Abstract
Objective.
To present through a systematic review a qualitative analysis of studies published on stereolithography-based 3D printing of restorative materials and their clinical applicability.
Methods.
The literature search was conducted based on the question: “What is the state-of-the-art of available restorative materials for 3D printing based on stereolithography?önline search was conducted in three databases (MEDLINE/PubMed, Scopus and Web of Science) with no restriction for year of publication. Data are reported based on PRISMA, including publication details such as authors and their countries, year and journal of publication, and study design. The synthesis is focused on describing the dental restorative materials and properties evaluated, applied methods, 3D printers used and clinical applicability.
Results.
Studies that fit the inclusion criteria were performed in Asia (21), Europe (16) and USA (10), mostly using polymer-based restorative materials (38) for 3D printing constructs. Stereolithographic-printed ceramic-based restorative structures were evaluated by 9 studies. Many studies reported on dimensional accuracy (14), strength (11) and surface morphology (9) of the printed structures. Antibacterial response, cytotoxicity, internal and marginal fit, fracture and wear resistance, density, viscosity, elastic modulus, hardness, structural shrinkage and reliability, degree of conversion, layer cure depth, fatigue, and color were also evaluated by the included studies. Many of them (11) published a proof of concept as an attempt to demonstrate the clinical feasibility and applicability of the technology to print restorative materials, but only 5 studies actually applied the 3D printed restorative structures in patients, which highlights an increasing interest but limited early-stage translation.
Significance.
The fast expansion of stereolithographic-based 3D printing has been impressive and represents a great technological progress with significant disruptive potential. Dentistry has demonstrated an incredible willingness to adapt materials, methods and workflows to this promising digital technology. However, esthetic appearance, wear resistance, wet strength and dimensional accuracy are the main current clinical limitations restricting the progression to functional part production with 3D printing, which may explain the absence of clinical trials and reports on permanent/definitive dental restorative materials and structures.
1. Introduction
Computer-aided design (CAD) and computer-aided manufacturing (CAM) technologies have led to major improvements in dentistry [1]. CAD-CAM subtractive methods produce reliable restorations with accurate dimensions, reducing manufacturing time and labor compared to other fabrication techniques [2–8]. However, subtractive manufacturing wastes unprocessed material and milling tools, and generates surface and sub-surface machining defects that are structural stress concentrators [9]. With the advances in computer-aided design (CAD) technology, additive manufacturing (AM), rapid prototyping or simply 3D-printing, is emerging in Dentistry as a promising technique to fabricate dental restorative and other appliance structures. Complex structures can be produced with 3D printing, which does not waste material in the process and it is more economical than subtractive manufacturing techniques in terms of hardware investment and overall production costs [1,10]. Among the various AM techniques [11], stereolithography (SL) is the most popular for dental applications, offering the greatest accuracy and resolution, fine building details and smooth surface finish [1,12,13]. In the SL technique an object is built through deposition of consecutive layers of photosensitive material that is readily polymerized. The thickness and orientation of the printed layer, and the depth and degree of polymerization along with any post-cure process are some of the factors influencing the mechanical and physical properties of the printed structure [14].
While stereolithography-based 3D printing (e.g. SLA- stereolithography apparatus, DLP- digital light processing, and LCM- lithography-based ceramic manufacturing) is widely recognized as producing to date the best spatial resolution and most isotropic mechanical properties among printable materials, there are still problems in both these areas that limit 3D printing from advancing and reaching the full potential of what can be done in dentistry and more broadly in the printing of fully functional parts as opposed to temporary restorations, models and prototypes [10,15,16]. Nevertheless, the rapid and dynamic progress of recent digital manufacturing technologies is a global sprint becoming an additional challenge to follow up its state of the art [17]. A systematic review is a way to map and present the existing literature on a topic using rigorous and transparent methods to broadly identify, select and critically appraise relevant literature pertaining to a research question [18–20]. Therefore, this comprehensive narrative work based on a systematic review aimed to present a qualitative analysis of studies published on stereolithography-based 3D printing of restorative materials and their clinical applicability.
2. Materials and methods
This review was conducted based on the following question: “What is the state-of-the-art of available restorative materials for 3D printing based on stereolithography?”
2.1. Protocol and registration
The protocol of this review was based on PRISMA-P for systematic review protocols [21] and is available at the following link: DOI 10.17605/OSF.IO/9W4M2.
2.2. Eligibility criteria
The present review included published studies in English language that used stereolithography-based 3D printers to print materials for use or potential use for restorative dentistry. In contrast, studies on materials and structures not applied to restorative dentistry, literature reviews, manufacturer reports, comments and conference abstracts were excluded from this review.
2.3. Information sources and search strategy
Electronic search was conducted in three different databases (MEDLINE/PubMed, Scopus and Web of Science) with no restriction for year of publication, and the last search was performed on June 12th 2020. The search strategy was outlined based on PubMed MeSH terms and adapted for each database.
-MEDLINE/PubMed:
D̈entistry, Operative[M̈esh] OR Öperative Dentistry[ẗitle/abstract] OR D̈ental Materials[M̈esh] OR M̈aterials, DentalÖR D̈ental MaterialÖR M̈aterial, DentalÖR B̈iomedical and Dental Materials[M̈esh] OR P̈rosthodontics[M̈esh] or D̈entistry, ProstheticÖR P̈rosthetic DentistryÖR D̈entistry[M̈esh] AND ((3Dprint* [title/abstract]) OR (additive manufact* [title/abstract]) OR “RP Technologies” [title/abstract] OR “Rapid Prototyping” [title/abstract] OR “rapidly prototyped” [title/abstract] OR “3D digital dentistry” [title/abstract] OR “three-dimensional printing” [title/abstract] OR “stereolithographic” [title/abstract] OR “stereolithographically printed” [title/abstract])
2.4. Selection of sources of evidence
The search was initially conducted using Mendeley program. Two researchers (V.C. and V.T.B) independently identified articles analyzing titles and abstracts for relevance and presence of eligibility criteria. Retrieved records were classified as “include”, “exclude”, or “uncertain”. The full-text articles of the “include” and “uncertain” records were selected for further eligibility screening by the same researchers (acting independently). Discrepancies in screening of titles/abstracts and full-text articles were resolved through discussion. In case of disagreement, the opinion of a third reviewer (A.D.B.) was obtained. In case of missing information or data, the corresponding author from such papers was contacted up to three times by e-mail.
2.5. Data charting process
The articles meeting the inclusion criteria were subjected to critical appraisal, which was carried out by two reviewers (V.C. and V.T.B) independently. Standardized data extraction form was created on Excel software (Microsoft Corporation, Redmond, WA, EUA) to collect the following data:
Publication details: authors, Country where the work was executed (based on the Institution location of the corresponding author), year and journal of publication.
Study characteristics: in-vitro studies and clinical studies.
Materials characteristics: polymers, metals and ceramics.
Methods characteristics: evaluated parameters, properties and concepts, and 3D printers used.
Clinical applicability: clinical evaluation of the printed structures.
2.6. Synthesis of results
This study focused on describing the dental restorative materials evaluated, applied methods and 3D printers used. A descriptive analysis was performed considering the study design, the characteristics of materials, methods and stereolithography-based 3D printing devices, which were presented in Figures and Table.
3. Results
Fig. 1 presents the flow chart for the study selection. The search initially yielded 3876 potentially relevant citations (PubMed: n = 2630; Scopus: n = 623; Web of Science: n = 623). After removing duplicates (764) and irrelevant articles (3035) that did not meet the inclusion criteria, 77 citations met the eligibility criteria based on title and abstract. These papers were obtained and full-text screened, resulting in 47 studies that were included in the analysis (qualitative synthesis).
