preference for psychiatry referral and counseling/psychotherapy. Top barriers to screening for anxiety and depression identified by epileptologists included lack of psychiatrists and other mental health providers and insurance barriers to mental health access[11]. There are substantial mental health specialist shortages, a shrinking psychiatry workforce relative to neurologists in the United States, and markedly unequal geographic distribution of psychiatrists in the US compared with other specialties[29, 30]. This shortage contributes to long wait times. Given a prior study indicating epilepsy patients valued speed of treatment more than modality for managing depression[17], delays to psychiatry access may have influenced the preference results in our analysis. Mental health related stigma could also contribute to lower preference for psychiatry referral; though we did not examine this possibility, concern about a potential mental health label was the main barrier to completing behavioral health referrals for anxiety and depression in a childhood epilepsy study[31]. Future research on the influence of mental health stigma on adult treatment preferences would be beneficial. Similarly, any general delays to access treatment by a non-neurologist provider (e.g., a primary care provider or alternative medicine practitioner) may have contributed to lower preference for these options. Given the extensive prior treatment history many of the participants reported for anxiety and depression symptoms, perhaps some found neurologist prescribing particularly appealing to simplify overall medical care following prior psychiatric consultation or other behavioral health care. Some individuals may prefer simplified medical care overall, such as seeing a primary care provider for all care rather than specialists including neurologists and or psychiatrists. Satisfaction with prior mental health treatment may have also influenced preferences; this would be important to examine in future research. Ultimately, our study results do not answer questions related to the reasons for preferring neurologist prescription over psychiatry referral. This is an important area for potential future qualitative or mixed methods research to investigate why patients have the management preferences that they do.
The study setting being an epilepsy clinic may have influenced the findings in favor of neurologist prescribing, since a neurology provider was present at the visit in which the survey was conducted. Although this may limit generalizability of the findings, this study setting is clinically pertinent, as it reflects the setting in which neurologists are incentivized to screen for anxiety and depression at each visit via current quality metrics[12]. Also, the study sample reflects the patients and setting for which a neurologist would encounter a management decision for anxiety and/or depression symptoms. Previous studies of mental health treatment preferences in epilepsy have not examined an exclusively symptomatic population in detail, nor have they examined all of the most common treatment modalities reported in an American Epilepsy Society epileptologist practice survey, as was accomplished in this study[11, 17–19]. Compared with a prior primary care-based United Kingdom treatment preference survey, the present study sample of exclusively symptomatic patients were more likely to seek treatment for anxiety and/or depression and consider medication treatment options[17].
4.3. The treatment gap for anxiety and depression in epilepsy and opportunities to close it
The importance of action to better manage anxiety and depression symptoms for people with epilepsy is highlighted by data on epilepsy patient preferences and general population mental health literature linking preference-based care to better outcomes. Numerous studies demonstrate that anxiety and depression in epilepsy are under-recognized and under-treated[9, 10]. Barriers to mental health specialty access previously outlined undoubtedly contribute to these gaps, as do gaps in screening for anxiety and depression symptoms in neurology clinics[11, 12]. Another contributor to the treatment gap may be a discrepancy between epilepsy physician management preferences and the patient preferences identified in the present study. In addition to published studies examining preferences for mental health comorbidity treatment among people with epilepsy[17–19], a study of patient preferences for overall epilepsy/seizure management found access to mental health resources was a priority, with >80% of participants indicating psychological support should be more readily available[32]. Other investigations demonstrated epilepsy patients desire greater involvement in discussing and selecting treatment options, and patients consider the impact of psychiatric symptoms (specifically psychiatric side effects) as being more important than neurologists do[33–35]. Preference based care is associated with better psychotherapy outcomes and better satisfaction with care in the general mental health literature[15, 16]. Thus, incorporating patient preference-based care for anxiety and depression symptoms in epilepsy may better address patients’ needs and potentially improve outcomes.
