Abstract
Objective:
Paramedics may perform endotracheal intubation (ETI) while treating patients with out-of-hospital cardiac arrest (OHCA). The gum elastic Bougie (Bougie) is an intubation adjunct that may optimize intubation success. There are few reports of Bougie-assisted intubation in OHCA nor its association with outcomes. We compared intubation success rates and OHCA outcomes between Bougie-assisted and non-Bougie ETI in the out-of-hospital Pragmatic Airway Resuscitation Trial (PART).
Methods:
This was a secondary analysis of patients receiving ETI enrolled in the Pragmatic Airway Resuscitation Trial (PART), a multicenter clinical trial comparing intubation-first vs. laryngeal tube-first strategies of airway management in adult OHCA. The primary exposure was use of Bougie for ETI-assistance. The primary endpoint was first-pass ETI success. Secondary endpoints included overall ETI success, time to successful ETI, return of spontaneous circulation, 72-hour survival, hospital survival and hospital survival with favorable neurologic status (modified Rankin Score ≤3). We analyzed the data using Generalized Estimating Equations and Cox Regression, adjusting for known confounders.
Results:
Of the 3,004 patients enrolled in PART, 1,227 received ETI, including 440 (35.9%) Bougie-assisted and 787 (64.1%) non-Bougie ETIs. First-pass ETI success did not differ between Bougie-assisted and non-Bougie ETI (53.1% vs. 42.8%; adjusted OR 1.12, 95% CI: 0.97 to 1.39). ETI overall success was slightly higher in the Bougie-assisted group (56.2% vs. 49.1%; adjusted OR 1.19, 95% CI: 1.01 to 1.32). Time to endotracheal tube placement or abandonment was longer for Bougie-assisted than non-Bougie ETI (median 13 vs. 11 min; adjusted HR 0.63, 95% CI: 0.45 to 0.90). While survival to hospital discharge was lower for Bougie-assisted than non-Bougie ETI (3.6% vs. 7.5%; adjusted OR 0.94, 95% CI: 0.92 to 0.96), there were no differences in ROSC, 72-hour survival or hospital survival or hospital survival with favorable neurologic status.
Conclusion:
While exhibiting slightly higher ETI overall success rates, Bougie-assisted ETI entailed longer airway placement times and potentially lower survival. The role of the Bougie assistance in ETI of OHCA remains unclear.
Keywords: cardiopulmonary arrest, airway management, intubation, emergency medical service
INTRODUCTION
Airway management plays an important role in cardiac arrest resuscitation. The most common advanced airway management technique performed by paramedics on out-of-hospital cardiac arrests (OHCA) is endotracheal intubation (ETI).2, 3 However, ETI is a difficult intervention associated with multiple complications such as tube placement failure, multiple attempts, unrecognized tube misplacement or dislodgement, and interruptions in chest compressions.4–7 These complications may prolong intubation efforts and worsen patient outcomes.
The gum elastic Bougie is a semi-rigid device used to facilitate ETI.8 The Bougie is inserted into the glottis during direct laryngoscopy, facilitating insertion of the ET tube into the trachea. While often reserved for patients with difficult airways or failed ETI efforts, some clinicians use the Bougie as an adjunct during initial ETI attempts.9 Driver, et al. found that first pass success was higher for Emergency Department intubations accomplished with the assistance of a Bougie.9 There have been few reports of Bougie use in the out-of-hospital setting.
The Pragmatic Airway Resuscitation Trial (PART) compared outcomes of patients with OHCA treated with a strategy of initial-ETI vs. initial laryngeal tube insertion.10 We sought to compare intubation success rates, airway placement times, and patient OHCA outcomes between Bougie and non-Bougie-assisted ETI in the PART trial.
METHODS
Study Design
We performed a post hoc analysis of data from the PART trial.10 The Institutional Review Boards of the participating institutions approved the parent PART study under federal rules for conduct of emergency research under Exception from Informed Consent (21 CFR 50.24). This analysis used deidentified data only, and was considered exempt from regulations related to human subjects research.
