Abstract
Objectives
The novel coronavirus disease 2019 (COVID-19) resulting from severe acute respiratory syndrome coronavirus 2 began to affect the United States in early 2020. This study aimed to assess the US public’s initial understanding about the disease and virus to inform public health communication efforts.
Methods
We conducted a survey of US households from February 28 through March 2, 2020, using a probability-based web-panel survey of 1021 US residents. To assess knowledge about COVID-19, we asked respondents a series of 16 true/false questions. We conducted descriptive statistics and linear regression analyses to examine differences in knowledge scores based on demographic and background characteristics.
Results
Knowledge about COVID-19 and the virus was relatively low overall at the beginning of the outbreak, with average scores of 62% on a 16-item knowledge index (ie, answers for 6 of the 16 questions were incorrect or unknown). Knowledge was especially low among people who had low education and income levels, were unemployed, were Hispanic, were non-Hispanic Black, were aged 18-24 and 35-49, indicated having “other” health insurance, and had limited exposure to information about the pandemic. Non-Hispanic Black respondents were less knowledgeable about COVID-19 and the virus at every education level compared with non-Hispanic White respondents at higher education levels. Non-Hispanic Black respondents with <high school degree were the least knowledgeable of all subgroups.
Conclusions
The findings of our study highlight the need for widespread, ongoing public health education about the virus and COVID-19, especially among certain populations. It is critical to effectively translate complex clinical and epidemiologic evidence into messages that most people can understand and act on during a pandemic, that combat misinformation about the virus and COVID-19, and that consider low levels of health literacy.
Keywords: COVID-19, public health communication, public understanding of science, disparities, pandemic, emerging infectious disease
In early 2020, much of the world was focused on news about the novel coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The epicenter of the outbreak was in Wuhan, Hubei Province, China. On January 30, 2020, the World Health Organization declared the novel coronavirus outbreak a Public Health Emergency of International Concern.1 In the United States, the first confirmed case of travel-associated COVID-19 was reported on January 20, 2020,2 and the first media statement of a COVID-19–related death in the United States appeared on February 29, 2020.3 On March 13, 2020, the President of the United States declared a national emergency.4
The challenges of educating and communicating with the public about a pandemic of a novel viral pathogen and new disease are substantial. In late February and early March, the scientific understanding of COVID-19 and SARS-CoV-2 was limited, including lack of clarity about how the virus is transmitted, the incubation period, peak infectiousness, risk factors, basic epidemiology, and effective transmission prevention. Findings from the early outbreak in Wuhan showed that some groups were at increased risk of serious complications, hospitalization, and death from COVID-19, including people aged >60 and people with underlying health conditions, such as diabetes, hypertension, cancer, cardiovascular disease, and chronic respiratory diseases.5-7
Research from previous viral outbreaks of novel pathogens identified knowledge gaps in transmission and prevention. A systematic review of community knowledge about the 2009 pandemic influenza A (H1N1) found that knowledge about transmission of the virus was “moderate” and knowledge about prevention was “reasonable.” However, levels of knowledge differed for certain subgroups. Knowledge about H1N1 was highest for people in older age groups, with higher education levels, and higher socioeconomic status than among people who were younger and had lower education levels and socioeconomic status.8 One study found that although much of the public had a good understanding of H1N1 and how to prevent contracting it, gaps in knowledge about transmission and signs and symptoms of the virus existed for people whose income and education levels were low and who reported their race as non-White.9
Effective communication about a new virus and associated disease is paramount for reducing morbidity and mortality and helping communities prepare for an outbreak and prevent transmission. The objective of this study was to elucidate what US residents did and did not understand about the virus and COVID-19 to help inform health communications campaigns. We assessed (1) what the general public knows and does not know about COVID-19 and (2) how this knowledge differs for vulnerable populations, including racial/ethnic minority groups, people with low levels of education or income, and people without health insurance.
Methods
To examine knowledge, we conducted a survey of US households from February 28 through March 2, 2020, using a prerecruited, address-based web panel consisting of 55 000 members. The panel is based on probability sampling of the US population. Households received a computer and/or internet access if needed to participate in the panel. The resulting sample includes households with listed and unlisted telephone numbers, telephone and nontelephone households, cell phone–only households, and households with and without internet access. The survey was conducted in English.
To assess knowledge about the virus and COVID-19, we asked respondents a series of 16 true/false questions. We calculated a mean knowledge index score as the number of items answered correctly, with values ranging from 0% to 100%. We developed the questions based on the existing scientific evidence available from authoritative sources at the time of the survey, including the Centers for Disease Control and Prevention10 and the World Health Organization.5 The knowledge index had a Cronbach α11 of .85, indicating high internal consistency.
