Abstract
Gestational diabetes mellitus (GDM) complicates 6-8% of pregnancies and up to 50% of women with GDM progress to type 2 diabetes mellitus (DM) within 5 years postpartum. Clinicians have little guidance on which women are most at risk for DM progression or when evidence-based prevention strategies should be implemented in a woman’s lifecycle. To help address this gap, we review identifiable determinants of progression from GDM to DM across the perinatal period, considering pre-pregnancy, pregnancy, and postpartum periods. We categorize evidence by pathways of risk including genetic, metabolic and behavioral factors that influence progression to DM among women with GDM.
Keywords: gestational diabetes, diabetes mellitus, progression to diabetes postpartum
Introduction
Gestational diabetes mellitus (GDM) complicates 6-8% of pregnancies every year in the United States and its prevalence is rising.1,2 GDM is characterized by insulin-resistance and glucose intolerance first detected or diagnosed during pregnancy.3 Among those with GDM, up to 50% progress to Type 2 diabetes mellitus (DM) within 5 years, making GDM one of the strongest risk factors for DM.4–6 Women with GDM are also at an increased risk of chronic conditions such as cardiovascular disease, stroke, and liver disease.7–9
Early intervention among women with GDM has the potential to reduce the risk of progressing to DM, lowering the growing burden of DM in the United States and substantially reducing healthcare costs.5,10 For women in the reproductive years, preventing progression to DM also reduces the risk of pregnancy complications and adverse neonatal outcomes associated with DM in subsequent pregnancies.11 The American College of Obstetrics and Gynecology (ACOG) and the American Diabetes Association (ADA) recommends that women with GDM undergo glucose testing at 4-12 weeks postpartum and every 1-3 years thereafter.3,11 However, less than 50% of women return for postpartum follow-up raising the importance of identifying women at high risk of progression during pregnancy and the early postpartum period prior to delivery.12
For providers caring for women with GDM there is little guidance on when the strategies known to reduce DM risk should be implemented in the course of clinical care, especially as these strategies may be difficult to adhere to. To help address this gap, we review the evidence about progression from GDM to DM across the life course, including determinants during the pre-pregnancy, pregnancy, and postpartum periods. Throughout the review, we major pathways of risk including genetic, metabolic and behavioral factors that influence progression to DM among women with GDM.
Pre-pregnancy
Genetic
Family History of Diabetes
Familial history of DM has been shown to be a pathophysiologically unique risk factor for GDM as it encompasses both inherited and lifestyle components. Studies have identified family history of DM as a main risk factor for developing not just GDM but DM as well. The Nurse’s Health Study II showed that a family history of diabetes was associated with an increased risk of GDM (RR 1.68, 95% CI 1.39-2.04) after adjusting for confounders.13 Several smaller studies have found limited evidence of an association between family history and progression from GDM to DM, particularly when conducting multivariable analyses.14,15 A study looking at South African women who were followed for 5 years found that family history of diabetes was not a risk factor for progression from GDM to DM after controlling for confounders.16 However, a large meta-analysis of over 95,000 women with GDM found that a family history of diabetes conferred a RR of 1.70 (95% CI 1.47-1.97) for progression to DM.17 Overall, the data is not as clear on whether a family history of DM puts women with GDM at higher risk of developing DM.
Genetic Risk Scores
While family history of diabetes may not clearly be associated with increased risk of progressions from GDM to DM, some genotypes do seem to be at increased risk. Genetic risk scores, developed based on an array of genetic variants, and have shown promise to identify women with GDM at high risk of progressing to DM. Using genomic data, a genetic risk score developed from 36 single nuclear polymorphisms along with BMI and age, had an AUC of 0.68 to identify women who developed DM within up to 9 years in a small cohort of 119 Canadian women.18 A separate genetic risk score developed from 48 genetic variants among 395 South Korean women with GDM marginally improved prediction of DM (c-statistic 0.78, 95% CI 0.72-0.83) within 45 months of delivery, relative to clinical risk factors alone (c-statistic 0.74, 95% CI 0.69-0.80).19 In a large prospective cohort study of over 2400 Caucasian women from the Diabetes and Women’s Health Study (n=1884) and the Danish National Birth Cohort (n=550), women in the highest quartile of a genetic risk score developed from 59 genetic variants had an increased risk (RR 1.19, 95% CI 0.97-1.45) for DM within up to 21 years of GDM diagnosis, relative to women in the lowest quartile over. 20 The use of genetic risk scores may help to elucidate the biological basis for progression from GDM to DM and provide important clues for improved interventions.
