Abstract
Background:
Few studies have examined primary care management for acute sciatica, including referral to physical therapy.
Objective:
To evaluate whether early referral to physical therapy reduced disability more than usual care (UC) alone for patients with acute sciatica.
Design:
Randomized controlled clinical trial. (ClinicalTrials.gov: NCT02391350)
Setting:
2 health care systems in Salt Lake City, Utah.
Patients:
220 adults aged 18 to 60 years with sciatica of less than 90 days’ duration who were making an initial primary care consultation.
Intervention:
All participants received imaging and medication at the discretion of the primary care provider before enrollment. A total of 110 participants randomly assigned to UC were provided 1 session of education, and 110 participants randomly assigned to early physical therapy (EPT) were provided 1 education session and then referred for 4 weeks of physical therapy, including exercise and manual therapy.
Measurements:
The primary outcome was the Oswestry Disability Index (OSW) score after 6 months. Secondary outcomes were pain intensity, patient-reported treatment success, health care use, and missed workdays.
Results:
Participants in the EPT group had greater improvement from baseline to 6 months for the primary outcome (relative difference, −5.4 points [95% CI, −9.4 to −1.3 points]; P = 0.009). The OSW and several secondary outcomes favored EPT after 4 weeks. After 1 year, between-group differences favored EPT for the OSW (relative difference, −4.8 points [CI, −8.9 to −0.7 points]) and back pain intensity (relative difference, −1.0 points [CI, −1.6 to −0.4 points]). The EPT group was more likely to self-report treatment success after 1 year (45.2%) than the UC group (27.6%) (relative risk, 1.6 [CI, 1.1 to 2.4]). There were no significant differences in health care use or missed workdays.
Limitation:
The patients and providers were unblinded, and specific physical therapy interventions responsible for effects could not be determined.
Conclusion:
Referral from primary care to physical therapy for recent-onset sciatica improved disability and other outcomes compared with UC.
TOC blurb
Some guidelines suggest the use of supervised exercise or manual therapy for management of low back pain with sciatica. Clinical trials of these treatments of sciatica are limited. This randomized controlled trial examined the effects of early referral to physical therapy plus a single educational session versus a single educational session alone on disability among patients with acute sciatica.
Back pain is the second most common reason for a primary care visit and the costliest medical condition in the United States, with an estimated $134 billion spent in 2016 (1, 2). Sciatica is a condition that accompanies some cases of low back pain (LBP) and is characterized by radiating symptoms in the leg. In most cases, sciatica is attributable to lumbar disk disorders (3). Sciatica is estimated to occur in about 30% of LBP episodes, with an annual incidence of 1% to 5% (4–6). Although sciatica is common, there is little research on the effectiveness of common nonpharmacologic management options to inform clinical guidelines directing primary care management (7, 8).
Persons with recent-onset sciatica often make an initial consultation in primary care (9). Although many persons with acute sciatica have substantial reductions in leg and back pain within weeks (6, 10), the overall prognosis for LBP with sciatica is worse than that for axial LBP (11). The presence of sciatica, particularly if leg pain extends distal to the knee with signs of nerve root compression, increases risk for worse outcomes and increased health care use, including surgery, during 1 year of follow-up (11–13). Observational cohorts from primary care settings report that 45% of patients with LBP and sciatica do not have meaningful improvement in disability after 1 year (14), and 34% of patients report chronic pain after 2 years (9).
Primary care clinical guidelines recommend educating patients with LBP and sciatica to remain active and avoid bed rest (8, 15–17). Nonsteroidal anti-inflammatory drugs are considered first-line analgesic medication, with consideration of systemic corticosteroids or weak opioids if nonsteroidal anti-inflammatory drugs are contraindicated or ineffective (15, 18). Some recent guidelines recommend supervised exercise and manual therapy as nonpharmacologic options, but more conclusive guidance is hampered by the limited number of clinical trials focused on acute sciatica in primary care (7, 8, 15). Research investigating the pragmatic question of how to provide supervised exercise and manual therapy from a primary care setting is needed (7, 19, 20). We did a randomized clinical trial of patients with an initial primary care visit for LBP and sciatica of less than 90 days’ duration. We compared usual care (UC) of advice and education with or without the addition of physical therapy referral over a 4-week treatment period. Participants were followed for 1 year, and patient-reported disability was the primary comparative effectiveness outcome.
Methods
Design Overview
This single-blind, parallel-group randomized trial is reported according to the CONSORT (Consolidated Standards of Reporting Trials) extension for nonpharmacologic trials (21). The study protocol and statistical analysis plan are available in the Supplement (available at Annals.org). Ethics approval was obtained from the University of Utah and Intermountain Healthcare institutional review boards. The trial was initiated by the investigators and funded by the Agency for Healthcare Research and Quality. It was registered with ClinicalTrials.gov (NCT02391350) on 18 March 2015. The first participant was enrolled in February 2015, and the final participant was enrolled in October 2018. Follow-up data collection was completed in October 2019. No changes were made to the study protocol after the trial began. Experimental treatments were provided to participants at no cost. No outside agency had any role in the trial design, data collection, analysis, or manuscript preparation. The authors vouch for the completeness and accuracy of the data and the analyses and fidelity of the trial to the protocol.
Setting and Participants
The trial was done in 2 health care systems (University of Utah and Intermountain Healthcare) in Salt Lake City, Utah. Adults with an initial primary care visit for LBP and sciatica were recruited. An initial visit was defined as one without treatment from any provider for LBP or sciatica in the prior 6 months. Potential participants were identified using electronic health records and were sent a letter about the study after completing a primary care visit. A research team made follow-up telephone calls to identify those interested in meeting with a research assistant to determine eligibility and provide consent. Additional eligibility criteria were age 18 to 60 years, Oswestry Disability Index (OSW) score of 20 or more, current symptoms present for 90 days or less, symptoms extending below the knee in the past 72 hours, and examination signs consistent with sciatica (positive result on straight leg raise test or sensory or motor deficit in a pattern consistent with a lumbar nerve root). Exclusion criteria were lumbar surgery in the past year, pregnancy, or signs of a potentially serious condition (for example, cauda equina syndrome, rapidly progressing neurologic deficit, or fracture) at the time of enrollment. All participants provided written informed consent.
Randomization and Interventions
Participants were randomly assigned in 1:1 allocation to receive early physical therapy (EPT) or UC. Randomization schemes were generated by a study statistician before enrollment with random number generation software using a random permuted block procedure in differing block sizes (2 or 4). Treatment group assignment was delivered through the randomization module of the Research Electronic Data Capture (REDCap) site developed for data management in the study (22). The random treatment assignment was revealed by the research assistant after all baseline assessments and education activities were complete to avoid bias in the baseline evaluation or education provision.
Given that study assessments and random assignment occurred after the primary care visit, all participants received medication and imaging referrals at the discretion of the primary care provider under usual clinical circumstances. After completing all baseline assessments, all participants were given a copy of The Back Book (23), a patient education booklet with evidence-based messages about the favorable prognosis of LBP and the importance of remaining active and avoiding bed rest (24). The research assistant reinforced these messages and advised all participants to follow up with their primary care provider as needed if unsatisfied with their progress. After these activities were completed, the randomization assignment was revealed to the research assistant and participant. Those assigned to UC received no further interventions. Those assigned to EPT were scheduled to begin physical therapy within 3 days with a physical therapist trained in study procedures.
