Abstract
Background/Objectives:
Hospitalization is common among older adults with disability, many of whom receive help from a caregiver and have dementia. Our objective was to evaluate the association between caregiver factors and risk of hospitalization and whether associations differ by dementia status.
Design:
Longitudinal observational study.
Setting:
1999 and 2004 National Long-term Care Survey and 2011 and 2015 National Health and Aging Trends Study, linked caregiver surveys, and Medicare claims.
Participants:
2,589 community-living Medicare fee-for-service beneficiaries age ≥ 65 (mean age 79, 63% women, 31% with dementia) with self-care or mobility disability and their primary family or unpaid caregiver.
Measurements:
Self-reported characteristics of older adults and their caregivers were assessed from older adult and caregiver survey interviews. Older adult hospitalization over the subsequent 12 months was identified in Medicare claims. Multivariable Cox proportional hazards models adjusted for older adult characteristics and were stratified by dementia status.
Results:
In this nationally representative cohort, 38% of older adults with disabilities were hospitalized over 12 months following interview. Increased hospitalization risk was associated with having a primary caregiver who helped with healthcare tasks (adjusted HR [95% CI] 1.22 [1.05, 1.40]), reported physical strain (aHR [95% CI] 1.21 [1.04, 1.42]), and provided > 40 hours of care weekly (aHR [95% CI] 1.26 [1.04, 1.54] versus ≤ 20 hours). Having a caregiver who had helped for ≥4 years (versus < 1 year) was associated with 38% lower risk of hospitalization (aHR [95% CI] 0.62 [0.49, 0.79]). Older adults with and without dementia had similar rates of hospitalization (39.5% versus 37.3%, p=0.4), and caregiving factors were similarly associated with hospitalization regardless of older adults’ dementia status.
Conclusion:
Select caregiving characteristics are associated with hospitalization risk among older adults with disability. Hospitalization risk reduction strategies may benefit from understanding and addressing caregiving circumstances.
Keywords: hospitalization, caregiving, disability, dementia
INTRODUCTION
Approximately 6.6 million community-living older adults in the United States are receiving help with self-care or mobility disabilities.1 These older adults are at heightened risk of hospitalization.2 Hospitalization is a major driver of spending in the Medicare program; inpatient services accounted for 20% of Medicare spending ($157 billion) in 2018.3 Hospitalization also exacerbates risk among older adults for a range of adverse health outcomes, such as functional decline,4 falls,5 delirium,6 and cognitive decline.7 Prevention of hospitalization in older adults with disability may thus reduce healthcare costs while benefitting patients’ health.
Although numerous efforts have been undertaken to identify factors associated with hospitalization risk, studies to date have largely focused on individual risk factors.8–11 Care of older adults with disability often extends beyond the individual, however, as approximately 95% of community-living older adults with self-care or mobility disability receive unpaid help.1 Although the adequacy of assistance with care needs affects hospitalization,12 few studies have investigated the potential impact of caregiver and caregiving factors on older adult hospitalization.13–18
A large proportion of older adults with self-care disability are living with dementia.19 Prior studies in the general older adult population have found that dementia is associated with greater caregiver burden20 and caregiving intensity.21,22 Persons living with dementia are at greater risk of hospitalization than those without dementia.23–26 Reducing preventable hospitalizations is explicitly named as a national public health goal for older adults with dementia;27 many evidence-based dementia care interventions have not been able to reduce hospitalizations, however.28,29 Understanding whether and how caregiver factors affect hospitalization in older adults may not only benefit risk prediction, but also inform opportunities for hospitalization prevention. The relevance of caregiver factors may vary by older adults’ dementia status, as cognitive impairment may amplify the importance of a caregiver.21,22,30
The objective of this population-based study was to evaluate the association between caregiver factors and risk of hospitalization in older adults with disability. Given the potential differential impact of dementia caregiving on hospitalization, we secondarily examined whether caregiver factors associated with hospitalization differ by older adults’ dementia status.
METHODS
Design and Participants
This study pools data from the 1999 and 2004 National Long-term Care Survey (NLTCS) and 2011 and 2015 National Health and Aging Trends Study (NHATS) with linked caregiver surveys and Medicare claims.31 The NLTCS and NHATS are nationally representative surveys of adults age 65 and older. Both studies draw population-based samples using Medicare enrollment files as the sampling frame. Longitudinal surveys, administered via in-person interviews, assess a range of sociodemographic, functional, and medical factors. Caregiver surveys were conducted in the years included in this study. The Informal Caregivers Survey (ICS) linked to NLTCS and the National Study of Caregiving (NSOC) linked to NHATS are nationally representative surveys of family and unpaid nonfamily caregivers who were helping NLTCS and NHATS participants with self-care, mobility, or household activities due to health or functioning. Family caregivers were eligible regardless of whether they received pay for caregiving.
Inclusion and exclusion criteria for this study maximized cross-year comparability in measurement of disability32 and caregiving33 and have been described previously.31,34,35 From NLTCS and NHATS, we included community-living older adult participants who received help with at least one self-care (eating, dressing, bathing, or toileting) or indoor mobility (transferring or getting around inside) task from family or unpaid caregivers who completed a caregiver survey. We excluded residents of nursing homes or other residential facilities (n=4,318). We also excluded older adults insured by Medicare Advantage plans (n=833) and focused on those enrolled in fee-for-service Medicare, for whom we could assess hospitalization. The NLTCS-linked ICS was administered to the “primary” caregiver, defined as the family or unpaid nonfamily caregiver who helped the participant the most. In the NHATS-linked NSOC, we included a single “primary” caregiver as well, defined as the family or unpaid nonfamily caregiver providing the most hours of help weekly among the caregivers interviewed. Our sample included 2,589 older adult and caregiver dyads.
