Abstract
Introduction
Reports vary on how sex influences the management and outcome from acute intracerebral haemorrhage. We aimed to quantify sex disparities in clinical characteristics, management, including response to blood pressure lowering treatment, and outcomes in patients with acute intracerebral haemorrhage, through interrogation of two large clinical trial databases.
Patients and Methods
Post-hoc pooled analysis of the Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage trials 1 and 2, where patients with a hypertensive response (systolic, 150–220 mmHg) after spontaneous intracerebral haemorrhage (<6 h) were randomised to intensive (target <140 mmHg <1 h) or guideline-recommended (<180 mmHg) blood pressure lowering treatment. The interaction of sex on early haematoma growth (24 h), death or major disability (modified Rankin scale scores 3–6 at 90 days), and effect of randomised treatment were determined in multivariable logistic regression models adjusted for baseline confounding variables.
Results
In 3233 participants, 1191 (37%) were women who were significantly older, had higher baseline National Institutes of Health Stroke Scale scores and smaller haematoma volumes compared to men. Men had higher three-month mortality (odds ratio 1.48, 95% confidence interval 1.10–2.00); however, there was no difference between women and men in the combined endpoint of death or major disability. There were no significant sex differences on mean haematoma growth or effect of randomised blood pressure lowering treatment.
Discussion
Men included in the Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage trials had more comorbidities, larger baseline haematoma volumes and higher mortality after adjustment for age, as compared with women.
Conclusion
Men included in the Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage trials had a greater odds of dying after intracerebral haemorrhage than women, which could not be readily explained by differing casemix or patterns of blood pressure management.
Clinical trial registration
The Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage trials studies are registered with ClinicalTrials.gov (NCT00226096 and NCT00716079).
Keywords: Sex differences, intracerebral haemorrhage, blood pressure, haematoma growth, perihaematomal oedema
Introduction
Spontaneous intracerebral haemorrhage (ICH) is the most serious type of stroke,1,2 where age and ethnicity are recognised predisposing risk factors. However, sex-related biological and social factors may also influence the pathophysiology, response to treatments, and thus prognosis for recovery from ICH. Although a recent individual patient data meta-analysis found no differences in the outcomes of death or major disability after ICH,3 there is some evidence for a lobar location of the haematoma to be more common in women.4,5 While haematoma volume and its expansion appears similar in women and men, perihaematomal oedema volume may be smaller in women6 while better control of blood pressure (BP) may influence the chances of survival but not overall functional outcome in men rather than women.7,8 Herein, we undertook a post-hoc analysis of the Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage trials (INTERACT 1 and 2) to determine sex differences in clinical characteristics, management and outcome of patients with acute ICH. In addition, we undertook analyses to determine sex differences in the effect of intensive versus guideline BP lowering treatment on outcome in patients with acute ICH.
Methods
The INTERACT 1 (n = 404) and 2 (n = 2829) studies were international, multicentre, open, blinded endpoint assessed, randomised controlled trials.9–12 In brief, a total of 3243 patients with spontaneous ICH within 6 h of onset and elevated systolic BP (SBP 150–220 mmHg) were randomly assigned to receive intensive (target BP <140 mmHg within 1 h) or contemporary guideline recommended (target SBP <180 mmHg) BP lowering therapy, according to standardised protocols. Patients were excluded if they had a structural cerebral cause for the ICH, were in deep coma (Glasgow coma scale (GCS) scores 3–5), had massive haematoma with poor prognosis or if early surgery to evacuate the haematoma was planned. Written informed consent was obtained from all participants (or approved surrogates) and the study protocol was approved by the ethics committee of each participating hospital. The INTERACT studies are registered with ClinicalTrials.gov, numbers NCT00226096 and NCT00716079.
Baseline demographic and clinical characteristics were recorded at the time of enrolment, including neurological severity assessed on the GCS and National Institutes of Health Stroke Scale (NIHSS).13 After the diagnostic CT scan in all patients, 1313 participants (346 and 1967 in INTERACT1 and 2, respectively) underwent a repeat CT scan at 24 ± 3 h using similar procedures, with de-identified uncompressed digital images on Digital Imaging and Communications in Medicine format assessed centrally for haematoma and perihaematomal oedema volumes by trained neurologists blind to clinical, time and sequence data, using computer-assisted multi-slice planimetric and voxel threshold techniques (MIStar@, Apollo Medical Imaging Technology, Melbourne, Australia).14 All patients were assessed by functional outcome by trained researchers blind to treatment allocation using the modified Rankin scale (mRS) at 90 days.
For these analyses, the primary clinical outcome was death at 90 days. Secondary outcomes were death or major disability (mRS scores 3–6), separately for major disability (mRS 3–5), achieved SBP over 24 h serious adverse events, and absolute growth over 24 h in haematoma and perihaematomal oedema volumes in the subgroup with repeat CT.
