Abstract
Background:
Several anatomic features of the knee have been shown to affect joint and anterior cruciate ligament (ACL) loading and the risk of subsequent injuries. While several studies have highlighted sex differences between these anatomic features, little is known on how these differences develop during skeletal growth and maturation.
Hypotheses:
(A) Anatomic features linked to an ACL injury will significantly change during skeletal growth and maturation. (B) The age-related changes in anatomic features linked to an ACL injury are different between male and female patients.
Study Design:
Cross-sectional study; Level of evidence, 3
Methods:
After institutional review board approval, magnetic resonance imaging data from 269 unique knees (patient age 3-18 years; 51% female), free from any injuries, were used to measure femoral notch width, posterior slope of the lateral tibial plateau (lateral tibial slope), medial tibial depth, tibial spine height, and posterior lateral meniscal bone angle. Linear regression was used to test the associations between age and quantified anatomic indices. Patients were then divided into 4 age groups: preschool (3-6 years), prepubertal (7-10 years), early adolescent (11-14 years), and late adolescent (15-18 years). Also, 2-way analysis of variance with the Holm-Sidak post hoc test was used to compare morphology between male and female patients in each age group.
Results:
The femoral notch width, medial tibial depth, and tibial spine height significantly increased with age (P < .001). The lateral tibial slope decreased with age only in male patients (P < .001). Except for the posterior lateral meniscal bone angle, the age-related changes in anatomy were different between male and female patients (P < .05). On average, early and late adolescent female patients had smaller femoral notches, steeper lateral tibial slopes, flatter medial tibial plateaus, and shorter tibial spines compared with age-matched male patients (P < .01).
Conclusion:
Overall, the findings supported our hypotheses, showing sex-specific changes in anatomic features linked to an ACL injury during skeletal growth and maturation. These observations help to better explain the reported age and sex differences in the prevalence of ACL injuries. The fact that most of these anatomic features undergo substantial changes during skeletal growth and maturation introduces the hypothesis that prophylactic interventions (ie, activity modification) would have the potential to reshape a maturing knee in a manner that lowers the risk of noncontact ACL injuries.
Keywords: knee, ACL, anatomy, skeletal maturation, sex
The growing prevalence as well as short- and long-term complications of anterior cruciate ligament (ACL) injuries has motivated research into identifying the risk factors for an ACL injury. In particular, the role of tibiofemoral joint anatomy on the risk of ACL injuries has become the focus of several research efforts over the past decade.‡ This is primarily because of the indisputable links between tibiofemoral joint morphology and its biomechanics.12,18,28,29,35
A narrow intercondylar femoral notch,30,35,44 steep posterior slope of the lateral tibial plateau (lateral tibial slope),3,13,26,29,39 shallow depth (less concave) of the medial tibial plateau,13 small tibial spine,37 and decreased posterior lateral meniscal bone angle39 have been shown to independently increase the risk of ACL injuries across different studies. Recent studies have also established links between some of these anatomic features and an increased risk of secondary ACL injuries6,24,25,32,41 as well as inferior outcomes after ACL reconstruction.19 Some of these anatomic features have also been reported to be different in male versus female patients, with female patients having a higher-risk anatomic profile.36 In addition, a few studies have also shown age-related changes in a subset of these anatomic features, including decreases in the lateral tibial slope and increases in the notch width by age.8,14 However, little is known on whether the reported sex differences in knee anatomy are influenced by age, in particular during skeletal growth and maturation, as well as if those anatomic features develop differently in male and female patients. Such knowledge may help to explain the reported age and sex discrepancies in the risk of ACL injuries (ie, primary and secondary)33,36 as well as the outcomes of ACL surgery.1,17,20,42 It may also help explain recent observations of sex differences in which anatomic features have been associated with an increased risk of ACL injuries in male and female patients.37,38
The overall objective of the current study was to systematically investigate how anatomic features linked to an ACL injury will change during skeletal growth and development in healthy male and female patients. We hypothesized that the anatomic features linked to an ACL injury would undergo significant changes during skeletal growth and maturation. We also hypothesized that the age-related changes in anatomic features linked to an ACL injury would be different between male and female patients.
METHODS
Participants
After institutional review board approval, medical and imaging records of all patients aged ≤18 years who had visited the orthopaedics or sports medicine clinics of our institute (2011-2015) and undergone magnetic resonance imaging (MRI) of the knee were reviewed (n = 2987). Participants were excluded if they had previous knee injuries, congenital or growth-related skeletal disorders, bony deformities, fractures of the tibial plateau or femoral condyle, and soft tissue (ie, cartilage, ligaments, and menisci) injuries or abnormalities across the tibiofemoral and patellofemoral joints (635 participants were excluded). Radiology reports provided by a musculoskeletal radiologist and clinical reports were used to document the injuries and abnormalities. From the 2352 eligible participants, we aimed to randomly select 10 male and 10 female patients for each age using a random number generator. We included all the patients in our database for the preschool age group in which the numbers for each age were <10. Data regarding the body mass index (BMI) of the participants were also extracted.
Anatomic Index Measurements
Essentially, 3-dimensional MRI (3-T SAG PD SPACE sequence with 1.5-mm slice thickness; Siemens) of the knee joint was used to measure femoral notch width, lateral tibial slope, maximum depth of the medial tibial plateau, tibial spine height, and posterior lateral meniscal bone angle following established techniques.12,37,38,44 An experienced examiner (A.M.K.) performed the anatomic measurements using OsiriX Viewer (Pixmeo SARL). Deidentified images were used for measurements to blind the examiner to participants’ sex and age.
To assess the reliability of the anatomic measurements, the same examiner performed the measurements on a subset of 20 knees randomly selected by a random number generator. The same subset was also reanalyzed by an independent examiner not involved in the study. Variance estimates were then used to compute the intraclass and interclass correlation coefficients (ICCs) using SPSS software (IBM Corp). Reliability analyses indicated good to strong7,21 intraobserver (0.83-0.95) and interobserver (0.81-0.92) ICCs for all measurements described here. This is consistent with ICCs reported in previous studies using the same measurement techniques.5,12,15,26,27,30,44
Femoral Notch Width.