We also asked participants to respond to the following statement, “I know what actions to take to prevent myself and my family from becoming infected with the coronavirus” using a 4-point Likert scale (from 1 = strongly agree to 4 = strongly disagree) and the following question, “How much have you seen, read, or heard about the coronavirus first detected in Wuhan, China?” (1 = a great deal, 2 = a fair amount, 3 = not very much, 4 = nothing at all). We also collected information from all respondents on age (18-24, 25-34, 35-49, 50-64, ≥65), sex (male, female), education (<high school graduate, high school graduate, some college, ≥bachelor’s degree), annual household income (<$25 000, $25 000-$49 999, $50 000-$99 999, $100 000-$149 999, ≥$150 000), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic “other”), and region of the country (Midwest, South, West, Northeast). In this analysis, race/ethnicity are combined. The data set also included responses to questions about current employment (employed, unemployed), self-reported health status (excellent/very good, good, fair/poor, unknown), type of health insurance (employer/union, Medicaid, Medicare/Veterans Affairs, other, none, unknown), and which sources of health information respondents had used in the past 12 months (eg, physician, relative/friend/coworker, social media, newspaper).
At the end of the survey, participants were told that the purpose of the survey was to understand what people in the United States do and do not know about the virus and COVID-19 and that some of the information on true/false questions was in fact false. To prevent misinformation, respondents were encouraged to learn what is known about how to protect themselves and their families from getting infected. All 1021 respondents received a link to the CDC website.
The panel provider drew a random sample of 2857 members from the panel. A total of 1021 (excluding respondents who did not complete the survey) adults aged ≥18 responded to the invitation, all of whom qualified for the survey, yielding a final stage completion rate of 36%. Once the survey sample was selected and fielded and all the study data were collected and finalized, the panel provider used a poststratification process to adjust for survey nonresponse and for any noncoverage, undersampling, or oversampling resulting from the study-specific sample design based on the Current Population Survey12 and weighted all respondents to these distributions. The panel provider scaled the sample size to the number of qualified respondents and used the following benchmark distributions for this poststratification adjustment: sex, age, race/ethnicity, education level, geographic region, annual household income, metropolitan area, and homeownership status.
We conducted the Rao-Scott χ2 test of significance and linear regression analyses to examine differences in knowledge scores and other survey questions based on the following demographic and background characteristics: sex; age; education; annual household income; employment status; race/ethnicity; self-reported health status; type of health insurance; geographic region; the amount of information seen, read, or heard about “the coronavirus”; and the number of sources of health information. Reference groups were female, age ≥65, bachelor’s degree, annual household income ≥$150 000, being employed, non-Hispanic White, excellent/very good health, employer-sponsored/union health insurance, residing in the West, and reporting “a great deal of information about the coronavirus.” In addition to the main effects regression model, we tested for possible interactions between demographic characteristics to identify potentially vulnerable subgroups. We modeled differences in overall knowledge and differences within categories or knowledge domains. We report 95% CIs for coefficients and considered P < .05 to be significant. We incorporated survey weights into the analyses, and we conducted all analyses using SAS version 9.3 (SAS Institute Inc).
The RTI International Institutional Review Board reviewed the study protocol and determined it to be exempt from human subjects approval.
Results
The distribution of the survey participants across sociodemographic characteristics and health-related variables suggests that a nationally representative sample was achieved (Table 1). Most respondents had seen, read, or heard about COVID-19: 50% (weighted n = 496) of respondents reported a fair amount of knowledge and 36% (weighted n = 364) reported a great deal of knowledge. We found significant differences in how much respondents had seen, read, or heard about COVID-19 by age, education, annual household income, and health insurance. A significantly higher percentage of non-Hispanic Black respondents than non-Hispanic White respondents answered “not very much/nothing at all” (23% vs 12%), χ2(2) = 14.0, P = .01.
Table 1.
Sociodemographic characteristics of respondents to a survey about COVID-19 knowledge (N = 1021), United States, February 28–March 2, 2020a
| Characteristic | Unweighted | Weightedb |
|---|---|---|
| No. (%)c | No. (%)c | |
| Sex | ||
| Male | 514 (50) | 484 (48) |
| Female | 507 (50) | 516 (52) |
| Age, y | ||
| 18-24 | 107 (10) | 127 (13) |
| 25-34 | 154 (15) | 153 (15) |
| 35-49 | 255 (25) | 248 (25) |
| 50-64 | 283 (28) | 268 (26) |
| ≥65 | 222 (22) | 211 (21) |
| Race/ethnicity | ||
| Non-Hispanic White | 722 (71) | 632 (63) |
| Non-Hispanic Black | 95 (9) | 118 (12) |
| Hispanic | 123 (12) | 164 (16) |
| Non-Hispanic other | 81 (8) | 86 (9) |
| Education | ||
| ≥Bachelor degree | 417 (41) | 323 (33) |
| Some college | 282 (28) | 278 (28) |
| High school graduate | 258 (25) | 283 (28) |
| <High school graduate | 64 (6) | 106 (11) |
| Annual household income, $ | ||
| <25 000 | 119 (12) | 135 (14) |
| 25 000-49 999 | 158 (15) | 182 (18) |
| 50 000-99 999 | 328 (32) | 307 (31) |
| 100 000-149 999 | 197 (19) | 170 (17) |
| ≥150 000 | 219 (21) | 206 (21) |
| Employment status | ||
| Employed | 687 (67) | 656 (66) |
| Unemployed | 334 (33) | 344 (34) |
| Health insurance | ||
| Employer/union | 524 (51) | 484 (48) |
| Medicaid | 190 (19) | 183 (18) |
| Medicare/Veterans Affairs | 55 (5) | 69 (7) |
| Other | 71 (7) | 74 (7) |
| None | 62 (6) | 71 (7) |
| Unknown | 119 (12) | 120 (12) |
| Self-reported health status | ||
| Excellent/very good | 493 (48) | 467 (47) |
| Good | 322 (32) | 315 (31) |
| Fair/poor | 131 (13) | 139 (14) |
| Unknown | 75 (7) | 79 (8) |
| Geographic region | ||
| Midwest | 243 (24) | 208 (21) |
| South | 351 (34) | 379 (38) |
| West | 236 (23) | 238 (24) |
| Northeast | 191 (19) | 175 (18) |
| How much have you seen, read, or heard about the coronavirus first detected in Wuhan, China? | ||
| A great deal | 380 (37) | 364 (36) |
| A fair amount | 512 (50) | 496 (50) |
| Not very much/nothing at all | 128 (13) | 139 (14) |
| Unknown | 1 (0) | 1 (0) |
aData source: RTI International–funded survey on coronavirus disease 2019 (COVID-19).