Fig. 1 –
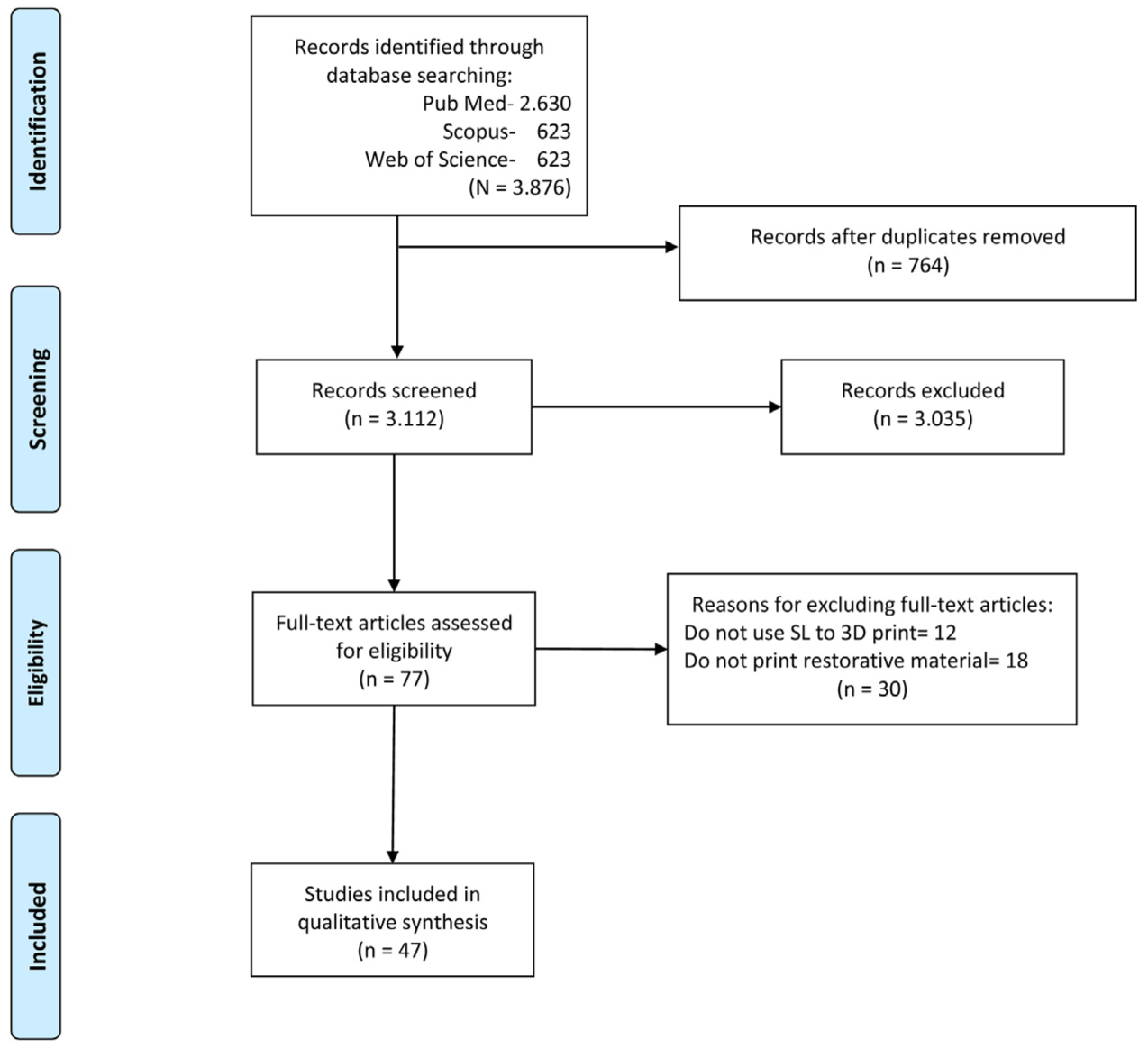
PRISMA flow diagram showing the flow of information through the different phases of the present systematic review.
The first study on stereolithography-based 3D printing of restorative materials was published in 2015. Such recent development gained increasing interest with four publications in 2016, six in 2017, twelve in 2018, twelve in 2019, and twelve publications on the subject up to the search date (June 12th) in 2020. The majority of the studies (37) were published in dental journals, mostly in the Journal of Prosthetic Dentistry (13) and in Dental Materials (6). Eight papers were published in materials science and engineering journals and two articles were published by medical journals. Most studies (21) were performed in Asia, mostly from South Korea (11), but also from China (7), Turkey (2) and India (1). Sixteen studies were performed in Europe with four studies from the Netherlands, three studies each from Switzerland and Germany, two from Bulgaria, and one study from each of the following countries: France, Austria, Romania and Spain. Ten studies were performed in the USA (Fig. 2).
Fig. 2 –
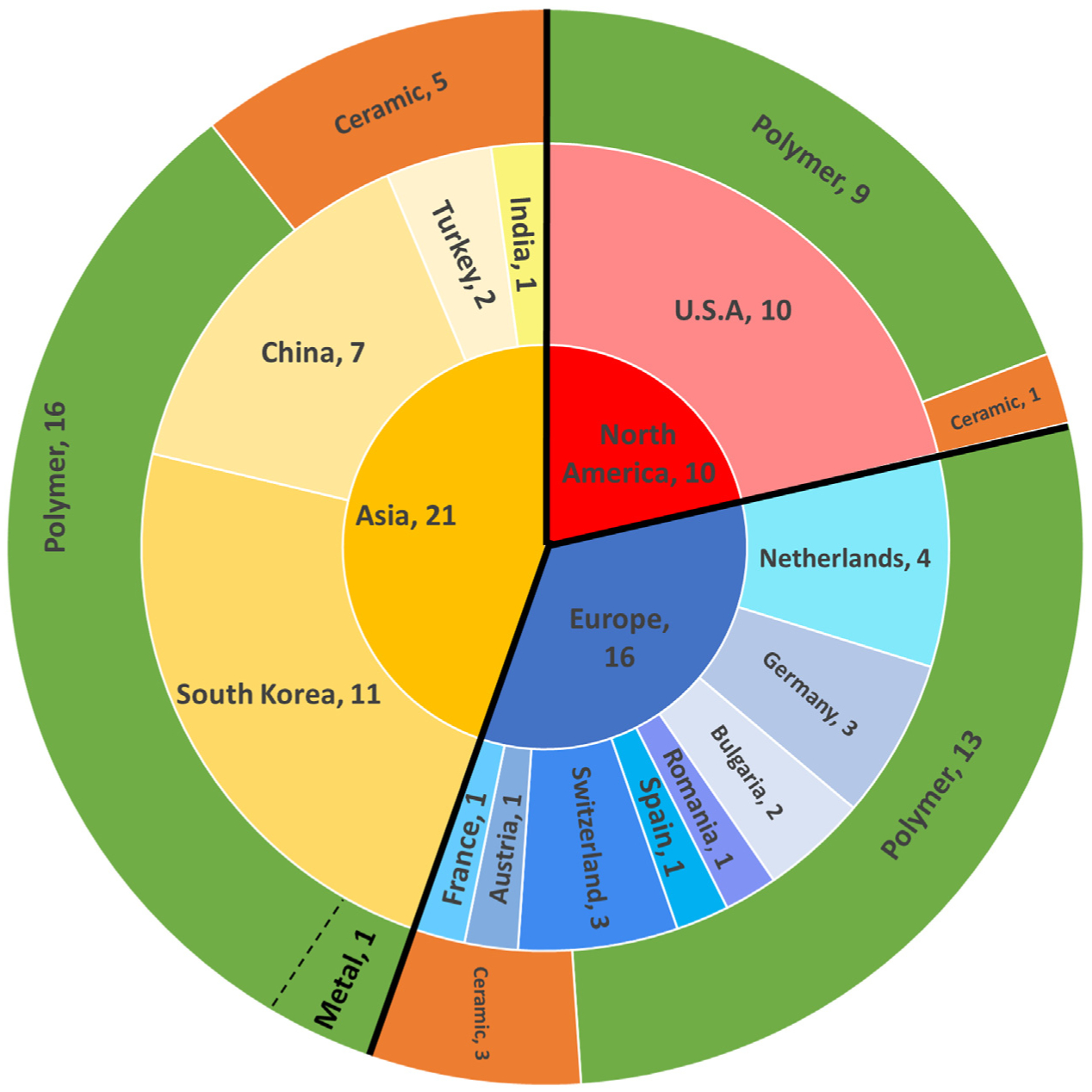
Chart showing the Country where the work was executed and materials used for the included studies on stereolithography-based 3D printing of restorative materials.
