Abstract
Background:
Social determinants of health (SDH) are individually associated with incident coronary heart disease (CHD) events. Indices reflecting social deprivation have been developed for population management, but are difficult to operationalize during clinical care. We examined whether a simple count of SDH is associated with fatal incident CHD and nonfatal myocardial infarction (MI).
Methods:
We used data from the prospective longitudinal REasons for Geographic And Racial Differences in Stroke cohort study, a national population-based sample of community-dwelling Black and white adults age ≥45 years recruited from 2003–7. Seven SDH from the five Healthy People 2020 domains included social context (Black race, social isolation); education (educational attainment); economic stability (annual household income); neighborhood (living in a zip code with high poverty); and healthcare (lacking health insurance, living in one of the 9 US states with the least public health infrastructure). Outcomes were expert adjudicated fatal incident CHD and nonfatal MI.
Results:
Of 22,152 participants free of CHD at baseline, 58.8% were women, 42.0% were Blacks, 20.6% had no SDH, 30.6% had 1, 23.0% had 2, and 25.8% had ≥3. There were 463 fatal incident CHD events and 932 nonfatal MIs over median 10.7 years [IQR 6.6–12.7]. Fewer SDH were associated with nonfatal MI than with fatal incident CHD. The age-adjusted incidence per 1000 person-years increased with the number of SDH for both fatal incident CHD (0 SDH 1.30, 1 SDH 1.44, 2 SDH 2.05, ≥3 SDH 2.86) and nonfatal MI (0 SDH 3.91, 1 SDH 4.33, ≥2 SDH 5.44). Compared to those without SDH, crude and fully adjusted hazard ratios (HR) for fatal incident CHD among those with ≥3 SDH were 3.00 (95% CI 2.17, 4.15) and 1.67 (95% CI 1.18, 2.37), respectively; and that for nonfatal MI among those with ≥2 SDH were 1.57 (95% CI 1.30, 1.90) and 1.14 (0.93, 1.41), respectively.
Conclusions:
A greater burden of SDH was associated with a graded increase in risk of incident CHD, with greater magnitude and independent associations for fatal incident CHD. Counting the number of SDH may be a promising approach that could be incorporated into clinical care to identify individuals at high risk of CHD.
Keywords: Social determinants of health, incident coronary disease, disparities, risk factors
Introduction
Disparities in coronary heart disease (CHD) persist in the modern era, and social determinants of health (SDH) are increasingly a focus of efforts to eliminate these disparities.1 SDH like low educational attainment, low income, social isolation, racism, suboptimal built environments, and barriers to accessing high quality healthcare have each been associated with worse CHD outcomes.2–7 The contribution of SDH to health outcomes may outweigh that of biological influences or medical care, yet they are not uniformly operationalized as distinct risk markers in clinical care settings.8
Previous studies have documented the independent influence of various SDH, and indices of social deprivation have been developed.9 However, indices often include characteristics of small geographic areas and may be difficult for clinicians to construct and interpret for their patients during a clinical encounter. A simple count of an individual’s burden of SDH may be more easily calculated, but the association between the number of SDH and health outcomes has not been well studied.10 We recently demonstrated that among individuals with guideline concordant indications for statins, only 45% of those with ≥4 SDH received statins compared with 65% of those without SDH, even after adjusting for numerous factors known to influence health services utilization.11 We recently reported a graded increase in risk of incident stroke and heart failure with increasing burden of SDH.12,13 A gap in our understanding is whether an individual’s burden of SDH is also associated with incident fatal or nonfatal CHD. Although fatal CHD has declined along with the overall incidence of CHD in the modern era, the proportion of incident events that are fatal varies from 40–44% among Blacks to only 23–29% among whites, supporting separate study of fatal and nonfatal events.14–20 Simple clinical tools to identify individuals at high risk of CHD events using SDH would be helpful to let physicians target patients for more aggressive risk factor management, complementing health system efforts to address SDH.
With its rich self-reported and rigorously assessed physiologic data as well as expert-adjudicated CHD endpoints, the large prospective biracial Reasons for Geographic And Racial Differences in Stroke (REGARDS) cohort is well suited for a study to fill this gap in the literature. This national biracial cohort offers an opportunity to examine the association between the number of SDH and fatal incident CHD and nonfatal MI in a national sample. We examined these endpoints separately because we have previously shown differences in patterns between fatal incident CHD and incident nonfatal myocardial infarction (MI).1 The overall objectives of this study were to determine the associations of the number of SDH and fatal incident CHD and, separately, incident nonfatal MI. We hypothesized that as the number of SDH increase, the risk of fatal incident CHD and nonfatal MI also increase.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study population
The REGARDS study was designed to elucidate reasons for regional and racial differences in stroke mortality; CHD outcomes are being investigated through an ancillary study. Details are provided elsewhere;21 briefly, between 2003 and 2007, community-dwelling Black and white adults age ≥45 years living in the 48 contiguous US states were enrolled. Sampling aimed to balance on race and sex, with oversampling of the Stroke Buckle (coastal North and South Carolina and Georgia) and the Stroke Belt (the remainder of North and South Carolina and Georgia, and Alabama, Mississippi, Louisiana, Arkansas, and Tennessee), regions with the highest stroke mortality in the US. Participants were recruited using commercially available lists and underwent 45-minute computer assisted telephone interviews (CATI) about medical history, health behaviors, and risk factors followed by in-home visits at which physiologic parameters (height, weight, blood pressure) and electrocardiography were assessed. Blood and urine samples were collected and shipped to the study’s central laboratory at the University of Vermont. Medications taken in the two weeks prior to the study visit were recorded through pill bottle review, and a food frequency questionnaire was left for self-administration. Participants were contacted every 6 months by telephone to detect potential study endpoints.
For this study, we selected participants free of vascular disease at baseline, defined as self-reported stroke, MI, coronary bypass, coronary angioplasty, vascular surgery, or MI on the baseline ECG. Institutional review boards of participating institutions approved the study, and all participants provided written informed consent.
