Abstract
This population epidemiology study characterizes trends in the prevalence of asymptomatic severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection among international entrants testing positive for SARS-CoV-2 at Chinese border checkpoints between mid-April and mid-October 2020.
The magnitude of asymptomatic severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is a question of global concern. Individuals who test positive for SARS-CoV-2 infection via a polymerase chain reaction (PCR) test but lack coronavirus disease 2019 (COVID-19)–like symptoms must be followed up through the incubation period to distinguish individuals with asymptomatic infection from those with presymptomatic infection.1
China successfully controlled its initial COVID-19 epidemic in March 20202 and has since focused on preventing importation of SARS-CoV-2 infection. Beginning April 1, 2020, persons entering China via air, sea, or land have been mandatorily tested for SARS-CoV-2 infection by PCR test at border checkpoints. Individuals who have tested positive have been hospitalized in isolation and those who have tested negative have been quarantined for 14 days at centralized facilities and then retested on day 13. We assessed the proportion of international entrants to China with asymptomatic SARS-CoV-2 infection.
Methods
This retrospective cohort study was approved by the institutional review board of the Chinese Center for Disease Control and Prevention; informed consent was not required. All international entrants found to have SARS-CoV-2 infection via a positive PCR test result at China’s border checkpoints from April 16 to October 12 were included in this study. This allowed 15 days for full policy implementation (April 1-15) and 13 days of follow-up for the last enrolled participant (October 13-25).
Participants were categorized as either confirmed COVID-19 cases (ie, positive test results for SARS-CoV-2 infection plus being symptomatic or presymptomatic) or asymptomatic SARS-CoV-2 infection cases (ie, positive test results for SARS-CoV-2 infection but having no symptoms throughout the 14-day quarantine).1 Although different from the that of the World Health Organization,3 this case definition is standard in China.1 Fifteen-day intervals during the study were used to investigate changes over time.
The χ2, Cochran-Mantel-Haenszel, and Jonckheere-Terpstra nonparametric trend tests were used. A 2-sided P < .05 was considered statistically significant. All analyses were performed using SAS software version 9.2 (SAS Institute Inc).
Results
Of the 19 398 384 international travelers who entered China during the study period, 3103 had SARS-CoV-2 infection. Most were male (75.5%) and were aged 20 to 49 years (80.8%) (Table). Among all SARS-CoV-2–positive entrants, 1354 (43.6%) had symptoms at entry (symptomatic) and 137 (4.4%) developed symptoms (presymptomatic; median time to symptom onset, 1 day; interquartile range [IQR], 0-5 days; 95th percentile, 10 days) and were categorized as confirmed COVID-19 cases, whereas 1612 (51.9%) never developed symptoms through day 13 and were considered to have asymptomatic SARS-CoV-2 infection.
Table. Characteristics of International Entrants to China From April 16, 2020, to October 12, 2020.
| Characteristics | No. (%) | P value | |||
|---|---|---|---|---|---|