From the 47 studies included in this review, 9 printed ceramic structures, 38 printed polymer-based constructs and one of them also printed the metallic cusps of the 3D-printed set of teeth [22] (Fig. 2). The majority of them (36) 3D printed dental restorative structures and eleven printed test specimens from restorative materials. Most of the restorative structures (28 out of 36) were printed out of polymer-based materials, resulting in removable prosthesis-related constructs [22–34], provisional restorations [35–47], or inlays [48,49]. Nine studies printed ceramic-based restorative structures and they were zirconia-based constructs [50–56], glass-ceramic crowns [57] or alumina-based crowns [16]. Yet, only 5 studies (gray-shaded in Table 1) included in this review actually applied the 3D printed restorative structures in patients, reporting the clinical cases [29,33,34,36,41].
Table 1 –
Studies in chronological and alphabetical order, reporting 3D printing of restorative materials using a stereolithography-based (SL) printer. Gray shaded studies clinically applied the printed structure(s).
| Study | Objective | SL material, printed structure (N; NS; n); 3D printer | Evaluated parameter(s) | Main conclusion |
|---|---|---|---|---|
| Bilgin et al., 2015 [23] | To fabricate dentures using CAD-CAM and RP, combining with conventional laboratory techniques. | Light-cured resin (E-Dent 100; EnvisionTEC) denture teeth set (n = 1); Perfactory® 4 DDP Mini (EnvisionTEC) | Feasibility and applicability of a technology (proof of concept) | Denture teeth sets fabricated by CAD/CAM and RP can be accomplished with reduced chair time, self-designed esthetics and occlusion. |
| Alharbi et al., 2016 [62] | To evaluate the effect of build direction (layer orientation) on the mechanical properties of a novel restorative material. | Hybrid composite resin (Temporis, DWS) cylinders (NS = 40; n = 20); DW028D 3D-printer (DWS) | Printing layer orientation and compressive strength | Composite material printed with the layers oriented perpendicular to load direction have greater compressive strength than material printed horizontally. |
| Alharbi et al., 2016 [35] | To evaluate the influence of build (support) angle and configuration on dimensional accuracy of 3D-printed crowns. | Hybrid composite resin (Temporis DD-1000, DWS) dental crowns (NS = 18; n = 1); DW028D 3D-printer (DWS) | Dimensional accuracy (9 build angles and 2 support types) | The 120° build angle should offer the crown the highest dimensional accuracy and self-supported geometry with the least necessary support surface area. |
| Digholkar et al., 2016 [63] | To evaluate and compare properties of provisional restorative materials fabricated by RP, CAD-CAM, and conventional methods. | Light-cured resin (E-Dent 100, Envision TEC) bar-shaped specimens (N = 60; NS = 20; n = 20); Perfactory® 4 Standard (EnvisionTEC) | Flexural strength and microhardness | All materials showed flexural strength higher than minimal acceptable for provisional restorations. RP specimens showed the highest hardness values. |
| Jooet al., 2016 [36] | To perform a complete mouth rehabilitation using 3D printing and CAD/CAM double-scanning method. | Light-cured resin (E-Dent, Envision TEC) provisional crowns (NS = 17; n = 1); DDP (EnvisionTEC) | Feasibility and applicability of a technology (proof of concept) | 3D printed resin-based provisional crowns showed adequate fitting and fractures during interim service. |
| Bae et al., 2017 [48] | To evaluate the accuracy of inlay restorations fabricated by AM comparing to subtractive methods. | Polymer (VisiJet FTX Green, 3D Systems) distal-occlusal inlays (N = 40; NS = 10; n = 10); ProJet 1200 (3D Systems) | Dimensional accuracy and surface morphology | The accuracy of inlays fabricated by AM is higher than that of subtractive methods. |
| Dehurtevent et al., 2017 [16] | To compare material’s properties of SL-manufactured alumina ceramics of different composition to those of subtractive- manufactured ceramics and to produce dental crown frameworks. | Experimental alumina slurries for testing bars (NS = 90; n = 15) and crown framework (n = 1); CryoCeram (CryoBeryl) | Viscosity, density, flexural strength, structural shrinkage, and Weibull structural reliability | Viscosity of the alumina slurry influenced the SL-manufacturing process. High particle size (d50≈ 1.6 μm) and volume fraction (80wt%) resulted in reliable anisotropic shrinkage, high density, flexural strength, and Weibull characteristics suitable for SL manufacturing. |
| Lee et al., 2017 [37] | To evaluate the internal and marginal fit of provisional crowns manufactured by CAD/CAM milling and 3D printing methods. | Polymer (ZMD-1000B, Dentis) provisional crowns (N = 30; NS = 10; n = 10); Zenith (Dentis) | Internal and marginal fit | SL-manufactured crowns showed similar or better marginal and internal fit than CAD-CAM milled crowns. |
| Lin et al., 2017 [24] | To duplicate a complete removable dental prosthesis (CRDP) using SL technology. | Polymer (Standard Clear Resin, Formlabs) CRDP (n = 1); Form 2 (Formlabs) | Proof of concept | It is feasible to duplicate a CRDP using SL technology. |
| Osman et al., 2017 [38] | To evaluate the effect of the build orientation/build angle on the dimensional accuracy of full-coverage dental restorations manufactured by DLP. | Resin (Next Dent C&B) provisional crowns (NS = 9; n = 1); D30 (Rapid Shape GmbH) | Dimensional accuracy (9 build angles) | The angle of 135° offered the highest dimensional accuracy and the most favorable deviation pattern, with a self-supporting crown geometry throughout the building process. |
| Totu et al., 2017 [25] | To obtain a PMMA-TiO2 material with improved antibacterial characteristics, suitable for manufacturing 3D printed dental prosthesis. | Resin (E-Dent 100, Envision TEC) + TiO2 nanoparticles specimens (NI) and denture (n = 1); Perfactory® (EnvisionTEC) | Microstructure and surface morphology, antibacterial effect; proof of concept | Significant improvements in polymer characteristics and nice dispersion of the TiO2 nanoparticles were noticed for 0.4wt%, which was used for stereolitographic complete denture prototyping. |
| Alharbi et al., 2018 [39] | To evaluate the influence of fabrication method (CAD-CAM and SL) and four finish line design on marginal and internal fit of provisional crowns. | Hybrid composite resin (Temporis A2, DWS) crowns (N = 80; NS = 40; n = 10); DW028D 3D-printer (DWS) | Marginal and internal fit | The fabrication methods influenced more on the fit than the finish-line design. SL-printed crowns showed lower marginal and internal gap than milled restorations, but both techniques showed adequate values. |
| Bae et al., 2018 [49] | To compare subtractive (CAD-CAM) and additive (SL) manufacturing methods to investigate if the CAD data of the proposed inlay shape is correctly machined. | Polymer (VisiJet FTX Green, 3D Systems) mesial-occlusal inlays (N = 40; NS = 10; n = 10); ProJet 1200 (3D Systems) | Dimensional accuracy and surface morphology | SL showed the best accuracy but both additive and subtractive methods can be used clinically |
| Chen et al., 2018 [64] | To synthesized a bioactive nanocomposite for enhanced antibacterial and biocompatibility characteristics suitable for 3D printing dental prosthesis. | Experimental PMMA-based nanocomposite (n = 1). Printer not mentioned. | Surface morphology, antibacterial efficacy, cytocompatibility | The nanocomposite showed excellent antibacterial efficacy and favorable compatibility with dental pulp cells, being efficaciously employed for denture manufacturing using SL. |
| Chen et al., 2018 [26] | To develop a composite of nanocrystalline cellulose-silver (CNCs-Ag) introduced into the PMMA matrix with enhanced mechanical properties, high antibacterial activities and excellent biocompatibilities. | PMMA-CNCs-Ag composite resin (NextDent Denture 3+) for bar-shaped specimens (n = 6) and denture base (n = 1); DLP Vida (Envision Tech) | Flexural strength, Surface morphology, antibacterial efficacy, cytotoxicity | The composite showed high antibacterial activity with no significant cytotoxic effect. It showed great potential and it is recommended as a functional dental restoration material. |
