Abstract
Evidence for the effectiveness of population health screenings to reduce the burden of non-communicable diseases in low income countries remains very limited. We investigate the sustained effects of a health screening in Malawi where individuals received a referral letter if they had elevated blood pressure. Using a regression discontinuity design and a matching estimator, we find that receiving a referral letter reduced blood pressure and the probability of being hypertensive by about 22 percentage points four years later. These lasting effects are explained by a 20 percentage points increase in the probability of being diagnosed with hypertension. There is also evidence of an increase in the uptake of medication, while we do not identify improvements in hypertension-related knowledge or risk behaviors. On the contrary, we find an increase in sugar intake and a decrease in physical activity both of which are considered risky behaviors in Western contexts. The health screening had some positive effects on mental health. Overall, this study suggests that population-based hypertension screening interventions are an effective tool to improve health in low-income contexts.
Keywords: Health Screening, Hypertension, Non-communicable Diseases, Regression Discontinuity Design, Matching Estimator, Low Income Countries, Malawi
JEL: C21, I12, I18
1. Introduction
Individuals often have very imperfect knowledge about their own health (Foot et al. 2014). This lack of knowledge can inhibit critical health decision making and result in preventable elevated mortality and morbidity (Kenkel 1991; Ruhm 2016). Limited knowledge about own health is of particular concern when severe medium/long-term health risks do not manifest themselves in instantaneous disease symptoms. Examples include: HIV infection, with infected individuals facing significantly elevated morbidity and mortality as the disease progresses, while experiencing virtually no specific indications of being HIV+ for a prolonged period of time (Tomar 1994); diseases with well-defined genetic risk factors but delayed manifestation of symptoms, including breast cancer or some inherited disorders such as Huntington’s disease (Müller et al. 2018; Oster et al. 2013); or conditions such as insulin resistance where early detection and intervention can reduce cumulative organ damage and delay disease progression to adult-onset diabetes (American Diabetes Association 2002). In this category of illnesses is also cardiovascular disease (CVD), an eminent disease burden in low- and middle-income countries (LMICs) that has emerged as the leading cause of disability and death among individuals aged 50+ (Figure A.1), including in sub-Saharan African (SSA) countries affected by the HIV epidemic (Figure A.2) (GBD Collaborators 2018). Hypertension is the primary modifiable risk factors for CVDs, but individuals with high blood pressure generally experience few noticeable indications of hypertension. Yet, they face heightened morbidity and mortality risks through stroke, heart attacks, metabolic syndrome, memory loss or dementia (Geldsetzer et al. 2019; Lackland and Weber 2015; Wang et al. 2006).
Improving individuals’ knowledge about their own health has the potential to reduce morbidity and mortality in the above cases, as informed individuals can respond to latent health risks through appropriate prevention and/or risk-reduction strategies. For example, HIV testing is a pathway to access antiretroviral treatment (ART), a diagnosis of hypertension can be followed up by behavioral changes or biomedical treatment to reduce CVD risks, women may opt to undergo mastectomy if they are identified as carriers of BRCA1 or BRCA2 genes, etc. Because of the basic insight that knowledge is key to prevention and treatment, health screenings have been promoted and implemented in many contexts as a tool to improve population health and enhance individuals’ ability to effectively invest in heath across the life course. In high-income countries, health screenings are routinely conducted as part of regular health care visits (Swenson and Ebell 2016). In countries affected by the HIV epidemic, HIV testing has become an essential component of pre-natal care, and door-to-door HIV testing, widespread screening as part of National HIV Testing Days, and HIV self-testing have all been promoted as effective health policy (CDC 2020; Ganguli et al. 2009; WHO 2016). Demand for such testing services is often high (Thornton 2008). In contrast to these well established screening programs, currently very limited non-communicable disease (NCD) screening is conducted in LMICs, which is in striking contrast to the rapidly rising NCD disease burden (GBD Collaborators 2018; NCD-RisC Collaboration 2017). As a result, poor and rural populations are likely to have a high prevalence of undiagnosed risk factors (Geldsetzer et al. 2019; Islam et al. 2014).
Population-based health screenings have been promoted in LMICs to address this rising NCD-related morbidity and mortality (Benziger et al. 2016a; Greenberg et al. 2011). Screening for hypertension is particularly relevant as the prevalence of hypertension in LMICs ranges between 20% and 40% (Ibrahim and Damasceno 2012). Yet, important concerns remain as to whether NCDs-screening in low income countries (LICs) is effective for improving population health for several reasons. First, individuals need to have basic NCDs-related health literacy in order to be able to act based on obtaining knowledge about hypertension or similar NCDs-risk factors (Das et al. 2017; Sjørensen et al. 2012; WHO 2015). Even if the health screening is accompanied by the respective health information about the determinants, behavioral and biomedical risk reduction strategies, because of limited health literacy and knowledge individuals may not be able to respond to the provided health information in ways that results in longer-term morbidity and mortality benefits. Second, prevention and treatment guidelines for NCDs and CVDs specifically in LICs are often based on established guidelines for higher-income countries. However, individuals’ ability to effectively respond to NCDs-related information revealed during heath screenings is made more complex in LICs by the fact that CVD and certain other NCDs are partially driven by a different set of risk factors than in higher-income contexts (WHO 2013a). Third, health systems in LICs are often inadequately prepared and equipped in terms of staffing, equipment, guidelines and medications to diagnose, manage and/or treat NCDs (Cappuccio and Miller 2016; Nulu et al. 2016). Individuals who present themselves to the health system based on NCD-related health screenings, therefore, often may not be able to receive treatment or guidance that allows them to reduce their underlying health risks.
The existing evidence about the effectiveness of NCDs-related health screenings is mixed, including the one generated in high-income countries with sophisticated health systems and relatively good NCDs-related health literacy (Krogsbøll et al. 2012). While there is some evidence about the effectiveness of NCDs-related health screenings in high and middle-income populations (Bhalotra et al. 2018; Chen et al. 2019; Rodriguez-Lesmes et al. 2017; Zhao et al. 2013), to date, no population-based evidence exists about its effectiveness in rural LICs contexts. Moreover, the effectiveness of NCDs-related health screenings in poor and/or rural LMICs populations cannot be inferred by relying on research evidence generated in higher-income countries, given the distinctly different health systems, distinct risk factors for common NCDs, and low NCDs-related health literacy in the population. The experience in LICs with HIV testing however provides useful guidance on how the benefits of population-based screening multiply once access to the respective health care is made available. Prior to the widespread availability of ART, the benefits of widespread population-based HIV testing were controversial (Denison et al. 2008). Once access to ART became widely available, HIV testing outside of clinical settings has became the gateway to accessing ART and the benefits of testing are widely accepted (CDC 2020).
This paper fills an important gap in the research on the effectiveness of population-based screening for NCDs in LICs by evaluating the long-term effects of a simple and inexpensive population-based health screening for hypertension in Malawi. Specifically, we investigate if screening for high blood pressure among mature adults with high prevalence of hypertension can lead to significant long-term gains in hypertension-related health outcomes such as reductions in blood pressure levels, or uptake in diagnosis and medication. The causal identification of these effects exploits a study design feature that provided “at-risk” study participants with a referral letter for further assessment by a health care provider if they were measured with blood pressure above a specific threshold (160 units of millimeters of mercury (mmHg) systolic or 110 mmHg diastolic blood pressure)1. We pursue two empirical strategies to evaluate the effects of the referral letter. Using a sharp regression discontinuity design (RDD), we compare the outcomes for individuals who are right above the cutoff for receiving the referral letter (treatment group) to the outcomes for those who are right below the cutoff (control group). The second strategy, a nearest-neighbor matching estimator, exploits the availability of multiple blood pressure measurements to estimate the causal effects of getting a referral letter on hypertension-related health outcomes away from the cutoff of 160 mmHg systolic blood pressure. The protocol requires the health professionals to measure blood pressure three times consecutively.2 This second strategy matches individuals based on the mean of the three blood pressure measurements while the RDD strategy is implicitly matching individuals on their maximum blood pressure measurements. The two methods complement each other: the discontinuity design controls best for selection, while matching allows to explore the results away from the critical cutoff and provides estimates with higher external validity. The results yield very similar estimates across the two different methods, although they vary in some cases in their statistical power.
Overall, our study finds that hypertension health screening was effective, and that providing referral letters to at-risk respondents resulted in a long-term reduction of blood pressure. More specifically, the regression discontinuity local average treatment effect on the change in systolic blood pressure between 2013 and 2017 is around −14.3 mmHg, which corresponds to about half a standard deviation in systolic blood pressure. The average treatment effect on the treated measured by the matching estimator is very similar at about −12.6 mmHg. We also find a negative treatment effect of about half a standard deviation for diastolic blood pressure (−6 mmHg) using both methods. As a consequence of this drop in blood pressure levels, individuals in the treatment group ended up being 22% less likely to be hypertensive in 2017. Such sustained long-term effects have not previously been documented for NCD-related health screening in rural LIC populations with low levels of health literacy, high NCD prevalence and limited access to NCDs care through the health system.
The observed drop in blood pressure among at-risk respondents subsequent to the Malawi Longitudinal Study of Families and Health - Mature Adults Cohort (MLSFH-MAC) health screening was most likely the consequence of a sharp increase in the rate of diagnosis for hypertension. Individuals who received the referral letter have a 20 percentage points higher chance to have been diagnosed as hypertensive by a medical provider within two years before the follow-up assessment in 2017. The increase in diagnosis rate that resulted from the referral letter also seemed to have lead to a higher share of individuals who were treated for hypertension by taking medication, although the effects are less precisely estimated and are statistically significant only in the matching estimates. In the matching specification, the health screening resulted in a 13 percentage points increase in the probability of taking medication at the time of the interview. This effect is rather large considering that only 9.4% of the sample was currently taking medication for hypertension in 2017.
Efforts to reduce blood pressure through medication could be reinforced or hampered by other hypertension-related risk behaviors such as unhealthy diet and lack of physical exercise. We fail to find any positive effects of the referral letter on these risk behaviors. If anything, we find some negative effects, according to Western recommendations, such as an increase in sugar intake and a decrease in physical exercise in the matching estimates only. These counter-intuitive behavioral responses are possibly related to the fact that some risk factors for CVDs in LICs are different from those established in higher-income contexts (our study population, for example, is physically very active, has almost no obesity or consumption of western diets, and nevertheless, is characterized by widespread hypertension Kohler et al. 2018b). It is therefore not clear that standard recommendations about how to reduce high blood pressure, which are generally derived based on evidence from Western high-income populations, are pertinent to LIC populations. Individuals in our study population might also be aware that their options for changing dietary behaviors or physical activity levels are very limited, and that any such changes might overall have no (or even negative) effects on their health and well-being. Given the intensity of physical activity in the day-to-day life of rural Malawi, reducing physical activity could actually be a strategy to improve their own health. These findings have important consequences for the design of NCDs screening protocols in low income contexts and future research should try to uncover the mechanisms behind this behavioral response. We also do not find any effect on improved hypertension knowledge such as knowing the symptoms of hypertension and its treatment options. Finally, we do not find that the referral had negative effects on subjective physical and mental health. If anything, we find some evidence of a positive effect on subjective mental health in the RDD specification. This is important for ethical reasons, as giving information about high blood pressure could have potentially been depressing and counterproductive.
In summary, social science research on global health is often out-of-sync with the changing disease burden in LMICs (Behrman et al. 2011), and particularly economic research on behavioral interventions to stem the growing NCD burden in low-income country settings remains rare. Our analyses contribute to the literature on health care demand for newly emerging disease burdens in LICs, and more broadly, to the literature on how individuals respond to new information about their own health in terms of life-course decision-making (Dupas and Miguel 2017). Our results are consistent with findings from high- and middle-income countries that evaluated the effects of population-based health screening for hypertension using similar identification strategies (Bhalotra et al. 2018; Chen et al. 2019; Rodriguez-Lesmes et al. 2017; Zhao et al. 2013) although very few other studies—and none in LMICs—have examined sustained population-based effects of health screening during a 4-year period. Our study expands this research by documenting the effects of NCD-related health screening in a very poor LIC context, and by investigating the pathways through which screening resulted in reduced blood pressure and improved hypertension management by affecting knowledge, diagnosis and medical treatment. Our study is also the first to exploit a dual methodological approach for establishing the causal effects of health screening. While the RDD strategy provides valid causal inference at the cutoff and has high internal validity, the matching strategy we employ allows to increase the external validity of our findings by estimating the effects of the referral for hypertension on different sets of individuals, therefore providing important insights for policies aiming at changing the different cutoffs for screening high blood pressure.
2. Non-communicable diseases (NCDs) and Health Screening in LICs
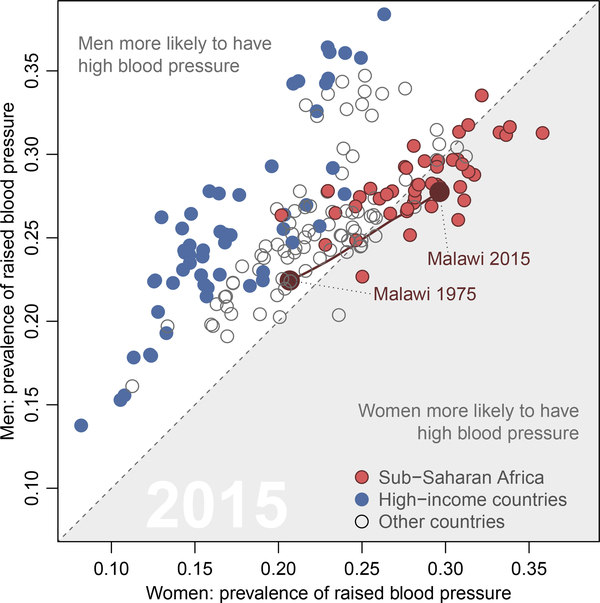
The prevalence of hypertension in African countries is high (Figure 1). While there have been important steps to improve treatment coverage for communicable diseases such as HIV and malaria (Lozano et al. 2012; Murray et al. 2012), the health care systems in these countries are ill-prepared to face the emergency of the rapidly increasing burden of hypertension and other NCDs (Beaglehole et al. 2008; Kämpfen et al. 2018). Moreover, despite the shifting burden of disease in SSA LICs, individuals’ knowledge about NCD risk factors, the symptoms and the importance of preventive health care to reduce NCD risk factors are generally very limited (Boateng et al. 2017; Das et al. 2017; Sjørensen et al. 2012; WHO 2015). NCD-related healthcare and knowledge is hampered by the fact that adequate information and resources are not provided to sub-populations at greatest risk and/or most affected by chronic conditions. Importantly this includes older populations above age 45, the majority of whom continues to live in rural areas, has very low levels of formal education and has very limited access to adequate NCD-related healthcare (Boateng et al. 2017; Kohler et al. 2018a; Malawi MOH and WHO 2010).