The EPT treatment was provided by 1 of 9 physical therapists. All physical therapists were licensed providers in the state of Utah and were trained by the investigators in a 1-day training session that included written materials and hands-on practice. The study protocol (Supplement) gives details of the EPT treatment. The approach was designed to pragmatically reflect physical therapy care for LBP and sciatica. Exercise and manual therapy intended to centralize and diminish sciatica symptoms were considered core components of the physical therapy protocol. The exercise program used principles of mechanical diagnosis and therapy (25). On the basis of mechanical diagnosis and therapy principles, each session began with an assessment of symptom response to repeated or sustained movements of the lumbar spine. Movements or positions that centralize or move symptoms toward the spinal midline form the basis for exercise recommendations. For patients with LBP and sciatica, lumbar extension exercises are often most effective for centralizing symptoms (26). Therapists were provided a general progression of extension exercises with instructions to individualize the program to maximize symptom centralization. Manual therapy for the EPT group could include mobilization or high-velocity thrust manipulation of the lumbar spine to facilitate symptom centralization. Manual therapy could be done with the patient prone or side-lying with varied amplitude and velocity to maximize symptom centralization.
Physical therapists were instructed to include exercise and manual therapy in each session, with specific content and dosage left to the pragmatic determination of the physical therapist. Traction could be used at the physical therapist’s discretion to facilitate centralization. Physical therapists recorded fidelity to the treatment protocol and reported any off-protocol interventions. Participants were provided written directions and instructed to do assigned exercises at home every 4 to 5 hours on days between sessions. The EPT protocol recommended 6 to 8 physical therapy sessions during the 4-week treatment period, with a frequency of 2 weekly sessions during the first 2 weeks and 1 to 2 sessions in weeks 3 and 4.
Outcomes and Follow-up
The primary outcome was score on the OSW, a 10-item measure of LBP-related disability (27). Scores range from 0 to 100, with higher scores indicating greater disability. Minimum important difference is 6 to 8 points for acute LBP and sciatica (28, 29). Mean change from baseline to 6 months was the primary analysis, and 4 weeks and 1 year were considered secondary time points for the primary outcome. Secondary outcomes included separate scores of 0 to 10 on the Numeric Pain Rating Scale for low back and leg pain severity; the Pain Catastrophizing Scale (30) (score range, 0 to 52; higher scores indicate greater catastrophizing); the Fear-Avoidance Beliefs Questionnaire physical activity and work subscales (31) (score ranges, 0 to 24 and 0 to 42, respectively; higher scores indicate greater fear-avoidance beliefs); and the EuroQol 5-dimension tool, which assessed self-rated overall health from 0 (worst) to 100 (best imaginable) and quality of life from 0 to 1.0, with higher numbers indicating greater quality of life (32).
Participants reported health care use and work outcomes monthly, including advanced imaging (computed tomography or magnetic resonance imaging), emergency department visits, injections, surgical procedures, and missed workdays for LBP or sciatica. Other data collected included the STarT Back Screening Tool to categorize patients as having low, medium, or high risk for prolonged symptoms (33). Side effects of EPT were assessed after 4 weeks (34). Self-reported treatment success was collected by asking about the amount of improvement since beginning the study with 15-level Likert responses (35). Responses were dichotomized to define success as occurring when a rating of “a great deal better” or “a very great deal better” was selected.
Outcomes were assessed at 4 weeks, 6 months, and 1 year after enrollment. The 4-week assessment was in person with a research assistant blinded to treatment assignment. Six-month and 1-year assessments and monthly reports of health care use were completed remotely through the study’s REDCap platform.
Statistical Analysis
We selected the sample size of 110 participants per group (total n = 220) to provide at least 86% power with a 2-sided α level of 0.05 to detect a treatment effect of 7 points (the approximate minimum clinically important difference) in mean change on the OSW from baseline to 6 months if 90% follow-up is assumed and to provide 82% power if 80% follow-up is assumed. Power analyses assumed an SD of 16 points for change in the OSW on the basis of prior work (26, 28). Unless stated otherwise, all analyses were done in the randomized study population with patients examined on the basis of randomly assigned treatment regardless of adherence. Analyses were done using SAS software, version 9.4 (SAS Institute).
We used longitudinal mixed-effects analysis of covariance models to estimate the effects of the randomized treatments on the mean changes from baseline to each follow-up assessment of the primary OSW outcome and numerical outcomes while controlling for the baseline levels of each outcome variable. The comparison of the OSW at 6 months was designated as the primary comparison. Treatment comparisons for the OSW at 4 weeks and 1 year, and for other outcomes across follow-up times, were interpreted as secondary comparisons and evaluated without adjustment for multiple comparisons.
We calculated relative risk to compare the risk for participants reporting at least 1 occurrence of each of the designated health care use outcomes between the randomized treatment groups. We used a generalized estimating equations analysis with robust SEs under a negative binomial outcome model to accommodate skewed data with a high proportion of 0 values to compare the number of missed workdays due to LBP per month over the 1-year follow-up between the randomized groups. We used relative risk statistics to compare the likelihood of patient-reported treatment success at 4-week, 6-month, and 1-year follow-ups between the randomized groups.
We used sensitivity analyses to address the robustness of our results. First, we did an as-treated analysis in which participants were analyzed according to the treatment received in the first 4 weeks. The as-treated analysis assigned participants randomly assigned to EPT who did not attend any therapy sessions to the UC group. Participants randomly assigned to UC who chose to attend physical therapy in the first 4 weeks were analyzed with the EPT group. Second, we repeated the primary and secondary analyses using fully sequential multiple imputation with an imputation model that included auxiliary variables to reduce the risk of bias due to loss to follow-up and missing follow-up measurements. Finally, we repeated analyses of health care use outcomes using Cox regression to compare time from randomization to the first reported occurrence of the outcome, with follow-up censored at the last month in which the health care use questionnaire was completed and intervening months with missing data excluded from the risk set (36).
Role of the Funding Source
This study was funded by the Agency for Healthcare Research and Quality, which had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Results
Study Participants
From February 2015 through October 2018, a total of 2116 persons were screened; 300 were eligible, and 220 were enrolled (Figure 1). Mean age of participants was 39.0 years (SD, 11.2), and 107 (48.6%) were women. Mean symptom duration was 35.8 days (SD, 26.1). Participants were randomly assigned to either the EPT group (n = 110) or the UC group (n = 110). Groups were similar at baseline (Table 1). Baseline OSW means were 35.8 points (SD, 15.8) and 38.9 points (SD, 13.8) for the UC and EPT groups, respectively.
Figure 1.
