Abstract
In recent years, more than half of all drug overdose deaths in United States involved an opioid. To address this epidemic, antecedents to opioid misuse must be identified and empirically validated. The objective of the current investigation was to examine whether illicit drug use was prospectively associated with nonprescription opioid use among adolescents from a vulnerable population with a greater prevalence of substance abuse. A population-based cohort study of 1060 adolescents from 29 alternative high schools in southern California was conducted over a two-year period. A total of 929 adolescents (mean age 17.5 years, 49.9% female, 76.4% Hispanic) who had not experimented with nonprescription opioids at the baseline assessment were included in the analytic sample. The outcome was self-reported use of nonprescription opioids within two years. The predictors tested were illicit drug use, illicit drug use excluding marijuana, and the use of nonmedical marijuana. Covariates included age, sex, ethnicity, socioeconomic status, parental education, weekly income, sensation seeking, stress, anxiety, depression, and the use of alcohol and nicotine products. Multilevel, covariate-adjusted logistic regression models indicated that the odds of experimentation with nonprescription opioids was greater among adolescents who had used illicit drugs or illicit drugs excluding marijuana. Nonmedical marijuana use alone was a statistically significant predictor in unadjusted but not covariate-adjusted models. While prior studies have examined the progression from nicotine, alcohol, and marijuana use to nonprescription opioid use, the present findings emphasize the importance of illicit drug use as a detectable and empirically supported risk factor for future opioid misuse.
Keywords: Adolescents, drug use, longitudinal, marijuana, opioid
INTRODUCTION1
Every year in the United States, approximately 700,000 youth between the ages of 12 and 17 and nearly 2 million young adults between the ages of 18 and 25 misuse opioids (Substance Abuse and Mental Health Services Administration, 2019). In 2018, 70% of drug overdose deaths in the country involved an opioid (Wilson, Kariisa, Seth, Smith, & Davis, 2020). A nationwide study revealed a 268% increase in pediatric mortality from opioid poisoning over the past two decades, with 88% of the cases among adolescents (Gaither, Shabanova, & Leventhal, 2018). This issue is critically important for behavioral health because nonmedical use of prescription opioids among adolescents has been strongly linked to subsequent heroin use (Kelley-Quon et al., 2019) and is predictive of substance abuse disorder symptoms in middle age (McCabe et al., 2019). To prevent opioid misuse, addiction, and mortality, detectable and actionable antecedents to nonprescription use must be identified and empirically validated. Prior meta-analyses have identified factors with sizable effect sizes, such as psychiatric disorders (Cragg et al., 2019), and results from national surveys have identified antecedents that might function as the focal point of large-scale interventions, such as family support (Edlund et al., 2015). However, few studies have examined antecedents that satisfy both criteria with the notable exception of prescription opioid use.
The link between prescription opioid use and nonprescription use has been well publicized, and there seems little doubt that prescription use poses a risk unless it is carefully monitored, controlled, and limited (McCabe et al., 2019). Yet, a related and potentially strong antecedent of nonprescription opioid use in adolescents has not been sufficiently investigated: illicit drug use. Several plausible explanations for the progression from illicit drug use to nonprescription opioid use exist. From a social network perspective (Dishion & Tipsord, 2011; Eitan, Emery, Bates, & Horrax, 2017; Otten, Mun, & Dishion, 2017), initiation of one form of drug by a teenager almost inevitably exposes the individual to increased availability and social influence from a drug using network. Since illicit drug using networks can be quite heterogeneous with respect to the class of drug used, adolescents using one form of illicit drug may be exposed to opioids and the social dynamics that encourage experimentation. From a biological viewpoint, evidence from animal models (Spear, 2011) suggests that substance use during adolescence, including the use of illicit drugs, may alter the mesolimbic reward pathway as well as multiple frontal cortical regions of the brain resulting in a greater likelihood of experimentation with previously untried drugs. Paired with mammalian studies indicating that illicit substances such as cannabis (Hurd, Michaelides, Miller, & Jutras-Aswad, 2014; Lecca et al., 2020) and ecstasy (Daza-Losada, Rodríguez-Arias, Aguilar, & Miñarro, 2008) may reinforce the effects of opioids while legal substances such as nicotine (Eklund, Nishida, Barry, Choi, & Grunberg, 2019) may not, there is compelling experimental research to warrant a closer examination of the association between the use of illicit drugs and the subsequent use of nonprescription opioids.
Because of scientific plausibility and contemporary importance, this study evaluates whether illicit drug use is a risk factor for nonprescription opioid use among adolescents who had not experimented with opioids but were from a vulnerable population—students referred to alternative high schools (AHS) due to poor academic performance, excessive truancy, or conduct problems resulting in probation or expulsion (Johnson, Morris, Rew, & Simonton, 2016). Mean prevalence rates of substance use and drug addiction are typically higher in these schools than in traditional schools (Johnson, McMorris, & Kubik, 2013; Johnson & Taliaferro, 2012; Sussman, Pokhrel, Sun, Rohrbach, & Spruijt-Metz, 2015), providing sufficient variability to prospectively study risk factors. At the same time, students in these schools are not dramatically different from students who have not yet reached the threshold for referral to an alternative school but exhibit comparable behaviors. Thus, AHS populations are relevant to a range of students at risk for nonprescription opioid use.
METHODS
Sample
Data provided by the California Department of Education were utilized to identify 183 alternative high schools within 100 miles of the program offices in Claremont, California that were attended by a minimum of 100 students. On February 6th, 2014 research staff began contacting each school in a randomly selected order. All schools were invited to participate in accordance with a protocol approved by the Claremont Graduate University Institutional Review Board. Schools were enrolled on a first-come, first-served basis until 29 sites agreed to participate. By June 5th, 2014 each participating school provided a letter confirming their involvement.
Between October 14th, 2014 and May 18th, 2015, research staff visited each school and invited all students to enroll in the study. Interest forms were distributed to 6,870 students who attended the schools. Completed forms were returned by 2,726 students. Each student that returned a form was assigned to a specific staff member. The staff member obtained written consent and provided a link to a web-based survey. Parental consent and youth assent were obtained for students under the age of 18. All students were given until September 1st, 2015 to complete the approximately 90-minute survey. A total of 1,060 students took part in the baseline assessment. This sample size was deemed sufficient based on prior research (Muthén & Curran, 1997; Olvera Astivia, Gadermann, & Guhn, 2019) indicating small to medium effects could be detected when utilizing latent growth curve models (Miller et al., 2020) or the multilevel models employed in the current investigation.