Figure 1: Prevalence of high blood pressure (systolic), by sex, 2015 (%, age-standardized).
Source: Adapted from The Economist (2017), based on NCD-RisC Collaboration (2017)
Policy options for addressing issues related to hypertension and the shifting burden of disease in LICs face formidable implementation challenges due to strained health systems that are coping with a dual burden of infectious and non-communicable diseases, have restricted resources for NCD-related health promotion and prevention, and serve populations with low NCD-related health literacy. Among the various measures that can potentially be put in place to contain the rising epidemic of hypertension and NCDs more generally, access to preventive care, screening interventions and early detection of health conditions are perhaps the ones that are the more efficient and recommended (WHO 2013b). Screening and early detection of health conditions, especially of high-blood pressure, have important benefits (American Heart Association 2019; Siu 2015). Indeed, high-blood pressure screening has no harms and facilitates the detection of associated CVDs diseases at an early stage and thus prevent individuals from going through unaffordable health care and more rigorous treatments that complications would require (Dehmer et al. 2017; Howard et al. 2010; Sheridan et al. 2003; Siu 2015; Wald et al. 1999). Given the limited health systems in SSA LICs, understanding the health behaviors and responses of individuals in the face of NCD awareness and screening is therefore crucial to contain the increasing burden of hypertension and NCDs more generally (Dupas 2011).
To date, however, very little evidence exists on the effectiveness of population-based health screening efforts focused on NCDs in LICs countries, in contrast to the extensive literature on screening (testing) for HIV and some other communicable diseases in LICs (e.g., Cohen et al. 2015; Delavande and Kohler 2012; Gong 2014; Thornton 2008).3 A general finding is that households in low-income countries spend a significant portion of their resources on remedial health care but very little in preventive health care (Dupas 2011). A growing research evidence supports interventions to increase investments in preventive health care (Dupas and Miguel 2017), among which health screening is perhaps the most efficient, particularly for newly proliferating NCDs (Strong et al. 2005; WHO 2014).
3. Context and Data
3.1. Context
Our study is based in Malawi, a SSA country with one of the lowest income per capita in the world, equal to about 2% of the global average, and a Human Development Index that is ranked 172 out of 189 countries (HDI2018 = .485). In rural areas, where our study is based and most Malawians (85%) live, the majority of individuals engage in home production of crops, complemented by some market activities. About 60% of the rural population is considered poor in 2016/17, thus having a total consumption that does not provide 2,400 calories per day per person plus some basic nonfood items, and 24% is considered ultrapoor (Malawi NSO and World Bank 2018; World Bank Group 2018). The HIV epidemic reached its peak in the 2000s when the availability of ART started to reduce the number of HIV-related deaths and initiated rebound of life expectancy (GBD Collaborators 2018; Jahn et al. 2008). NCDs have since become a major cause of death, as is also the case in other LMICs. Underlying this shifting disease burden is a high and increasing prevalence of NCD-risk factors such as hypertension (Figure 1). Our study population is no exception: more than than 60% of the mature adults in 2013 were at least pre-hypertensive, and 42.30% had Stage 1 or Stage 2 hypertension, exposing more than two-fifth of respondents to substantially elevated CVD risks (Kohler et al. 2018b).4 Similar high levels of hypertension have been documented in other studies in Malawi (Price et al. 2018). In Malawi and other LICs, however, the increasing importance of NCDs is not matched with a significant increase in financial and human resources dedicated to NCDs-related health care (Beaglehole et al. 2008). Hospitals in Malawi are understaffed and the medical staff is poorly trained to treat NCDs (Malawi Ministry of Health and ICF International 2014). In our study areas, about 85 percent of health facilities do not have staff recently trained to provide services for diabetes or for cardiovascular diseases. As a consequence of limited NCD-related heath care services, people are not routinely screened for NCDs, a situation that is especially pronounced in rural areas. As a result, very few people get screened for hypertension either because they are not aware of the risks associated with high blood pressure or because routine high blood pressure testing is not done as part of health examinations (Msyamboza et al. 2012).5
Estimates suggest that CVD, stroke, and hypertension alone account for over 35% of disability-adjusted life years (DALYs) lost over the age of 45 in Eastern SSA (Murray et al. 2012). More than 1/2 of all coronary disease in SSA can be attributed to high blood pressure (Ibrahim and Damasceno 2012; Ogah and Rayner 2013), and in South Africa the risk of death from high blood pressure has increased by >25% in a decade (Mayosi 2007; Mensah 2008). There also prevails a substantial burden of depression, anxiety, and other mental health disorders, accounting for over 34% of total years lived with disability (YLDs) (Murray et al. 2012). This relatively high burden of NCD takes a toll on the lives of older individuals, and a recent MLSFH study estimated that 45-year old women in Malawi can expect to spend a striking 58% of their remaining 28 years of life with functional limitations, while 45-year old men can expect to live 41% of their remaining 25.4 years subject to such limitations (Payne et al. 2013). While rising NCD burdens are a global phenomenon (Benziger et al. 2016b), their social, economic and health consequences are exacerbated in low-income countries because adequate information and resources are not provided to those who are at greatest risk and/or most affected by them (Boateng et al. 2017; WHO 2015). First, at health system level, few SSA LICs have developed effective and/or viable health policies and health-system guidelines to address the shifting disease burden towards NCDs (Echouffo-Tcheugui et al. 2015; Kämpfen et al. 2018), and the knowledge of health care providers about NCDs and treatment options, are often utterly inadequate (Muula and Misiri 2009). This is the case for NCDs in general, but also hypertension in particular: Our recent health care facility survey for instance documented that, out of 28 facilities serving the MLSFH-MAC study areas, in only 28% of the facilities staff has the experience to treat patients with CVDs (Kohler and Kohler 2020). Second, on the individual level, mature adults, while often affected by NCDs, have only limited awareness and knowledge about behavioral risk factors, symptoms, treatment and preventive care options for NCDs (Boateng et al. 2017; Kohler et al. 2018b; Malawi MOH and WHO 2010). Third, on the societal level, basic knowledge gaps exist for understanding the social and economic consequences of the high NCD-related disease burden, and for developing adequate public health policies and health-system responses needed for preventing the NCDs and related disabilities (Maharaj 2013; Malawi Ministry of Health 2011; Mayosi 2013).
3.2. The Mature Adults Cohort of the Malawi Longitudinal Study of Families and Health (MLSFH-MAC)
Our analyses use data from the Mature Adults Cohort of the Malawi Longitudinal Study of Families and Health (MLSFH-MAC), a longitudinal cohort study of individuals (mostly) aged 45 years and older in rural areas in three districts in Malawi (Mchinji, Rumphi and Balaka).6 The cohort was established in 2012, with follow-up waves in 2013, 2017 and 2018 collecting extensive information on physical, mental and cognitive health, NCDs-related health knowledge and NCDs-related health care utilization, socioeconomic well-being, household production and consumption, household structure and family change. The study population is broadly representative of the 45+ years old rural population in Malawi. The MLSFH and MLSFH-MAC Cohort Profiles provides detailed information on sampling procedures, study design and study instruments (Kohler et al. 2015, 2020).
3.3. Screening for high blood pressure in the MLSFH-MAC
The MLSFH-MAC screened all respondents for high blood pressure in 2013 and 2017 following the protocol established by the U.S. Health and Retirement Study (HRS) and using a Omron HEM-780 Blood Pressure Monitor (or comparable device). Three measurements by trained medical personnel were taken on the respondent’s left arm, about 45 seconds apart7, towards the end of the interview. Data recorded for each measurement included systolic and diastolic blood pressure, pulse, and the time of day the reading was taken. As part of the study protocol requirement, respondents who recorded at least one systolic blood pressure measurement above 160 mmHg, or at least one diastolic blood pressure measurement above 110 mmHg, were given referral letters for further assessment by a health care provider. The referral letter, which was handed over to respondents immediately after the blood measurements were taken, simply stated that the person was measured with high blood pressure surpassing 160 mmHg systolic and/or 110 mmHg diastolic and is referred to further assessment.8,9 The referral letter did not provide any additional information, including where and with whom the respondent should go for further assessment. Interviewers were also instructed to inform the respondent only about their blood pressure measurements, and not to provide additional information on blood pressure or hypertension, or indicate a diagnosis that a respondent might be hypertensive. The referral letter is included in the Appendix.
In addition, MLSFH-MAC asked the study participants if they have been diagnosed with hypertension by a medical provider (doctor or nurse) in the last 2 years prior to the survey and if they were taking medication for the treatment of hypertension at the time of the interviews in 2013 and 2017. MLSFH-MAC collected also detailed information on respondents’ knowledge about risk factors, symptoms and treatment of hypertension.
Table 1 shows the characteristics of our baseline sample in 2013, when blood pressure was measured for the first time in MLSFH-MAC. Specifically, the study sample is restricted to MLSFH-MAC respondents for whom we have three non-missing systolic and diastolic blood pressure measurements both in 2013 and 2017 (N=1,075).10 The average age of the sample used in this analysis is about 62 years, and women represent 59% of the study population. Respondents are almost equally distributed across the three study areas.
Table 1:
Descriptive statistics of the MLSFH-MAC sample, 2013-2017
| Mean (1) |
Std. dev. (2) |
10th (3) |
90th (4) |
|
|---|---|---|---|---|
| Blood pressure, referral letters, health behaviors ami literacy | ||||
| Mean systolic BP (2017) | 135.1 | 25.21 | 108 | 170.7 |
| Mean systolic BP (2013) | 134.26 | 25.31 | 106.3 | 170 |
| Mean diastolic BP (2017) | 83.67 | 12.69 | 69 | 100 |
| Mean diastolic BP (2013) | 85.94 | 12.49 | 71.3 | 102 |
| Hypertensive 2017a | .41 | .49 | 0 | 1 |
| Hypertensive in 2013a | .41 | .49 | 0 | 1 |
| Received a referral letter in 2013 | .19 | .4 | 0 | 1 |
| Being diagnosed in 2017 | .16 | .37 | 0 | 1 |
| Taking medication in 2017 | .09 | .29 | 0 | 0 |
| Know what high BP is (2017) | .82 | .39 | 0 | 1 |
| Know symptoms of high BP (2017) | .63 | .48 | 0 | 1 |
| Know will have to take treatment forever (2017) | .78 | .41 | 0 | 1 |
| Add extra salt to plate (2017) | .54 | .5 | 0 | 1 |
| Consume at least 1 sweet drink per day (2017) | .24 | .43 | 0 | 1 |
| Total number of teaspoons of sugar used in tea/coffee per day (2017) | 2.71 | 1.91 | 0 | 5 |
| Change in standardized SF12 physical score | 0 | 1.05 | −1.4 | 1.3 |
| Change in standardized SF12 mental score | 0 | 1.24 | −1.7 | 1.6 |
| Control variables | ||||
| Female | .59 | .49 | 0 | 1 |
| Age | 62.38 | 10.69 | 50 | 78 |
| Central region | .31 | .46 | 0 | 1 |
| South region | .34 | .47 | 0 | 1 |
| North region | .35 | .48 | 0 | 1 |
| Nb of observations in benchmark sample | 1075 | |||
Note: The sample is derived from the MLSFH-MAC 2013 and 2017 waves. Our analysis is based on a sample of 1075 individuals for which we have non-missing systolic and diastolic blood pressure measurements in 2013 and who were interviewed in 2017. The descriptive statistics of some of the variable in Table 1 are derived from a smaller sample because of missing values. Note also that we restricted our analysis to individuals who were 40 years or older in 2017.
We define someone as hypertensive if the mean systolic or diastolic blood pressure measurements was greater or equal to 140 and 90, respectively. 10th and 90th represent the 10th and 90th percentiles of the distributions, respectively.
The mean systolic blood pressure of individuals in our sample (based on three measurements) is equal to 134 mmHg in 2013 and 135 mmHg in 2017, and the corresponding mean values for diastolic blood pressure are 86 mmHg and 84 mmHg, respectively. The average blood pressure of mature adults is thus close to the thresholds used to classify an individual as hypertensive (i.e., currently these thresholds are 140 mmHg for systolic and 90 mmHg for diastolic blood pressure; Geldsetzer et al. 2019). In fact, according to these official guidelines, the prevalence of hypertension in our sample was 41% in both years.
About 19% of the individuals in our sample received a referral letter in 2013 because one of their systolic or diastolic blood pressure measurements was above 160 or 110, respectively. The rate of individuals being diagnosed with hypertension by a medical professional in the two years prior to the 2017 interview is almost as high, 16%, while only a subset of them, 9%, were taking medication for hypertension at the time of the survey.
In 2017, the vast majority of respondents know what hypertension is (82%) and 63% of them know the characteristics of the symptoms of hypertension.11,12 Moreover, the majority of the respondents is aware that, once diagnosed as hypertensive, they will have to take treatment forever (78%). About 24% of the study participants consume at least one sweet drink per day and on average they add daily about 2.71 teaspoons of sugar to their tea/coffee consumption. More than half of the respondents adds extra salt to their plate (54%).
Our analysis will also assess whether the high blood pressure screening has had any effects on overall physical and mental health. To do so, we compute respondent’s standardized SF12 physical and mental health scores and create individual change in these two scores between 2013 and 2017. SF12 subjective physical health and mental health scores are based on 12 questionnaire items that summarize the overall physical and mental health status of individuals by asking them to answer questions pertaining to several health subdomains, including general health, physical functioning, role functioning (physical and emotional), bodily pain, vitality, mental health and social functioning. The scores represent weighted sums of the answers to these 12 items and the difference between the physical and mental health scores lies in the different weights given to each item. The SF-12 scores have been widely used in different socio and demographic contexts, including in Sub Saharan African (Allotey and Reidpath 2007; Gandek et al. 1998; Jenkinson et al. 1997; Nduka et al. 2016; Ware Jr et al. 1996) and have been shown to be valid and reliable in the MLSFH (Ohrnberger et al. 2020). The last two rows of the first panel of Table 1 show the distributions of the change in the standardized SF12 physical and mental health scores between 2013 and 2017, whose means are mechanically equal to zero.