In all, results of this survey and related literature may suggest that neurologists should consider incorporating prescribing for anxiety and depression symptoms into their practice, and that neurology clinic-based models of care merit further investigation. More than one survey demonstrated most epileptologists were willing to prescribe antidepressants and/or anxiolytics[11, 36]. Further, a recently published randomized trial demonstrated efficacy of sertraline for Major Depression in active epilepsy[37] and multiple publications outline practical strategies and evidence-based techniques for medication prescribing to manage symptoms of anxiety and depression in epilepsy[14, 38, 39]. Successful management of depression and other psychiatric symptoms by non-psychiatrists has been demonstrated using measurement-based care (antidepressant prescribing with repeated symptom monitoring using brief screening instruments) and collaborative care models (incorporating limited psychiatry input to optimize prescribing by non-psychiatrists)[40–42]. Additional education of neurologists on treatment of common psychiatric comorbidities and improved communication between neurology and psychiatry may facilitate care models for neurologist prescribing for anxiety and depression symptoms[43]. Further research is needed to explore collaborative care models, neurologist prescribing for anxiety and depression symptoms in real world care settings, and preference-based care for anxiety and depression symptoms in epilepsy.
In addition to direct neurologist prescribing for anxiety and depression symptoms in epilepsy, efforts to promote or incorporate other preferred management options which circumvent barriers to mental health care are worth considering. In addition to neurologist prescribing, the majority of participants were likely or very likely to choose two other management options: wellness activities and complementary/alternative therapies. These modalities also merit additional research, and consideration as options for neurologists to recommend in clinical practice.
4.4. Strengths and limitations
Strengths of this study include assessment of patient preferences among standard treatment modalities for anxiety and depression in a symptomatic clinic population, detailed review of current and past treatment modalities, and testing an a priori conceptual multivariable model of treatment preference. Limitations include sample size; although there was adequate power to assess the primary endpoint (ratio of treatment preference for neurologist prescribing versus psychiatry referral), complexity of the multivariable treatment preference modeling was slightly constrained by sample size, and statistical assessment for association of detailed aspects of past or current psychiatric care modalities with management preference was not possible. Although the study setting may have biased the results in favor of neurologist prescribing, a neurology/epilepsy clinic setting is the most relevant setting to assess because it reflects real clinical care circumstances for neurologists. The study was conducted at a single tertiary center among three epilepsy providers who routinely prescribe antidepressants, at a center where psychiatry outpatient clinics are distant from the main campus epilepsy clinic, and where intermittent social work support is available to facilitate some behavioral health referrals. This practice style and center resources may differ from other settings and may limit generalizability of the findings. Validated screeners were used to define anxiety and depression symptoms rather than a standard diagnostic interview; thus, these results pertain to anxiety and depression symptoms, not necessarily DSM diagnoses of an anxiety disorder or Major Depressive Disorder. However, due to the learning health system study design (study conduct embedded in routine care visits) we were unable to conduct diagnostic interviews such as the full Mini-International Neuropsychiatric Interview in the study sample. In routine practice in epilepsy clinics, there is insufficient time and expertise to conduct psychiatric diagnostic interviews, so the study sample represents individuals who would likely have symptoms detected in clinic settings, using validated instruments feasible for routine care.
5. Conclusions
In summary, this adult epilepsy clinic study of individuals with symptoms of anxiety and/or depression demonstrated strong prioritization of anxiety and depression treatment, with marked preference for neurologist prescribing rather than psychiatry referral. These results suggest neurologist action may be important to close the treatment gap for anxiety and depression symptoms in epilepsy. Models of neurologist prescribing for these symptoms should be studied and adopted in clinical practice, along with shared decision making/patient preference-based care models to potentially optimize outcomes.
Supplementary Material
Highlights.
65% of the sample rated treating anxiety or depression a high or moderate priority.
These symptomatic patients preferred neurology prescribing to psychiatry referral.
For anxiety or depression, patients preferred neurologist prescribing or wellness.
Overall, the least preferred management options were no treatment and psychiatry.
Past treatment was not associated psychiatry versus neurology treatment preference.