Annual follow-up assessments were administered online (96.7%) and over the phone (3.3%) utilizing evidence-based procedures (McCuller, Sussman, Holiday, Craig, & Dent, 2002) documented in prior publications (Pike et al., 2019). One-year follow-up assessments were conducted between September 21st, 2015 and September 1st, 2016. The average length of time between the baseline assessment and the one-year follow-up assessment was 330 days (SD = 26.6). The retention rate was 87.1% (923/1060).
Two-year follow-up assessments were administered between September 26th, 2016 and September 1st, 2017. The average length of time between the baseline assessment and the two-year follow-up assessment was 695 days (SD = 33.7) and the retention rate was 81.0% (859/1060). At the baseline assessment, 87.6% (929/1060) of students had not experimented with opioids. These students were included in an analytic dataset designed to test whether the use of illicit drugs would be associated with subsequent experimentation with nonprescription opioids.
Measures
Drug Use.
During each assessment, a previously validated measure (Graham et al., 1984) employed in prior studies of substance use among AHS students (Ames, Xie, Shono, & Stacy, 2017) was administered. Students were asked ‘About how many times have you used each of the drugs below in the past year (without a doctor telling you to take them or taking more than a doctor told you to take)?’ The substances listed included opioids (heroin, opium, morphine, etc.), illicit drugs (cocaine, crack, ecstasy, hallucinogens, methamphetamines, tranquilizers, inhalants, ketamine, GHB, etc.), common prescription drugs that may be used illicitly (Ritalin, Adderall, etc.), and drugs legal for adults but illegal for youth to consume (alcohol) or purchase (cigarettes, cigars, etc.). Although recreational cannabis sales were legalized in California on January 1st, 2018 under the Control, Regulate and Tax Adult Use of Marijuana Act, in this investigation nonmedical marijuana was classified as illegal since all assessments were administered before the law was enacted.
For each drug, students indicated whether they had used the substance ‘0 times’, ‘1–10 times’, ‘11–20 times’, ‘21–30 times’, ‘31–40 times’, ‘41–50 times’, ‘51–60 times’, ‘61–70 times’, ‘71–80 times’, ‘81–90 times’, or ‘91+ times’ in the past year. From these responses, dichotomous variables were created (0 = nonuse, 1 = use) for opioid use, nonmedical marijuana use, use of any illicit drug including misuse of marijuana, Ritalin, or Adderall, use of any illicit drug excluding marijuana, and use of drugs legal for adults but not for youth such as nicotine and alcohol.
Socio-Demographic.
Given the documented associations between opioid use and sex (Edlund et al., 2015), Hispanic ethnicity (Edlund et al., 2015; Hudgins, Porter, Monuteaux, & Bourgeois, 2019), and socioeconomic status (Edlund et al., 2015), multiple socio-demographic constructs were measured. Each student reported their sex (0 = female, 1 = male), and ethnicity (0 = non-Hispanic, 1 = Hispanic). Students also provided their birthdate, which was used to calculate their age in years at the baseline assessment. Socioeconomic status was ascertained by three questions that asked students if they received a free lunch at school or if their family received a welfare check or food stamps. Responses were aggregated into a dichotomous variable (0 = no nutritional or financial assistance, 1 = nutritional or financial assistance).
Each student reported the level of education attained by their parent(s). The highest level attained by either parent was incorporated into a single variable comprised of the categories ‘Did not finish high school’, ‘Completed high school’, ‘Some college’, ‘Completed college’, and ‘Completed graduate school’. Average weekly income was assessed utilizing three items adapted from the Monitoring the Future survey (Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2017) that inquired how much money students received from a job, their family, or other sources. For each source of income, students selected from the response options ‘$0’, ‘$1–5’, ‘$6–10’, ‘$11–20’, ‘$21–35’, ‘$36–50’, ‘$51–75’, ‘$76–125’, ‘$126–175’, and ‘$176+’. The mean of all three sources was computed for each student.
Psychological.
Prior reviews and meta-analyses (Cragg et al., 2019; Groenman, Janssen, & Oosterlaan, 2017; Roberti, 2004) have provided strong evidence for an association between psychological characteristics and youth substance use. To adjust for these risk factors, several psychological constructs were measured. Sensation seeking was assessed with a 19-item subscale of the Zuckerman-Kuhlman Personality Questionnaire that was used to assess students’ tendency to act impulsively, take risks, or otherwise engage in experience seeking behavior (Zuckerman, Kuhlman, Joireman, Teta, & Kraft, 1993). The subscale demonstrated good internal reliability (Cronbach’s α = .80) in prior studies (Roberti, Storch, & Bravata, 2003) and comparable properties in the current cohort (α = .82). The subscale presented a series of statements (e.g. ‘I often do things on impulse’). For each statement, students selected ‘True’ if they agreed that the statement described them or ‘False’ if they disagreed. The percentage of ‘True’ responses was computed for each student.
Stress, anxiety, and depression were evaluated by the 21-item Depression Anxiety Stress Scale (DASS-21), which has shown excellent construct validity (Henry & Crawford, 2005) and psychometric properties (α = .93) in adolescent samples (Szabo, 2010). Each student was asked to read seven statements describing feelings of stress (‘I felt that I was using a lot of nervous energy’), anxiety (‘I felt I was close to panic’), or depression (‘I felt that I had nothing to look forward to’) that they might have experienced in the past week. For each statement, the student chose from four response options (0 = Did not apply to me at all, 1 = Applied to me to some degree, or some of the time, 2 = Applied to me to a considerable degree, or a good part of time, or 3 = Applied to me very much, or most of the time). The mean of each 7-item subscale was computed for each student. The subscales of stress (α = .85), anxiety (α = .82), and depression (α = .89) demonstrated good internal reliability.
Analyses
All analyses were executed in SAS 9.4 (SAS Institute, Cary, NC). The analytic sample comprised 929 students from 29 schools. To account for similarities between students attending the same school, generalized linear mixed models were employed to generate subject-specific, conditional likelihood parameter estimates. Unstructured covariance matrices were utilized to estimate school-level random effects. An examination of Akaike’s Information Criterion (AIC) and Bayesian Information Criterion (BIC) revealed that models with random intercepts exhibited a better fit to the data than models with random intercepts and slopes (ΔAIC = −1.52 to −4.94, ΔBIC = −4.50 to −7.91). Consequently, models with random intercepts were utilized in the analyses.
A comparison between students with complete data versus those with missing responses at either the one-year or two-year follow-up assessment revealed no statistically significant differences by ethnicity (77.0% Hispanic vs 75.0% Hispanic) or age (17.5 vs 17.5). Differences in the use of illicit drugs excluding marijuana (19.0% vs 19.1%) and the use of drugs legal for adults (55.3% vs 58.1%) were also not statistically significant. However, students with complete data were less likely to be male (45.8% vs 59.4%) and less likely to use nonmedical marijuana (44.1% vs 55.5%). To minimize biased parameter estimates stemming from informative attrition, multivariate imputation by chained equations (Van Buuren, 2007) was utilized to generate 40 imputed datasets (Graham, Olchowski, & Gilreath, 2007) which exceeded the 8 imputations suggested by a two-stage analysis (von Hippel, 2018). The imputation model included the variables described plus a time variable that assumed students with missing data would have completed their final assessment two years after the baseline assessment.