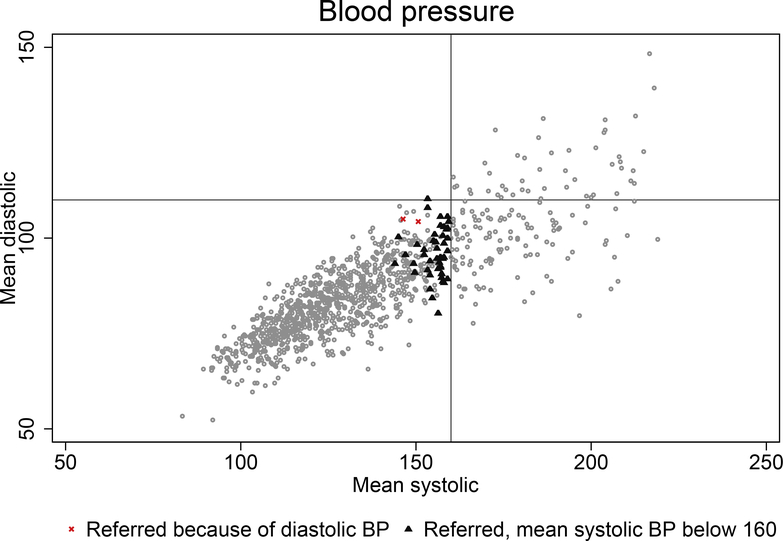
Figure 2 shows the distribution of mean values of systolic and diastolic blood pressure measurements in our sample. The vertical line along the x-axis represents the threshold that determines whether a respondent receives a referral letter because of a systolic measure above 160 and the horizontal line along the y-axis because of diastolic blood pressure at 110. Almost all study participants who received a referral letter did so because they had at least one systolic blood pressure measurement that exceeded the threshold of 160 mmHg. There are only two individuals in our sample who received a referral letter because at least one of their diastolic blood pressure measurements exceeded 110 mmHg while none of their systolic blood pressure measurements was 160 mmHg or above. These two individuals are represented by the two red x in the plot. In the empirical analysis, we exclude these 2 observations to include only respondents who received a referral letter because of their high level of systolic blood pressure. Corresponding graph using the respondents’ maximum systolic and diastolic blood pressure measurements instead of their respective mean can be found in the Appendix Figure A.3.
Figure 2: Blood pressure of respondents of the 2013 MLSFH survey.
Notes: The graphs shows average of the three measures of systolic and diastolic blood pressure for respondents of the 2013 MLSFH-MAC survey. Dots represents mean values of systolic (x-axis) and diastolic (y-axis) blood pressure. Small triangles represent individuals whose maximum systolic blood pressure is at least 160 but their mean systolic blood pressure is below 160. Small red x represent the individuals who were given a referral letter because their diastolic blood pressure is at least 110.
4. Methodology
The procedures implemented for providing a referral letter to study participants whose blood pressure measured above a specific threshold suggests the use of a sharp regression discontinuity design (RDD) as an appropriate application to evaluate the effects of the referral letter on hypertension-related outcomes. The method compares individuals whose maximum measurement of blood pressure is right below the cutoff (i.e., 160 mmHg systolic blood pressure) with those whose maximum measurement is right above it, assuming that individuals around the cutoff share similar observable and unobservable characteristics with the exception of having received a referral letter.13
The RDD specification benefits from strong internal validity whereas it potentially lacks external validity as it does not reveal much about what is happening away from the cutoff (Wing and Bello-Gomez 2018). The availability of multiple blood pressure measurements for each individual allows however to estimate the causal effects of receiving a referral letter on hypertension-related outcomes away from the critical cutoff. Indeed, one can use a nearest-neighbor matching estimator and match individuals based on similar blood pressure levels but where some had a maximum blood pressure above the critical threshold and hence received a referral letter and some other who did not fulfill the condition to receive such a referral letter. In particular, the proposed estimator matches individuals on the mean of the three systolic blood pressure measurements, with the average across measurements providing an estimator for the (unobserved) “true” blood pressure of individuals at the time of screening.
Estimating corresponding effects away from the cutoff allows to determine whether our RDD results hold for a different subset of the population (Angrist and Rokkanen 2015; Lee and Lemieux 2010; Mealli and Rampichini 2012), hence increasing the external validity of the findings. In our matching analysis, the mean systolic blood pressure of treated individuals ranges between 144 and 159.3, which allows to estimate the causal effects of the health screening substantially far away from the 160 cutoff. This could therefore be particularly relevant and informative to policy makers in the case they would consider lowering the threshold of the cutoff in a screening intervention for instance. Analyzing the effects of getting a referral letter away from the cutoff can also helps in identifying possible heterogeneous effects in the population along the distribution of blood pressure.
4.1. Sharp Regression Discontinuity Design (RDD)
We exploit the discontinuity in the probability of receiving a referral letter—the treatment D—that is assigned based on the maximum systolic blood pressure (= the score Xi). More formally, we observe n individuals, indexed by i = 1, 2, … , N whose systolic blood pressure was measured three times (s1i, s2i, s3i). Each respondent received a referral letter if max(s1i, s2i, s3i) = Xi ⩾ 160, with 160 being the cutoff determining treatment D. Because the assignment rule is in our setting, each unit complies perfectly with its assignment and thus treatment corresponds to a deterministic function of the score. Because of this deterministic decision rule at a precise cutoff, a sharp RDD design can be used to estimate the causal effects of receiving a referral letter on hypertension-related health outcomes.
The fundamental problem with causal inference in social sciences is that we only observe realized outcomes Yi and rarely potential outcomes (Holland 1986). In other words, we observe the health outcomes of those who received a referral letter and those who did not, but never their respective counterfactual outcomes. That is, we observe:
| (1) |
with Yi(0) the health outcomes of those who did not get a referral letter (= our control group) and Yi(1) the outcomes of those who got a referral letter (= our treatment group).14 However, as discussed in the RDD literature (Calonico et al. 2014b, 2019; Hahn et al. 2001), one can obtain average treatment effects at the cutoff, by comparing individuals just below and just above it and calculating the vertical distance between and . Hahn et al. (2001) showed that if the conditional expectation functions of Yi are continuous in x at x = c, then one can derive the average treatment effect at the cutoff τrd(c) as:
| (2) |
Because the true functional form of and is not known, we follow the recommendations of Skovron and Titiunik (2015) and nonparametrically approximate these regression functions with local polynomials of order 1.15 Furthermore, in our benchmark analysis, we use triangular weights determined by kernel functions and centered at the cutoff c to put more weights on observations closer to c,16 and restrict our analysis to observations that are between 160 − h− and 160 + h+ with h− and h+ representing bandwidths on each side of the cutoff.17 We allow these optimal bandwidths to be different on both sides of the cutoff c and present results in the Appendix where we restrict our analysis to use the same optimal bandwidths on both sides of the cutoff.18
Although not necessary for identification, we also estimate all our models with a set of exogenous/predetermined control variables to assess the robustness of our findings to the inclusion of covariates and potentially increase the precision of our estimates. The set of control variables consists of sex, age and region dummy variables to control for any systematic differences in the three regions where the MLSFH-MAC data are collected.
4.2. Matching strategy
Our matching strategy estimation of the treatment effect τ exploits the fact that treatment was determined based on the maximum of the three systolic blood pressure measurements, and not on the “true” systolic blood pressure, to estimate the causal effect of getting a referral letter away from the 160 cutoff. We do not observe the “true” blood pressure at the time of the interview but we proxy it with the average of the three measures Ri = mean(s1, s2, s3). Indeed, there are respondents in our sample who were treated and therefore received a letter because max(s1, s2, s3) = Xi ⩾ 160, but for whom their “true” blood pressure was lower than the cutoff. These respondents are represented by small triangles in Figure 2. This setup therefore allows us to implement a nearest-neighbor matching estimator (Abadie and Imbens 2002, 2006; Abadie et al. 2004) to estimate the causal effect of getting a referral letter on Yi away from the cutoff, by comparing outcomes of interests of those who were given a referral letter with those who were not, matching respondents with similar values of “true” blood pressure.
More formally, for this specific set of respondents, conditioning on the “true” blood pressure Ri, Di is random because Di is based on the maximum of the three measurements and is thus purely error-driven and independent to individual characteristics except Ri. By assuming that Ri can be measured by the mean of the three systolic measurements, that is Ri = mean(s1, s2, s3), one obtains {Yi(0),Yi(1)} ⫫ Di | Ri, which implies that conditioning on Ri, treatment Di is given at random and is therefore independent to potential outcomes.
It follows that one can estimate the potential counterfactual outcomes of each individual using information from the nearest neighbors in the opposite treatment group. That is, for each i, if Di = D, and otherwise, for D ∈ {0, 1}. In this relation, Ωi represents the set of individuals j in the neighborhood of i (as defined below) with Dj = 1 − Di and |.| the cardinality function. The average treatment effect on treated (ATET)19 can then be expressed as:
| (3) |
where we define, for our benchmark analysis, Ωi for each i as , where ∥.∥e represents the euclidean distance on R which has to be less than 10 mmHg for individual j to be in the neighborhood of individual i and K is the number of matches.20
To assess the quality of our matching, we report the average distance between our treated and untreated observations. We estimate our matching model in which individuals are matched based on a vector of characteristics x where x includes (1) only R, or (2) R, sex, region dummy variables and age (i.e. the same set of control variables we use in our RDD specification).21
It is possible that people might be different not only in terms on mean blood pressure but also in terms of variance. We may therefore be matching individuals with identical means but with very different variance. Because the mean itself is explained by the maximum value, which may or may not be systematically different across different individual characteristics, the mean systolic blood pressure measurements may not reflect the “true” underlying blood pressure of the individuals, such that the treatment, conditioning on the mean blood pressure, is not random as assumed. We therefore augment the specification in which we include our basic set of control variables by adding the standard deviation of the three systolic blood pressure measurements in our matching function. By doing so, we match individuals not only on their mean but also on the variance of their systolic blood pressure, therefore increasing the chance that individuals who are matched with one another are similar in terms of systolic blood pressure characteristics (not only the first but also the second moment of the systolic blood pressure distribution).
As robustness check, we present matching estimates when the “true” blood pressure R of respondents is based on the median of {s1, s2, s3} instead of the mean of these three measurements and when R is based on the mean of the last two measures (Leung et al. 2016). In all the results using our matching estimator, we report robust standard errors estimated using the number of matches (4 for our benchmark results, and 3 and 5 as robustness checks) in the neighborhood of each observation.
5. Results
We first present results derived from the application of the RDD approach followed by the corresponding results based on the matching specification. Specifically, we focus on the following effects of receiving a referral letter: (a) changes in the average systolic and diastolic blood pressures between 2013 and 2017, the probability of being hypertensive in 2017, the probability of having been diagnosed by a medical professional during a period of two years prior to the follow-up interview in 2017 and on the probability of taking blood pressure medication at the time of the interview; (b) corresponding estimates of the effects of referral cards on health behaviors such as diet and physical exercise and on high blood pressure-related knowledge; and (c) effects of the referral letter on overall subjective physical and mental health of the study participants.
5.1. Effects of receiving a referral letter—RDD estimates
a). Blood pressure and hypertension diagnosis/treatment:
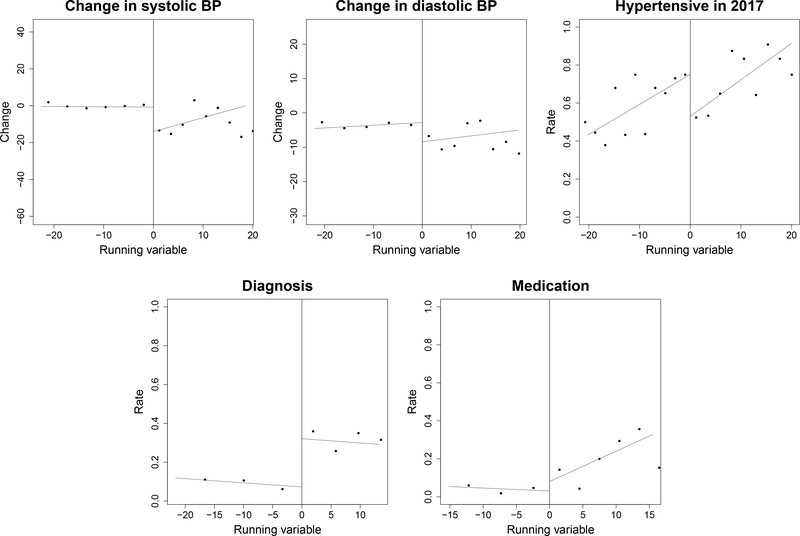
The left graph of Figure 3 plots the change in the mean systolic blood pressure between 2013 and 2017 with respect to the running variable, that is the maximum of the three systolic measurements taken in 2013 (x-axis). The bandwidths on both sides of the cutoffs are derived optimally using Mean Square Error (MSE) (Gelman and Imbens 2019; Skovron and Titiunik 2015), and triangular kernels to put more weight on observations closer to the cutoff.22 Each dot represents the averages of the respective outcome in a given bin.23 The solid line represents the predicted outcome based on those local polynomial regressions.
Figure 3: RDD estimates—Effects of receiving a referral letter on 2013–17 changes in blood pressure, on probability of being hypertensive, diagnosed with hypertension, or treated for hypertension in 2017.
Notes: The graphs show average blood pressure outcomes conditional on the maximum systolic blood pressure in 2013. Individuals located to the right of the vertical line received the referral card in 2013. The outcome in the top-left graph represent the average changes in systolic blood pressure from 2013 to 2017. The outcome in the top-middle graph is the average changes in diastolic blood pressure from 2013 to 2017. In the top-right graph, we define someone as being hypertensive if the mean of the three systolic or diastolic blood pressure measurements was greater or equal to 140 and 90, respectively. The outcome in the bottom-left graph is whether individuals got diagnosed by a medical professional in the two years prior to 2017. The outcome in the bottom-right graph is whether individuals are currently taking medication during the follow-up survey in 2017. We employed Mean Square Error (MSE) optimal bandwidth selector and generated the plots above using first order local-polynomial and triangular kernels. Bins are derived optimally using variance evenly-spaced method using spacing estimators (Calonico et al. 2014a,b, 2015, 2017). Each dot represents the means of the respective outcome in a given bin.
The causal effects of receiving a referral letter on the outcome variables are represented in Figure 3 by the vertical distance between the two different solid lines at the cutoff (running variable Xi = 0). The top-left plot shows a drop of about 13 mmHg in the changes in systolic blood pressure between 2017 and 2013 at the cutoff, reflecting that an individual who received a referral letter and whose maximum systolic blood pressure was just above the cutoff had a mean systolic blood pressure in 2017 that was on average 13 mmHg lower than those who were right below the cutoff. A corresponding drop in blood pressure can also be observed in the changes in diastolic blood pressure (top-middle plot), where individuals at the right of the cutoff appear to have a diastolic blood pressure to be on average about 5 mmHg lower than their counterparts located on the left of the cutoff. The top-right graph shows that getting a referral letter in 2013 did not only lower blood pressure, but also reduced their probability of being hypertensive in 2017 (hypertension is indicated if the mean of the three systolic or diastolic blood pressure measurements was greater or equal to 140/90). A large discontinuity at the cutoff can also be observed when looking at whether respondents were diagnosed with hypertension during the two years prior to the follow-up interview in 2017. Indeed, the bottom-left plot in Figure 3 shows a discontinuous increase of about 0.24 points in the probability of being diagnosed as a result of receiving a referral letter for those at the cutoff24. The effect of the referral card on medication is less pronounced and the discontinuity at the cutoff on whether respondents are currently taking medication is, if any, small (bottom-right plot).