Sociodemographic Characteristics
Among women with GDM, non-white ethnicity is a risk factor for progression to DM. Data on race/ethnicity and progression to DM among women with GDM is challenging to interpret, given that a majority of studies do not use self-identified race or ethnicity and race is a social, rather than genetic, construct. Consequently, race and ethnicity likely reflects a complex interplay of genetics, social, and structural barriers influencing disparities in progression to DM after GDM.21 In a large retrospective study of almost 13,000 women in Southern California that compared women without GDM to women with GDM, the risk of developing DM over 15 years was somewhat higher for Hispanic women (HR 7.7, 95% CI 5.2-8.0) and highest for Black women (HR 9.9, 95% CI 7.5-13.1) when compared to Caucasian women (HR 6.5, 95% CI 5.2, 8.0), after adjusting for other risk factors.22 A recent meta-analysis of women with GDM found that non-white ethnicity conferred a relative risk of developing DM of 1.49 (95% CI 1.14-1.94) even when adjusting for other confounders.23
Given the higher risk of progression to DM in non-white women, risk by specific ethnicity has been studied. A retrospective study in the UK demonstrated that 35% of Asian women with recent GDM had persistent glucose intolerance at 6-12 weeks postpartum consistent with DM, compared to only 7% of Caucasian women and 5% of women of Afro-Caribbean descent.24 Similar findings were observed in a study from Australia where 17% of South Asian women developed DM compared to 8.8% of Caucasians within 5 years of GDM diagnosis.25 Additionally, in a direct comparison of two studies, Ali et al found that only 3.4% of Swedish women with a history of GDM developed DM compared to 62% of women from Trinidad.26
Metabolic
Among women who develop GDM, both higher pre-pregnancy weight and BMI are associated with an increased risk of progression to abnormal glucose tolerance and DM postpartum. In a prospective cohort of 311 Korean women with GDM, a one-unit increase in pre-pregnancy weight independently predicted both impaired glucose tolerance and DM at 4-8 weeks postpartum.27 These findings were confirmed in a cohort of 788 women where pre-pregnancy obesity (defined as BMI >27 kg/m2) increased the likelihood of DM 3-6 months postpartum.28 However, data from a cohort of 170 women with recent GDM followed for four years did not find evidence that BMI>23 increased the risk of DM within 4 years postpartum.29 In a separate study with long-term follow-up, pre-pregnancy obesity was associated with 2.8 times the odds of DM at 5 years postpartum, compared to women with lower BMI in a cohort of 235 women with recent GDM.6
Pregnancy
Metabolic
Gestational weight gain & BMI
Both gestational weight gain and BMI during pregnancy have been evaluated as potential predictors of progression to DM in women with GDM. In a recent systematic review and meta-analysis, gestational weight gain was not identified as an independent risk factor for DM; however these findings were not stratified by pre-pregnancy BMI which influences gestational weight gain.17 However, weight gain through early postpartum in the highest tertile has been identified as a risk factor for impaired glucose tolerance at 1-6 months postpartum.30 Among women in the Diabetes & Women’s Health study, a prospective cohort of 1695 women from the Nurses’ Health Study who reported GDM during pregnancy and were followed up 8-18 years after the index pregnancy, a one unit increase in BMI at GDM diagnosis increased the risk of progression to DM by 16% (HR 1.16, 95% CI 1.12, 1.19).31 In a separate cohort of 300 women, BMI ≥ 30 in pregnancy doubled the risk of DM through 8 years postpartum (HR 2.2, 95% CI 1.5, 3.3).32
Insulin, glucose tolerance, HbA1c
Women with lower insulin sensitivity during pregnancy and who require insulin have also been noted to be at increased risk for progressing to DM postpartum.32 Higher levels of glucose intolerance, as indicated by fasting and 2- or 3-hour plasma glucose and glycated hemoglobin (HbA1c) typically measured in the first or second trimester of pregnancy, have also been identified as predictors of future DM risk. In a prospective study of 671 Latino women with GDM, in multivariable analyses area under the OGTT glucose curve during pregnancy, and the highest fasting serum glucose concentration during pregnancy predicted progression to DM within 5-7 years postpartum. 33 Among 316 non-Hispanic white women with GDM, a 1% increase in HbA1c at GDM diagnosis was associated with a 2-fold increase in odds of abnormal glucose tolerance at 6 weeks postpartum (OR 2.36, 95% CI 1.19–4.68).34 In a cohort of 306 Japanese women, in multivariable analyses HbA1c ≥5.6% (RR 4.67, 95% CI 1.53-16.73) and 2-hour plasma glucose ≥183 mg/dl (RR 7.02, 95% CI 2.51-20.72) at the time of GDM diagnosis were strongly associated with DM risk through approximately 1 year postpartum.35