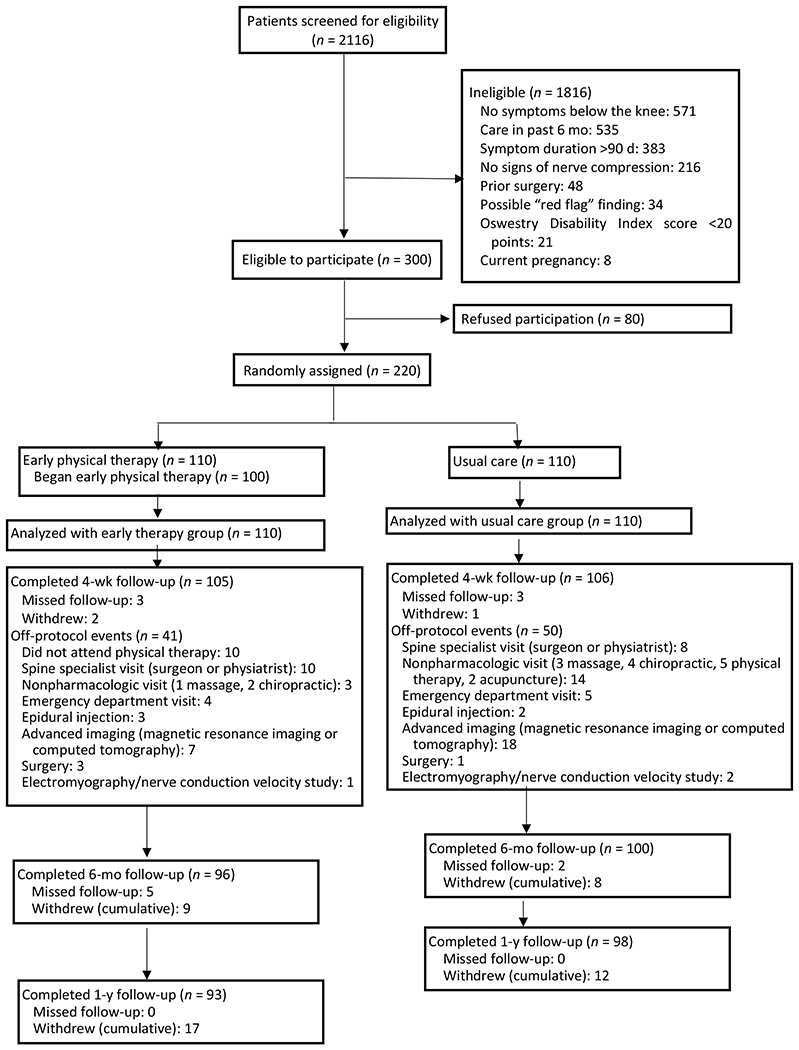
Enrollment and assessments, by treatment group.
Table 1.
Baseline Participant Characteristics
| Characteristic | UC Group (n = 110) | EPT Group (n = 110) |
|---|---|---|
| Mean age (SD), y * | 37.9 (11.2) | 40.0 (11.2) |
| Female, n (%) * | 59 (53.6) | 48 (43.6) |
| Race, n (%) | ||
| American Indian or Alaskan Native | 2 (1.8) | 5 (4.5) |
| African American or Black | 3 (2.7) | 1 (0.9) |
| Asian | 5 (4.5) | 2 (1.8) |
| Native Hawaiian or other Pacific Islander | 1 (0.9) | 1 (0.9) |
| White | 89 (80.9) | 92 (83.6) |
| Other or multiracial | 7 (6.4) | 7 (6.4) |
| Not reported | 3 (2.7) | 2 (1.8) |
| Ethnicity, n (%) | ||
| Hispanic or Latino | 16 (14.5) | 14 (12.7) |
| Not Hispanic or Latino | 84 (76.3) | 81 (73.6) |
| Not reported | 10 (9.0) | 15 (13.6) |
| Mean body mass index (SD), kg/m2 | 29.5 (7.9) | 29.5 (7.0) |
| Married/live with significant other, n (%) | 56 (50.9) | 59 (53.7) |
| Education (completed post–high school degree), n (%) | 52 (47.3) | 57 (52.3) |
| Employment (employed outside the home), n (%) | 87 (79.1) | 85 (77.3) |
| Comorbid health conditions, n (%)† | ||
| Diabetes | 4 (3.7) | 5 (4.6) |
| Hypertension | 9 (8.2) | 10 (9.1) |
| Anxiety | 25 (23.4) | 21 (19.3) |
| Depression | 24 (22.2) | 22 (20.2) |
| Upper back/neck pain | 26 (23.6) | 19 (17.3) |
| Current medication use for back pain, n (%)‡ | ||
| Nonsteroidal anti-inflammatory drug | 60 (54.5) | 65 (59.1) |
| Opioids | 26 (23.6) | 24 (21.8) |
| Muscle relaxers | 23 (20.9) | 28 (25.4) |
| Oral steroid | 10 (9.1) | 17 (15.4) |
| Gabapentin | 9 (8.2) | 7 (6.4) |
| Imaging procedures for current back pain episode, n (%)§ | ||
| Radiography | 42 (38.2) | 47 (42.7) |
| Advanced imaging (magnetic resonance imaging or computed tomography scan) | 19 (17.3) | 20 (18.2) |
| Current smoker, n (%) | 15 (13.6) | 9 (8.3) |
| Previous nonfusion back surgery, n (%) | 4 (3.7) | 6 (5.5) |
| Mean duration of current back pain symptoms (SD), d* | 35.9 (26.8) | 35.8 (25.6) |
| STarT Back Screening Tool category, n (%) | ||
| High | 28 (25.5) | 26 (23.6) |
| Medium | 63 (56.4) | 68 (61.8) |
| Low | 19 (17.3) | 16 (14.5) |
| Mean Oswestry Disability Index score (SD) | 35.8 (15.8) | 38.9 (13.8) |
| Mean Numeric Pain Rating Scale score (back pain intensity) (SD)‖ | 4.8 (1.9) | 5.1 (1.8) |
| Mean Numeric Pain Rating Scale score (leg pain intensity) (SD)*‖ | 3.8 (2.2) | 4.3 (2.2) |
| Mean Fear-Avoidance Beliefs Questionnaire score (SD) | ||
| Physical activity subscale* | 14.0 (5.9) | 15.2 (5.7) |
| Work subscale* | 13.9 (11.8) | 15.4 (12.3) |
| Mean Pain Catastrophizing Scale score (SD)* | 19.0 (11.9) | 20.9 (12.6) |
| Mean EQ-5D score (SD)¶ | ||
| Quality of life | 0.64 (0.2) | 0.64 (0.2) |
| Overall health self-rating* | 54.9 (20.3) | 57.7 (19.1) |
EPT = early physical therapy; EQ-5D = EuroQol 5-dimension; UC = usual care.
Missing baseline scores; sex (n = 1 EPT), age (n = 1 UC), duration of symptoms (n = 1 UC), Numeric Pain Rating Scale–leg pain intensity (n = 1 EPT), Pain Catastrophizing Scale (n = 3 EPT, n = 2 UC), Fear-Avoidance Beliefs Questionnaire physical activity subscale (n = 1 UC) and work subscale (n = 4 EPT, n = 1 UC), and EQ-5D overall health rating (n = 6 EPT, n = 3 UC).
Comorbid conditions based on participants’ self-report that they either have, or are receiving treatment for, the condition.
Medication use based on participants’ report that the medication has been prescribed to them and they are taking the medication either regularly or as needed for back pain. For nonsteroidal anti-inflammatory drugs, over-the-counter use is included.
Imaging use since the beginning of the current episode based on participants’ self-report.
Pain intensity assessed on a 0 to 10 numerical rating scale, with 0 indicating “no pain at all” and 10 “worst imaginable pain.”
The EQ-5D score is based on U.S. valuations ranging from 0.0 to 1.0, with higher scores indicating greater quality of life. The EQ-5D overall health self-rating ranges from 0 to 100, with higher numbers indicating greater self-rated overall health.
Overall, 213 participants (96.8%) completed the 4-week assessment, and 196 (89.5%) and 191 (86.8%) completed 6-month and 1-year assessments for the primary outcome, respectively. Twelve UC participants received nonpharmacologic care during the treatment period, including 5 participants who received physical therapy. Among participants randomly assigned to EPT, 100 (90.1%) began treatment, with a mean of 5.5 physical therapy sessions (SD, 2.4) attended. Of 552 physical therapy sessions, 96.4% included exercise, 67.6% included manual therapy, and 13.6% included traction. The most common off-protocol interventions were massage in 49 sessions (8.9%), dry needling in 8 sessions (1.4%), a heating pad in 3 sessions, and transcutaneous electrical nerve stimulation in 1 session. Three participants received a back brace or support. Thirty-seven patients receiving EPT (37.0%) reported a total of 133 side effects associated with treatment. Most common were increased back pain (n = 24) and stiffness (n = 19). Thirteen side effects were rated by the patient as severe with respect to intensity, and 7 of these effects persisted beyond 24 hours.