Setting
PART was a clinical trial comparing different methods of paramedic airway management strategies in patients with OHCA.10 The 27 participating EMS agencies were associated with Birmingham (Alabama), Dallas-Fort Worth (Texas), Milwaukee (Wisconsin), Pittsburgh (Pennsylvania) and Portland (Oregon) sites of the Resuscitation Outcomes Consortium. EMS agencies were cluster-randomized with cross-over to strategies of initial airway management with ETI vs. laryngeal tube (LT) in adult out-of-hospital cardiac arrest (OHCA). The primary outcome was 72-hour hospital survival. Enrollment occurred during 2015–2017.
Selection of Participants
For this study, we limited the analysis to patients who were enrolled in PART and received initial airway management using ETI. We included instances where a patient randomized to initial-LT received initial airway management with ETI. We excluded patients receiving only bag-valve-mask ventilation.
Primary Exposure
The primary exposure of interest for this analysis was use of the Bougie to facilitate ETI. Identification of Bougie use was defined as a clinical variable a priori before the trial. EMS personnel reported use of Bougie assistance for any attempt and the number of attempts, but not the specific sequence of techniques used for each patient. Therefore, we could not identify the individual ETI attempt where the Bougie was used including Bougie use following failed initial ETI versus Bougie use as an adjunct during initial ETI attempt. We defined Bougie-assisted ETI as any Bougie use during ETI attempts and non-Bougie ETI as ETI without the assistance of a Bougie.
Outcomes
We examined endpoints related to the process and outcomes of ETI. The primary outcome was first pass success, defined as successful intubation on a single attempt. Other outcomes included overall airway insertion success, defined as successful intubation on any attempt. Additional process endpoints included the number of ETI attempts, and time to ETI or abandonment of ETI efforts. EMS personnel reported the number of ETI attempts. Time to intubation was defined as the elapsed time from EMS unit arrival on-scene to successful ETI, censored at the point of abandonment of ETI efforts, termination of resuscitation or hospital arrival.
Clinical outcomes consisted of 72-hour survival, return of spontaneous circulation (ROSC), hospital survival, and hospital survival with favorable neurologic status (Modified Rankin Score ≤3).
Analysis
We compared baseline characteristics between Bougie and non-Bougie-assisted cases, including age, sex, race, witnessed arrest (bystander and EMS), bystander chest compression and initial cardiac arrest rhythm. We examined the association of first pass ETI success between Bougie and non-Bougie-assisted ETI using Generalized Estimating Equations (GEE), accounting for clustering by randomized cluster, and adjusting for age, sex, race, witnessed arrest (bystander and EMS), bystander chest compression and initial electrocardiographic rhythm. We repeated the analysis for overall airway success. We examined the variation in Bougie use across participating EMS agencies.
We compared time to ETI between Bougie and non-Bougie cases using Kaplan-Meier survival graphs and Cox Regression. The model was adjusted for relevant confounders (adjusted for age, sex, race, witnessed arrest (bystander and EMS), bystander chest compression and initial electrocardiographic rhythm) and used a shared frailty model to account for randomization cluster.11 Using GEE, we examined the associations between Bougie use and key adverse events, including pneumothorax, rib fractures, oropharyngeal or hypopharyngeal injury, airway swelling or edema, and aspiration pneumonia or pneumonitis. We also analyzed the associations between Bougie assistance and patient outcomes using GEE, accounting for clustering by randomized cluster, and adjusting for age, sex, race, witness arrest (bystander and EMS), bystander chest compression and initial cardiac arrest rhythm.