Treatment
ACOG and the ADA recommend insulin to treat GDM when diet and exercise are not sufficient to manage glucose levels in pregnancy.3,11 In a recent systematic review and meta-analysis, women with GDM requiring insulin treatment during pregnancy were more than 3 times as likely to develop DM in the future, compared to women with GDM not requiring insulin treatment (RR 3.66, 95% CI 2.78-4.82).17 When insulin is not an option, limited data support use of metformin or glyburide, both oral antidiabetic medications, to treat GDM during pregnancy.36 Whether oral antidiabetic medications taken in pregnancy affect progression to DM postpartum is not known.3
Clinical
Parity
It has been suggested that recurrent pregnancies after a pregnancy complicated by GDM may increase the risk of progression to DM. However, studies evaluating this are often confounded by increasing maternal age. In a cohort of over 600 Latina women in the US with recent GDM, having an additional pregnancy after the index GDM pregnancy increased the risk of DM by over 3-fold (HR 3.34 95% CI 1.80, 6.19) in multivariable analyses.37 In a population-based cohort of 1400 nulliparous women in Canada with GDM, having a subsequent pregnancy with GDM doubled the risk of DM within 13 years of the index pregnancy (RR 2.3, 95% CI 1.6-3.4).38
Pregnancy complications
During pregnancy, hypertensive disorders in pregnancy and preterm birth are associated with an increased risk for developing DM in the future, compared to women who did not develop these conditions in pregnancy.39,40 The link between adverse pregnancy outcomes and future DM risk among women with GDM may, in part, be explained by the fact that both adverse pregnancy outcomes and DM are more common among obese women. However, there is evidence that women with pre-eclampsia or gestational hypertension and GDM are at higher risk of postpartum DM, relative to women with GDM alone.40
Postpartum
Behavioral
Exercise and Diet
The use of prophylactic metformin (discussed below) and lifestyle changes to prevent or delay the onset of DM in high risk groups was investigated in The Diabetes Prevention Program (DPP) Study. Women in the DPP with GDM were able to decrease their DM risk by 53% at 3 years and 35% at 10 years after randomization with a weight reduction goal of 7% of their baseline weight through ≥150 min per week of physical activity and a low-fat, low-calorie diet, relative to the placebo group.41,42
Not surprising, healthful behaviors, including diet and physical activity, confer protection against development of DM in women with GDM.43 A prospective study by Bao et al followed women in the Nurse’s Health Study II with a history of GDM and tracked their physical activity. Compared with women who maintained their total physical activity levels over 16 years, women who increased their total physical activity levels by 150 minutes per week of moderate-intensity physical activity had a 47% lower risk of DM (RR, 0.53; 95% CI, 0.38-0.75) even when adjusting for BMI.44 A meta-analysis of studies addressing lifestyle modifications in women with GDM to mitigate risk of progression to DM found that lifestyle changes started within 6 months after a pregnancy complicated by GDM produced a 39% (RR 0.61, 95% CI: 0.40-0.94) reduction in progression to DM at any point postpartum.45
Breastfeeding
Robust prospective data has shown that both intensity and duration of breastfeeding can markedly decrease risk of developing DM after diagnosis of GDM. The SWIFT study (Study of Women, Infant Feeding and Type 2 Diabetes After GDM Pregnancy) provided evidence that lactation conferred a 36% to 57% relative reduction in the risk of developing DM in the first two years after diagnosis of GDM. The protective effect of breastfeeding was stronger in women with higher intensity of lactation in the first two months after delivery and in those able to breastfeed for > 2 months.46 Other prospective studies that followed women with GDM found that breastfeeding was associated with a >40% long-term reduction of the risk of developing DM over 15 years (34.8%, 95% CI 18.3-41.3 among women who breastfed > 3 months vs 71.7%, 95% CI 60.3-83.1 among women who breastfed for < 3 months).47 A meta-analysis in 2017 that included 3408 women with GDM showed that lactation intensity for more than 4 to 12 weeks postpartum lowered DM risk over 5 years (OR 0.22, 95% CI 0.13-0.36).48 Only a retrospective analysis of women with a history of GDM from the Nurses’ Health Study cohort found no association between lifetime lactation and incidence of DM for years postpartum in women with GDM.49
