Abstract
Containing coronavirus disease 2019 (COVID-19) through case investigation and contact tracing is a crucial strategy for governmental public health agencies to control the spread of COVID-19 infection in the United States. Because of the recency of the pandemic, few examples of COVID-19 contact-tracing models have been shared among local, state, and federal public health officials to date. This case study of the Anne Arundel County Department of Health (Maryland) illustrates one model of contact-tracing activity developed early in the outbreak. We describe the contact-tracing effort’s place within the broader county health agency Incident Command System, as well as the capabilities needed, team composition, special considerations, and major lessons learned by county health officials. Other local, state, tribal, territorial, and federal health officials and policy makers can use this case study to innovate, iterate, and further refine contact-tracing efforts to prevent the spread of COVID-19 infection and support community members in isolation or quarantine.
Keywords: disease investigation, contact tracing, public health, COVID-19, local and state governmental public health, communicable disease control
The importance of contact tracing to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or coronavirus disease 2019 (COVID-19) outbreak containment has been highlighted by many public health practitioners and policy makers.1-5 Contact tracing, a core function of most local and state health agencies, involves supporting patients (cases or case patients) with suspected or confirmed infection and working with those patients to recall everyone with whom they have had close contact during the time frame in which they may have been infectious (contacts).5 Public health professionals then follow up with contacts to inform them of their potential exposure, assess their health status, and refer them to public health and health care professionals for screening and treatment. In the COVID-19 response, both COVID-19 case patients and their contacts are also told by public health authorities to isolate or quarantine themselves and practice physical distancing to avoid potential transmission to others.
The number of contact tracers needed to adequately contain a COVID-19 outbreak in most US states and territories greatly exceeded the number available early in the COVID-19 response, which is why many states moved to stay-at-home orders and took broad measures to prevent COVID-19 transmission. As transmission expanded exponentially nationwide, there were not enough contact tracers or COVID-19 tests available at the local and state levels to identify case patients and their contacts and contain people with the virus from infecting others.1,3 The Association of State and Territorial Health Officials (ASTHO) and the National Coalition for STD Directors estimated the pre–COVID-19 workforce of disease intervention specialists (DISs) to be approximately 2200 full-time–equivalent employees performing contact-tracing activities for people who receive a positive test result for sexually transmitted diseases/sexually transmitted infection, HIV, or tuberculosis.6
Although DISs are not the only professionals performing contact-tracing activities at the local and state levels, even the highest estimates of governmental public health agency capacity compiled by ASTHO are at or below 10 000 DISs, communicable disease control specialists, epidemiologists, community outreach workers, public health preparedness coordinators, and similar professionals who may be deployed as contact tracers and case investigators in an outbreak (unpublished data, ASTHO Profile Survey, April 2020). The National Association of County and City Health Officials (NACCHO) drafted a nonemergency benchmark of 15 contact tracers per 100 000 population, or 49 500 contact tracers needed nationwide, or 1 contact tracer per 6667 population.4 In Wuhan, China, a city of 11 million people, 9000 contact tracers organized into teams of 5 (equivalent to 1 tracer per every 1222 residents) worked locally to perform contact tracing and isolation/quarantine enforcement, which was >5 times the nonemergency benchmark of 15 per 100 000 population recommended by NACCHO.7 The only national, evidence-based estimator of the number of contact tracers needed at the state, county, and tribal levels was rapidly developed through collaboration between the Fitzhugh Mullan Institute for Health Workforce Equity, ASTHO, and NACCHO in April–May 2020 as the United States prepared reopening plans and realized the urgent and enormous need for contact tracers nationwide.8
Despite the importance of contact tracing to communicable disease control, few studies or practical guides are available on the effective deployment of contact tracing in public health practice beyond the use of DISs at local and state levels. Recently, the Centers for Disease Control and Prevention published guidance for health officials on contact tracing, including training guidance, review of digital tools, core principles of contact tracing, and other technical information for public health practice.9 In addition to guidance, a need exists for practical examples of implementing effective COVID-19 contact-tracing operations at scale in counties, cities, states, and territories. Because of the scale of the response and the number of contact tracers needed to contain COVID-19, health officials and their teams have had to quickly scale up approaches to deploying contact tracers. Sharing these approaches and adapting them at the local and state levels is vital as states restart their economies, reopen institutions such as schools, and look to deploy teams of contact tracers in their jurisdictions with new federal resources to support COVID-19 testing and tracing.3
The purpose of this case study is to describe the contact-tracing process used by the Anne Arundel County Department of Health (AACDOH) in Maryland in its activities to contain the spread of COVID-19 before widespread community mitigation efforts at the state level and national recommendations in March and April 2020. We describe the early formation of contact-tracing teams and their composition, tasks, and major objectives to inform efforts by other public health agencies to create contact-tracing teams at the local, state, and territorial levels to respond to COVID-19 in the future.