Multilevel, multivariable logistic regression models were used to analyze the imputed datasets and generate odds ratios (OR) and 95% confidence intervals (CI) depicting the probability that a student who had not used opioids at the baseline assessment would try nonprescription opioids within two years. Model 1 estimated the relationship between nonprescription opioid use and the use of any illicit drug including the misuse of marijuana, Ritalin, or Adderall. Age, sex, ethnicity, socioeconomic status, parental education, and weekly income at the baseline assessment were incorporated into the model as covariates. Model 2 additionally adjusted for sensation seeking, stress, anxiety, and depression. Model 3 adjusted for the use of substances legal for adults such as alcohol and nicotine.
Equivalent logistic regression models separately estimated whether the use of nonmedical marijuana or illicit drugs excluding marijuana were associated with future nonprescription opioid use. A supplemental analysis was performed to facilitate comparisons between ORs from multilevel logistic regression models, risk ratios (RRs) from multilevel modified Poisson regression models, and hazard ratios (HRs) from multilevel discrete time survival models. Parameter estimates from the Poisson regression models were used to examine whether the ratio (RR) between the likelihood of nonprescription opioid use among illicit drug users versus nonusers was similar to the ratio (OR) between the likelihood of nonprescription opioid use to nonuse among illicit drug users versus nonusers. Parameter estimates from discrete time survival models depicted whether the ORs and RRs, which denote risk over the duration of the study, were comparable to the instantaneous risk (HR) at any given time within the study.
Exploratory analyses examining the potential modifying effect of sex and ethnicity were performed by fitting fully-adjusted models that included an interaction with the various permutations of illicit drug use. Two-sided p-values were generated for each interaction and statistical significance was defined as P < .05. Parameter estimates from stratified models were generated to gauge the consistency of ORs, RRs, and HRs across subgroups.
RESULTS
The mean age of students in the analytic sample at the baseline assessment was 17.5 years old (SD = 0.9) as presented in Table 1. The sample was 49.9% (461/924) female, which was greater than the 40.3% (2755/6835) reported by the 29 schools that agreed to participate in the study and the 45.7% (32339/70718) documented in the 183 schools eligible to participate. The sample also had a greater proportion of Hispanic students (76.4%, 690/903) than observed within participating (71.0%, 4851/6835) and eligible (64.1%, 45339/70718) schools. More than three-quarters of the students (78.2%, 708/905) in the sample received some form of nutritional or financial assistance while less than one-fifth (17.2%, 140/813) had a parent who obtained a college degree. Although the sample was restricted to youth who had not experimented with nonprescription opioids at the baseline assessment, the prevalence of illicit drug use remained high at 49.4% (459/929). At the two-year follow-up, 5.2% of the students had experimented with nonprescription opioids.
Table 1.
Characteristics of longitudinal cohort of 929 alternative high school students who did not use nonprescription opioids at the baseline assessment
| Complete Cases (n) | Responses mean (SD) / n (%) | |
|---|---|---|
| Age in Years, mean (SD) | 926 | 17.5 (0.9) |
| Sex, n (%) | ||
| Female | 924 | 461 (49.9) |
| Male | 463 (50.1) | |
| Ethnicity, n (%) | ||
| Hispanic | 903 | 690 (76.4) |
| Non-Hispanic | 213 (23.6) | |
| Socioeconomic Status, n (%) | ||
| Family receives welfare check | 900 | 147 (16.3) |
| Family receives food stamps | 902 | 288 (31.9) |
| Student receives free lunch at school | 905 | 677 (74.8) |
| Highest Education Level of Parent(s), n (%) | ||
| Did not finish high school | 813 | 250 (30.8) |
| Completed high school | 263 (32.3) | |
| Some college | 160 (19.7) | |
| Completed college | 93 (11.4) | |
| Completed graduate school | 47 (5.8) | |
| Weekly Income, n (%) | ||
| 0$ | 879 | 82 (9.3) |
| $1 to $100 | 525 (59.7) | |
| More than $100 | 272 (31.0) | |
| Sensation Seeking, mean (SD) | 927 | 0.4 (0.2) |
| DASS 21: Depression, mean (SD) | 927 | 0.4 (0.6) |
| DASS 21: Anxiety, mean (SD) | 927 | 0.3 (0.5) |
| DASS 21: Stress, mean (SD) | 926 | 0.4 (0.6) |
| Use of Drugs Legal for Adultsa, n (%) | 929 | 522 (56.2) |
| Use of Marijuana, n (%) | 914 | 435 (47.6) |
| Use of Illicit Drugsb Except Marijuana, n (%) | 929 | 177 (19.1) |
| Use of Illicit Drugsb Including Marijuana, n (%) | 929 | 459 (49.4) |
| Use of Opioids, n (%) | ||
| Baseline Assessment | 929 | 0 (0.0) |
| One-Year Follow-Up | 753 | 22 (2.9) |
| Two-Year Follow-up | 713 | 37 (5.2) |
Note: Students were permitted to skip survey questions they did not want to answer. Consequently, the number of complete cases varied for each measure.
Drugs legal for adults in California during the timeframe in which the study was conducted included alcohol, cigarettes, electronic cigarettes, cigars, and smokeless tobacco.
Illicit drugs include the unauthorized use of cocaine, crack, ecstasy, hallucinogens, methamphetamines, tranquilizers, inhalants, Ritalin, Adderall, and club drugs such as ketamine and GHB.
