Abstract
Background:
Experience of childhood maltreatment (CM) is a risk factor for opioid use disorder (OUD). CM is also associated with comorbid mental disorders and poor treatment outcomes among people with OUD. To our knowledge, this is the first systematic review and meta-analysis to estimate the prevalence of CM among people with OUD.
Methods:
We searched MEDLINE, EMBASE, and PsycINFO to identify observational studies that evaluated CM among people with OUD from January 1990 to June 2020. Prevalence of each CM type, sample characteristics, and methodological factors were extracted from each eligible study. Random-effects meta-analyses were used to pool prevalence estimates. Stratified meta-analyses were used to assess heterogeneity.
Results:
Of the 6,438 publications identified, 113 studies reported quantitative CM data among people with OUD and 62 studies (k=62; N=21,871) were included in primary analyses. Among people with OUD, the estimated prevalence of sexual abuse was 41% (95%CI 36–47%; k=38) among women and 16% (95%CI 12–20%; k=25) among men. Among all people with OUD, prevalence estimates were 38% (95%CI 33–44%; k=48) for physical abuse, 43% (95%CI 38–49%; k=31) for emotional abuse, 38% (95%CI 30–46%; k=17) for physical neglect, and 42% (95%CI 32–51%; k=17) for emotional neglect. Sex, history of injecting drug use, recruitment methods, and method of assessing CM were associated with substantial heterogeneity.
Conclusions:
People with OUD frequently report CM, supporting the need for trauma-informed interventions among this population. Future research should consider the impact of CM on OUD presentations and when assessment is appropriate, use of validated instruments.
Keywords: Opioid use disorders, Opioid dependence, Childhood maltreatment, Childhood abuse, Prevalence, Meta-analysis
1. Introduction
Globally, an estimated 40.5 million people live with opioid use disorder (OUD) (GBD 2017 causes of death collaborators, 2018). OUD is a chronic relapsing disorder that increases risk of blood borne virus transmission (Camacho et al., 1996), non-fatal overdose (Brady et al., 2017), and mortality (Degenhardt et al., 2019; Larney et al., 2020). The mortality rate of people with OUD is ten times that of comparable general population samples (Larney et al., 2020) and deaths attributable to OUD have increased exponentially over the past four decades (Hall et al., 2020). Risk factors for OUD include socioeconomic disadvantage (Needle et al., 1990), peer illicit substance use (Tucker et al., 2020), mental disorders (Martins et al., 2009), and the experience of childhood maltreatment (CM; Conroy et al., 2009).
CM is defined as the experience of sexual abuse, physical abuse, emotional abuse, or neglect of an individual under 18 years old (World Health Organization, 2006). Definitions for each type of CM are provided in Panel 1. Associations between CM and psychopathology related to substance use disorder are well-documented (Cicchetti and Handley, 2019). CM increases risk of behavioural disorders during childhood (Jones et al., 2004; Kendall-Tackett, 2004), youth mental health issues (Cicchetti and Valentino, 2006), and earlier onset of opioid and injection drug use (Kerr et al., 2009; Larance et al., 2018; Taplin et al., 2014). CM increases both risk of OUD (Conroy et al., 2009) and OUD severity. Among people with OUD, people who report experience of CM have higher rates of comorbid mental and substance use disorders (Darke, 2013; Maloney et al., 2007), engagement in risky injecting (McCurdy et al., 2010; Stein et al., 2017) and sexual behaviour (Engstrom et al., 2016), non-fatal overdose (Lake et al., 2015; Stein et al., 2017), and suicidal behaviour (Darke and Ross, 2002).
Panel 1: Definitions of each type of childhood maltreatment.
Sexual abuse
An attempted or completed sexual act or exploitation of a child (World Health Organization, 2006). Perpetrators of sexual abuse may be adults or other children in positions of power over the victim (World Health Organization, 2006). Examples include penetrative sexual abuse, sexual contact, and noncontact sexual abuse (e.g. child pornography) (Leeb et al., 2008).
Physical abuse
An intentional physical act by a caregiver that causes, or potentially causes, harm to a child’s health, survival, development, or dignity (World Health Organization, 2006). Examples include hitting, beating, kicking, and burning. Often inflicted with the object of punishment (World Health Organization, 2006) and recognised by physical injury (e.g. bruises) (Leeb et al., 2008).
Emotional abuse
An act or pattern of non-physical acts by a caregiver that have the potential to damage a child’s mental, physical, or social health and development (World Health Organization, 2006). Acts of emotional abuse may convey rejection and produce a hostile environment (World Health Organization, 2006). Examples include belittling, blaming, threating, ridiculing, terrorizing, and isolating (Leeb et al., 2008; World Health Organization, 2006). Also described as ‘psychological abuse’ (Leeb et al., 2008).
Physical neglect
Failure of a caregiver to provide for the child’s physical development and well-being, when they are in a position to do so (Leeb et al., 2008; World Health Organization, 2006). Examples include failure to provide adequate nutrition, appropriate clothing, hygiene, or shelter (Barnett et al., 1993; World Health Organization, 2006). The most commonly reported form of neglect (Stoltenborgh et al., 2015).
Emotional neglect
A caregiver’s failure to seek care for mental, emotional, or behavioural health problems and/or the omission of adequate affection (Barnett et al., 1993; Leeb et al., 2008). Examples include ignoring a younger child’s cry or an older child’s attempt to interact (Barnett et al., 1993; Leeb et al., 2008).
Panel notes:
Definitions derived from the World Health Organization (WHO) and United States Centers for Disease Control and Prevention (CDC)
Although studies of people with OUD report higher rates of CM than control groups (Conroy et al., 2009) and general population samples (Afifi et al., 2012; Evans et al., 2020), estimates vary widely (Conroy et al., 2009; Kumar et al., 2016).
To our knowledge, there has not yet been a systematic review and meta-analysis of the prevalence of any type of CM among people with OUD. Systematic reviews and meta-analyses of prevalence of CM exist for community samples (Stoltenborgh et al., 2015) and certain clinical populations, for example, people with psychosis (Bonoldi et al., 2013). These reviews have found that definitions of each type of CM are subject to cultural-geographical interpretation (Elliott and Urquiza, 2006; Stoltenborgh et al., 2013b, 2015), evolve over time (Miller-Perrin and Perrin, 2013), and vary by the methodology and instrument used to assess the experience (Baldwin et al., 2019).
We aimed to:
Estimate the prevalence of each major type of CM among people with OUD;
Examine sample characteristics and methodological factors associated with heterogeneity for each prevalence estimate;
Compare estimates of CM among people with OUD to global prevalence estimates of CM from a series of global reviews by Stoltenborgh et al (Stoltenborgh et al., 2015).
2. Methods
This review followed the PRISMA reporting guidelines (eAppendix 1; Moher, 2009) and was registered with PROSPERO (registration number: CRD42018094623).
2.1. Search strategy and study selection
Search terms were tailored for MEDLINE, Embase and PsycINFO databases using the OVID interface. Searches identified citations that reported any type of CM data among people with OUD published from January 1st, 1990 to June 18th, 2020. We aimed to estimate global prevalence of CM among people with OUD, therefore we did not restrict by language and used Google Translate to translate non-English studies. More details on the search strategy are provided in the supplementary material (eAppendix 2).
Study screening was conducted in Covidence, a web-based systematic review management tool (Veritas Health Innovation, 2016). After removing duplicates, we conducted title and abstract screening to identify observational studies of participants with OUD or proxy measures. Proxy measures for OUD included receiving treatment for opioid use (e.g. Opioid Agonist Therapy (OAT), detoxification, etc.), daily illicit opioid use, or frequent opioid use among people who inject drugs (PWID). Evaluation of CM was not considered at title and abstract screening stage to avoid selection bias. Relevant reviews were noted at title and abstract screening and citations were screened for eligibility. At the full-text screening stage, studies were excluded if the authors did not report any type of quantitative CM data among people with OUD (or proxy characteristics). Studies with less than 40 participants with OUD were also excluded. Full-text screening was conducted by two team members.
Authors were contacted if CM data and assessment of OUD (or proxy) were reported separately among the sample. Authors of citations that reported only continuous or aggregate types of CM data and those that did not report sexual abuse by sex were also contacted. eAppendix 3 includes details regarding the study selection process.
2.2. Data extraction
Data were extracted into a Microsoft Access database and double-checked by a second team member. Conflicts were resolved by discussion and referred to a third reviewer if necessary. eAppendix 4 includes details on the variables extracted and double-checking process.
2.2.1. CM Prevalence
The number and proportion of participants reporting each type of CM were extracted. Details on the instrument utilised and definition of maltreatment were collected. Details on the definition of CM included the instrument or scale utilised, cut-off used for continuous measurements, description of the event(s) or experience, and age cut-off for “childhood”.
2.2.2. Study characteristics
Sample characteristics, publication year, and recruitment method details were collected. Sample characteristics included age, proportion of men, proportion of people with a history of injecting drug use (IDU), description of opioid use patterns (i.e. details for ‘proxy’ OUD), childhood socio-economic status (SES) of the sample, history of parental SUD, and study location. Recruitment method details included setting and details on the participant inclusion and exclusion criteria. Recruitment setting of each study was stratified by four categories: sub-samples of general population studies, samples of people prescribed opioids for chronic non-cancer pain (CNCP), people with OUD recruited from OUD treatment settings (i.e. OAT, rehabilitation programs, supervised detoxification, and other in-patient services), and people recruited from non-treatment settings (i.e. community samples of PWID out of OAT, harm reduction services, and prisons).
2.2.3. Risk of bias and study quality
Study risk of bias was assessed by three domains: study inclusion or exclusion criteria, definition of OUD, and definition of CM, according to definitions described in Panel 1 (Leeb et al., 2008; World Health Organization, 2006). Risk of bias measures were adapted from published systematic reviews of people with OUD (Larney et al., 2020) and those with CM (Stoltenborgh et al., 2015). Risk of inclusion or exclusion criteria bias was a qualitative measure based on associations between CM and pre-defined risk of bias variables (e.g. studies that excluded participants with comorbid substance use or mental disorders were “high risk of underestimate”). These categorisations are not indicative of study quality, as the aims of included studies were not necessarily aligned with the aims of the current study. Each of the three domains was assessed by two independent reviewers and conflicts were resolved by a third party if necessary. Further details are provided in the supplementary material.
Statistical analyses were conducted in STATA 16.1 (StataCorp, 2017) using the metaprop_one command (Nyaga et al., 2014). Stratified random-effects meta-analyses were conducted by subgroup according to sex, history of IDU, recruitment setting, region, language of publication and language of survey administration. Random-effects meta-analyses were used as studies of retrospective CM data often report substantial heterogeneity (Baldwin et al., 2019). Stratified meta-analyses and meta-regressions were repeated by sex given that sex is a confounding variable in the experience of CM (Stoltenborgh et al., 2011). Sensitivity analyses were conducted by excluding studies at high risk of any form of bias, studies of adolescents, studies requiring translation, and studies before 2010.
Meta-regression analyses were conducted using the metareg function (Harbord and Higgins, 2009) to determine associations with continuous study-level variables, such as average sample age, percentage of men in the samples, and publication year.
3. Results
3.1. Included studies
Of the 113 studies (k=113) eligible for inclusion, 62 were included in one of the six primary analyses. Of the studies omitted from the primary analyses, 15 reported only continuous CM data, 8 reported only aggregate types of CM (i.e. ‘childhood adversity’), and 28 were secondary publications (i.e. participant overlap with primary studies). The PRISMA Flow diagram (Figure 1) provides further detail on the study inclusion and exclusion decisions. eAppendix 5 presents information on eligible studies excluded from the primary analyses.
Figure 1: PRISMA flowchart for included studies in the current review.