bSurvey weights were calculated to represent the US population based on estimates from the Current Population Survey.12
cSome percentages do not sum to 100 because of rounding.
The mean score on the 16-item knowledge index was 61.7% (95% CI, 59.9%-63.4%; Table 2). The percentage of correct responses for the 16 questions ranged from 36.2% to 90.3%, with a sizeable proportion of respondents indicating that they did not know the correct answer to several questions (the source of the correct answer is noted after each question). US residents had knowledge gaps about the potential severity and associated mortality of COVID-19: 58.8% knew that most people would recover after getting the virus, and 40.5% were either incorrect (9.7%) or did not know the answer (30.8%). About one-third (32.6%) of respondents incorrectly believed (11.9%) or did not know (20.7%) that most people would die from getting the virus, and 63.1% of respondents were unclear that most people who are infected would have only mild symptoms (25.0% answered incorrectly and 38.1% did not know).
Table 2.
Sixteen-item knowledge index and percentage correct and incorrect, by knowledge domain, in a survey about COVID-19 (N = 1021), United States, February 28–March 2, 2020a
| Survey question (answer) | Correct | Incorrect | Don’t know |
|---|---|---|---|
| Most people who are infected with the coronavirus only have mild symptoms (True)13 | 36.2 | 25.0 | 38.1 |
| Most people who are infected with the coronavirus recover from it (True)13 | 58.8 | 9.7 | 30.8 |
| Most people who are infected with the coronavirus die from it (False)13 | 66.6 | 11.9 | 20.7 |
| People of all racial and ethnic groups can become infected with the coronavirus (True)14 | 88.8 | 2.3 | 8.3 |
| People of all ages can become infected with the coronavirus (True)15 | 90.3 | 2.0 | 6.8 |
| The coronavirus is spread through coughing and sneezing (True)13 | 77.6 | 2.9 | 18.5 |
| The coronavirus is very contagious (True)13 | 82.1 | 3.0 | 14.1 |
| Antibiotics can be used to treat the coronavirus (False)16 | 45.6 | 14.4 | 39.3 |
| Antibiotics can be used to prevent infection from the coronavirus (False)16 | 57.2 | 7.0 | 34.9 |
| A vaccine is now available to prevent infection from the coronavirus (False)16 | 68.3 | 4.1 | 26.9 |
| You can become infected with the coronavirus by touching a package sent from China (False)15 | 42.8 | 13.2 | 43.1 |
| The coronavirus was deliberately created (False)17 | 43.2 | 11.7 | 44.4 |
| Spraying alcohol or chlorine on your body kills the coronavirus (False)15 | 48.7 | 6.4 | 43.9 |
| Rinsing your nose with saline prevents infection from coronavirus (False)15 | 52.2 | 3.7 | 43.4 |
| Hand dryers are effective at killing the coronavirus (False)15 | 59.1 | 4.3 | 35.7 |
| Eating garlic can lower your chances of getting infected with the coronavirus (False)15 | 62.6 | 2.9 | 33.7 |
aData source: RTI International–funded survey on coronavirus disease 2019 (COVID-19). All values are percentages. Some percentages do not sum to 100 because of rounding. Overall mean knowledge index score is 61.7% correct (95% CI, 59.9%-63.4%).
Most people understood that the virus can affect people of all ages (90.3%) and racial/ethnic groups (88.8%), but some did not. About 1 in 5 respondents did not know that coughing and sneezing can spread the virus (2.9% incorrect, 18.5% did not know) and that it is very contagious (3.0% incorrect, 14.1% did not know). Most respondents thought a vaccine was available (68.3%) or were not sure (26.9%). Some respondents believed that certain behaviors would protect them from the virus and others were unsure; for example, 40.0% of respondents did not know that hand dryers were ineffective at killing the virus (3.7% answered incorrectly, 43.4% did not know), and 50.3% of respondents either believed or did not know that spraying alcohol or chlorine on your body would not kill the virus.