The use of illicit drugs including the misuse of marijuana, Ritalin, and Adderall was positively associated with subsequent opioid misuse in unadjusted models (OR = 2.83, 95% CI = 1.33, 6.01). This medium size effect (Chinn, 2000) was largely unaffected by the addition of socio-demographic (Model 1: OR = 2.93, 95% CI = 1.37, 6.26) and psychological covariates (Model 2: OR = 2.80, 95% CI = 1.29, 6.11) as depicted in Table 2. Parameter estimates for each covariate are documented in the supplemental materials. The association remained statistically significant after adjusting for the use of nicotine and alcohol (Model 3: OR = 2.51, 95% CI = 1.04, 6.08), although the effect size was of a lesser magnitude. A comparable unadjusted association (OR = 2.31, 95% CI = 1.13, 4.71) and pattern of attenuation was observed in models estimating the association between nonmedical marijuana use and nonprescription opioid use. However, the effect of marijuana use alone was no longer statistically significant in the fully-adjusted model (Model 3: OR = 1.88, 95% CI = 0.81, 4.40). Use of any illicit drug excluding marijuana was positively associated with future opioid misuse in both unadjusted (OR = 2.84, 95% CI = 1.44, 5.60) and covariate-adjusted models. This pattern of findings was replicated in models that calculated RRs and HRs. In the fully-adjusted model, the association between illicit drug use excluding marijuana and nonprescription opioid use had an OR of 2.43 (95% CI = 1.10, 5.38), a RR of 2.30 (95% CI = 1.08, 4.87), and a HR of 2.38 (95% CI = 1.11, 5.10). These results indicate (OR) that the odds are more than two times greater that students who use illicit drugs will experiment with opioids within one to two years, (RR) that students who use illicit drugs are more than twice as likely to use nonprescription opioids, and (HR) that the hazard rate of opioid misuse among these students at any given point in time is 238% higher.
Table 2.
Multilevel models examining the relationship between illicit drug use and subsequent nonprescription opioid use among 929 alternative high school students assessed over a two-year timeframe
| Model 1a | Model 2b | Model 3c | |
|---|---|---|---|
| Logistic Regression |
|||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Use of Illicit Drugsd | 2.93 (1.37–6.26) | 2.80 (1.29–6.11) | 2.51 (1.04–6.08) |
| Use of Marijuana | 2.37 (1.15–4.87) | 2.22 (1.06–4.65) | 1.88 (0.81–4.40) |
| Use of Illicit Drugs Except Marijuana | 2.97 (1.48–5.95) | 2.80 (1.32–5.93) | 2.43 (1.10–5.38) |
| Modified Poisson Regression |
|||
| RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Use of Illicit Drugsd | 2.81 (1.34–5.90) | 2.69 (1.26–5.75) | 2.43 (1.03–5.73) |
| Use of Marijuana | 2.30 (1.14–4.63) | 2.16 (1.06–4.43) | 1.86 (0.82–4.21) |
| Use of Illicit Drugs Except Marijuana | 2.78 (1.44–5.36) | 2.62 (1.29–5.35) | 2.30 (1.08–4.87) |
| Discrete Time Survival |
|||
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Use of Illicit Drugsd | 2.85 (1.35–6.00) | 2.74 (1.27–5.87) | 2.46 (1.04–5.81) |
| Use of Marijuana | 2.31 (1.14–4.70) | 2.18 (1.06–4.50) | 1.86 (0.81–4.25) |
| Use of Illicit Drugs Except Marijuana | 2.86 (1.48–5.56) | 2.72 (1.32–5.61) | 2.38 (1.11–5.10) |
Abbreviations: OR = Odds Ratio; RR = Risk Ratio; HR = Hazard Ratio.
Note: Multilevel, multivariable regression models were used to estimate the association between illicit drug use and nonprescription opioid use. Multivariate imputation by chained equations was employed to impute missing data.
Model 1 adjusted for age, sex, ethnicity, socioeconomic status, parental education, and weekly income at the baseline assessment.
Model 2 additionally adjusted for sensation seeking, stress, anxiety, and depression.
Model 3 added the use of drugs legal for adults as a covariate. Drugs legal for adults in California during the timeframe in which the study was conducted included alcohol, cigarettes, electronic cigarettes, cigars, and smokeless tobacco.
Illicit drugs included the unauthorized use of marijuana, cocaine, crack, ecstasy, hallucinogens, methamphetamines, tranquilizers, inhalants, Ritalin, Adderall, and club drugs such as ketamine and GHB.
Neither sex nor ethnicity were statistically significant moderators as presented in Figures 1 and 2. Point estimates were higher among females except in models that examined the prospective association between illicit drug use excluding marijuana and subsequent opioid misuse. Models stratified by ethnicity revealed that the point estimates of Hispanic and non-Hispanic students were comparable. Inferences from these point estimates must interpreted with caution given the overlapping 95% CIs.
Figure 1. Multilevel models examining the relationship between illicit drug use and subsequent nonprescription opioid use stratified by sex.

Abbreviations: OR = Odds Ratio; RR = Risk Ratio; HR = Hazard Ratio.
Note: Stratified, multilevel, multivariable regression models were used to estimate the association between illicit drug use and nonprescription opioid use. Multivariate imputation by chained equations was employed to impute missing data. P values denote the interaction between sex and illicit drug use calculated from models that included all participants. All models adjusted for age, ethnicity, socioeconomic status, parental education, weekly income at the baseline assessment, sensation seeking, stress, anxiety, depression, and the use of drugs legal for adults. Drugs legal for adults in California during the timeframe in which the study was conducted included alcohol, cigarettes, electronic cigarettes, cigars, and smokeless tobacco. Illicit drugs included the unauthorized use of marijuana, cocaine, crack, ecstasy, hallucinogens, methamphetamines, tranquilizers, inhalants, Ritalin, Adderall, and club drugs such as ketamine and GHB.
Figure 2. Multilevel models examining the relationship between illicit drug use and subsequent nonprescription opioid use stratified by ethnicity.