Methods
Anne Arundel County, Maryland, with a population of about 576 000, is a mixed urban–rural county located east of the Washington, DC, metropolitan area in central Maryland on the Chesapeake Bay.10 The county is home to Maryland’s capitol, the US Naval Academy, and many large employers including state government. It is also a diverse county, with a population that is 68% non-Hispanic White, 16% non-Hispanic African American, 8% Hispanic, and 4% Asian.11 Although it is a largely affluent community (2018 median household income of $97 814),10 Anne Arundel County has populations living in poverty and health disparities similar to the United States overall.11 Maryland has a mixed state–local public health system: 23 county health agencies have state-delegated responsibility for public health in their jurisdictions, the agencies’ health officers are appointed by local government but approved by the state’s secretary of health, and 51%-75% of the county health agency budget is provided through state funds, whereas 1 city health department (Baltimore) operates autonomously.12
In May 2019, the AACDOH, the county’s public health agency, employed 713 staff members comprising 622 full-time–equivalent employees, most of whom worked in 5 functional areas: disease prevention and management, school health, environmental health, behavioral health, and family health services. The agency employed 6 epidemiology nurses and also relied on epidemiologists at the state health department for additional guidance and support as needed. Pre–COVID-19 health priorities included preventing opioid misuse and addiction, preventing gun violence and injury, and addressing the impact of chronic diseases, including heart disease, diabetes, and cancer prevention.
The first 3 cases of COVID-19 in Maryland were confirmed on March 6, 2020, and the first case of COVID-19 in Anne Arundel County was confirmed on March 11, 2020. (This case was subsequently assigned to Montana based on official residency status.) On March 18, 2020, AACDOH initiated the highest level of its continuity of operations plan and provided only essential services or services that could be delivered remotely. Case investigations and contact tracing started in the county on March 10, 2020, and initially involved mostly travel-related cases. Additional COVID-19 contact-tracing capacity became necessary in mid-March 2020 with confirmed cases and the identification of unlinked transmission. At the start of the COVID-19 outbreak, AACDOH had 6 nurses and 1 administrative staff member who monitored case patients through the National Electronic Disease Surveillance System (NEDSS) and conducted disease intervention activities for outbreaks of influenza in congregate settings, pertussis, and other communicable diseases. As the number of cases of COVID-19 began to increase, the initial team grew and expanded to include agency staff members with some previous work experience in epidemiology and surveillance or similar case investigation and case management work in tuberculosis and HIV programs.
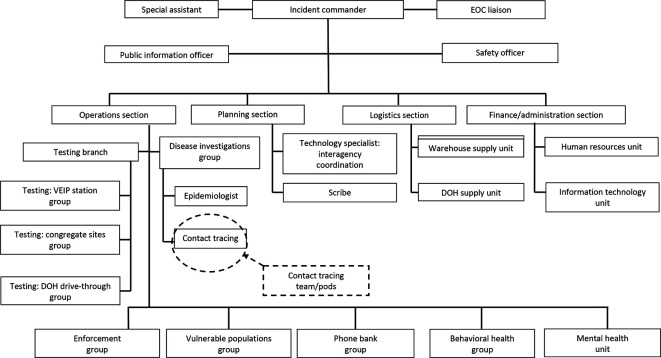
During routine operations, the AACDOH epidemiology team conducts 20-25 contact tracings per month. During the first days of the COVID-19 outbreak in the United States, the AACDOH team was conducting 2 or 3 contact tracings per day. By the time the agency reached 10 new cases of COVID-19 per day, the decision was made to expand tracing capacity to contact trace 100 people per day to meet projected numbers of new infections. Based on case rates in other counties and states, the AACDOH estimated a doubling rate of 4 or 5 days, which would result in 2 or 3 weeks of continued contact tracing. Once the need for contact tracers grew beyond the capacity of the AACDOH staff, the department engaged county school health staff members, who had been placed on administrative leave because of school closures and stay-at-home orders. These teams were clustered into staff member “pods” that were able to safely physically work and use the telephone and computer equipment in 2 county office buildings that had been vacated because of the county’s administrative leave policy. Health officials assembled teams to conduct contact tracing and follow-up activities and included 3-5 registered nurses or licensed practical nurses and 1 or 2 certified nurse assistants or certified medical technicians (Table 1). The contact-tracing function was organized within the overall AACDOH Incident Command System structure (Figure).