There was a statistically significant between-group difference for the primary outcome of mean change in OSW to 6 months, with greater improvement in the EPT group (relative difference, −5.4 points [95% CI, −9.4 to −1.3 points]; P = 0.009). Differences in OSW were also present at the assessments at 4 weeks (relative difference, −8.2 points [CI, −12.1 to −4.3 points]) and 1 year (relative difference, −4.8 points [CI, −8.9 to −0.7 points]) (Table 2). The groups also differed in back pain intensity after 4 weeks (relative difference, −1.4 points [CI, −2.0 to −0.9 points]), 6 months (relative difference, −0.7 points [CI, −1.3 to −0.2 points]), and 1 year (relative difference, −1.0 points [CI, −1.6 to −0.4 points]). Other secondary outcomes differed between groups favoring the EPT group (Table 2). Figure 2 shows the time course of the unadjusted scores for disability (OSW) and back and leg pain intensity.
Table 2.
Primary and Secondary Study Outcomes
| Outcome and Visit | UC Group (n = 110) | EPT Group (n = 110) | |||
|---|---|---|---|---|---|
| Unadjusted Mean (95% CI) | Mean Change From Baseline (95% CI) | Unadjusted Mean (95% CI) | Mean Change From Baseline (95% CI) | Relative Difference Between Groups* (95% CI) | |
| Oswestry Disability Index | |||||
| Baseline | 35.8 (32.8 to 38.7) | – | 38.9 (36.3 to 41.4) | – | – |
| 4 wk | 28.1 (25.4 to 30.8) | −8.8 (−11.5 to −6.0) | 19.9 (17.2 to 22.7) | −17.0 (−19.7 to −14.2) | −8.2 (−12.1 to −4.3) |
| 6 mo | 19.8 (17.0 to 22.7) | −17.0 (−19.9 to −14.2) | 14.5 (11.6 to 17.3) | −22.4 (−25.3 to −19.6) | −5.4 (−9.4 to −1.3) |
| 1 y | 19.2 (16.3 to 22.0) | −17.7 (−20.6 to −14.8) | 14.4 (11.5 to 17.4) | −22.5 (−25.4 to −19.5) | −4.8 (−8.9 to −0.7) |
| Numeric Pain Rating Scale (back pain) | |||||
| Baseline | 4.8 (4.4 to 5.1) | – | 5.1 (4.8 to 5.5) | – | – |
| 4 wk | 3.9 (3.5 to 4.3) | −1.0 (−1.4 to −0.6) | 2.4 (2 to 2.8) | −2.4 (−2.8 to −2.1) | −1.4 (−2.0 to −0.9) |
| 6 mo | 3.3 (2.9 to 3.7) | −1.5 (−1.9 to −1.1) | 2.6 (2.2 to 3) | −2.3 (−2.7 to −1.9) | −0.7 (−1.3 to −0.2) |
| 1 y | 3.3 (2.9 to 3.7) | −1.6 (−2 to −1.2) | 2.3 (1.9 to 2.7) | −2.6 (−3 to −2.2) | −1.0 (−1.6 to −0.4) |
| Numeric Pain Rating Scale (leg pain) | |||||
| Baseline | 3.8 (3.4 to 4.3) | – | 4.3 (3.9 to 4.7) | – | – |
| 4 wk | 3.0 (2.6 to 3.4) | −1.0 (−1.4 to −0.6) | 2.2 (1.7 to 2.6) | −1.8 (−2.3 to −1.4) | −0.8 (−1.4 to 0.2) |
| 6 mo | 2.1 (1.7 to 2.6) | −1.9 (−2.3 to −1.5) | 2.2 (1.8 to 2.7) | −1.8 (−2.2 to −1.3) | 0.1 (−0.5 to 0.8) |
| 1 y | 2.2 (1.8 to 2.7) | −1.8 (−2.2 to −1.3) | 1.8 (1.3 to 2.2) | −2.2 (−2.7 to −1.8) | −0.4 (−1.1 to 0.2) |
| Fear-Avoidance Beliefs Questionnaire (physical activity) | |||||
| Baseline | 14.0 (12.9 to 15.1) | – | 15.2 (14.1 to 16.2) | – | – |
| 4 wk | 11.3 (10.1 to 12.5) | −3.2 (−4.4 to −2) | 9.5 (8.3 to 10.7) | −4.9 (−6.1 to −3.7) | −1.8 (−3.5 to −0.1) |
| 6 mo | 9.6 (8.3 to 10.8) | −4.9 (−6.1 to −3.6) | 8.9 (7.6 to 10.1) | −5.6 (−6.9 to −4.3) | −0.7 (−2.5 to 1) |
| 1 y | 10.7 (9.5 to 12.0) | −3.7 (−5 to −2.5) | 7.1 (5.9 to 8.4) | −7.3 (−8.6 to −6) | −3.6 (−5.4 to −1.8) |
| Fear-Avoidance Beliefs Questionnaire (work) | |||||
| Baseline | 13.9 (11.7 to 16.1) | – | 15.4 (13.0 to 17.7) | – | – |
| 4 wk | 12.7 (11.0 to 14.4) | −1.4 (−3.1 to 0.2) | 11.1 (9.4 to 12.8) | −3.0 (−4.7 to −1.3) | −1.6 (−3.9 to 0.8) |
| 6 mo | 11 (9.2 to 12.7) | −3.2 (−4.9 to −1.4) | 9.1 (7.4 to 10.9) | −5.0 (−6.8 to −3.3) | −1.9 (−4.3 to 0.6) |
| 1 y | 11.5 (9.8 to 13.3) | −2.6 (−4.3 to −0.9) | 7.9 (6.1 to 9.7) | −6.2 (−8 to −4.4) | −3.6 (−6.1 to −1.1) |
| EQ-5D (quality of life)† | |||||
| Baseline | 0.64 (0.61 to 0.68) | – | 0.63 (0.6 to 0.67) | – | – |
| 4 wk | 0.7 (0.66 to 0.73) | 0.05 (0.02 to 0.08) | 0.76 (0.73 to 0.8) | 0.12 (0.08 to 0.15) | 0.07 (0.02 to 0.11) |
| 6 mo | 0.79 (0.75 to 0.82) | 0.14 (0.1 to 0.17) | 0.80 (0.77 to 0.84) | 0.15 (0.12 to 0.19) | 0.02 (−0.03 to 0.07) |
| 1 y | 0.78 (0.74 to 0.81) | 0.13 (0.1 to 0.17) | 0.82 (0.79 to 0.86) | 0.17 (0.14 to 0.21) | 0.04 (−0.01 to 0.09) |
| EQ-5D (self-rated health)† | |||||
| Baseline | 57.7 (54.0 to 61.3) | – | 54.9 (51.0 to 58.8) | – | – |
| 4 wk | 61.8 (58.5 to 65.2) | 5.2 (1.9 to 8.5) | 70.3 (67.0 to 73.7) | 13.7 (10.3 to 17.1) | 8.5 (3.8 to 13.3) |
| 6 mo | 68.3 (64.8 to 71.8) | 11.7 (8.2 to 15.2) | 68.8 (65.2 to 72.3) | 12.2 (8.6 to 15.7) | 0.5 (−4.5 to 5.5) |
| 1 y | 72.0 (68.4 to 75.6) | 15.4 (11.8 to 19) | 76 (72.4 to 79.7) | 19.4 (15.7 to 23.1) | 4.0 (−1.1 to 9.2) |
| Pain Catastrophizing Scale | |||||
| Baseline | 19.0 (16.8 to 21.3) | – | 20.9 (18.5 to 23.3) | – | – |
| 4 wk | 15.6 (13.7 to 17.4) | −3.7 (−5.5 to −1.9) | 13.7 (11.8 to 15.5) | −5.6 (−7.5 to −3.7) | −1.9 (−4.5 to 0.7) |
| 6 mo | 12.5 (10.6 to 14.4) | −6.7 (−8.7 to −4.8) | 11.2 (9.3 to 13.2) | −8.0 (−9.9 to −6.1) | −1.3 (−4.0 to 1.5) |
| 1 y | 11.4 (9.5 to 13.4) | −7.8 (−9.7 to −5.9) | 10.3 (8.2 to 12.3) | −9.0 (−11.0 to −7.0) | −1.2 (−4.0 to 1.6) |
EPT = early physical therapy; EQ-5D = EuroQol 5-dimension; UC = usual care.