Outcomes: fatal incident CHD and incident nonfatal MI
The first outcome in this study was fatal incident CHD, defined as death within 28 days of an adjudicated definite or probable MI, or CHD or sudden death as the adjudicated cause of death. Heart-related hospitalizations or deaths detected during follow-up triggered medical record retrieval and adjudication of study endpoints by clinician experts using national guidelines.22–24 Main underlying cause of death was determined by two trained adjudicators who examined all available information including interviews with next of kin, death certificates, autopsy reports, medical history, and the National Death Index.
The second outcome was nonfatal MI. MI adjudicators examined medical records. MIs required a clinical presentation consistent with ischemia; a rising and/or falling pattern of troponin over at least 6 hours with a peak at least twice the upper limit of normal; or imaging findings consistent with ischemia. Disagreements were resolved by committee and the κ for agreement was >0.80.1 Events through December 31, 2017 were available for this study.
Primary exposure: SDH
The Healthy People 2020 framework of SDH guided the selection of SDH.25 This framework includes five domains of SDH: 1) economic stability; 2) education; 3) social/community context; 4) neighborhood/built environment; and 5) health and healthcare. The economic stability domain included annual household income <$35,000. The education domain included <high school educational attainment. The social/community context domain included Black race and social isolation (reporting not seeing close friends or family members at least once a month; having no one to care for you should you become ill or disabled). The neighborhood/built environment domain included residing in a zip code with >25% of residents living below the Federal poverty line, and by rural residence (rural urban commuting area [RUCA] codes 9 and 10). The health and healthcare domain included residence in a Health Professional Shortage Area (HPSA), lacking health insurance, and living in a US state with low public health infrastructure as derived from America’s Health Rankings (see Supplemental Materials text and Tables I andII).26
SDH with age and gender adjusted associations with fatal incident CHD and, separately, with incident nonfatal MI, with p<0.10 were retained for analysis (see correlations in Supplemental Figure I). The total number of a person’s SDH was reflected in a count variable.
Covariates
Sociodemographics included age at baseline and gender. Medical conditions included hypertension (self-report, use of antihypertensive medication, or systolic/diastolic blood pressure ≥140/90 mm Hg at the in-home visit), hyperlipidemia (self-reported diagnosis of “high cholesterol” by a health professional or low-density lipoprotein cholesterol [LDL] ≥130 mg/dL), and diabetes (use of diabetes medications, fasting blood glucose ≥126 mg/dL, or non-fasting glucose ≥200 mg/dL). Additional medications included statins and insulin. Physical and mental health were assessed using the Physical Component Summary (PCS) and Mental Component Summary (MCS) scores, respectively, from the Short Form-12.27 Health behaviors included cigarette smoking, gender-specific alcohol use (based on sex-specific National Institute of Alcohol Abuse and Alcoholism cut points, i.e., ≥7 drinks weekly for women and ≥14 drinks for weekly for men), physical activity (enough activity to work up a sweat on most days of the week), and adherence to a Mediterranean diet using the Mediterranean diet score (highest quartile of adherence vs. others).28–30 Physiologic variables included body mass index (BMI), systolic blood pressure, diastolic blood pressure, total cholesterol, high density lipoprotein (HDL) cholesterol, high sensitivity c-reactive protein (hsCRP, dichotomized as >3 mg/l), urinary albumin-to-creatinine ratio (ACR, dichotomized as >30 mg/g), and estimated glomerular filtration rate (eGFR) using the CKD-Epi equation.31
Statistical analysis
We first calculated the distribution of each SDH and examined collinearity using variance inflation factors (VIF). Using the retained SDH as described above, we described sample characteristics by number of SDH. Next, we estimated hazard ratios (HR) and 95% confidence intervals (CI) in Cox models, examining associations of the count of each retained SDH with fatal incident CHD and incident nonfatal MI, separately. We then adjusted each model for the covariates as defined above to determine independent associations of the count of SDH in fully adjusted models, separately.
Using Poisson models, we separately calculated age-adjusted incidence of fatal CHD and nonfatal MI by SDH count per 1,000 person-years using Kaplan-Meier curves.
We tested the assumption of proportionality of all Cox models using Martingale residuals for individual variables and global Χ2 tests. We used multiple imputation by chained equations to minimize bias attributed to missing data. Statistical significance was set at p<0.05 except for SDH selection, where we used p<0.10. All analyses were conducted in SAS version 9.4 and R version 3.4.1.
Results
The study sample included 22,152 individuals free of vascular disease at baseline (see Supplemental Figure II for exclusion cascade). Over a median follow-up of 10.7 years [IQR 6.6–12.7], 411 fatal CHD events and 828 nonfatal MIs occurred.
Selection of SDH
The minimally adjusted associations between each of the candidate SDH and fatal incident CHD and incident nonfatal MI are shown in Table 1. Black race, low education, low income, living in a zip code with high poverty, residence in the US states with least public health infrastructure, not seeing close friends/family in the past month, and lack of health insurance were associated with fatal incident CHD at p<0.10; these seven SDH were retained for further analyses of fatal incident CHD. Low education, low income, and lack of health insurance were associated with nonfatal MI (p<0.10); these three SDH were retained for further analyses of nonfatal MI. The sample distribution of count of SDH is shown in Supplemental Figures IIIa and IIIb.
Table 1.
Age and Gender Adjusted Associations of Social Determinants of Health with Fatal Incident Coronary Heart Disease and Incident Nonfatal Myocardial Infarction
| Healthy People 2020 Domain | Social Determinants of Health | Incident Fatal CHD | Incident Nonfatal MI | ||
|---|---|---|---|---|---|
| HR (95% CI) |
p | HR (95% CI) |
p | ||
| Social and community context | Black race |
1.65
(1.37, 1.98) |
<0.001 | 0.95 (0.83, 1.09) |
0.463 |
| Social isolation (Saw no friends/family in the past month) |
1.38
(0.95, 2.01) |
0.093 | 1.09 (0.81, 1.46) |
0.587 | |
| Social isolation (Do not have anyone to care for you if you become ill or disabled) | 0.94 (0.71, 1.25) |
0.674 | 1.00 (0.82, 1.22) |
0.982 | |
| Education | Low education (< High school) |
2.10
(1.67, 2.63) |
<0.001 |
1.43
(1.19, 1.73) |
0.0002 |
| Economic stability | Low annual household income (<$35,000) |
1.91
(1.55, 2.36) |
<0.001 |
1.32
(1.15, 1.53) |
0.0001 |
| Neighborhood/ built environment | Zip code with high poverty (>25% residents living below Federal poverty line) |
1.34
(1.08, 1.66) |
0.009 | 1.00 (0.84, 1.18) |
0.971 |
| Health and healthcare | Residence in a Health Professional Shortage Area | 1.08 (0.90, 1.30) |
0.405 | 0.93 (0.81, 1.06) |
0.206 |
| Residence in a State with least public health infrastructure* |
1.21
(1.00, 1.55) |
0.005 | 1.06 (0.93, 1.21) |
0.398 | |
| Lack of health insurance |
1.41
(0.94, 2.13) |
0.100 |
1.35
(1.04, 1.76) |
0.026 | |
Public Health Infrastructure is calculated based on America’s Health Ranking data; see text.