The width of the femoral notch was measured in the coronal plane, parallel to a line along the most inferior aspects of the femoral condyles.30 The measurement was performed at the middle of the ACL attachment (Figure 1).44 The bicondylar width of the femur was also measured at the level of the popliteal groove in the same coronal view.26 The notch width index was then calculated by dividing the notch width by the bicondylar width.
Figure 1.
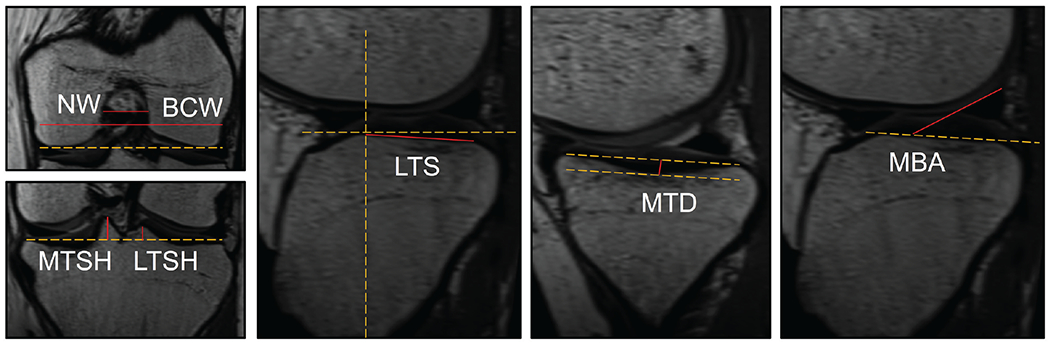
Measurement techniques used to quantify femoral notch width (NW), bicondylar width (BCW), lateral tibial slope (LTS), medial tibial depth (MTD), height of the medial (MTSH) and lateral (LTSH) tibial spines, and posterior lateral meniscal bone angle (MBA).
Lateral Tibial Slope.
The lateral tibial slope was measured using the technique described by Hudek et al.15 Briefly, a central sagittal slice in which the tibial attachment of the posterior cruciate ligament, the intercondylar eminence, and the anterior and posterior tibial cortices appeared in a concave shape was selected. Then, 1 cranial circle (touching the anterior, posterior, and cranial tibial cortices) and 1 caudal circle (touching the anterior and posterior cortices) were fitted to the tibial head. The line connecting the center of the 2 circles was defined as the longitudinal tibial axis.15 This technique has been shown to be highly repeatable and independent of proximal tibial length on MRI.27 The lateral tibial slope was measured in a sagittal slice at the center of the lateral plateau as the angle between a line that joined the peak points on the anterior and posterior rims of the plateau and a line perpendicular to the longitudinal axis of the tibia (Figure 1).12 This method has been shown to be able to quantify the tibial slope with a sensitivity of 1°.13
Medial Tibial Depth.
The medial tibial depth was measured as the perpendicular distance between a line connecting the anterior and posterior rims of the medial tibial plateau and the deepest point of the medial plateau in a sagittal slice passing through the middle of the medial tibial plateau (Figure 1).12
Tibial Spine Height.
The height of the medial and lateral tibial spines were measured in the coronal plane using the technique described by Cavaignac et al.5 Briefly, the coronal slice in which the entire height of the tibial spine was visible was used for analysis. The height of the medial and lateral tibial spines were measured as the perpendicular distance from the peak of each spine and a line connecting the peak points on the medial and lateral aspects of the plateau (Figure 1).
Posterior Lateral Meniscal Bone Angle.
The posterior bone angle of the lateral meniscus was measured using the technique described by Sturnick et al.39 The posterior lateral meniscal bone angle was measured as the angle between the superior surface of the posterior lateral meniscus and the subchondral bone surface in a sagittal slice used to quantify the lateral tibial slope (Figure 1).
Statistical Analysis
A multivariate general linear model was used to investigate the effect of age, sex, and interaction between age and sex (age × sex) on quantified anatomic features. A significant P value for the interaction term indicated different age-related changes in anatomy between male and female patients. Linear regression analysis was used to evaluate the relationships between age and quantified anatomic features. Separate analyses were conducted for each sex group. The slope of the linear regression model (beta ± SE) was used to estimate the change in anatomy per year, which was then compared between male and female patients using an independent t test. To assess sex differences at different ages, patients were classified into 8 subgroups (4 age groups for each sex) based on the following age ranges: preschool (3-6 years), prepubertal (7-10 years), early adolescent (11-14 years), and late adolescent (15-18 years).22 Additionally, 2-way analysis of variance was used to compare the quantified anatomic features between male and female patients in each age group (4 pairwise comparisons). The same analyses were performed to assess the relationships between BMI, age, and sex of the patients. The P values of all 4 pairwise comparisons were then adjusted using Holm-Sidak post hoc to account for any potential increase in type I errors because of multiple comparisons. For these analyses, the anatomic parameters and age were defined as continuous variables, and sex was defined as a categorical and dichotomous variable. All P values are two sided and considered statistically significant at α = .05. The analysis was done in GraphPad Prism (Version 8.4, GraphPad Software).
RESULTS
A total of 269 unique knees were included (aged 3-18 years; 51% female). The BMI increased, on average, by 0.7 ± 0.3 kg/m2 in male patients (R2 = 0.42; P < .001) and by 0.6 ± 0.1 kg/m2 in female patients (R2 = 0.38; P < .001) per year. There were no differences in BMI between male and female patients across all age groups (P > .3 for all comparisons). The P values for the effect of age, sex, and the interaction between age and sex (age × sex), which was included to further investigate whether the age-dependent changes in anatomy were affected by sex, on changes in quantified anatomic features are presented in Table 1. Except for the notch width index and posterior lateral meniscal bone angle, all anatomic features were significantly affected by age and sex, with different age effects seen in male compared with female patients.