Acknowledgements:
We would like to acknowledge Deanna Oates (Wake Forest Baptist Health, Clinical and Translational Science Institute), Brittany Briceno (Wake Forest Baptist Health, Clinical and Translational Science Institute), Mingyu Wan (Wake Forest University, Neuroscience Graduate Program), Mysha Sissine, MSPH (Wake Forest School of Medicine, Department of Neurology), and Matthew Wong, MD (Wake Forest School of Medicine, Department of Neurology) for data collection, other technical assistance, and general support for the parent project.
Funding
Supported by the National Institutes of Health [grant numbers R25 NS088248; UL1 TR001420, U24 NS107197, 2KL2TR001421–05.] Dr. Duncan is supported by the following U.S. federal grants: U24 NS107197, PCS-11403–14531; RO1 HS025723–01. Funders had no role in study design, data collection, analysis, or interpretation. Funders also had no role in manuscript preparation or decision to submit for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest:
Dr. Conner has served as a paid consultant for SK Life Sciences.
Dr. Duncan has received support from the following entities: Moleac, Duke-NUS Singapore Medical School, Care Directions, Woods-Duncan, University of Kansas for SIS-impact license, University of Pittsburgh-PRIMA DSMB, Maine Medical Center Research Institute’s COBRE, CoHstar, and she serves as Chair of the NINDS Stroke Common Data Elements-Outcomes.
The remaining authors have no declarations of interest.
References
- [1].Scott AJ, Sharpe L, Hunt C, Gandy M. Anxiety and depressive disorders in people with epilepsy: A meta-analysis. Epilepsia 2017;58: 973–982. [DOI] [PubMed] [Google Scholar]
- [2].Kwan P, Yu E, Leung H, Leon T, Mychaskiw MA. Association of subjective anxiety, depression, and sleep disturbance with quality-of-life ratings in adults with epilepsy. Epilepsia 2009;50: 1059–66. [DOI] [PubMed] [Google Scholar]
- [3].Choi H, Hamberger MJ, Munger Clary H, Loeb R, Onchiri FM, Baker G, Hauser WA, Wong JB. Seizure frequency and patient-centered outcome assessment in epilepsy. Epilepsia 2014;55: 1205–12. [DOI] [PubMed] [Google Scholar]
- [4].Fazel S, Wolf A, Langstrom N, Newton CR, Lichtenstein P. Premature mortality in epilepsy and the role of psychiatric comorbidity: a total population study. Lancet 2013;382: 1646–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Petrovski S, Szoeke CE, Jones NC, Salzberg MR, Sheffield LJ, Huggins RM, O’Brien TJ. Neuropsychiatric symptomatology predicts seizure recurrence in newly treated patients. Neurology 2010;75: 1015–21. [DOI] [PubMed] [Google Scholar]
- [6].Au A, Leung P, Kwok A, Li P, Lui C, Chan J. Subjective memory and mood of Hong Kong Chinese adults with epilepsy. Epilepsy Behav 2006;9: 68–72. [DOI] [PubMed] [Google Scholar]
- [7].Kanner AM, Barry JJ, Gilliam F, Hermann B, Meador KJ. Depressive and anxiety disorders in epilepsy: do they differ in their potential to worsen common antiepileptic drug-related adverse events? Epilepsia 2012;53: 1104–8. [DOI] [PubMed] [Google Scholar]
- [8].Caller TA, Chen JJ, Harrington JJ, Bujarski KA, Jobst BC. Predictors for readmissions after video-EEG monitoring. Neurology 2014;83: 450–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Thompson AW, Kobau R, Park R, Grant D. Epilepsy care and mental health care for people with epilepsy: California Health Interview Survey, 2005. Prev Chronic Dis 2012;9: E60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Reid AY, Metcalfe A, Patten SB, Wiebe S, Macrodimitris S, Jette N. Epilepsy is associated with unmet health care needs compared to the general population despite higher health resource utilization--a Canadian population-based study. Epilepsia 2012;53: 291–300. [DOI] [PubMed] [Google Scholar]