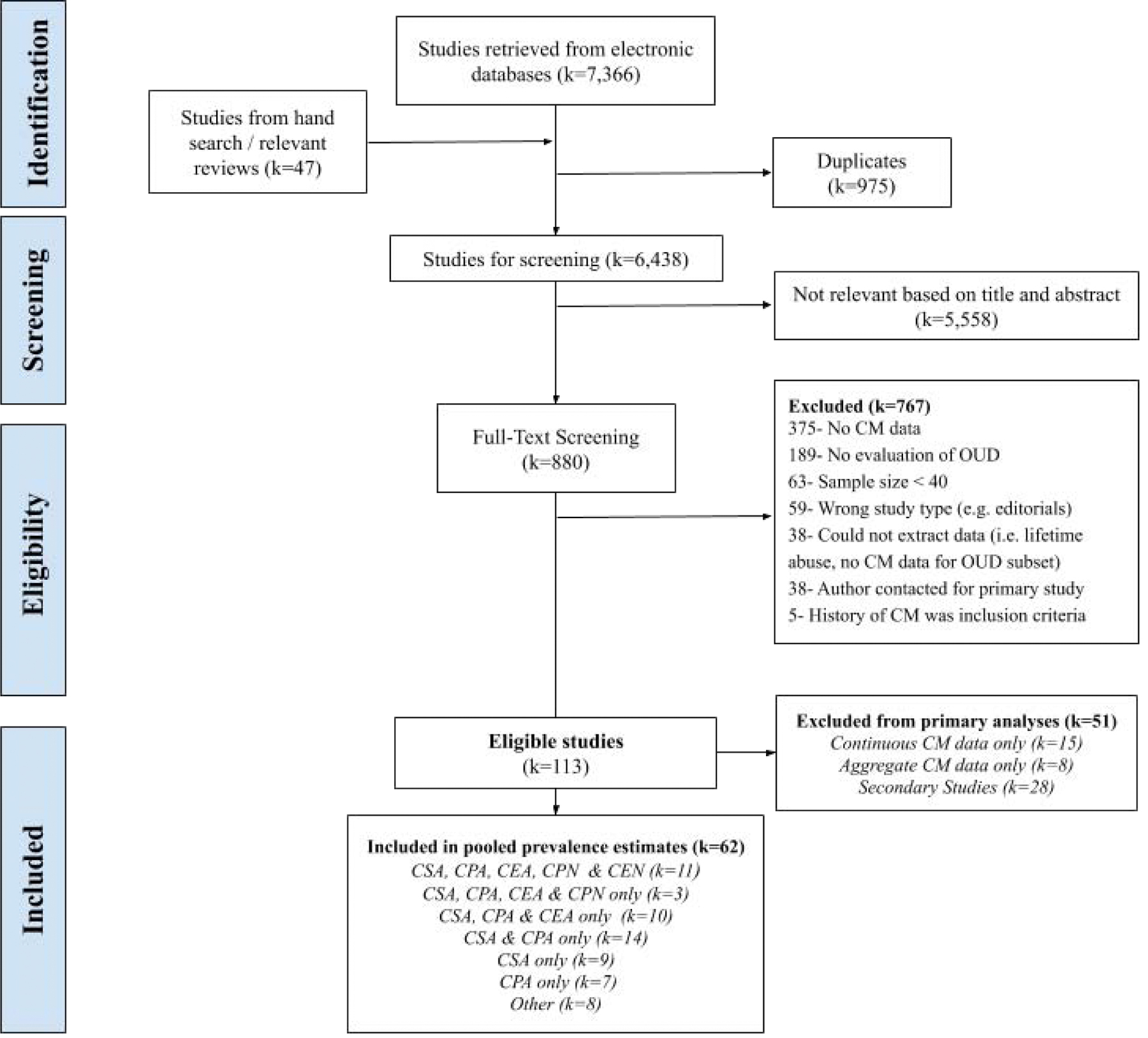
Notes: k=number of studies; OUD=Opioid Use Disorder; CM=Childhood Maltreatment; CSA= Childhood Sexual Abuse, CPA= Childhood Physical Abuse, CEA= Childhood Emotional Abuse, CPN=Childhood Physical Neglect, CEN=Childhood Emotional Neglect
Of the k=62 studies included in the primary analyses, there were samples from 18 different countries. Most studies recruited participants from North America (k=36; 58%) and evaluated CM among people in treatment for illicit OUD (e.g. heroin; k=45; 73%). Only one study evaluated history of CM among people with OUD who were prescribed opioids for CNCP. Over half of the included studies were published in 2010 or later (k=32; 52%) and 38 studies reported results among both men and women (61%). All estimates were self-report from observational studies, and most were published in English (94%). Table 1 presents detailed study-level descriptions.
Table 1:
Description of studies included in primary analyses
| Study Author, Year | Location | Total (N) | Men (n) | Women (n) | Setting | Description | OUD Definition | Inclusion / Exclusion Criteria | IDU Status | CSA-Women | CSA-Men | CPA | CEA | CPN | CEN |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Afifi et al., 2012 | USA (National) | 700 | 350 | 268 | General Population | Subset from representative population of USA adults. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC)-II. | DSM-4 OUD | Excl: Institutionalised | - | 40% | 14% | 38% | 20% | 43% | 18% |
| Alexander, 2018 (Alexander et al., 2019) | Philadelphia, Pennsylvania, USA | 175 | - | 175 | OAT | Women receiving methadone with a child or pregnant enrolled in a mindfulness intervention trial. | OAT | Incl: Women with children < 3 years or pregnant | - | - | - | 30% | - | - | |
| Bailey et al., 1994 | Norco, California, USA | 354 | 354 | - | Prison | Men in the Civil Addict Program, a rehabilitation ‘alternative’ to prison for ‘narcotic addicts’. | Other treatment | Excl: LTFU 24 years after recruitment | - | - | 5% | - | - | - | - |
| Bartholomew et al., 2005 | Texas, USA (One city) | 137 | - | 137 | OAT | Women in a no-fee methadone program at a private clinic. | OAT | - | - | 39% | - | - | - | - | - |
| Blatchley et al., 2000 | Baltimore & Washington-DC, USA | 248 | - | 248 | OAT | Women in OAT with adolescent children. Children enrolled in a psycho-educational program. | OAT | Incl: Mothers with custody of children | - | 32% | - | - | - | - | - |
| SAMHSA, 2009 (From Bohnert et al., 2011) | USA (National) | 1275 | 892 | 393 | OAT, Rehabilitation | Adults surveyed as part of the National Treatment Improvement Evaluation Study (NTIES), a survey of publicly funded treatment centres in the USA | Other treatment | Incl: Admitted to treatment for heroin or ‘street’ methadone use | 75%-Ever | 22% | 5% | 36% | - | - | - |
| Browne et al., 1998 | Dublin, Ireland | 52 | 28 | 24 | OAT | Consecutive patients admitted for methadone detoxification (n=33) or OAT (n=19). Patients referred by GPs, addiction councillors, or selfreferral. | OAT | - | - | - | - | 23% | - | - | - |
| Campbell et al., 2016 | Australia (National) | 381 | 203 | 178 | Prescribed for CNCP | Subset of people with pharmaceutical opioid dependence prescribed opioids for CNCP. Recruited from community pharmacies in Australia. | ICD-10 Dependence | Excl: Only prescribed opioids for OAT or cancer pain | 38%-Ever | 46% | 22% | 43% | 55% | 17% | - |
| Cash and Wilke, 2003 | USA (National) | 336 | - | 336 | Rehabilitation, Detoxification | Subset of mothers from the DATOS study. Recruited from drug treatment programs, hospitals, and criminal justice programs. | Other treatment | Incl: Women with children | - | 27% | - | 18% | - | - | - |
| Cohen et al., 2009 | USA (Multisite) | 214 | - | 214 | OAT | Sexually active women enrolled in one of seven OAT programs participating in a national multisite clinical trial for HIV/STD interventions. | OAT | Incl: OAT > 30 days, Past 6-month HIV risk; Excl: Pregnant | - | 40% | - | - | - | - | - |
| Darke and Torok, 2013 (Darke and Torok, 2014; Torok et al., 2016) | Sydney, NSW, Australia | 300 | 201 | 99 | Harm Reduction | Subset of people who frequent needle and syringe programs and use heroin. | Frequent Illicit Use | Incl: > Weekly injecting | 100%-Current | - | - | 77% | - | - | - |
| Davis et al., 2019a | Illinois, USA | 2067 | 1373 | 694 | Rehabilitation, Detoxification | Subset of adolescents with OUD in Chestnut Health Systems, a substance use treatment provider in Illinois. | DSM-4 OUD | Incl: Adolescents only | - | 30% | 3% | 61% | 42% | - | - |
| Derefinko et al., 2019 | Tennessee, USA | 87 | 65 | 12 | OAT | Medical chart review of a rural clinic providing OAT and counselling. | OAT | - | - | - | - | - | 45% | - | 40% |
| Dissabandara et al., 2009 | Kandy, Sri Lanka | 278 | 278 | - | Prison | Male inmates in prison for drug related offenses. 98% past-month heroin use, mean use: 13 years. | Frequent Illicit Use | - | 16%-Ever | - | 7% | 22% | - | - | - |
| El-Bassel et al., 2001 (El-Bassel et al., 2000) | NYC, USA | 280 | - | 28- | OAT | Women recruited from OAT clinics in Harlem through outreach and staff referrals (1995–96). 32% sex workers | OAT | Incl: ≥ 2 HIV-risk behaviours | - | 31% | - | 38% | - | - | - |
| Engstrom et al., 2012 (El-Bassel N. et al., 2019; Engstrom et al., 2016; Panchanadeswaran et al., 2008; Rojas, 2006) | NYC, USA | 390 | - | 390 | OAT | Women recruited from OAT clinics in a sexual relationship. Subset of random sample from OAT sites in NYC. | OAT | Incl: Sexually active with men | - | 58% | - | 38% | - | - | - |
| Evans et al., 2020 (Blanco C. et al., 2020; Hassan and Le Foll, 2019) | USA (National) | 778 | 390 | 388 | General Population | Subset of participants with lifetime illicit OUD from a 2012–13 representative USA household survey (NESARC-III) | DSM-5 OUD | Excl: Institutionalised | - | 36% | 12% | 38% | 30% | 54% | 19% |
| Fudalej et al., 2015 | Warsaw, Poland | 240 | 169 | 71 | OAT | Sample of people with opioid dependence from an OAT Clinic. | ICD-10 Dependence | - | - | - | - | 24% | - | - | - |
| Gardner S.M. et al., 2020 | Columbus, Ohio, USA | 40 | 16 | 24 | Rehabilitation, Detoxification | Adolescents, young adults receiving outpatient treatment for OUD. | Any OUD | - | - | - | - | 35% | 57% | 35% | 43% |
| Garfield et al., 2017 | Melbourne, Australia | 121 | 87 | 34 | OAT, Rehabilitation, Detoxification | People receiving OAT (n=90) and recently abstinent people (n=31) from residential services. | DSM-4 Dependence | Excl: Psychosis, bipolar, major depression | - | - | 28% | 45% | 50% | 36% | 49% |
| Gilbert et al., 1997 (Gilbert et al., 2000) | NYC, USA | 151 | - | 151 | OAT | Women enrolled in OAT programs in Bronx/Harlem, recruited through staff referrals and printed announcements in 1994. | OAT | - | - | 27% | - | 39% | - | - | - |
| Golden, 2018 | Alaska, USA | 43 | - | 43 | OAT | Sample of 43 Alaskan women seeking opioid-treatment without PTSD from a dissertation. | OAT | Excl: Comorbid PTSD | - | 40% | - | 30% | 25% | - | - |
| Grella et al., 1995 | Los Angeles, California, USA | 209 | - | 209 | Snowballing, Harm Reduction | Subset of women recruited to an OAT trial by outreach and snowballing. Targeted sex workers. | OAT | Excl: LTFU (13%) | 100%-Ever | 38% | - | 40% | 57% | - | - |
| Heffernan et al., 2000 | NYC, USA | 136 | 84 | 52 | Hospital | Subset of opiate users (> daily use) from a sample of consecutive admissions to a psychiatric hospital. | Frequent Illicit Use | - | - | 27% | - | 46% | - | - | - |
| Hien et al., 2000 | Long Island, NY, USA | 96 | 47 | 49 | OAT | People at a rehabilitation centre seeking methadone for OUD. | OAT | - | - | 29% | 4% | 23% | - | - | - |
| Isralowitz et al., 2002; Isralowitz and Bar Hamburger, 2002 | Negev, Israel | 152 | 98 | 54 | OAT, Detoxification | Israeli-born patients in an outpatient drug treatment program. | OAT | - | - | 26% | 5% | 32% | - | - | - |
| Isralowitz, 2001 | Negev, Israel | 154 | 93 | 61 | OAT, Detoxification | Russia/Ukraine-born patients in an outpatient drug treatment program. | OAT, other treatment | - | - | 43% | 12% | 40% | - | - | - |
| Kaboski, 2013 | Chicago, Illinois, USA | 205 | - | 205 | OAT | Mothers of infants and pre-schoolers at one of seven public OAT clinics. | OAT | - | - | 35% | - | 33% | - | - | - |
| Kang et al., 2002 | NYC, USA | 432 | 294 | 138 | Snowballing, Harm Reduction | Participants recruited from a list of OAT treatment dropouts and by local outreach workers from 1997–1999. | OAT | Incl: Only people who left OAT | - | 48% | 31% | 60% | 58% | 66% | - |
| Khosravani et al., 2019 (Ghorbani et al., 2019) | Tehran, Iran | 350 | 350 | - | Detoxification | Men with heroin dependence at a treatment centre in Tehran (N=450). Survey 2 weeks post detoxification. | DSM-4 Heroin Dependence | Excl: Health comorbidity, refusal, women | 50%-Ever | - | - | - | 74% | - | 59% |
| Koyuncu et al., 2003 | Istanbul, Turkey | 100 | 89 | 11 | Detoxification | People with heroin dependence at an inpatient hospital detoxification centre. | DSM-4 Heroin Dependence | Excl: Comorbid psychiatric diagnosis | - | - | - | 59% | 62% | - | - |
| Kumar et al., 2016 | Little Rock, Arkansas, USA | 113 | 63 | 50 | OAT | Chart review of adults receiving buprenorphine at an outpatient clinic. | OAT | - | 27%-Ever | 16% | 18% | 19% | 25% | 23% | 18% |
| Lake et al., 2015 (Braitstein et al., 2003; Cheng et al., 2018) | Vancouver, Canada | 2393 | 1489 | 903 | Snowballing, Harm Reduction | People with a history of OAT or ≥ daily illicit opioid use from the VIDUS/ARYS/ACCESS cohorts. | OAT, Frequent Illicit Use | - | 100%-Ever | 46% | 21% | 36% | 51% | 32% | 53% |