Caregiver Factors
Caregiver characteristics and caregiving circumstances were self-reported in ICS and NSOC. Sociodemographic caregiver characteristics included age, gender, and relationship to older adult (spouse or non-spouse). Caregiving circumstances included duration of caregiving, whether the caregiver lived with the older adult, employment status (holding paid employment unrelated to caregiving), hours of care provided each week, type of help provided, and self-rated health. Type of help encompassed self-care tasks, mobility, and healthcare tasks. Healthcare tasks included medication management or assistance, skin, wound, or dressing care, and administration of injections. We also examined measures of caregiving support and challenges. Caregiving support included support group and respite care use. Caregiving challenges refer to appraisal of financial strain, emotional strain, and physical strain based on responses to questions about whether helping the participant was financially, emotionally, or physically difficult for them.31
Outcome and covariates
All-cause hospitalization in the 12 months following the older adult interview was assessed from Medicare Part A claims. Key covariates considered in analyses of associations between caregiver factors and older adult hospitalization included survey- and claims-based measures of older adult characteristics. Self or proxy-reported older adult characteristics consisted of age, gender, race, education, living arrangement (alone or not), number of impairments in self-care or mobility activities, number of comorbid conditions (depression, diabetes, cancer, stroke, hip fracture in prior year, arthritis, lung disease, coronary artery disease), and hospitalization in the prior year. Older adult Medicare-Medicaid dual eligible status and enrollment in hospice were drawn from Medicare claims data. Survey year was included as a covariate.
We classified older adults as having dementia or not having dementia using methods previously described.31 In NHATS, probable dementia was assessed by self or proxy-report of a dementia or Alzheimer’s diagnosis, a score indicating likely dementia on the AD8 dementia screening interview administered to proxy respondents,36,37 or cognitive impairment in at least two of the three cognitive domains tested.38 Cognitive impairment in memory, orientation, and executive function was defined as a score ≥ 1.5 standard deviations (SD) below the mean for self-respondents in each domain.38 From NLTCS, we similarly used report of the diagnosis and cognitive impairment on testing, again using a cutoff of 1.5 SDs below the mean, to indicate probable dementia. For participants missing information from cognitive testing and no report of the diagnosis in NLTCS, we constructed measures using behaviors or symptoms of memory impairment that were significantly associated with report of the diagnosis or low cognitive test scores.31
Statistical Analysis
Both NLTCS and NHATS provide analytic sampling weights and design variables that reflect their complex multistage sampling strategy, which were applied in all analyses as previously described.31 We followed a phased approach to analyses. First, we descriptively examined characteristics of older adults and their caregivers. We then examined bivariate associations between older adult and caregiver factors with older adults’ subsequent hospitalization. Statistically significant differences were defined as p < 0.05 using a chi-square or Wald statistic. Older adult factors that were associated with hospitalization in bivariate analyses were included in multivariable models after excluding older adult characteristics that were expected to correlate with caregiver factors of interest such as older adult living arrangement and number of self-care or mobility impairments. All analyses were conducted first in the entire cohort and then stratified by dementia status. Differences in the dementia stratified cohorts were examined descriptively.
To examine the effect of caregiver factors on risk of hospitalization by 12 months, we constructed cause-specific Cox proportional hazards models that accounted for the date of first hospitalization and date of censoring events (death or end of 12-month study period). The cause-specific hazard estimates the instantaneous risk of experiencing hospitalization at each point in time among older adults still at risk of the outcome. Each caregiver factor was examined individually in a model that adjusted for older adult factors and survey year, first in the entire cohort and then in the dementia stratified cohort. Sensitivity analyses considered hospitalization in the prior year as a covariate, examined death or hospitalization as a composite outcome (156 participants or 4.8% of the sample died without being hospitalized), and excluded the second observation for dyads who participated in two survey years (n=136). Results of sensitivity analyses were similar to primary analyses and are not further presented. Analyses were conducted using SAS v. 9.4 (SAS Institute Inc, Cary, NC).
RESULTS
Older Adult Characteristics
Nearly 4 in 10 older adults with disability (38.0%) were hospitalized within 12 months of interview (Table 1). The cohort had a mean age of nearly 79 years and were mostly female (63.3%) and White (81.9%) with ≥ 12 years of education (62.3%). Participants had, on average, 2 of 8 comorbidities. Almost 45% of participants reported being hospitalized during the prior year. About one-third of the cohort (31.3%) had dementia. Mortality was 14.7% (n=451 deaths) over 12 months. Older adults with disability who were hospitalized were more likely to be older, male, to have < 12 years of education, greater number of comorbidities, greater self-care or mobility impairments, and to have been hospitalized in the prior year; they were less likely to be enrolled in hospice (Table 1). Dementia was not significantly associated with hospitalization risk: 39.5% of participants with dementia were hospitalized over 12 months as compared with 37.3% of participants without dementia (p=0.4).
Table 1.
Characteristics of older adults with self-care or mobility disability, overall and by hospitalization over 12 months
| Characteristica | Overall | Hospitalized | Not Hospitalized | P-valueb |
|---|---|---|---|---|
| Sample | 2589 | 1018 (38.0) | 1571 (62.0) | --- |
| Age, mean (SE) | 78.9 (0.2) | 79.7 (0.3) | 78.4 (0.3) | 0.002 |
| Gender | ||||
| Female | 1720 (63.3) | 643 (35.6) | 1077 (64.4) | 0.02 |
| Male | 869 (36.7) | 375 (42.0) | 494 (58.0) | |
| Race | ||||
| White | 2032 (81.9) | 814 (37.9) | 1218 (62.1) | 0.94 |
| Black | 421 (11.0) | 160 (39.0) | 261 (61.0) | |
| Other | 136 (7.1) | 44 (36.9) | 92 (63.1) | |
| Education | ||||
| < 12 years | 1202 (37.7) | 492 (40.7) | 710 (59.3) | 0.03 |
| ≥ 12 years | 1387 (62.3) | 526 (36.3) | 861 (63.7) | |
| Dual eligible | ||||
| Yes | 804 (27.2) | 333 (41.4) | 471 (58.6) | 0.06 |
| No | 1785 (72.8) | 685 (36.7) | 1100 (63.3) | |
| Living arrangement | ||||
| Alone | 488 (14.6) | 190 (39.4) | 298 (60.6) | 0.61 |
| With others | 2101 (85.4) | 828 (37.7) | 1273 (62.3) | |
| Comorbidities,c mean (SE) | 2.1 (0.0) | 2.4 (0.1) | 2.0 (0.1) | <0.001 |
| Dementia status | ||||
| Dementia | 925 (31.3) | 361 (39.5) | 564 (60.5) | 0.4 |
| No dementia | 1664 (68.7) | 657 (37.3) | 1007 (62.7) | |
| Self-care/mobility impairments, mean (SE) | 2.3 (0.0) | 2.5 (0.1) | 2.2 (0.1) | 0.01 |
| Hospitalized in prior year | ||||
| Yes | 1071 (44.5) | 509 (47.7) | 562 (52.3) | <0.001 |
| No | 1518 (55.5) | 509 (30.2) | 1009 (69.8) | |
| Hospice use | ||||
| Yes | 134 (4.4) | 17 (11.2) | 117 (88.8) | <0.001 |
| No | 2455 (95.6) | 1001 (39.2) | 1454 (60.8) |
SE=standard error
Unweighted n (weighted %) unless specified. Percentages use analytic sample weights accounting for survey design and represent column percent for the overall sample column and row percent for hospitalization columns.