Baseline means are raw means. Follow-up means are adjusted for baseline levels of the particular outcome. Analyses were done with unstructured covariance matrix. Differences between groups for each outcome control for the baseline level of the outcome. A positive difference favors EPT for the EQ-5D quality-of-life and self-rated health outcomes. A negative difference favors EPT for the Oswestry Disability Index, Numeric Pain Rating Scale for back and leg pain, fear avoidance, and pain catastrophizing outcomes.
The EQ-5D quality-of-life score is based on U.S. valuations ranging from 0.0 to 1.0, with higher scores indicating greater quality of life. The EQ-5D overall health self-rating ranges from 0 to 100, with higher numbers indicating greater self-rated overall health.
Figure 2.
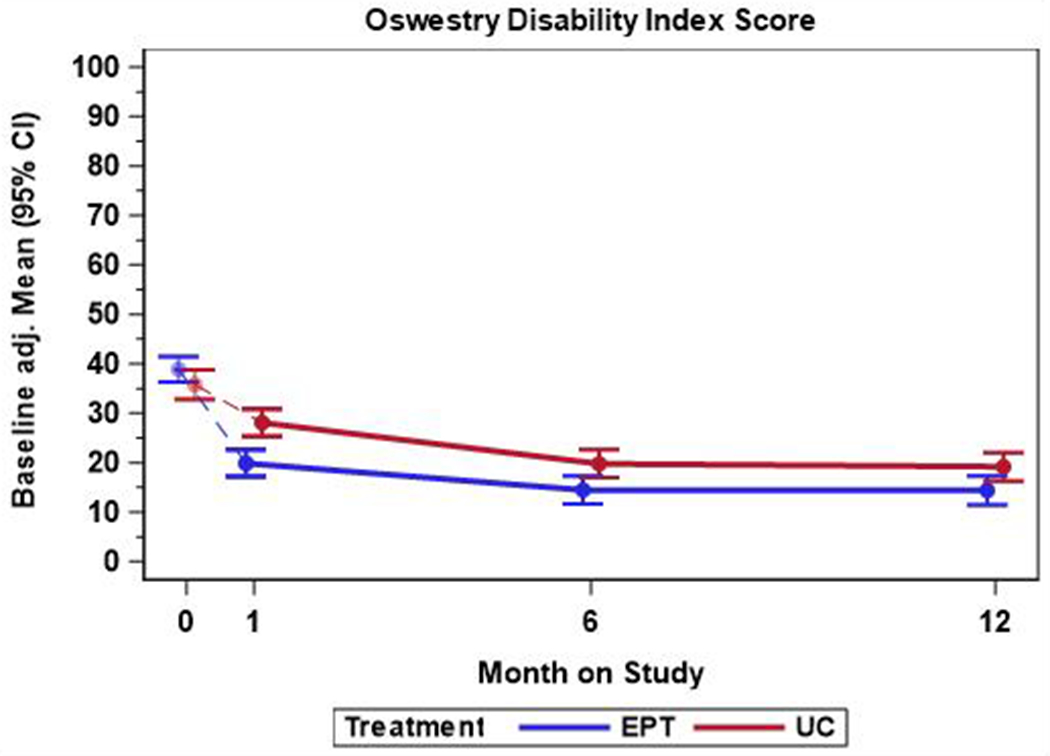
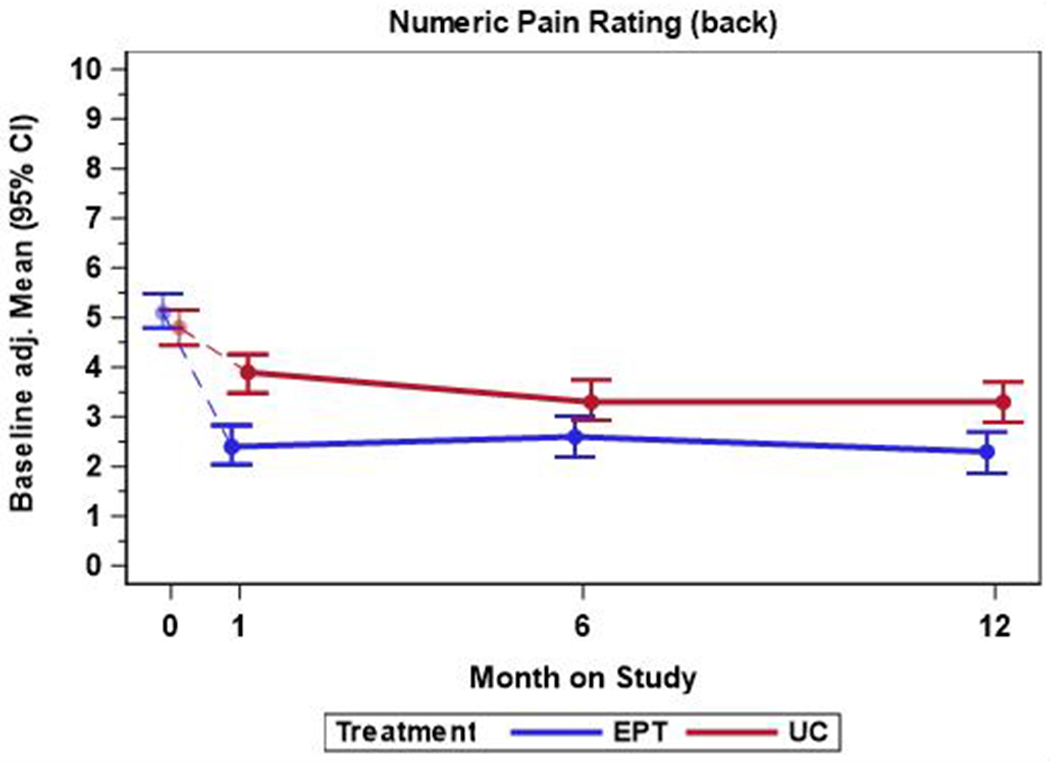
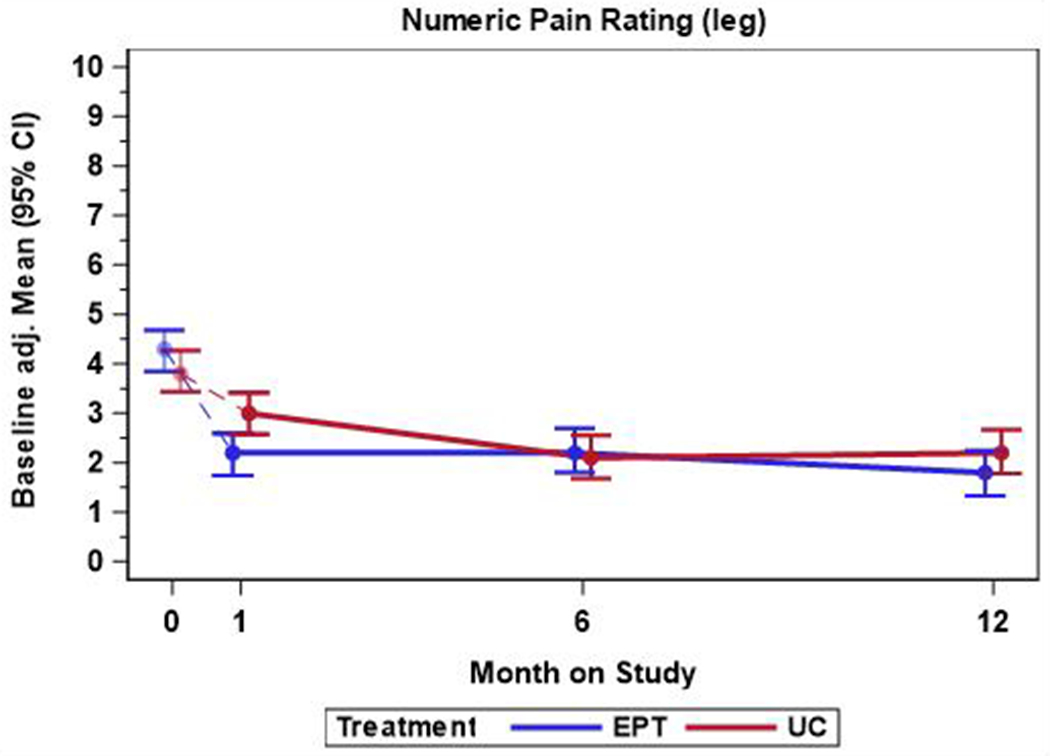
Time course of back pain–related disability, back pain intensity, and leg pain intensity, by treatment group. EPT = early physical therapy; UC = usual care. Top. The mean back pain–related disability scores were measured using the Oswestry Disability Index. Scores range from 0 to 100, with higher scores representing greater disability. Middle. Mean score for back pain intensity. Scores range from 0 to 10, with 0 indicating no pain and 10 indicating worst imaginable pain. Bottom. Mean score for leg pain intensity. Scores range from 0 to 10, with 0 indicating no pain and 10 indicating worst imaginable pain. Mean differences were calculated with linear mixed models. Error bars indicate 95% CIs. Raw means are provided at baseline.
Sensitivity analyses did not alter the significance of findings for any outcome at any time point. The as-treated sensitivity analysis included 10 participants randomly assigned to EPT who did not attend physical therapy with the UC group and 5 participants randomly assigned to UC who received physical therapy in the first 4 weeks with the EPT group. For the primary outcome of the OSW at 6 months, the as-treated analysis found a relative difference of −5.7 points (CI, −9.8 to −1.6 points). For the multiple imputation sensitivity analysis, the relative difference for the primary outcome was −4.6 points (CI, −0.7 to −8.4 points) (Supplement Tables 1 and 2, available at Annals.org).
Overall, 16 participants (7.4%) had surgery, 29 (13.2%) had injections, 55 (25%) had advanced imaging, and 21 (9.7%) had an emergency department visit for back pain or sciatica over the 1-year follow-up, with no differences between groups (Table 3). Sensitivity analyses for health care use outcomes using Cox regression analysis provided similar conclusions (Supplement Table 3, available at Annals.org). Differences in self-reported treatment success were seen between groups, and a higher proportion of participants in the EPT group self-reported success after 4 weeks (28.6% vs. 12.3%) and 1 year (45.2% vs. 27.6%). A total of 114 participants (52.5% of 217 reporting) missed at least 1 workday during the 1-year follow-up, with no difference between groups (Table 3). Among participants who missed work, the mean number of missed days per month was 0.7 days (CI, 0.5 to 1.1 days) in the EPT group and 1.2 days (CI, 0.8 to 2.0 days) in UC group (ratio of the means between EPT and UC, 0.6 [CI, 0.3 to 1.1]). Supplement Tables 4 and 5 (available at Annals.org) show further details on the analysis of missed workdays.