| Lovell, 2002 | Marseille, France | 111 | 111 | - | Snowballing, Harm Reduction | People with past year IDU recruited from 3 areas in Marseille. > 82% on OAT and injecting duration 10 years. | Frequent Illicit Use | - | 100%-Ever | - | - | 18% | 15% | - | - |
| McCurdy et al., 2010 | Dar es Salaam, Tanzania | 169 | - | 169 | Snowballing, Harm Reduction | Women injected recently and had sex in the month prior. Of 559 screened, 249 remained at 5-month FU. | Frequent Illicit Use | Incl: Current IDU Excl: LTFU at 5 months (44%) | 100%-Past 2 days | 25% | - | - | - | - | - |
| Medrano et al., 1999 | San Antonio, Texas, USA | 80 | - | 80 | Snowballing, Harm Reduction | Subset of participants that primarily use opioids from women recruited to an AIDS prevention program. | Frequent Illicit Use | Excl: Past month drug treatment | 100%-Ever | 60% | - | 57% | 47% | 64% | 79% |
| Mirhashem et al., 2017 | Northern New England, USA | 84 | 45 | 39 | Snowballing, Harm Reduction | Participants with lifetime SUD, identified opioids as primary substance. 29% had received OAT. | DSM-4 OUD | Excl: Active psychosis | - | - | 27% | 51% | 49% | 58% | 49% |
| Moselhy et al., 2010 (Elhammady et al., 2014; Moselhy, 2009) | Birmingham, United Kingdom | 120 | 90 | 30 | Rehabilitation, Detoxification | Outpatient attendees at a drug treatment service without mental or SUD comorbidities. | Other treatment | Excl: Other illicit substance use, Alcohol SUD, psychosis, trauma | - | - | - | 27% | - | - | - |
| Naqavi et al., 2011 | Bardsir, Iran | 212 | 179 | 33 | Rehabilitation, Detoxification | People who visited one of four drug treatment centres | DSM-4 Dependence | - | - | - | - | - | 34% | 52% | |
| Nelson et al., 2006 | Australia (National) | 73 | 29 | 44 | General Population | Young adults from Australian Twin Register. Participants with OUD born 1964–71. Substance use resembled general population. | DSM-4 OUD | Excl: LTFU | - | 57% | - | - | - | - | - |
| Nyamathi et al., 2010 | Los Angeles, California, USA | 256 | 152 | 104 | OAT | People in OAT with moderate-heavy alcohol use at five sites promoting HAV/HBV vaccinations. | OAT | Incl: Moderateheavy alcohol use | - | - | - | 25% | - | - | - |
| Orellana et al., 2014 (Orellana, 2010) | NYC, USA | 356 | 356 | - | OAT | Males in heterosexual relationships in OAT. Parent study was a sample of males enrolled in at seven sites. | OAT | Incl: OAT > 3 months; Past year sexual partner | - | - | 34% | - | - | - | - |
| Palis et al., 2016 | Vancouver, Canada | 172 | 96 | 96 | Snowballing, Harm Reduction | Participants used opioids chronically from GeMa trial (≥5 years use, chronic use 6 months prior to survey, ≥1 OAT attempt). Recruited through snowballing and community. | OAT | Incl: ≥5 years use, ≥1 OAT attempt | 100%-Ever | 67% | 29% | 48% | 70% | 40% | 43% |
| Peles et al., 2016 (Peles et al., 2012) | Tel Aviv, Israel | 125 | 49 | 76 | OAT | People at OAT clinic and the CSA prevalence determined. Of initial group, 79 patients after LTFU. Next wave, invited all women in OAT to participate: 46 agreed. | DSM-4 OUD | Incl: Daily heroin use for ≥ 1 year Excl: LTFU (19%) | - | 89% | 24% | - | - | - | - |
| Pinto et al., 2011 | USA (Multisite) | 137 | - | 137 | Rehabilitation, Detoxification | Women with > sub-threshold PTSD from six community-based treatment sites in different US regions from Women and Trauma Study (WTS). | DSM-4 Dependence | Incl: Past 6-month substance use; DSM-4 PTSD | - | 72% | - | 59% | |||
| Plotzker et al., 2007 | Philadelphia, Pennsylvania, USA | 113 | - | 113 | Snowballing, Harm Reduction | Women recruited from two needle and syringe programs. | Frequent Illicit Use | - | 100%- Past 3 month | 56% | - | 68% | - | - | - |
| Rodriguez et al., 2017 | Tulsa, Oklahoma, USA | 48 | - | - | OAT | Receiving buprenorphine at an addiction centre medicine practice. Patients approached during regular clinic visit with their physician. | OAT | - | - | - | - | - | 52% | - | 48% |
| Rovis D. et al., 2019 | Rijeka, Croatia, Koper, Slovenia | 167 | 129 | 38 | Rehabilitation, Detoxification | Participants recruited from two in-treatment Rehab. Programs in Croatia and Slovenia. OAT (86%) | DSM-5 OUD | - | - | - | 6% | 13% | 12% | 8% | 7% |
| Sansone et al., 2009 | Dayton, Ohio, USA | 113 | 61 | 52 | Rehabilitation, Detoxification | Participants presented for admission to sub-acute detoxification 24-hr care unit that uses buprenorphine. | Other Treatment | Excl: Withdrawal or psychosis | - | - | - | 40% | 60% | 23% | - |
| Santos Goni et al., 2010 | Castilla & León, Spain | 50 | - | 50 | Rehabilitation, Detoxification | Subset of women with opiate dependence from a sample of women at 27 residential centres. | ICD-10 Dependence | Excl: Severe depression, psychosis | - | 33%* | - | 47% | 59% | - | - |
| Sartor et al., 2014 | USA (Multisite) | 3513 | 2178 | 1335 | General Population | Sub-set of clinical and general community samples of people with OUD. Recruited by family pairs from five east coast university medical schools for case-control studies. | DSM-4 Dependence | Excl: Major psychotic illness | - | 32% | 11% | 13% | - | - | - |
| Schiff et al., 2010 (Schiff et al., 2006, 2002) | Israel (Multisite) | 144 | - | 144 | OAT | Women from methadone clinics in Israel were approached for their consent to participate. | OAT | Excl: Participant, social worker refused (25%) | - | 72% | - | - | - | - | - |
| Shand et al., 2011 (Conroy et al., 2009; Larance et al., 2018; Larney et al, 2016; Maloney et al., 2010, 2009, 2007; Shand et al., 2010) | Sydney, NSW, Australia | 1513 | 914 | 599 | OAT | Participants from CATS Study were receiving OAT for heroin dependence at 34 of 35 OAT clinics in Sydney. | OAT | - | - | 71% | 36% | 62% | 53% | 37% | 61% |
| Shannon, 2007 | Lexington, Kentucky, USA | 68 | - | 68 | Rehabilitation, Detoxification | Pregnant women entered unit to receive methadone-supervised detoxification or OAT. | OAT, other treatment | Incl: Pregnant | - | 39% | - | 30% | 50% | - | - |
| Somer et al., 2010 (Somer, 2003) | Northern Israel | 149 | - | 111 | OAT, Rehabilitation, Detoxification | Receiving treatment in main heroin recovery program of northern Israel. Detoxification (n=49), outpatient treatment (n=48), OAT (n=52). | OAT | Excl: < 3 weeks in program - | - | - | 30% | 28% | - | 42% | |
| Stein et al., 2017 | Fall River, Massachusetts, USA | 457 | 326 | 131 | Rehabilitation, Detoxification | Sample of patients seeking and admitted to inpatient opioid detoxification at 24-hour medically supervised detoxification facility. | Other treatment | - | - | 42% | 11% | 36% | 48% | 18% | 42% |
| Teegen and Zumbeck, 2000 | Northern Germany | 122 | 96 | 26 | Rehabilitation, Detoxification | Participants were recruited from 10 addiction therapy facilities, all of whom use opioids. 53% in OAT. | Other treatment | - | - | - | 4% | 16% | - | - | - |
| Vogel et al., 2011 | Basel, Switzerland | 193 | 128 | 65 | OAT | People from OAT, diacetylmorphine outpatient treatment centres. | OAT | - | - | 40% | 20% | 31% | 34% | 40% | 41% |
| Walker et al., 2014 | Dallas, Texas | 72 | 25 | 47 | Rehabilitation, Detoxification | Adolescents with “cheese” heroin SUD from residential drug treatment or juvenile detention programs. | Other treatment | Excl: Psychosis, withdrawal, suicidal/homicidal ideation | 13%-Ever | 17% | - | 17% | 11% | - | - |
| Wang et al., 2010 | Shanghai, China | 341 | 123 | 218 | Rehabilitation, Detoxification | Participants were currently injecting and recruited through convenience sampling from three government operated drug rehabilitation facilities. | DSM-4 Heroin Dependence | Excl: Cardiovascular, neurological issues | 100%-Past Month | 29% | 20% | 56% | 36% | - | - |
| Weiss et al., 2019 | Tel Aviv, Israel | 51 | 33 | 18 | OAT | Patients at an OAT clinic. All clients approached (81% participation). | OAT | Incl: OAT > 3 months | 63% -Ever | - | - | 53% | - | - | - |
| Wickersham et al., 2016 | Kuala Lumpur, Malaysia | 60 | - | 60 | Snowballing, Harm Reduction | Sub-set of women in OAT recruited from community sites and shelters. | OAT | Incl: Past year other illicit substance use | - | 27% | - | 47% | - | - | - |
Table Notes: Secondary studies cited in parentheses; Abbreviations: OAT=Opioid Agonist Therapy, IDU=Injecting Drug Use, OUD=Opioid Use Disorder; CM=Childhood Maltreatment, CSA= Childhood Sexual Abuse, CPA= Childhood Physical Abuse, CEA= Childhood Emotional Abuse, CPN=Childhood Physical Neglect, CEN=Childhood Emotional Neglect, LTFU: Lost to follow-up, PTSD: posttraumatic stress disorder, Incl= Key inclusion criteria for study, Excl= Key exclusion criteria for study
3.2. Prevalence of CM
Studies of people with OUD most commonly report frequency of childhood sexual abuse (k=53; n=20,522). Among samples of people with OUD, 41% of women reported a history of childhood sexual abuse (95%CI: 36–47%; k=38; n=8,478), compared to 16% of men (95%CI: 12–20%; k=25; n=9,940). A history of childhood physical abuse was reported by 38% of all people with OUD (95%CI: 33–44%; k=48; n=18,324) and 43% reported a history of emotional abuse (95%CI: 38–49%; k=31; n=11,8030). Prevalence of physical neglect was reported in 17 studies (n=7,504; 38%, 95%CI: 30–46%) and prevalence of emotional neglect was reported in 17 studies (n=6,964; 42%, 95%CI: 32–51%) among people with OUD. Every pooled estimate of CM reported substantial heterogeneity (Table 2). eAppendix 7 presents forest plots by study for each analysis.