Bolded SDOH had associations with p<0.10.
Baseline characteristics of participants
Characteristics of participants by 0, 1, 2, and ≥3 SDH for fatal incident CHD are shown in Table 2; those for 0, 1, and ≥2 SDH for incident nonfatal MI are shown in Supplemental Table III. There were 4016 individuals without SDH, 5944 with 1, 4468 with 2, and 5030 with ≥3 SDH. Participants with a greater number of SDH were more likely to be women, be Black, have hypertension or diabetes, and have lower mental and physical functioning. Participants with greater numbers of SDH also were more likely to smoke cigarettes, less likely to exercise, and less likely to adhere to a Mediterranean diet. Those with greater numbers of SDH also had higher BMI, blood pressure, HDL cholesterol, eGFR, CRP>3 mg/L, and ACR>30 mg/g. The highest rates of missing data stemmed from participants declining to share their income (12.2%) and dietary data (27.8%) (Supplemental Table III).
Table 2.
Participant Characteristics by Number of Social Determinants of Health and Fatal Incident Coronary Heart Disease
| Number of Social Determinants of Health | |||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 or more | p-value | |
| N | 4,016 | 5,944 | 4,468 | 5,030 | |
| Social Determinants | |||||
| Black, N (%) | 0 | 1825 (30.7%) | 2399 (53.7%) | 4252 (84.5%) | <0.001 |
| <High school education, N (%) | 0 | 69 (1.2%) |
328 (7.3%) |
1776 (35.3%) | <0.001 |
| <$35,000 income, N (%) | 0 | 1676 (28.2%) | 2837 (63.5%) | 4135 (82.2%) | <0.001 |
| >25% residents living below Federal poverty line, N (%) | 0 | 204 (3.4%) |
863 (19.3%) |
2891 (57.5%) | <0.001 |
|
Residence in a state with least public health infrastructure, N (%)* |
0 | 1932 (32.5%) | 1939 (43.4%) | 3016 (60%) | <0.001 |
| No health insurance, N (%) | 0 | 70 (1.2%) |
283 (6.3%) |
1144 (22.7%) | <0.001 |
| Saw no friends/family in the past month, N (%) | 0 | 168 (2.8%) |
287 (6.4%) |
468 (9.3%) |
<0.001 |
|
Sociodemographics | |||||
| Age, mean (±SD) | 61.9 (±8.7) | 63.5 (±9.1) | 64.3 (±9.3) | 64.4 (±9.6) | <0.001 |
| Female, N (%) | 1892 (47.1%) | 3269 (55.0%) | 2777 (62.2%) | 3297 (65.5%) | <0.001 |
| Stroke Belt or Stroke Buckle, N (%)† | 1569 (39.1%) | 3243 (54.6%) | 2665 (59.6%) | 3305 (65.7%) | <0.001 |
|
Medical Conditions | |||||
| Hypertension, N (%) | 1787 (44.5%) | 3337 (56.1%) | 2800 (62.7%) | 3652 (72.6%) | <0.001 |
| Hyperlipidemia, N (%) | 2452 (61.1%) | 3642 (61.3%) | 2764 (61.9%) | 3062 (60.9%) | 0.67 |
| Diabetes, N (%) | 369 (9.2%) |
885 (14.9%) |
916 (20.5%) |
1394 (27.7%) | <0.001 |
|
Medications | |||||
| Antihypertensives, N (%) | 1579 (39.3%) | 2968 (49.9%) | 2551 (57.1%) | 3205 (63.7%) | <0.001 |
| Statins, N (%) | 1029 (25.6%) | 1500 (25.2%) | 1076 (24.1%) | 1145 (22.8%) | 0.005 |
| Insulin, N (%) | 58 (1.4%) |
169 (2.8%) |
191 (4.3%) |
376 (7.5%) |
<0.001 |
|
Health Status | |||||
| Physical functioning, median [IQR]‡ | 53.2 [47.9, 55.9] |
52.0 [44.8, 55.5] |
50.3 [41.4, 54.8] |
47.7 [37.8, 53.6] |
<0.001 |
| Mental functioning, median [IQR] § | 57.0 [53.7, 58.8] |
57.0 [53.0, 59.3] |
56.8 [51.7, 59.5] |
55.9 [48.7, 59.3] |
<0.001 |
|
Health Behaviors | |||||
| Current cigarette smoking, N (%) | 372 (9.3%) |
689 (11.6%) |
687 (15.4%) |
1010 (20.1%) | <0.001 |
| Risky alcohol consumption, N (%) | 253 (6.3%) |
262 (4.4%) |
155 (3.5%) |
136 (2.7%) |
<0.001 |
| Physical activity,|| N (%) | 2899 (72.2%) | 4123 (69.4%) | 2884 (64.5%) | 3083 (61.3%) | <0.001 |
| High adherence to Mediterranean diet, N (%) | 922 (23.0%) |
1383 (23.3%) | 787 (17.6%) |
634 (12.6%) |
<0.001 |
|
Physiological Factors | |||||
| Body mass index, mean kg/m2 (±SD) | 28.1 (±5.3) |
29.0 (±5.9) |
29.7 (±6.4) |
30.8 (±7.0) |
<0.001 |
| Systolic blood pressure, mean mm Hg (±SD) | 122.9 (±14.6) | 125.8 (±15.8) | 127.5 (±16.2) | 130.6 (±17.4) | <0.001 |
| Diastolic blood pressure, mean mm Hg (±SD) | 75.6 (±8.9) |
76.4 (±9.4) |
76.8 (±9.4) |
78.4 (±10.3) |
<0.001 |
| Total cholesterol, mean mg/dL (±SD) | 194.9 (±36.5) | 195.2 (±38.0) | 196.1 (±39.4) | 195.5 (±41.7) | 0.55 |
| High density lipoprotein cholesterol, median mg/dL [IQR] | 49.0 [40.0, 62.0] |
50.0 [41.0, 62.0] |
50.0 [41.0, 62.0] |
51.0 [42.0, 62.0] |
0.011 |
| C-reactive protein >3 mg/L, N (%) | 1114 (27.7%) | 2073 (34.9%) | 1826 (40.9%) | 2311 (45.9%) | <0.001 |
| Urinary albumin/creatinine ratio >30 mg/g, N (%) | 318 (7.9%) |
571 (9.6%) |
576 (12.9%) |
877 (17.4%) |
<0.001 |
| Estimated GFR, median [IQR] | 89.1 [77.8, 96.8] |
88.8 [76.0, 98.6] |
89.7 [74.8, 101.3] |
92.5 [75.9, 106.1] |
<0.001 |
Public health infrastructure based on America’s Health Rankings; see also Supplemental Materials.