Table 2 presents the corresponding estimated coefficients of the causal effects of receiving a referral letter on our five main outcomes of interests using our RDD specification. The estimates use first order polynomial and allow the sizes of the optimal bandwidths on both sides of the cutoff to be different. The first row of Panel A of Table 2 shows that those who received a referral letter in 2013 had a change in systolic blood pressure (between 2013 and 2017) that was about 12.9 mmHg lower (p-value = 0.03) than those who did not receive a letter. This effect is statistically significant at 95%, and slightly higher (14.3, p-value=0.016) with the inclusion of our basic set of predetermined control variables sex, age and region (second row of each panel). Similar effects on blood pressure can be observed on changes in mean diastolic blood pressure, where individuals who received a letter had an average decrease in diastolic blood pressure of about 5.5 mmHg (p-value=0.053) and 5.8 mmHg (p-value=0.034) depending on whether our set of control variables are included in the specification or not. Panel C of the same table also confirms the results shown in Figure 3: individuals who received a referral letter in 2013 were about 20 percentage points less likely to be hypertensive in 2017 as compared to those who did not receive such letter and whose maximum systolic blood pressure was just below the 160 cutoff. This effect is particularly precisely estimated in the specification in which the set of predetermined controls are included in the model (p-value=0.044)
Table 2:
RDD estimates-Effect of the referral letter on 2013-17 change in systolic and diastolic blood pressure, and probability of being hypertensive, diagnosed with hypertension, and treated for hypertension in 2017
| Specification | Effects | Std. errors | P-values | OB- | OB+ | N- | N+ |
|---|---|---|---|---|---|---|---|
| A. Change in systolic blood pressure 2013–17 | |||||||
| Linear | −12.88** | 5.947 | 0.030 | 23.57 | 18.43 | 312 | 108 |
| Linear with controls | −14.28** | 5.952 | 0.016 | 21.30 | 18.72 | 275 | 107 |
| B. Change in diastolic blood pressure 2013–17 | |||||||
| Linear | −5.503* | 2.849 | 0.053 | 22.60 | 19.32 | 294 | 109 |
| Linear with controls | −5.790** | 2.730 | 0.034 | 20.33 | 21.66 | 256 | 115 |
| C. Probability of being hypertensive in 2017 | |||||||
| Linear | −0.199* | 0.114 | 0.079 | 20.403 | 19.734 | 260 | 109 |
| Linear with controls | −0.225** | 0.112 | 0.044 | 20.693 | 19.981 | 256 | 108 |
| D. Diagnosed with hypertension in 2017 | |||||||
| Linear | 0.241** | 0.106 | 0.023 | 22.22 | 13.29 | 294 | 87 |
| Linear with controls | 0.201** | 0.101 | 0.046 | 19.25 | 14.50 | 229 | 90 |
| E. Treated for hypertension in 2017 | |||||||
| Linear | 0.045 | 0.073 | 0.538 | 16.15 | 15.56 | 192 | 96 |
| Linear with controls | 0.038 | 0.072 | 0.598 | 14.89 | 15.53 | 160 | 95 |
Notes: The table shows estimates of the effect of receiving a referral card in 2013 on blood pressure related outcomes using a regression discontinuity design. Change in systolic blood pressure is the difference between the average of the three systolic blood pressure measures in 2017 and in 2013. Change in diastolic blood pressure is the difference between the average of the three diastolic blood pressure measures in 2017 and in 2013. We define someone as being hypertensive if the mean systolic or diastolic blood pressure measurements was greater or equal to 140 and 90, respectively. Diagnosis is a dummy equal to 1 if the respondent has been diagnosed by a medical professional in the last two years (2017 survey). Medication is a dummy equal to 1 if the respondent is currently taking medication for blood pressure (2017 survey). All these specifications use triangular weights and first order local polynomials. OB- and OB+ represent the optimal bandwidths below and above the cutoffs, respectively. N- and N+ represent the number of observations included in the optimal bandwidths below and above the cutoffs, respectively. The change in systolic and diastolic blood pressure is mean(x1, x2, x3)2017 -mean(x1, x2, x3)2013 with x = {systolic, diastolic}. We use a Mean Square Error (MSE) optimal bandwidth selector. Specifications with controls includes a sex dummy, age and region dummies.
p < 0.1,
p < 0.05,
p < 0.01.
One possible explanation for the improvement in these blood pressure outcomes is that individuals who received a referral letter indeed followed up with a health care provider regarding their high blood pressure levels. In Panel D of Table 2 we therefore show the effects of getting a referral letter in 2013 on the probability of being diagnosed as hypertensive by a medical professional in the two years preceding the 2017 interview. For individuals located at the cutoff, receiving a referral letter caused an increase in the probability of being diagnosed by about 24.1 percentage points (p-value = 0.023). Again, this effect is significant and robust to the inclusion of various control variables.25
People who get diagnosed by a doctor or a nurse should in theory receive treatment and advice on how to control their blood pressure with appropriate health behavior changes such as adoption of better diet and increase in physical activity, as is commonly recommended in developed countries. The causal effects of receiving a referral letter on the probability of currently taking medication (Panel E) is about 4.5 percentage points, but fails to be precisely estimated at conventional statistical levels. One possible explanation for this absence of a significant effect is that the study asks whether respondents are currently taking medication but we do not know if they have been taking medication at some point in time between 2013 and 2017. It could also be due to traditional cultural beliefs and weak health care systems for hypertension primary care in SSA that make individuals turn away from “standard” high BP medication and use traditional herbal medicine instead, which is still widely used in SSA (Liwa et al. 2014).
Table A.1 in the Appendix shows that our results in Table 2 are not driven by the choice of the polynomial order we use. Indeed, the effects appear very similar when using local polynomials of order two. The effects on the changes in systolic blood pressure range from −14 to −15 when using a quadratic specification, as compared to −12.9 and −14.3 in our benchmark specification. The effects on the probability of being hypertensive in 2017 are similar in magnitude as well, although less precisely estimated. The effects on diagnosis and on medication when allowing for more flexible specification are also in the ballpark of those obtained in our linear specification. Moreover, while our benchmark specification uses triangular kernels to put more weight on observations closer to the cutoff, Table A.2 in the Appendix shows that our results are robust to using rectangular weights, which weight all observations within the optimal bandwidths equally. We also investigate whether our results hold when we impose the optimal bandwidths on both sides of the cutoff to be equal. Table A.3 in the Appendix shows that this is the case. In the same vein, Table A.4 shows that our results hold when the optimal bandwidth for systolic blood pressure is used for all the other outcomes. These robustness checks show that our results are therefore not driven by the choice of the sample taken into consideration in our analysis. Finally, Tables A.5 and A.6 in the Appendix check for the potential confounding of the cutoff that determines treatment by estimating the placebo effects that take place 3 mmHg below and above the actual cutoff (160). As we would expect at these placebo cutoffs, the treatment effects at these two hypothetical cutoffs are not statistically significant at conventional levels.
b). Health behaviors and knowledge:
While our RDD strategy suggests some important causal effects of receiving a referral letter on hypertension-related health outcomes, it is of particular interest to better understand the pathways through which these effects operate and especially if health behaviors other than diagnosis and medication play a role. Specifically, we investigate whether receiving a referral letter also had an effect on diet. Changes in health behaviors such as diet and eating habits for instance are possible channels through which the referral letter can have an effect on blood pressure. The consumption of salt and sugar-sweetened beverages for instance have been shown to be strongly associated with higher blood pressure and the incidence of hypertension (Cappuccio and Miller 2016; He and MacGregor 2016; Malik et al. 2014).
Table 3 shows that although receiving a referral letter seems to have reduced the probability of adding extra salt to one’s plate, this effect is not precisely estimated at conventional statistical levels. Opposite to what one would expect, the referral letter has had positive effects on the probability of consuming sweet drinks in a given day and on the total number of teaspoons of sugar individuals consume in a given day in their tea or coffee. Individuals who received a referral letter were about 12 percentage points more likely to consume a sweet drink in a given day and also consumed about half a spoon more of sugar in their hot beverage per day as compared to others. These effects fail to be statistically significant, which suggests that referral letters have not had any effects on change in diet, possibly because diet recommendations are not given or are difficult to follow by respondents diagnosed with hypertension.
Table 3:
RDD estimates-Effect of the referral letter on pathways for changing blood pressure during 2013-17
| Specifications | Effects | Std. errors | P-values | OB- | OB+ | N- | N+ |
|---|---|---|---|---|---|---|---|
| Pathways 1: Health Behaviors | |||||||
| A. Extra salt to plate | |||||||
| Linear | −0.127 | 0.134 | 0.345 | 12.38 | 21.06 | 136 | 117 |
| Linear with controls | −0.130 | 0.131 | 0.322 | 12.70 | 23.50 | 133 | 122 |
| B. Consume sweet drinks | |||||||
| Linear | 0.119 | 0.111 | 0.282 | 20.95 | 14.69 | 260 | 91 |
| Linear with controls | 0.127 | 0.110 | 0.248 | 21.94 | 14.10 | 275 | 90 |
| C. Total number of teaspoons of sugar used in teal coffee per day | |||||||
| Linear | 0.539 | 0.485 | 0.267 | 14.782 | 23.754 | 163 | 123 |
| Linear with controls | 0.489 | 0.457 | 0.285 | 14.174 | 21.616 | 160 | 116 |
| D. Change in zveekly MET score | |||||||
| Linear | −60.971 | 39.124 | 0.119 | 12.23 | 16.43 | 134 | 101 |
| Linear with controls | −56.842 | 37.02 | 0.125 | 12.80 | 17.61 | 132 | 102 |
| Pathways 2: Knowledge | |||||||
| A. Know about HBP | |||||||
| Linear | −0.025 | 0.100 | 0.800 | 25.03 | 16.06 | 336 | 102 |
| Linear with controls | −0.050 | 0.102 | 0.628 | 24.58 | 15.70 | 320 | 95 |
| B. Know symptoms | |||||||
| Linear | 0.042 | 0.123 | 0.729 | 20.246 | 13.462 | 260 | 87 |
| Linear with controls | 0.019 | 0.127 | 0.881 | 18.339 | 13.621 | 214 | 86 |
| C. Know about treatment | |||||||
| Linear | −0.032 | 0.121 | 0.792 | 18.04 | 13.72 | 218 | 87 |
| Linear with controls | −0.104 | 0.124 | 0.400 | 16.74 | 12.24 | 188 | 82 |
Notes: The table shows estimates of the effect of receiving a referral card in 2013 on diet and knowledge about hypertension in 2017 using a regression discontinuity design. Extra salt to plate and consumption of sweet drinks are dummies. The knowledge measures are dummies based on whether they know what high blood pressure is, whether they are able to name at least one of its symptoms and whether they now that having high blood pressure required life-long treatment. All these specifications use triangular weights and first order local polynomials. OB- and OB+ represent the optimal bandwidths below and above the cutoffs, respectively. N- and N+ represent the number of observations included in the optimal bandwidths below and above the cutoffs, respectively. We use a Mean Square Error (MSE) optimal bandwidth selector. Specifications with controls includes a sex dummy, age and region dummies. “MET” stands for metabolic equivalent of task and it is a measure of physical activity.
p < 0.1,
p < 0.05,
p < 0.01.
Our analysis further shows a negative causal effects of receiving a referral letter on physical activity, as evidenced in Panel D of Table 3.26 The coefficient associated to MET score equals −61 in the linear specification without controls, which corresponds to a decrease of about 8 hours of vigorous physical activity per week (≈ −61/7.5), or about 70 minutes per day. While negative, these effects again fail to be precisely estimated. However, when we focus on vigorous activity (Table A.7), we do find a negative effect significant at the 10% level.
These results suggest that, as opposed to changes in behaviors that are commonly recommended for those with hypertension in developed countries (i.e., increasing physical activities), this is not a likely pathway through which respondents who received a referral letter achieve a reduction in their blood pressure levels. While it is impossible to identify the specific reasons why this is the case, one possible explanation is that the study population is indeed physically quite active, with strenuous agricultural labor present in their daily life and hence little space for improvement in physical activity.
Further analyses show that referral letters did not have any effect on hypertension-related knowledge such as high blood pressure treatments and symptoms. Indeed, the lower part of Table 3 shows that individuals at the cutoff who received a referral letter did not have a higher probability of knowing what high blood pressure was, nor were they more likely to know the characteristics of the symptoms of hypertension and to know that having high blood pressure required life-long treatment. This is not surprising since our descriptive statistics in Table 1 showed that on average this population is aware of what hypertension is and its consequences.
c). Overall subjective health:
Table 4 shows the effects of the referral letter on two indicators of respondents overall subjective health: the SF12 subjective physical and mental health score. Our main specification focuses on changes in the standardized SF-12 subjective physical and mental health score between 2013 and 2017, and we observe an increase of about half a standard deviation in both the SF-12 subjective physical and mental health scores. These results are very similar when we include the set of predetermined control variables (age, sex and region). The results are statistically significant for mental health (p-value = 0.04 when including controls) and close to be marginally significant for the physical health score (p-value = 0.1). Although our results show no statistically significant effects on changes in diet and negative effects on physical activity, these estimates indicate that individuals either realize that a drop in their blood pressure is a positive improvement in their health or that they are taking steps to improve their health in ways we do not fully observe. Importantly, we do not find a negative effect of giving referral letters on mental health, as measured by the change in PHQ-9 score,27 which could have been an ex-ante concern of this type of screening. We also do not find any effect on subjective 5-year survival expectations (last rows of Table 4).28
Table 4:
RDD estimates-Effect of the referral letter on overall health status
| Specifications | Effects | Std. errors | P-values | OB- | OB+ | NT- | N+ |
|---|---|---|---|---|---|---|---|
| A. Change in standardized SF12 physical score 2013–17 | |||||||
| Linear | 0.529 | 0.323 | 0.101 | 21.29 | 13.49 | 273 | 85 |
| Linear with controls | 0.510 | 0.311 | 0.101 | 21.98 | 13.63 | 273 | 85 |
| B. Change in standardized SF12 mental score 2013-17 | |||||||
| Linear | 0.511* | 0.284 | 0.072 | 19.04 | 23.00 | 227 | 121 |
| Linear with controls | 0.568** | 0.279 | 0.042 | 19.46 | 22.21 | 227 | 119 |
| C. Change in 5-year survival expectation | |||||||
| Linear | −0.089 | 0.096 | 0.352 | 21.04 | 26.82 | 260 | 124 |
| Linear with controls | −0.016 | 0.097 | 0.872 | 17.91 | 25.55 | 189 | 121 |
Note: The table shows estimates of the effect of receiving a referral card in 2013 on health in 2017 using a regression discontinuity design. SF12 subjective physical and mental health scores are constructed using twelve questions about general health status, mobility and ability to perform daily activities as well as emotional health. 5-year survival expectation is the subjective probability of survival in 5 years elicited using a methodology developed by Delavande and Kohler (2009). All these specification use triangular weights and first order local polynomials. OB- and OB+ represent the optimal bandwidths below and above the cutoffs, respectively. N- and N+ represent the number of observations included in the optimal bandwidths below and above the cutoffs, respectively. We use a Mean Square Error (MSE) optimal bandwidth selector. Specifications with controls includes a sex dummy, age and region dummies.
p < 0.1,
p < 0.05,
p < 0.01.