| Chung et al., 2018 [27] | To evaluate chipping and fracture resistance of 3D printing resin material compared with resin denture teeth. | Methacrylate-based resin (Dentca) denture teeth (N = 50; NS = 10; n = 10); Zenith (Dentis) | Chipping and fracture resistance | Fracture resistance of 3D printed resin teeth was comparable to prefabricated denture teeth. |
| Dikova et al., 2018 [40] | To compare the dimensional accuracy and surface roughness of polymeric dental bridges produced by different 3D printers. | Methacrylate-based resins (NextDent C + B and Formlabs) 4-unit dental bridges (N = 9; NS = 6; n = 3); Form 1+ (Formlabs) and D30 (Rapid Shape GmbH) | Dimensional accuracy and surface roughness | Printing settings, polymer properties, sample position and building direction influence geometric characteristics and surface roughness. SL can be successfully used to fabricate 4-unit dental bridges. |
| Katreva et al., 2018 [41] | A case report to demonstrate that 3D printing is a precise alternative to fabricate dental restorations. | Resin (Next Dent C&B) provisional crown (n = 1); D30 (Rapid Shape GmbH) | Clinical applicability | 3D printing offers time saving, precise accuracy and fitting of the constructions, no risk of distortions and laboratory mistakes, production of complex shapes with no need of special tools and almost no waste material. |
| Li et al., 2018 [42] | To use a SL-based technology to 3D print provisional dental crown and bridge | Commercially available high viscosity polymers (Unifast LC; Revotek LC; and Ervotek LC) for temporary restorations (NS = 3; n = 1); custom made 3D printer | Proof of concept | The temperature controlled SL-based method can 3D print high viscous crown material with fast speed and high resolution. |
| Lin et al., 2018 [28] | To propose a digital workflow for fabricating a mandibular interim complete removable dental prosthesis (CRDP) with an in-office DLP 3D printer. | Soft-tissue colored (NextDent Base) and A2-shade (Freeprint temp UV; DETAX Ettlingen) resins for CRDP (n = 1); MAX (Asiga) | Proof of concept | Further studies are need to investigate the design parameters in different CAD software programs and printing strategies in different 3D printers to achieve optimal clinical outcome. |
| Park et al., 2018 [66] | To evaluate the wear resistance of 3D printing resin material compared with milling and conventional resin materials. | Resin (Next Dent C&B) specimens (N = 60; NS = 20; n = 20); D1–150 (Veltz3D) | Wear resistance (volume loss and maximal depth loss of wear) | Wear resistance of the 3D printed resin material was in a range comparable to milled or conventionally fabricated resin materials. |
| Tahayeri et al., 2018 [58] | To optimize the 3D printing of a dental material for provisional restorations using a low-cost SL 3D printer, and compare its mechanical properties against two conventionally cured provisional dental materials. | Resin (NextDent C&B) bar-shaped samples (N = 36; NS = 24; n = 6); Form 1+ (Formlabs) | Printing accuracy, degree of conversion, elastic modulus and peak stress. | 3D printable provisional restorative material allows for sufficient mechanical properties for intraoral use, despite the limited 3D printing accuracy of the printing system of choice. |
| Unkovskiy et al., 2018 [59] | To evaluate the influence of printing parameters on flexural properties and accuracy of SL-printed standard objects. | Dental SG resin (Formlabs) bar-shaped samples (NS = 30; n = 10 for 3 orientations; NS = 49; n = 49 for positioning; NS = 40; n = 10 for post-curing); Form 2 (Formlabs) | Printing orientation, positioning and accuracy, flexural strength and flexural modulus | 45° printing orientation showed the best accuracy and 90° specimens with layer orientation parallel to the axial load showed superior flexural strength and flexural modulus. Objects printed on the borders of build platform are rather prone to inaccuracies than those in the center. |
| Clark et al., 2019 [29] | To propose a digitally replicated denture technique (DRDT) demonstrating a predictable workflow for fabricating complete dentures for patients with existing dentures. | Resin (NI) for replicated and trial dentures (n = 2); Form 2 (Formlabs) | Proof of concept | The clinical case showed that DRDT using rapid prototyping can streamline the process of complete denture fabrication for patients with existing dentures. |
| Jang et al., 2019 [50] | To analyze suspensions with various zirconia (Zr) volume fractions (Vv) and their influence on microstructural and physical properties of products produced by DLP-AM and sintering processes. | Six (48–58vol% in Vv) experimental Zr-based suspensions for bars (NS = 60; n = 10), discs (NS = 60; n = 10) and crowns (NI); Octave Light R1 (Octave Light Ltd.). | Viscosity, depth of cure (DC), geometrical overgrowth, thermal behavior, sintering shrinkage, density, and flexural strength | As Zr Vv increased in the suspensions, the viscosity increased and DC decreased. Distortion due to geometrical overgrowth was observed after polymerization. Maximum strength was 675 MPa for a Vv of 58vol%. |
| Kalberer et al., 2019 [30] | To compare the differences in trueness between the CAD-CAM milled and 3D-printed complete dentures. | Resin (NextDent Denture 3+) for complete denture (N = 20; NS = 10; n = 10); RapidShape D30 (Rapid Shape) | Trueness (accuracy of fit to a master model) considering 8 regions | CAD-CAM milled complete dentures were superior to 3D-printed complete dentures in terms of trueness of the intaglio surfaces. |
| Kessler et al., 2019 [65] | To investigate the three body wear resistance of 3D printed resin materials in comparison to one milled PMMA and one direct composite materials. | Resins (3Delta temp; NextDent C&B; Freeprint temp) specimens (N = 40; NS = 24; n = 8); D20II (Rapid Shape) | Three-body wear resistance | 3D printed temporary resins showed comparative wear resistance to established materials for temporary use. Differences between materials were more pronounced than between manufacturing techniques. |
| Lee et al., 2019 [31] | To evaluate the accuracy and surface resolution of denture bases fabricated by three methods: injection molding, milling, and DLP RP using surface matching software. | Resin (NextDent Base) for denture base (N = 30; NS = 10; n = 10); Bio3D W1 (Bio3D Inc.) | Dimensional accuracy and surface resolution | Overall accuracy of denture base is higher in milling and RP methods than the injection molding method. Surface resolution is higher in the injection molding method than the milling or RP methods. |
| Li et al., 2019 [51] | To use AM to fabricate dental bridges and implants made of zirconia. | Custom made resin-based zirconia slurry for dental bridges and implants (n = NI); DLP 3D printer (brand NI) | Structural and morphological characterization | Several technical barriers have to be overcome to apply 3D printed all-ceramic prostheses to clinical practice. |
| Li et al., 2019 [52] | To evaluate the physical and mechanical properties of SL-manufactured zirconia dental crowns and analyze their internal and marginal adaptation. | Custom made resin-based zirconia (45vol%) slurry for experimental samples (n = 22) and molar crowns (n = 5); CSL 150 (Porimy) | Density, sintering shrinkage, flexural strength, Weibull parameters, internalmarginal adaptation. | The strength of SL-manufactured zirconia was adequate to fabricate dental crowns, which showed less than ideal internal and marginal adaptation for clinical application. |
| Sa et al., 2019 [43] | To evaluate the antibacterial properties and mechanical behavior of an experimental resin for 3D printing restorations. | Experimental resin for crowns and bridges (n = 1) and testing samples (n = NI); DLP printing system | Flexural strength and modulus, antibacterial activity and cytotoxicity | The 3D printable composite material with Ag-HNT/SLR showed high strength, sustaining antibacterial activity and non-toxicity. |
| Uçar et al., 2019 [55] | To compare mechanical and microstructural properties of a ceramics from lithography-based ceramic manufacturing (LCM) with pressing and CAD/CAM methods. | High-purity alumina (LithaLox HP 500, Lithoz) for disc-shaped specimens (N = 30; NS = 10; n = 10); CeraFab 7500 (Lithoz) | Biaxial flexural strength, hardness, fracture toughness, structural reliability | LCM can be used to produce ceramic parts. Mechanical properties and manufacturing of LCM ceramics seem to be promising but need improvements, mainly to reduce porosity. |