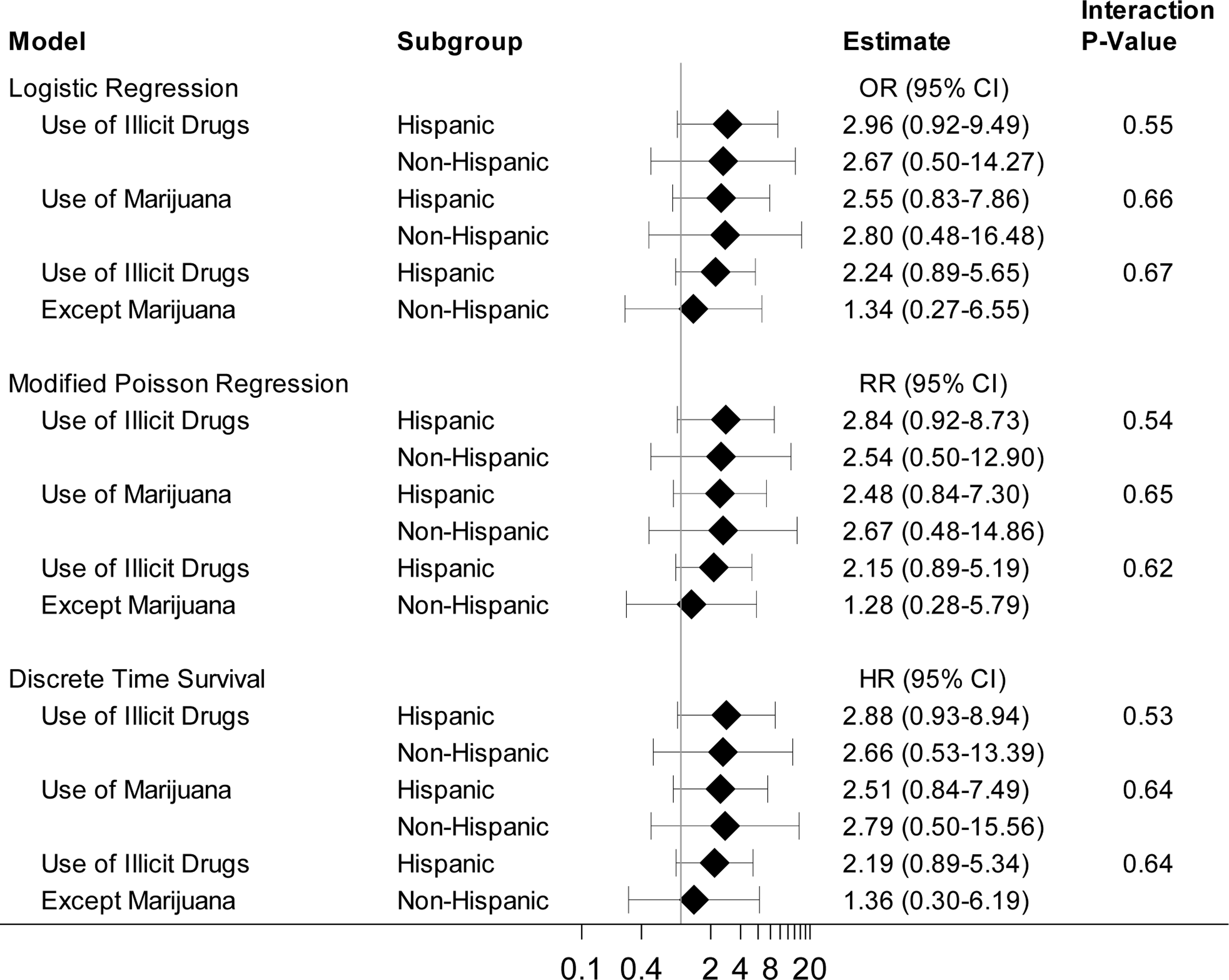
Abbreviations: OR = Odds Ratio; RR = Risk Ratio; HR = Hazard Ratio.
Note: Stratified, multilevel, multivariable regression models were used to estimate the association between illicit drug use and nonprescription opioid use. Multivariate imputation by chained equations was employed to impute missing data. P values denote the interaction between ethnicity and illicit drug use calculated from models that included all participants. All models adjusted for age, sex, socioeconomic status, parental education, weekly income at the baseline assessment, sensation seeking, stress, anxiety, depression, and the use of drugs legal for adults. Drugs legal for adults in California during the timeframe in which the study was conducted included alcohol, cigarettes, electronic cigarettes, cigars, and smokeless tobacco. Illicit drugs included the unauthorized use of marijuana, cocaine, crack, ecstasy, hallucinogens, methamphetamines, tranquilizers, inhalants, Ritalin, Adderall, and club drugs such as ketamine and GHB.
DISCUSSION
The empirical evidence from the current investigation suggests that among vulnerable adolescents illicit drug use is a risk factor for subsequent opioid misuse. Although causality cannot be ascertained given the observational design, both social and biological explanations (Kandel & Kandel, 2015; Otten, Mun, & Dishion, 2017) offer converging and potentially synergistic pathways that support the notion of a causal mechanism. Moreover, even if illicit drug use is merely symptomatic of other intrapersonal or interpersonal risk factors, it may nonetheless be relevant as an early warning sign of opioid use disorders that could be used to improve prevention efforts ranging from informing pediatric prescription practices to identifying youth in need of evidence-based interventions (Das, Salam, Arshad, Finkelstein, & Bhutta, 2016). Practically, illicit drug may serve as a more easily detectable and actionable antecedent to nonprescription opioid use than other established risk factors such as genetic predispositions (Crist, Reiner, & Berrettini, 2019) or childhood trauma (Swedo et al., 2020). Moreover, the medium effect size observed suggests that the use of illicit drugs may be a more powerful predictor of opioid misuse than nicotine and alcohol, which have exhibited small effect sizes in prior studies (Fiellin, Tetrault, Becker, Fiellin, & Hoff, 2013).
Less clear from the current findings is the specific role of nonmedical marijuana use. If subsequent opioid misuse is driven by a biological process documented in pharmacological research (Hurd, Michaelides, Miller, & Jutras-Aswad, 2014; Lecca et al., 2020), then the effects of marijuana may be more relevant than its legal classification. If that is the case, then the recent trend to legalize marijuana in the United States may have the unintended effect of increasing youth marijuana use (Yu, Chen, Chen, & Yan, 2020), which in turn may escalate opioid experimentation and addiction (Hurd, Michaelides, Miller, & Jutras-Aswad, 2014; McCabe, Veliz, Dickinson, Schepis, & Schulenberg, 2019). However, if social network influences (Allen, Donohue, Griffin, Ryan, & Turner, 2003; Hudgins, Porter, Monuteaux, & Bourgeois, 2019) and the increase in drug use opportunities associated with illicit drug using networks (Siegel, Tan, Navarro, Alvaro, & Crano, 2015; Wagner & Anthony, 2002) are primarily responsible for subsequent nonprescription opioid use, then the legal status of marijuana is pertinent. Legalizing marijuana could remove the need for access to illicit drug using networks, which may mitigate opioid abuse and overdose mortality. Preliminary evidence is mixed (Chihuri & Li, 2019; Wong & Lin, 2019), and while the greater effect size associated with illicit drug use excluding marijuana as compared to marijuana use alone suggests that biological mechanisms may not fully explain the transition to nonprescription opioids (Hall & Lynskey, 2005), further research is needed.
Additional scientific research may also address some of the limitations of the current investigation. Compared to 2015 prevalence rates of past-year drug use among 12th graders in the United States (Johnston, O’Malley, Miech, Bachman, & Schulenberg, 2017), students in the analytic sample reported greater use of marijuana (47.6%, vs 34.9%) and illicit drugs other than marijuana (19.1% vs 15.2%). The sample was also predominantly Hispanic, which may have biased effect size estimates (Edlund et al., 2015; Hudgins, Porter, Monuteaux, & Bourgeois, 2019). Thus, the current findings may be most relevant to vulnerable youth populations in California and other geographic regions with a high percentage of Hispanic students.