Table 2:
Pooled prevalence estimates for each type of childhood maltreatment in people with opioid use disorder stratified by sample characteristics
| Sexual Abuse (Women) | Sexual Abuse (Men) | Physical Abuse | Emotional Abuse | Physical Neglect | Emotional Neglect | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Strata | Study (k) (Total N) | Estimate (95%CI) p-value | I2 | Study (k) (Total N) | Estimate (95%CI) p-value | I2 | Study (k) (Total N) | Estimate (95%CI) p-value | I2 | Study (k) (Total N) | Estimate (95%CI) p-value | I2 | Study (k) (Total N) | Estimate (95%CI) p-value | I2 | Study (k) (Total N) | Estimate (95%CI) p-value | I2 |
| Community Sample Estimates (95%CI)1 | k=193 | 18 (16–20) | - | k=104 | 8 (6–9) | - | k=157 | 23 (20–26) | - | k=42 | 36 (28–45) | k=13 | 16 (12–22) | - | k=18 | 18 (13–25) | - | |
| Sex | - | |||||||||||||||||
| Total | - | - | - | - | - | - | 48 (18324) | 38 (33–44) | 99 | 33 (11030) | 43 (38–49) | 97 | 17 (7504) | 38 (30–45) | 96 | 17 (6964) | 42 (32–51) | 99 |
| p<0.01* | p=0.40 | p=0.04* | p=0.38 | p=0.29 | ||||||||||||||
| Men | - | - | - | 25 (9940) | 16 (12–20) | 97 | 23 (9438) | 36 (27–46) | 99 | 15 (5847) | 39 (31–48) | 98 | 12 (4121) | 34 (25–44) | 98 | 11 (3960) | 38 (24–51) | 99 |
| Women | 38 (8478) | 41 (36–47) | 96 | - | - | - | 35 (7418) | 41 (35–47) | 97 | 19 (3735) | 50 (44–57) | 94 | 13 (2793) | 40 (32–49) | 95 | 11 (2458) | 45 (32–57) | 98 |
| Lifetime injecting history of sample | p=0.01* | p=0.01* | p<0.01* | p=0.68 | p<0.01* | p<0.01* | ||||||||||||
| <100% | 4 (658) | 25 (12–39) | 92 | 4 (1429) | 12 (6–18) | 92 | 7 (2426) | 30 (23–38) | 93 | 3 (915) | 41 (14–68) | 99 | 2 (513) | 18 (15–21) | - | 2 (463) | 44 (40–49) | - |
| 100% | 8 (2222) | 49 (36–61) | 97 | 4 (2443) | 27 (17–36) | 95 | 9 (4884) | 51 (40–63) | 98 | 7 (4423) | 47 (39–56) | 96 | 4 (3792) | 40 (32–47) | 95 | 5 (3775) | 58 (50–67) | 95 |
| Recruitment Setting | p=0.56 | p=0.56 | p=0.12 | p<0.01* | p<0.01* | p<0.01* | ||||||||||||
| General population subsample | 3 (699) | 41 (33–49) | - | 2 (740) | 13 (11–15) | - | 2 (1397) | 38 (36–41) | - | 2 (1128) | 26 (23–29) | - | 2 (1397) | 49 (46–52) | - | 2 (1397) | 19 (17–21) | - |
| CNCP patients with OUD | 1 (178) | 46 (39–54) | - | 1 (203) | 22 (16–28) | - | 1 (381) | 43 (38–48) | - | 1 (380) | 55 (50–60) | - | 1 (400) | 17 (13–21) | - | - | - | - |
| OUD treatment settings2 | 26 (5971) | 39 (32–47) | 97 | 17 (7120) | 14 (10–18) | 98 | 34 (12780) | 35 (28–42) | 99 | 21 (6308) | 42 (36–49) | 96 | 9 (2783) | 30 (20–39) | 96 | 11 (3092) | 41 (28–54) | 98 |
| Non-Treatment Settings3 | 8 (1630) | 46 (37–54) | 91 | 5 (1877) | 22 (12–32) | 95 | 11 (3766) | 47 (36–58) | 98 | 7 (3214) | 50 (40–60) | 95 | 5 (2924) | 52 (34–70) | 98 | 4 (2475) | 56 (44–68) | 92 |
Table Notes:
=Significant (<0.05) results subgroup comparison from stratified meta-analysis;
Estimates from series of meta-analyses by Stoltenborgh et al.1;
Abbreviations:
Treatment settings include Opioid Agonist Treatment (OAT), rehabilitation, and other inpatient services;
Non-Treatment Settings include harm reduction services, community samples of people who inject drugs, and prisons; k=number of studies, CNCP=Chronic Non-Cancer Pain
3.3. Sample characteristic associations
In stratified sub-analyses (Table 2), women reported significantly higher rates of childhood sexual and emotional abuse than men with OUD. Samples of people with a history of IDU and OUD had substantially higher rates of all types of CM, excluding emotional abuse, than samples with lower rates of history of IDU and OUD. Prevalence rates of sexual abuse among men, emotional abuse, physical neglect, and emotional neglect varied substantially in stratified analyses of recruitment setting. Meta-regressions of average sample age and CM prevalence did not produce significant results, however, in stratified meta-analyses of age, studies of adolescents reported significantly lower rates of sexual abuse among women and men and emotional abuse among all people with OUD. Further information is presented in eAppendix 7 of the supplementary material. There was insufficient information to examine childhood SES and parental SUD as potential sources of heterogeneity.
3.4. Quality and risk of bias of included studies
Table 3 displays results from stratified analyses of each prevalence estimate according to risk of bias. Study inclusion or exclusion criteria was associated with substantial variance for prevalence estimates of sexual abuse among men and emotional abuse among women. The method of assessment of OUD (i.e. evaluation assessed via structured interviews versus proxy measures) did not affect prevalence estimates of any type of CM. Studies that used similar definitions to the “gold standard” WHO or CDC definitions reported significantly higher prevalence rates of sexual abuse among men, physical abuse, and physical neglect compared to less rigorous measures. eAppendix 6 provides further detail on risk of bias measures and classifications by study.
Table 3:
Pooled prevalence estimates for each type of childhood maltreatment in people with opioid use disorder stratified by risk of bias measures
| Sexual Abuse (Women) | Sexual Abuse (Men) | Physical Abuse | Emotional Abuse | Physical Neglect | Emotional Neglect | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Strata | Study (k) (Total N) | Estimate (95%CI) p-value | I2 | Study (k) (Total N) | Estimate (95%CI) p-value | I2 | Study (k) (Total N) | Estimate (95%CI) p-value | I2 | Study (k) (Total N) | Estimate (95%CI) p-value | I2 | Study (k) (Total N) | Estimate (95%CI) p-value | I2 | Study (k) (Total N) | Estimate (95%CI) p-value | I2 |
| Inclusion/Exclusion criteria1 | p=0.17 | p<0.01* | p=0.09 | p=0.01* | p=0.35 | p=0.10 | ||||||||||||
| Low risk of inclusion/exclusion criteria bias | 26 (5637) | 39 (32–46) | 97 | 19 (6399) | 15 (11–19) | 96 | 31 (11756) | 35 (28–41) | 98 | 20 (5554) | 40 (32–48) | 97 | 12 (4543) | 34 (25–43) | 98 | 13 (4452) | 37 (25–49) | 99 |
| High risk of underestimate | 4 (921) | 40 (16–64) | 97 | 3 (1805) | 9 (3–15) | - | 8 (2597) | 40 (26–55) | 96 | 6 (2437) | 43 (29–56) | 95 | 1 (121) | 36 (27–45) | - | 1 (121) | 49 (40–58) | - |
| High risk of overestimate | 8 (1920) | 50 (41–59) | 94 | 3 (1736) | 26 (19–34) | - | 9 (3971) | 49 (38–60) | 98 | 5 (3039) | 57 (50–64) | 88 | 4 (2840) | 50 (30–71) | 99 | 3 (2391) | 58 (43–73) | - |
| OUD evaluation | p=0.09 | p=0.66 | p=0.42 | p=0.99 | p=1.00 | p=0.37 | ||||||||||||
| Structured evaluation (DSM, ICD) | 10 (3634) | 50 (37–63) | 98 | 10 (5354) | 17 (10–24) | 98 | 15 (9485) | 42 (29–55) | 99 | 12 (6219) | 40 (32–49) | 98 | 8 (3667) | 38 (26–50) | 98 | 7 (3405) | 36 (18–55) | 99 |
| Proxy measure (i.e. OAT, ~daily use, etc.) | 28 (4844) | 38 (33–43) | 94 | 15 (4586) | 15 (10–20) | 96 | 33 (8839) | 36 (32–41) | 95 | 19 (4811) | 43 (36–50) | 95 | 9 (3837) | 38 (27–49) | 98 | 10 (3559) | 45 (37–53) | 94 |
| CM Definition | p=0.18 | p<0.01* | p=0.04* | p=0.60 | p<0.01* | - | ||||||||||||
| Similar to WHO or CDC Definitions2 | 16 (3774) | 45 (36–59) | 97 | 16 (6038) | 21 (14–27) | 98 | 25 (11298) | 44 (38–49) | 98 | 22 (8237) | 43 (37–50) | 97 | 15 (6991) | 43 (35–50) | 97 | 17 (6694) | 42 (32–51) | 99 |
| Specific (e.g. ‘severe’, <15 year, etc.) | 13 (3782) | 35 (29–41) | 93 | 4 (3183) | 7 (3–10) | 93 | 8 (4498) | 30 (19–41) | 98 | 8 (2729) | 43 (30–55) | 96 | 1 (113) | 23 (16–32) | - | - | - | - |
| Non-specific (e.g. were you abused?) | 9 (922) | 43 (30–56) | 95 | 5 (719) | 10 (4–15) | 85 | 15 (2044) | 34 (27–40) | 91 | 1 (64) | 50 (37–63) | - | 1 (400) | 17 (13–21) | - | - | - | - |
Table Notes:
Further information on each study provided in eAppendix 6; :
See Panel 1 for additional details; Abbreviations: k=number of studies, CI= Confidence Intervals, OUD= Opioid Use Disorder, DSM=Diagnostic and Statistical Manual of Mental Disorders, OAT= Opioid Agonist Therapy, ICD=International Classification of Diseases, WHO=World Health Organization, CDC=Centers for Disease Control and Prevention
Publication year was associated with lower prevalence of physical and emotional neglect in meta-regressions. In stratified meta-analyses, studies published after 2010 reported higher rates of sexual abuse among men and significantly lower rates of emotional neglect among all people with OUD. Studies published in English reported higher rates of sexual abuse among men, physical neglect, and emotional neglect, however, only two non-English studies were included in these analyses. More detail is provided in eAppendix 7.
3.5. Sensitivity analyses
We performed sensitivity analyses by pooling CM estimates of studies with low risk of inclusion or exclusion criteria bias, studies excluding adolescents, studies with “gold-standard” definitions of CM, studies published in English, and studies published after 2010. Results from sensitivity analyses were similar to those presented in Table 1, however, I2 values remained significant. We present the results of sensitivity analyses in eAppendix 8.
3.6. Comparison to community samples
Figure 2 presents prevalence estimates for each type of CM among people with OUD alongside global, self-report estimates of each CM type from a series of reviews by Stoltenborgh et al (Stoltenborgh et al., 2015, 2013a, 2013b, 2012, 2011). Similar to the current review, studies included in the pooled estimates from Stoltenborgh et al were predominantly from North America (Stoltenborgh et al., 2015). Although it is difficult to formally compare the pooled estimates of CM prevalence from the different reviews, all pooled self-report estimates of CM prevalence are higher among people with OUD compared to community samples. Excluding emotional abuse, the 95% CIs of the two random-effects meta-analyses do not overlap.