Metabolic
Weight/BMI
Postpartum weight gain, independent of BMI before and during pregnancy, may be an important modifiable factor influencing progression to DM risk. The Diabetes and Women’s Health study reported that for each 5 kg of weight gain after GDM diagnosis, there was a 27% increased risk of DM (HR 1.27, 95% CI 1.04-1.54) over up to 18 years of follow-up, controlling for BMI at GDM diagnosis and other major diabetic risk factors. The risk of DM was even higher among women who were obese at GDM diagnosis and gained ≥ 5 kgs after GDM diagnosis, compared to women with a BMI <25 who gained <5 kgs after GDM.31
The deleterious effect of postpartum weight gain on DM risk was also found among women with GDM or impaired glucose tolerance in a cohort of 418 Korean women. Women in the highest tertile of weight change (mean increase of 1.6 kgs) within 4 years postpartum were twice as likely to develop DM, compared to women in the lowest tertile (mean loss of 1.8 kg), after controlling for initial postpartum BMI and age. Women in the highest tertile group also experienced greater deterioration in lipid profile and insulin sensitivity, after controlling for most recent postpartum BMI.50 Data from a small cohort of women with GDM the US (n=72) showed that, on average, women who maintained or gained weight between 6 and 12 weeks postpartum had larger increases in fasting and 2-hour plasma glucose during the same time frame, compared to women who lost weight postpartum.51
Postpartum glucose levels
Sustained levels of glucose intolerance in the postpartum period is a risk factor for early progression to DM.52 ACOG and the ADA recommend that women diagnosed with GDM during pregnancy receive a postpartum oral glucose tolerance test (OGTT) at 4-12 weeks postpartum and every 1-3 years thereafter to monitor progression to pre-DM and DM (Figure 1).3,11 Among women with recent GDM, the prevalence of abnormal glucose metabolism, including diabetes and pre-diabetes, at 4-12 weeks postpartum is approximately 14%,34 and increases significantly to ~50% by approximately one year postpartum.53 Recently, an OGTT at 2 days postpartum was demonstrated to have comparable ability to predict impaired glucose tolerance within 1 year postpartum as an OGTT at 4-12 weeks postpartum, with vastly greater uptake among women.54
Figure 1.
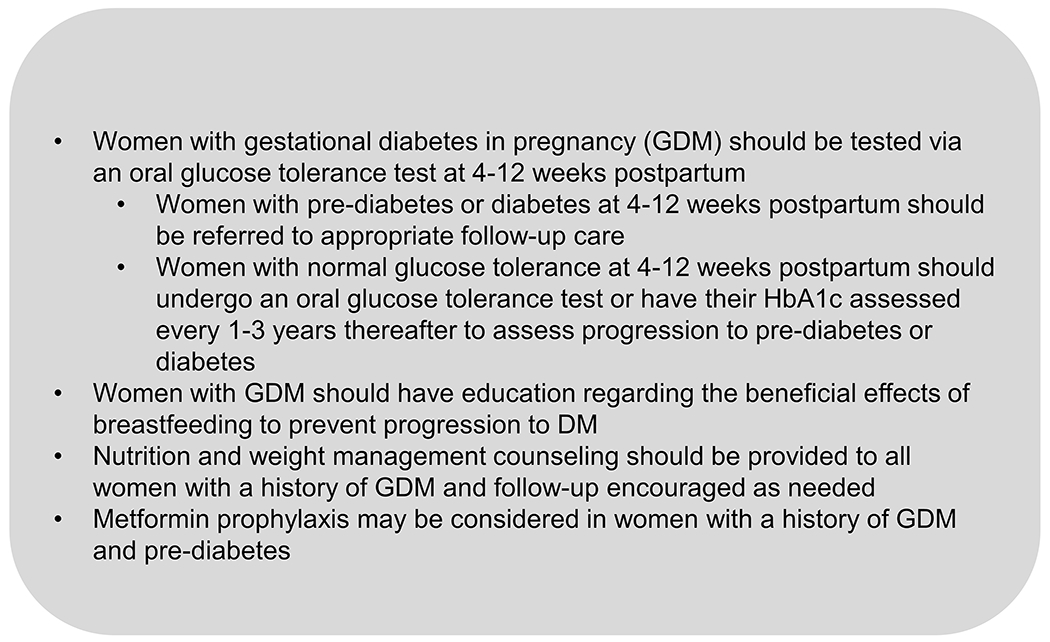
Summary of Current Clinical Recommendations to Prevent Progression to Diabetes in Women with Gestational Diabetes
Metabolomics
In recent years, metabolomic studies have shown increasing promise to improve prediction of women with recent GDM most likely to progress to postpartum DM. In a small cohort of ~100 Australian women followed 8-10 years after GDM diagnosis, C-peptide levels >450 pg/mL and ghrelin levels ≤400 pg/mL at 12 weeks postpartum were associated with an increased odds of DM within 8-10 years.55 In two recent nested case-control studies of women enrolled in the SWIFT cohort and matched on age, pre-pregnancy BMI and race/ethnicity, researchers identified 21 metabolites (AUC 77%, sensitivity 74%, specificity 77%) and subsequently a seven lipid-metabolites (AUC 91%, sensitivity 87%, specificity 93%) at 6-9 weeks postpartum which predicted progression to DM within 2-4 years postpartum. In both studies the metabolomic biomarkers improved prediction of DM relative to fasting plasma glucose or 2-hour glucose values at 6-9 weeks postpartum alone.56,57 In a separate cohort, three different lipid species predicted DM within 8-10 years in women with GDM. When added to a model with traditional clinical risk factors including age, BMI, and levels of pregnancy fasting glucose, postnatal fasting glucose, triacylglycerol and total cholesterol, the three lipid species improved the AUC from 76% to 87% with 90% specificity, although sensitivity remained low (59%).58 While metabolomics holds promise for improving the identification of women at high risk for progressing to DM postpartum, such methods are not yet part of routine clinical care and management.