| Wang et al., 2019 [53] | To evaluate the trueness of zirconia crowns fabricated by 3D printing in comparison with crowns fabricated by CAD-CAM milling as a control. | Photosensitive resin mixed with zirconia paste (3DMixZrO2L, 3DCeram Co.) for crowns (N = 20; NS = 10; n = 10); Ceramaker 900 (3DCeram Co.) | Trueness (dimensional accuracy considering 4 crown locations) | Zirconia crowns produced by 3D printing met the trueness requirements, and 3D printing may be suitable for fabricating zirconia crowns. |
| Zandinejad et al., 2019 [54] | To compare the fracture resistance of milled zirconia (MZr), milled lithium disilicate (MLD), and AM zirconia (AMZr) crowns when cemented to MZr implant abutment. | Zirconia paste (3DMix ZrO2, 3DCeram Co.) for crowns (N = 30; NS = 10; n = 10); Ceramaker 900 (3DCeram Co.) | Fracture resistance and mode of failure | AMZr crowns showed comparable fracture resistance to milled restorations. AM appears to be a promising technology for the fabrication of all ceramic restorations. |
| Zimmermann et al., 2019 [44] | To evaluate the fracture behavior of different CAD/CAM ceramics and composites and one 3D-printed composite as a function of different crown thicknesses (0.5, 1 and 1.5 mm). | Composite (els-3D Harz, Saremco Dental AG) for crowns (N = 180; NS = 30; n = 10); DLP Freeform Pro 2 (ASIGA) | Fatigue and fracture load | As none of the 0.5-mm ceramic crowns survived fatigue testing and all 0.5-mm composite crowns did, composites may have advantageous material characteristics compared to ceramic CAD/CAM materials for minimal restoration thicknesses. |
| Cha et al., 2020 [32] | To compare the wear resistance of 3D-printed denture teeth with that of conventionally prefabricated denture teeth. | Dentca PMMA-based resin (Dentca Inc.) for denture teeth (N = 80; NS = 12; n = 12); Zenith D (Dentis) | Wear resistance | The wear behavior of 3D-printed denture tooth resin was comparable to that of prefabricated denture teeth. |
| Ioannidis et al., 2020 [56] | To test the load-bearing capacity of ultra-thin molar occlusal veneers fabricated with 3D-printed zirconia, CAD-CAM milled zirconia, and pressed glass-ceramic. | Zirconia slurry (LithaCon 3Y 610 white, Lithoz) for occlusal veneers (N = 60; NS = 20; n = 20); CeraFab 7500 (Lithoz) | Load-bearing capacity (dynamic aging by cyclic fatigue and temperature variation) | Despite significant differences between restorative materials, all load-bearing capacities exceeded the clinically expected normal bite forces. |
| Jurado et al., 2020 [34] | Using case reports to compare subtractive and additive technologies for the manufacture of immediate complete dentures. | Dentca PMMA-based resin (Dentca Inc.) for denture teeth (N = 2; NS = 1; n = 1); M2 SpeedCell (Carbon) | Case report | Both approaches resulted in well-fitted immediate complete dentures. Printing technology does not provide anatomical details and needs to improve the bonding between teeth set and baseplate. |
| Lin et al., 2020 [61] | To evaluate materials based on Bis-EMA, UDMA, and TEGDMA as 3D printing resins and to characterize the mechanical and biological properties and accuracy of the 3D-printed objects. | Experimental resins based on Bis-EMA, UDMA, and TEGDMA for disc-, cube-, and bar-shaped specimens(NS = 168; n = 8, 5, and 3); custom-made UV-DLP printer (NI) | Viscosity, dimensional accuracy, flexural strength and modulus, depth of cure (DC), and hardness | The experimental resins are good candidates for 3D printing dental parts, which showed favorable biological and mechanical properties. The accuracy of the printed specimens showed potential for clinical application. |
| Park et al., 2020 [22] | To 3D print resin (PMMA) dentures with metal cusps. | Ti6Al4V alloy (LaserForm Ti Grade 23) for cusps printed with ProX 100 DMP (3D systems); a photopolymer (NextDent C&B) for denture base and teeth printed with Bio3D-L12 (Bio3D) | Proof of concept | Metal and PMMA resin were designed separately and combined by using general purpose software to produce digitally fabricated dentures, demonstrating digital prosthesis designs with improved functionality. |
| Peng et al., 2020 [45] | To evaluate the internal fit and marginal discrepancy of interim crowns made by different manufacturing methods. | Resin (NextDent C&B MFH) for crowns (N = 48; NS = 16; n = 16); DLP MiiCraft125 (Young Optics) | Internal fit and marginal discrepancy | Digitally fabricated crowns (CAD-CAM and 3D-printed) had better internal fit and smaller marginal discrepancy than manually constructed crowns. |
| Peng et al., 2020 [46] | To compare the internal fit and marginal discrepancy of interim crowns fabricated by different manufacturing methods. | Resin (NextDent C&B MFH) for crowns (N = 36; NS = 12; n = 12); DLP MiiCraft125 (Young Optics) | Internal fit and marginal discrepancy | Digitally fabricated interim crowns (CAD-CAM and 3D-printed) had better internal fit and smaller marginal discrepancy than manually fabricated interim crowns |
| Revilla-León et al., 2020 [67] | To measure and compare color dimensions of five different AM and two conventional interim restorative materials. | Resins (*Detax FreePrint temp; †Envisiontec E-Dent 400; *NextDent C&B; *NextDent C&B MFH; ┼Stratasys Med620 VEROGlaze) disks (N = 420; NS = 300; n = 60); *D30 (Rapid Shape), †VIDA (EnvisionTEC), and ┼Eden 260VS (Stratasys) | Color differences | None of the additively manufactured interim materials tested matched the conventional interim materials in all 3 CIELab color dimensions. |
| Reymus et al., 2020 [47] | To investigate the impact of 3D print material, build direction, post-curing, and artificial aging on fracture load of interim 3-unit fixed dental prostheses (FDPs). | Resins (EXP- experimental; CB- NextDent C&B; FT- DetaxFreePrint temp; DT- Deltamed 3Delta temp) for FDPs (N = 405; NS = 360; n = 15); D20II (Rapidshape) | Fracture load | Interim 3D-printed FDPs might offer an alternative to milled and conventionally fabricated ones. Adequate post-curing is crucial for 3D-printed materials to ensure sufficient mechanical properties, but they are more prone to artificial aging than milled PMMA, questioning their long-term use. |
| Schönherr et al., 2020 [57] | To optimize the precision of glass ceramic additively manufactured parts, especially dental molar crowns. | Experimental lithium disilicate-based ceramic filled photosensitive resin slurries for crowns (NI); DLP printer (NI). | Dimensional accuracy of 3D-printed glass-ceramic crowns | The best precision of the final part was obtained from micro computed tomography (CT) scanning. It resulted in an optimized process allowing for possible production of high precision molar crowns with dimensional accuracy and high reproducibility. |
| Shim et al., 2020 [60] | To evaluate the effect of 3 printing orientations (0°, 45° and 90°) on the printing accuracy, flexural strength, surface characteristics, and microbial response of 3D-printed denture base resin. | PMMA for denture base (NextDent Base) specimens (NS = 30; n = 10); Form 2 (Formlabs) | Printing accuracy, flexural strength, surface roughness, hydrophilicity, surface energy, and microbial response to Candida albicans | Printing orientation influenced printing accuracy, flexural strength, roughness, and response to C. albicans. Thus, printing orientation should be carefully decided to fabricate products with appropriate properties. |
| Takeda et al., 2020 [33] | To fabricate 3D-printed replication dentures using digital workflow. | Photopolymerizing resin (Formlabs Dental SG V1) replication dentures (NS = 2); Form 2 (Formlabs) | Proof of concept | Digital replication of dentures allows for necessary repairs and changes to be made while also maintaining the desirable features of the existing dentures. |
AM- additive manufacturing; RP- rapid prototyping; SLA- stereolithography apparatus; DLP- digital light processing; LCM- lithography-based ceramic manufacturing; CAD-CAM- computer-aided design and computer-aided manufacturing; PMMA- Poly(methylmethacrylate); Bis-EMA- ethoxylated bisphenol A-dimethacrylate; UDMA- urethane dimethacrylate; TEGDMA- triethylene glycol dimethacrylate; N- total number of structures/samples in the study, and/or NS- total number of SL structures/samples in the study; n- SL sample size (per experimental group); NI- not informed.