TABLE 1.
P Values for the Effects of Age and Sex and Their Interaction (Age × Sex) on Related Changes in Quantified Anatomic Featuresa
|
P Value |
|||
|---|---|---|---|
| Anatomic Features | Age | Sex | Age × Sex |
| Femoral notch width | <.001 | <.001 | .043 |
| Notch width index | .712 | .847 | .361 |
| Lateral tibial slope | .021 | <.001 | .007 |
| Medial tibial depth | <.001 | <.001 | .010 |
| Medial tibial spine height | <.001 | <.001 | .035 |
| Lateral tibial spine height | <.001 | <.001 | .008 |
| Posterior lateral meniscal bone angle | .304 | .112 | .956 |
P < .05 indicates a statistically significant effect.
Age and Sex Differences in Femoral Notch Width
The femoral notch width significantly increased by age in male (R2 = 0.23; P < .001) and female patients (R2 = 0.11; P < .001). The rate of age-related changes in the femoral notch width was higher in male (0.3 ± 0.1 mm/y) compared with female patients (0.2 ± 0.1 mm/y) (P = .044). Male patients had a significantly larger notch width compared with female patients aged 3-6 years (by 2.6 ± 0.9 mm; P = .009), 11-14 years (by 1.4 ± 0.5 mm; P = .014), and 15-18 years (by 2.7 ± 0.5 mm; P < .001). The sex difference in femoral notch width in patients aged 7-10 years was 1.4 ± 0.5 mm, which approached statistical significance (P = .079). There were no changes in the notch width index by age in either male or female patients (R2 < 0.01; P > .30). There were no sex differences in the notch width index in any age group (P > .50 for all comparisons) (Figure 2).
Figure 2.
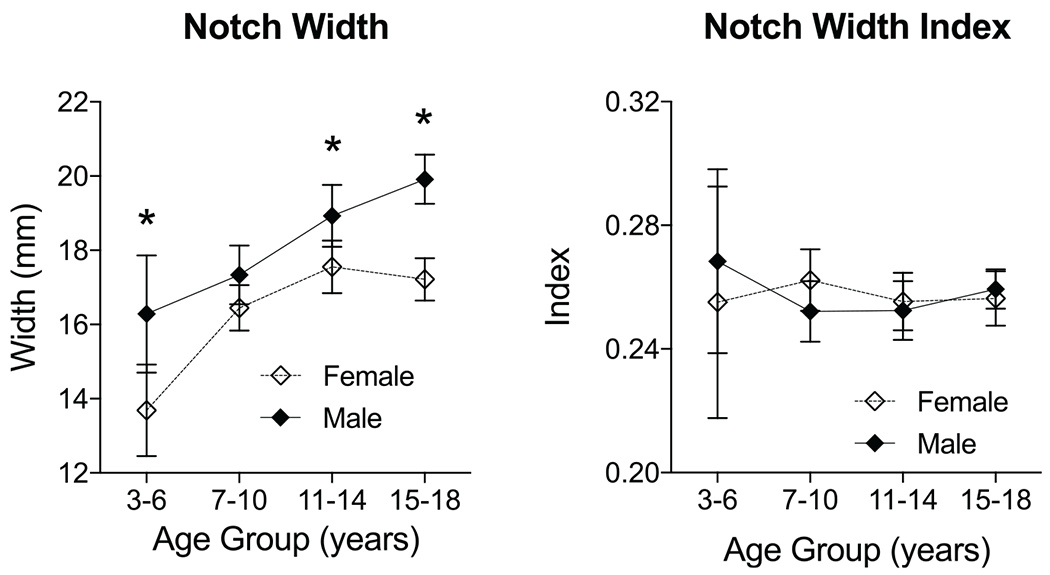
Pairwise comparisons of femoral notch width and notch width index between male and female patients in each age group. Data are reported as mean ± 95% CI. *P < .01.
Age and Sex Differences in Lateral Tibial Slope
The lateral tibial slope significantly decreased by age in male patients at a rate of 0.2 ± 0.1 deg/y (R2 = 0.13; P < .001), while it remained unchanged by age in female patients (R2 = 0.00; P = .932). While male and female patients had similar slopes in those aged 3-6 years (P = .652), there was a significantly lower slope in male patients aged 7-10 years (by 1.9 ± 0.7 mm; P = .013), 11-14 years (by 2.9 ± 0.7 mm; P < .001), and 15-18 years (by 3.3 ± 0.6 mm; P < .001) (Figure 3).
Figure 3.