Finally, the first panel of Table A.8 in the Appendix shows that individuals who received a referral letter at the cutoff did not have a higher probability of dying between 2013 and 2017.29 Having received a referral card does not seem to have any impact on attrition either,30 as we show that receiving a referral letter in 2013 did not increase the probability of not participating in the interview in 2017 due to refusals, hospitalizations or temporarily absence or because of migration. Our analysis therefore does not appear to suffer from sample selection in the follow-up survey.
5.2. Effect of receiving a referral letter—Matching/nearest-neighbor estimates
Our matching/nearest-neighbor approach for estimating the causal effect of a referral letter matches treated and untreated individuals based on the mean of their three systolic blood pressure measurements. A total of 46 individuals had mean systolic blood pressure below 160 the cutoff for receiving a referral letter, but they received one because their maximum recorded blood pressure reading exceeded 160/110. These respondents constitute the “treatment group,” and are matched with up to 161 nearest-neighbor respondents as control group. A minimum of 4 matches is used for each individual who received a referral letter and whose mean systolic blood pressure was below 160. The average value of the mean systolic blood pressures of the individuals in our treatment group is equal to 155.4, with a minimum of 144 and a maximum of 159.3; in the control group, corresponding numbers are equal to 146.8, 140 and 157, respectively.31
a). Blood pressure and hypertension diagnosis/treatment:
Table 5 shows that individuals who received a referral letter experienced a change in systolic blood pressure of about −12 mmHg when including our set of control variables along with the standard deviation of the three measurements (p-value=0.02) and −6.4 mmHg in diastolic blood pressure (p-value=0.01). These effects are rather similar in the specifications in which individuals are matched on their mean systolic blood pressure and our set of basic predetermined control variables only, although they are less precisely estimated. Similarly, our results indicate negative effects on the probability of being hypertensive in 2017 and these effects are along the lines to those reported in our RDD specification, albeit smaller and again not precisely estimated in the specifications in which standard deviation is excluded from the matching score. When it is included, the effect appears to be larger than our RDD estimates and precisely estimated however. The effects on the probability of having been diagnosed with hypertension is about 27.7 percentage points when the matching is based only on the mean of the three measurements and 21–22 percentage points when we add our set of control variables in the matching score. It is worth noting that the ATET on both changes in systolic/diastolic blood pressure and on the probabilities of being hypertensive and diagnosed in 2017 are very similar to our RDD results. This would indicate that the effects of receiving a referral letter are rather constant along the range of blood pressure between 140 and 160 mmHg.
Table 5:
Matching/nearest neighbor estimates-Effect of receiving a referral letter on change in blood pressure, diagnosis and use of medication
| Change in systolic blood pressure 2013–17 | Change in diastolic blood pressure 2013–17 | Prob. of being hypertensive (2017) | Diagnosis (2017) | Medication (2017) | |
|---|---|---|---|---|---|
| No controls | |||||
| ATET | −8.484 | −2.817 | −.196 | .277*** | .117** |
| P-value | .321 | .365 | .171 | .000 | .023 |
| Obs. | 207 | 207 | 207 | 207 | 207 |
| Average distance | 1.21 | 1.21 | 1.21 | 1.21 | 1.21 |
| With controls | |||||
| ATET | −9.810* | −2.270 | −.122 | .225*** | .132** |
| P-value | .078 | .354 | .217 | .005 | .010 |
| Obs. | 204 | 204 | 204 | 204 | 204 |
| Average distance | .984 | .984 | .984 | .984 | .984 |
| With controls + SD | |||||
| ATET | −12.63** | −6.394** | −.374*** | .207** | .136*** |
| P-value | .024 | .010 | .000 | .011 | .009 |
| Obs. | 204 | 204 | 204 | 204 | 204 |
| Average distance | 1.59 | 1.59 | 1.59 | 1.59 | 1.59 |
Note: The table shows Average Treatment Effects on Treated (ATET) estimates of receiving a referral card in 2013 on blood pressure related outcomes using a matching estimator. Change in systolic blood pressure is the difference between the average of the three systolic blood pressure measures in 2017 and in 2013. Change in diastolic blood pressure is the difference between the average of the three diastolic blood pressure measures in 2017 and in 2013. We define someone as being hypertensive if the mean systolic or diastolic blood pressure measurements was greater or equal to 140 and 90, respectively. Diagnosis is a dummy equal to 1 if the respondent has been diagnosed by a medical professional in the last two years (2017 survey). Medication is a dummy equal to 1 if the respondent is currently taking medication for blood pressure (2017 survey). We restrict the number of matches to be at least 4 and match respondents based on their mean systolic blood pressure in 2013, limiting the distance for possible matches to be at most 10. “Distance” represent the mean of the average distances between each observation and their matches. “With controls” includes a sex dummy, age and region dummies.
p < 0.1,
p < 0.05,
p < 0.01.
In contrast to the RDD results, our matching analysis suggests a statistically significant and positive effect on the probability of taking medication. The last column of Table 5 shows that individuals who received a referral letter were about 11.7 percentage points (p-value = 0.02) more likely to be taking medication than others in our specification without controls and 13.2 percentage points (p-value = 0.01) when we match individuals based on our set of control variables. The effects are very similar once the standard deviation of the three measurements are also included in the matching function (13.6 percentage points, p-value = 0.01). These effects are about twice larger than those reported in our RDD setting. One possible explanation could stem from the fact that the effects of our matching specification presented in Table 5 uncovers the average treatment effect on treated individuals with “true” levels of blood pressure that are different from the “true” levels of blood pressure of individuals whose maximum systolic measurement is at the cutoff. Therefore, it is not surprising that our results can potentially be qualitatively similar but differ in magnitude and statistical power across our two different econometric strategies.
To assess the quality of our matching, we computed the average distance in the mean systolic blood pressure between treated individuals and their nearest neighbors that are used in the estimation. A short average distance between these two groups would indicate that they are similar in terms of mean systolic blood pressure and therefore comparable. In our benchmark analysis without any controls, the average distance in systolic blood pressure between treated and untreated individual is about 1.21 mmHg, suggesting that our treated individuals are indeed matched with comparable individuals in terms of mean systolic blood pressure.
Table A.9 in the Appendix shows that our results are similar when increasing or decreasing the number of minimum matches to 5 and 3, respectively, instead of 4. Expanding or reducing the distance between the mean blood pressures to be at maximum 12, or 8 and 5 units, respectively, instead of 10 results in similar average treatment effects on the treated as well (Tables A.10, A.11 and A.12 in the Appendix). Moreover, we investigate whether our results hold when assuming that the “true” systolic blood pressure is proxied by the median of the three blood pressure measurements instead of the mean. Because the mean is correlated with the maximum value whereas the median is not, matching treated and untreated individuals based on their median systolic blood pressure could better reflect the actual effect of getting a referral letter by comparing individuals that are more similar in terms of their “true blood” pressure. Table A.13 in the Appendix shows that the results are once again very similar. Conclusion is similar when we consider the last two systolic blood pressure measurements instead of the three we have at hand. As the first blood pressure measurement could be more prone to measurement error and less reflect the “true” underlying blood pressure of individuals, due to stress, anxiety and so on, taking into account only the last two measurements could potentially better represent individual’s “true” blood pressure. We show in Table A.14 of the Appendix that our results are robust to that restriction as well, albeit less precisely estimated in the case of change in diastolic blood pressure. 32
b). Health behaviors and knowledge:
As it was the case in our RDD analysis, we investigate the pathways through which the referral letters could have had an effect on change in blood pressure. Tables 6 present the corresponding matching estimates of the ATET of getting a referral letter on the various pathways discussed above. Again, our matching analysis suggests no statistically significant changes in high blood pressure-related knowledge. Our results do suggest however a change in health behaviors. More specifically, while receiving a referral card did not have any effect on the probability of adding extra salt to one’s plate and on consuming sweet drinks in a given day, our results indicate that individuals who received a referral letter consume more teaspoons of sugar in their tea or coffee per day than others (about 1 teaspoon depending on the specification). They were also more likely to decrease their physical activity between 2013 and 2017, as evidenced in the last column of Table 6.33 These results are in line with those obtained in our RDD specification, although they are precisely estimated in our matching analysis whereas they were not as precise in our RDD strategy.
Table 6:
Matching/nearest neighbor estimates-Effect of receiving a referral letter on hypertension knowledge and diet
| Knowledge | Health Behaviors | ||||||
|---|---|---|---|---|---|---|---|
| Know about HBP | Know symptoms | Know about treatment | Extra salt to plate | Consume sweet drinks | # teaspoons sugar used in tea/coffee per day | Change in weekly MET score | |
| No controls | |||||||
| ATET | .115 | .072 | .056 | −.018 | .099 | .765 | −44.1 |
| P-value | .473 | .663 | .714 | .885 | .514 | .120 | .100 |
| Obs. | 207 | 207 | 207 | 207 | 207 | 207 | 204 |
| Average distance | 1.21 | 1.21 | 1.21 | 1.21 | 1.21 | 1.21 | 1.23 |
| With controls | |||||||
| ATET | −.077 | −.115 | .009 | −.213* | .067 | 1.30*** | −77.9** |
| P-value | .260 | .273 | .920 | .051 | .423 | .001 | .005 |
| Obs. | 204 | 204 | 204 | 204 | 204 | 204 | 202 |
| Average distance | .984 | .984 | .984 | .984 | .984 | .984 | .995 |
| With controls+SD | |||||||
| ATET | −.071 | −.126 | .09 7 | −.094 | −.029 | .923** | −137*** |
| P-value | .303 | .193 | .291 | .358 | .733 | .010 | .000 |
| Obs. | 204 | 204 | 204 | 204 | 204 | 204 | 202 |
| Average distance | 1.59 | 1.59 | 1.59 | 1.59 | 1.59 | 1.59 | 1.59 |
Notes: The table shows Average Treatment Effects on Treated (ATET) estimates of receiving a referral card in 2013 on knowledge about hypertension and diet in 2017 using a matching estimator. The knowledge measures are dummies based on whether they know what high blood pressure is, whether they are able to name at least one of its symptoms and whether they know that having high blood pressure required life-long treatment. Extra salt to plate and consumption of sweet drinks are dummies. We restrict the number of matches to be at least 4 and match respondents based on their mean systolic blood pressure in 2013, limiting the distance for possible matches to be at most 10. “Distance” represent the mean of the average distances between each observation and their matches. “With controls” includes a sex dummy, age and region dummies. “MET” stands for metabolic equivalent of task and it is a maeasure of physical activity.
p < 0.1,
p < 0.05,
p < 0.01.
These results are surprising because they go against the usual “Western” recommendations to treat high blood pressure. While usual recommendations in developed countries advocate a decrease in salt and sugar consumption, in conjunction with increase in physical activity, individuals who received a referral letter do not seem to follow these guidelines in this context. While it is not possible to find a precise reason for this behavior, possible explanations are: 1) presence of a substitution effect of medication, where individuals rely on medical treatment rather than behavior changes to control their blood pressure; 2) given the very poor context characterized by dietary restrictions, individuals cannot “afford” to change their diets; 3) given the high intensity agricultural labor context, individuals are physically active on a daily basis and there is little “room” to make further improvements.
c). Overall subjective health:
Table 7 shows the effects of receiving a referral letter on subjective physical and mental health SF12 scores and 5-year survival expectation. Results on these three outcome variables are not consistent across the different specifications and it is therefore hard to draw any hard evidence on the effects of the referral card on subjective health based on the matching specification. The fact that the significant effects reported in the first row of Table 7 disappear once we include our basic set of control variables in the matching function suggest that the differences in subjective health among treated and non treated individuals are mainly driven by differences in sex, age and region. Finally, the second panel of Table A.8 shows that receiving a referral letter did not have any statistically significant effect on the probability of dying between 2013 and 2017, nor has it had any impact on attrition. This confirms the RDD results presented before that our analysis is not biased due to sample selection.
Table 7:
Matching/nearest neighbor estimates-Effect of receiving a referral letter on overall subjective health
| Change in standardized SF12 physical score 2013–17 | Change in standardized SF12 mental score 2013–17 | Change in 5-year survival expectation 2013–17 | |
|---|---|---|---|
| No controls | |||
| ATET | .729** | .588* | −.326** |
| P-value | .046 | .072 | .026 |
| Obs. | 201 | 201 | 190 |
| Average distance | 1.239 | 1.239 | 1.308 |
| With controls | |||
| ATET | .070 | .200 | −.039 |
| P-value | .757 | .476 | .656 |
| Obs. | 201 | 201 | 190 |
| Average distance | 1.000 | 1.000 | 1.031 |
| With controls + SD | |||
| ATET | −.013 | .111 | .033 |
| P-value | .954 | .690 | .688 |
| Obs. | 201 | 201 | 190 |
| Average distance | 1.603 | 1.603 | 1.641 |
Note: The table shows Average Treatment Effects on Treated (ATET) estimates of receiving a referral card in 2013 on health in 2017 using a matching estimator. SF12 subjective physical and mental health scores are constructed using twelve questions about general health status, mobility and ability to perform daily activities as well as emotional health. 5-year survival expectation is the subjective probability of survival in 5 years elicited using a methodology developed by Delavande and Kohler (2009). We restrict the number of matches to be at least 4 and match respondents based on their mean systolic blood pressure in 2013, limiting the distance for possible matches to be at most 10. “Distance” represent the mean of the average distances between each observation and their matches. “With controls” includes a sex dummy, age and region dummies.
p < 0.1,
p < 0.05,
p < 0.01.