COVID-19 knowledge was lower for some subgroups than for others based on the regression models. For example, people who had lower education levels (eg, some college vs a bachelor’s degree (β = –4.14; SE = 1.89; P = .03), had lower income levels (eg, annual household income <$50 000 vs $≥150 000; β = –8.95; SE = 2.62; P < .001), were unemployed versus employed (β = –3.91; SE = 1.99; P = .49), were Hispanic (β = –7.19; SE = 2.46; P = .004) or non-Hispanic Black (β = –13.88; SE = 2.76; P < .001) versus non-Hispanic White, were younger (eg, 18-24 vs ≥65; β = –9.48; SE = 3.89; P = .02), indicated having “other” health insurance versus private health insurance (β = –6.23; SE = 2.86; P = .03), and had limited exposure to information about the pandemic (eg, exposed to not very much/nothing at all vs a great deal; β = –17.78; SE = 2.89; P < .001; Table 3).
Table 3.
Regression models of knowledge index scores, by knowledge domain, in a survey of knowledge about COVID-19 (N = 1021), United States, February 28–March 2, 2020a
| Characteristic | Coefficient (SE) [P value]b | |||||
|---|---|---|---|---|---|---|
| Overall | Severity and mortality | Susceptibility | Transmission | Vaccines and treatment | Misinformation | |
| Sex | ||||||
| Male | 2.20 (1.54) [.15] | 6.89 (2.30) [.003] | 3.33 (1.94) [.09] | 2.90 (2.34) [.22] | 2.61 (2.53) [.30] | –0.97 (2.20) [.66] |
| Female | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Age, y | ||||||
| 18-24 | –9.48 (3.89) [.02] | –11.02 (5.33) [.04] | –6.73 (5.22) [.20] | –0.35 (5.64) [.95] | –12.46 (6.40) [.05] | –11.17 (5.29) [.04] |
| 25-34 | –5.43 (3.17) [.09] | –1.76 (4.75) [.71] | –1.93 (3.98) [.63] | 2.18 (4.62) [.64] | –7.05 (5.31) [.18] | –10.16 (4.54) [.03] |
| 35-49 | –7.14 (2.82) [.01] | –3.90 (4.46) [.38] | –1.92 (3.25) [.56] | 5.55 (3.93) [.16] | –13.30 (4.73) [.01] | –11.64 (4.12) [.01] |
| 50-64 | –3.97 (2.50) [.11] | 0.90 (4.05) [.82] | 1.04 (2.83) [.71] | 4.71 (3.63) [.20] | –6.79 (4.25) [.11] | –9.57 (3.74) [.01] |
| ≥65 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Race/ethnicity | ||||||
| Non-Hispanic White | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Non-Hispanic Black | –13.88 (2.76) [<.001] | –22.76 (4.06) [<.001] | –6.62 (3.93) [.09] | –11.50 (4.61) [.01] | –18.44 (4.39) [<.001] | –10.37 (3.74) [.01] |
| Hispanic | –7.19 (2.46) [.004] | –14.76 (3.65) [<.001] | 5.58 (3.02) [.07] | 0.20 (3.87) [.96] | –11.27 (4.16) [.01] | –8.09 (3.53) [.02] |
| Non-Hispanic other | –4.63 (3.28) [.16] | –10.76 (4.61) [.02] | –5.35 (4.48) [.23] | 1.47 (4.55) [.75] | –5.55 (5.25) [.29] | –2.88 (4.64) [.54] |
| Education | ||||||
| <High school graduate | –16.56 (3.83) [<.001] | –27.98 (5.79) [<.001] | –14.59 (5.85) [.01] | –4.96 (5.87) [.40] | –19.39 (6.27) [.002] | –13.96 (4.68) [.003] |
| High school graduate | –1.30 (2.18) [<.001] | –19.11 (3.41) [<.001] | –3.97 (2.52) [.12] | 0.12 (3.06) [.97] | –17.66 (3.61) [<.001] | –15.04 (3.24) [<.001] |
| Some college | –4.14 (1.89) [.03] | –9.96 (3.02) [.001] | 0.10 (2.29) [.96] | –0.12 (2.77) [.97] | –1.82 (3.21) [.57] | –5.15 (2.65) [.05] |
| ≥Bachelor’s degree | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Annual household income, $ | ||||||
| <50 000 | –8.95 (2.62) [<.001] | –14.98 (4.22) [<.001] | –5.78 (3.40) [.09] | –8.29 (3.82) [.03] | –11.13 (4.38) [.01] | –6.14 (3.58) [.09] |
| 50 000-99 999 | –6.20 (1.99) [.002] | –4.51 (3.22) [.16] | –1.36 (2.40) [.57] | –6.30 (2.99) [.04] | –7.19 (3.42) [.04] | –8.12 (2.88) [.01] |
| 100 000-149 999 | –3.56 (2.21) [.11] | –8.34 (3.54) [.02] | –1.87 (2.33) [.42] | –0.66 (3.03) [.83] | 0.75 (3.57) [.83] | –4.84 (3.23) [.13] |
| ≥150 000 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Employment status | ||||||
| Unemployed | –3.91 (1.99) [.049] | –1.12 (2.93) [.70] | –1.40 (2.56) [.59] | –1.55 (2.94) [.60] | –2.48 (3.10) [.42] | –7.65 (2.72) [.01] |
| Employed | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Health insurance | ||||||
| Employer/union | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Medicaid | –6.03 (3.67) [.10] | –4.83 (6.20) [.44] | –3.18 (5.26) [.55] | –2.14 (6.31) [.73] | 1.90 (6.87) [.78] | –12.83 (4.61) [.01] |
| Medicare/Veterans Affairs | –4.09 (2.61) [.12] | –0.09 (3.91) [.98] | 1.68 (2.81) [.55] | 3.03 (3.48) [.38] | –7.20 (4.48) [.11] | –8.83 (3.95) [.03] |