Figure 2:
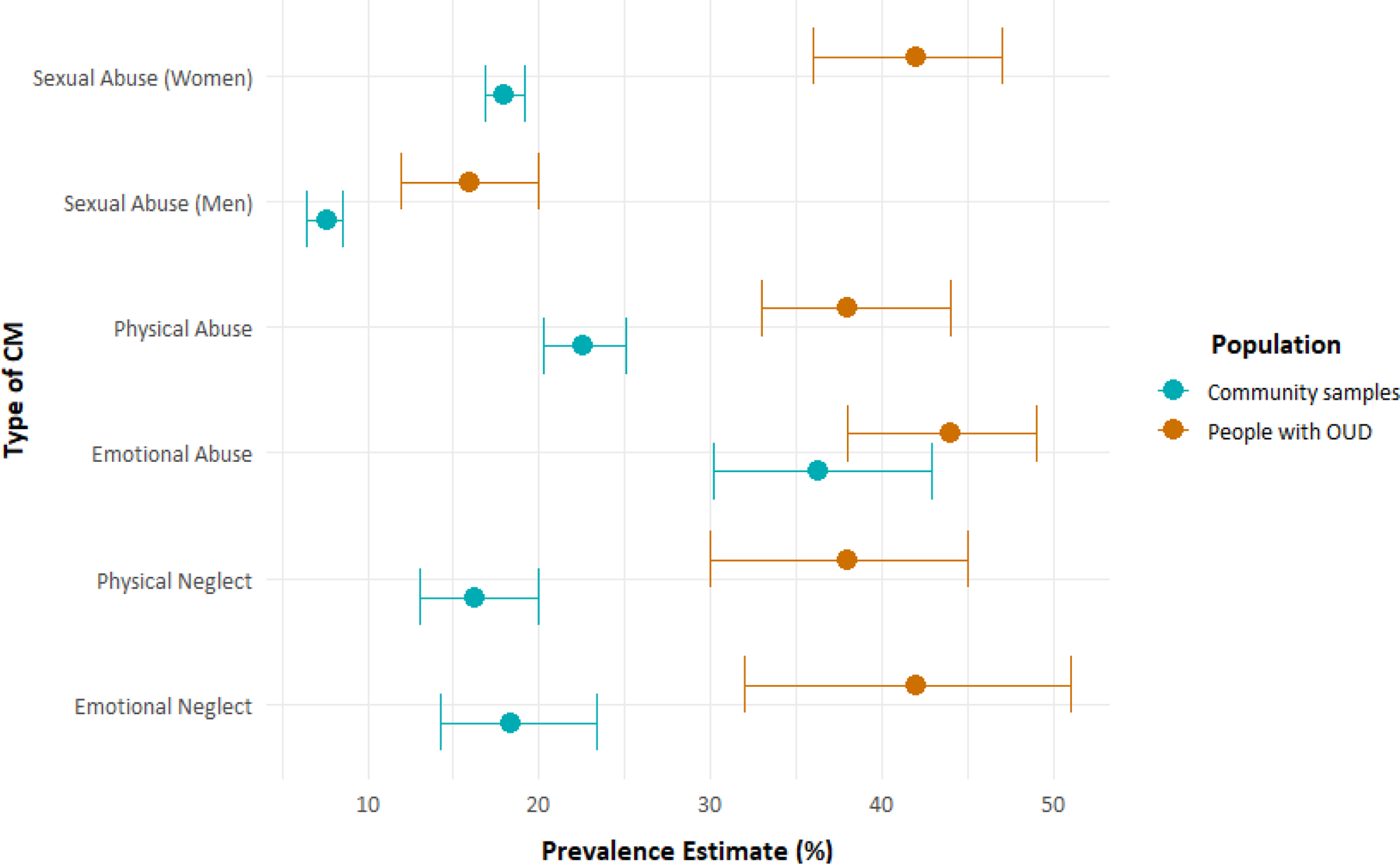
Prevalence estimates of childhood maltreatment (CM) among people with opioid use disorder (OUD) versus community samples
4. Discussion
4.1. Major findings and implications
The experience of CM among people with OUD was common, ranging between 16–43% across different types of CM. With the exception of emotional abuse, people with OUD report significantly higher rates of all types of CM when compared to community samples (Stoltenborgh et al., 2015). Our findings provide further evidence for CM as a risk factor for OUD (Conroy et al., 2009; Darke, 2013; Rossow and Lauritzen, 2001). Children who are abused or neglected often experience adversity and stress, which can increase risk of OUD later in life (Cicchetti and Handley, 2019). Additionally, CM and OUD share common environmental risk factors, including low SES (Young et al., 2007; Zielinski and Bradshaw, 2006) and parental SUD (Chatterjee et al., 2018), contributing to the elevated prevalence rates of CM among people with OUD.
There is clearly an integral relationship between a history of CM and OUD in adolescence and adulthood. Findings from the current review provide further evidence that prevention efforts of OUD may consider the long-term impact of CM. Policies that aim to reduce the overall prevalence of CM and opioid use following experience of CM, particularly during adolescence (Davis et al., 2019a), could help to reduce the burden of OUD in the general population (Afifi et al., 2012). Findings from the current review also have implications for interventions for people with OUD. Evidence suggests that experience of CM may affect an individual’s cognitions, beliefs, and feelings about their opioid use (Cicchetti and Handley, 2019). Additionally, there is strong evidence to support the relationship between CM and externalising disorders (Darke, 2011), which can play an important role in the frequency of opioid use (Cicchetti and Handley, 2019). The associations between CM and harms related to OUD, including overdose (Lake et al., 2015), alongside the extensive prevalence of CM among people with OUD reported in the current review, provides further evidence for interventions that aim to integrate CM experiences into OUD treatment.
Our findings underscore recommendations in clinical guidelines (Center for Substance Abuse Treatment, 2000) and research (Davis et al., 2019a, 2019b) for greater screening for CM among people in treatment for OUD. The high prevalence of CM within this population emphasises the importance of providing trauma-informed care for people with OUD, including the education of treatment providers around the sensitivities and complexities regarding disclosure of potentially traumatic experiences (Center for Substance Abuse Treatment, 2000; Elwyn and Smith, 2013). Trauma-informed care is critical for people with OUD because negative experiences with disclosure of victimisation is a significant treatment barrier, especially among women with OUD (Davis et al., 2019b; Green, 2006). Appropriate screening for experience of CM may also help to identify signs and symptoms of comorbid mental disorders, including depression (Center for Substance Abuse Treatment, 2000), post-traumatic stress disorder (Darke, 2013), and other anxiety-related disorders (Lawson et al., 2013). Since people with OUD and CM are more likely to present to treatment with comorbid mental disorders (Maloney et al., 2007); the findings of this review may have implications on the availability of treatment for comorbid mental disorders and OUD.
OAT is the most effective treatment for OUD (Degenhardt et al., 2019; Mattick et al., 2009; Sordo et al., 2017), including individuals with comorbid mental disorders (Trafton et al., 2006). However, people receiving OAT for OUD with a history of CM or comorbid mental disorders have higher levels of non-fatal overdose (Caudarella et al., 2016; Kang et al., 2002) and OAT treatment dropout (Hassan et al., 2017; Schiff et al., 2006), respectively. Adjunct psychosocial services have demonstrated mixed effectiveness in increasing retention in OAT and reducing psychological distress for people with OUD (Amato et al., 2011). There is some evidence that adjunct mental health and behavioural services may reduce symptoms of mental disorders among people with OUD (Fingleton et al., 2015; Hassan et al., 2017), including those who have experienced CM (Alexander, 2018). Examples of such services include psychopharmacological management of mental disorders (Hassan et al., 2017), cognitive behavioural therapy (Langdon et al., 2019; McHugh et al., 2017), and contingency management (Ainscough et al., 2017; Carroll and Weiss, 2017). Clinicians providing mental health treatment to people with OUD (Adams J.M. and Giroir B.P., 2019) may explore how experiences of CM can be integrated into comprehensive treatment plans for OUD and mental disorders (Davis et al., 2019b). Associations between inclusion or exclusion of participants with comorbid mental or substance use disorders and CM provides further evidence for the relationship between CM, polydrug use and mental health comorbidities. However, further research on the effective management of OUD among people with complex medical histories that include trauma and comorbid mental disorders is necessary.
Subgroup analyses of CM prevalence among different groups of people with OUD demonstrated that some groups of people with OUD have been exposed to higher rates of CM than others. Women with OUD reported significantly higher rates of childhood sexual abuse compared to men with OUD. Multiple studies included in our review report associations between CM and experience of revictimization and intimate partner violence among women with OUD (Engstrom et al., 2012, 2008; Green, 2006). People with a history of IDU and OUD, a clinical sample that commonly reports mental health comorbidities (Darke, 2011), reported elevated rates of multiple forms of CM. Finally, low rates of sexual abuse reported by adolescents are likely because these samples have not yet experienced the entire childhood period (Stoltenborgh et al., 2011) and fear of disclosure (Paine and Hansen, 2002) rather than true prevalence rates. Findings from the current review support further research on trauma-informed interventions (Alexander, 2018; Davis et al., 2019b) tailored to the needs and experiences of subgroups of people with OUD.
4.2. Limitations
Limitations of studies that assess CM prevalence among people with OUD are similar to limitations described in the wider literature on CM prevalence. For example, studies specific to people with OUD assess physical and sexual abuse most frequently (Stoltenborgh et al., 2015), despite evidence that all types of CM may have similar adverse health and social effects (Darke, 2011; Vachon et al., 2015). Several studies used questions that provided little detail on the experience of CM, which is critical to defining each CM type (Baldwin et al., 2019). The current review identified higher rates of CM in studies that used validated scales or definitions similar to the “gold standard” definitions for three of six pooled estimates, which implies that questions that require participant interpretation may be underestimating the true prevalence of CM.
Additionally, as all studies reported retrospective CM data, issues with memory and recall bias need to be considered when interpreting CM data (Baldwin et al., 2019). There is some concern that retrospective measures may identify a different group of people than prospective measurements of CM, particularly for individuals with substance use disorders (Elwyn and Smith, 2013). Despite these issues, use of retrospective measures do not necessarily indicate poor validity (Baldwin et al., 2019).
One notable limitation of existing evidence concerns sparse evidence on people with OUD whose primary opioid of concern is a pharmaceutical opioid, primarily because studies reporting on CM in such populations did not assess OUD as required for this review (Bouvier et al., 2019; Merrick et al., 2020; Williams J.R. et al., 2020). Given the widespread concerns over OUD among people prescribed opioids, more evidence on this population is needed.
Finally, there was substantial heterogeneity for each CM estimate. Heterogeneity is a common limitation in meta-analyses of retrospective CM data (Baldwin et al., 2019; Stoltenborgh et al., 2015), and inherent of many epidemiological reviews. Despite the heterogeneity, patterns identified in community samples (Stoltenborgh et al., 2015) were also identified in the current study, demonstrating consistency with the broader literature related to CM. For example, emotional abuse was the most prevalent type of CM reported by people with OUD and in community samples (Stoltenborgh et al., 2015; Vachon et al., 2015). Due to limited data, we were unable to control for potential sources of heterogeneity including childhood SES and parental SUD. However, we accounted for inclusion or exclusion of participants with comorbid mental or substance use disorders, language and year of publication, measurement of CM type, and geographic location in sensitivity analyses. Sensitivity analyses did not produce significantly different results to the pooled estimates of all studies of people with OUD that assessed CM.
4.3. Conclusions
This is the first systematic review and meta-analysis of CM prevalence among people with OUD. People with OUD commonly experience CM, and the prevalence of CM history is much higher than community samples. As such, comorbid mental health and SUD treatment providers should ensure that trauma-informed care for people with OUD is accessible, particularly for women and people with a history of IDU. Research on interventions that mitigate the long-term health and social consequences of CM among people with OUD is critical, and when appropriate, researchers should utilise validated instruments to assess history of CM.
Supplementary Material
Highlights.
Childhood maltreatment (CM) is common among people with opioid use disorder (OUD)
Women with OUD experience childhood sexual abuse (41%) more often than men (16%)
People with OUD often report childhood physical abuse (43%) and neglect (40%)
Most studies evaluate childhood sexual or physical abuse among OUD treatment samples
“Gold standard” definitions of CM produce the highest prevalence rates of CM
Acknowledgments
We would like to thank Shally Zhou and Carla Puca for their assistance with screening and data extraction. We would also like to thank all authors that provided additional data and information. In particular, we would like to thank the team at the British Columbia Centre on Substance Use for providing additional data from the Vancouver Injection Drug Users Study (VIDUS; US NIH Grant Number: U01DA038886), At-Risk Youth Study (ARYS; US NIH Grant Number: U01DA038886), and the AIDS Care Cohort to Evaluate Exposure to Survival Services (ACCESS) Cohorts (US NIH Grant Number: U01DA021525). We would also like to thank Dr. Sandra Müller, Dr. Margit Proescholdt, Dr. Michael Krausz, Dr. Saddichha Sahoo, and Dr. Brandon Marshall for providing additional information to inform decisions about study eligibility. Finally, we thank Phillip Hungerford for his assistance with graphics.
Role of Funding Source
The National Drug and Alcohol Research Centre (UNSW Sydney) is supported by funding from the Australian Government Department of Health under the Drug and Alcohol Program. TS is supported by higher degree research scholarship from the National Drug and Alcohol Research Centre (UNSW Sydney). LD and GC, are supported by Australian National Health and Medical Research Council (NHMRC) research fellowships (#1135991, #1119992). LD receives support from a US National Institute of Health (NIH) National Institute on Drug Abuse (NIDA) grant (R01DA1104470). NG is supported by a UNSW Scientia Fellowship. SC acknowledges PhD scholarship funding from the National Health and Medical Research Council and UNSW Scientia Scholarship funding schemes. The funders had no role in the design, data collection, analysis, interpretation of findings, or article submission.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
LD has received investigator-initiated untied educational grants for studies of opioid medications in Australia from Indivior and Seqirus. GC has received investigator-initiated untied educational grants for studies of opioid medications in Australia from Indivior. GLDT has received a consultancy fee for methodological support from Amgen Inc. outside the scope of this work.