6. Conclusions
This study is the first to provide estimates of the long-term causal effects on health outcomes of a population-based NCD-focused health screening in a SSA low-income population. Filling this knowledge gap is critical because of NCD screening interventions have been heralded as a critical component of possible responses to the emerging NCDs epidemic in LMICs (Geldsetzer et al. 2019; Islam et al. 2014; WHO 2013a). Specifically, we analyze the effects of a referral letter given to at-risk individuals in Malawi who were measured with high blood pressure and therefore face a heightened likelihood of CVDs. Comparing individuals whose blood pressure was just above the cutoff that determines whether a referral letter is given to those just below that cutoff, we are able to identify the causal effects of at-risk individuals receiving a referral letter. Outcomes of interest are measured four years after the screening, and include hypertension as well as health behavior and subjective health indicators.
A summary of the main results is presented in Table 8. Our analysis shows that screening was effective in reducing both systolic and diastolic blood pressure among at-risk individuals. Our findings indicate that individuals who received a referral letter in 2013 were also less likely to be hypertensive in the follow-up survey four years later in 2017. We also show that at-risk individuals were more likely to be diagnosed as hypertensive by a medical professional as a result of getting the referral letter, and we find evidence that they were also more likely to be taking medication for blood pressure at the time of the interview. Our key findings are robust to various sample selections and econometric methods, which reinforces both the internal and external validity of our findings, the latter being particularly relevant to policy makers.
Table 8:
Summary of the causal effects found in this study
| Blood pressure | Hypertension | Diagnosis | Medication | Knowledge | Risky health behaviors | Subjective health | |
|---|---|---|---|---|---|---|---|
| RDD | ⇓ | ⇓ | ⇑ | – | – | – | ↑ |
| Matching | ⇓ | ⇓ | ⇑ | ⇑ | – | ↑ | – |
Note: Upwards (downwards) double arrows show the presence of positive (negative) and statistically significant effects at conventional levels (p-value=0.05). Upwards (downwards) arrows show the presence of positive (negative) and statistically significant effects at conventional levels on some dimensions of the characteristics considered. Dashes represent lack of statistically significant effects or not consistent/ambiguous effects across specifications.
A “back-of-the-envelope” calculation suggests that the blood pressure screening and referral letter may have averted approximately three deaths by 2018/19 among about 1,200 mature adults who were screened at baseline in 2013.34 While we acknowledge that this estimate of the number of lives saved needs to be interpreted with considerable caution, it compares favorably to the cost of a door-to-door blood pressure screening campaign for 1,200 mature adults would only cost around US$1,200 in wages assuming each counselor screens 20 people per day.35 Our analyses thus support earlier conclusions—albeit not based on causal inference designs—that suggest a likely cost-effectiveness of blood pressure screening in lower-middle-income countries (Nguyen et al. 2016; Rosendaal et al. 2016), and our analyses suggest that this cost-effectiveness of blood pressure screening extends to low-income contexts where high blood pressure may be more likely to underdiagnosed.
Our study also shows that individuals do not seem to modify other health behaviors that could reduce blood pressure such as lowering their consumption of salt and sugar. Although this might initially be surprising, it is consistent with several aspects of the local LIC context. For example, individuals, including persons at elevated risk of CVDs, may have very limited options in adjusting their health behaviors along these margins. Hypertension is also driven by distinctive risk factors (e.g., obesity and Western diets continue to be rare; see Kohler et al. 2018b), therefore rendering conventional behavioral responses less effective. In addition, behavioral guidelines for the treatment of hypertension are developed mostly on research from high- and middle-income countries, and are often not adopted to the realities of LIC contexts.
If anything, we observe a behavioral response that is the opposite to what one would expect given the current “Western” recommendations in terms of high blood pressure management. Our findings suggest that at-risk individuals who receive a referral letter tend to consume more sugar and are less physically active. While the precise reasons for these behavioral changes related to diet and physical activity are difficult to determine, several possible explanations exist. For instance, this could be due to a substitution effect, with individuals relying on medical treatment rather than behavior changes to control their blood pressure. Alternatively, given an overall unbalanced and calorie-restricted diet, individuals may also be very limited in their options to make any changes in their food consumption, and recommendations to reduce specific food consumption may even be perceived counterfactual. Due to the high intensity of agricultural labor, being physically active is also part of individuals’ daily routine with only limited abilities for further improvement. Interestingly, and consistent with our finding that at-risk individuals are less active after receiving a referral latter, 80% of respondents in our sample reported that their blood pressure was indicative of the amount of work they can perform. While this can indeed be true for individuals suffering from very high blood pressure, knowing one’s blood pressure level is generally not informative on the amount of work one can perform.
The long-term effects of receiving a referral letter pertain not only to hypertension per se, but have spillover effects on other health dimensions. Specifically, we find some evidence that at-risk individuals who received a referral letter perceived their mental health more favorably than others. The effects are statistically significant only in the RDD specification, but we can at least rule out any negative effects of learning about having high blood pressure on subjective health. We were also not able to clearly identify which factors above and beyond the increase in the use of hypertension medications can explain this pattern.
Overall, our findings are important in that they document the effectiveness of a simple and inexpensive population-based health screening that resulted in sustained increases in health-seeking behaviors for NCDs among at-risk individuals in a rural LIC context. Similar to related findings about preventive versus curative health care seeking among the poor (Banerjee and Duflo 2011), our study thus shows that individuals seem to be willing to spend time and effort to treat NCDs (in our case, through hypertension medication), but they are less willing to modify their habits and day-to-day routines as risk-reduction strategies to prevent or delay the onset of such NCDs. Given the lack of conventional risk factors for hypertension in SSA LICs, the behavioral responses to high blood pressure are not fully clear from a public health/biomedical perspective. On the one hand, recommendations from the Western context, like losing weight or increasing physical activity, are not necessarily the appropriate recommendations in LICs. Other recommendations like reduction in salt consumption may be hard to follow, as salt use is probably deeply ingrained in the local food culture and may also play important roles in the preservation of food. On the other hand, the possibilities of at-risk individuals to respond to the referral card with health care seeking are often limited because access to care is difficult and costly, and service providers are often ill-prepared to manage or treat NCDs. Yet, as our findings illustrate, diagnosis and treatment through medication seems to be the primary pathway through which at-risk individuals managed to reduce their hypertension risk subsequent to receiving a referral letter. Our results suggest that individuals do not find information about their high blood pressure level distressing in the sense that we do not observe any negative effects on self-rated mental health and depressive symptoms in at-risk individuals who were given a referral letter. This is an important finding because a potential downside of population-based screenings are concerns about possible negative mental health implications of alerting individuals about underlying disease risk factors when they may have limited options to prevent or treat the respective diseases.
Supplementary Material
Acknowledgments:
We gratefully acknowledge the generous support for the Mature Adults Cohort of the Malawi Longitudinal Study of Families and Health (MLSFH-MAC) by the Swiss Programme for Research on Global Issues for Development (SNF r4d Grant 400640_160374) and the pilot funding received through the Penn Center for AIDS Research (CFAR), supported by NIAID AI 045008 and the Penn Institute on Aging. We are also grateful for support for the Malawi Longitudinal Study of Families and Health (MLSFH) by the Rockefeller Foundation; the National Institute of Child Health and Human Development (NICHD, Grant Nos. R01 HD044228, R01 HD053781, R01 HD087391); the National Institute on Aging (NIA, Grant Nos. P30 AG12836 andR21 AG053763); the Boettner Center for Pensions and Retirement Security at the University of Pennsylvania; and the NICHD Population Research Infrastructure Program (Grant Nos. R24 HD-044964), all at the University of Pennsylvania. We would like to thank Jere Behrman, Adeline Delavande, Jürgen Maurer, Owen O’Donnell, Meghan Skira and Petra Todd for their comments that greatly improved the quality of this work.
Footnotes
Note that these non-clinical blood pressure measurements do not allow to determine whether respondents suffer from hypertension, as they do not constitute a proper medical diagnosis. These measurements indicate that respondents might have hypertension, which is the reason why we defined them as “at-risk” study participants.
Blood pressure can vary even if measured in short intervals and blood pressure readers measure blood pressure with error (Eguchi et al. 2009; Koehler et al. 2004; Yarows et al. 2001).
Specifically, among the studies that have analyzed screening interventions for communicable diseases in Africa, Thornton (2008) finds that a financial incentive substantially increases the likelihood that an individual travels to learn the result of an HIV test in Malawi. Delavande and Kohler (2012) use the same intervention to look at beliefs over transmission risk and risky sexual behavior, and find that receiving an HIV-negative test result implies higher subjective expectations about being HIV-positive after two years, and individuals tend to have larger prediction errors about their HIV status after learning their HIV status. Gong (2014) looks at a randomized HIV testing campaign in Kenya and Tanzania and find that being tested reduce the likelihood of getting a sexually transmitted infection (STI), and document behavioral responses to HIV tests when tests provide unexpected information. Cohen et al. (2015) randomize access to rapid malaria diagnostic tests in Kenya where overtreatment of malaria is very common, and find that those who learn their status are less likely to buy the antimalarial drug but around half of individuals testing negative still purchase the drug.
Interestingly, individuals in Malawi and more generally in SSA LICs lack the presence of conventional risk factors such as obesity or lack of physical activity that are associated with hypertension. In the MLSFH-MAC study population, only 15% of study participants are overweight (body mass index (BMI) between 25 to 30) and less than 5% are obese (BMI ≥ 30).
For example, the WHO STEPS Survey conducted in 2009 in Malawi found that 75% of the participants never had their blood pressure measured before and 94.9% of the individuals who were tested with high blood pressure were unaware of their hypertensive conditions (Msyamboza et al. 2012).
There are no birth certificates and/or other reliable records of when individuals are born in Malawi. MLSFH-MAC makes several attempts to verify age of the study participants. Eligibility for enrollment in MLSFH-MAC was determined by ages reported in 2010 and earlier. A small number of individuals reported ages below 45 at enrollment in 2012. These individuals were nevertheless enrolled in the study and this resulted in small number of respondents below age 45. In our MLSFH-MAC sample used in this analysis includes 12 respondents who are between ages 40 and 45.
A one-minute interval between readings is usually recommended, but studies have shown that shorter time-intervals, even less than 15 seconds, can be as accurate as conventional one-minute intervals (Eguchi et al. 2009; Koehler et al. 2004; Yarows et al. 2001).
Note that the referral letter and the questionnaire mention that respondents were being referred if their systolic or diastolic blood pressure “surpassed” 160 and 110mm/Hg, respectively. In practice, referral letters were given if one of the systolic or diastolic blood pressure measurements was greater or equal to 160 and 110, respectively. As robustness checks, we check that our results hold when dropping individuals who are exactly at the 160 cutoff. Results are available upon request.
The reasons why 160 mm Hg systolic blood pressure was considered for the threshold are threefold. First, this was considered at that time as the cutoff when individuals would be treated with medications for hypertension (at least in the Western world). Second, 160 systolic BP reflected stage two hypertension. For people without any additional risk factors, this cutoff/stage two hypertension would put individuals under moderate risk for CVD events. Rural population in Malawi is generally considered low risk in terms of other CVD factors. By choosing a level lower than 160, one could capture some random increase in BP (e.g., dehydration, etc) and not individual’s higher level of BP (Anderson et al. 2013). Third, health systems support for hypertension in rural Malawi in 2013 was still fairly weak (and continues to be), and available treatment resources for individuals at elevated CVD risk were limited. As a result, a relatively high threshold to determine whether an individual receives a referral letter would target individuals who are the most at risk. The use of the maximum of the three measurements to determine treatment was implemented to facilitate interviewers work and to avoid making them compute the average of the three measurements during the survey –which is prone to mistake.
The 2013 MLSFH-MAC survey consists of 1,257 completed interviews, among which 1,244 interviews contained three non-missing systolic and diastolic blood pressure measurements.
Health knowledge and behaviors were measured differently in 2013. Therefore, we focus on the 2017 measures only.
Hypertension is usually asymptomatic but can result in various symptoms such as shortness of breath and headache in some cases. In our analysis, we consider that an individual knows about the characteristics of the symptoms of hypertension if she either says that hypertension is asymptomatic or can identify at least one of its symptoms.
Analyzing the effects of a blood pressure screening in the UK Understanding Society Survey, Bhalotra et al. (2018) do not adopt a RDD strategy as they have concerns about blood pressure measurement. In particular, they find evidence that a large share of those hypertensive according to the survey would turn out normotensive in a visit with a doctor. For example, because of significant variation in blood pressure over the day, they find that 16% of respondents who were hypertensive according to the survey, are normotensive once they adjust for the time of the day. In this case, a referral may not lead to behavioral changes as the doctor would not diagnose the patient with hypertension. In our setting, however, the cutoff for getting the referral (160 mmHg systolic) is much higher than the cutoff used by medical doctors in Malawi to diagnose someone with hypertension (140 mmHg systolic). In Appendix Figure A.4, we also show that variation in blood pressure averages over the day in our MLSFH-MAC study sample is less than 6 mmHg for systolic blood pressure. Only 2 respondents who got the referral card have an average systolic blood pressure below 146 (the lowest average is 144) which is 6 mmHg away from the 140 mmHg cutoff to be diagnosed hypertensive. Therefore, the respondents who got the referral letter are all very likely to be diagnosed hypertensive by a medical doctor. The considerations that caused Bhalotra et al. (2018) to adopt an instrumental variable instead of RDD design therefore do not apply to our context, and a RDD strategy is an appropriate approach to identify the causal effects of the referral card on subsequent blood pressure and health behaviors.
The main health outcomes of interest in our analysis Yi are changes in systolic and diastolic blood pressures between 2017 and 2013, probability of being hypertensive in 2017 as defined in the previous section, whether respondents have been diagnosed with hypertension and whether they have been taking medication to control their blood pressure.
We will show however as robustness checks that our results are consistent when using quadratic polynomials, that is polynomials of order 2.
Note that our results are robust to to using rectangular kernel function and hence giving equal weight to all observations within the range [160 − h−; 160 + h+].
These bandwidths are chosen optimally following data-driven techniques developed by Calonico et al. (2014a,b, 2015) using Mean Square Error (MSE) optimal bandwidth selector. In addition, the estimates of the standard errors are computed using heteroskedasticity-robust plug-in residuals variance estimator (Calonico et al. 2017). Note that the estimates of the variance covariance matrix are very similar when including weights for finite sample adjustments or when using nearest neighbor variance estimator.
For ease of comparisons across the different outcome variables we consider, we will also show results where we impose the bandwidths on both sides of the cutoff to be identical across all the dependent variables we consider in our analysis. Again, our results are very robust to these restrictions as well.
Our main interest is in as we are more interested in the effects of treatment on the subpopulation of treated units than on the effects on the population as a whole (Heckman et al. 1998; Imbens 2004). We will however also present estimates of the average treatment effect (ATE), , defined as in the Appendix.