Table 1.
Contact-tracing team composition, responsibilities, and equipment needed at the Anne Arundel County Department of Health (AACDOH), Maryland, 2020
| Position/job type (no. of people per team; qualifications) | Main responsibilities | Equipment needed |
|---|---|---|
| Nurses (3-5 registered nurses and licensed practical nurses) | Establish contact with people meeting the definition of a case patient, identify contacts, establish communication with contacts, review symptoms, outline isolation and quarantine requirements, identify barriers to isolation/quarantine, identify and deploy resources to support isolation/quarantine | Telephone, computer |
| Health assistants (1 or 2 certified nurse assistants or certified medical technicians) | Make daily symptom calls/checks | Telephone, computer |
| Runners (1 or 2 per building) | Deliver thermometers, face masks, and quarantine supplies (food, water as needed) and provide letters to residents who were not reached by AACDOH via telephone. Pick up isolation agreements that were used in the beginning of the operation (ended March 31, 2020, because the logistics and personal protective equipment requirements became unmanageable in the face of daily increases in number of new cases) | Vehicle, cell phone, thermometers, personal protective equipment, food, water, official documents |
Figure.
Coronavirus disease 2019 (COVID-19) Incident Command System organizational chart with location of contact-tracing teams, Anne Arundel County Department of Health, Maryland, April 2020. Abbreviations: DOH, Department of Health; EOC, emergency operations center; VEIP, vehicle emissions inspection program.
Because the new contact tracers were already fluent in providing clinical services, they had a baseline level of clinical material and experience that did not need to be taught. However, staff members attended a 2-hour training offered by the county (Table 2) to provide an overview of contact tracing and case investigation.
Table 2.
Instructional units, content, and topics for coronavirus disease 2019 (COVID-19) contact tracers,a Anne Arundel County Department of Health (AACDOH), Maryland, 2020
| Unit | Overall content | Topics |
|---|---|---|
| 1 | Overview of contact-tracing model |
|
| 2 | Initial interview with case patient and script |
|
| 3 | Identification of close contacts |
|
| 4 | Daily symptom check |
|
| 5 | Education about self-isolation |
|
| 6 | Education about quarantine |
|
| 7 | Management of children/dependents in the home |
|
| 8 | Pets |
|
| 9 | Practice scenarios |
|
| 10 | Frequently asked questions |
|
| 11 | Resources |
|
| 12 | Documentation and forms review |
|
aEach team received an initial 1.5- to 2-hour training that included information delivered by AACDOH team members. Privacy and confidentiality training were not included in the course content because staff members had already received this training.
An epidemiology supervisor provided ongoing assistance and support to each team. Teams had a designated team lead (a nurse) who met each morning with their teams to discuss workflow and process issues or concerns. The team leads met with the epidemiology supervisor later that morning to address concerns and to update procedures with new guidance as needed, and the epidemiology supervisor consulted with the team leaders to discuss difficult case investigations.
Positive COVID-19 test results were received electronically via NEDSS, and a designated nurse reviewed cases with the support of an epidemiology team. Staff members created case files in NEDSS and assigned case patients and contacts across the teams for follow-up. Each team had a team leader who assigned case investigations to nurse team members. The nurse team member then initiated contact with the case patient and elicited a list of close contacts who were with the case patient starting from 48 hours before the onset of symptoms to the present time. For positive asymptomatic case patients, contact tracing began from 48 hours before the time of testing. The nurse reviewed symptoms with the case patient, discussed the duration of isolation/quarantine, identified barriers to care (eg, adequate housing, food, income, and transportation to appointments), and addressed these barriers through collaboration with governmental and community-based organizations.
Once the case patient and contacts were identified, the nurse handed the case investigation to health assistants who telephoned the case patients and their contacts daily to obtain temperatures, assess for symptoms, reinforce quarantine and isolation recommendations, and identify any additional barriers or needs. Case patients or contacts who could not be reached by telephone received a hand-delivered letter to the address on record; in the event the case patient or contact was not home, a staff member mailed the letter via certified and regular mail.