References
- Adams JM, Giroir BP, 2019. Opioid Prescribing Trends and the Physician’s Role in Responding to the Public Health Crisis. JAMA Intern. Med 179, 476–478. 10.1001/jamainternmed.2018.7934 [DOI] [PubMed] [Google Scholar]
- Afifi TO, Henriksen CA, Asmundson GJG, Sareen J, 2012. Childhood Maltreatment and Substance Use Disorders among Men and Women in a Nationally Representative Sample. Can. J. Psychiatry 57, 677–686. 10.1177/070674371205701105 [DOI] [PubMed] [Google Scholar]
- Ainscough TS, Mcneill A, Strang J, Calder R, Brose LS, 2017. Contingency Management interventions for non-prescribed drug use during treatment for opiate addiction: A systematic review and meta-analysis. Drug Alcohol Depend 178, 318–339. 10.1016/j.drugalcdep.2017.05.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander K, 2018. The effect of a mindfulness intervention on the depression symptoms of mothers in treatment for an opioid use disorder. Diss. Abstr. Int. Sect. B Sci. Eng 79. [Google Scholar]
- Alexander K, Kronk R, Sekula K, Short V, Abatemarco D, 2019. Implementation of a Mindfulness Intervention for Women in Treatment for Opioid Use Disorder and Its Effects on Depression Symptoms. Issues Ment. Health Nurs 40, 690–696. 10.1080/01612840.2019.1585499 [DOI] [PubMed] [Google Scholar]
- Amato L, Minozzi S, Davoli M, Vecchi S, 2011. Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Database Syst. Rev 10.1002/14651858.CD004147.pub4 [DOI] [PubMed] [Google Scholar]
- Bailey RC, Hser Y-I, Hsieh S-C, Anglin MD, 1994. Influences affecting maintenance and cessation of narcotics addiction. J. Drug Issues 24, 249–272. [Google Scholar]
- Baldwin JR, Reuben A, Newbury JB, Danese A, 2019. Agreement Between Prospective and Retrospective Measures of Childhood Maltreatment. JAMA Psychiatry 76, 584 10.1001/jamapsychiatry.2019.0097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett D, Manly JT, Cicchetti D, Toth SL, 1993. Child abuse, child development, and social policy.
- Bartholomew NG, Courtney K, Rowan-Szal GA, Simpson DD, 2005. Sexual abuse history and treatment outcomes among women undergoing methadone treatment. J. Subst. Abuse Treat 29, 231–235. [DOI] [PubMed] [Google Scholar]
- Blanco C, Wall MM, Liu S-M, Olfson M, 2020. Toward a comprehensive developmental model of prescription opioid use disorder. J. Clin. Psychiatry 81, 19m12775 10.4088/JCP.19m12775 [DOI] [PubMed] [Google Scholar]
- Blatchley RJ, Hanlon TE, Nurco DN, O’Grady K, 2000. Childhood sexual abuse among female addicts and changes in parenting across two generations 14–1.
- Bohnert AS, Roeder KM, Ilgen MA, 2011. Suicide attempts and overdoses among adults entering addictions treatment: comparing correlates in a U.S. National Study. Drug Alcohol Depend 119, 106–12. 10.1016/j.drugalcdep.2011.05.032 [DOI] [PubMed] [Google Scholar]
- Bonoldi I, Simeone E, Rocchetti M, Codjoe L, Rossi G, Gambi F, Balottin U, Caverzasi E, Politi P, Fusar-Poli P, 2013. Prevalence of self-reported childhood abuse in psychosis: A meta-analysis of retrospective studies 210, 8–15. 10.1016/j.psychres.2013.05.003 [DOI] [PubMed] [Google Scholar]
- Bouvier BA, Kinnard EN, Yedinak JL, Li Y, Elston B, Green TC, Hadland SE, Marshall BDL, 2019. Prevalence and Correlates of Depressive Symptomology among Young Adults Who Use Prescription Opioids Non-medically. J. Psychoactive Drugs 51, 441–452. 10.1080/02791072.2019.1654151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady JE, Giglio R, Keyes KM, DiMaggio C, Li G, 2017. Risk markers for fatal and non-fatal prescription drug overdose: a meta-analysis. Inj Epidemiol 4, 24 10.1186/s40621-017-0118-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braitstein P, Li K, Tyndall M, Spittal P, O’Shaughnessy MV, Schilder A, Johnston C, Hogg RS, Schechter MT, 2003. Sexual violence among a cohort of injection drug users. Soc. Sci. Med 57, 561–569. 10.1016/s0277-9536(02)00403-3 [DOI] [PubMed] [Google Scholar]
- Browne R, Keating S, O’Connor JJ, 1998. Sexual abuse in childhood and subsequent illicit drug abuse in adolescence and early adulthood. Ir. J. Psychol. Med 15, 123–126. 10.1017/S079096670000481X [DOI] [Google Scholar]
- Camacho LM, Bartholomew NG, Joe GW, Cloud MA, Simpson DD, 1996. Gender, cocaine and during-treatment HIV risk reduction among injection opioid users in methadone maintenance. Drug Alcohol Depend 41, 1–7. 10.1016/0376-8716(96)01235-5 [DOI] [PubMed] [Google Scholar]
- Campbell G, Bruno R, Darke S, Shand F, Hall W, Farrell M, Degenhardt L, 2016. Prevalence and correlates of suicidal thoughts and suicide attempts in people prescribed pharmaceutical opioids for chronic pain. Clin. J. Pain 32, 292–301. 10.1097/AJP.0000000000000283 [DOI] [PubMed] [Google Scholar]
- Carroll KM, Weiss RD, 2017. The role of behavioral interventions in buprenorphine maintenance treatment: a review. Am. J. Psychiatry 174, 738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cash SJ, Wilke DJ, 2003. An Ecological Model of Maternal Substance Abuse and Child Neglect: Issues, Analyses, and Recommendations. Am. J. Orthopsychiatry 73, 392–404. 10.1037/0002-9432.73.4.392 [DOI] [PubMed] [Google Scholar]
- Caudarella A, Dong H, Milloy MJ, Kerr T, Wood E, Hayashi K, 2016. Non-fatal overdose as a risk factor for subsequent fatal overdose among people who inject drugs. Drug Alcohol Depend. 162, 51–55. 10.1016/j.drugalcdep.2016.02.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment, 2000. Substance abuse treatment for persons with child abuse and neglect issues. [PubMed]
- Chatterjee A, Yu EJ, Tishberg L, 2018. Exploring opioid use disorder, its impact, and treatment among individuals experiencing homelessness as part of a family. Drug Alcohol Depend 188, 161–168. [DOI] [PubMed] [Google Scholar]
- Cheng T, Small W, Nosova E, Hogg B, Hayashi K, Kerr T, DeBeck K, 2018. Nonmedical prescription opioid use and illegal drug use: initiation trajectory and related risks among people who use illegal drugs in Vancouver, Canada. BMC Res. Notes 11, 35 10.1186/s13104-018-3152-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Handley ED, 2019. Child maltreatment and the development of substance use and disorder. Neurobiol. Stress 10, 100144 10.1016/j.ynstr.2018.100144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Valentino K, 2006. An ecological-transactional perspective on child maltreatment: Failure of the average expectable environment and its influence on child development, in: Developmental Psychopathology: Risk, Disorder, and Adaptation, Vol. 3, 2nd Ed. John Wiley & Sons Inc, Hoboken, NJ, US, pp. 129–201. [Google Scholar]
- Cohen LR, Tross S, Pavlicova M, Hu MC, Campbell AN, Nunes EV, 2009. Substance use, childhood sexual abuse, and sexual risk behavior among women in methadone treatment. Am. J. Drug Alcohol Abuse 35, 305–10. 10.1080/00952990903060127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy E, Degenhardt L, Mattick RP, Nelson EC, 2009. Child maltreatment as a risk factor for opioid dependence: Comparison of family characteristics and type and severity of child maltreatment with a matched control group. Child Abuse Negl 33, 343–352. 10.1016/j.chiabu.2008.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S, 2013. Pathways to heroin dependence: time to re‐ appraise self‐ medication. Addiction 108, 659–667. [DOI] [PubMed] [Google Scholar]
- Darke S, 2011. The life of the heroin user: typical beginnings, trajectories and outcomes. Cambridge University Press. [Google Scholar]
- Darke S, Ross J, 2002. Suicide among heroin users: rates, risk factors and methods. Addiction 97, 1383–1394. 10.1046/j.1360-0443.2002.00214.x [DOI] [PubMed] [Google Scholar]
- Darke S, Torok M, 2014. The association of childhood physical abuse with the onset and extent of drug use among regular injecting drug users. Addiction 109, 610–616. 10.1111/add.12428 [DOI] [PubMed] [Google Scholar]
- Darke S, Torok M, 2013. Childhood physical abuse, non-suicidal self-harm and attempted suicide amongst regular injecting drug users. Drug Alcohol Depend 133, 420–426. 10.1016/j.drugalcdep.2013.06.026 [DOI] [PubMed] [Google Scholar]
- Davis JP, Dworkin ER, Helton J, Prindle J, Patel S, Dumas TM, Miller S, 2019a. Extending poly-victimization theory: Differential effects of adolescents’ experiences of victimization on substance use disorder diagnoses upon treatment entry. Child Abuse Negl 89, 165–177. 10.1016/j.chiabu.2019.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JP, Prindle JJ, Eddie D, Pedersen ER, Dumas TM, Christie NC, 2019b. Addressing the opioid epidemic with behavioral interventions for adolescents and young adults: A quasi-experimental design. J. Consult. Clin. Psychol 87, 941–951. 10.1037/ccp0000406 [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Grebely J, Stone J, Hickman M, Vickerman P, Marshall BDL, Bruneau J, Altice FL, Henderson G, Rahimi-Movaghar A, Larney S, 2019. Global patterns of opioid use and dependence: harms to populations, interventions, and future action. Lancet 394, 1560–1579. 10.1016/s0140-6736(19)32229-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derefinko KJ, Salgado Garcia FI, Talley KM, Bursac Z, Johnson KC, Murphy JG, McDevitt-Murphy ME, Andrasik F, Sumrok DD, 2019. Adverse childhood experiences predict opioid relapse during treatment among rural adults. Addict. Behav 96, 171–174. 10.1016/j.addbeh.2019.05.008 [DOI] [PubMed] [Google Scholar]
- Dissabandara LO, Dias SR, Dodd PR, Stadlin A, 2009. Patterns of substance use in male incarcerated drug users in Sri Lanka. Drug Alcohol Rev 28, 600–7. 10.1111/j.1465-3362.2009.00062.x [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Gilbert L, Schilling R, Wada T, 2000. Drug abuse and partner violence among women in methadone treatment. J. Fam. Violence 15, 209–228. 10.1023/A:1007532917759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Marotta PL, Goddard-Eckrich D, Chang M, Hunt T, Wu E, Gilbert L, 2019. Drug overdose among women in intimate relationships: The role of partner violence, adversity and relationship dependencies. PLoS ONE 14, e0225854 10.1371/journal.pone.0225854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Simoni JM, Cooper DK, Gilbert L, Schilling RF, 2001. Sex trading and psychological distress among women on methadone. Psychol. Addict. Behav 15, 177–184. 10.1037/0893-164X.15.3.177 [DOI] [PubMed] [Google Scholar]
- Elhammady M, Awara M, Aty AA, Yousef S, Moselhy HF, 2014. Self-reported child sexual abuse, physical abuse, and parental history of drug misuse in opioid dependence syndrome. Addict. Disord. Their Treat 13, 151–158. 10.1097/ADT.0b013e31829bb3b9 [DOI] [Google Scholar]
- Elliott K, Urquiza A, 2006. Ethnicity, Culture, and Child Maltreatment. J. Soc. Issues 62, 787–809. 10.1111/j.1540-4560.2006.00487.x [DOI] [Google Scholar]
- Elwyn L, Smith C, 2013. Child Maltreatment and Adult Substance Abuse: The Role of Memory. J. Soc. Work Pract. Addict 13, 269–294. 10.1080/1533256x.2013.814483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engstrom M, El-Bassel N, Gilbert L, 2012. Childhood sexual abuse characteristics, intimate partner violence exposure, and psychological distress among women in methadone treatment. J. Subst. Abuse Treat 43, 366–376. 10.1016/j.jsat.2012.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engstrom M, El-Bassel N, Go H, Gilbert L, 2008. Childhood sexual abuse and intimate partner violence among women in methadone treatment: A direct or mediated relationship? J. Fam. Violence 23, 605–617. 10.1007/s10896-008-9183-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engstrom M, Winham K, Gilbert L, 2016. Types and Characteristics of Childhood Sexual Abuse: How Do They Matter in HIV Sexual Risk Behaviors Among Women in Methadone Treatment in New York City? Subst. Use Misuse 51, 277–94. 10.3109/10826084.2015.1058823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans EA, Goff SL, Upchurch DM, Grella CE, 2020. Childhood adversity and mental health comorbidity in men and women with opioid use disorders. Addict. Behav 102, 106149 10.1016/j.addbeh.2019.106149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fingleton N, Matheson C, Jaffray M, 2015. Changes in mental health during opiate replacement therapy: A systematic review. Drugs Educ. Prev. Policy 22, 1–18. 10.3109/09687637.2014.899986 [DOI] [Google Scholar]
- Fudalej S, Ilgen M, Kolodziejczyk I, Podgorska A, Serafin P, Barry K, Wojnar M, Blow FC, Bohnert A, 2015. Somatic Comorbidity and Other Factors Related to Suicide Attempt Among Polish Methadone Maintenance Patients. J. Addict. Med 9, 433–9. 10.1097/ADM.0000000000000153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner SM, Cottrill AC, McKnight ER, Cottrill CB, Bonny A, 2020. 260. Trauma and Resiliency in Adolescents and Young Adults with Opioid Use and Eating Disorders. J. Adolesc. Health, Adolescent Health: Transforming Risk to Wellness. United States. 66, S131–S132. 10.1016/j.jadohealth.2019.11.263 [DOI] [Google Scholar]
- Garfield JB, Cotton SM, Allen NB, Cheetham A, Kras M, Yucel M, Lubman DI, 2017. Evidence that anhedonia is a symptom of opioid dependence associated with recent use. Drug Alcohol Depend 177, 29–38. 10.1016/j.drugalcdep.2017.03.012 [DOI] [PubMed] [Google Scholar]
- GBD 2017 causes of death collaborators, 2018. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1736–1788. 10.1016/s0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghorbani F, Khosravani V, Mohammadzadeh A, Shadnia S, 2019. The role of emotion dysregulation in the relation of childhood trauma to heroin craving in individuals with heroin dependence. Drug Alcohol Depend 195, 132–139. 10.1016/j.drugalcdep.2018.12.008 [DOI] [PubMed] [Google Scholar]
- Gilbert L, El-Bassel N, Schilling RF, Friedman E, 1997. Childhood abuse as a risk for partner abuse among women in methadone maintenance. Am. J. Drug Alcohol Abuse 23, 581–595. 10.3109/00952999709016897 [DOI] [PubMed] [Google Scholar]
- Gilbert L, El-Bassel N, Schilling RF, Wada T, Bennet B, 2000. Partner violence and sexual HIV risk behaviors among women in methadone treatment. AIDS Behav 4, 261–269. 10.1023/A:1009568718804 [DOI] [Google Scholar]
- Golden FM, 2018. Lived experiences and coping styles of Alaskan women with opioid use disorders. Diss. Abstr. Int. Sect. B Sci. Eng 78, No Pagination Specified. [Google Scholar]
- Green CA, 2006. Gender and use of substance abuse treatment services. Alcohol Res. Health J. Natl. Inst. Alcohol Abuse Alcohol 29, 55–62. [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Annon JJ, Anglin MD, 1995. Ethnic Differences in HIV Risk Behaviors, Self-Perceptions, and Treatment Outcomes among Women in Methadone Maintenance Treatment. J. Psychoactive Drugs 27, 421–433. 10.1080/02791072.1995.10471706 [DOI] [PubMed] [Google Scholar]
- Hall W, Degenhardt L, Hickman M, 2020. Generational trends in US opioid-overdose deaths. Nat. Med 26, 651–652. 10.1038/s41591-020-0875-7 [DOI] [PubMed] [Google Scholar]
- Harbord R, Higgins J, 2009. Metareg: Stata module to perform meta-analysis regression.