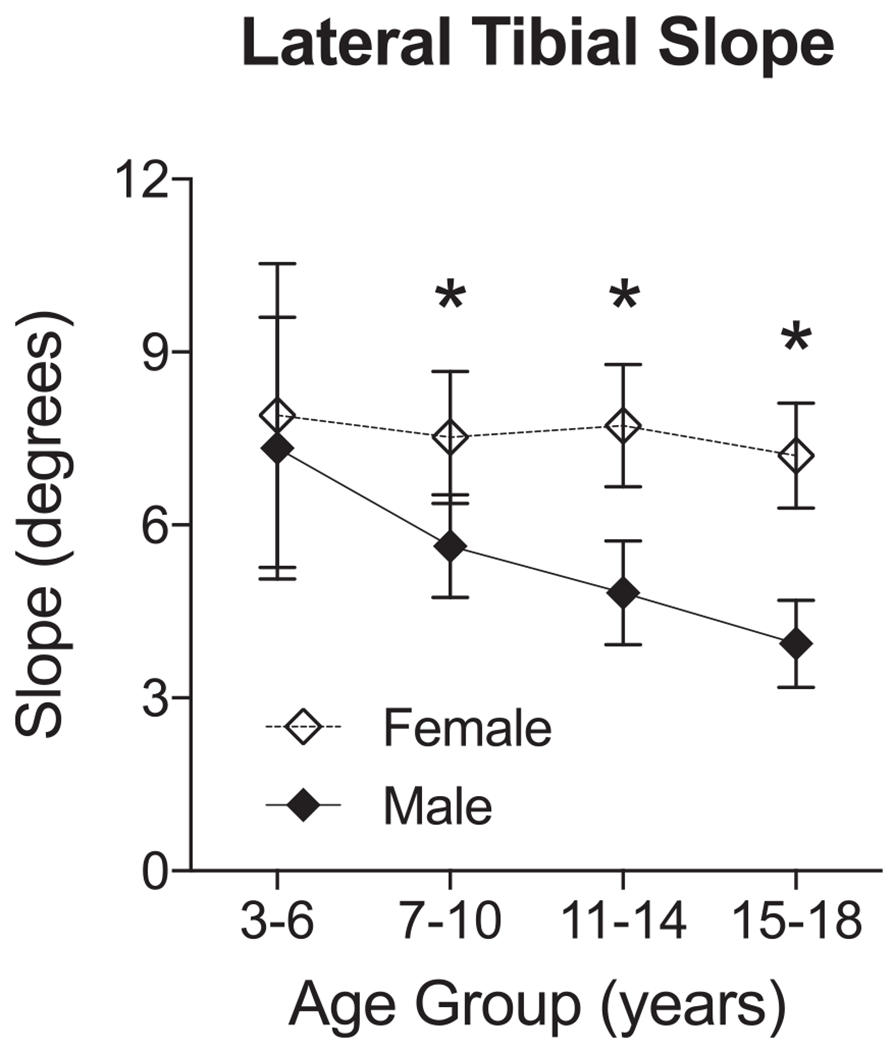
Pairwise comparisons of the lateral tibial slope between male and female patients in each age group. Data are reported as mean ± 95% CI. *P < .01.
Age and Sex Differences in Maximum Depth of the Medial Tibial Plateau
The maximum depth of the medial tibial plateau significantly increased by age in male (R2 = 0.37; P < .001) and female patients (R2 = 0.10; P < .001). The rate of age-related changes in the medial tibial depth was higher in male (0.09 ± 0.01 mm/y) compared with female patients (0.04 ± 0.01 mm/y) (P = .002). While male and female patients had a similar depth in those aged 3-6 years (P = .205), there were significantly deeper medial tibial plateaus in male patients aged 7-10 years (by 0.3 ± 0.1 mm; P = .027), 11-14 years (by 0.3 ± 0.1 mm; P = .016), and 15-18 years (by 0.8 ± 0.1 mm; P < .001) (Figure 4).
Figure 4.
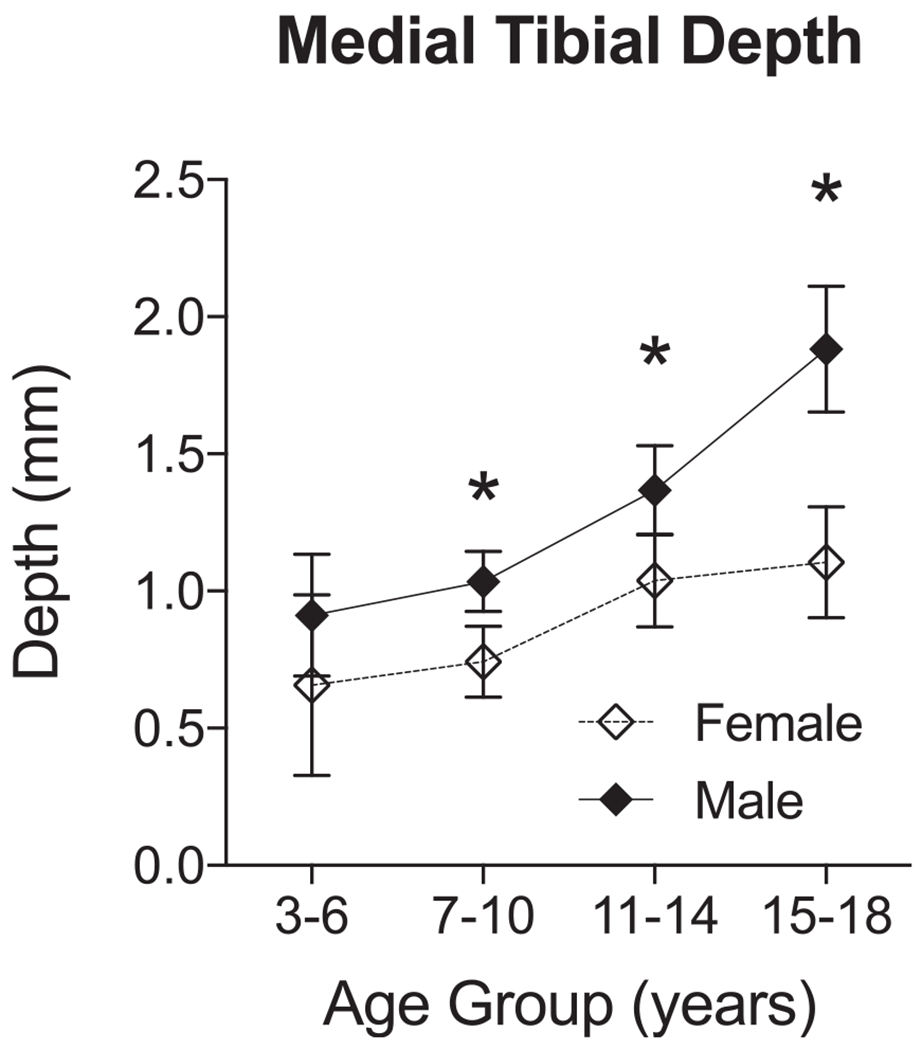
Pairwise comparisons of medial tibial depth between male and female patients in each age group. Data are reported as mean ± 95% CI. *P < .03.