Clinical
Glycemic medications
For women with GDM, pharmacological prophylaxis may help to prevent progression to DM. In analyses of the Diabetes Prevention Program trial and follow-up including women with a history of GDM, metformin reduced the incidence of DM by 50% in the first three years after randomization and by 40% at 10 years of follow-up, compared to the placebo group.41,42 Over 15 years of follow-up, metformin was significantly more effective in women with a history of GDM, leading to a 41% reduction in DM incidence.59 Metformin was not as effective at reducing DM incidence in all high risk groups, leading to metformin prophylaxis being recommended only for women with a history of GDM and those with higher baseline fasting glucose or higher HbA1C. 59 Despite its efficacy in women with GDM, metformin in not widely prescribed in the United States.60 Other drugs, including troglitazone pioglitazone, have shown efficiency in randomized controlled trials in enhancing insulin sensitivity and reducing the incidence DM in high-risk women with previous GDM.61,62 However, troglitazone is no longer used due to liver toxicity.
Contraception
In women with previous GDM, contraceptive choice may influence postpartum risk of DM. Oral contraceptives, most notably progestin-only oral contraceptives, influence insulin sensitivity. Changes in insulin sensitivity related to OC use are not clinically significant in normoglycemic women but may influence progression to DM in women with GDM.63 For example, in a cohort of 443 Hispanic women with recent GDM, progestin-only oral contraceptive pills, compared to low-dose combination oral contraceptive, were associated with a nearly 3-fold risk of developing diabetes within 7 years of the index pregnancy.64 One other study has noted a potential small increased risk of postpartum DM among women with GDM who use depomedroxyprogesterone acetate (DMPA) use compared to combination oral contraceptives; however the majority of risk associated with DMP is thought to be related to DMPA-associated weight gain and confounding factors such as BMI, breastfeeding status, and family history of DM, that correlated with DMPA use and DM risk.65
Conclusion
Women with GDM during pregnancy are at extremely high risk for progression to DM postpartum overall, yet among women with GDM there is marked variation in the likelihood of going on to develop DM. The causal pathways from GDM to DM postpartum remain unclear, but available evidence suggests that women who are obese pre-pregnancy, with a genetic predisposition to DM, who require insulin treatment during pregnancy, who gain most weight postpartum, and who have unfavorable diets and low levels of physical activity may be at particularly high risk for progression to DM. Postpartum weight management through diet and physical activity, breastfeeding, and metformin treatment may help to prevent progression. However, in order to reduce the risk of progression, women with GDM should have their glucose metabolism tested regularly, be counseled on effective nutritional and lifestyle management strategies, and metformin should be considered to reduce the risk of progression to DM.
Acknowledgments
Funding: This work was supported by the National Institute of Mental Health l (grant number R00 MH112413) and the American Diabetes Association (grant number 1-16-ICTS-118).
Footnotes
Conflicts of interest: None declared
References
- 1.Casagrande SS, Linder B, Cowie CC. Prevalence of gestational diabetes and subsequent Type 2 diabetes among U.S. women. Diabetes Res Clin Pract. 2018;141:200–208. [DOI] [PubMed] [Google Scholar]
- 2.Deputy NP, Kim SY, Conrey EJ, Bullard KM. Prevalence and Changes in Preexisting Diabetes and Gestational Diabetes Among Women Who Had a Live Birth - United States, 2012-2016. MMWR Morbidity and mortality weekly report. 2018;67(43):1201–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Committee on Practice BO. ACOG Practice Bulletin No. 190: Gestational Diabetes Mellitus. Obstet Gynecol. 2018;131(2):e49–e64. [DOI] [PubMed] [Google Scholar]
- 4.Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373(9677):1773–1779. [DOI] [PubMed] [Google Scholar]
- 5.Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25(10):1862–1868. [DOI] [PubMed] [Google Scholar]
- 6.Metzger BE, Cho NH, Roston SM, Radvany R. Prepregnancy weight and antepartum insulin secretion predict glucose tolerance five years after gestational diabetes mellitus. Diabetes Care. 1993;16(12):1598–1605. [DOI] [PubMed] [Google Scholar]