- [11].Bermeo-Ovalle A Psychiatric Comorbidities in Epilepsy: We Learned to Recognize Them; It Is Time to Start Treating Them. Epilepsy Currents 2016;16: 270–272. [Google Scholar]
- [12].Patel AD, Baca C, Franklin G, Herman ST, Hughes I, Meunier L, Moura L, Munger Clary H, Parker-McFadden B, Pugh MJ, Schultz RJ, Spanaki MV, Bennett A, Josephson SA. Quality improvement in neurology: Epilepsy Quality Measurement Set 2017 update. Neurology 2018;91: 829–836. [DOI] [PubMed] [Google Scholar]
- [13].Kanner AM. Is it time to train neurologists in the management of mood and anxiety disorders? Epilepsy Behav 2014;34: 139–43. [DOI] [PubMed] [Google Scholar]
- [14].Munger Clary HM, Salpekar JA. Should adult neurologists play a role in the management of the most common psychiatric comorbidities? Practical considerations. Epilepsy Behav 2019;98: 309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Swift JK, Callahan JL, Cooper M, Parkin SR. The impact of accommodating client preference in psychotherapy: A meta-analysis. J Clin Psychol 2018;74: 1924–1937. [DOI] [PubMed] [Google Scholar]
- [16].Waltz TJ, Campbell DG, Kirchner JE, Lombardero A, Bolkan C, Zivin K, Lanto AB, Chaney EF, Rubenstein LV. Veterans with depression in primary care: provider preferences, matching, and care satisfaction. Fam Syst Health 2014;32: 367–77. [DOI] [PubMed] [Google Scholar]
- [17].Margrove KL, Thapar AK, Mensah SA, Kerr MP. Help-seeking and treatment preferences for depression in epilepsy. Epilepsy Behav 2011;22: 740–4. [DOI] [PubMed] [Google Scholar]
- [18].Fraser RT, Johnson EK, Miller JW, Temkin N, Barber J, Caylor L, Ciechanowski P, Chaytor N. Managing epilepsy well: self-management needs assessment. Epilepsy Behav 2011;20: 291–8. [DOI] [PubMed] [Google Scholar]
- [19].Lai ST, Lim KS, Tang V, Low WY. Positive psychological interventions for people with epilepsy: An assessment on factors related to intervention participation. Epilepsy Behav 2018;80: 90–97. [DOI] [PubMed] [Google Scholar]
- [20].Munger Clary HM, Croxton RD, Allan J, Lovato J, Brenes G, Snively BM, Wan M, Kimball J, Wong MH, O’Donovan CA, Conner K, Jones V, Duncan P. Who is willing to participate in research? A screening model for an anxiety and depression trial in the epilepsy clinic. Epilepsy Behav 2020;104: 106907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Gilliam FG, Barry JJ, Hermann BP, Meador KJ, Vahle V, Kanner AM. Rapid detection of major depression in epilepsy: a multicentre study. Lancet Neurol 2006;5: 399–405. [DOI] [PubMed] [Google Scholar]
- [22].Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166: 1092–7. [DOI] [PubMed] [Google Scholar]
- [23].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42: 377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Thompson NJ, Walker ER, Obolensky N, Winning A, Barmon C, Diiorio C, Compton MT. Distance delivery of mindfulness-based cognitive therapy for depression: project UPLIFT. Epilepsy Behav 2010;19: 247–54. [DOI] [PubMed] [Google Scholar]
- [25].Micoulaud-Franchi JA, Lagarde S, Barkate G, Dufournet B, Besancon C, Trebuchon-Da Fonseca A, Gavaret M, Bartolomei F, Bonini F, McGonigal A. Rapid detection of generalized anxiety disorder and major depression in epilepsy: Validation of the GAD-7 as a complementary tool to the NDDI-E in a French sample. Epilepsy Behav 2016;57: 211–216. [DOI] [PubMed] [Google Scholar]
- [26].Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986;24: 67–74. [DOI] [PubMed] [Google Scholar]
- [27].Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59 Suppl 20: 22–33;quiz 34–57. [PubMed] [Google Scholar]