Age and Sex Differences in Tibial Spine Height
The height of the medial tibial spine significantly increased by age in male (R2 = 0.23; P < .001) and female patients (R2 = 0.14; P < .001). There were no differences in the rate of age-related changes in the medial tibial spine height between male (0.21 ± 0.03 mm/y) and female patients (0.14 ± 0.03 mm/y) (P = .125). Male patients aged 3-6 years (by 2.5 ± 0.7 mm; P = .001), 11-14 years (by 1.0 ± 0.3 mm; P = .003), and 15-18 years (by 1.1 ± 0.3 mm; P = .003) had a significantly larger medial tibial spine compared with female patients. There was no sex difference in the medial tibial spine height in patients aged 7-10 years (P = .961) (Figure 5). The height of the lateral tibial spine significantly increased by age in male (R2 = 0.19; P < .001) and female patients (R2 = 0.06; P = .008). Male patients had a higher rate of age-related changes in the lateral tibial spine height (0.19 ± 0.04 mm/y) compared with female patients (0.09 ± 0.03 mm/y), which was marginally significant (P = .053). Male patients aged 3-6 years (by 2.5 ± 0.7 mm; P = .003), 11-14 years (by 1.2 ± 0.3 mm; P = .003), and 15-18 years (by 1.1 ± 0.3 mm; P = .003) had a significantly larger lateral tibial spine compared with female patients. There was no sex difference in the lateral tibial spine height in patients aged 7-10 years (P = .748) (Figure 5).
Figure 5.
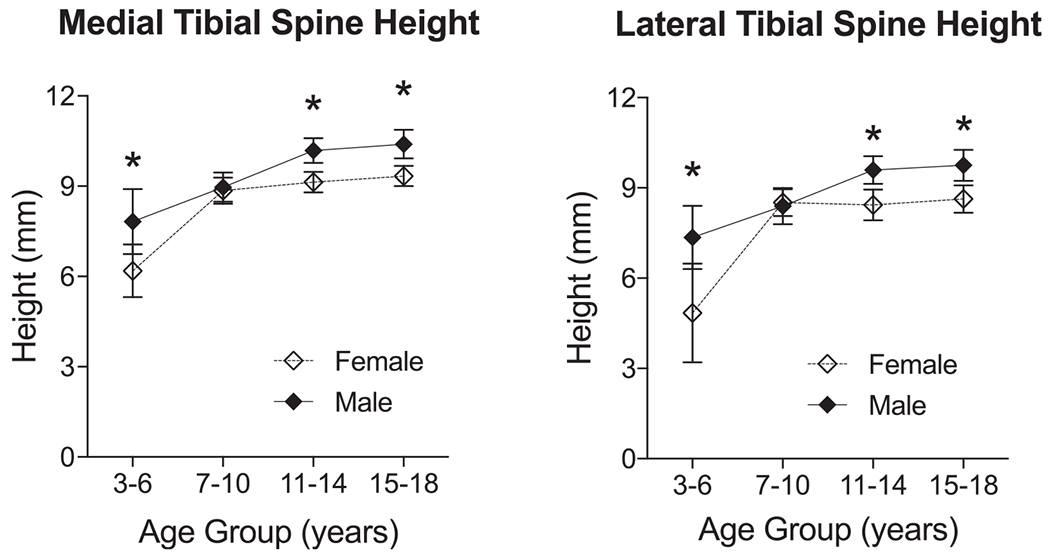
Pairwise comparisons of medial and lateral tibial spine height between male and female patients in each age group. Data are reported as mean ± 95% CI. *P < .004.
Age and Sex Differences in Posterior Bone Angle of the Lateral Meniscus
The posterior bone angle of the lateral meniscus marginally decreased by age in male patients (R2 = 0.03; P = .063) at a rate of 0.2 ± 0.1 deg/y. There was no age-related change in the posterior bone angle of the lateral meniscus in female patients (R2 < 0.01; P = .449). There were no sex differences in the posterior lateral meniscal bone angle in any age group (P > .80 for all comparisons) (Figure 6).
Figure 6.
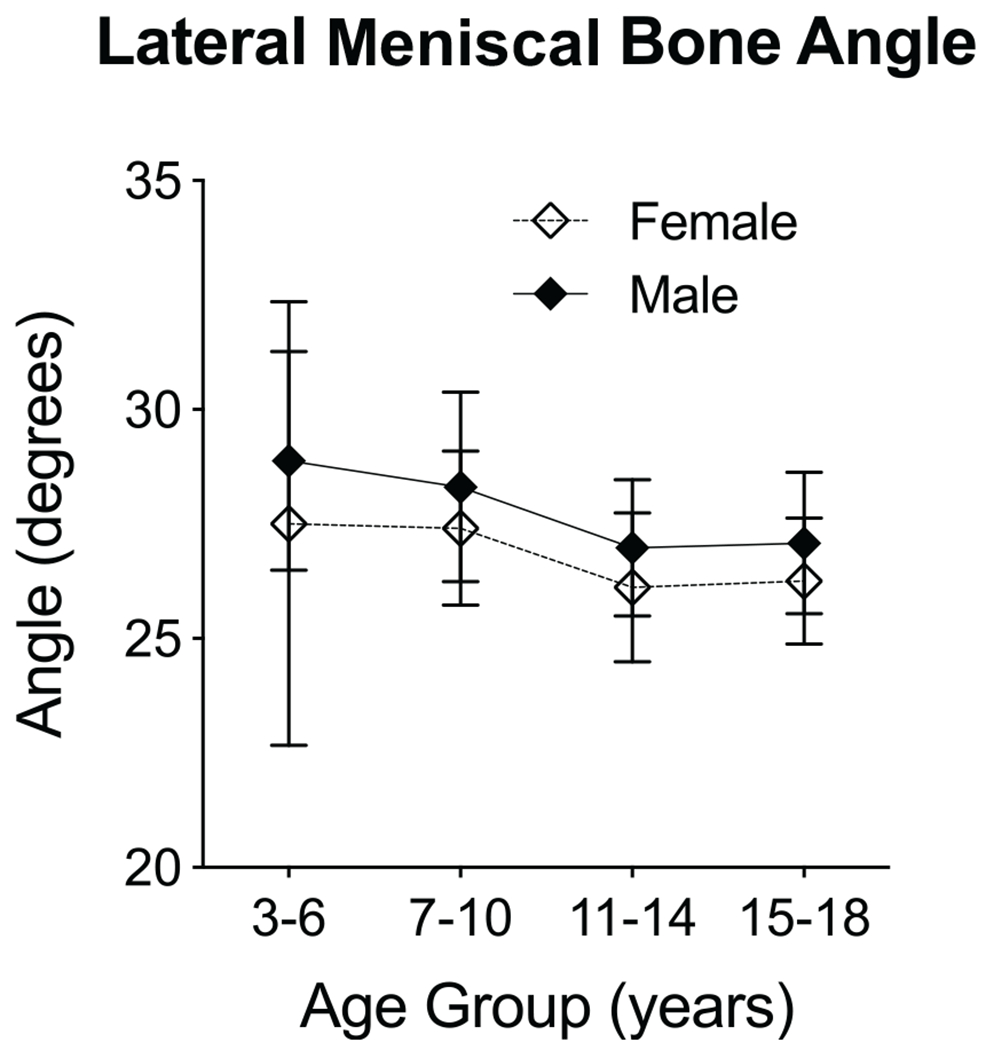
Pairwise comparisons of posterior lateral meniscal bone angle between male and female patients in each age group. Data are reported as mean ± 95% CI.