| Other | –6.23 (2.86) [.03] | –9.03 (4.12) [.03] | –1.10 (3.91) [.78] | 1.19 (4.21) [.78] | –9.75 (4.77) [.04] | –7.26 (4.14) [.08] |
| None | –5.21 (3.92) [.18] | –8.84 (4.89) [.07] | 1.21 (5.12) [.81] | –1.62 (6.01) [.79] | –4.98 (6.24) [.42] | –6.85 (4.96) [.17] |
| Unknown | 5.65 (11.01) [.61] | 15.48 (19.38) [.43] | –2.31 (8.71) [.55] | 1.20 (24.92) [.96] | 8.32 (28.21) [.77] | 5.75 (20.51) [.78] |
| Self-reported health status | ||||||
| Excellent/very good | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Good | –2.16 (1.74) [.22] | –1.50 (2.61) [.57] | –0.41 (2.20) [.85] | –1.12 (2.58) [.66] | –5.21 (2.92) [.08] | –1.90 (2.37) [.42] |
| Fair/poor | –0.35 (2.66) [.89] | –4.55 (3.80) [.23] | 0.99 (3.25) [.76] | –4.41 (3.94) [.26] | 0.45 (4.09) [.91] | 2.25 (3.65) [.54] |
| Unknown | –7.03 (4.01) [.08] | –7.51 (7.83) [.34] | –2.31 (8.71) [.79] | 6.84 (8.01) [.39] | –22.92 (8.14) [.01] | –5.03 (7.50) [.50] |
| Geographic region | ||||||
| Midwest | –0.62 (2.38) [.80] | 0.44 (3.56) [.90] | 5.34 (3.03) [.08] | –3.26 (3.43) [.34] | –2.75 (3.85) [.48] | –1.18 (3.21) [.71] |
| Northeast | –1.95 (2.39) [.42] | –8.96 (3.58) [.01] | 5.01 (2.64) [.06] | 3.96 (3.26) [.23] | 0.74 (4.00) [.85] | –4.07 (3.39) [.23] |
| South | –2.38 (2.10) [.26] | –2.21 (3.18) [.49] | 3.69 (2.80) [.19] | –2.49 (3.19) [.43] | –0.84 (3.42) [.81] | –5.23 (2.84) [.07] |
| West | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| How much have you seen, read, or heard about the coronavirus first detected in Wuhan, China? | ||||||
| A great deal | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| A fair amount | –4.33 (1.57) [.01] | –5.98 (2.48) [.02] | –0.40 (1.69) [.81] | –3.81 (2.33) [.10] | –7.26 (2.64) [.01] | –3.51 (2.32) [.13] |
| Not very much/nothing at all | –17.78 (2.89) [<.001] | –21.13 (4.12) [<.001] | –9.26 (4.07) [.02] | –10.96 (4.44) [.01] | –22.33 (4.61) [<.001] | –18.95 (3.67) [<.001] |
| Number of sources of health information | 1.84 (0.54) [<.001] | 2.26 (0.90) [.01] | 1.39 (0.64) [.03] | 2.15 (0.83) [.01] | 1.38 (0.90) [.13] | 1.90 (0.80) [.02] |
Abbreviation: SE, standard error.
aData source: RTI International–funded survey on coronavirus disease 2019 (COVID-19). Total N = 868 for overall model. R 2 = 0.36. Means are adjusted for sex, age, education, annual household income, employment status, race/ethnicity, self-reported health status, health insurance, and geographic region; amount of information seen, read, or heard about the coronavirus; and number of sources of information.
bBased on linear regression analysis, with P < .05 considered significant.
Scores on knowledge domains also differed by subgroup. Knowledge was significantly lower among Hispanic and non-Hispanic Black respondents than among non-Hispanic White respondents and lower-income respondents across all domains except susceptibility. Respondents who were aged <65 and who had Medicaid or Veterans Affairs health insurance were less knowledgeable about items about misinformation than respondents who were younger and had employer-sponsored health insurance, respectively, and male respondents had higher knowledge scores about severity and mortality than female respondents. Respondents who reported seeing or hearing a greater amount of information about COVID-19 had higher knowledge scores across all domains than respondents who were exposed to less information, and respondents who used more sources of information had higher scores across all domains except vaccines than respondents who used fewer sources of information.
The mean knowledge index score was 43% for respondents with <high school degree and 61% for respondents with ≥bachelor’s degree. The mean knowledge score was 42% for non-Hispanic Black respondents and 58% for non-Hispanic White respondents. The impact of education on knowledge varied by race/ethnicity (Figure 1). Across all racial/ethnic groups, respondents with ≥bachelor’s degree were most knowledgeable. Non-Hispanic Black respondents across all education levels were less knowledgeable than non-Hispanic White respondents. Non-Hispanic Black respondents with <high school education were the least knowledgeable of all subgroups.