RESULTS
From the 3,004 patients enrolled in PART, we included 1,227 receiving ETI as the airway management device, including 440 Bougie-assisted, and 787 non-Bougie-assisted. (Figure 1) Patients receiving Bougie-assisted ETI were more likely to be white and of Hispanic ethnicity. (Table 1) Bystander chest compressions were more common with Bougie-assisted ETI. Other characteristics were similar between Bougie and non-Bougie cases. There were 13 cases where video laryngoscopy was used in non-Bougie-assisted ETI. Bougie use varied from 0% to 100% across the 27 EMS agencies. Bougies were used in 15 of 27 EMS agencies.
Figure 1 –
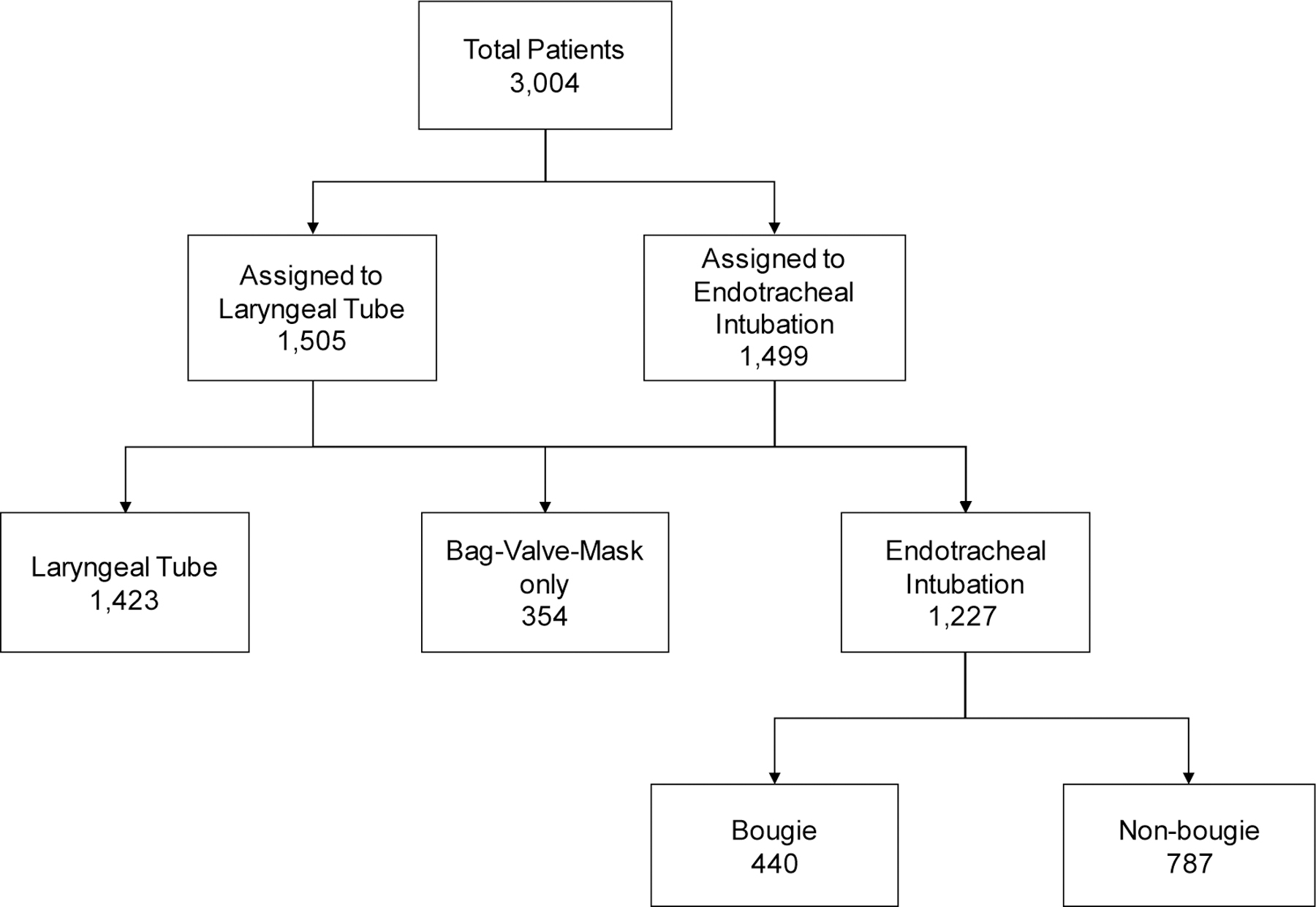
Overview of study population.