- [28].Scheffer IE, Berkovic S, Capovilla G, Connolly MB, French J, Guilhoto L, Hirsch E, Jain S, Mathern GW, Moshe SL, Nordli DR, Perucca E, Tomson T, Wiebe S, Zhang YH, Zuberi SM. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia 2017;58: 512–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Gardner JS, Plaven BE, Yellowlees P, Shore JH. Remote Telepsychiatry Workforce: a Solution to Psychiatry’s Workforce Issues. Curr Psychiatry Rep 2020;22: 8. [DOI] [PubMed] [Google Scholar]
- [30].Bishop TF, Seirup JK, Pincus HA, Ross JS. Population Of US Practicing Psychiatrists Declined, 2003–13, Which May Help Explain Poor Access To Mental Health Care. Health Aff (Millwood) 2016;35: 1271–7. [DOI] [PubMed] [Google Scholar]
- [31].Wagner JL, Ferguson PL, Kellermann T, Smith G, Brooks B. Behavioral health referrals in pediatric epilepsy. Epilepsy Res 2016;127: 72–77. [DOI] [PubMed] [Google Scholar]
- [32].Ring A, Jacoby A, Baker G, Holmes E, Hughes D, Kierans C, Marson A. What really matters? A mixed methods study of treatment preferences and priorities among people with epilepsy in the UK. Epilepsy Behav 2019;95: 181–191. [DOI] [PubMed] [Google Scholar]
- [33].Bellon M, Pfeiffer W, Maurici V. Choice and control: how involved are people with epilepsy and their families in the management of their epilepsy? Results from an Australian survey in the disability sector. Epilepsy Behav 2014;37: 227–32. [DOI] [PubMed] [Google Scholar]
- [34].Ross J, Stefan H, Schauble B, Day R, Sander JW. European survey of the level of satisfaction of patients and physicians in the management of epilepsy in general practice. Epilepsy Behav 2010;19: 36–42. [DOI] [PubMed] [Google Scholar]
- [35].Ettinger AB, Carter JA, Rajagopalan K. Patient versus neurologist preferences: A discrete choice experiment for antiepileptic drug therapies. Epilepsy Behav 2018;80: 247–253. [DOI] [PubMed] [Google Scholar]
- [36].Mula M, Cavalheiro E, Guekht A, Kanner AM, Lee HW, Ozkara C, Thomson A, Wilson SJ. Educational needs of epileptologists regarding psychiatric comorbidities of the epilepsies: a descriptive quantitative survey. Epileptic Disord 2017;19: 178–185. [DOI] [PubMed] [Google Scholar]
- [37].Gilliam FG, Black KJ, Carter J, Freedland KE, Sheline YI, Tsai WY, Lustman PJ. A Trial of Sertraline or Cognitive Behavior Therapy for Depression in Epilepsy. Ann Neurol 2019;86: 552–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Mula M Treatment of anxiety disorders in epilepsy: an evidence-based approach. Epilepsia 2013;54 Suppl 1: 13–8. [DOI] [PubMed] [Google Scholar]
- [39].Kanner AM. The treatment of depressive disorders in epilepsy: what all neurologists should know. Epilepsia 2013;54 Suppl 1: 3–12. [DOI] [PubMed] [Google Scholar]
- [40].Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, Norquist G, Howland RH, Lebowitz B, McGrath PJ, Shores-Wilson K, Biggs MM, Balasubramani GK, Fava M, Team SDS. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry 2006;163: 28–40. [DOI] [PubMed] [Google Scholar]
- [41].Unutzer J, Katon W, Callahan CM, Williams JW Jr., Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EH, Arean PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C, Treatment IIIM-PAtC. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 2002;288: 2836–45. [DOI] [PubMed] [Google Scholar]
- [42].Huffman JC, Adams CN, Celano CM. Collaborative Care and Related Interventions in Patients With Heart Disease: An Update and New Directions. Psychosomatics 2018;59: 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Lopez MR, Schachter SC, Kanner AM. Psychiatric comorbidities go unrecognized in patients with epilepsy: “You see what you know”. Epilepsy Behav 2019;98: 302–305. [DOI] [PubMed] [Google Scholar]
- [44].Mula M, McGonigal A, Micoulaud-Franchi JA, May TW, Labudda K, Brandt C. Validation of rapid suicidality screening in epilepsy using the NDDIE. Epilepsia 2016;57: 949–55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.