REGARDS study oversampled residents from the Stroke Belt (Alabama, Arkansas, Louisiana, Mississippi, Tennessee, and the noncoastal regions in North Carolina, South Carolina, and Georgia) and the Stroke Buckle (coastal North and South Carolina, and coastal Georgia).
Range 0 to 100 with higher scores indicating better physical functioning.
Range 0 to 100 with higher scores indicating better mental functioning.
Getting enough physical activity to work up a sweat on most days of the week.
Note. p-values from ANOVA for continuous variables that are normally distributed, Wilcoxon rank-sum (2 groups) or Kruskal-Wallis (>2 groups) for continuous variables that are skewed, and Pearson’s Χ2 or Fisher’s exact test for binary and categorical variables.
Fatal incident CHD by count of SDH
Fatal incident CHD per 1000 person-years increased with each additional SDH, with incidence over twice as high for those with ≥3 SDH (2.86/1000 person-years) compared with those without SDH (1.30/1000 person-years) (Figure 1a). Participants with greater counts of SDH also had progressively lower survival probability (Figure 2a, p<0.001).
Figure 1.
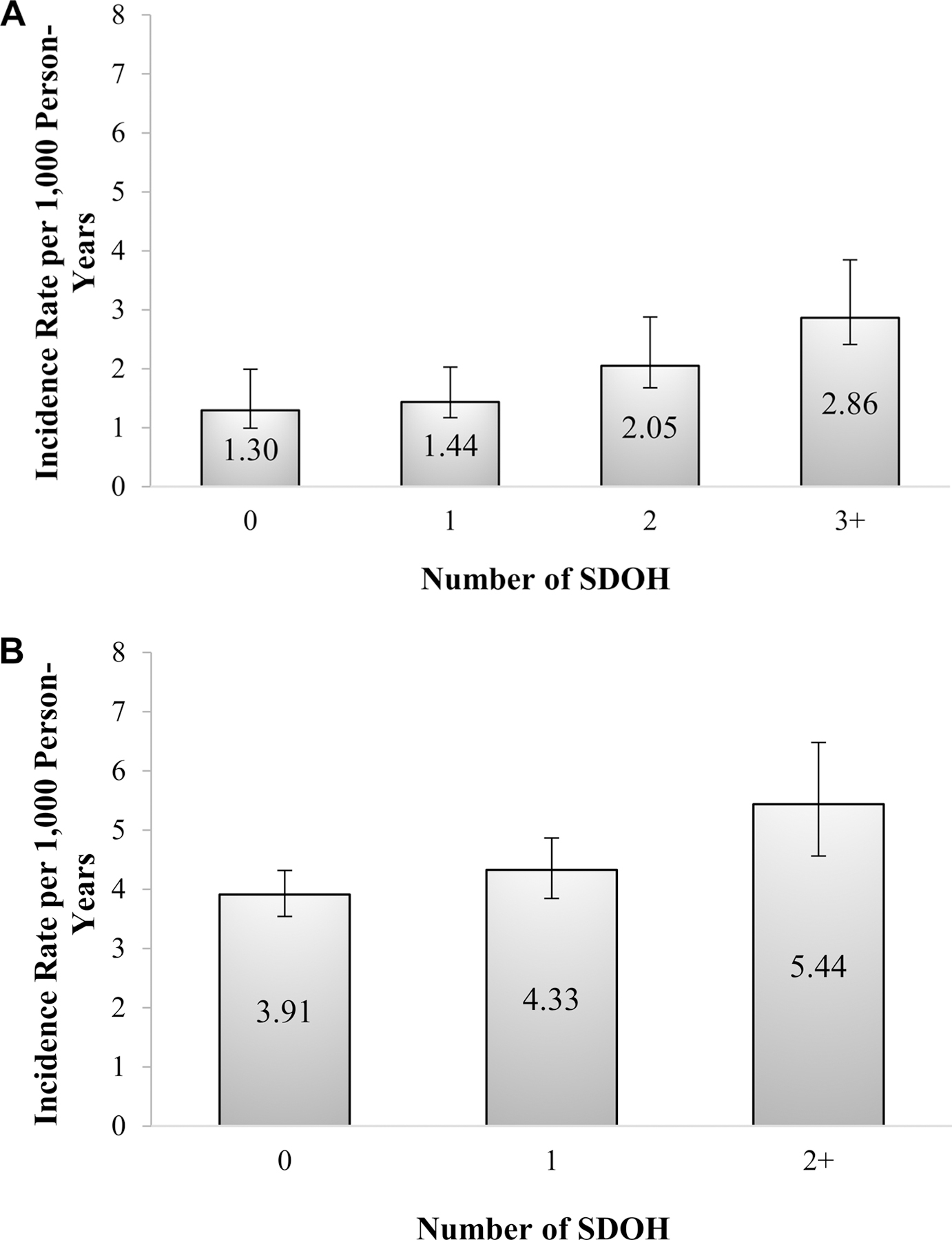
Age-adjusted Fatal Incidence of Coronary Heart Disease (A)* and Age-Adjusted Incidence of Nonfatal Myocardial Infarction (B)** per 1,000 Person-years, by Number of Social Determinants of Health*
*Social determinants for fatal incident coronary heart disease included Black race, low education, low annual household income, zip code with high poverty, residence in the worst ranked states for public health infrastructure, lack of health insurance, social isolation (saw no friends/family in the past month).