- 7.Kramer CK, Campbell S, Retnakaran R. Gestational diabetes and the risk of cardiovascular disease in women: a systematic review and meta-analysis. Diabetologia. 2019;62(6):905–914. [DOI] [PubMed] [Google Scholar]
- 8.Li J, Song C, Li C, Liu P, Sun Z, Yang X. Increased risk of cardiovascular disease in women with prior gestational diabetes: A systematic review and meta-analysis. Diabetes Res Clin Pract. 2018;140:324–338. [DOI] [PubMed] [Google Scholar]
- 9.Retnakaran R, Luo J, Shah BR. Gestational diabetes in young women predicts future risk of serious liver disease. Diabetologia. 2019;62(2):306–310. [DOI] [PubMed] [Google Scholar]
- 10.American Diabetes A Economic Costs of Diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Diabetes A 13. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl 1):S137–S143. [DOI] [PubMed] [Google Scholar]
- 12.Hunt KJ, Logan SL, Conway DL, Korte JE. Postpartum screening following GDM: how well are we doing? Current diabetes reports. 2010;10(3):235–241. [DOI] [PubMed] [Google Scholar]
- 13.Ley SH, Ardisson Korat Andres V., Qi Sun, Tobias Deirdre K., Cuilin Zhang, Lu Qi, Willett Walter C., Manson JoAnn E., and Hu Frank B.. Contribution of the Nurses’ Health Studies to uncovering risk factors for type 2 diabetes: diet, lifestyle, biomarkers, and genetics. Vol 9 American journal of public health 2016:1624–1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Damm P, Kühl C, Bertelsen A, Mølsted-Pedersen L. Predictive factors for the development of diabetes in women with previous gestational diabetes mellitus. American journal of obstetrics and gynecology. 1992;167(3):607–616. [DOI] [PubMed] [Google Scholar]
- 15.Vambergue A, Dognin C, Boulogne A, Réjou M, Biausque S, Fontaine P. Increasing incidence of abnormal glucose tolerance in women with prior abnormal glucose tolerance during pregnancy: DIAGEST 2 study. Diabetic medicine. 2008;25(1):58–64. [DOI] [PubMed] [Google Scholar]
- 16.Chivese T, Norris SA, Levitt NS. Progression to type 2 diabetes mellitus and associated risk factors after hyperglycemia first detected in pregnancy: A cross-sectional study in Cape Town, South Africa. PLoS medicine. 2019;16(9):e1002865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rayanagoudar G, Hashi AA, Zamora J, Khan KS, Hitman GA, Thangaratinam S. Quantification of the type 2 diabetes risk in women with gestational diabetes: a systematic review and meta-analysis of 95,750 women. Diabetologia. 2016;59(7):1403–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cormier H, Vigneault J, Garneau V, et al. An explained variance-based genetic risk score associated with gestational diabetes antecedent and with progression to pre-diabetes and type 2 diabetes: a cohort study. Bjog. 2015;122(3):411–419. [DOI] [PubMed] [Google Scholar]
- 19.Kwak SH, Choi SH, Kim K, et al. Prediction of type 2 diabetes in women with a history of gestational diabetes using a genetic risk score. Diabetologia. 2013;56(12):2556–2563. [DOI] [PubMed] [Google Scholar]
- 20.Li M, Rahman ML, Wu J, et al. Genetic factors and risk of type 2 diabetes among women with a history of gestational diabetes: findings from two independent populations. BMJ Open Diabetes Research and Care. 2020;8(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yudell M, Roberts D, DeSalle R, Tishkoff S. Taking race out of human genetics. Science. 2016;351(6273):564–565. [DOI] [PubMed] [Google Scholar]
- 22.Xiang A, Li B, Black M, et al. Racial and ethnic disparities in diabetes risk after gestational diabetes mellitus. Diabetologia. 2011;54(12):3016–3021. [DOI] [PubMed] [Google Scholar]
- 23.Rayanagoudar G, Hashi AA, Zamora J, Khan KS, Hitman GA, Thangaratinam S. Quantification of the type 2 diabetes risk in women with gestational diabetes: a systematic review and meta-analysis of 95,750 women. Springer; 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sinha B, Brydon P, Taylor R, et al. Maternal ante-natal parameters as predictors of persistent postnatal glucose intolerance: a comparative study between Afro-Caribbeans, Asians and Caucasians. Diabetic Medicine. 2003;20(5):382–386. [DOI] [PubMed] [Google Scholar]
- 25.Oldfield MD, Donley P, Walwyn L, Scudamore I, Gregory R. Long term prognosis of women with gestational diabetes in a multiethnic population. Postgrad Med J. 2007;83(980):426–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ali Z, Alexis SD. Occurrence of diabetes mellitus after gestational diabetes mellitus in Trinidad. Diabetes Care. 1990;13(5):527–529. [DOI] [PubMed] [Google Scholar]
- 27.Jang HC, Yim CH, Han KO, et al. Gestational diabetes mellitus in Korea: prevalence and prediction of glucose intolerance at early postpartum. Diabetes Res Clin Pract. 2003;61(2):117–124. [DOI] [PubMed] [Google Scholar]