P-value calculated using chi-square or Wald test.
Comorbidities include depression, diabetes, cancer, stroke, hip fracture, arthritis, lung disease, coronary artery disease.
Caregiving Characteristics
Nearly half (48.5%) of caregivers were age 65 or older (Table 2). Caregivers were mostly female (64.4%), non-spouses (56.2%), and lived with the care recipient (75.3%). More than half (53.1%) had been providing care for 4 or more years. A minority of caregivers used support groups (4.6%) or respite care (14.4%). With regard to caregiving challenges, 31.7% reported financial strain, 55.7% reported emotional strain, and 41.4% reported physical strain. Older adults who experienced hospitalization were more likely to rely on a non-spousal caregiver and a caregiver who was helping with healthcare tasks (Table 2). Duration of caregiving was inversely associated with hospitalization, with lower percentages of older adults hospitalized as duration of caregiving increased. Older adults with caregivers who provided greater hours of care per week or reported physical strain were more likely to be hospitalized; financial and emotional strain demonstrated trends toward greater risk of hospitalization but were not statistically significant.
Table 2.
Characteristics of caregivers of older adults with self-care or mobility disability, overall and by older adult hospitalization over 12 months
| Characteristica | Overall | Hospitalized | Not Hospitalized | P-valueb |
|---|---|---|---|---|
| Age | ||||
| < 45 | 234 (9.8) | 85 (37.1) | 149 (62.9) | 0.89 |
| 45 - 64 | 1162 (41.6) | 465 (38.9) | 697 (61.1) | |
| 65 - 74 | 594 (25.9) | 231 (36.5) | 363 (63.5) | |
| 75+ | 599 (22.6) | 237 (38.4) | 362 (61.6) | |
| Gender | ||||
| Female | 1768 (64.4) | 694 (38.3) | 1074 (61.7) | 0.69 |
| Male | 821 (35.6) | 324 (37.3) | 497 (62.7) | |
| Relationship | ||||
| Spouse | 905 (43.8) | 340 (34.6) | 565 (65.4) | 0.03 |
| Non-spouse | 1684 (56.2) | 678 (40.6) | 1006 (59.4) | |
| Living arrangement with older adult | ||||
| Coreside | 1870 (75.3) | 742 (37.9) | 1128 (62.1) | 0.90 |
| Reside apart | 719 (24.7) | 276 (38.3) | 443 (61.7) | |
| Self-rated health | ||||
| Fair/poor | 704 (26.4) | 291 (37.3) | 413 (62.7) | 0.73 |
| Better | 1885 (73.6) | 727 (38.2) | 1158 (61.8) | |
| Employed for pay | ||||
| Yes | 815 (30.2) | 323 (36.2) | 492 (63.8) | 0.38 |
| No | 1774 (69.8) | 695 (38.7) | 1079 (61.3) | |
| Duration of caregiving | ||||
| < 1 year | 356 (12.9) | 167 (48.0) | 189 (52.0) | <0.001 |
| 1-4 years | 883 (34.0) | 378 (42.2) | 505 (57.8) | |
| ≥ 4 years | 1350 (53.1) | 473 (32.8) | 877 (67.2) | |
| Weekly hours of care | ||||
| 0 - 20 | 1166 (49.0) | 414 (33.9) | 752 (66.1) | 0.01 |
| 21 - 40 | 692 (23.5) | 294 (40.8) | 398 (59.2) | |
| > 40 | 731 (27.4) | 310 (42.7) | 421 (57.3) | |
| Provides self-care help | ||||
| Yes | 1754 (69.5) | 708 (38.9) | 1046 (61.1) | 0.23 |
| No | 835 (30.5) | 310 (35.8) | 525 (64.2) | |
| Provides mobility help | ||||
| Yes | 1841 (73.9) | 732 (38.0) | 1109 (62.0) | 0.99 |
| No | 748 (26.1) | 286 (38.0) | 462 (62.0) | |
| Provides healthcare task help | ||||
| Yes | 1575 (65.3) | 641 (39.6) | 934 (60.4) | 0.03 |
| No | 1014 (34.7) | 377 (35.0) | 637 (65.0) | |
| Caregiving support and challenges | ||||
| Support group use | ||||
| Yes | 135 (4.6) | 50 (37.6) | 85 (62.4) | 0.95 |
| No | 2454 (95.4) | 968 (38.0) | 1486 (62.0) | |
| Respite care use | ||||
| Yes | 391 (14.4) | 148 (38.2) | 243 (61.8) | 0.95 |
| No | 2198 (85.6) | 870 (37.9) | 1328 (62.1) | |
| Financial strain | ||||
| None | 1717 (68.3) | 642 (36.6) | 1075 (63.4) | 0.11 |
| Some/a lot | 872 (31.7) | 376 (40.8) | 496 (59.2) | |
| Emotional strain | ||||
| None | 1127 (44.3) | 429 (35.8) | 698 (64.2) | 0.09 |
| Some/a lot | 1462 (55.7) | 589 (39.7) | 873 (60.3) | |
| Physical strain | ||||
| None | 1409 (58.6) | 506 (34.4) | 903 (65.6) | <0.001 |
| Some/a lot | 1180 (41.4) | 512 (43.1) | 668 (56.9) | |
Unweighted n (weighted %). Percentages use analytic sample weights accounting for survey design and represent column percent for the overall sample column and row percent for hospitalization columns.
P-value calculated using chi-square.
Multivariable Analyses
Caregivers’ sociodemographic characteristics and caregiving circumstances were associated with older adults’ risk of hospitalization by 12 months in multivariable models that adjusted for older adult factors (age, gender, education, chronic conditions, hospice enrollment) and survey year (Figure 1A). Having a female caregiver was associated with 18% lower risk of hospitalization (aHR 0.82, 95%CI [0.68, 0.99], p=0.04). Longer duration of caregiving was associated with lower risk of hospitalization: older adults relying on a caregiver providing care for ≥ 4 years (versus < 1 year) had aHR (95%CI) of 0.62 (0.49, 0.79) for being hospitalized within 12 months (p<0.001). Having a caregiver who provided more than 40 hours of care per week was associated with increased risk of hospitalization (aHR 1.26, 95%CI [1.04, 1.54], p=0.02) compared to having a caregiver providing ≤ 20 hours of care per week. Having a caregiver who did (versus did not) help with healthcare tasks was associated with 22% greater risk of hospitalization (aHR 1.22, 95%CI [1.05, 1.40], p=0.01). Among caregiving supports and challenges (Figure 1B), having a caregiver who did (versus did not) report caregiving-related physical strain was associated with increased risk of hospitalization (aHR 1.21, 95%CI [1.04, 1.42], p=0.02).