**Social determinants for incident nonfatal myocardial infarction included low education, low annual household income and lack of health insurance
Figure 2.
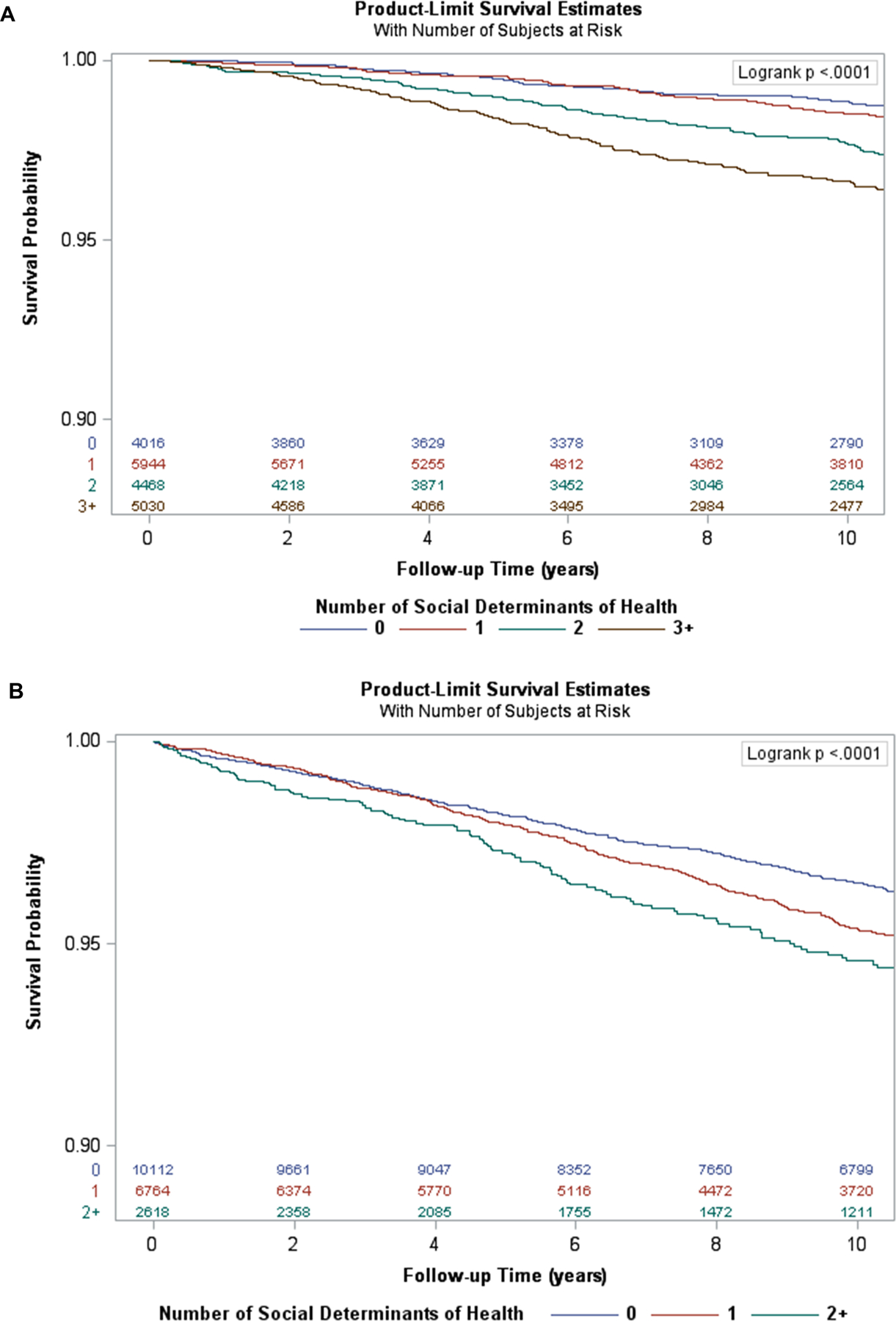
Kaplan-Meier Survival Curves by Number of Social Determinants of Health* and Fatal Incident Coronary Heart Disease (A)* and Incident Nonfatal Myocardial Infarction (B)**
*Social determinants for fatal incident coronary heart disease included Black race, low education, low annual household income, zip code with high poverty, residence in the worst ranked states for public health infrastructure, lack of health insurance, social isolation (saw no friends/family in the past month)
**Social determinants for nonfatal myocardial infarction include low education, low annual household income and lack of health insurance
Nonfatal incident MI by count of SDH
Non-fatal incident MI per 1000 person-years increased with each additional SDH; those with ≥2 SDH (5.44/1000 person-years) had 39% higher incidence compared to those with no SDH (3.91/1000 person-years) (Figure 1b). Participants with greater counts of SDH also had progressively higher cumulative incidence of nonfatal MI (Figure 2b, p<0.001).
Count of SDH and hazard of fatal incident CHD
Participants with higher counts of SDH had greater risk for fatal incident CHD (Table 3). Crude HR comparing participants with ≥3 versus no SDH was 2.78 (95% CI 2.07, 3.74). Having ≥3 versus no SDH was associated with fully adjusted HR 1.50 (95% CI 1.09, 2.06) with p for trend <0.0001 for both minimally and fully adjusted models.
Table 3.