Figure 1.
Adjusted mean knowledge index scores, by race/ethnicity and education, from a 16-item knowledge assessment survey about coronavirus disease 2019 (COVID-19) knowledge, United States, February 28–March 2, 2020. Sample size for regression model was 868 and R 2 = 0.39. The overall F-test for race × education interaction is F(9, 867) = 3.04, P < .001. Values for “other” race/ethnicity not shown because of small sample size. Means are adjusted for sex, age, education, annual household income, employment status, race/ethnicity, self-reported health status, and geographic region; amount of information seen, read, or heard about the coronavirus; number of information sources; and interaction of race/ethnicity and education. Error bars indicate 95% CIs.
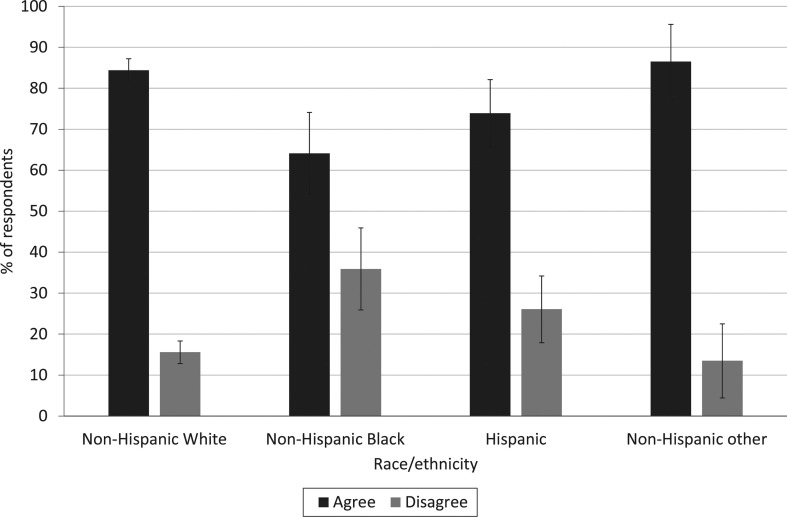
Finally, although 81% of respondents agreed or strongly agreed that they knew what actions to take to prevent themselves and their families from becoming infected with COVID-19, non-Hispanic Black respondents were less likely than non-Hispanic White respondents (P < .001) and respondents of other racial/ethnic groups (P = .004) to endorse this statement (Figure 2).
Figure 2.
Percentage of US residents who said they know how to prevent getting infected with coronavirus, by race/ethnicity, in a survey about coronavirus disease 2019 (COVID-19) knowledge, United States, February 28–March 2, 2020 (N = 1021). Errors bars indicate 95% CIs. Data source: RTI International–funded survey on COVID-19.
Discussion
These findings offer a unique perspective about knowledge levels at the beginning of the COVID-19 epidemic in the United States. Although one survey assessed the public’s knowledge of COVID-19,18 few surveys were administered as the United States had its first death caused by COVID-19 and before the White House declared a public health emergency on March 13, 2020. Overall, knowledge levels were low, with respondents scoring, on average, 62% on the 16-item knowledge index, meaning that answers for 6 of the 16 questions were incorrect or not known. Although respondent knowledge was higher about certain topics than about others (eg, who is susceptible to becoming infected), knowledge about other questions indicated deficiencies. We found gaps in knowledge about disease severity and mortality rates, with respondents believing the mortality rate to be higher than initially indicated. Our study findings align with the results of another study that assessed knowledge of people living in the United States and the United Kingdom 1 week before our study was fielded.19 Because we conducted our study early in the pandemic, it is likely that knowledge levels changed over time given media coverage and state- and local-level guidance to socially distance and wear face coverings. Our findings can serve as a baseline of knowledge among various subgroups in the United States in the early days of the pandemic.
Our findings highlight that some vulnerable subgroups had limited knowledge overall and in certain knowledge domains. Respondents who had low income levels and were unemployed at the time of the survey were less knowledgeable than their higher-income, employed counterparts. Lower-income people include many frontline employees deemed “essential”—such as grocery store clerks, hospital housekeepers, food service staff, and employees at food-processing plants and in the transportation industry.20 Lower-income workers may not have employer-sponsored health insurance and may wait to seek health care.21-24 Ensuring that workers are aware of protective actions is important to their safety and the safety of their households and communities. COVID-19 and SARS-CoV-2 education efforts should be developed for workplace education, and employers should be encouraged to provide access to ongoing education as information about transmission and prevention evolves.
Respondents who were non-Hispanic Black and had low education levels had the lowest knowledge level, potentially putting them at high risk of becoming infected with SARS-CoV-2. Data from multiple states and some cities show that racial/ethnic minority populations have disproportionately higher rates of SARS-CoV-2 infection and mortality than non-Hispanic White people.25,26 Developing and implementing SARS-CoV-2 and COVID-19 education campaigns that use trusted messengers, sources of information, and channels most frequently accessed by these and other groups—such as unemployed people—should be prioritized because they may not rely on mainstream media for their information.