DISCUSSION
Here, we showed that femoral notch width, lateral tibial slope, maximum depth of the medial tibial plateau, and tibial spine height significantly changed by age during skeletal growth and maturation. The observed age-related changes in male and female patients suggest that the development and maturation of these anatomic features linked to an ACL injury are sex-specific, with the development of more high-risk anatomy in female compared with age-matched male patients. Contrary to our hypotheses, we did not find any age- or sex-related changes in the notch width index and posterior lateral meniscal bone angle. Therefore, these results partially support our hypotheses and highlight the importance of age and sex in investigating the role of anatomy on knee biomechanics as well as the injury risk.
A narrow femoral notch has been associated with increased ACL loading and a greater risk of ACL injuries.2,23,34,35,44 It has been theorized that a small notch is an indication of a small ACL, which is more susceptible to injuries.9,10 Another described mechanism is that a narrow notch produces mechanical impingement of the ACL, which results in localized shear forces that could act to tear the ligament during high-risk movements or where repetitive contact between the ligament and bone reduces the structural properties of the ligament over time.35 In agreement with previous literature,14 we observed significant increases in the femoral notch width by age in both male and female patients. Male patients had a larger notch width and faster growth rate compared with female patients. Interestingly, these age and sex differences went away after normalizing to the notch width index. This suggests that the observed age- and sex-related changes in the femoral notch width are only a function of knee size in normal knees. It is possible that disruption in proportional growth of the femoral notch width can lead to previously reported smaller femoral notches in ACL-injured knees compared with matched controls.2,23,26,44 Further studies in ACL-injured knees can help better address this discrepancy.
A steep lateral tibial slope has been consistently linked to an increased risk of noncontact ACL injuries3,8,13,26,28,40 as well as higher rates of graft failure after ACL reconstruction.6,25,32,41 During weightbearing tasks, the lateral tibial slope produces an anterior shear force component that acts on the tibia as an axial compression force applied across the tibiofemoral joint.11 Accordingly, an increased lateral tibial slope could lead to an increased anterior tibial shear force,28 anterior tibial acceleration and translation,29 and ACL strain.26,29 The lateral tibial slope has also been shown to contribute to knee rotation in coronal (abduction)18 and axial (internal tibial rotation)12,35 planes, which both can increase ACL loading.16,31 Dare and colleagues8 reported an inverse correlation between the lateral tibial slope and age in a cohort of male and female adolescents aged between 12 and 17 years. This is in agreement with our results, showing a significant age effect on the lateral tibial slope in the combined analysis (Table 1). Most interestingly, this relationship was strongly influenced by sex, with a high and unchanged slope in female patients compared with significant decreases in male patients during skeletal growth and maturation. The higher tibial slope in female patients can be a contributing factor to a higher incidence of ACL injuries in female compared with male patients. Further, the observed sex differences in how the tibial slope changes during skeletal growth and maturation can help explain reported discrepancies in how the lateral tibial slope influences the risk of ACL injuries in male versus female patients.3,38 Theoretically, any disruption in age-related reduction of the lateral tibial slope in male patients could result in the development of a steep lateral tibial slope in late adolescence, which can then lead to an increased risk of ACL injuries in male patients.3,40
The maximum depth of the medial tibial plateau has been suggested as a surrogate for the extent of medial tibial plateau concavity.12,13 A deeper (more concave) medial tibial plateau will constrain the femoral condyle to a greater extent and may result in increased resistance to displacement of the tibia relative to the femur.12 Conversely, knees with a shallower medial tibial plateau may be more prone to anterior translation of the tibia. Previous studies have shown a significantly shallower medial tibial depth in participants with an injured ACL compared with matched uninjured controls.13 In the current study, we observed an increased depth (concavity) of the medial tibial plateau by age, although with higher rates in male compared with female patients. We also noted that, on average, male patients had a more concave medial tibial plateau than that of female patients, which can also be a contributor to higher rates of ACL injuries in female patients.
Distinct morphology of the tibial spine has been shown to have significant implications in knee function in primates.43 The tibial spine has been suggested to control axial rotation and medial-lateral translation of the knee joint.37 Considering the importance of internal tibial rotation and medial tibial translation in ACL loading, a short tibial spine can contribute to an increased risk of ACL injuries.37 Our current findings suggest that the tibial spine grows with age but with different patterns in male and female patients. In male patients, the spine continuously grows until midadolescence, whereas in female patients, tibial spine growth slows down or stops after rapid growth before puberty. These sex differences in spine growth lead to a shorter tibial spine in adolescent female compared with male patients, which can then contribute to a higher risk of ACL injuries in female patients.