Number of Social Determinants of Health and Associations with Fatal Incident Coronary Heart Disease and Incident Nonfatal Myocardial Infarction
| Fatal Incident CHD |
Incident Nonfatal MI |
||||||
|---|---|---|---|---|---|---|---|
| Number of SDH † | Number of events | HR (95% CI) |
Number of SDH †† | Number of events | HR (95% CI) |
||
| Crude | Fully adjusted * | Crude | Fully adjusted * | ||||
| 0 | 55 | 1.00 (reference) | 1.00 (reference) | 0 | 390 | 1.00 (reference) | 1.00 (reference) |
| 1 | 97 | 1.24 (0.90, 1.71) |
1.00 (0.72, 1.38) |
1 | 310 | 1.32 (1.14, 1.53) |
1.02 (0.87, 1.20) |
| 2 | 105 | 1.96 (1.43, 2.68) |
1.25 (0.91, 1.74) |
≥2 | 128 | 1.57 (1.30, 1.90) |
1.14 (0.93, 1.41) |
| ≥3 | 154 | 2.78 (2.07, 3.74) |
1.50 (1.09, 2.06) |
||||
| p for trend | <0.0001 | <0.0001 | <0.0001 | 0.26 | |||
Adjusted for sociodemographic factors, medical conditions, use of medications, functional status, health behaviors, and physiologic variables
SDOH included Black race, low education, low annual household income, zip code with high poverty, residence in the worst ranked states for public health infrastructure, lack of health insurance, social isolation (saw no friends/family in the past month). Note that not all available events are included in this table due to missing data on SDH; all events were used in modeling with multiple imputation.
SDOH included low education, low annual household income and lack of health insurance
CHD = coronary heart disease. CI = confidence interval. HR = hazard ratio. MI = myocardial infarction. SDH = social determinants of health
Count of SDH and hazard of incident nonfatal MI
Participants with higher counts of SDH had greater risk for non-fatal MI (Table 3). Crude HR comparing participants with ≥2 versus no SDH was 1.57 (95% CI 1.30, 1.90). A graded association remained present after multivariable adjustment but was not statistically significant (adjusted HR for ≥2 SDH vs. none 1.14; 95% CI 0.93, 1.41).
Discussion
We observed increasing risk of fatal incident CHD and nonfatal MI as the number of SDH increased. Individuals with ≥3 SDH had more than double the incidence of fatal CHD compared to those with none, a magnitude similar to the Black-white disparity in the incidence of stroke in the US.32 The risk of fatal incident CHD in the fully adjusted model was more than 67% higher for individuals with three or more SDH compared to those with none, demonstrating an independent association between a person’s burden of SDH and risk of fatal incident CHD. Similarly, the risk of incident nonfatal MI rose as the number of SDH increased, but this finding attenuated with full adjustment. Together, these findings suggest that a simple count of an individual’s number of SDH may be a novel approach that could be used in clinical care to quickly and easily identify patients at higher risk of CHD.
Our study is among the first to examine the association between the simple count of SDH and risk of incident CHD events.7 While associations with each SDH studied here and incident CHD have been described previously, few studies have examined the association between a count of SDH and CHD outcomes. Prior studies have shown differences in CHD mortality by urbanization, region, and race.33 Previous REGARDS studies demonstrated greater risk of incident CHD for the combination of low income and low education,34 higher risk of incident stroke as the count of SDH increased,12 and higher risk of incident heart failure as the count of SDH increased.13 The independent and cumulative associations with SDH could stem from toxic stresses of living with social disadvantage, with numerous studies suggesting a role for allostatic load.35–41 Allostatic stress responses include the stimulation of stress hormones, endothelial dysfunction, metabolic disturbances, and inflammation; although we had CRP, blood pressure, and glucose and diabetes status, we did not have measures of physiologic stress hormones or endothelial dysfunction. Life course factors have also been implicated as playing a role, but assessments prior to baseline were not available.42–45
Although incident CHD has declined dramatically since the 1970’s, more of these gains have been in the incidence of nonfatal than fatal CHD, and while death immediately following MI has reduced dramatically, sudden cardiac death remains frustratingly common.14 Epidemiologic trends of death at the presentation of CHD are not frequently reported, since most studies include individuals with known CHD. These studies demonstrate declines in both in-hospital and out-of-hospital cardiac arrest, with more modest declines among women and the elderly.14,15 Many studies also show that Black Americans continue to have twice the risk of sudden cardiac death compared with whites.16–19 Furthermore, although nationally the proportions of out-of-hospital deaths treated by Emergency Medical Services or receiving bystander cardiopulmonary resuscitation are rising, Black Americans are less likely to receive pre-hospital resuscitative efforts and they face worse prognosis after an out-of-hospital cardiac arrest.46,47 Although the associations for nonfatal MI were not significant after full adjustment, the current study suggests that efforts to achieve health equity by preventing CHD, especially fatal incident CHD, can be aided by recognition of the risks incurred by an individual’s burden of SDH.
This study has implications for both clinical care and population health management. Our findings suggest that assessing a person’s SDH burden may be a practical strategy for identifying high risk individuals for targeted intervention. The variables used here could be widely implemented as part of the social history, alerting treating physicians to intensify aggressiveness of CHD risk factor management, since the majority of out-of-hospital cardiac arrests are related to structural CHD.14 Our findings demonstrated lower risks with addition of behavioral and physiologic risk factors to models; these factors are amenable to intervention. Multi-level interventions that mobilize system level changes to mitigate the risks conferred by SDH while improving risk factor management at the individual level could reduce the high CHD risks faced by individuals with multiple SDH.48 Population health managers could use the simple count of SDH to identify patients for intervention to improve linkages to community resources including housing, social support, availability of healthy foods, or transportation.
While our study opens the door to a practical new risk marker for incident CHD outcomes, many questions remain. Our findings should be confirmed in other cohorts. Additional study is warranted to examine whether a core set of SDH can be used across health outcomes; existing studies each had some variation in which SDH were associated, as we saw here.12,13 Although our study operationalized at least one SDH in each of the Healthy People 2020 domains, there are other conceptual frameworks and additional variables that we did not have available, most notably structural racism, perceptions of discrimination, health literacy, and additional measures of allostatic load. Measures of the built environment such as healthy food availability, crime, and neighborhood walkability were not available. The differences in the relationship between SDH and fatal and nonfatal CHD warrant further study, especially in light of our past unexplained findings of lower nonfatal CHD among Black vs white men, a finding first observed in the REGARDS cohort but confirmed to have been present in earlier cohorts.1,49 Past reports have also observed differences in the specific SDH associated with CVD outcomes.12,50
Our study’s strengths include the large, national, biracial sample with rigorously collected data and CHD endpoints. The SDH included are widely available. Its limitations include the observational design, limiting causal inference, and some design features such as self-reported variables. Despite the availability of a host of variables, some potentially important SDH or direct physiologic measures of allostatic load were not available, limiting our ability to explore the role of these potential mechanisms to explain the findings. Several variables were only available at a single time point, precluding the ability to capture lifetime burden. The REGARDS study engaged only English speaking whites and Blacks, potentially limiting generalizability to Latinos. Finally, our approach was not internally or externally validated.