Figures 1A and 1B. Multivariable adjusted hazard ratio for older adult hospitalization as a function of caregiver characteristics.
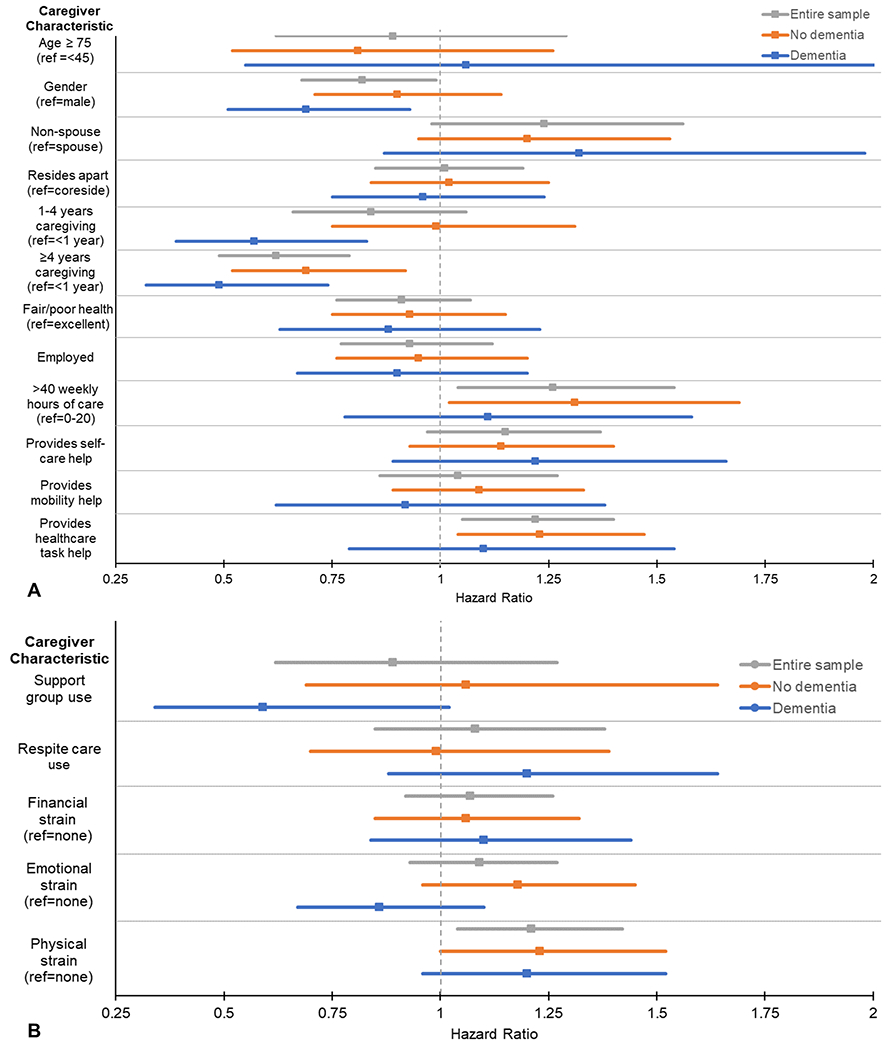
Figure 1 displays the hazard ratio and 95% confidence interval for risk of older adult hospitalization within 12 months for each caregiver factor (A) and caregiving challenge and support (B). Each model included the caregiving characteristic of interest adjusted for older adult age, gender, education, chronic condition count, hospice enrollment, and survey year. Results are shown for the entire sample (gray) and the dementia-stratified sample (orange = no dementia; blue = dementia). CG= caregiver
Dementia stratified cohort
Caregivers of older adult participants with dementia were younger and more likely to be female and non-spouses compared to the non-dementia caregivers (Table 3). Dementia caregivers provided more hours of care per week and were more likely to help with self-care, mobility, and healthcare tasks. Dementia caregivers were both more likely to use supports and to report financial, emotional, and physical strain than non-dementia caregivers.
Table 3.
Characteristics of caregivers of older adults with self-care or mobility disability by older adults’ dementia status
| Dementia subcohorts | |||
|---|---|---|---|
| Characteristica | No dementia | Dementia | P-valueb |
| Age | |||
| < 45 | 159 (9.7) | 75 (10.2) | 0.001 |
| 45 - 64 | 676 (38.2) | 486 (49.1) | |
| 65 - 74 | 411 (28.3) | 183 (20.7) | |
| 75+ | 418 (23.8) | 181 (20.1) | |
| Gender | |||
| Female | 1077 (60.8) | 691 (72.2) | <0.001 |
| Male | 587 (39.2) | 234 (27.8) | |
| Relationship | |||
| Spouse | 688 (50.2) | 217 (29.5) | <0.001 |
| Non-spouse | 976 (49.8) | 708 (70.5) | |
| Living arrangement with older adult | |||
| Coreside | 1215 (76.3) | 655 (73.2) | 0.14 |
| Reside apart | 449 (23.7) | 270 (26.8) | |
| Self-rated health | |||
| Fair/poor | 433 (25.4) | 271 (28.5) | 0.25 |
| Better | 1231 (74.6) | 654 (71.5) | |
| Employed for pay | |||
| Yes | 507 (29.1) | 308 (32.5) | 0.20 |
| No | 1157 (70.9) | 617 (67.5) | |
| Duration of caregiving | |||
| < 1 year | 251 (13.8) | 105 (10.9) | 0.09 |
| 1-4 years | 551 (32.4) | 332 (37.5) | |
| ≥ 4 years | 862 (53.7) | 488 (51.6) | |
| Weekly hours of care | |||
| 0 - 20 | 854 (55.1) | 312 (35.7) | <0.001 |
| 21 - 40 | 442 (22.9) | 250 (24.9) | |
| > 40 | 368 (22.0) | 363 (39.4) | |
| Provides self-care help | |||
| Yes | 1048 (65.9) | 706 (77.6) | <0.001 |
| No | 616 (34.1) | 219 (22.4) | |
| Provides mobility help | |||
| Yes | 1116 (70.7) | 725 (80.8) | <0.001 |
| No | 548 (29.3) | 200 (19.2) | |
| Provides healthcare task help | |||
| Yes | 863 (57.9) | 712 (81.5) | <0.001 |
| No | 801 (42.1) | 213 (18.5) | |
| Caregiving support and challenges | |||
| Support group use | |||
| Yes | 70 (3.8) | 65 (6.4) | 0.008 |
| No | 1594 (96.2) | 860 (93.6) | |
| Respite care use | |||
| Yes | 172 (10.3) | 219 (23.4) | <0.001 |
| No | 1492 (89.7) | 706 (76.6) | |
| Financial strain | |||
| None | 1163 (71.4) | 554 (61.5) | <0.001 |
| Some/a lot | 501 (28.6) | 371 (38.5) | |
| Emotional strain | |||
| None | 841 (50.2) | 286 (31.3) | <0.001 |
| Some/a lot | 823 (49.8) | 639 (68.7) | |
| Physical strain | |||
| None | 986 (63.1) | 502 (51.1) | <0.001 |
| Some/a lot | 678 (36.9) | 423 (48.9) | |
Unweighted n (weighted %). Percentages use analytic sample weights accounting for survey design and represent column percent.