TABLE 1 –
Characteristics of the Study Population. Includes n=440 Bougie and n=787 non-Bougie endotracheal intubation cases.
| Characteristics | Bougie-Assisted Intubation N (%) | Non-Bougie-Assisted Intubation N (%) |
|---|---|---|
| Age, median (IQR) | 65 (22) | 64 (22) |
| Sex | ||
| Male | 253 (57.5) | 488 (62.0) |
| Female | 187 (42.5) | 299 (38.0) |
| Race | ||
| White | 233 (53.0) | 387 (49.2) |
| Hispanic | 38 (8.8) | 36 (4.6) |
| Black | 108 (24.6) | 276 (35.1) |
| Asian | 9 (2.1) | 12 (1.5) |
| Pacific Islander | 1 (0.2) | 2 (0.3) |
| Native American | 0 | 2 (0.3) |
| Other | 9 (2.1) | 4 (0.5) |
| Witnessed Arrest, | 233 (53.7) | 347 (48.5) |
| EMS witnessed | 55 (12.5) | 81 (10.3) |
| Bystander witnessed | 178 (47.0) | 266 (42.0) |
| Not witnessed | 201 (46.3) | 368 (51.5) |
| Missing | 6 (1.4) | 72 (9.2) |
| Bystander CPR, n / N [%] | ||
| Yes | 239 (54.3) | 341 (43.3) |
| No | 138 (31.4) | 335 (42.6) |
| Missing | 63 (14.3) | 111 (14.1) |
| First rhythm | ||
| Shockable | 77 (17.5) | 130 (16.5) |
| Non-shockable | 363 (82.5) | 656 (83.5) |
First pass success was higher with Bougie (52.1%) than without (43.8%); however, this difference was not significant after adjustment for confounders (OR 1.12, 95% CI: 0.97 to 1.39). Overall ETI success was higher in the Bougie (56.1%) than non-Bougie group (49.1%) (adjusted OR 1.16; 95% CI: 1.01 to 1.32). The number of attempts were higher in the non-Bougie group than the Bougie-assisted group. (Table 2) Time to successful ETI was longer with than without Bougie assistance; 13.0 min vs. 11.0 min, HR 0.63 (95% CI: 0.45 to 0.90) (Figure 2).
TABLE 2 –
Association of Bougie assistance with endotracheal intubation performance.
| Characteristics | Bougie N (%) | Non-Bougie N (%) | Unadjusted OR (95% CI) | *Adjusted OR (95% CI) |
|---|---|---|---|---|
| First pass success | 229 (52.1) | 345 (43.8) | 1.15 (1.03 to 1.30) | 1.12 (0.97 to 1.39) |
| Overall success | 247 (56.1) | 386 (49.1) | 1.19 (1.08 to 1.31) | 1.16 (1.01 to 1.32) |
| Number of attempts | ||||
| 1 | 399 (90.7) | 580 (73.7) | ||
| 2 | 38 (8.6) | 193 (24.5) | ||
| 3 | 2 (0.5) | 13 (1.7) | ||
| 4 | 1 (0.2) | 1 (0.1) |
Adjusted for age, sex, race, witnessed arrest, bystander chest compression and initial cardiac rhythm.