Selecting the number of matches involves the traditional trade-off between bias and variance, as a lower number of matches decreases bias and increase variance whereas the other way around holds when the number of matches increases (Rosenbaum and Rubin 1985). In terms of the number of matches, it is usually recommended to choose a small number and four matches has been shown to perform well in terms of mean-squared error (Abadie and Imbens 2002). We therefore restrict the number of matches to be at least 4 and show in the Appendix that our results are robust when decreasing and increasing the number of matches to 3 and 5, respectively. In cases of ties, all observations with equal R are used to compute and . Note also that we allow the same control unit to be matched to treated unit several times, that is, we are matching observations with replacement. We are to the best of our knowledge the first to match individuals over their blood pressure and hence there is no study on which we can rely to determine the optimal Euclidean distance for the matching between treated and untreated observations. The choice of 10, which roughly corresponds to the average distance between the maximum and minimum systolic blood pressure measurement for a given individual in our matching sample (10.96), was made to achieve a balance between power and bias. We also explore the robustness of our findings when shrinking the neighborhood around each Ri to 12, 8 and 5. The magnitude of the effects is very similar although the estimates are sometimes not as precise.
When matching individuals not only on R but also on a set of covariates x, we impose the same distance restriction as in our benchmark analyses, where, instead of the distance being computed based on the euclidean metric, the distance will be calculated using the mahalanobis metric.
Similar plots but using second order local polynomials can can be found in the Appendix Figure A.5.
Bins are derived optimally using variance evenly-spaced method estimators (Calonico et al. 2014a,b, 2015, 2017).
It is worth noting that the survey asks respondents whether they have been diagnosed with hypertension over the past two years. Given the four-year gap between the two surveys, it is possible that this effect corresponds to an underestimate of the true effect of the health screening on the probability of having been diagnosed over the period between 2013 and 2017, as some respondents may have been diagnosed before 2015.
We also investigated whether there is a discontinuity at the cutoff in diagnosis in 2013 before the blood pressure screening. Reassuringly, we do not see a statistically significant discontinuity using several different polynomials and controls.
For physical activity, we use “MET” which stands for metabolic equivalent of task. MET is a measure of oxygen consumption generated by physical activities which are ranked according to their level of intensities relative to the standard resting metabolic rate (Ainsworth et al. 2000). We create the MET score as a weighted physical activity score based on the number of hours per week of vigorous physical activity multiplied by 7.5 METs and the number of hours per week of moderate physical activity by 4 METs. These two subjective coefficients have been confirmed as being reliable for objective measures of moderate and vigorous physical activities (Brown et al. 2008). Table A.7 in the Appendix shows that getting a referral card does not change physical activity when broken down by moderate or vigorous activity, nor does it have any effect on body mass, as measured by BMI and waist to hip ratio.
The multi-item Patient Health Questionnaire (PHQ-9) is a widely used and validated depression instrument that assess the presence and severity of depressive symptoms in clinical and general settings as well as large population-based studies (Kroenke et al. 2001). These results are available upon request.
Subjective survival expectations are routinely collected in the MLSFH. In particular, the MLSFH asks about the probability of dying in 5 and in 10 years. Delavande and Kohler (2009) developed an elicitation technique ad-hoc for a context with low literacy and numeracy.
Among the 1,240 individuals we consider in our analysis for which we have all blood pressure measurements in 2013, we know the survival status of 1,216 of them in 2017. Out of these 1,216 individuals, 104 have died between 2013 and 2017. This constitutes a mortality rate of about 8.6%.
Among those who were still alive in 2017, 6 individuals refused to participate, 1 was hospitalized, 9 were temporarily absent and 11 have migrated.
Note that in our benchmark specification, we drop respondents whose mean systolic blood pressure is below 140 to restrict our study sample of treated and untreated individuals to have a relatively common support within the matching tolerance. As detailed in the methodology section, we restrict the distance between the mean blood pressure between treated and untreated individuals to be less than 10 units in order to compare individuals with similar underlying blood pressure. As discussed below, our results are robust to decreasing and increasing the number of matches to 3 and 5, respectively. We will also show that the effects are also very similar when reducing the distance in mean systolic blood pressure between treated and untreated individuals to 8 and 5. When allowing the distance to be maximum 8, we restrict our sample to individuals with at least 142 of mean systolic blood pressure. When the maximum distance is set to 5, our sample consists of individuals with at least 148 of mean systolic blood pressure.
Table A.15 in the Appendix presents the ATE instead the ATET. The quality of the matches is not as good in the ATE as in the ATET because ATE requires all individuals who have not received a referral letter to be matched with individuals who did received a referral letter. As shown in Figure 3, those who received a referral letter are not uniformly distributed in the range of the mean systolic blood pressure considered in our matching strategy. This means that a large share of the individuals who did not receive a referral letter is matched with individuals who have on on average higher mean systolic blood pressure. The effects presented in Table A.15 are however in line with those presented in our benchmark specification.
Table A.16 shows that the decrease in physical activity is in fact due to a drop in vigorous physical activity. It is also worth noting that the drop in physical activity does not seem to be accompanied by an increase in body mass, either measured in terms of BMI or waist-to-hip ratio.
There are 130 deaths between 2013 and 2019/19 among 1,249 mature adults screened at baseline in 2013. The estimate for the number of death averted is obtained by predicting the probability of dying as a function of age, gender and systolic blood pressure, then reducing the systolic blood pressure by 12.6 base points (= estimated treatment effect in the nearest neighbor/matching approach; see Table 5) for all respondents who received a referral card, and obtaining again the predicted number of deaths. The difference in the predicted number of death before and after reducing systolic blood pressure is a back-of-the envelope estimate of the number of deaths averted by the MLSFH-MAC blood pressure screening. This interpretation relies on strong assumptions, among others, that the association between systolic blood pressure and mortality is a reasonably proxy for the causal effect. No other reliable estimates of the potential causal relationship between blood pressure and mortality exist for this study context.
We assume a wage of $20 per day, the daily rate the MLSFH-MAC team paid health counselors in 2018. At a larger scale, some efficiency improvements in screening are surely possibly, which would further reduce the costs of blood pressure screening as part of a door-to-door testing.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abadie A and Imbens G (2002). Simple and bias-corrected matching estimators. Technical report, NBER Technical Working Paper No. 283. [Google Scholar]
- Abadie A and Imbens GW (2006). Large sample properties of matching estimators for average treatment effects. Econometrica, 74(1), 235–267. [Google Scholar]
- Abadie A, Drukker D, Herr JL, and Imbens GW (2004). Implementing matching estimators for average treatment effects in Stata. The Stata Journal, 4(3), 290–311. [Google Scholar]
- Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O Brien WL, Bassett DR, Schmitz KH, Emplaincourt PO, et al. (2000). Compendium of physical activities: an update of activity codes and MET intensities. Medicine and Science in Sports and Exercise, 32(9; SUPP/1), S498–S504. [DOI] [PubMed] [Google Scholar]
- Allotey P and Reidpath D (2007). Epilepsy, culture, identity and well-being: a study of the social, cultural and environmental context of epilepsy in Cameroon. Journal of Health Psychology, 12(3), 431–443. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association (2002). Screening for diabetes. Diabetes Care, 25(Suppl 1), s21. [DOI] [PubMed] [Google Scholar]
- American Heart Association (2019). Heart-health screenings. https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease/heart-health-screenings Accessed: 2020–01-08.
- Anderson CS, Heeley E, Huang Y, Wang J, Stapf C, Delcourt C, Lindley R, Robinson T, Lavados P, Neal B, et al. (2013). Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl j Med, 368, 2355–2365. [DOI] [PubMed] [Google Scholar]
- Angrist JD and Rokkanen M (2015). Wanna get away? Regression discontinuity estimation of exam school effects away from the cutoff. Journal of the American Statistical Association, 110(512), 1331–1344. [Google Scholar]
- Banerjee A and Duflo E (2011). Poor Economics: A Radical Rethinking of the Way to Fight Global Poverty. Public Affairs. [Google Scholar]
- Beaglehole R, Epping-Jordan J, Patel V, Chopra M, Ebrahim S, Kidd M, and Haines A (2008). Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. The Lancet, 372(9642), 940–949. [DOI] [PubMed] [Google Scholar]
- Behrman JR, Behrman JA, and Perez N (2011). Out of sync? Social science research on health and development and health conditions in developing countries. Demographic Research, 24(2), 45–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benziger CP, Roth GA, and Moran AE (2016a). The global burden of disease study and the preventable burden of NCD. Global Heart, 11(4), 393–397. [DOI] [PubMed] [Google Scholar]
- Benziger CP, Roth GA, and Moran AE (2016b). The Global Burden of Disease Study and the preventable burden of NCD: Has recognition of global chronic disease reached a tipping point? Global Heart, 11(4), 393–397. [DOI] [PubMed] [Google Scholar]
- Bhalotra S, Delavande A, Fisher P, and James J (2018). The impact of a personalised blood pressure warning on health behaviours. University of Essex, ISER Working Paper. [Google Scholar]
- Boateng D, Wekesah F, Browne JL, Agyemang C, Agyei-Baffour P, Aikins A. d.-G., Smit HA, Grobbee DE, and Klipstein-Grobusch K (2017). Knowledge and awareness of and perception towards cardiovascular disease risk in sub-saharan africa: A systematic review. PLOS ONE, 12(12), e0189264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown WJ, Burton NW, Marshall AL, and Miller YD (2008). Reliability and validity of a modified self-administered version of the Active Australia Physical Activity Survey in a sample of mid-age women. Australian and New Zealand Journal of Public Hhealth, 32(6), 535–541. [DOI] [PubMed] [Google Scholar]
- Calonico S, Cattaneo MD, and Titiunik R (2014a). Robust data-driven inference in the regression-discontinuity design. The Stata Journal, 14(4), 909–946. [Google Scholar]
- Calonico S, Cattaneo MD, and Titiunik R (2014b). Robust nonparametric confidence intervals for regression-discontinuity designs. Econometrica, 82(6), 2295–2326. [Google Scholar]
- Calonico S, Cattaneo MD, and Titiunik R (2015). rdrobust: An r package for robust nonparametric inference in regression-discontinuity designs. R Journal, 7(1), 38–51. [Google Scholar]
- Calonico S, Cattaneo MD, Farrell MH, and Titiunik R (2017). rdrobust: Software for regression-discontinuity designs. The Stata Journal, 17(2), 372–404. [Google Scholar]
- Calonico S, Cattaneo MD, Farrell MH, and Titiunik R (2019). Regression discontinuity designs using covariates. Review of Economics and Statistics, 101(3), 442–451. [Google Scholar]
- Cappuccio FP and Miller MA (2016). Cardiovascular disease and hypertension in sub-Saharan Africa: burden, risk and interventions. Internal and Emergency Medicine, 11(3), 299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC (2020). National HIV Testing Day—June 27. Website of the Centers for Disease Control and Prevention (CDC), Accessed February 1, 2020. [Google Scholar]
- Chen S, Sudharsanan N, Huang F, Liu Y, Geldsetzer P, and Bärnighausen T (2019). Impact of community based screening for hypertension on blood pressure after two years: regression discontinuity analysis in a national cohort of older adults in china. bmj, 366, l4064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Dupas P, and Schaner S (2015). Price subsidies, diagnostic tests, and targeting of malaria treatment: evidence from a randomized controlled trial. American Economic Review, 105(2), 609–45. [Google Scholar]
- Das S, Mia MN, Hanifi SMA, Hoque S, and Bhuiya A (2017). Health literacy in a community with low levels of education: findings from Chakaria, a rural area of Bangladesh. BMC Public Health, 17(1), 203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehmer SP, Maciosek MV, LaFrance AB, and Flottemesch TJ (2017). Health benefits and cost-effectiveness of asymptomatic screening for hypertension and high cholesterol and aspirin counseling for primary prevention. The Annals of Family Medicine, 15(1), 23–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delavande A and Kohler H-P (2009). Subjective expectations in the context of HIV/AIDS in Malawi. Demographic Research, 20, 817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delavande A and Kohler H-P (2012). The impact of HIV testing on subjective expectations and risky behavior in Malawi. Demography, 49(3), 1011–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denison J, O’Reilly K, Schmid G, Kennedy C, and Sweat M (2008). HIV voluntary counseling and testing and behavioral risk reduction in developing countries: A meta-analysis, 1990–2005. AIDS and Behavior, 12(3), 363–373. [DOI] [PubMed] [Google Scholar]
- Dupas P (2011). Health behavior in developing countries. Annu. Rev. Econ, 3(1), 425–449. [Google Scholar]
- Dupas P and Miguel E (2017). Impacts and determinants of health levels in low-income countries In Handbook of Economic Field Experiments, volume 2, pages 3–93. Elsevier. [Google Scholar]
- Echouffo-Tcheugui JB, Kengne AP, Erqou S, and Cooper RS (2015). High blood pressure in Sub-Saharan Africa: The urgent imperative for prevention and control. The Journal of Clinical Hypertension, 17(10), 751–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eguchi K, Kuruvilla S, Ogedegbe G, Gerin W, Schwartz JE, and Pickering TG (2009). What is the optimal interval between successive home blood pressure readings using an automated oscillometric device? Journal of hypertension, 27(6), 1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foot C, Gilburt H, Dunn P, Jabbal J, Seale B, Goodrich J, Buck D, and Taylor J (2014). People in control of their own health and care. King’s Fund. [Google Scholar]
- Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, et al. (1998). Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. Journal of Clinical Epidemiology, 51(11), 1171–1178. [DOI] [PubMed] [Google Scholar]
- Ganguli I, Bassett I, Dong K, and Walensky R (2009). Home testing for HIV infection in resource-limited settings. Current HIV/AIDS Reports, 6(4), 217–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD Collaborators (2018). Global, regional, and national disability-adjusted life-years (dalys) for 359 diseases and injuries and healthy life expectancy (hale) for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet, 392(10159), 1859–1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geldsetzer P et al. (2019). The state of hypertension care in 44 low-income and middle-income countries: a cross-sectional study of nationally representative individual-level data from 1.1 million adults. Lancet, 394(10199), 652–662. [DOI] [PubMed] [Google Scholar]