P-value calculated using chi-square.
Caregiving factors that were associated with older adults’ hospitalization were largely consistent, or demonstrated similar trends, by older adults’ dementia status in unadjusted (Table 4) and multivariable adjusted (Figures 1A and 1B) models. Having a caregiver who had been providing help over a longer duration was associated with lower risk of hospitalization among older adults with and without dementia (aHR 0.49, 95%CI [0.32, 0.74], p < 0.001 and aHR 0.69, 95%CI [0.52, 0.92], p=0.01 for ≥ 4 years versus < 1 year of caregiving in older adults with and without dementia, respectively). Having a caregiver who reported physical strain was associated with higher risk of hospitalization among older adults with and without dementia in unadjusted analyses but remained statistically significant after adjustment in the absence of dementia only (aHR 1.23, 95%CI [1.00, 1.52], p = 0.048 in older adults without dementia, aHR 1.20, 95%CI [0.96, 1.52], p=0.1 in older adults with dementia). Relying on a caregiver who was providing 40 or more hours of help per week (aHR 1.31, 95%CI [1.02, 1.69], p=0.03 compared to 0-20 hours per week) – or a caregiver who was providing help with healthcare tasks (aHR 1.23, 95%CI [1.04, 1.47], p=0.02) was associated with greater risk of hospitalization among older adults without dementia only. Having a female caregiver was associated with lower risk of hospitalization among older adults with dementia only (aHR 0.69, 95%CI [0.51, 0.93], p=0.02).
Table 4.
Bivariate associations between caregiver characteristics and older adult hospitalization over 12 months by older adults’ dementia status
| No dementia | Dementia | |||||
|---|---|---|---|---|---|---|
| Characteristica | Hospitalized | Not Hospitalized | P-valueb | Hospitalized | Not Hospitalized | P-valueb |
| Age | ||||||
| < 45 | 56 (35.4) | 103 (64.6) | 0.93 | 29 (40.6) | 46 (59.4) | 0.79 |
| 45 - 64 | 270 (38.5) | 406 (61.5) | 195 (39.6) | 291 (60.4) | ||
| 65 - 74 | 167 (36.7) | 244 (63.3) | 64 (35.8) | 119 (64.2) | ||
| 75+ | 164 (36.8) | 254 (63.2) | 73 (42.6) | 108 (57.4) | ||
| Gender | ||||||
| Female | 430 (38.9) | 647 (61.1) | 0.18 | 264(37.3) | 427 (62.7) | 0.08 |
| Male | 227 (34.8) | 360 (65.2) | 97 (45.2) | 137 (54.8) | ||
| Relationship | ||||||
| Spouse | 258 (34.0) | 430 (66.0) | 0.03 | 82 (37.0) | 135 (63.0) | 0.63 |
| Non-spouse | 399 (40.6) | 577 (59.4) | 279 (40.6) | 429 (59.4) | ||
| Living arrangement with older adult | ||||||
| Coreside | 485 (36.9) | 730 (63.1) | 0.59 | 257 (40.1) | 398 (59.9) | 0.53 |
| Reside apart | 172 (38.5) | 277 (61.5) | 104 (37.8) | 166 (62.2) | ||
| Self-rated health | ||||||
| Fair/poor | 176 (35.6) | 257 (64.4) | 0.56 | 115 (40.8) | 156 (59.2) | 0.72 |
| Better | 481 (37.8) | 750 (62.2) | 246 (39.0) | 408 (61.0) | ||
| Employed for pay | ||||||
| Yes | 204 (36.2) | 303 (63.8) | 0.66 | 119 (36.4) | 189 (63.6) | 0.27 |
| No | 453 (37.7) | 704 (62.3) | 242 (41.0) | 375 (59.0) | ||
| Duration of caregiving | ||||||
| < 1 year | 109 (43.3) | 142 (56.7) | <0.001 | 58 (61.0) | 47 (39.0) | 0.001 |
| 1-4 years | 244 (44.0) | 307 (56.0) | 134 (38.9) | 198 (61.1) | ||
| ≥ 4 years | 304 (31.7) | 558 (68.3) | 169 (35.4) | 319 (64.6) | ||
| Weekly hours of care | ||||||
| 0 - 20 | 301 (33.0) | 553 (67.0) | 0.009 | 113 (37.1) | 199 (62.9) | 0.65 |
| 21 - 40 | 198 (41.6) | 244 (58.4) | 96 (39.2) | 154 (60.8) | ||
| > 40 | 158 (43.4) | 210 (56.6) | 152 (41.9) | 211 (58.1) | ||
| Provides self-care help | ||||||
| Yes | 426 (38.0) | 622 (62.0) | 0.49 | 282 (40.6) | 424 (59.4) | 0.27 |
| No | 231 (35.8) | 385 (64.2) | 79 (35.8) | 140 (64.2) | ||
| Provides mobility help | ||||||
| Yes | 448 (37.5) | 668 (62.5) | 0.77 | 284 (38.8) | 441 (61.2) | 0.54 |
| No | 209 (36.6) | 339 (63.4) | 77 (42.5) | 123 (57.5) | ||
| Provides healthcare task help | ||||||
| Yes | 355 (39.4) | 508 (60.6) | 0.04 | 286 (39.8) | 426 (60.2) | 0.76 |
| No | 302 (34.3) | 499 (65.7) | 75 (38.2) | 138 (61.8) | ||
| Caregiving support and challenges | ||||||
| Support group use | ||||||
| Yes | 29 (45.9) | 41 (54.1) | 0.20 | 21 (26.9) | 44 (73.1) | 0.05 |
| No | 628 (36.9) | 966 (63.1) | 340 (40.4) | 520 (59.6) | ||
| Respite care use | ||||||
| Yes | 63 (38.3) | 109 (61.7) | 0.83 | 85 (38.0) | 134 (62.0) | 0.64 |
| No | 594 (37.1) | 898 (62.9) | 276 (40.0) | 430 (60.0) | ||
| Financial strain | ||||||
| None | 434 (36.1) | 729 (63.9) | 0.28 | 208 (38.0) | 346 (62.0) | 0.31 |
| Some/a lot | 223 (40.1) | 278 (59.9) | 153 (42.0) | 218 (58.0) | ||
| Emotional strain | ||||||
| None | 307 (33.7) | 534 (66.3) | 0.02 | 122 (43.2) | 164 (56.8) | 0.20 |
| Some/a lot | 350 (40.8) | 473 (59.1) | 239 (37.8) | 400 (62.2) | ||
| Physical strain | ||||||
| None | 356 (34.3) | 630 (65.7) | 0.01 | 150 (34.6) | 273 (65.4) | 0.009 |
| Some/a lot | 301 (42.4) | 377 (57.6) | 211 (44.2) | 291 (55.8) | ||
Unweighted n (weighted %). Percentages use analytic sample weights accounting for survey design and represent row percent.