Another limitation was the relatively small size of the cohort, which resulted in inconclusive subgroup analyses. Given documented sex differences in opioid prescription practices (Friedman et al., 2019) and the rising rate of opioid-related mortality among women (Mack, Jones, & Ballesteros, 2017), additional inquiries into the potential modifying effect of sex are warranted. Equally worthy of scrutiny is whether race and ethnicity do not function as effect modifiers of the relationship between illicit drug use and nonprescription opioid use. If the risks associated with experimentation and the prevalence of nonprescription opioid use are similar across ethnic and racial subgroups (Wu, Woody, Yang, Pan, & Blazer, 2011) but disparities exist in opioid-related mortality rates (Lippold, Jones, Olsen, & Giroir, 2019), then the manner in which nonprescription opioid use is treated within these subgroups should be closely examined.
The current investigation had a limited timespan, which prevented an in-depth analysis of the progression from experimentation to sustained use of nonprescription opioids (Cicero & Ellis, 2017; Guarino, Mateu-Gelabert, Teubl, & Goodbody, 2018) as well as an examination of the impact of marijuana legalization in California (Bachhuber, Saloner, Cunningham, & Barry, 2014; Segura et al., 2019; Smart & Pacula, 2019). Measurement of opioid use within the cohort was also restricted to self-report and did not delineate the types of opioids AHS students preferred. Understanding which substances are accessible to and prevalent among vulnerable youth populations may offer insights into federal and state policies (Soelberg, Brown, Du Vivier, Meyer, & Ramachandran, 2017) that may decrease the availability, addictive potency, and lethality of opioids. A more detailed assessment of illicit drug use, including the misuse of prescription and over-the-counter medications, may also be relevant to identifying behavioral patterns that precede nonprescription opioid use.
CONCLUSION
While further research is needed to elucidate the causal mechanisms through which illicit drug use may lead to nonprescription opioid use, it does not diminish the importance of the central finding that vulnerable youth who use illicit drugs may be at greater risk for misusing opioids. This prospective association is particularly pertinent given that in 2018 an estimated 17 million youth and young adults between the ages of 12 and 25 experimented with illicit drugs (Substance Abuse and Mental Health Services Administration, 2019). Adopting evidence-based approaches in schools (Das, Salam, Arshad, Finkelstein, & Bhutta, 2016; Sun, Skara, Sun, Dent, & Sussman, 2006), healthcare settings (Sterling, Valkanoff, Hinman, & Weisner, 2012), and within the juvenile court system (Chandler, Fletcher, & Volkow, 2009) tailored to youth who have already tried some form of illicit drug may prevent further escalation of drug abuse and mitigate future opioid addiction and mortality.
Supplementary Material
Highlights.
Adolescents who used illicit drugs were more likely to misuse opioids.
The association persisted after adjusting for the use of nicotine and alcohol.
The effect was greater than the effects reported for nicotine and alcohol use.
The effect of marijuana use was smaller than the effect of using other illicit drugs.
Acknowledgments
The authors wish to thank Sandy Asad, Sara J Asad, Melissa Garrido, Sarah Z Gonzalez, Hannah Jornacion, and Brenda Lisa Lucero for their tireless efforts recruiting and tracking alternative high school students. Additional thanks to Jerry Grenard for helping to design the study and refine the central concepts.
Role of Funding Source
Research reported in this publication was supported by the National Institute of Child Health and Human Development and the Food and Drug Administration Center for Tobacco Products (R01HD077560). The content is solely the responsibility of the authors and does not necessarily represent the official views of either institution.
Footnotes
Declarations of Competing Interests
None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Abbreviations: AHS, Alternative High School; AIC, Akaike’s Information Criterion; BIC, Bayesian Information Criterion; CI, Confidence Interval; GHB, Gamma-hydroxybutyrate; HR, Hazard Ratio; OR, Odds Ratio; RR, Risk Ratio; SD, Standard Deviation
REFERENCES
- Allen M, Donohue W, Griffin A, Ryan D, Turner M, 2003. Comparing the influence of parents and peers on the choice to use drugs: a meta-analytic summary of the literature. Crim. Justice Behav. 30(2), 163–186. 10.1177/0093854802251002 [DOI] [Google Scholar]
- Ames S, Xie B, Shono Y, Stacy A, 2017. Adolescents at risk for drug abuse: a 3-year dual-process analysis. Addiction 112(5), 852–863. 10.1111/add.13742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachhuber M, Saloner B, Cunningham C, Barry C, 2014. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Intern. Med. 174(10), 1668–1673. 10.1001/jamainternmed.2014.4005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler R, Fletcher B, Volkow N, 2009. Treating drug abuse and addiction in the criminal justice system: improving public health and safety. JAMA 301(2), 183–190. 10.1001/jama.2008.976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chihuri S, Li G, 2019. State marijuana laws and opioid overdose mortality. Inj. Epidemiol. 6(38). 10.1186/s40621-019-0213-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinn S, 2000. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat. Med. 19(22), 3127–3131. [DOI] [PubMed] [Google Scholar]
- Cicero T, Ellis M, 2017. The prescription opioid epidemic: a review of qualitative studies on the progression from initial use to abuse. Dialogues Clin. Neurosci. 19(3), 259–269. 10.31887/DCNS.2017.19.3/tcicero [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cragg A, Hau J, Woo S, Kitchen S, Liu C, Doyle-Waters M, Hohl C, 2019. Risk factors for misuse of prescribed opioids: A systematic review and meta-analysis. Ann. Emerg. Med. 74(5), 634–646. 10.1016/j.annemergmed.2019.04.019 [DOI] [PubMed] [Google Scholar]
- Crist R, Reiner B, Berrettini W, 2019. A review of opioid addiction genetics. Curr. Opin. Psychol. 27, 31–35. 10.1016/j.copsyc.2018.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das J, Salam R, Arshad A, Finkelstein Y, Bhutta Z, 2016. Interventions for adolescent substance abuse: an overview of systematic reviews. J. Adolesc. Health 59(4 Suppl), S61–S75. 10.1016/j.jadohealth.2016.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daza-Losada M, Rodríguez-Arias M, Aguilar M, Miñarro J, 2008. Effect of adolescent exposure to MDMA and cocaine on acquisition and reinstatement of morphine-induce CPP. Prog. Neuropsychopharmacol. Biol. Psychiatry 32(3), 701–709. 10.1016/j.pnpbp.2007.11.017 [DOI] [PubMed] [Google Scholar]