Table 3.
Dichotomized Secondary Outcomes
| Secondary Outcome | UC Group (n = 110) | EPT Group (n = 110) | Relative Risk* (95% CI) | ||
|---|---|---|---|---|---|
| Total Events, n | Patients, n (%) | Total Events, n | Patients, n (%) | ||
| Health care use outcome† | |||||
| Surgery (discectomy, decompression, fusion) | 7 | 7 (6.4) | 9 | 9 (8.3) | 1.3 (0.50–3.4) |
| Lumbar epidural injection | 20 | 14 (12.8) | 25 | 15 (13.9) | 1.1 (0.55–2.1) |
| Advanced imaging (magnetic resonance imaging or computed tomography scan) | 38 | 31 (28.2) | 30 | 24 (21.8) | 0.78 (0.49–1.2) |
| Emergency department visit | 11 | 11 (10.0) | 11 | 10 (9.1) | 0.92 (0.41–2.1) |
| Missed work | – | 60 (55.0) | – | 54 (50.0) | 0.91 (0.70–1.2) |
| Patient-reported success‡ | |||||
| 4 wk | – | 13 (12.3) | – | 30 (28.6) | 2.3 (1.3–4.2) |
| 6 mo | – | 27 (27.0) | – | 34 (35.4) | 1.3 (0.86–2.0) |
| 1 y | – | 27 (27.6) | – | 42 (45.2) | 1.6 (1.1–2.4) |
EPT = early physical therapy; UC = usual care.
Indicates the likelihood of occurrence of the outcome in the EPT group compared with the likelihood of its occurrence in the UC group. A value >1.0 indicates a greater likelihood of the outcome in the EPT group. A value <1.0 indicates a lower likelihood in the EPT group.
217 participants reported.
Patient-reported success was collected from a single-item rating of the amount of improvement since beginning the study with responses on a 15-level Likert scale. Responses were dichotomized to define success as occurring when a rating of “a great deal better” or “a very great deal better” was selected. A total of 211 patients reported at 4 wk, 196 at 6 mo, and 191 at 1 y.
Discussion
This randomized clinical trial found that referral to EPT from primary care was more effective in reducing disability than UC alone for LBP and sciatica of less than 90 days’ duration. The EPT group showed greater improvement in disability and back pain intensity across all follow-up times. Differences between groups were robust across sensitivity analyses. Several secondary outcomes also favored EPT. The groups did not differ in health care use or missed work during the 1-year follow-up. Patients receiving EPT were more likely to rate their treatment as successful at 4 weeks and 1 year.
Practice guidelines recommend an initial period of conservative care focused on nonpharmacologic treatments, including exercise and manual therapy, for persons with recent-onset sciatica, except in rare instances of rapidly progressing or severe neurologic deficits that may require immediate surgical intervention (7, 8, 15, 37). In practice, some primary care providers use a stepped-care approach with an initial period of advice, medication, and self-management, with referral to physical therapy restricted to patients with insufficient improvement (38). In this study, an EPT referral hastened functional improvement, indicating that EPT can be offered to patients as first-line nonpharmacologic care. The magnitude of effects favoring EPT on the primary outcome of disability measured by the OSW was within the minimum clinically important difference range of 6 to 8 points (28, 29) only at the 4-week assessment. At 6 months and 1 year, the magnitude of effects fell below this range (5.0 to 5.5 points of difference between groups).