P-value calculated using chi-square.
DISCUSSION
This study of a nationally representative sample of older adults with self-care or mobility disability and their primary caregivers finds that caregiving characteristics and challenges were associated with older adult hospitalization risk even after controlling for older adult factors. Shorter duration of caregiving, greater hours of care provided weekly, helping with healthcare tasks, physical strain, and male gender were associated with greater risk of hospitalization. Similar trends were observed when the cohort was stratified by dementia status. Notably, dementia was not significantly associated with greater risk of hospitalization in this cohort of older adults with disability.
Few studies have previously examined whether caregiver factors are associated with hospitalization:14,39 prior studies have primarily considered only whether a caregiver or care services are present11,40 or adequate.12 Several studies have found that caregiver distress,13 depression,41 low perceived social support,17,18 and perceived competence16 increased hospitalization risk, but focused on specific groups of older adults (congestive heart failure17,41 or dementia13,15) or on readmissions.18,41 Our study thus contributes new knowledge by identifying caregiving factors longitudinally associated with older adult all-cause hospitalization in a national sample after controlling for patient level factors associated with hospitalization.
The association between shorter duration of caregiving and greater risk of hospitalization merits comment. Although the intensity of care provided often increases over time,42 caregivers may also develop confidence and competence with time. Caregivers rarely receive adequate training/support for their role,43,44 instead learning “on the job” through trial and error.44,45 Thus, over time caregivers may become increasingly capable in managing complex care and new older adult needs. Prior work does suggest that caregiver capacity, particularly related to healthcare tasks, may increase with experience in the caregiving role.46 It is also possible that caregivers who report a longer caregiving duration experience lower burden and are thus willing and able to continue providing care. They might also be caring for older adults who have fewer underlying health conditions or are able to remain safely in the community for longer.
Study results are relevant to efforts to reduce rates of hospitalization in a population particularly vulnerable to adverse events and outcomes. Focusing research and efforts on certain groups of caregivers or aspects of caregiving may be one potential strategy: training and education to better recognize and support the role of caregivers new to a caregiving role or providing help with healthcare tasks, for example, might prevent older adult hospitalization.44,47,48 Referral to services that afford access to paid help to mitigate physical strain and reduce hours of care could also affect hospitalization. Further research into the impact of targeted caregiver interventions on older adult hospitalization in this population is warranted. Traditional Medicare currently covers hospitalization but does not reimburse for caregiver support services, although recent changes afford greater flexibility to cover such services to beneficiaries enrolled in Medicare Advantage.49 Research into the potential impact of Medicare coverage of different forms of caregiver support on hospitalization and overall Medicare costs is also warranted.
While overall hospice use was low (4.4%), hospice enrollment was strongly associated with lower risk of hospitalization. Where patients may be eligible for hospice, timely referrals to hospice might prevent hospitalization by clarifying whether hospitalization is congruent with patient goals of care and making available supportive services that may otherwise be difficult to obtain or afford. Further, systems changes that address physical strain for caregivers of patients not yet eligible for hospice, such as expanded availability and scope of palliative care services, could both reduce caregiver strain and potentially reduce hospitalizations.
Our results call attention to similarities and differences in older adults’ caregiving circumstances and hospitalization by dementia status. The greater care needs of older adults with dementia is well established.21 A large body of evidence has also demonstrated that dementia is highly associated with caregiver burden.20,44,50 This study shows that greater care needs and caregiver strain in dementia persist even when focusing only on older adults with self-care or mobility disability. However, caregiving circumstances for all older adults with disability, regardless of dementia status, may impact older adult hospitalization. Our findings suggest that efforts to reduce hospitalization in older adults with disability may be able to target dementia and non-dementia caregivers together or using similar strategies – it is notable that dementia was not associated with greater risk of hospitalization despite greater functional impairment, caregiving intensity, and caregiving challenges in older adults with dementia.
The comparable rates of hospitalization by older adults’ dementia status found in this study contrasts with prior studies of hospitalization that have found higher hospitalization rates in dementia.23–26 This difference may be due to our focus on a specific subgroup of older adults: individuals with disability who are receiving help from a family or unpaid caregiver, all of whom have functional impairment and help available to address their needs. In addition, dementia caregivers were more likely to access support resources. Older adults with dementia may also have a wider network of caregivers,21 such that the primary caregiver, the focus of this study, receives support from additional caregivers.