Regarding the materials parameters and properties evaluated, a great number of studies reported on dimensional accuracy [30,31,35,38,40,48–50,53,57–61], strength [16,26,43,50,52,55,59–63] and surface morphology [25,26,31,40,48,49,51,60,64]. In addition, antibacterial effect [25,26,43,60,64], cytotoxicity [26,43,64], internal and marginal fit [37,39,45,46,52], fracture resistance [27,44,47,54–56], wear resistance [32,65,66], elastic modulus [52,58,59,61], density [16,50,52], structural shrinkage [16,50,52] and reliability [16,35,55], viscosity [16,50,61], hardness [55,61,63], printing orientation [59,62], degree of conversion [58], layer cure depth [50,61], fatigue [44], and color [67] were evaluated. Eleven papers published a proof of concept as an attempt to demonstrate the clinical feasibility and applicability of the technology to print restorative materials [22–25,28,29,33,34,36,41,42].
Considering the 3D printers based on stereolithography (SL) technology, 26 studies used digital light processing (DLP), 19 used stereolithography apparatus (SLA), and two studies used lithography-based ceramic manufacturing (LCM). The most frequent manufacturer for DLP was Rapid Shape and for SLA was FormLabs.
4. Discussion
A technology undergoing rapid progress often brings faster benefits to the society, but it can also generate some turmoil involving clear communication and, as a result, not the best possible use of such technology. Additive manufacturing (AM), or simply 3D printing, fits well on this rationale. Despite standardization efforts to attempt to reduce confusion that hampers communication and potentially wider application of AM, there is a clear mismatch between the literature and the standard description of this technology [11]. The standard is intended to provide a basic understanding of the fundamental principles for AM offering definitions for terms and nomenclature associated with it, facilitating adequate communication worldwide. It was actually a rare joint effort from the two main international organization for standardization, ISO and ASTM, putting together a standard. The final version of the standard [11] was published in the same year of the earliest report [23] that fit the inclusion criteria of the present review, offering the opportunity to minimize terminology mismatches that were observed in the literature. Nevertheless, it may be time for new effort to update the standard terms and definitions on this very dynamic development that applies to the hardware, software and materials in order to prevent near-term future disparities.
As this review aimed to present a qualitative analysis of studies published on stereolithography-based 3D printing of restorative materials and their clinical applicability, focus was on a specific AM process (SL- stereolithography) with application to restorative dentistry. SL-based 3D printing (e.g. SLA, DLP, and LCM) is one of the most used AM processes in Dentistry, offering the greatest accuracy and resolution, fine building details and smooth surface finish among printing technologies [1,10,12,13,17]. An SL-printed construct is built through deposition of consecutive layers of a photosensitive material, which is readily polymerized. This may be the reason for the earliest studies to investigate the influence of thickness and orientation of the printed layer on dimensional accuracy of the constructs [35,62]. Yet, this has been the research concern from many authors in this topic [30,31,35,38,40,48–50,53,57–61]. It has been shown that printing orientation, build angle and position influence not only printing accuracy but other properties, such as strength, surface morphology, and bacterial response [40,60]. In addition, the print orientation can affect other aspects such as print efficiency (print time and packing density accommodated on the build plate) as well as the amount of material consumed as sacrificial structural supports. Considering polymer-based structures, bar-shaped specimens printed with 45° orientation showed the best accuracy, but the 90° specimens with layer orientation parallel to the axial load showed superior flexural strength and modulus [59]. For dental restorations, e.g. crowns, build angles of 120° [35] and 135° [38] have offered the highest dimensional accuracy and self-supported geometry throughout the building process. Objects printed on the borders of the build platform are rather prone to inaccuracies as compared to those positioned in the center [59]. When considering printing accuracy of polymer-based structures, which may be influenced by the tuning between the material, the printer and the process parameters used, some authors showed adequate accuracy [48,49] and others reported inferior accuracy [30,31,58] compared to other manufacturing processes. Printing accuracy of ceramic constructs has been associated with the crystalline volume fraction (Vv) [50]. As zirconia Vv increases, the flowability of a Zr-based suspension decreases, which makes it more difficult to reliably 3D print. The viscosity of zirconia suspensions sharply increased from a volume fraction (Vv) of ≥ 54 vol%, therefore, the maximum Vv of Zr in suspensions possible for printing was 58 vol% (or 89 wt%), which also produced the higher mean flexural strength (675 MPa). The cure depth of zirconia suspensions decreased as the Vv increased, yet it was greater than 100 μm after photocuring any of the suspensions for 15 s [50]. As zirconia has a strong light scattering effect, with a refractive index 20–27% higher than other ceramic materials such as silica and alumina [7,68], it can cause significant scattering of the incident light during polymerization of a photopolymer, limiting its depth of cure [69–71]. Further, all ceramic constructs showed some distortion after polymerization [50]. Nevertheless, AM of ceramic crowns is very promising [53].
Inherent to material science and as noticed above, material properties and structural behavior are associated. Therefore, strength [16,26,43,50,52,55,59–63] and surface morphology [25,26,31,40,48,49,51,60,64] were also significantly examined in the included studies. Despite of the heterogeneity of experimental methods and material composition, all printed polymer-based structures showed strength higher than minimal acceptable for provisional restorations [26,43,59,60,62,63]. As mentioned above, the strength of printed alumina- and zirconia-based constructs is strongly associated with the crystalline content, with high particle size (d50 ≈ 1.6 μm) and Vv (≈80 wt%) resulting in reliable anisotropic shrinkage and high strength [16,50]. However, the resulting ceramic structures need improvements, mainly to reduce defects (e.g. cracks and porosity) and enhance internal and marginal adaptation (dimensional accuracy) for clinical application [52,55]. Although surface morphology is an important clinical parameter, polymer-based restorations are not difficult to polish and it is a routine dental practice [72]. This parameter is mostly related to printing settings, post-cure processing and polymer properties [40,60], directly influencing on surface roughness, color [67] and bacterial response and adherence [25,26,43,60,64].
The main goal of the present review was to present the most recent developments and clinical evaluation of SL-printed structures. The clinical applicability of 3D-printed structures was, somehow, present in the majority of studies included in this review. Most of them reported a proof of concept as an attempt to demonstrate the clinical feasibility and applicability of the technology to print restorative materials [22–25,28,29,33,34,36,41,42]. However, only five studies (gray-shaded in Table 1) placed the printed temporary/interim restorative structures in service, reporting the clinical cases [29,33,34,36,41]. Up to date there is no clinical trial on stereolithography-based 3D printed restorative constructs.
5. Conclusion
The fast expansion in photopolymerized-based AM using stereolithographic processes has been notable and represents great technological progress. The ability to rapidly produce customized objects and functional parts is expected to digitally transformed many practices. This review showed that Dentistry has demonstrated an incredible ability to adapt materials, methods and workflows to this promising digital technology. However, full realization of the potential promise of 3D printing is reliant on sustained improvement in adequate dental materials and processes. Esthetic appearance, wear resistance, and dimensional accuracy are the main current clinical limitations that restrict progression to functional part production with 3D printing, which may explain the absence of clinical trials and reports on permanent/definitive dental restorative materials and structures.
Acknowledgements
This study was partially supported by CNPq do Brasil grant 302587/2017-9; CAPES do Brasil PVEX 88881.337090/2019-01; and NIH/NIDCR R21 grant DE028444.