| All entrants to Chinaa | All participantsa,b | Confirmed COVID-19 casesc,d | Asymptomatic SARS-CoV-2 infectionc,e | ||
| Overall | 19 398 384 (100) | 3103 (100) | 1491 (48.1) | 1612 (51.9) | |
| Sex | |||||
| Male | 2343 (75.5) | 1109 (47.3) | 1234 (52.7) | .61f | |
| Female | 760 (24.5) | 382 (50.3) | 378 (49.7) | ||
| Age group, y | |||||
| <20 | 167 (5.4) | 79 (47.3) | 88 (52.7) | <.001g | |
| 20-29 | 931 (30.0) | 426 (45.8) | 505 (54.2) | ||
| 30-39 | 854 (27.5) | 389 (45.6) | 465 (54.4) | ||
| 40-49 | 721 (23.2) | 347 (48.1) | 374 (51.9) | ||
| ≥50 | 430 (13.9) | 250 (58.1) | 180 (41.9) | ||
| Country traveling from | |||||
| Philippines | 500 (16.1) | 209 (41.8) | 291 (58.2) | ||
| Russian Federation | 453 (14.6) | 193 (42.6) | 260 (57.4) | ||
| Singapore | 242 (7.8) | 75 (31.0) | 167 (69.0) | ||
| US | 160 (5.2) | 103 (64.4) | 57 (35.6) | ||
| 86 other countries | 1748 (56.3) | 911 (52.1) | 837 (47.9) | ||
| Entry SARS-CoV-2 screening result | |||||
| Negative | 19 395 281 (>99.9) | 0 | 0 | 0 | |
| Positive | 3103 (<0.1) | 3103 (100) | 1491 (48.1) | 1612 (51.9) | |
| Timing of symptoms | |||||
| Present at first test (ie, symptomatic cases) | 1354 (43.6) | 1354 (100) | 0 | ||
| Present at second test (ie, presymptomatic cases) | 137 (4.4) | 137 (100) | 0 | ||
| Never present (ie, asymptomatic infections) | 1612 (51.9) | 0 | 1612 (100) | ||
| Study period | |||||
| April 16-30 | 538 905 (2.8) | 162 (5.2) | 117 (72.2) | 45 (27.8) | <.001g |
| May 1-15 | 669 229 (3.5) | 40 (1.3) | 28 (70.0) | 12 (30.0) | |
| May 16-30 | 737 938 (3.8) | 61 (2.0) | 43 (70.5) | 18 (29.5) | |
| May 31–June 14 | 757 881 (3.9) | 161 (5.2) | 98 (60.9) | 63 (39.1) | |
| June 15-29 | 999 726 (5.2) | 123 (4.0) | 80 (65.0) | 43 (35.0) | |
| June 30–July 14 | 1 252 065 (6.5) | 142 (4.6) | 69 (48.6) | 73 (51.4) | |
| July 15-29 | 1 759 192 (9.1) | 143 (4.6) | 72 (50.4) | 71 (49.7) | |
| July 30–August 13 | 2 272 675 (11.7) | 337 (10.9) | 192 (57.0) | 145 (43.0) | |
| August 14-28 | 2 842 526 (14.7) | 485 (15.6) | 222 (45.8) | 263 (54.2) | |
| August 29–September 12 | 2 479 043 (12.8) | 443 (14.3) | 165 (37.3) | 278 (62.8) | |
| September 13-27 | 2 589 730 (13.4) | 479 (15.4) | 191 (39.9) | 288 (60.1) | |
| September 28–October 12 | 2 499 474 (12.9) | 527 (17.0) | 214 (40.6) | 313 (59.4) | |
Abbreviations: COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Percentages generated using the overall total value in the column as the denominator.
Tested positive for SARS-CoV-2 infection via a polymerase chain reaction test.
Percentages generated using the category value in the “all participants” column as the denominator.
Tested positive for SARS-CoV-2 infection and had symptoms or was presymptomatic.
Did not have symptoms throughout the 14-day quarantine.
The χ2 test was used to compare sex distribution between confirmed cases of COVID-19 and those with asymptomatic SARS-CoV-2 infection.
The Cochran-Mantel-Haenszel test was used to determine whether the presence of symptoms (ie, confirmed COVID-19 cases vs those with asymptomatic SARS-CoV-2 infection) changed by age group or by study period.