Only 2 previous randomized clinical trials have examined the effectiveness of referral to physical therapy after a primary care visit as a strategy to provide recommended nonpharmacologic care (39, 40). Hofstee and colleagues (39) found no differences among physical therapy, bed rest, and advice to continue daily activities for LBP and sciatica of less than 1 month’s duration in outcomes of pain intensity or disability over a 6-month follow-up. A subsequent study compared UC from a general practitioner with or without physical therapy for LBP and sciatica of less than 6 weeks’ duration (40). After 1 year, patients randomly assigned to physical therapy were more likely to rate themselves as having improved, but no differences were seen in back pain intensity or disability (40). Our results may have been more favorable toward physical therapy because our exercise and manual therapy protocol focused on centralization of symptoms, which is advised in practice guidelines (8). The prior studies also enrolled patients with more acute conditions who may have been more prone to spontaneous recovery than our participants.
Our results were more favorable than those of past studies toward the benefits of physical therapy. Benefits of EPT in this study may be attributable to the focus on evidence-based interventions, specifically exercise and manual therapy, as core treatment components. The EPT protocol used a repeated directional exercise program to centralize symptoms (25). This type of exercise has been found to be beneficial for sciatica (41) and is commonly used by physical therapists (42, 43). Direct comparisons with other forms of exercise are lacking, and our study cannot address whether repeated directional exercise is superior to other exercise programs. We also included manual therapy as a core EPT component on the basis of limited research indicating that exercise and manual therapy combined may be more beneficial than exercise alone for sciatica (44). Manual therapy was also used with the intent to promote centralization.
We sought to examine a pragmatic physical therapy protocol with the potential for scalability if it was found to be effective. Physical therapists in this study had good adherence to the core components of exercise and, to a lesser extent, manual therapy in our protocol. The physical therapy protocol was safe. About one third of patients reported side effects of therapy, which were transient and mostly mild or moderate in nature. Our protocol was designed to provide 6 to 8 treatment sessions to avoid overuse; a mean of 5.5 sessions were actually provided to EPT participants. Further research is needed to examine the generalizability of the findings in this study.
This study has limitations. First, we did not balance provider time during the 4-week treatment period, and differential contact time may have contributed to differences between groups. Second, the EPT protocol was multimodal, and we could not isolate which components contributed to effectiveness. Third, the UC protocol standardized the provision of education, which may not reflect what is typically done in primary care practice. Fourth, it was not possible to blind participants or physical therapists to treatment assignment. Fifth, our participant sample was 83% White and 86% non-Hispanic, which limits generalizability. Finally, stratification-based decision making has been advocated to identify and target referral to a subgroup of patients most likely to benefit from EPT (40, 45–47). Our study did not address risk stratification. Further research should compare EPT as first-line treatment in stepped-care delivery versus stratification-based referral.
In conclusion, our results found that EPT referral after an initial primary care visit for recent-onset LBP and sciatica resulted in greater improvement in disability and secondary outcomes than UC across the 1-year follow-up. Health care use did not differ by treatment group assignment.
Supplementary Material
Acknowledgments
Primary Funding Source: Agency for Healthcare Research and Quality.
Grant Support: The research reported in this publication was supported by the Agency for Healthcare Research and Quality through grant R18HS022641. The study was supported by the University of Utah Study Design and Biostatistics Center, with funding in part through grant 5UL1TR001067-02 (formerly 8UL1TR000105 and UL1RR025764) from the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health.
Footnotes
Disclosures: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M20-4187.
Data Sharing Statement: The following data will be made available with publication: deidentified participant data and data dictionary (data sets available to approved persons through a written data sharing agreement with Dr. Fritz [julie.fritz@utah.edu]). The following supporting documents will be made available with publication: statistical/analytic code (access to these documents will be available on request sent to Dr. Fritz [julie.fritz@utah.edu]). These data will be made available to researchers whose proposed use of the data has been approved by the investigators, for any research purpose, after approval of a proposal (restrictions: none).
Supplement. Supplementary Material
Contributor Information
Julie M. Fritz, College of Health, University of Utah, Salt Lake City, Utah.
Elizabeth Lane, University of Utah, Salt Lake City, Utah.
Molly McFadden, School of Medicine, University of Utah, Salt Lake City, Utah.
Gerard Brennan, Rehabilitation Services, Intermountain Healthcare, Salt Lake City, Utah.
John S. Magel, University of Utah, Salt Lake City, Utah.
Anne Thackeray, University of Utah, Salt Lake City, Utah.
Kate Minick, Intermountain Healthcare, Salt Lake City, Utah.
Whitney Meier, University of Utah Health, Salt Lake City, Utah.
Tom Greene, School of Medicine, University of Utah, Salt Lake City, Utah.
References
- 1.Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996-2016. JAMA. 2020;323:863–884. doi: 10.1001/jama.2020.0734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finley CR, Chan DS, Garrison S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician. 2018;64:832–840. [PMC free article] [PubMed] [Google Scholar]
- 3.Porchet F, Wietlisbach V, Burnand B, et al. Relationship between severity of lumbar disc disease and disability scores in sciatica patients. Neurosurgery. 2002;50:1253–9; discussion 1259-60. [DOI] [PubMed] [Google Scholar]
- 4.Schoenfeld AJ, Laughlin M, Bader JO, et al. Characterization of the incidence and risk factors for the development of lumbar radiculopathy. J Spinal Disord Tech. 2012;25:163–7. doi: 10.1097/BSD.0b013e3182146e55 [DOI] [PubMed] [Google Scholar]
- 5.Stafford MA, Peng P, Hill DA. Sciatica: a review of history, epidemiology, pathogenesis, and the role of epidural steroid injection in management. Br J Anaesth. 2007;99:461–73. [DOI] [PubMed] [Google Scholar]
- 6.Weber H, Holme I, Amlie E. The natural course of acute sciatica with nerve root symptoms in a double-blind placebo-controlled trial evaluating the effect of piroxicam. Spine (Phila Pa 1976). 1993;18:1433–8. [PubMed] [Google Scholar]
- 7.Chou R, Deyo R, Friedly J, et al. Nonpharmacologic therapies for low back pain. A systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med. 2017;166:493–505. doi: 10.7326/M16-2459 [DOI] [PubMed] [Google Scholar]
- 8.Stochkendahl MJ, Kjaer P, Hartvigsen J, et al. National clinical guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur Spine J. 2018;27:60–75. doi: 10.1007/s00586-017-5099-2 [DOI] [PubMed] [Google Scholar]
- 9.Mehling WE, Gopisetty V, Bartmess E, et al. The prognosis of acute low back pain in primary care in the United States: a 2-year prospective cohort study. Spine (Phila Pa 1976). 2012;37:678–84. doi: 10.1097/BRS.0b013e318230ab20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vroomen PC, de Krom MC, Knottnerus JA. Predicting the outcome of sciatica at short-term follow-up. Br J Gen Pract. 2002;52:119–23. [PMC free article] [PubMed] [Google Scholar]