Geometric features of the posterior aspect of the lateral meniscus have been shown to influence the risk of noncontact ACL injuries.38,39 In particular, the angle between the superior surface of the posterior lateral meniscus and the subchondral bone has been identified as a risk factor for noncontact ACL injuries in both univariate and multivariate analyses.38,39 A higher meniscal bone angle can better restrict anterior tibial translation, therefore lowering the risk of ACL injuries. Interestingly, we did not see any strong age- or sex-related changes in the posterior lateral meniscal bone angle. Further studies on the development of the meniscus in patients with an ACL injury are essential to better understand the links between meniscal morphology and the risk of ACL injuries.
There are several limitations to consider. First, the study was conducted retrospectively, so the findings may be subject to patient selection bias. We tried to minimize the bias by stringent adoption of inclusion/exclusion criteria, random selection, and careful review of the medical and imaging records to confirm eligibility. Second, the study was conducted in a cross-sectional manner and may not fully represent the longitudinal changes in knee morphology during growth. Future prospective longitudinal cohorts are required to confirm the current findings. Third, chronological age may not correspond to skeletal maturity; however, from a practical point of view, we were more interested in analyzing data by chronological age rather than by other bone maturity scores, allowing for greater generalizability. Fourth, we did not control for other factors that may have contributed to differences in morphology, including race, physical activity, and genetic background. While we had access to participants’ race, significant heterogeneity in the distribution of races across different age groups and sexes (the majority were non-Hispanic white) limited our ability to evaluate if the observed trends are influenced by race.
In conclusion, we determined that major anatomic risk factors for an ACL injury (ie, femoral notch width, lateral tibial slope, medial tibial depth, and tibial spine height) undergo significant changes during skeletal growth and maturation. Interestingly, these age-related changes are different in female and male patients, leading to the development of more high-risk anatomy in adolescent female compared with age-matched male patients. These observations help to better explain the reported age and sex differences in the prevalence of ACL injuries. While most of these anatomic features are largely considered to be nonmodifiable, they can be used for the development of risk screening tools to identify at-risk patients. However, further studies into intrinsic and extrinsic factors that regulate and influence the development of these anatomic features as well as their direct links to injuries are essential.
ACKNOWLEDGMENT
The authors thank Drs Martha Murray, Carlo Camathias, Jakob Sieker, Benedikt Proffen, and Seyed Alireza Emami at Boston Children’s Hospital for clinical guidance and consultation. They also thank Dr Leslie Kalish at Boston Children’s Hospital for assistance with statistical analysis.
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was conducted with support from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (R01-AR065462), the Boston Children’s Hospital Orthopaedic Surgery Foundation, the National Football League Players Association through the Harvard Football Players Health Study, the Harvard Catalyst | The Harvard Clinical and Translational Science Center, and the National Center for Advancing Translational Sciences of the National Institutes of Health (UL 1TR002541) as well as financial contributions from Harvard University and its affiliated academic health care centers. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the funding agencies. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Footnotes
REFERENCES
- 1.Ageberg E, Forssblad M, Herbertsson P, Roos EM. Sex differences in patient-reported outcomes after anterior cruciate ligament reconstruction: data from the Swedish knee ligament register. Am J Sports Med. 2010;38(7):1334–1342. [DOI] [PubMed] [Google Scholar]
- 2.Anderson AF, Dome DC, Gautam S, Awh MH, Rennirt GW. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29(1):58–66. [DOI] [PubMed] [Google Scholar]
- 3.Beynnon BD, Hall JS, Sturnick DR, et al. Increased slope of the lateral tibial plateau subchondral bone is associated with greater risk of noncontact ACL injury in females but not in males: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med. 2014;42(5):1039–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bojicic KM, Beaulieu ML, Imaizumi Krieger DY, Ashton-Miller JA, Wojtys EM. Association between lateral posterior tibial slope, body mass index, and ACL injury risk. Orthop J Sports Med. 2017;5(2): 2325967116688664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cavaignac E, Perroncel G, Thepaut M, Vial J, Accadbled F, De Gauzy JS. Relationship between tibial spine size and the occurrence of osteochondritis dissecans: an argument in favour of the impingement theory. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2442–2446. [DOI] [PubMed] [Google Scholar]
- 6.Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(10):2510–2514. [DOI] [PubMed] [Google Scholar]
- 7.Cicchetti DV, Sparrow SA. Developing criteria for establishing interrater reliability of specific items: applications to assessment of adaptive behavior. Am J Ment Defic. 1981;86(2):127–137. [PubMed] [Google Scholar]
- 8.Dare DM, Fabricant PD, McCarthy MM, et al. Increased lateral tibial slope is a risk factor for pediatric anterior cruciate ligament injury: an MRI-based case-control study of 152 patients. Am J Sports Med. 2015;43(7):1632–1639. [DOI] [PubMed] [Google Scholar]
- 9.Davis TJ, Shelbourne KD, Klootwyk TE. Correlation of the intercondylar notch width of the femur to the width of the anterior and posterior cruciate ligaments. Knee Surg Sports Traumatol Arthrosc. 1999;7(4): 209–214. [DOI] [PubMed] [Google Scholar]
- 10.Dienst M, Schneider G, Altmeyer K, et al. Correlation of intercondylar notch cross sections to the ACL size: a high resolution MR tomographic in vivo analysis. Arch Orthop Trauma Surg. 2007;127(4): 253–260. [DOI] [PubMed] [Google Scholar]
- 11.Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376–382. [DOI] [PubMed] [Google Scholar]
- 12.Hashemi J, Chandrashekar N, Gill B, et al. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90(12):2724–2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hashemi J, Chandrashekar N, Mansouri H, et al. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):54–62. [DOI] [PubMed] [Google Scholar]