- Gelman A and Imbens G (2019). Why high-order polynomials should not be used in regression discontinuity designs. Journal of Business & Economic Statistics, 37(3), 447–456. [Google Scholar]
- Gong E (2014). HIV testing and risky sexual behaviour. The Economic Journal, 125(582), 32–60. [Google Scholar]
- Greenberg H, Raymond SU, and Leeder SR (2011). The prevention of global chronic disease: academic public health’s new frontier. American Journal of Public Health, 101(8), 1386–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn J, Todd P, and Van der Klaauw W (2001). Identification and estimation of treatment effects with a regression-discontinuity design. Econometrica, 69(1), 201–209. [Google Scholar]
- He FJ and MacGregor GA (2016). Hypertension: salt: flawed research should not divert actions to reduce intake. Nature Reviews Nephrology, 12(9), 514. [DOI] [PubMed] [Google Scholar]
- Heckman JJ, Ichimura H, and Todd P (1998). Matching as an econometric evaluation estimator. The Review of Economic Studies, 65(2), 261–294. [Google Scholar]
- Holland PW (1986). Statistics and causal inference. Journal of the American Statistical Association, 81(396), 945–960. [Google Scholar]
- Howard K, White S, Salkeld G, McDonald S, Craig JC, Chadban S, and Cass A (2010). Cost-effectiveness of screening and optimal management for diabetes, hypertension, and chronic kidney disease: A modeled analysis. Value in health, 13(2), 196–208. [DOI] [PubMed] [Google Scholar]
- Ibrahim MM and Damasceno A (2012). Hypertension in developing countries. The Lancet, 380(9841), 611–619. [DOI] [PubMed] [Google Scholar]
- Imbens GW (2004). Nonparametric estimation of average treatment effects under exogeneity: A review. Review of Economics and Statistics, 86(1), 4–29. [Google Scholar]
- Islam SMS, Purnat TD, Phuong NTA, Mwingira U, Schacht K, and Fröschl G (2014). Non-communicable diseases (ncds) in developing countries: a symposium report. Globalization and health, 10(1), 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahn A, Floyd S, Crampin AC, Mwaungulu F, Mvula H, Munthali F, McGrath N, Mwafilaso J, Mwinuka V, Mangongo B, et al. (2008). Population-level effect of HIV on adult mortality and early evidence of reversal after introduction of antiretroviral therapy in Malawi. Lancet, 371(9624), 1603–1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkinson C, Layte R, Jenkinson D, Lawrence K, Petersen S, Paice C, and Stradling J (1997). A shorter form health survey: can the SF-12 replicate results from the SF-36 in longitudinal studies? Journal of Public Health, 19(2), 179–186. [DOI] [PubMed] [Google Scholar]
- Kämpfen F, Wijemunige N, and Evangelista B (2018). Aging, non-communicable diseases, and old-age disability in low-and middle-income countries: a challenge for global health. International Journal of Public Health, 63. [DOI] [PubMed] [Google Scholar]
- Kenkel DS (1991). Health behavior, health knowledge, and schooling. Journal of Political Economy, 99(2), 287–305. [Google Scholar]
- Koehler NR, Poli de Figueiredo CE, and Mendes-Ribeiro AC (2004). Time interval between pairs of arterial blood pressure measurements—does it matter? American journal of hypertension, 17(2), 194–196. [DOI] [PubMed] [Google Scholar]
- Kohler H-P, Watkins SC, Behrman JR, Anglewicz P, Kohler IV, Thornton RL, Mkandawire J, Honde H, Hawara A, Chilima B, Bandawe C, and Mwapasa V (2015). Cohort profile: The Malawi Longitudinal Study of Families and Health (MLSFH). International Journal of Epidemiology, 44(2), 394–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohler IV et al. (2018a). Preliminary analyses of the 2017 MLSFH data on NCD knowledge and awareness Available upon request. Population Studies Center, University of Pennsylvania. [Google Scholar]
- Kohler IV and Kohler H-P (2020). Own analyses of 2019 mlsfh-mac health care facility (hcf data) (variables m11_qicvd12 m11_qimh14). [Google Scholar]
- Kohler IV, Sudharsanan N, Bandawe C, and Kohler H-P (2018b). Hypertension without conventional risk factors—high prevalence of high blood pressure in a low risk, low income African population. Paper presented at the 2018 Annual Meeting of the Population Association of America, Denver, CO, April 26–28, 2018. [Google Scholar]
- Kohler IV, Bandawe C, Ciancio A, Kämpfen F, Payne C, Mwera J, Mkandawire J, and Kohler H-P (2020). Cohort profile: The Mature Adults Cohort of the Malawi Longitudinal Study of Families and Health (MLSFH-MAC). University of Pennsylvania Population Center (PSC/PARC) Working Paper 2020–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, and Williams JB (2001). The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krogsbøll LT, Jørgensen KJ, Larsen CG, and Gøtzsche PC (2012). General health checks in adults for reducing morbidity and mortality from disease: Cochrane systematic review and meta-analysis. BMJ, 345, e7191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lackland DT and Weber MA (2015). Global burden of cardiovascular disease and stroke: hypertension at the core. Canadian Journal of Cardiology, 31(5), 569–571. [DOI] [PubMed] [Google Scholar]
- Lee DS and Lemieux T (2010). Regression discontinuity designs in economics. Journal of Economic Literature, 48(2), 281–355. [Google Scholar]
- Leung AA, Nerenberg K, Daskalopoulou SS, McBrien K, Zarnke KB, Dasgupta K, Cloutier L, Gelfer M, Lamarre-Cliche M, Milot A, et al. (2016). Hypertension canada’s 2016 canadian hypertension education program guidelines for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Canadian Journal of Cardiology, 32(5), 569–588. [DOI] [PubMed] [Google Scholar]
- Liwa AC, Smart LR, Frumkin A, Epstein H-AB, Fitzgerald DW, and Peck RN (2014). Traditional herbal medicine use among hypertensive patients in sub-saharan africa: a systematic review. Current hypertension reports, 16(6), 437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, et al. (2012). Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet, 380(9859), 2095–2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maharaj P, editor (2013). Aging and Health in Africa, International Perspectives on Aging, Berlin and New York: Springer. [Google Scholar]
- Malawi Ministry of Health (2011). Malawi: Health Sector Strategic Plan 2011–2016 (Draft III). Malawi Ministry of Health, Lilongwe, Malawi: (28 March 2011). [Google Scholar]
- Malawi Ministry of Health and ICF International (2014). Malawi Service Provision Assessment Survey 2013–14: Key Findings. Technical report, MMOH and ICF International. [Google Scholar]
- Malawi MOH and WHO (2010). Malawi national STEPS survey for chronic non-communicable diseases and their risk factors final report. Ministry of Health (MOH) Malawi and World Health Organization (WhO). [Google Scholar]
- Malawi NSO and World Bank (2018). Methodology for poverty measurement in malawi (2016/2017). The National Statistics Office of Malawi and The World Bank, Poverty and Equity Global Practice, Report No. 129570. [Google Scholar]
- Malik AH, Akram Y, Shetty S, Malik SS, and Njike VY (2014). Impact of sugar-sweetened beverages on blood pressure. The American Journal of Cardiology, 113(9), 1574–1580. [DOI] [PubMed] [Google Scholar]
- Mayosi BA (2007). A statement of intent on the formation of the NCRP on cardiovascular and metabolic disease: a new initiative to fight heart disease, stroke, diabetes and obesity in South Africa. Cardiovascular, 18, 4–6. [PubMed] [Google Scholar]
- Mayosi BM (2013). The 10 “Best Buys” to combat heart disease, diabetes and stroke in Africa. Heart, 99(14), 973–974. [DOI] [PubMed] [Google Scholar]
- Mealli F and Rampichini C (2012). Evaluating the effects of university grants by using regression discontinuity designs. Journal of the Royal Statistical Society: Series A (Statistics in Society), 175(3), 775–798. [Google Scholar]
- Mensah GA (2008). Epidemiology of stroke and high blood pressure in Africa. Heart, 94(6), 697. [DOI] [PubMed] [Google Scholar]
- Msyamboza KP, Kathyola D, Dzowela T, and Bowie C (2012). The burden of hypertension and its risk factors in Malawi: nationwide population-based STEPS survey. International Health, 4(4), 246–252. [DOI] [PubMed] [Google Scholar]
- Müller D, Danner M, Rhiem K, Stollenwerk B, Engel C, Rasche L, Borsi L, Schmutzler R, and Stock S (2018). Cost-effectiveness of different strategies to prevent breast and ovarian cancer in german women with a BRCA 1 or 2 mutation. European Journal of Health Economics, 19(3), 341–353. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, et al. (2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet, 380(9859), 2197–2223. [DOI] [PubMed] [Google Scholar]
- Muula AS and Misiri HE (2009). Pain management among medical in-patients in blantyre, malawi. International archives of medicine, 2(1), 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCD-RisC Collaboration (2017). Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet, 389(10064), 37–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nduka CU, Stranges S, Bloomfield GS, Kimani PK, Achinge G, Malu AO, and Uthman OA (2016). A plausible causal link between antiretroviral therapy and increased blood pressure in a sub-Saharan African setting: a propensity score-matched analysis. International Journal of Cardiology, 220, 400–407. [DOI] [PubMed] [Google Scholar]
- Nguyen T-P-L, Wright EP, Nguyen T-T, Schuiling-Veninga C, Bijlsma M, Nguyen T-B-Y, and Postma M (2016). Cost-effectiveness analysis of screening for and managing identified hypertension for cardiovascular disease prevention in vietnam. PloS one, 11(5), e0155699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nulu S, Aronow WS, and Frishman WH (2016). Hypertension in Sub-Saharan Africa. Cardiology in Review, 24(1), 30–40. [DOI] [PubMed] [Google Scholar]
- Ogah OS and Rayner BL (2013). Recent advances in hypertension in sub-saharan africa. Heart. [DOI] [PubMed] [Google Scholar]
- Ohrnberger J, Anselmi L, Fichera E, and Sutton M (2020). Validation of the sf12 mental and physical health measure for the population from a low-income country in sub-saharan africa. Health and quality of life outcomes, 18(1), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oster E, Shoulson I, and Dorsey ER (2013). Limited life expectancy, human capital and health investments. American Economic Review, 103(5), 1977–2002. [DOI] [PubMed] [Google Scholar]
- Payne C, Mkandawire J, and Kohler H-P (2013). Disability transitions and health expectancies among adults 45 years and older mature in Malawi: A cohort modeling approach. PLOS Medicine, 10(5), e1001435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price AJ, Crampin AC, Amberbir A, Kayuni-Chihana N, Musicha C, Tafatatha T, Branson K, Lawlor DA, Mwaiyeghele E, Nkhwazi L, Smeeth L, Pearce N, Munthali E, Mwagomba BM, Mwansambo C, Glynn JR, Jaffar S, and Nyirenda M (2018). Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub-Saharan Africa: A cross-sectional, population-based study in rural and urban Malawi. Lancet Diabetes & Endocrinology, 6(3), 208–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Lesmes PA et al. (2017). Early diagnosis of chronic conditions and lifestyle modification. Technical report. [Google Scholar]
- Rosenbaum PR and Rubin DB (1985). The bias due to incomplete matching. Biometrics, 41(1), 103–116. [PubMed] [Google Scholar]
- Rosendaal NT, Hendriks ME, Verhagen MD, Bolarinwa OA, Sanya EO, Kolo PM, Adenusi P, Agbede K, Van Eck D, Tan SS, et al. (2016). Costs and cost-effectiveness of hypertension screening and treatment in adults with hypertension in rural nigeria in the context of a health insurance program. PLoS One, 11(6), e0157925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhm CJ (2016). Health effects of economic crises. Health Economics, 25(S2), 6–24. [DOI] [PubMed] [Google Scholar]
- Sheridan S, Pignone M, and Donahue K (2003). Screening for high blood pressure: a review of the evidence for the us preventive services task force. American journal of preventive medicine, 25(2), 151–158. [DOI] [PubMed] [Google Scholar]
- Siu AL (2015). Screening for high blood pressure in adults: Us preventive services task force recommendation statement. Annals of internal medicine, 163(10), 778–786. [DOI] [PubMed] [Google Scholar]
- Sjørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, and Brand H (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12(1), 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skovron C and Titiunik R (2015). A practical guide to regression discontinuity designs in political science. American Journal of Political Science, 2015, 1–36. [Google Scholar]
- Strong K, Wald N, Miller A, Alwan A, and Group WC (2005). Current concepts in screening for noncommunicable disease: World Health Organization Consultation Group Report on methodology of noncommunicable disease screening. Journal of Medical Screening, 12(1), 12–19. [DOI] [PubMed] [Google Scholar]
- Swenson PF and Ebell MH (2016). Introducing a one-page adult preventive health care schedule: USPSTF recommendations at a glance. American Family Physician, 93(9), 738–740. [PubMed] [Google Scholar]
- The Economist (2017). Daily chart: The curious case of high blood pressure around the world. Economist. January 13, 2017. [Google Scholar]
- Thornton RL (2008). The demand for, and impact of, learning HIV status. American Economic Review, 98(5), 1829–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomar RH (1994). Breaking the asymptomatic phase of hiv-1 infection. Journal of clinical laboratory analysis, 8(2), 116–119. [DOI] [PubMed] [Google Scholar]
- Wald N, Hackshaw A, and Frost C (1999). When can a risk factor be used as a worthwhile screening test? Bmj, 319(7224), 1562–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W, Lee ET, Fabsitz RR, Devereux R, Best L, Welty TK, and Howard BV (2006). A longitudinal study of hypertension risk factors and their relation to cardiovascular disease: the Strong Heart Study. Hypertension, 47(3), 403–409. [DOI] [PubMed] [Google Scholar]
- Ware JE Jr, Kosinski M, and Keller SD (1996). A 12-item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical Care, pages 220–233. [DOI] [PubMed] [Google Scholar]
- WHO (2013a). Global Action Plan for the Prevention and Control of NCDs 2013–2020. World Health Organization (WHO), Geneva, Switzerland. [Google Scholar]
- WHO (2013b). Global action plan for the prevention and control of noncommunicable diseases 2013–2020. [Google Scholar]
- WHO (2014). Global status report on noncommunicable diseases 2014. Technical report, World Health Organization (WHO), Geneva, Switzerland. [Google Scholar]
- WHO (2015). Health literacy toolkit for low- and middle-income countries: A series of information sheets to empower communities and strengthen health systems. World Health Organization (WHO), Regional Office for South-East Asia, New Dehli, India. [Google Scholar]
- WHO (2016). Guidelines on HIV self-testing and partner notification Supplement to consolidated guidelines on HIV testing services. World Health Organization (WHO), Geneva, Switzerland. [PubMed] [Google Scholar]
- Wing C and Bello-Gomez RA (2018). Regression discontinuity and beyond: Options for studying external validity in an internally valid design. American Journal of Evaluation, 39(1), 91–108. [Google Scholar]
- World Bank Group (2018). Breaking the cycle of low growth and slow poverty reduction. Malawi - Systematic Country Diagnostic, Report No. 132785. [Google Scholar]
- Yarows SA, Patel K, and Brook R (2001). Rapid oscillometric blood pressure measurement compared to conventional oscillometric measurement. Blood pressure monitoring, 6(3), 145–147. [DOI] [PubMed] [Google Scholar]
- Zhao M, Konishi Y, and Glewwe P (2013). Does information on health status lead to a healthier lifestyle? evidence from china on the effect of hypertension diagnosis on food consumption. Journal of Health Economics, 32(2), 367–385. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.