Among all international entrants (part A in the Figure), the proportion of SARS-CoV-2–positive persons screened remained stable at 0.01% to 0.03% (part B), but the proportion of individuals with symptomatic, presymptomatic, and asymptomatic SARS-CoV-2 infection did not remain stable (part C). Among all SARS-CoV-2–positive entrants, the proportion of asymptomatic infections increased significantly over time from 27.8% during April 16 to April 30 to 59.4% during September 28 to October 12 (P < .001) (Table).
Figure. International Entrants to China From April 16, 2020, to October 12, 2020.
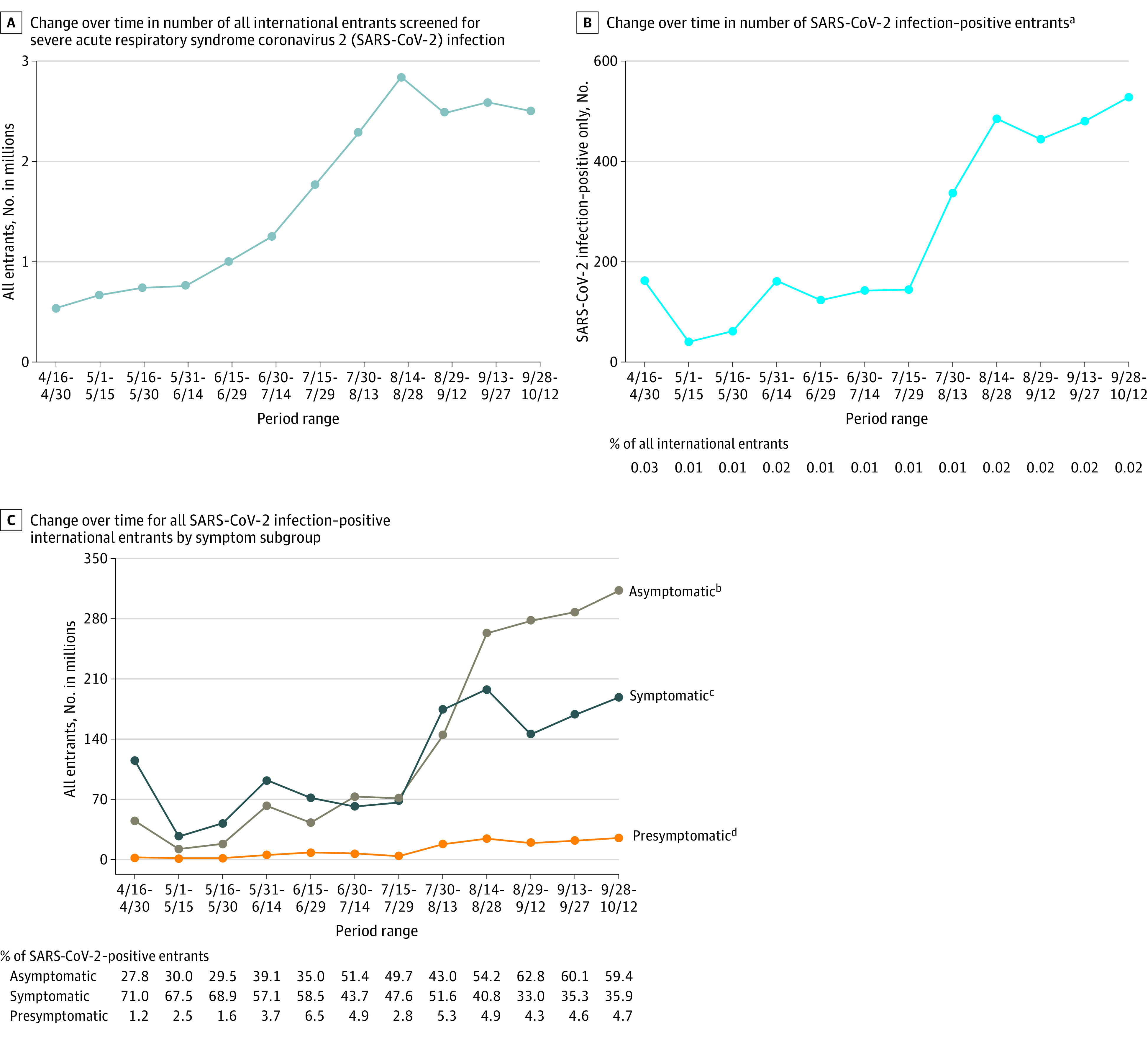
aTested positive for SARS-CoV-2 infection via a polymerase chain reaction test.
bDid not have symptoms throughout the 14-day quarantine.
cHad symptoms throughout the 14-day quarantine.
dDeveloped symptoms during the 14-day quarantine.
No association was found between presence of symptoms and sex (P = .61). A significant association was found between presence of symptoms and age (P < .001) (Table). Although median age was highest in the April 16-30 period at 38 years (IQR, 23-45 years), it decreased to 24 years (IQR, 20-33 years) in the May 1-15 period, then significantly increased, reaching 35 years (IQR, 29-46 years) in the September 28–October 12 period. Of SARS-CoV-2–positive entrants, 43.7% arrived from just 4 of 86 countries (Table). Among confirmed COVID-19 cases, the proportion who were symptomatic (median, 95.4%; range, 93.0%-98.7%) vs presymptomatic (median, 4.6%; range, 1.3%-5.6%) did not change significantly over time (P = .27).
Discussion
The finding of a high and increasing proportion of asymptomatic infections among all SARS-CoV-2–positive international entrants to China may signal an increase in asymptomatic infection globally. Because asymptomatic SARS-CoV-2 infection is thought to be more common in young people,4 and severe and critical case status is more common in older adults,5 the finding of increasing age in the population over time indicates that the results were not biased by age. Moreover, the unchanging proportion of symptomatic cases among all confirmed cases suggests that the increase in asymptomatic infections over time was not due to symptomatic persons being screened out before travel.
The main limitation was the inability to directly ascertain how many symptomatic individuals were screened out or whether any individuals were screened in because of prior infection and prolonged viral shedding. Nevertheless, this study has implications for traveler screening policies and procedures.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Wu Z, McGoogan JM. Asymptomatic and pre-symptomatic COVID-19 in China. Infect Dis Poverty. 2020;9(1):72. doi: 10.1186/s40249-020-00679-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou L, Wu Z, Li Z, et al. ; China COVID-19 Task Force . One hundred days of COVID-19 prevention and control in China. Clin Infect Dis. Published online June 5, 2020. doi: 10.1093/cid/ciaa725 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization WHO COVID-19 case definition. Accessed September 19, 2020. https://www.who.int/ publications/i/item/WHO-2019-nCoV-Surveillance_Case_Definition-2020.1
- 4.Davies NG, Klepac P, Liu Y, Prem K, Jit M, Eggo RM; CMMID COVID-19 Working Group . Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020;26(8):1205-1211. doi: 10.1038/s41591-020-0962-9 [DOI] [PubMed] [Google Scholar]
- 5.Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(24):759-765. doi: 10.15585/mmwr.mm6924e2 [DOI] [PMC free article] [PubMed] [Google Scholar]