- 14.Hirtler L, Rohrich S, Kainberger F. The femoral intercondylar notch during life: an anatomic redefinition with patterns predisposing to cruciate ligament impingement. AJR Am J Roentgenol. 2016;207(4): 836–845. [DOI] [PubMed] [Google Scholar]
- 15.Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467(8):2066–2072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kiapour AM, Demetropoulos CK, Kiapour A, et al. Strain response of the anterior cruciate ligament to uniplanar and multiplanar loads during simulated landings: implications for injury mechanism. Am J Sports Med. 2016;44(8):2087–2096. [DOI] [PubMed] [Google Scholar]
- 17.Kiapour AM, Fleming BC, Murray MM. Biomechanical outcomes of bridge-enhanced anterior cruciate ligament repair are influenced by sex in a preclinical model. Clin Orthop Relat Res. 2015;473(8): 2599–2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kiapour AM, Kiapour A, Goel VK, et al. Uni-directional coupling between tibiofemoral frontal and axial plane rotation supports valgus collapse mechanism of ACL injury. J Biomech. 2015;48(10):1745–1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kiapour AM, Yang DS, Badger GJ, et al. Anatomic features of the tibial plateau predict outcomes of ACL reconstruction within 7 years after surgery. Am J Sports Med. 2019;47(2):303–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim DK, Park WH. Sex differences in knee strength deficit 1 year after anterior cruciate ligament reconstruction. J Phys Ther Sci. 2015;27(12):3847–3849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016; 15(2):155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kraus T, Svehlik M, Singer G, Schalamon J, Zwick E, Linhart W. The epidemiology of knee injuries in children and adolescents. Arch Orthop Trauma Surg. 2012;132(6):773–779. [DOI] [PubMed] [Google Scholar]
- 23.LaPrade RF, Burnett QM 2nd. Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries: a prospective study. Am J Sports Med. 1994;22(2):198–203. [DOI] [PubMed] [Google Scholar]
- 24.Levins JG, Argentieri EC, Sturnick DR, et al. Geometric characteristics of the knee are associated with a noncontact ACL injury to the contralateral knee after unilateral ACL injury in young female athletes. Am J Sports Med. 2017;45(14):3223–3232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levins JG, Sturnick DR, Argentieri EC, et al. Geometric risk factors associated with noncontact anterior cruciate ligament graft rupture. Am J Sports Med. 2016;44(10):2537–2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lipps DB, Oh YK, Ashton-Miller JA, Wojtys EM. Morphologic characteristics help explain the gender difference in peak anterior cruciate ligament strain during a simulated pivot landing. Am J Sports Med. 2012;40(1):32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lipps DB, Wilson AM, Ashton-Miller JA, Wojtys EM. Evaluation of different methods for measuring lateral tibial slope using magnetic resonance imaging. Am J Sports Med. 2012;40(12):2731–2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McLean SG, Lucey SM, Rohrer S, Brandon C. Knee joint anatomy predicts high-risk in vivo dynamic landing knee biomechanics. Clin Biomech (Bristol, Avon). 2010;25(8):781–788. [DOI] [PubMed] [Google Scholar]
- 29.McLean SG, Oh YK, Palmer ML, et al. The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg Am. 2011;93(14):1310–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park JS, Nam DC, Kim DH, Kim HK, Hwang SC. Measurement of knee morphometrics using MRI: a comparative study between ACL-injured and non-injured knees. Knee Surg Relat Res. 2012; 24(3):180–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quatman CE, Kiapour AM, Demetropoulos CK, et al. Preferential loading of the ACL compared with the MCL during landing: a novel in sim approach yields the multiplanar mechanism of dynamic valgus during ACL injuries. Am J Sports Med. 2014;42(1):177–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salmon LJ, Heath E, Akrawi H, Roe JP, Linklater J, Pinczewski LA. 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior tibial slope. Am J Sports Med. 2018;46(3):531–543. [DOI] [PubMed] [Google Scholar]
- 33.Schilaty ND, Nagelli C, Bates NA, et al. Incidence of second anterior cruciate ligament tears and identification of associated risk factors from 2001 to 2010 using a geographic database. Orthop J Sports Med. 2017;5(8):2325967117724196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shelbourne KD, Davis TJ, Klootwyk TE. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears: a prospective study. Am J Sports Med. 1998;26(3):402–408. [DOI] [PubMed] [Google Scholar]
- 35.Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43(9):1702–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature, part 1: Neuromuscular and anatomic risk. Sports Health. 2012;4(1):69–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sturnick DR, Argentieri EC, Vacek PM, et al. A decreased volume of the medial tibial spine is associated with an increased risk of suffering an anterior cruciate ligament injury for males but not females. J Orthop Res. 2014;32(11):1451–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sturnick DR, Vacek PM, DeSarno MJ, et al. Combined anatomic factors predicting risk of anterior cruciate ligament injury for males and females. Am J Sports Med. 2015;43(4):839–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sturnick DR, Van Gorder R, Vacek PM, et al. Tibial articular cartilage and meniscus geometries combine to influence female risk of anterior cruciate ligament injury. J Orthop Res. 2014;32(11):1487–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Waiwaiole A, Gurbani A, Motamedi K, et al. Relationship of ACL injury and posterior tibial slope with patient age, sex, and race. Orthop J Sports Med. 2016;4(11):2325967116672852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med. 2013;41(12):2800–2804. [DOI] [PubMed] [Google Scholar]
- 42.Webster KE, Feller JA, Kimp AJ, Whitehead TS. Revision anterior cruciate ligament reconstruction outcomes in younger patients: medial meniscal pathology and high rates of return to sport are associated with third ACL injuries. Am J Sports Med. 2018;46(5):1137–1142. [DOI] [PubMed] [Google Scholar]
- 43.White JL, Gebo DL. Unique proximal tibial morphology in strepsir-rhine primates. Am J Primatol. 2004;64(3):293–308. [DOI] [PubMed] [Google Scholar]
- 44.Whitney DC, Sturnick DR, Vacek PM, et al. Relationship between the risk of suffering a first-time noncontact ACL injury and geometry of the femoral notch and ACL: a prospective cohort study with a nested case-control analysis. Am J Sports Med. 2014;42(8):1796–1805. [DOI] [PMC free article] [PubMed] [Google Scholar]