- Dishion T, Tipsord J, 2011. Peer contagion in child and adolescent social and emotional development. Annu. Rev. Psychol. 62, 189–214. 10.1146/annurev.psych.093008.100412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund M, Forman-Hoffman V, Winder C, Heller D, Kroutil L, Lipari R, Colpe L, 2015. Opioid abuse and depression in adolescents: results from the National Survey on Drug Use and Health. Drug Alcohol Depend. 152, 131–138. 10.1016/j.drugalcdep.2015.04.010 [DOI] [PubMed] [Google Scholar]
- Eitan S, Emery M, Bates M, Horrax C, 2017. Opioid addiction: who are your real friends? Neurosci. Biobehav. Rev. 83, 697–712. 10.1016/j.neubiorev.2017.05.017 [DOI] [PubMed] [Google Scholar]
- Eklund K, Nishida K, Barry E, Choi K, Grunberg N, 2019. Examination of the Gateway Hypothesis in a rat model. Pharmacol. Biochem. Behav. 179, 89–97. 10.1016/j.pbb.2019.02.006 [DOI] [PubMed] [Google Scholar]
- Fiellin L, Tetrault J, Becker W, Fiellin D, Hoff R, 2013. Previous use of alcohol, cigarettes, and marijuana and subsequent abuse of prescription opioids in young adults. J. Adolesc. Health 52(2), 158–163. 10.1016/j.jadohealth.2012.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J, Kim D, Schneberk T, Bourgois P, Shin M, Celious A, Schriger D, 2019. Assessment of racial/ethnic and income disparities in the prescription of opioids and other controlled medications in California. JAMA Intern. Med. 179(4), 469–476. 10.1001/jamainternmed.2018.6721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaither J, Shabanova V, Leventhal J, 2018. US national trends in pediatric deaths from prescription and illicit opioids, 1999–2016. JAMA Netw. Open 1(8), e186558. 10.1001/jamanetworkopen.2018.6558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham J, Flay B, Johnson C, Hansen W, Grossman L, Sobel J, 1984. Reliability of self-report measures of drug use in prevention research: evaluation of the Project SMART questionnaire via the test-retest reliability matrix. J. Drug Educ. 14(2), 175–193. 10.2190/Cyv0-7dpb-Djfa-Ej5u [DOI] [PubMed] [Google Scholar]
- Graham J, Olchowski A, Gilreath T, 2007. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prev. Sci. 8(3), 206–213. 10.1007/s11121-007-0070-9 [DOI] [PubMed] [Google Scholar]
- Groenman A, Janssen T, Oosterlaan J, 2017. Childhood psychiatric disorders as risk factor for subsequent substance abuse: a meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry 56(7), 556–569. 10.1016/j.jaac.2017.05.004 [DOI] [PubMed] [Google Scholar]
- Guarino H, Mateu-Gelabert P, Teubl J, Goodbody E, 2018. Young adults’ opioid use trajectories: from nonmedical prescription opioid use to heroin, drug injection, drug treatment and overdose. Addict. Behav. 86, 118–123. 10.1016/j.addbeh.2018.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, Lynskey M, 2005. Is cannabis a gateway drug? Testing hypotheses about the relationship between cannabis use and the use of other illicit drugs. Drug Alcohol Rev. 24(1), 39–48. 10.1080/09595230500126698 [DOI] [PubMed] [Google Scholar]
- Henry J, Crawford J, 2005. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 44(2), 227–239. 10.1348/014466505X29657 [DOI] [PubMed] [Google Scholar]
- Hudgins J, Porter J, Monuteaux M, Bourgeois F, 2019. Prescription opioid use and misuse among adolescents and young adults in the United States: a national survey study. PLoS Med. 16(11), e1002922. 10.1371/journal.pmed.1002922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurd Y, Michaelides M, Miller M, Jutras-Aswad D, 2014. Trajectory of adolescent cannabis use on addiction vulnerability. Neuropharmacology 76, 416–424. 10.1016/j.neuropharm.2013.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K, Taliaferro L, 2012. Health behaviors and mental health of students attending alternative high schools: a review of the research literature. J. Spec. Pediatr. Nurs. 17(2), 79–97. 10.1111/j.1744-6155.2011.00311.x [DOI] [PubMed] [Google Scholar]
- Johnson K, McMorris B, Kubik M, 2013. Comparison of health-risk behaviors among students attending alternative and traditional high schools in Minnesota. J. Sch. Nurs. 29(5), 343–352. 10.1177/1059840512469409 [DOI] [PubMed] [Google Scholar]
- Johnson K, Morris M, Rew L, Simonton A, 2016. A systematic review of consent procedures, participation rates, and main findings of health-related research in alternative high schools from 2010 to 2015. J. Sch. Nurs. 32(1), 20–31. 10.1177/1059840515620841 [DOI] [PubMed] [Google Scholar]
- Johnston L, O’Malley P, Miech R, Bachman J, Schulenberg J, 2017. Monitoring the Future national survey results on drug use, 1975–2016: overview, key findings on adolescent drug use. Ann Arbor, MI: Institute for Social Research, The University of Michigan. [Google Scholar]
- Kandel D, Kandel E, 2015. The Gateway Hypothesis of substance abuse: developmental, biological and societal perspectives. Acta Paediatr. 104(2), 130–137. 10.1111/apa.12851 [DOI] [PubMed] [Google Scholar]
- Kelley-Quon L, Cho J, Strong D, Miech R, Barrington-Trimis J, Kechter A, Leventhal A, 2019. Association of nonmedical prescription opioid use with subsequent heroin use initiation in adolescents. JAMA Pediatr. 173(9), e191750. 10.1001/jamapediatrics.2019.1750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecca D, Scifo A, Pisanu A, Valentini V, Piras G, Sil A, Cadoni C, Di Chiara G, 2020. Adolescent cannabis exposure increases heroin reinforcement in rats genetically vulnerable to addiction. Neuropharmacology, 166, 107974. 10.1016/j.neuropharm.2020.107974 [DOI] [PubMed] [Google Scholar]
- Lippold K, Jones C, Olsen E, Giroir B, 2019. Racial/ethnic and age group differences in opioid and synthetic opioid-involved overdose deaths among adults aged ≥18 years in metropolitan areas - United States, 2015–2017. Morb. Mortal. Wkly. 68(43), 967–973. 10.15585/mmwr.mm6843a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack K, Jones C, Ballesteros M, 2017. Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan areas - United States. MMWR Surveill. Summ. 66(SS-19), 1–12. 10.15585/mmwr.ss6619a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe S, Veliz P, Boyd C, Schepis T, McCabe V, Schulenberg J, 2019. A prospective study of nonmedical use of prescription opioids during adolescence and subsequent substance use disorder symptoms in early midlife. Drug Alcohol Depend. 194, 377–385. 10.1016/j.drugalcdep.2018.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe S, Veliz P, Dickinson K, Schepis T, Schulenberg J, 2019. Trajectories of prescription drug misuse during the transition from late adolescence into adulthood in the USA: a national longitudinal multicohort study. Lancet Psychiatry 6(10), 840–850. 10.1016/S2215-0366(19)30299-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCuller W, Sussman S, Holiday K, Craig S, Dent C, 2002. Tracking procedures for locating high-risk youth. Eval. Health Prof. 25(3), 345–362. 10.1177/0163278702025003006 [DOI] [PubMed] [Google Scholar]