- Hassan AN, Howe AS, Samokhvalov AV, Le Foll B, George TP, 2017. Management of mood and anxiety disorders in patients receiving opioid agonist therapy: Review and meta-analysis. Am. J. Addict 26, 551–563. 10.1111/ajad.12581 [DOI] [PubMed] [Google Scholar]
- Hassan AN, Le Foll B, 2019. Polydrug use disorders in individuals with opioid use disorder. Drug Alcohol Depend 198, 28–33. 10.1016/j.drugalcdep.2019.01.031 [DOI] [PubMed] [Google Scholar]
- Heffernan K, Cloitre M, Tardiff K, Marzuk PM, Portera L, Leon AC, 2000. Childhood trauma as a correlate of lifetime opiate use in psychiatric patients. Addict. Behav 25, 797–803. 10.1016/S0306-4603(00)00066-6 [DOI] [PubMed] [Google Scholar]
- Hien DA, Nunes E, Levin FR, Fraser D, 2000. Posttraumatic stress disorder and short-term outcome in early methadone treatment. J. Subst. Abuse Treat 19, 31–37. 10.1016/S0740-5472(99)00088-4 [DOI] [PubMed] [Google Scholar]
- Isralowitz R, Afifi M, Rawson RA, 2002. Drug problems: cross-cultural policy and program development. Greenwood Publishing Group. [Google Scholar]
- Isralowitz R, Bar Hamburger R, 2002. Immigrant and native-born female heroin addicts in Israel. J. Psychoactive Drugs 34, 97–103. [DOI] [PubMed] [Google Scholar]
- Isralowitz RE, 2001. Toward an understanding of Russian speaking heroin addicts and drug treatment services in Israel. J. Soc. Work Pract. Addict 1, 33–44. 10.1300/J160v01n02_04 [DOI] [Google Scholar]
- Jones D, Trudinger P, Crawford M, 2004. Intelligence and achievement of children referred following sexual abuse 40, 455–460. 10.1111/j.1440-1754.2004.00427.x [DOI] [PubMed] [Google Scholar]
- Kaboski JR, 2013. An empirically-derived typology of risks for mothers with substance use problems. Diss. Abstr. Int. Sect. Humanit. Soc. Sci 74, No Pagination Specified. [Google Scholar]
- Kang SY, Deren S, Goldstein MF, 2002. Relationships between childhood abuse and neglect experience and HIV risk behaviors among methadone treatment drop-outs. Child Abuse Negl 26, 1275–1289. 10.1016/S0145-2134(02)00412-X [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett KA, 2004. Health consequences of abuse in the family: A clinical guide for evidence-based practice. American Psychological Association. [Google Scholar]
- Kerr T, Stoltz J-A, Marshall BDL, Lai C, Strathdee SA, Wood E, 2009. Childhood Trauma and Injection Drug Use Among High-Risk Youth. J. Adolesc. Health 45, 300–302. 10.1016/j.jadohealth.2009.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khosravani V, Messman-Moore TL, Mohammadzadeh A, Ghorbani F, Amirinezhad A, 2019. Effects of childhood emotional maltreatment on depressive symptoms through emotion dysregulation in treatment-seeking patients with heroin-dependence. J. Affect. Disord 256, 448–457. 10.1016/j.jad.2019.06.021 [DOI] [PubMed] [Google Scholar]
- Koyuncu A, Mirsal H, Yavuz M, Kalyoncu O, Beyazyurek M, 2003. Suicide ideation, planning and attempt of heroin dependent patients. Bagimlik Derg 4, 101–104. [Google Scholar]
- Kumar N, Stowe ZN, Han X, Mancino MJ, 2016. Impact of early childhood trauma on retention and phase advancement in an outpatient buprenorphine treatment program. Am. J. Addict 25, 542–8. 10.1111/ajad.12437 [DOI] [PubMed] [Google Scholar]
- Lake S, Hayashi K, Milloy M-J, Wood E, Dong H, Montaner J, Kerr T, 2015. Associations between childhood trauma and non-fatal overdose among people who inject drugs 43, 83–88. 10.1016/j.addbeh.2014.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langdon KJ, Dove K, Ramsey S, 2019. Comorbidity of opioid-related and anxiety-related symptoms and disorders. Curr. Opin. Psychol 30, 17–23. 10.1016/j.copsyc.2018.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larance B, Gisev N, Cama E, Nelson EC, Darke S, Larney S, Degenhardt L, 2018. Predictors of transitions across stages of heroin use and dependence prior to treatment-seeking among people in treatment for opioid dependence. Drug Alcohol Depend 191, 145–151. 10.1016/j.drugalcdep.2018.03.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larney S, Cama E, Nelson E, Larance B, Degenhardt L, 2016. A cross-sectional study of correlates of imprisonment in opioid-dependent men and women in New South Wales, Australia. Drug Alcohol Rev 35, 686–692. 10.1111/dar.12357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larney S, Tran LT, Leung J, Santo T, Santomauro D, Hickman M, Peacock A, Stockings E, Degenhardt L, 2020. All-cause and cause-specific mortality among people using extramedical opioids: a systematic review and meta-analysis. JAMA Psychiatry 77, 493–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson KM, Back SE, Hartwell KJ, Maria MMS, Brady KT, 2013. A comparison of trauma profiles among individuals with prescription opioid, nicotine, or cocaine dependence. Am. J. Addict 22, 127–131. 10.1111/j.1521-0391.2013.00319.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeb R, Paulozzi L, Melanson C, Simon T, Arias I, 2008. Child maltreatment surveillance: Uniform definitions for public health and recommended data elements. Centers for Disease Control and Prevention (CDC). [Google Scholar]
- Lovell AM, 2002. Risking risk: The influence of types of capital and social networks on the injection practices of drug users. Soc. Sci. Med 55, 803–821. 10.1016/S0277-9536(01)00204-0 [DOI] [PubMed] [Google Scholar]
- Maloney E, Degenhardt L, Darke S, Mattick RP, Nelson E, 2007. Suicidal behaviour and associated risk factors among opioid-dependent individuals: A case-control study. Addiction 102, 1933–1941. 10.1111/j.1360-0443.2007.01971.x [DOI] [PubMed] [Google Scholar]
- Maloney E, Degenhardt L, Darke S, Nelson EC, 2010. Investigating the co-occurrence of self-mutilation and suicide attempts among opioid-dependent individuals. Suicide Life. Threat. Behav 40, 50–62. 10.1521/suli.2010.40.1.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maloney E, Degenhardt L, Darke S, Nelson EC, 2009. Are non-fatal opioid overdoses misclassified suicide attempts? Comparing the associated correlates. Addict. Behav 34, 723–9. 10.1016/j.addbeh.2009.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Keyes KM, Storr CL, Zhu H, Chilcoat HD, 2009. Pathways between nonmedical opioid use/dependence and psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend 103, 16–24. 10.1016/j.drugalcdep.2009.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M, 2009. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst. Rev 10.1002/14651858.cd002209.pub2 [DOI] [PubMed] [Google Scholar]
- McCurdy SA, Ross MW, Williams ML, Kilonzo GP, Leshabari MT, 2010. Flashblood: blood sharing among female injecting drug users in Tanzania. Addiction 105, 1062–70. 10.1111/j.1360-0443.2010.02908.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Votaw VR, Barlow DH, Fitzmaurice GM, Greenfield SF, Weiss RD, 2017. Development of an integrated cognitive behavioral therapy for anxiety and opioid use disorder: Study protocol and methods. Contemp. Clin. Trials 60, 105–112. 10.1016/j.cct.2017.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medrano MA, Desmond DP, Zule WA, Hatch JP, 1999. Histories of childhood trauma and the effects on risky HIV behaviors in a sample of women drug users. Am. J. Drug Alcohol Abuse 25, 593–606. 10.1081/ADA-100101881 [DOI] [PubMed] [Google Scholar]
- Merrick MT, Ford DC, Haegerich TM, Simon T, 2020. Adverse Childhood Experiences Increase Risk for Prescription Opioid Misuse. J. Prim. Prev 41, 139–152. 10.1007/s10935-020-00578-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller-Perrin CL, Perrin R %J C. maltreatment: A. introduction, 2013. History and definitions of child maltreatment 1–29.