Conclusion
In conclusion, a simple count of widely available SDH may be a novel approach to identify individuals at high risk of incident CHD events that could be used in the course of clinical care. Our findings suggest that clinicians could substantially reduce these risks by aggressively managing risk factors in individuals with a greater number of SDH, and population health managers could target this population for interventions intended to overcome SDH.
Supplementary Material
Expanded methods
Supplemental Figures I-III
Supplemental Tables I-IV
Clinical Perspective.
What is new?
A simple count of social determinants of health identified individuals in this cohort at high risk of CHD events.
These effects were independently associated with fatal incident CHD, with 67% higher hazards after adjustment for a host of individual characteristics including CVD risk factors for individuals with three or more social determinants compared to those with none.
The count of social determinants was not independently associated with nonfatal incident CHD.
What are the clinical implications?
Social determinants can be obtained as part of the social history during a clinical encounter, and a simple count of social determinants is easy to implement.
If our findings are confirmed in other populations, they suggest a simple strategy to integrate social determinants into clinical care.
While clinicians may not be able to eradicate social determinants, they can use the count of social determinants as a signal to pay extra attention to CVD risk factor control in such high risk patients.
Acknowledgements
We thank investigators, staff, and participants of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study for their valuable contributions. A full list of investigators and institutions can be found at http://www.regardsstudy.org.
Sources of Funding
This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, and R01 HL80477 from the National Heart Lung and Blood Institute, National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. JNB received research support through American Heart Association grant SFRN 15SFRN2390002
Non-standard Abbreviations and Acronyms:
- REGARDS
REasons for Geographic And Racial Differences in Stroke
- SDH
social determinants of health
Footnotes
Conflicts of Interest
MMS and PMM receive research grant funding from Amgen, Inc. None of the other authors have any conflicts of interest to report.
References
- 1.Safford MM, Brown TM, Muntner PM, Durant RW, Glasser S, Halanych JH, Shikany JM, Prineas RJ, Samdarshi T, Bittner VA, et al. Association of race and sex with risk of incident acute coronary heart disease events. JAMA 2012;308(17):1768–1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.AHRQ. National Healthcare Disparities Report 2003; http://www.qualitytools.ahrq.gov/disparitiesreport/download_report.aspx, 2003.
- 3.AHRQ. 2015 National Healthcare Quality and Disparities Report and 5th Anniversary Update on the National Quality Strategy Rockville, MD: AHRQ; 2016. [Google Scholar]
- 4.CDC. CDC Health Disparities and Inequalities Report - United States, 2013 Atlanta, GA: November 22 2013. [Google Scholar]
- 5.Institute of Medicine. Guidance for the National Healthcare Disparities Report Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- 6.Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart 2016;102(13):1009–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation 2015;132(9):873–898. [DOI] [PubMed] [Google Scholar]
- 8.Schroeder SA. Shattuck Lecture. We can do better--improving the health of the American people. N Engl J Med 2007;357(12):1221–1228. [DOI] [PubMed] [Google Scholar]
- 9.Butler DC, Petterson S, Phillips RL, Bazemore AW. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res 2013;48(2 Pt 1):539–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO. A Conceptual Framework for Action on the Social Determinants of Health Geneva: World Health Organization;2010. [Google Scholar]
- 11.Schroff P, Gamboa CM, Durant RW, Oikeh A, Richman JS, Safford MM. Vulnerabilities to Health Disparities and Statin Use in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) Study. J Am Heart Assoc 2017;6(9):e005449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reshetnyak E, Ntamatungiro M, Pinheiro LC, Howard VJ, Carson AP, Martin KD, Safford MM. Impact of Multiple Social Determinants of Health on Incident Stroke. Stroke 2020;51(8):2445–2453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pinheiro LC, Reshetnyak E, Sterling MR, Levitan EB, Safford MM, Goyal P. Multiple Vulnerabilities to Health Disparities and Incident Heart Failure Hospitalization in the REGARDS Study. Circ Cardiovasc Qual Outcomes 2020;13(8):e006438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018;137(12):e67–e492. [DOI] [PubMed] [Google Scholar]
- 15.Gerber Y, Jacobsen SJ, Frye RL, Weston SA, Killian JM, Roger VL. Secular trends in deaths from cardiovascular diseases: a 25-year community study. Circulation 2006;113(19):2285–2292. [DOI] [PubMed] [Google Scholar]
- 16.Becker LB, Han BH, Meyer PM, Wright FA, Rhodes KV, Smith DW, Barrett J. Racial differences in the incidence of cardiac arrest and subsequent survival. The CPR Chicago Project. N Engl J Med 1993;329(9):600–606. [DOI] [PubMed] [Google Scholar]
- 17.Cowie MR, Fahrenbruch CE, Cobb LA, Hallstrom AP. Out-of-hospital cardiac arrest: racial differences in outcome in Seattle. Am J Public Health 1993;83(7):955–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bertoia ML, Allison MA, Manson JE, Freiberg MS, Kuller LH, Solomon AJ, Limacher MC, Johnson KC Curb JD, Wassertheil-Smoller S, Eaton CB. Risk factors for sudden cardiac death in post-menopausal women. J Am Coll Cardiol 2012;60(25):2674–2682. [DOI] [PubMed] [Google Scholar]
- 19.Okin PM, Kjeldsen SE, Julius S, Hille DA, Dahlof B, Devereux RB. Effect of changing heart rate during treatment of hypertension on incidence of heart failure. Am J Cardiol 2012;109(5):699–704. [DOI] [PubMed] [Google Scholar]
- 20.Deo R, Safford MM, Khodneva YA, Jannat-Khah DP, Brown TM, Judd SE, McClellan WM, Rhodes JD, Shlipak MG, Soliman EZ, Albert CM. Differences in Risk of Sudden Cardiac Death Between Blacks and Whites. J Am Coll Cardiol 2018;72(20):2431–2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The REasons for Geographic And Racial Differences in Stroke study: objectives and design. Neuroepidemiology 2005;25(3):135–143. [DOI] [PubMed] [Google Scholar]
- 22.Luepker RV, Apple FS, Christenson RH, Crow RS, Fortmann SP, Goff D, Goldbeg RJ, Hand MM, Jaffe AS, Julian DG, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: A statement from the AHA Council on Epidemiology and Prevention, AHA Statistics Committee, World Heart Federation Council on Epidemiology and Prevention, European Society of Cardiology Working Group on Epidemiology and Prevention, Centers for Disease Control and Prevention, and the National Heart Lung and Blood Institute. Circulation 2003;108(20):2543–2549. [DOI] [PubMed] [Google Scholar]
- 23.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Katus HA, Apple FS, Lindahl B, Morrow DA, et al. Third universal definition of myocardial infarction. Eur Heart J 2012;33(20):2551–2567. [DOI] [PubMed] [Google Scholar]
- 24.Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD. Fourth Universal Definition of Myocardial Infarction (2018). Circulation 2018;138(20):e618–e651. [DOI] [PubMed] [Google Scholar]
- 25.HealthyPeople.gov. Social Determinants of Health Available at https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed November 18, 2020.