- Miller S, Pike J, Shono Y, Beleva Y, Xie B, Stacy A, 2020. The role of negative affect in the persistence of nicotine dependence among alternative high school students: a latent growth curve analysis. Drug Alcohol Depend. 209, 107883. 10.1016/j.drugalcdep.2020.107883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, Curran P, 1997. General longitudinal modeling of individual differences in experimental designs: a latent variable framework for analysis and power estimation. Psychol. Methods 2(4), 371–402. 10.1037/1082-989X.2.4.371 [DOI] [Google Scholar]
- Olvera Astivia O, Gadermann A, Guhn M, 2019. The relationship between statistical power and predictor distribution in multilevel logistic regression: a simulation-based approach. BMC Med. Res. Methodol. 19(1), 97 10.1186/s12874-019-0742-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otten R, Mun C, Dishion T, 2017. The social exigencies of the gateway progression to the use of illicit drugs from adolescence into adulthood. Addict. Behav. 73, 144–150. 10.1016/j.addbeh.2017.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pike J, Tan N, Miller S, Cappelli C, Xie B, Stacy A, 2019. The effect of e-cigarette commercials on youth smoking: a prospective study. Am. J. Health Behav. 43(6), 1103–1118. 10.5993/AJHB.43.6.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberti J, 2004. A review of behavioral and biological correlates of sensation seeking. J. Res. Pers. 38(3), 256–279. 10.1016/S0092-6566(03)00067-9 [DOI] [Google Scholar]
- Roberti J, Storch E, Bravata E, 2003. Further psychometric support for the Sensation Seeking Scale--Form V. J. Pers. Assess. 81(3), 291–292. 10.1207/S15327752JPA8103_12 [DOI] [PubMed] [Google Scholar]
- Segura L, Mauro C, Levy N, Khauli N, Philbin M, Mauro P, Martins S, 2019. Association of US medical marijuana laws with nonmedical prescription opioid use and prescription opioid use disorder. JAMA Netw. Open 2(7), e197216. 10.1001/jamanetworkopen.2019.7216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel J, Tan C, Navarro M, Alvaro E, Crano W, 2015. The power of the proposition: frequency of marijuana offers, parental knowledge, and adolescent marijuana use. Drug Alcohol Depend. 148, 34–39. 10.1016/j.drugalcdep.2014.11.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart R, Pacula R, 2019. Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: findings from state policy evaluations. Am. J. Drug Alcohol Abuse 45(6), 644–663. 10.1080/00952990.2019.1669626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soelberg C, Brown RJ, Du Vivier D, Meyer J, Ramachandran B, 2017. The US opioid crisis: current federal and state legal issues. Anesth. Analg. 125(5), 1675–1681. 10.1213/ANE.0000000000002403 [DOI] [PubMed] [Google Scholar]
- Spear L, 2011. Rewards, aversions and affect in adolescence: emerging convergences across laboratory animal and human data. Dev. Cogn. Neurosci. 1(4), 392–400. 10.1016/j.dcn.2011.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling S, Valkanoff T, Hinman A, Weisner C, 2012. Integrating substance use treatment into adolescent health care. Curr. Psychiatry Rep. 14(5), 453–461. 10.1007/s11920-012-0304-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2019. Key substance use and mental health indicators in the United States: results from the 2018 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Sun W, Skara S, Sun P, Dent C, Sussman S, 2006. Project Towards No Drug Abuse: long-term substance use outcomes evaluation. Prev. Med. 42(3), 188–192. 10.1016/j.ypmed.2005.11.011 [DOI] [PubMed] [Google Scholar]
- Sussman S, Pokhrel P, Sun P, Rohrbach L, Spruijt-Metz D, 2015. Prevalence and co-occurrence of addictive behaviors among former alternative high school youth: a longitudinal follow-up study. J. Behav. Addict. 4(3), 189–194. 10.1556/2006.4.2015.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swedo E, Sumner S, de Fijter S, Werhan L, Norris K, Beauregard J, Montgomery MP, Rose E, Hillis S, Massetti G, 2020. Adolescent opioid misuse attributable to adverse childhood experiences. J. Pediatr. 224, 102–109. 10.1016/j.jpeds.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabo M, 2010. The short version of the Depression Anxiety Stress Scales (DASS-21): factor structure in a young adolescent sample. J. Adolesc. 33(1), 1–8. 10.1016/j.adolescence.2009.05.014 [DOI] [PubMed] [Google Scholar]
- Van Buuren S, 2007. Multiple imputation of discrete and continuous data by fully conditional specification. Stat. Methods. Med. Res. 16(3), 219–242. 10.1177/0962280206074463 [DOI] [PubMed] [Google Scholar]
- von Hippel P, 2018. How many imputations do you need? A two-stage calculation using a quadratic rule. Sociol. Methods. Res. 1–20. 10.1177/0049124117747303 [DOI] [Google Scholar]
- Wagner F, Anthony J, 2002. Into the world of illegal drug use: exposure opportunity and other mechanisms linking the use of alcohol, tobacco, marijuana, and cocaine. American Int. J. Epidemiol. 155(10), 918–925. 10.1093/aje/155.10.918 [DOI] [PubMed] [Google Scholar]
- Wilson N, Kariisa M, Seth P, Smith H, Davis N, 2020. Drug and opioid-involved overdose deaths — United States, 2017–2018. Morb. Mortal. Wkly. 69, 290–297. 10.15585/mmwr.mm6911a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S, Lin H, 2019. Medical marijuana legalization and associated illicit drug use and prescription medication misuse among adolescents in the U.S. Addict. Behav. 90, 48–54. 10.1016/j.addbeh.2018.10.017 [DOI] [PubMed] [Google Scholar]
- Wu L, Woody G, Yang C, Pan J, Blazer D, 2011. Racial/ethnic variations in substance-related disorders among adolescents in the United States. Arch. Gen. Psychiatry 68(11), 1176–1185. 10.1001/archgenpsychiatry.2011.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu B, Chen X, Chen X, Yan H, 2020. Marijuana legalization and historical trends in marijuana use among US residents aged 12–25: results from the 1979–2016 national survey on drug use and health. BMC Public Health, 20(1), 156 10.1186/s12889-020-8253-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman M, Kuhlman D, Joireman J, Teta P, Kraft M, 1993. A comparison of three structural models for personality: the big three, the big five, and the alternative five. J. Pers. Soc. Psychol. 65(4), 757–768. 10.1037/0022-3514.65.4.757 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