- 11.Hartvigsen L, Hestbaek L, Lebouef-Yde C, et al. Leg pain location and neurological signs relate to outcomes in primary care patients with low back pain. BMC Musculoskelet Disord. 2017;18:133. doi: 10.1186/s12891-017-1495-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hider SL, Whitehurst DG, Thomas E, et al. Pain location matters: the impact of leg pain on health care use, work disability and quality of life in patients with low back pain. Eur Spine J. 2015;24:444–51. doi: 10.1007/s00586-014-3355-2 [DOI] [PubMed] [Google Scholar]
- 13.Kongsted A, Kent P, Jensen TS, et al. Prognostic implications of the Quebec Task Force classification of back-related leg pain: an analysis of longitudinal routine clinical data. BMC Musculoskelet Disord. 2013;14:171. doi: 10.1186/1471-2474-14-171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Konstantinou K, Dunn KM, Ogollah R, et al. ATLAS Study Team. Prognosis of sciatica and back-related leg pain in primary care: the ATLAS cohort. Spine J. 2018;18:1030–1040. doi: 10.1016/j.spinee.2017.10.071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernstein IA, Malik Q, Carville S, et al. Low back pain and sciatica: summary of NICE guidance. BMJ. 2017;356:i6748. doi: 10.1136/bmj.i6748 [DOI] [PubMed] [Google Scholar]
- 16.Qaseem A, Wilt TJ, McLean RM, et al. Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166:514–530. doi: 10.7326/M16-2367 [DOI] [PubMed] [Google Scholar]
- 17.Traeger A, Buchbinder R, Harris I, et al. Diagnosis and management of low-back pain in primary care. CMAJ. 2017;189:E1386–E1395. doi: 10.1503/cmaj.170527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pinto RZ, Verwoerd AJH, Koes BW. Which pain medications are effective for sciatica (radicular leg pain)? BMJ. 2017;359:j4248. doi: 10.1136/bmj.j4248 [DOI] [PubMed] [Google Scholar]
- 19.Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J. 2018;27:2791–2803. doi: 10.1007/s00586-018-5673-2 [DOI] [PubMed] [Google Scholar]
- 20.Pangarkar SS, Kang DG, Sandbrink F, et al. VA/DoD clinical practice guideline: diagnosis and treatment of low back pain. J Gen Intern Med. 2019;34:2620–2629. doi: 10.1007/s11606-019-05086-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boutron I, Altman DG, Moher D, et al. CONSORT NPT Group. CONSORT statement for randomized trials of nonpharmacologic treatments: a 2017 update and a CONSORT extension for nonpharmacologic trial abstracts. Ann Intern Med. 2017;167:40–47. doi: 10.7326/M17-0046 [DOI] [PubMed] [Google Scholar]
- 22.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roland M, Waddell G, Klaber-Moffet J, et al. The Back Book. The Stationary Office; 1996. [Google Scholar]
- 24.Burton AK, Waddell G, Tillotson KM, et al. Information and advice to patients with back pain can have a positive effect: a randomized controlled trial of a novel educational booklet in primary care. Spine (Phila Pa 1976). 1999;24:2484–91. [DOI] [PubMed] [Google Scholar]
- 25.McKenzie RA, May S. The Lumbar Spine: Mechanical Diagnosis & Therapy. 2nd ed Orthopedic Physical Therapy Products; 2003. [Google Scholar]
- 26.Browder DA, Childs JD, Cleland JA, et al. Effectiveness of an extension-oriented treatment approach in a subgroup of subjects with low back pain: a randomized clinical trial. Phys Ther. 2007;87:1608–18; discussion 1577-9. [DOI] [PubMed] [Google Scholar]
- 27.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25:2940–52; discussion 2952. [DOI] [PubMed] [Google Scholar]
- 28.Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81:776–88. [DOI] [PubMed] [Google Scholar]
- 29.Lauridsen HH, Hartvigsen J, Manniche C, et al. Responsiveness and minimal clinically important difference for pain and disability instruments in low back pain patients. BMC Musculoskelet Disord. 2006;7:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7:524–32. doi: 10.1037/1040-3590.7.4.524 [DOI] [Google Scholar]
- 31.Waddell G, Newton M, Henderson I, et al. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–68. [DOI] [PubMed] [Google Scholar]
- 32.Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care. 2005;43:203–20. [DOI] [PubMed] [Google Scholar]
- 33.Hill JC, Dunn KM, Lewis M, et al. A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum. 2008;59:632–41. doi: 10.1002/art.23563 [DOI] [PubMed] [Google Scholar]
- 34.Hurwitz EL, Morgenstern H, Vassilaki M, et al. Frequency and clinical predictors of adverse reactions to chiropractic care in the UCLA Neck Pain Study. Spine (Phila Pa 1976). 2005;30:1477–84. [DOI] [PubMed] [Google Scholar]
- 35.Jaeschke R, Singer J, Guyatt GH. Measurement of health status: ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–15. [DOI] [PubMed] [Google Scholar]
- 36.Therneau TM, Grambsch PM. Multiple events per subject In: Therneau TM, Grambsch PM, eds. Modeling Survival Data: Extending the Cox Model. Springer; 2000:169–230. [Google Scholar]
- 37.Foster NE, Anema JR, Cherkin D, et al. Lancet Low Back Pain Series Working Group. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391:2368–2383. doi: 10.1016/S0140-6736(18)30489-6 [DOI] [PubMed] [Google Scholar]
- 38.Jensen RK, Kongsted A, Kjaer P, et al. Diagnosis and treatment of sciatica. BMJ. 2019;367:l6273. doi: 10.1136/bmj.16273 [DOI] [PubMed] [Google Scholar]
- 39.Hofstee DJ, Gijtenbeek JM, Hoogland PH, et al. Westeinde Sciatica Trial: randomized controlled study of bed rest and physiotherapy for acute sciatica. J Neurosurg. 2002;96:45–9. [DOI] [PubMed] [Google Scholar]
- 40.Luijsterburg PA, Verhagen AP, Ostelo RW, et al. Physical therapy plus general practitioners’ care versus general practitioners’ care alone for sciatica: a randomised clinical trial with a 12-month follow-up. Eur Spine J. 2008;17:509–17. doi: 10.1007/s00586-007-0569-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Albert HB, Manniche C. The efficacy of systematic active conservative treatment for patients with severe sciatica: a single-blind, randomized, clinical, controlled trial. Spine (Phila Pa 1976). 2012;37:531–42. doi: 10.1097/BRS.0b013e31821ace7f [DOI] [PubMed] [Google Scholar]
- 42.Delitto A, George SZ, Van Dillen L, et al. Orthopaedic Section of the American Physical Therapy Association. Low back pain. J Orthop Sports Phys Ther. 2012;42:A1–57. doi: 10.2519/jospt.2012.42.4.A1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ladeira CE, Cheng MS, da Silva RA. Clinical specialization and adherence to evidence-based practice guidelines for low back pain management: a survey of US physical therapists. J Orthop Sports Phys Ther. 2017;47:347–358. doi: 10.2519/jospt.2017.6561 [DOI] [PubMed] [Google Scholar]
- 44.Bronfort G, Hondras MA, Schulz CA, et al. Spinal manipulation and home exercise with advice for subacute and chronic back-related leg pain: a trial with adaptive allocation. Ann Intern Med. 2014;161:381–91. doi: 10.7326/M14-0006 [DOI] [PubMed] [Google Scholar]
- 45.Konstantinou K, Dunn KM, van der Windt D, et al. SCOPiC Study Team. Subgrouping patients with sciatica in primary care for matched care pathways: development of a subgrouping algorithm. BMC Musculoskelet Disord. 2019;20:313. doi: 10.1186/s12891-019-2686-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Verwoerd AJ, Luijsterburg PA, Koes BW, et al. Does kinesiophobia modify the effects of physical therapy on outcomes in patients with sciatica in primary care? Subgroup analysis from a randomized controlled trial. Phys Ther. 2015;95:1217–23. doi: 10.2522/ptj.20140458 [DOI] [PubMed] [Google Scholar]
- 47.Linton SJ, Nicholas M, Shaw W. Why wait to address high-risk cases of acute low back pain? A comparison of stepped, stratified, and matched care. Pain. 2018;159:2437–2441. doi: 10.1097/j.pain.0000000000001308 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