Case investigations were closed when everyone associated with the case completed the required isolation or quarantine. If a case patient could not be followed because of an inability to contact the case patient, it was deemed “lost to follow-up” and closed. The case investigation file was then returned to the epidemiology section, and the core epidemiology team nurse entered information into NEDSS and closed the investigation. Staff members then delivered closed case investigation forms to the Maryland Department of Health. Staff members used a paper-based system because of the rapid need for the agency to increase contact-tracing efforts, which did not allow time to create and deploy a new system. Future contact-tracing efforts may use some of the new application (app)-based or web-based contact-tracing systems to streamline reporting, data management, and case management, but these apps and other software developments for managing case patients and contacts were not available early in the pandemic.
Outcomes
During the period March 10–April 30, 2020, a total of 2024 cases of COVID-19 were recorded in the county; 625 (30.9%) cases were in congregate settings such as nursing homes, assisted-living facilities, or other settings, which had their own contact-tracing and isolation and quarantine procedures. The remaining 1399 cases were in the community setting, and case patients were interviewed by county health agency teams. A total of 1119 (80.0%) case patients were contacted within 24 hours of a confirmed positive COVID-19 test result. Of 1399 case patients, 1337 (95.6%) initiated isolation, 1234 (92.3%) of whom documented successful completion of isolation. One hundred twenty-four (6.1%) of the 2024 case patients were lost to follow-up. A total of 4175 contacts were elicited from case patients (average of 3 contacts per case patient), 3371 (80.7%) of whom were interviewed; all but 1 interviewee entered quarantine. A total of 390 (9.3%) of 4175 contacts were converted to case patients based on testing. The largest number of new cases in a day was 104. One hundred seventy-six (8.7%) of the 2024 case patients required social services/assistance to support isolation and quarantine; masks, thermometers, food, medication delivery, baby formula, and referrals to primary care providers were some of the greatest needs.
Lessons Learned
Contact tracing was effective in initiating isolation for 95.6% of people who received a positive test result for COVID-19 and quarantining >80% of contacts. This level of isolation and quarantine suggests that rapid, comprehensive contact tracing can be used to interrupt the transmission of COVID-19, especially early in an outbreak. As COVID-19 continued to spread across the nation in the summer months, media reports and anecdotes from health officials observed reduced compliance with isolation or quarantine recommendations and people who refused to participate in contact-tracing efforts.13-15 More research is needed to better understand the effectiveness of contact tracing and ways to sustain adherence over time. One of the main lessons learned was the centrality of case management as part of the overall contact-tracing strategy, particularly in supporting successful compliance with isolation and quarantine orders. County nurses managed any case patient or contact who required support with housing, food, supplies, medication, and connection to other clinical services to enter or remain in isolation and quarantine. By providing needed services, contact-tracing staff members built trust with community members and provided needed resources to maintain isolation and quarantine. Feedback from community members indicated that this case management support was a critical factor in continued engagement with staff members who conducted contact tracing.
Although the county had a readily available and ideal group of workers to augment the initial surge in the contact-tracing workforce, other options could have included reassigning additional county staff members from current duties, recruiting students from local colleges and universities as contact tracers, and partnering with community-based organizations. An electronic application or other mobile phone or web-based technology was not used in the initial AACDOH contact tracing because of ease of adoption and simplicity of distribution of paper charts. The downside of the paper-based approach was that it made data collection difficult; volumes of cases to investigate and their contacts increased and did not allow easy sharing of the work for any particular case beyond the team to which it was assigned. An online contact-tracing platform would allow greater standardization of data collection and ease in assigning cases to one person or a team, and future efforts will assess the feasibility of adopting such a system.
This case study had several limitations. First, it was conducted in the early weeks of the US COVID-19 pandemic, when rates of community transmission may have been lower than in subsequent months and, as such, may or may not apply to jurisdictions with high rates of community transmission. Second, the resources of a large county such as Anne Arundel may not be the same in counties with fewer public health resources at the local or state level, or counties in states that have no local health department, or where school nurses and other county staff members had been asked to take administrative leave. The outcomes associated with the AACDOH contact-tracing effort took place before Memorial Day weekend, 2020, which was a turning point in the national COVID-19 response, and before extensive public debate about the need to isolate, quarantine, wear face coverings, and otherwise follow the recommendations and/or orders of public health agencies. Rates of compliance with recommendations, including returning calls to local health departments and/or complying with isolation and quarantine guidelines, may be lower in the current environment of open questioning and, in some cases, outright hostility, toward health officials.