- 26.United Health Foundation. America’s Health Rankings Available at https://www.americashealthrankings.org. Accessed November 17, 2020.
- 27.Pinheiro LC, Reshetnyak E, Sterling MR, Richman JS, Kern LM, Safford MM. Using health-related quality of life to predict cardiovascular disease events. Qual Life Res 2019;28(6):1465–1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scarmeas N, Luchsinger JA, Schupf N, Brickman AM, Cosentiono S, Tank MX, Stern Y. Physical activity, diet, and risk of Alzheimer disease. JAMA 2009;302(6):627–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scarmeas N, Stern Y, Mayeux R, Manly JJ, Schupf N, Luchsinger JA. Mediterranean diet and mild cognitive impairment. Arch Neurol 2009;66(2):216–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Feart C, Samieri C, Rondeau V, Amieva H, Portet F, Dartigues JF, Scarmeas N, Barberger-Gateau P. Adherence to a Mediterranean diet, cognitive decline, and risk of dementia. JAMA 2009;302(6):638–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150(9):604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation 2020;141(9):e139–e596. [DOI] [PubMed] [Google Scholar]
- 33.Kulshreshtha A, Goyal A, Dabhadkar K, Veledar E, Vaccarino V. Urban-rural differences in coronary heart disease mortality in the United States: 1999–2009. Public Health Rep 2014;129(1):19–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lewis MW, Khodneva Y, Redmond N, et al. The impact of the combination of income and education on the incidence of coronary heart disease in the prospective Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort study. BMC Public Health 2015;15:1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med 1998;338(3):171–179. [DOI] [PubMed] [Google Scholar]
- 36.McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci 1998;840:33–44. [DOI] [PubMed] [Google Scholar]
- 37.McEwen BS, Seeman T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci 1999;896:30–47. [DOI] [PubMed] [Google Scholar]
- 38.Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health 2006;96(5):826–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sabbah W, Watt RG, Sheiham A, Tsakos G. Effects of allostatic load on the social gradient in ischaemic heart disease and periodontal disease: evidence from the Third National Health and Nutrition Examination Survey. J Epidemiol Community Health 2008;62(5):415–420. [DOI] [PubMed] [Google Scholar]
- 40.Duru OK, Harawa NT, Kermah D, Norris KC. Allostatic load burden and racial disparities in mortality. J Natl Med Assoc 2012;104(1–2):89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gruenewald TL, Karlamangla AS, Hu P, Stein-Merkin S, Crandall D, Koretz B, Seeman TE. History of socioeconomic disadvantage and allostatic load in later life. Soc Sci Med 2012;74(1):75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lemelin ET, Diez Roux AV, Franklin TG, Carnethon M, Lutsey PL, Ni H, O’Meara E, Shrager S. Life-course socioeconomic positions and subclinical atherosclerosis in the multi-ethnic study of atherosclerosis. Soc Sci Med 2009;68(3):444–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Albert MA, Glynn RJ, Buring J, Ridker PM. Impact of traditional and novel risk factors on the relationship between socioeconomic status and incident cardiovascular events. Circulation 2006;114(24):2619–2626. [DOI] [PubMed] [Google Scholar]
- 44.Loucks EB, Pilote L, Lynch JW, Richard H, Almeida ND, Benjamin EJ, Murabito JM. Life course socioeconomic position is associated with inflammatory markers: the Framingham Offspring Study. Soc Sci Med 2010;71(1):187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Matthews KA, Schwartz JE, Cohen S. Indices of socioeconomic position across the life course as predictors of coronary calcification in black and white men and women: coronary artery risk development in young adults study. Soc Sci Med 2011;73(5):768–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sasson C, Magid DJ, Chan P, Root ED, McNally BF, Kellermann AL, Haukoos JS. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med 2012;367(17):1607–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shah KS, Shah AS, Bhopal R. Systematic review and meta-analysis of out-of-hospital cardiac arrest and race or ethnicity: black US populations fare worse. Eur J Prev Cardiol 2014;21(5):619–638. [DOI] [PubMed] [Google Scholar]
- 48.Andermann A, Collaboration C. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ 2016;188(17–18):E474–E483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Colantonio LD, Gamboa CM, Richman JS, Levitan EB, Soliman EZ, Howard G, Safford MM. Black-White Differences in Incident Fatal, Nonfatal, and Total Coronary Heart Disease. Circulation 2017;136(2):152–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sterling MR, Ringel JB, Pinheiro LC, Safford MM, Levitan EB, Phillips E, Brown TM, Goyal P. Social Determinants of Health and 90-Day Mortality After Hospitalization for Heart Failure in the REGARDS Study. J Am Heart Assoc 2020;9(9):e014836. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Expanded methods
Supplemental Figures I-III
Supplemental Tables I-IV