Figure 2 –
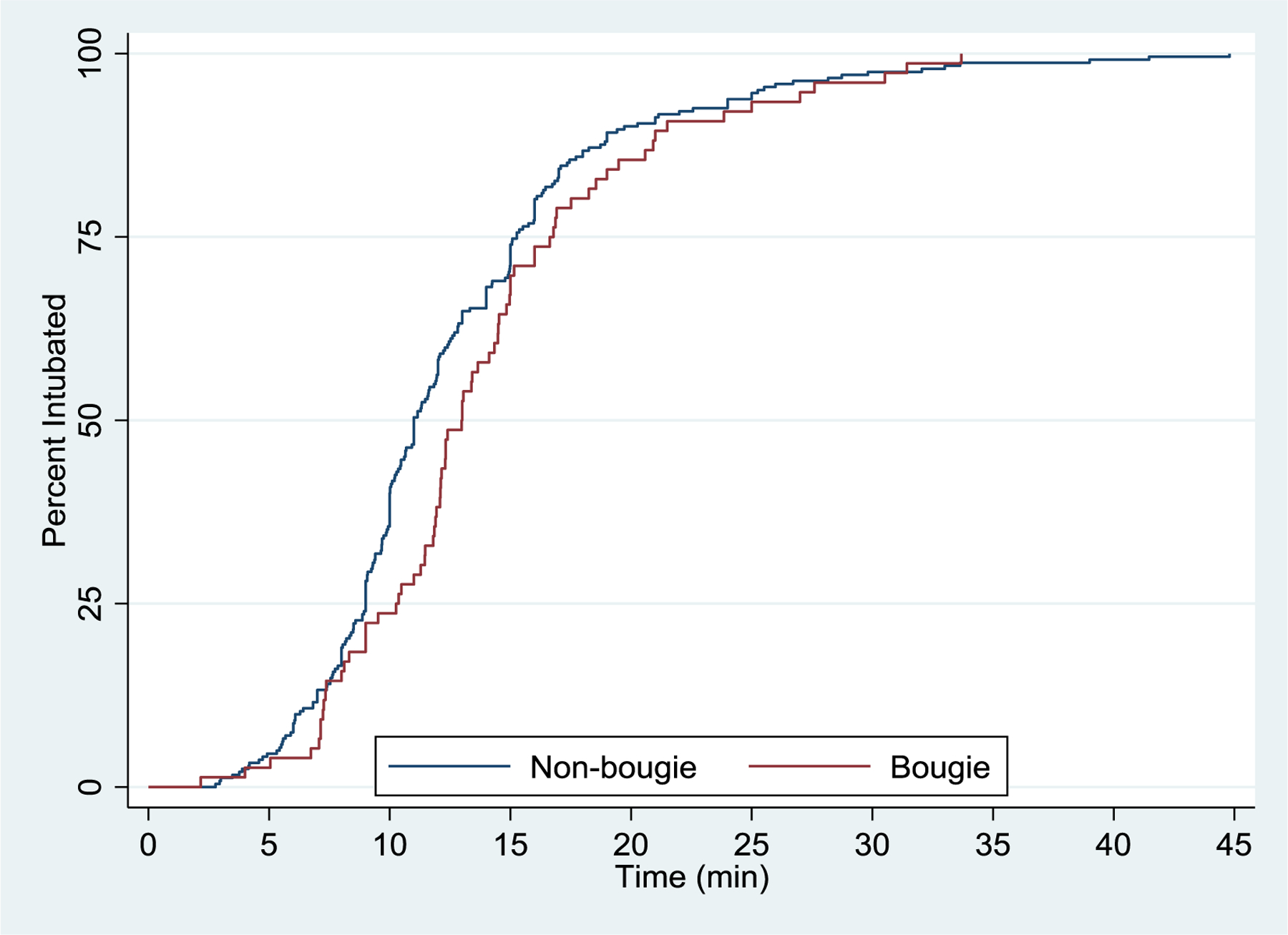
Time to intubation for Bougie vs non-Bougie endotracheal intubation. Median time to intubation was 13 minutes for Bougie use and 11 minutes for non-Bougie use (adjusted hazard ratio 0.63, 95% CI: 0.95 to 1.00)
Bougie use was not associated with select adverse events. (Table 3) Survival to 72-hours did not differ significantly between Bougie and non-Bougie ETI (10.7% vs. 15.1%; adjusted OR 0.97, 95% CI: 0.92 to 1.03). (Table 4) There was also no difference in ROSC between the Bougie and non-Bougie (31.7% vs. 41.4% adjusted OR 1.00, 95% CI: 0.89 to 1.12). However, survival to hospital discharge was lower in the Bougie group than the non-Bougie group (3.6% vs. 7.5%; adjusted OR 0.94, 95% CI: 0.92 to 0.96). Hospital survival with favorable functional outcome did not differ between Bougie and non-Bougie ETI (1.6% vs. 4.3% adjusted OR 0.98, 95% CI: 0.95 to 1.00).