- 28.Pallardo F, Herranz L, Garcia-Ingelmo T, et al. Early postpartum metabolic assessment in women with prior gestational diabetes. Diabetes Care. 1999;22(7):1053–1058. [DOI] [PubMed] [Google Scholar]
- 29.Cho NH, Lim S, Jang HC, Park HK, Metzger BE. Elevated homocysteine as a risk factor for the development of diabetes in women with a previous history of gestational diabetes mellitus: a 4-year prospective study. Diabetes Care. 2005;28(11):2750–2755. [DOI] [PubMed] [Google Scholar]
- 30.Buchanan TA, Xiang A, Kjos SL, et al. Gestational diabetes: antepartum characteristics that predict postpartum glucose intolerance and type 2 diabetes in Latino women. Diabetes. 1998;47(8):1302–1310. [DOI] [PubMed] [Google Scholar]
- 31.Bao W, Yeung E, Tobias DK, et al. Long-term risk of type 2 diabetes mellitus in relation to BMI and weight change among women with a history of gestational diabetes mellitus: a prospective cohort study. Diabetologia. 2015;58(6):1212–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Löbner K, Knopff A, Baumgarten A, et al. Predictors of postpartum diabetes in women with gestational diabetes mellitus. Diabetes. 2006;55(3):792–797. [DOI] [PubMed] [Google Scholar]
- 33.Kjos SL, Peters RK, Xiang A, Henry OA, Montoro M, Buchanan TA. Predicting future diabetes in Latino women with gestational diabetes. Utility of early postpartum glucose tolerance testing. Diabetes. 1995;44(5):586–591. [DOI] [PubMed] [Google Scholar]
- 34.Ogonowski J, Miazgowski T. The prevalence of 6 weeks postpartum abnormal glucose tolerance in Caucasian women with gestational diabetes. Diabetes Res Clin Pract. 2009;84(3):239–244. [DOI] [PubMed] [Google Scholar]
- 35.Kugishima Y, Yasuhi I, Yamashita H, et al. Risk factors associated with the development of postpartum diabetes in Japanese women with gestational diabetes. BMC Pregnancy Childbirth. 2018;18(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brown J, Martis R, Hughes B, Rowan J, Crowther CA. Oral anti-diabetic pharmacological therapies for the treatment of women with gestational diabetes. The Cochrane database of systematic reviews. 2017;1:CD011967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peters RK, Kjos SL, Xiang A, Buchanan TA. Long-term diabetogenic effect of single pregnancy in women with previous gestational diabetes mellitus. Lancet. 1996;347(8996):227–230. [DOI] [PubMed] [Google Scholar]
- 38.Russell C, Dodds L, Armson BA, Kephart G, Joseph KS. Diabetes mellitus following gestational diabetes: role of subsequent pregnancy. BJOG. 2008;115(2):253–259; discussion 260. [DOI] [PubMed] [Google Scholar]
- 39.Damm P, Kühl C, Bertelsen A, Mølsted-Pedersen L. Predictive factors for the development of diabetes in women with previous gestational diabetes mellitus. Am J Obstet Gynecol. 1992;167(3):607–616. [DOI] [PubMed] [Google Scholar]
- 40.Feig DS, Shah BR, Lipscombe LL, et al. Preeclampsia as a risk factor for diabetes: a population-based cohort study. PLoS Med. 2013;10(4):e1001425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ratner RE, Christophi CA, Metzger BE, et al. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. The Journal of clinical endocrinology and metabolism. 2008;93(12):4774–4779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aroda VR, Christophi CA, Edelstein SL, et al. The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up. The Journal of clinical endocrinology and metabolism. 2015;100(4):1646–1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pan X-R, Li G-w, Hu Y-H, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and Diabetes Study. Diabetes care. 1997;20(4):537–544. [DOI] [PubMed] [Google Scholar]
- 44.Bao W, Tobias DK, Bowers K, et al. Physical activity and sedentary behaviors associated with risk of progression from gestational diabetes mellitus to type 2 diabetes mellitus: a prospective cohort study. JAMA internal medicine. 2014;174(7):1047–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goveia P, Cañon-Montañez W, Santos DdP, et al. Lifestyle intervention for the prevention of diabetes in women with previous gestational diabetes mellitus: a systematic review and meta-analysis. Frontiers in endocrinology. 2018;9:583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gunderson EP, Hurston SR, Dewey KG, et al. The study of women, infant feeding and type 2 diabetes after GDM pregnancy and growth of their offspring (SWIFT Offspring study): prospective design, methodology and baseline characteristics. BMC Pregnancy Childbirth. 