REFERENCES
- [1].van Noort R The future of dental devices is digital. Dent Mater 2012;28:3–12. [DOI] [PubMed] [Google Scholar]
- [2].Alessandretti R, Borba M, Benetti P, Corazza PH, Ribeiro R, Della Bona A. Reliability and mode of failure of bonded monolithic and multilayer ceramics. Dent Mater 2017;33:191–7. [DOI] [PubMed] [Google Scholar]
- [3].Alessandretti R, Borba M, Della Bona A. Cyclic contact fatigue resistance of ceramics for monolithic and multilayer dental restorations. Dent Mater 2020;36:535–41. [DOI] [PubMed] [Google Scholar]
- [4].Basso GR, Moraes RR, Borba M, Duan Y, Griggs JA, Della Bona A. Reliability and failure behavior of CAD-on fixed partial dentures. Dent Mater 2016;32:624–30. [DOI] [PubMed] [Google Scholar]
- [5].Colpani JT, Borba M, Della Bona A. Evaluation of marginal and internal fit of ceramic crown copings. Dent Mater 2013;29:174–80. [DOI] [PubMed] [Google Scholar]
- [6].Corazza PH, Duan Y, Kimpara ET, Griggs JA, Della Bona A. Lifetime comparison of Y-TZP/porcelain crowns under different loading conditions. J Dent 2015;43:450–7. [DOI] [PubMed] [Google Scholar]
- [7].Della Bona A Bonding to ceramics: scientific evidences for clinical dentistry. Sao Paulo: Artes Medicas; 2009. [Google Scholar]
- [8].Leeson D The digital factory in both the modern dental lab and clinic. Dent Mater 2020;36:43–52. [DOI] [PubMed] [Google Scholar]
- [9].Corazza PH, de Castro HL, Feitosa SA, Kimpara ET, Della Bona A. Influence of CAD-CAM diamond bur deterioration on surface roughness and maximum failure load of Y-TZP-based restorations. Am J Dent 2015;28:95–9. [PubMed] [Google Scholar]
- [10].Stansbury JW, Idacavage MJ. 3D printing with polymers: challenges among expanding options and opportunities. Dent Mater 2016;32:54–64. [DOI] [PubMed] [Google Scholar]
- [11].Standardization IOf. ISO/ASTM 52900:2015 - Additive manufacturing - General principles - Terminology. ISO; 2015. [Google Scholar]
- [12].Melchels FP, Feijen J, Grijpma DW. A review on stereolithography and its applications in biomedical engineering. Biomaterials 2010;31:6121–30. [DOI] [PubMed] [Google Scholar]
- [13].Abduo J, Lyons K, Bennamoun M. Trends in computer-aided manufacturing in prosthodontics: a review of the available streams. Int J Dent 2014;2014:783948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Puebla K, Arcaute K, Quintana R, Wicker RB. Effects of environmental conditions, aging, and build orientations on the mechanical properties of ASTM type I specimens manufactured via stereolithography. Rapid Prototyp J 2012;18:374–88. [Google Scholar]
- [15].Childress KK, Alim MD, Hernandez JJ, Stansbury JW, Bowman CN. Additive manufacture of lightly crosslinked semicrystalline thiol-enes for enhanced mechanical performance. Polym Chem 2020;11:39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Dehurtevent M, Robberecht L, Hornez J-C, Thuault A, Deveaux E, Béhin P. Stereolithography: A new method for processing dental ceramics by additive computer-aided manufacturing. Dent Mater 2017;33:477–85. [DOI] [PubMed] [Google Scholar]
- [17].Rekow ED. Digital dentistry: The new state of the art - Is it disruptive or destructive? Dent Mater 2020;36:9–24. [DOI] [PubMed] [Google Scholar]
- [18].Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Brandeburski SBN, Vidal ML, Collares K, Zhang Y, Della Bona A. Edge chipping test in dentistry: a comprehensive review. Dent Mater 2020;36:e74–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Perroni AP, Kaizer MR, Della Bona A, Moraes RR, Boscato N. Influence of light-cured luting agents and associated factors on the color of ceramic laminate veneers: a systematic review of in vitro studies. Dent Mater 2018;34:1610–24. [DOI] [PubMed] [Google Scholar]
- [21].Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Park C, Kee W, Lim HP, Park SW. Combining 3D-printed metal and resin for digitally fabricated dentures: a dental technique. J Prosthet Dent 2020;123:389–92. [DOI] [PubMed] [Google Scholar]
- [23].Bilgin MS, Erdem A, Aglarci OS, Dilber E. Fabricating complete dentures with CAD/CAM and RP technologies. J Prosthodont 2015;24:576–9. [DOI] [PubMed] [Google Scholar]
- [24].Lin WS, Harris BT, Morton D. Use of CBCT Imaging, Open-Source Modeling Software, and Desktop Stereolithography 3D Printing to Duplicate a Removable Dental Prosthesis-A Proof of Concept. Compend Contin Educ Dent 2017;38:e5–8. [PubMed] [Google Scholar]
- [25].Totu EE, Nechifor AC, Nechifor G, Aboul-Enein HY, Cristache CM. Poly(methyl methacrylate) with TiO(2) nanoparticles inclusion for stereolitographic complete denture manufacturing - the fututre in dental care for elderly edentulous patients? J Dent 2017;59:68–77. [DOI] [PubMed] [Google Scholar]
- [26].Chen S, Yang J, Jia YG, Lu B, Ren L. A study of 3D-Printable reinforced composite resin: PMMA modified with silver nanoparticles loaded cellulose nanocrystal. Materials (Basel) 2018;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Chung YJ, Park JM, Kim TH, Ahn JS, Cha HS, Lee JH. 3D printing of resin material for denture artificial teeth: chipping and indirect tensile fracture resistance. Materials (Basel) 2018;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Lin WS, Harris BT, Pellerito J, Morton D. Fabrication of an interim complete removable dental prosthesis with an in-office digital light processing three-dimensional printer: a proof-of-concept technique. J Prosthet Dent 2018;120:331–4. [DOI] [PubMed] [Google Scholar]
- [29].Clark WA, Duqum I, Kowalski BJ. The digitally replicated denture technique: a case report. J Esthet Restor Dent 2019;31:20–5. [DOI] [PubMed] [Google Scholar]
- [30].Kalberer N, Mehl A, Schimmel M, Müller F, Srinivasan M. CAD-CAM milled versus rapidly prototyped (3D-printed) complete dentures: an in vitro evaluation of trueness. J Prosthet Dent 2019;121:637–43. [DOI] [PubMed] [Google Scholar]
- [31].Lee S, Hong SJ, Paek J, Pae A, Kwon KR, Noh K. Comparing accuracy of denture bases fabricated by injection molding, CAD/CAM milling, and rapid prototyping method. J Adv Prosthodont 2019;11:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Cha HS, Park JM, Kim TH, Lee JH. Wear resistance of 3D-printed denture tooth resin opposing zirconia and metal antagonists. J Prosthet Dent 2020. [DOI] [PubMed] [Google Scholar]
- [33].Takeda Y, Lau J, Nouh H, Hirayama H. A 3D printing replication technique for fabricating digital dentures. J Prosthet Dent 2020. [DOI] [PubMed] [Google Scholar]
- [34].Jurado CA, Tsujimoto A, Alhotan A, Villalobos-Tinoco J, AlShabib A. Digitally fabricated immediate complete dentures: case reports of milled and printed dentures. Int J Prosthodont 2020;33:232–41. [DOI] [PubMed] [Google Scholar]
- [35].Alharbi N, Osman RB, Wismeijer D. Factors Influencing the Dimensional Accuracy of 3D-Printed Full-Coverage Dental Restorations Using Stereolithography Technology. Int J Prosthodont 2016;29:503–10. [DOI] [PubMed] [Google Scholar]
- [36].Joo HS, Park SW, Yun KD, Lim HP. Complete-mouth rehabilitation using a 3D printing technique and the CAD/CAM double scanning method: a clinical report. J Prosthet Dent 2016;116:3–7. [DOI] [PubMed] [Google Scholar]
- [37].Lee WS, Lee DH, Lee KB. Evaluation of internal fit of interim crown fabricated with CAD/CAM milling and 3D printing system. J Adv Prosthodont 2017;9:265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Osman RB, Alharbi N, Wismeijer D. Build angle: does it influence the accuracy of 3D-Printed dental restorations using digital light-processing technology? Int J Prosthodont 2017;30:182–8. [DOI] [PubMed] [Google Scholar]