Other subgroups had low knowledge in some domains, which suggests the need for targeted communication efforts. For example, people aged <65 and people with Medicaid/Veterans Affairs health insurance were more prone to misinformation than older adults and people with employer-sponsored or union health insurance. Our results show that substantial misinformation and uncertainty about the virus and COVID-19 existed at the time of the survey (end of February/early March 2020), particularly about transmission and risk-reduction strategies. As misinformation proliferates during the pandemic, directing communication efforts to specific populations, including younger adults and via Medicaid/Veterans Affairs channels, could be beneficial to providing these groups with accurate information. Finally, respondents who reported seeing or hearing more information about COVID-19 and used more sources of information generally had higher knowledge levels about COVID-19 than respondents who reported seeing or hearing less information about COVID-19. Lack of interest, strongly held beliefs, and information-processing capabilities may also influence the successful uptake and application of information regardless of the amount of information disseminated.27
Certain subgroups may be susceptible to both lack of information about public health topics and negative effects of epidemics. According to the Kaiser Family Foundation, Black people in the United States have been disproportionately affected by HIV/AIDS since the beginning of the epidemic, and that disparity has deepened over time.28 National public health education and social marketing campaigns have been implemented for major public health issues such as HIV, because exposure to targeted public health information can positively influence attitudes, beliefs, and behaviors.29 Effective risk communication is a critical component of protecting public health during an infectious disease epidemic.30 As noted by Vaughn and Tinker, “The consequences of pandemic influenza for vulnerable populations will depend partly on the effectiveness of health risk communications. If ignored, current communication gaps for vulnerable populations could result in unequal protection across society during an influenza pandemic.”31
Limitations
Our study had several limitations. First, the survey completion rate was only 36%. However, the study was conducted using a probability-based web panel to capitalize on an already existing US population-based sample and survey structure, which allowed for speed and representativeness of data collection. Second, the survey included a small percentage of Hispanic respondents with <high school degree, and we did not collect information on English-language proficiency, where Hispanic respondents received information about COVID-19, and their most trusted sources of information about COVID-19. Having this information could have provided important insights into message development and dissemination for this subpopulation. These factors should be considered in future research.
Conclusion
Our findings provide important insights about how and where to focus public health education and communications to inform people about the virus and COVID-19, especially people who are at high risk of morbidity and mortality from COVID-19. Understanding how much US residents know about the virus and COVID-19—including how it spreads, how to prevent infection, and how to separate myths from facts—is critical to providing public health education to US residents so that they know how to protect themselves, their families, and their communities. Although COVID-19 has been widely covered by the news media, a science-based and strategic public health education campaign is needed to translate complex clinical and epidemiologic evidence into messages that most people can understand and act on and that reach people through multiple channels.
The messaging should be constructed carefully to combat ongoing myths and misinformation about the virus and COVID-19, particularly in social media,32 and consider people with low levels of health literacy. Providing new and ongoing information about what is known and what is yet to be known is a best practice for risk communication.33 Monitoring changes in knowledge over time will enable communication strategies to be refined during the trajectory of the pandemic and to prepare for the wave of needed information, such as that related to a vaccine. Accurate and timely information about the virus and COVID-19 that successfully reaches the public is a public health intervention that can change the course of the pandemic for the better.
Acknowledgments
The authors thank Jeffrey Novey for his review and editing of the article and Ashley Wheeler for her research assistance.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by RTI International.
ORCID iD
Lauren A. McCormack, PhD, MSPH https://orcid.org/0000-0002-5362-0540
References
- 1. World Health Organization 2019-nCoV outbreak is an emergency of international concern. Updated January 31, 2020. Accessed April 16, 2020 http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/01/2019-ncov-outbreak-is-an-emergency-of-international-concern
- 2. Stokes EK., Zambrano LD., Anderson KN. et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(24):759-765. 10.15585/mmwr.mm6924e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. CDC, Washington State report first COVID-19 death [press release] Atlanta, GA: Centers for Disease Control and Prevention; February 29, 2020. Accessed April 16, 2020 https://www.cdc.gov/media/releases/2020/s0229-COVID-19-first-death.html
- 4. The White House Proclamation on declaring a national emergency concerning the novel coronavirus disease (COVID-19) outbreak. March 13, 2020. Accessed September 1, 2020 https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak
- 5. World Health Organization Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Published February 28, 2020. Accessed April 16, 2020 https://www.who.int/publications-detail/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19)