TABLE 3 –
Association of Bougie-assisted endotracheal intubation with adverse events.
| Outcomes | Bougie N (%) | Non-Bougie N (%) | Unadjusted OR (95% CI) | *Adjusted OR (95% CI) |
|---|---|---|---|---|
| Pneumothorax (first chest x-ray) | 8 (6.8) | 19 (8.3) | 0.92 (0.85 to 0.99) | 0.98 (0.92 to 1.05) |
| Rib fractures (first chest x-ray) | 11 (9.4) | 13 (5.7) | 1.10 (0.998 to 1.21) | 1.13 (0.98 to 1.31) |
| Oropharyngeal or hypopharyngeal injury (first 24 hours) | 1 (0.4) | 1 (0.2) | 1.268 (1.267 to 1.269) | 1.25 (1.20 to 1.30) |
| Airway swelling or edema (first 24 hours) | 0 (0.0) | 4 (0.9) | 0.985 (0.985 to 0.986) | 0.98 (0.95 to 1.02) |
| Pneumonia or aspiration pneumonia (first 72 hours) | 13 (4.6) | 30 (6.5) | 1.00 (0.89 to 1.13) | 1.03 (0.89 to 1.19) |
Adjusted for age, sex, race, witnessed arrest, bystander chest compression and initial cardiac rhythm.
TABLE 4 –
Association of Bougie-assisted endotracheal intubation with patient outcomes.
| Outcomes | Bougie N (%) | Non-Bougie N (%) | Unadjusted OR (95% CI) | *Adjusted OR (95% CI) |
|---|---|---|---|---|
| 72 Hour Survival | 47 (10.7) | 118 (15.1) | 0.97 (0.94 to 1.01) | 0.97 (0.9 to 1.03) |
| ROSC | 91 (31.7) | 193 (41.4) | 0.96 (0.86 to 1.06) | 1.00 (0.89 to 1.12) |
| Hospital Survival | 16 (3.6) | 59 (7.5) | 0.97 (0.94 to 0.99) | 0.94 (0.92 to 0.96) |
| Hospital Survival with Favorable Neurologic Status (MRS ≤3) | 7 (1.6) | 34 (4.3) | 0.98 (0.96 to 1.01) | 0.98 (0.95 to 1.00) |
Adjusted by age, sex, race, witnessed arrest, bystander chest compression and initial cardiac rhythm.
DISCUSSION
In this analysis we compared the process and outcomes of care between Bougie-with non-Bougie-assisted ETI in the PART trial. While there was no significant difference in first pass success rate, we observed slightly higher ETI overall success with Bougie assistance. Time to airway insertion was longer with Bougie use. While hospital survival was slightly lower with Bougie use, there were no other outcome differences between Bougie and non-Bougie use. Our analysis provides one of the first and largest descriptions of Bougie use as an adjunct for ETI in adults with OHCA.