- [39].Alharbi N, Alharbi S, Cuijpers V, Osman RB, Wismeijer D. Three-dimensional evaluation of marginal and internal fit of 3D-printed interim restorations fabricated on different finish line designs. J Prosthodont Res 2018;62:218–26. [DOI] [PubMed] [Google Scholar]
- [40].Dikova TD, Dzhendov DA, Ivanov D, Bliznakova K. Dimensional accuracy and surface roughness of polymeric dental bridges produced by different 3D printing processes. Arch Mater Sci Eng 2018;94:65–75. [Google Scholar]
- [41].Katreva I, Dikova T, Tonchev T. 3D printing - an alternative of conventional crown fabrication: a case report. J Imab - Annu Proceeding 2018;24:2048–54. [Google Scholar]
- [42].Li X, Xie B, Jin J, Chai Y, Chen Y. 3D Printing Temporary Crown and Bridge by Temperature Controlled Mask Image Projection Stereolithography. Procedia Manuf 2018;26:1023–33. [Google Scholar]
- [43].Sa L, Kaiwu L, Shenggui C, Junzhong Y, Yongguang J, Lin W, et al. 3D printing dental composite resins with sustaining antibacterial ability. J Mater Sci 2019;54:3309–18. [Google Scholar]
- [44].Zimmermann M, Ender A, Egli G, Özcan M, Mehl A. Fracture load of CAD/CAM-fabricated and 3D-printed composite crowns as a function of material thickness. Clin Oral Investig 2019;23:2777–84. [DOI] [PubMed] [Google Scholar]
- [45].Peng CC, Chung KH, Yau HT, Ramos V Jr. Assessment of the internal fit and marginal integrity of interim crowns made by different manufacturing methods. J Prosthet Dent 2020;123:514–22. [DOI] [PubMed] [Google Scholar]
- [46].Peng CC, Chung KH, Ramos V Jr. Assessment of the adaptation of interim crowns using different measurement techniques. J Prosthodont 2020;29:87–93. [DOI] [PubMed] [Google Scholar]
- [47].Reymus M, Fabritius R, Keßler A, Hickel R, Edelhoff D, Stawarczyk B. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: the impact of resin material, build direction, post-curing, and artificial aging-an in vitro study. Clin Oral Investig 2020;24:701–10. [DOI] [PubMed] [Google Scholar]
- [48].Bae EJ, Jeong ID, Kim WC, Kim JH. A comparative study of additive and subtractive manufacturing for dental restorations. J Prosthet Dent 2017;118:187–93. [DOI] [PubMed] [Google Scholar]
- [49].Bae EJ, Jeong ID, Kim WC, Kim JH. A study on the machining accuracy of dental digital method focusing on dental inlay. J Adv Prosthodont 2018;10:321–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Jang KJ, Kang JH, Fisher JG, Park SW. Effect of the volume fraction of zirconia suspensions on the microstructure and physical properties of products produced by additive manufacturing. Dent Mater 2019;35:e97–106. [DOI] [PubMed] [Google Scholar]
- [51].Li H, Song L, Sun J, Ma J, Shen Z. Dental ceramic prostheses by stereolithography-based additive manufacturing: potentials and challenges. Adv Appl Ceram 2019;118:30–6. [Google Scholar]
- [52].Li R, Wang Y, Hu M, Wang Y, Xv Y, Liu Y, et al. Strength and Adaptation of Stereolithography-Fabricated Zirconia Dental Crowns: An In Vitro Study. Int J Prosthodont 2019;32:439–43. [DOI] [PubMed] [Google Scholar]
- [53].Wang W, Yu H, Liu Y, Jiang X, Gao B. Trueness analysis of zirconia crowns fabricated with 3-dimensional printing. J Prosthet Dent 2019;121:285–91. [DOI] [PubMed] [Google Scholar]
- [54].Zandinejad A, Methani MM, Schneiderman ED, Revilla-León M, Bds DM. Fracture resistance of additively manufactured zirconia crowns when cemented to implant supported zirconia abutments: an in vitro study. J Prosthodont 2019;28:893–7. [DOI] [PubMed] [Google Scholar]
- [55].Uçar Y, Aysan Meriç İ, Ekren O. Layered manufacturing of dental ceramics: fracture mechanics, microstructure, and elemental composition of lithography-sintered ceramic. J Prosthodont 2019;28, e310–e8. [DOI] [PubMed] [Google Scholar]
- [56].Ioannidis A, Bomze D, Hämmerle CHF, Hüsler J, Birrer O, Mühlemann S. Load-bearing capacity of CAD/CAM 3D-printed zirconia, CAD/CAM milled zirconia, and heat-pressed lithium disilicate ultra-thin occlusal veneers on molars. Dent Mater 2020;36, e109–e16. [DOI] [PubMed] [Google Scholar]
- [57].Schönherr JA, Baumgartner S, Hartmann M, Stampfl J. Stereolithographic additive manufacturing of high precision glass ceramic parts. Materials (Basel) 2020;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Tahayeri A, Morgan M, Fugolin AP, Bompolaki D, Athirasala A, Pfeifer CS, et al. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent Mater 2018;34:192–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Unkovskiy A, Bui PH, Schille C, Geis-Gerstorfer J, Huettig F, Spintzyk S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent Mater 2018;34, e324–e33. [DOI] [PubMed] [Google Scholar]
- [60].Shim JS, Kim JE, Jeong SH, Choi YJ, Ryu JJ. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J Prosthet Dent 2020. [DOI] [PubMed] [Google Scholar]
- [61].Lin CH, Lin YM, Lai YL, Lee SY. Mechanical properties, accuracy, and cytotoxicity of UV-polymerized 3D printing resins composed of Bis-EMA, UDMA, and TEGDMA. J Prosthet Dent 2020;123:349–54. [DOI] [PubMed] [Google Scholar]
- [62].Alharbi N, Osman R, Wismeijer D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J Prosthet Dent 2016;115:760–7. [DOI] [PubMed] [Google Scholar]
- [63].Digholkar S, Madhav VN, Palaskar J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J Indian Prosthodont Soc 2016;16:328–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Chen S, Yang J, Li K, Lu B, Ren L. Carboxylic acid-functionalized TiO2 nanoparticle-loaded PMMA/PEEK copolymer matrix as a dental resin for 3D complete denture manufacturing by stereolitographic technique. Int J Food Prop 2018;21:2557–65. [Google Scholar]
- [65].Kessler A, Reymus M, Hickel R, Kunzelmann KH. Three-body wear of 3D printed temporary materials. Dent Mater 2019;35:1805–12. [DOI] [PubMed] [Google Scholar]
- [66].Park JM, Ahn JS, Cha HS, Lee JH. Wear resistance of 3D printing resin material opposing zirconia and metal antagonists. Materials (Basel) 2018;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Revilla-León M, Umorin M, Özcan M, Piedra-Cascón W. Color dimensions of additive manufactured interim restorative dental material. J Prosthet Dent 2020;123:754–60. [DOI] [PubMed] [Google Scholar]
- [68].Mitteramskogler G, Gmeiner R, Felzmann R, Gruber S, Hofstetter C, Stampfl J, et al. Light curing strategies for lithography-based additive manufacturing of customized ceramics. Addit Manuf 2014;1–4:110–8. [Google Scholar]
- [69].Hinczewski C, Corbel S, Chartier T. Ceramic suspensions suitable for stereolithography. J Eur Ceram Soc 1998;18:583–90. [Google Scholar]
- [70].Chartier T, Chaput C, Doreau F, Loiseau M. Stereolithography of structural complex ceramic parts. J Mater Sci 2002;37:3141–7. [Google Scholar]
- [71].Johansson E, Lidström O, Johansson J, Lyckfeldt O, Adolfsson E. Influence of Resin Composition on the Defect Formation in Alumina Manufactured by Stereolithography. Materials (Basel) 2017;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Wheeler J, Deb S, Millar BJ. Evaluation of the effects of polishing systems on surface roughness and morphology of dental composite resin. Br Dent J 2020;228: 527–32. [DOI] [PubMed] [Google Scholar]