- 6. Guan WJ., Ni ZY., Hu Y. et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li Q., Guan X., Wu P. et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199-1207. 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tooher R., Collins JE., Street JM., Braunack-Mayer A., Marshall H. Community knowledge, behaviours and attitudes about the 2009 H1N1 influenza pandemic: a systematic review. Influenza Other Respir Viruses. 2013;7(6):1316-1327. 10.1111/irv.12103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Savoia E., Testa MA., Viswanath K. Predictors of knowledge of H1N1 infection and transmission in the U.S. population. BMC Public Health. 2012;12:328. 10.1186/1471-2458-12-328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention Coronavirus disease 2019. Published 2019. Accessed April 16, 2020 https://www.cdc.gov/coronavirus/2019-ncov/index.html
- 11. Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297-334. 10.1007/BF02310555 [DOI] [Google Scholar]
- 12. US Department of Commerce, US Census Bureau Current Population Survey (CPS). A joint effort between the Bureau of Labor Statistics and the Census Bureau. Published 2012. Accessed September 1, 2020 http://www.census.gov/cps
- 13. Cascella M., Rajnik M., Cuomo A., Dulebohn SC., Di Napoli R. Features, Evaluation and Treatment of Coronavirus (COVID-19). StatPearls; 2020. [PubMed] [Google Scholar]
- 14. Centers for Disease Control and Prevention Stop the spread of rumors. Updated June 30, 2020. Accessed August 22, 2020 https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/share-facts.html?CDC_AA_refVal=
- 15. World Health Organization Coronavirus disease (COVID-19) advice for the public: mythbusters. Published 2020. Accessed May 19, 2020 https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters
- 16. US Food and Drug Administration COVID-19 frequently asked questions. Published 2020. Accessed May 19, 2020 https://www.fda.gov/emergency-preparedness-and-response/mcm-issues/coronavirus-disease-2019-covid-19-frequently-asked-questions
- 17. Andersen KG., Rambaut A., Lipkin WI., Holmes EC., Garry RF. The proximal origin of SARS-CoV-2. Nat Med. 2020;26(4):450-452. 10.1038/s41591-020-0820-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Alsan M., Stantcheva S., Yang D., Cutler D. Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among US adults. JAMA Netw Open. 2020;3(6):e2012403. 10.1001/jamanetworkopen.2020.12403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Geldsetzer P. Use of rapid online surveys to assess people’s perceptions during infectious disease outbreaks: a cross-sectional survey on COVID-19. J Med Internet Res. 2020;22(4):e18790. 10.2196/18790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lund S., Ellingrud K., Hancock B., Manyika J., Dua A. Lives and livelihoods: assessing the near-term impact of COVID-19 on US workers. Published April 2, 2020. Accessed April 16, 2020 https://www.mckinsey.com/industries/public-sector/our-insights/lives-and-livelihoods-assessing-the-near-term-impact-of-covid-19-on-us-workers
- 21. Liang H., Beydoun MA., Eid SM. Health needs, utilization of services and access to care among Medicaid and uninsured patients with chronic disease in health centres. J Health Serv Res Policy. 2019;24(3):172-181. 10.1177/1355819619836130 [DOI] [PubMed] [Google Scholar]
- 22. McMorrow S., Kenney GM., Goin D. Determinants of receipt of recommended preventive services: implications for the Affordable Care Act. Am J Public Health. 2014;104(12):2392-2399. 10.2105/AJPH.2013.301569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cole MB., Trivedi AN., Wright B., Carey K. Health insurance coverage and access to care for community health center patients: evidence following the Affordable Care Act. J Gen Intern Med. 2018;33(9):1444-1446. 10.1007/s11606-018-4499-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Seo V., Baggett TP., Thorndike AN. et al. Access to care among Medicaid and uninsured patients in community health centers after the Affordable Care Act. BMC Health Serv Res. 2019;19(1):291. 10.1186/s12913-019-4124-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19): COVIDView. Updated August 21, 2020. Accessed August 22, 2020 https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html
- 26. NYC Health Age adjusted rate of fatal lab confirmed COVID-19 cases per 100,000 by race/ethnicity group as of April 6, 2020. Accessed April 16, 2020 https://www1.nyc.gov/assets/doh/downloads/pdf/imm/covid-19-deaths-race-ethnicity-04082020-1.pdf
- 27. Griffin RJ., Dunwoody S., Yang ZJ. Linking risk messages to information seeking and processing. Ann Int Comm Assoc. 2016;36(1):323-362. 10.1080/23808985.2013.11679138 [DOI] [Google Scholar]
- 28. Kaiser Family Foundation Black Americans and HIV/AIDS: the basics. Published February 7, 2020. Accessed April 16, 2020 https://www.kff.org/hivaids/fact-sheet/black-americans-and-hivaids-the-basics
- 29. Davis KC., Uhrig J., Rupert D., Fraze J., Goetz J., Slater M. Effectiveness of a mass media campaign in promoting HIV testing information seeking among African American women. J Health Commun. 2011;16(9):1024-1039. 10.1080/10810730.2011.571342 [DOI] [PubMed] [Google Scholar]
- 30. Association of State and Territorial Health Officials At-risk populations and pandemic influenza: planning guidance for state, territorial, tribal, and local health departments. Published 2008. Accessed July 21, 2020 https://asprtracie.hhs.gov/technical-resources/resource/961/at-risk-populations-and-pandemic-influenza-planning-guidance-for-state-and-territorial-tribal-and-local-health-departments
- 31. Vaughan E., Tinker T. Effective health risk communication about pandemic influenza for vulnerable populations. Am J Public Health. 2009;99(suppl 2):S324-S332. 10.2105/AJPH.2009.162537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. RTI International Social media analysis describes spread of COVID-19 misinformation online and strategies being used to counter it. Published April 13, 2020. Accessed April 16, 2020 https://www.rti.org/news/social-media-analysis-describes-spread-covid-19-misinformation-online-and-strategies-being-used
- 33. Covello VT. Best practices in public health risk and crisis communication. J Health Commun. 2003;8(suppl 1):5-8. 10.1080/713851971 [DOI] [PubMed] [Google Scholar]