This study has several limitations. First, though we considered several older adult characteristics associated with hospitalization, there may be additional factors that confound the association between caregiver factors and hospitalization that we were unable to examine from the data available. As an example, helping with healthcare tasks could be a surrogate marker for older adult healthcare needs rather than a direct contributor to older adult hospitalization. Second, among older adults with disability, death and nursing home placement serve as competing risks when examining hospitalization as the outcome of interest. We did examine death or hospitalization as a composite outcome in sensitivity analysis, and nursing home placement was expected to be infrequent in this cohort in the 12-month follow up period based on a prior study.34 Third, dementia was measured epidemiologically rather than clinically; methods used in this study reflect methods used in most large population-based studies, however.38 Fourth, study findings only apply to older adults who have a caregiver though most community-living older adults with disability do receive unpaid help.1 With regard to generalizability, though we examine a nationally representative sample, older adult participants were largely White, female, and with 12 or more years of education. Additional study in more diverse samples or specific subgroups is needed to understand the role of caregiver factors in more diverse populations. Lastly, while the use of longitudinal rather than cross-sectional assessment of hospitalization is a strength, we cannot make inferences regarding causality. In fact, caregiver factors are unlikely to lead to older adult hospitalization in isolation; rather, they may be contributory in the setting of older adult comorbidities, acute symptoms, and other psychosocial factors.
This study is the first to consider the association between caregiving factors and older adult hospitalization in a nationally representative sample of older adults with self-care or mobility disability. Our findings suggest that efforts to identify and support caregivers new to their role, providing over 40 hours of care per week, experiencing physical strain, or responsible for assisting with healthcare activities could hold promise for reduced rates of hospitalization in a vulnerable group of older adults regardless of dementia status.
ACKNOWLEDGEMENTS
I certify that everyone who has contributed significantly to this work is listed as an author.
Funding Sources: This work was supported by the National Institute on Aging (R01 AG047859).
Footnotes
Presentations: Results were presented at the 2019 Gerontological Society of America scientific meeting in Austin, TX.
Conflict of Interest: The authors have no conflicts to disclose.
Sponsor’s Role: The sponsor had no role in study design, methods, analysis, or preparation of the manuscript.
REFERENCES
- 1.Freedman VA, Spillman BC. Disability and Care Needs Among Older Americans. Milbank Q. 2014;92(3):509–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional Disability and Health Care Expenditures for Older Persons. JAMA Intern Med. 2001;161(21):2602–2607. [DOI] [PubMed] [Google Scholar]
- 3.Medicare Payment Advisory Commission. Health Care Spending and the Medicare Program. MedPAC (online) D.C. Available at: http://www.medpac.gov/-documents-/data-book Accessed April 20, 2020.
- 4.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of Independence in Activities of Daily Living in Older Adults Hospitalized with Medical Illnesses: Increased Vulnerability with Age. J Am Geriatr Soc. 2003;51(4):451–458. [DOI] [PubMed] [Google Scholar]
- 5.Corsinovi L, Bo M, Ricauda Aimonino N, et al. Predictors of falls and hospitalization outcomes in elderly patients admitted to an acute geriatric unit. Arch Gerontol Geriatr. 2009;49(1):142–145. [DOI] [PubMed] [Google Scholar]
- 6.Inouye SK, Schlesinger MJ, Lydon TJ. Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care. Am J Med. 1999;106(5):565–573. [DOI] [PubMed] [Google Scholar]
- 7.Wilson RS, Hebert LE, Scherr PA, Dong X, Leurgens SE, Evans DA. Cognitive decline after hospitalization in a community population of older persons. Neurology. 2012;78(13):950–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller EA, Weissert WG. Predicting Elderly People’s Risk for Nursing Home Placement, Hospitalization, Functional Impairment, and Mortality: A Synthesis. Med Care Res Rev. 2000;57(3):259–297. [DOI] [PubMed] [Google Scholar]
- 9.Morris JN, Howard EP, Steel K, et al. Predicting risk of hospital and emergency department use for home care elderly persons through a secondary analysis of cross-national data. BMC Health Serv Res. 2014;14(1):519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wallace E, Stuart E, Vaughan N, Bennett K, Fahey T, Smith SM. Risk Prediction Models to Predict Emergency Hospital Admission in Community-dwelling Adults. Med Care. 2014;52(8):751–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Landi F, Onder G, Cesari M, et al. Comorbidity and social factors predicted hospitalization in frail elderly patients. J Clin Epidemiol. 2004;57(8):832–836. [DOI] [PubMed] [Google Scholar]
- 12.Xu H, Covinsky KE, Stallard E, Thomas J, Sands LP. Insufficient help for activity of daily living disabilities and risk of all-cause hospitalization. J Am Geriatr Soc. 2012;60(5):927–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maust DT, Kales HC, McCammon RJ, Blow FC, Leggett A, Langa KM. Distress Associated with Dementia-Related Psychosis and Agitation in Relation to Healthcare Utilization and Costs. Am J Geriatr Psychiatry. 2017;25(10):1074–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Longacre ML, Wong YN, Fang CY. Caregiver psychological health and hospitalization characteristics of older adult care recipients: An integrative review of U.S. studies. Res Gerontol Nurs. 2014;7(3):139–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thorpe JM, van Houtven CH, Sleath BL, Thorpe CT. Rural-urban differences in preventable hospitalizations among community-dwelling veterans with dementia. J Rural Heal. 2010;26(2):146–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wolff JL, Kasper JD. Informal caregiver characteristics and subsequent hospitalization outcomes among recipients of care. Aging Clin Exp Res. 2004;16(4):307–313. [DOI] [PubMed] [Google Scholar]
- 17.Saunders MM. Family caregiver support and hospitalizations of patients with heart failure. Home Healthc Nurse. 2008;26(10):624–632. [DOI] [PubMed] [Google Scholar]
- 18.Schwarz KA. Predictors of early hospital readmissions of older adults who are functionally impaired. J Gerontol Nurs. 2000;26(6):29–36. [DOI] [PubMed] [Google Scholar]
- 19.Agüero-Torres H, Fratiglioni L, Guo Z, Viitanen M, von Strauss E, Winblad B. Dementia is the major cause of functional dependence in the elderly: 3-year follow-up data from a population-based study. Am J Public Health. 1998;88(10):1452–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riffin C, Van Ness PH, Wolff JL, Fried T. Multifactorial Examination of Caregiver Burden in a National Sample of Family and Unpaid Caregivers. J Am Geriatr Soc. 2019;67(2):277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kasper JD, Freedman VA, Spillman BC, Wolff JL. The Disproportionate Impact Of Dementia On Family And Unpaid Caregiving To Older Adults. Health Aff. 2015;34(10):1642–1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ory MG, Hoffman RR, Yee JL, Tennstedt S, Schulz R. Prevalence and Impact of Caregiving: A Detailed Comparison Between Dementia and Nondementia Caregivers. Gerontologist. 1999;39(2):177–186. [DOI] [PubMed] [Google Scholar]
- 23.Phelan EA, Borson S, Grothaus L, Balch S, Larson EB. Association of incident dementia with hospitalizations. Jama. 2012;307(2):165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhao Y, Kuo TC, Weir S, Kramer MS, Ash AS. Healthcare costs and utilization for Medicare beneficiaries with Alzheimer’s. BMC Health Serv Res. 2008;8:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhu CW, Cosentino S, Ornstein K, Gu Y, Andrews H, Stern Y. Use and cost of hospitalization in dementia: longitudinal results from a community-based study. Int J Geriatr Psychiatry. 2015;30(8):833–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bynum JP, Rabins PV, Weller W, Niefeld M, Anderson GF, Wu AW. The relationship between a dementia diagnosis, chronic illness, medicare expenditures, and hospital use. J Am Geriatr Soc. 2004;52(2):187–194. [DOI] [PubMed] [Google Scholar]
- 27.Office of Disease Prevention and Health Promotion, US Department of Health and Human Services. Healthy People 2020: Dementias, Including Alzheimer’s Disease. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/dementias-including-alzheimers-disease/objectives. Accessed April 20, 2020.