2015;15:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ziegler AG, Wallner M, Kaiser I, et al. Long-term protective effect of lactation on the development of type 2 diabetes in women with recent gestational diabetes mellitus. Diabetes. 2012;61(12):3167–3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tanase-Nakao K, Arata N, Kawasaki M, et al. Potential protective effect of lactation against incidence of type 2 diabetes mellitus in women with previous gestational diabetes mellitus: A systematic review and meta-analysis. Diabetes/metabolism research and reviews. 2017;33(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stuebe AM, Rich-Edwards JW, Willett WC, Manson JE, Michels KB. Duration of lactation and incidence of type 2 diabetes. JAMA. 2005;294(20):2601–2610. [DOI] [PubMed] [Google Scholar]
- 50.Moon JH, Kwak SH, Jung HS, et al. Weight Gain and Progression to Type 2 Diabetes in Women With a History of Gestational Diabetes Mellitus. The Journal of clinical endocrinology and metabolism. 2015;100(9):3548–3555. [DOI] [PubMed] [Google Scholar]
- 51.Ehrlich SF, Hedderson MM, Quesenberry CP Jr., et al. Post-partum weight loss and glucose metabolism in women with gestational diabetes: the DEBI Study. Diabet Med. 2014;31(7):862–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tura A, Grassi A, Winhofer Y, et al. Progression to type 2 diabetes in women with former gestational diabetes: time trajectories of metabolic parameters. PLoS One. 2012;7(11):e50419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Picón MJ, Murri M, Muñoz A, Fernández-García JC, Gomez-Huelgas R, Tinahones FJ. Hemoglobin A1c versus oral glucose tolerance test in postpartum diabetes screening. Diabetes Care. 2012;35(8):1648–1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Werner EF, Has P, Rouse D, Clark MA. Two day post-partum compared to 4-12 week post-partum glucose tolerance testing for women with gestational diabetes. Am J Obstet Gynecol. 2020. [DOI] [PubMed] [Google Scholar]
- 55.Lappas M, Jinks D, Ugoni A, Louizos CC, Permezel M, Georgiou HM. Post-partum plasma C-peptide and ghrelin concentrations are predictive of type 2 diabetes in women with previous gestational diabetes mellitus. J Diabetes. 2015;7(4):506–511. [DOI] [PubMed] [Google Scholar]
- 56.Allalou A, Nalla A, Prentice KJ, et al. A Predictive Metabolic Signature for the Transition From Gestational Diabetes Mellitus to Type 2 Diabetes. Diabetes. 2016;65(9):2529–2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Khan SR, Mohan H, Liu Y, et al. The discovery of novel predictive biomarkers and early-stage pathophysiology for the transition from gestational diabetes to type 2 diabetes. Diabetologia. 2019;62(4):687–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lappas M, Mundra PA, Wong G, et al. The prediction of type 2 diabetes in women with previous gestational diabetes mellitus using lipidomics. Diabetologia. 2015;58(7):1436–1442. [DOI] [PubMed] [Google Scholar]
- 59.Group DPPR. Long-term effects of metformin on diabetes prevention: identification of subgroups that benefited most in the Diabetes Prevention Program and Diabetes Prevention Program Outcomes Study. Diabetes Care. 2019;42(4):601–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moin T, Schmittdiel JA, Flory JH, et al. Review of Metformin Use for Type 2 Diabetes Prevention. American journal of preventive medicine. 2018;55(4):565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Berkowitz K, Peters R, Kjos SL, et al. Effect of troglitazone on insulin sensitivity and pancreatic beta-cell function in women at high risk for NIDDM. Diabetes. 1996;45(11):1572–1579. [DOI] [PubMed] [Google Scholar]
- 62.Xiang AH, Peters RK, Kjos SL, et al. Effect of pioglitazone on pancreatic beta-cell function and diabetes risk in Hispanic women with prior gestational diabetes. Diabetes. 2006;55(2):517–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Petersen KR, Skouby SO, Jespersen J. Contraception guidance in women with pre-existing disturbances in carbohydrate metabolism. The European journal of contraception & reproductive health care : the official journal of the European Society of Contraception. 1996;1(1):53–59. [PubMed] [Google Scholar]
- 64.Kjos SL, Peters RK, Xiang A, Thomas D, Schaefer U, Buchanan TA. Contraception and the risk of type 2 diabetes mellitus in Latina women with prior gestational diabetes mellitus. JAMA. 1998;280(6):533–538. [DOI] [PubMed] [Google Scholar]
- 65.Xiang AH, Kawakubo M, Kjos SL, Buchanan TA. Long-acting injectable progestin contraception and risk of type 2 diabetes in Latino women with prior gestational diabetes mellitus. Diabetes Care. 2006;29(3):613–617. [DOI] [PubMed] [Google Scholar]