While several studies have described Bougie use in the simulated airway emergencies, few studies describe its use in clinical out-of-hospital practice.12–14 In a clinical trial by a ground and air-based critical care transport service, Heegard, et al. randomized 51 patients to Bougie-assisted or standard intubation, finding no significant difference in ETI success or time to intubation.15 In a French out-of-hospital series, Combes, et al. described Bougie use as an adjunct for 41 difficult ETIs, finding that the device facilitated successful intubation in 78%.16 In the emergency department, the most prominent study is Driver, et al.’s randomized trial of 757 rapid sequence intubations, which found significantly greater first pass success with Bougie than standard ETI.9
There are many potential reasons for the unexpected findings of our study. Our series was non-randomized, and thus Bougie use was likely influenced by paramedic practices or protocols. Of the 27 EMS agencies, in the series, 94% of all the Bougie uses were performed in 5 agencies; Bougie use was per paramedic discretion at all of these EMS agenciesWe do not know if paramedics chose Bougie use to optimize initial ETI efforts or in a rescue capacity after unsuccessful ETI attempts. The structure of the data set did not allow us to ascertain whether these variations may have been due to variations in organizational structure or paramedic perceptions of airway difficulty. The almost two-minute longer time to airway placement for Bougie-assisted ETI may be partially explained if Bougie was used as a rescue device. The observed 8 percent difference in first pass and overall ETI success rates may be considered clinically important, but formal inferences were limited by the sample size; a larger series may have revealed an association with Bougie use. Also, the differences in first-pass and overall ETI success were mitigated after adjustment for confounders, further reinforcing the possibility of confounding by indication as a source of bias. While most likely due to confounding by indication, the lower OHCA survival to discharge associated with Bougie use may also reflect unidentified harms associated with the device and prolonged ETI efforts.
Our results neither support nor refute Bougie-assisted ETI in OHCA. The perceived advantages of Bougie over conventional intubation include its thinner profile, easier technique for insertion through the glottis, and tactile feedback as the tip of the Bougie touches tracheal rings. In the setting of emergency out-of-hospital airway management, these practical features could ease initial or subsequent ETI attempts. Randomized clinical trials are ultimately needed to definitively indicate the effect of Bougie assistance upon ETI success or patient outcomes. The optimal design for such a trial would be to randomize patients to either Bougie-assisted or conventional ETI as the initial strategy in advanced airway management. Additional study must also ascertain injuries and adverse events occurring from Bougie use.
LIMITATIONS
PART was not designed to study the efficacy of Bougie assistance. Bougie use was applied by paramedic discretion and was not randomized. Bougie use varied across the agencies. We were able to identify Bougie use but not the sequence or individual attempt where the device was used. We could not ascertain complications associated with Bougie use. We could not determine EMS personnel airway insertion success patterns. We did not examine the association between Bougie uses upon chest compression or ventilation patterns. We did not have information on the protocols for Bougie use. We observed significant associations between Bougie use and hospital survival but not other clinical outcomes. The current analysis is post hoc in nature and should not be used to define causation. Cormack-Lehane or glottic visualization ratings were not available.17 The structure of the PART data did not allow us to ascertain the exact attempt where the Bougie was used. Airway performance was self-reported by paramedics. We could not ascertain reasons for racial differences in Bougie use.
CONCLUSION
In this post hoc analysis of prospectively collected data from PART, we found that Bougie-assisted ETI exhibited slightly higher overall ETI success rates with longer airway placement times and lower survival. Additional study is needed to verify the safety and effectiveness of Bougie-assisted out-of-hospital intubation for cardiac arrest.