- Mirhashem R, Allen HC, Adams ZW, van Stolk-Cooke K, Legrand A, Price M, 2017. The intervening role of urgency on the association between childhood maltreatment, PTSD, and substance-related problems. Addict. Behav 69, 98–103. 10.1016/j.addbeh.2017.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, 2009. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med 151, 264 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- Moselhy HF, 2009. Co-morbid post-traumatic stress disorder and opioid dependence syndrome. J. Dual Diagn 5, 30–40. 10.1080/15504260802620293 [DOI] [Google Scholar]
- Moselhy HF, Fahmy E, Mikhael VS, El-Sheikh H, 2010. Impact of self-reported life events on the profile of opioid dependence syndrome. Am. J. Drug Alcohol Abuse 36, 7–12. 10.3109/00952990903544786 [DOI] [PubMed] [Google Scholar]
- Naqavi MR, Mohammadi M, Salari V, Nakhaee N, 2011. The Relationship between Childhood Maltreatment and Opiate Dependency in Adolescence and Middle Age. Addict. Health 3, 92–98. [PMC free article] [PubMed] [Google Scholar]
- Needle RH, Su S, Doherty WJ, 1990. Divorce, remarriage, and adolescent drug involvement: A longitudinal study. J. Marriage Fam 52, 157–169. [Google Scholar]
- Nelson EC, Heath AC, Lynskey MT, Bucholz KK, Madden PAF, Statham DJ, Martin NG, 2006. Childhood sexual abuse and risks for licit and illicit drug-related outcomes: A twin study. Psychol. Med 36, 1473–1483. 10.1017/S0033291706008397 [DOI] [PubMed] [Google Scholar]
- Nyaga VN, Arbyn M, Aerts M, 2014. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch. Public Health 72, 39 10.1186/2049-3258-72-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A, Tyler D, Sinha K, Marfisee M, Cohen A, Greengold B, 2010. Predictors of hepatitis knowledge improvement among methadone maintained clients enrolled in a hepatitis intervention program. J. Community Health 35, 423–32. 10.1007/s10900-010-9266-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orellana ER, 2010. Childhood sexual abuse, sex trading and hiv risks among men in methadone treatment: The mediating effects of early sexual and substance use initiation, mental health and adult substance use factors. Diss. Abstr. Int. Sect. Humanit. Soc. Sci 70, 3194. [Google Scholar]
- Orellana ER, El-Bassel N, Gilbert L, Miller KM, Catania J, Epperson M, Wu E, 2014. Sex trading and other HIV risks among drug- involved men: Differential associations with childhood sexual abuse. Soc. Work Res 38, 117–126. 10.1093/swr/svu012 [DOI] [Google Scholar]
- Paine ML, Hansen DJ, 2002. Factors influencing children to self-disclose sexual abuse. Clin. Psychol. Rev 22, 271–295. 10.1016/s0272-7358(01)00091-5 [DOI] [PubMed] [Google Scholar]
- Palis H, Marchand K, Peng D, Fikowski J, Harrison S, Spittal P, Schechter MT, Oviedo-Joekes E, 2016. Factors Associated with Perceived Abuse in the Health Care System Among Long-Term Opioid Users: A Cross-Sectional Study. Subst. Use Misuse 51, 763–76. 10.3109/10826084.2016.1155605 [DOI] [PubMed] [Google Scholar]
- Panchanadeswaran S, El-Bassel N, Gilbert L, Wu E, Chang M, 2008. An examination of the perceived social support levels of women in methadone maintenance treatment programs who experience various forms of intimate partner violence. Womens Health Issues 18, 35–43. 10.1016/j.whi.2007.10.007 [DOI] [PubMed] [Google Scholar]
- Peles E, Potik D, Schreiber S, Bloch M, Adelson M, 2012. Psychiatric comorbidity of patients on methadone maintenance treatment with a history of sexual abuse. Eur. Neuropsychopharmacol 22, 883–891. 10.1016/j.euroneuro.2012.04.002 [DOI] [PubMed] [Google Scholar]
- Peles E, Seligman Z, Bloch M, Potik D, Sason A, Schreiber S, Adelson M, 2016. Sexual Abuse and its Relation to Chronic Pain among Women from a Methadone Maintenance Clinic versus a Sexual Abuse Treatment Center. J. Psychoactive Drugs 48, 279–287. 10.1080/02791072.2016.1205763 [DOI] [PubMed] [Google Scholar]
- Pinto RM, Campbell ANC, Hien DA, Yu G, Gorroochurn P, 2011. Retention in the National Institute on Drug Abuse Clinical Trials Network Women and Trauma Study: Implications for Posttrial Implementation. Am. J. Orthopsychiatry 81, 211–217. 10.1111/j.1939-0025.2011.01090.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plotzker RE, Metzger DS, Holmes WC, 2007. Childhood sexual and physical abuse histories, PTSD, depression, and HIV risk outcomes in women injection drug users: a potential mediating pathway. Am. J. Addict 16, 431–438. [DOI] [PubMed] [Google Scholar]
- Rodriguez K, Davis S, Ferguson Z, Suthar K, Jelley M, 2017. Adverse childhood experiences in addiction medicine patients receiving buprenorphine therapy. J. Gen. Intern. Med 32 (2 Supplement 1), S109. [Google Scholar]
- Rojas VC, 2006. Post-Traumatic Stress Disorder as a risk factor for HIV among African American and Latina women in methadone treatment in New York City. Diss. Abstr. Int. Sect. Humanit. Soc. Sci 66, 2726. [Google Scholar]
- Rossow I, Lauritzen G, 2001. Shattered childhood: a key issue in suicidal behavior among drug addicts? Addiction 96, 227–240. 10.1046/j.1360-0443.2001.9622275.x [DOI] [PubMed] [Google Scholar]
- Rovis D, Vasiljev V, Jenko-Praznikar Z, Petelin A, Drevensek G, Peruc D, Cernelic-Bizjak M, 2019. Mental health and drug use severity: the role of substance P, neuropeptide Y, self-reported childhood history of trauma, parental bonding and current resiliency. J Ment Health. 10.1080/09638237.2019.1644492 [DOI] [PubMed] [Google Scholar]
- Sansone RA, Whitecar P, Wiederman MW, 2009. The prevalence of childhood trauma among those seeking buprenorphine treatment. J. Addict. Dis 28, 64–67. 10.1080/10550880802545101 [DOI] [PubMed] [Google Scholar]
- Santos Goni MA, Garcia Colmenero L, Bernardo Carrasco A, Quijano Arenas E, Sanchez Pardo L, 2010. Traumatic events among drugs addict women: Childhood sexual, physical and psychological abuse. [Spanish]. Trastor. Adict 12, 109–117. 10.1016/S1575-0973(10)70021-0 [DOI] [Google Scholar]
- Sartor CE, Kranzler HR, Gelernter J, 2014. Rate of progression from first use to dependence on cocaine or opioids: a cross-substance examination of associated demographic, psychiatric, and childhood risk factors. Addict. Behav 39, 473–9. 10.1016/j.addbeh.2013.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiff M, El-bassel N, Engstrom M, Gilbert L, 2002. Psychological distress and intimate physical and sexual abuse among women in methadone maintenance treatment programs. Soc. Serv. Rev 76, 302–320. 10.1086/339665 [DOI] [Google Scholar]
- Schiff M, Gilbert L, El-Bassel N, 2006. Perceived positive aspects of intimate relationships among abused women in Methadone Maintenance Treatment Programs (MMTP). J. Interpers. Violence 21, 121–138. 10.1177/0886260505282102 [DOI] [PubMed] [Google Scholar]
- Schiff M, Levit S, Cohen-Moreno R, 2010. Childhood sexual abuse, post-traumatic stress disorder, and use of heroin among female clients in Israeli methadone maintenance treatment programs (MMTPS). Soc. Work Health Care 49, 799–813. 10.1080/00981381003745103 [DOI] [PubMed] [Google Scholar]
- Shand FL, Degenhardt L, Nelson EC, Mattick RP, 2010. Predictors of social anxiety in an opioid dependent sample and a control sample. J. Anxiety Disord 24, 49–54. 10.1016/j.janxdis.2009.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shand FL, Degenhardt L, Slade T, Nelson EC, 2011. Sex differences amongst dependent heroin users: histories, clinical characteristics and predictors of other substance dependence. Addict. Behav 36, 27–36. 10.1016/j.addbeh.2010.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon LM, 2007. Understanding motivations and intentions for long-term substance abuse treatment among pregnant, drug-dependent women. Diss. Abstr. Int. Sect. Humanit. Soc. Sci 68, 1662. [Google Scholar]
- Somer E, 2003. Prediction of abstinence from heroin addiction by childhood trauma, dissociation, and extent of psychosocial treatment. Addict. Res. Theory 11, 339–348. 10.1080/1606635031000141102 [DOI] [Google Scholar]
- Somer E, Altus L, Ginzburg K, 2010. Dissociative psychopathology among opioid use disorder patients: exploring the “chemical dissociation” hypothesis. Compr. Psychiatry 51, 419–25. 10.1016/j.comppsych.2009.09.007 [DOI] [PubMed] [Google Scholar]
- Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, Ferri M, Pastor-Barriuso R, 2017. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ 357 10.1136/bmj.j1550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp, L.L.C., 2017. Stata statistical software: Release 15 (2017). Coll. Stn. TX StataCorp LP. [Google Scholar]
- Stein MD, Conti MT, Kenney S, Anderson BJ, Flori JN, Risi MM, Bailey GL, 2017. Adverse childhood experience effects on opioid use initiation, injection drug use, and overdose among persons with opioid use disorder. Drug Alcohol Depend 179, 325–329. 10.1016/j.drugalcdep.2017.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LRA, Van Ijzendoorn MH, 2015. The Prevalence of Child Maltreatment across the Globe: Review of a Series of Meta-Analyses. Child Abuse Rev 24, 37–50. 10.1002/car.2353 [DOI] [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LRA, Van Ijzendoorn MH, 2012. The Universality of Childhood Emotional Abuse: A Meta-Analysis of Worldwide Prevalence 21, 870–890. 10.1080/10926771.2012.708014 [DOI] [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg MJ, Van Ijzendoorn MH, 2013a. The neglect of child neglect: a meta-analytic review of the prevalence of neglect. Soc. Psychiatry Psychiatr. Epidemiol 48, 345–355. 10.1007/s00127-012-0549-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg MJ, Van Ijzendoorn MH, Alink LRA, 2013b. Cultural–geographical differences in the occurrence of child physical abuse? A meta-analysis of global prevalence. Int. J. Psychol 48, 81–94. 10.1080/00207594.2012.697165 [DOI] [PubMed] [Google Scholar]
- Stoltenborgh M, Van Ijzendoorn MH, Euser EM, Bakermans-Kranenburg MJ, 2011. A Global Perspective on Child Sexual Abuse: Meta-Analysis of Prevalence Around the World. Child Maltreat 16, 79–101. 10.1177/1077559511403920 [DOI] [PubMed] [Google Scholar]
- Taplin C, Saddichha S, Li K, Krausz MR, 2014. Family history of alcohol and drug abuse, childhood trauma, and age of first drug injection. Subst. Use Misuse 49, 1311–1316. [DOI] [PubMed] [Google Scholar]
- Teegen F, Zumbeck S, 2000. Prevalence of traumatic experiences and posttraumatic stress disorder in substance dependent persons. An explorative study. Psychotherapeut 45, 44–49. 10.1007/s002780050007 [DOI] [Google Scholar]
- Torok M, Darke S, Shand F, Kaye S, 2016. Investigating heterogeneity in violent offending liability among injection drug users from a developmental perspective. Addict. Behav 60, 165–170. 10.1016/j.addbeh.2016.04.013 [DOI] [PubMed] [Google Scholar]
- Trafton JA, Minkel J, Humphreys K %J J. of S. on A., 2006. Opioid substitution treatment reduces substance use equivalently in patients with and without posttraumatic stress disorder 67, 228–235. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Davis JP, Seelam R, Stein BD, D’Amico EJ, 2020. Predictors of Opioid Misuse During Emerging Adulthood: An Examination of Adolescent Individual, Family and Peer Factors. Drug Alcohol Depend 214, 108188 10.1016/j.drugalcdep.2020.108188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Center for Substance Abuse Treatment, 2009. National Treatment Improvement Evaluation Study (NTIES), 1992–1997. 10.3886/ICPSR02884.v4 [DOI] [Google Scholar]
- Vachon DD, Krueger RF, Rogosch FA, Cicchetti D, 2015. Assessment of the Harmful Psychiatric and Behavioral Effects of Different Forms of Child Maltreatment. JAMA Psychiatry 72, 1135 10.1001/jamapsychiatry.2015.1792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veritas Health Innovation, 2016. Covidence systematic review software.
- Vogel M, Dursteler-Macfarland KM, Walter M, Strasser J, Fehr S, Prieto L, Wiesbeck GA, 2011. Prolonged use of benzodiazepines is associated with childhood trauma in opioid-maintained patients. Drug Alcohol Depend. 119, 93–8. 10.1016/j.drugalcdep.2011.05.037 [DOI] [PubMed] [Google Scholar]
- Walker R, Maxwell JC, Adinoff B, Carmody T, Coton CE, Tirado CF, 2014. Characteristics of Mexican and Mexican American adolescents in treatment for “cheese” heroin use. J. Ethn. Subst. Abuse 13, 258–272. 10.1080/15332640.2014.883582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Du J, Sun H, Wu H, Xiao Z, Zhao M, 2010. Patterns of childhood trauma and psychological distress among injecting heroin users in China 5, e15882 10.1371/journal.pone.0015882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss O, Levy-Gigi E, Adelson M, Peles E, 2019. Methadone maintenance treatment patients with a history of childhood trauma succeed more in a cognitive paradigm that is associated with a negative reward. Psychiatry Res. 271, 381–388. 10.1016/j.psychres.2018.11.062 [DOI] [PubMed] [Google Scholar]
- Wickersham JA, Loeliger KB, Marcus R, Pillai V, Kamarulzaman A, Altice FL, 2016. Patterns of substance use and correlates of lifetime and active injection drug use among women in Malaysia. Am. J. Drug Alcohol Abuse 42, 98–110. 10.3109/00952990.2015.1101467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JR, Cole V, Girdler S, Cromeens MG, 2020. Exploring stress, cognitive, and affective mechanisms of the relationship between interpersonal trauma and opioid misuse. PLoS ONE 15, e0233185 10.1371/journal.pone.0233185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2006. Preventing child maltreatment: a guide to taking action and generating evidence.
- Young NK, Boles SM, Otero C, 2007. Parental substance use disorders and child maltreatment: Overlap, gaps, and opportunities. Child Maltreat. 12, 137–149. [DOI] [PubMed] [Google Scholar]
- Zielinski DS, Bradshaw CP, 2006. Ecological Influences on the Sequelae of Child Maltreatment: A Review of the Literature. Child Maltreat. 11, 49–62. 10.1177/1077559505283591 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