- 28.Reilly S, Miranda-Castillo C, Malouf R, et al. Case management approaches to home support for people with dementia. Cochrane Database Syst Rev. 2015;1. doi: 10.1002/14651858.CD008345.pub2. [DOI] [PMC free article] [PubMed]
- 29.Tam-Tham H, Cepoiu-Martin M, Ronksley PE, Maxwell CJ, Hemmelgarn BR. Dementia case management and risk of long-term care placement: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2013;28(9):889–902. [DOI] [PubMed] [Google Scholar]
- 30.Kim Y, Schulz R. Family caregivers’ strains: comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. J Aging Health. 2008;20(5):483–503. [DOI] [PubMed] [Google Scholar]
- 31.Wolff JL, Mulcahy J, Huang J, Roth DL, Covinsky K, Kasper JD. Family Caregivers of Older Adults, 1999–2015: Trends in Characteristics, Circumstances, and Role-Related Appraisal. Gerontologist. 2018;58(6):1021–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Freedman VA, Crimmins EM, Schoeni RF, et al. Resolving Inconsistencies in Trends in Old-Age Disability: Report From a Technical Working Group. Demography. 2004;41(3):417–441. [DOI] [PubMed] [Google Scholar]
- 33.Giovannetti ER, Wolff JL. Cross-survey differences in national estimates of numbers of caregivers of disabled older adults. Milbank Q. 2010;88(3):310–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wolff JL, Mulcahy J, Roth DL, et al. Long-Term Nursing Home Entry: A Prognostic Model for Older Adults with a Family or Unpaid Caregiver. J Am Geriatr Soc. 2018;66(10):1887–1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burgdorf J, Mulcahy J, Amjad H, Kasper JD, Covinsky K, Wolff JL. Family Caregiver Factors Associated With Emergency Department Utilization Among Community-Living Older Adults With Disabilities. J Prim Care Community Heal. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Galvin JE, Roe CM, Powlishta KK, et al. The AD8: a brief informant interview to detect dementia. Neurology. 2005;65(4):559–564. [DOI] [PubMed] [Google Scholar]
- 37.Galvin JE, Roe CM, Xiong C, Morris JC. Validity and reliability of the AD8 informant interview in dementia. Neurology. 2006;67(11):1942–1948. [DOI] [PubMed] [Google Scholar]
- 38.Kasper JD, Freedman VA, Spillman CB. Classification of Persons by Dementia Status in the National Health and Aging Trends Study . Technical Paper #5. Baltimore: Johns Hopkins University School of Public Health; 2013. Available at: www.NHATS.org. Accessed April 20, 2020. [Google Scholar]
- 39.Leggett AN, Polenick CA, Maust DT, Kales HC. Falls and Hospitalizations Among Persons With Dementia and Associated Caregiver Emotional Difficulties. Gerontologist. 2018;58(2):e78–e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rosati RJ, Huang L, Navaie-Waliser M, Feldman PH. Risk factors for repeated hospitalizations among home healthcare recipients. J Healthc Qual. 2003;25(2). 4–10. [DOI] [PubMed] [Google Scholar]
- 41.Schwarz KA, Elman CS. Identification of factors predictive of hospital readmissions for patients with heart failure. Hear Lung J Acute Crit Care. 2003;32(2):88–99. [DOI] [PubMed] [Google Scholar]
- 42.National Research Council (US) Committee on the Role of Human Factors in Home Health Care. The Role of Human Factors in Home Health Care: Workshop Summary. Washington (DC): National Academies Press (US); 2010. [PubMed] [Google Scholar]
- 43.Burgdorf J, Roth DL, Riffin C, Wolff JL. Factors Associated with Receipt of Training among Caregivers of Older Adults. JAMA Intern Med. 2019;179(6):833–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.National Academies of Sciences, Engineering, and Medicine. Families Caring for an Aging America . Washington DC: The National Academies Press, 2016. [PubMed] [Google Scholar]
- 45.Reinhard SC, Young HM, Levine C, et al. Home Alone Revisited: Family Caregivers Providing Complex Care. 2019. Available at: http://www.aarp.org/ppi. Accessed July 13, 2020.
- 46.Burgdorf JG, Arbaje AI, Wolff JL. Training Needs Among Family Caregivers Assisting During Home Health, as Identified by Home Health Clinicians. J Am Med Dir Assoc. Epub ahead of print July 5, 2020. doi: 10.1016/j.jamda.2020.05.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brodaty H, Arasaratnam C. Meta-analysis of nonpharmacological interventions for neuropsychiatric symptoms of dementia. Am J Psychiatry. 2012;169(9):946–953. [DOI] [PubMed] [Google Scholar]
- 48.Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: A systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.CMS. Announcement of Calendar Year (CY) 2019 Medicare Advantage Capitation Rates and Medicare Advantage and Part D Payment Policies and Final Call Letter. 2018. Available at: https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Downloads/Announcement2019.pdf. Accessed June 30, 2020.
- 50.Pinquart M, Sörensen S. Correlates of physical health of informal caregivers: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2007;62(2):126–37. [DOI] [PubMed] [Google Scholar]