Acknowledgments
Conflicts of Interest:
Research Supported by Grant UH2/UH3-HL125163 from National Heart Lung and Blood Institute
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hasegawa K, Shigemitsu K, Hagiwara Y, et al. Association between repeated intubation attempts and adverse events in emergency departments: an analysis of a multicenter prospective observational study. Annals of emergency medicine. 2012;60:749–754 e742. [DOI] [PubMed] [Google Scholar]
- 2.Wang HE, Mann NC, Mears G, Jacobson K, Yealy DM. Out-of-hospital airway management in the United States. Resuscitation. 2011;82:378–385. [DOI] [PubMed] [Google Scholar]
- 3.Nwanne T, Jarvis J, Barton D, Donnelly JP, Wang HE. Advanced airway management success rates in a national cohort of emergency medical services agencies. Resuscitation. 2020;146:43–49. [DOI] [PubMed] [Google Scholar]
- 4.Wang HE, Kupas DF, Paris PM, Bates RR, Costantino JP, Yealy DM. Multivariate predictors of failed prehospital endotracheal intubation. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2003;10:717–724. [DOI] [PubMed] [Google Scholar]
- 5.Wang HE, Kupas DF, Paris PM, Bates RR, Yealy DM. Preliminary experience with a prospective, multi-centered evaluation of out-of-hospital endotracheal intubation. Resuscitation. 2003;58:49–58. [DOI] [PubMed] [Google Scholar]
- 6.Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Annals of emergency medicine. 2001;37:32–37. [DOI] [PubMed] [Google Scholar]
- 7.Wang HE, Simeone SJ, Weaver MD, Callaway CW. Interruptions in cardiopulmonary resuscitation from paramedic endotracheal intubation. Annals of emergency medicine. 2009;54:645–652 e641. [DOI] [PubMed] [Google Scholar]
- 8.Jabre P, Combes X, Leroux B, et al. Use of gum elastic bougie for prehospital difficult intubation. The American journal of emergency medicine. 2005;23:552–555. [DOI] [PubMed] [Google Scholar]
- 9.Driver BE, Prekker ME, Klein LR, et al. Effect of Use of a Bougie vs Endotracheal Tube and Stylet on First-Attempt Intubation Success Among Patients With Difficult Airways Undergoing Emergency Intubation: A Randomized Clinical Trial. JAMA : the journal of the American Medical Association. 2018;319:2179–2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang HE, Schmicker RH, Daya MR, et al. Effect of a Strategy of Initial Laryngeal Tube Insertion vs Endotracheal Intubation on 72-Hour Survival in Adults With Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA : the journal of the American Medical Association. 2018;320:769–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu L, Wolfe RA, Huang X. Shared frailty models for recurrent events and a terminal event. Biometrics. 2004;60:747–756. [DOI] [PubMed] [Google Scholar]
- 12.Messa MJ, Kupas DF, Dunham DL. Comparison of bougie-assisted intubation with traditional endotracheal intubation in a simulated difficult airway. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2011;15:30–33. [DOI] [PubMed] [Google Scholar]
- 13.Evrin T, Smereka J, Gorczyca D, et al. Comparison of Different Intubation Methods in Difficult Airways during Simulated Cardiopulmonary Resuscitation with Continuous Chest Compression: A Randomized Cross-Over Manikin Trial. Emerg Med Int. 2019;2019:7306204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phelan MP, Moscati R, D’Aprix T, Miller G. Paramedic use of the endotracheal tube introducer in a difficult airway model. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2003;7:244–246. [DOI] [PubMed] [Google Scholar]
- 15.Heegaard WG, Black C, Pasquerella C, Miner J. Use of the endotracheal tube introducer as an adjunct for oral tracheal intubation in the prehospital setting. Air medical journal. 2003;22:28–31. [DOI] [PubMed] [Google Scholar]
- 16.Combes X, Leroux B, Jabre P, Margenet A, Dhonneur G. Out-of-hospital rescue oxygenation and tracheal intubation with the intubating laryngeal mask airway in a morbidly obese patient. Annals of emergency medicine. 2004;43:140–141. [DOI] [PubMed] [Google Scholar]
- 17.Cormack RS, Lehane JR, Adams AP, Carli F. Laryngoscopy grades and percentage glottic opening. Anaesthesia. 2000;55:184. [DOI] [PubMed] [Google Scholar]