Summary
This effort to contain COVID-19 through contact tracing early in the outbreak provides important lessons for future phases of COVID-19 response and for controlling new outbreaks. Although contact tracing is a core function of most local and state health agencies, the scale needed for COVID-19 contact tracing is challenging even to a large agency with sizable staff capacity. The lessons learned from the early response can be used to shape further refinements of contact-tracing activities and team composition at the local, state, territorial, and tribal levels. As contact-tracing practices evolve, the importance of case management, scalable staff pods, and other lessons learned from the early AACDOH contact-tracing effort will inform future innovations in contact-tracing practice and policy at local and state public health agencies.
Footnotes
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr Kalyanaraman is the health officer of the county described in this case study.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Nilesh Kalyanaraman, MD https://orcid.org/0000-0002-5811-1665
Michael R. Fraser, PhD, MS https://orcid.org/0000-0002-5811-1665
References
- 1.Watson C., Cicero A., Blumenstock J., Fraser M. A National Plan to Enable Comprehensive COVID-19 Case Finding and Contact Tracing in the US. Association of State and Territorial Health Officials; 2020. Accessed September 8, 2020 https://www.astho.org/Press-Room/Scaling-Up-Public-Health-Contact-Investigation-Key-to-US-Recovery/04-10-20
- 2.Association of State and Territorial Health Officials Roadmap to recovery: a public health guide for governors. Published April 21, 2020. Accessed September 8, 2020 https://www.nga.org/wp-content/uploads/2020/04/NGA-Report.pdf
- 3.Fox M. “We need an army”: hiring of coronavirus trackers seen as key to curbing disease spread. Published April 13, 2020. Accessed May 9, 2020 https://www.statnews.com/2020/04/13/coronavirus-health-agencies-need-army-of-contact-tracers
- 4.National Association of County and City Health Officials NACCHO position statement: building COVID-19 contact tracing capacity in health departments to support reopening American society safely. Published April 16, 2020. Accessed September 8, 2020 https://www.naccho.org/uploads/full-width-images/Contact-Tracing-Statement-4-16-2020.pdf
- 5.Centers for Disease Control and Prevention Case investigation and contact tracing: part of a multipronged approach to fight the COVID-19 pandemic. April 29, 2020. Accessed May 9, 2020 https://www.cdc.gov/coronavirus/2019-ncov/php/principles-contact-tracing.html
- 6.Association of State and Territorial Health Officials A coordinated, national approach to scaling public health capacity for contact tracing and disease investigation. 2020. Accessed May 9, 2020 https://www.astho.org/COVID-19/A-National-Approach-for-Contact-Tracing
- 7.World Health Organization Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 2020. Accessed May 9, 2020 https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
- 8.George Washington University, Fitzhugh Mullan Institute for Health Workforce Equity Contact tracing workforce estimator. Accessed May 9, 2020 https://www.gwhwi.org/estimator-613404.html
- 9.Centers for Disease Control and Prevention Contact tracing for COVID-19. Updated July 22, 2020. Accessed August 5, 2020 https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/contact-tracing.html
- 10.Census Reporter Anne Arundel County, MD. Accessed September 11, 2020 https://censusreporter.org/profiles/05000US24003-anne-arundel-county-md
- 11.Anne Arundel County Department of Health Anne Arundel County report card 2019. 2019. Accessed May 9, 2020 https://aahealth.org/anne-arundel-county-report-card-2019
- 12.NORC at the University of Chicago, Association of State and Territorial Health Officials State public health agency classification: understanding the relationship between state and local public health. Published 2012. Accessed May 9, 2020 https://www.astho.org/Research/Major-Publications/ASTHO-NORC-Governance-Classification-Report
- 13.Becker J. This contact tracer is fighting two contagions: the virus and fear. The New York Times. August 9, 2020. Accessed September 17, 2020 https://www.nytimes.com/2020/08/09/us/california-contact-tracing.html
- 14.Dalton M. Contact tracing, the West’s big hope for suppressing COVID-19, is in disarray. The Wall Street Journal. September 17, 2020. Accessed September 17, 2020 https://www.wsj.com/articles/contact-tracing-the-wests-big-hope-for-suppressing-covid-19-is-in-disarray-11600337670?mod=djem10point
- 15.Ollstein AM., Tahir D. Contact tracing foiled by conspiracy theories, lack of federal messaging. Politico. September 3, 2020. Accessed September 17, 2020 https://www.politico.com/news/2020/09/03/contact-tracing-conspiracy-theories-trump-messaging-408611?cid=covid_m