Baseline characteristics were summarised as mean (standard deviation) or median (interquartile range) for continuous variables, and number (%) for categorical variables, with sex differences tested using Wilcoxon and chi-square tests, respectively. Using women as the reference, associations between sex and outcomes were examined using logistic regression with adjustments for age, region of recruitment (China versus non-China), history of ischaemic stroke or other undifferentiated stroke, and antihypertensive treatment, baseline blood glucose (>6.5 versus ≤6.5 mmol/l), NIHSS score (<15 versus ≥15), haematoma volume, and randomised BP lowering treatment. In the CT substudies, associations of sex and baseline volumes of haematoma and perihaematomal oedema, and their absolute growth over 24 h, were assessed by analysis of covariance, with similar adjustment variables as above. Data are reported with odds ratios (OR) and 95% confidence intervals (CI). A P value <0.05 was indicative of statistical significance. All analyses were performed using SAS software (version 9.3; SAS Institute, Cary, NC).
Results
Of 3233 INTERACT studies participants, 1191 (37%) were women who were older, more likely to have taken prior antihypertensive medication, and present with higher blood glucose levels and greater neurological deficits than men (Table 1). However, men were more likely to have had prior ischaemic stroke and to be intubated during hospitalisation. There were no sex differences in other aspects of in-hospital management over seven days.
Table 1.
Patient characteristics by sex.
| Women (n = 1191) | Men (n = 2042) | P value | |
|---|---|---|---|
| Age, years | 64.9 (13.0) | 62.5 12.6) | <0.0001 |
| Chinese | 859 (72.1) | 1445 (70.8) | 0.410 |
| History of cardiac disease | 139 (11.7) | 202 (9.9) | 0.112 |
| Diabetes mellitus | 115 (9.7) | 224 (11.0) | 0.234 |
| History of intracerebral haemorrhage | 95 (8.0) | 180 (8.8) | 0.403 |
| History of ischaemic/undifferentiated stroke | 110 (9.2) | 259 (12.7) | 0.003 |
| History of hypertension | 902 (75.7) | 1446 (70.9) | 0.003 |
| Use of antihypertensive therapy | 574 (48.2) | 875 42.9) | 0.004 |
| Use of antithrombotic agents | 122 (10.2) | 246 (12.1) | 0.119 |
| Lipid lowering therapy | 69 (5.8) | 140 (6.9) | 0.232 |
| Clinical features | |||
| Systolic BP (mmHg) | 179.8 (16.9) | 179.0 17.3) | 0.130 |
| NIHSS score | 11 (7–16) | 10 (6–15) | 0.002 |
| NIHSS score ≥15 | 371 (31.3) | 544 (26.8) | 0.006 |
| GCS score | 14 (12–15) | 14 (13–15) | 0.002 |
| GCS <13 | 340 (28.6) | 481 (23.6) | 0.002 |
| Hyperglycaemia. >6.5 mmol/l | 600 (52.7) | 889 (46.4) | 0.001 |
| Haematoma volume (ml) | 9.9 (5.3–17.7) | 11.3 (5.8–19.9) | 0.004 |
| Left hemisphere | 556 (50.3) | 935 (50.5) | 0.921 |
| Deep location of haematoma | 910 (82.3) | 1560 (84.2) | 0.176 |
| Intraventricular extension | 320 (28.9) | 501 (27.0) | 0.265 |
| Randomised to intensive BP lowering | 581 (48.8) | 1021 (50.0) | 0.504 |
| Time from onset to randomisation | 3.7 (2.8–4.7) | 3.7 (2.8–4.7) | 0.856 |
| Any intravenous BP lowering treatment | 549 (46.5) | 994 (49.7) | 0.084 |
| Management over seven days | |||
| Intensive care unit admission | 380 (36.6) | 681 (39.1) | 0.178 |
| Intubation | 62 (5.3) | 158 (7.9) | 0.005 |
| IV mannitol | 763 (64.7) | 1293 (64.7) | 0.995 |
| Any surgery | 64 (5.4) | 119 (5.9) | 0.539 |
| Venous thromboembolism prophylaxis | 233 (19.8) | 395 (19.8) | 0.998 |
| Haemostatic therapy | 40 (3.4) | 92 (4.6) | 0.098 |
BP: blood pressure; GCS: Glasgow coma scale; IV: intravenous; NIHSS: National Institutes of Health stroke scale.
Data are n (%), mean (SD) or median (IQR). P values are based on chi-square or Wilcoxon test.
Men had greater odds of death compared to women, adjusted OR 1.38 (95% CI 1.05–1.83; P = 0.022) (Table 2), but there were no significant differences in functional outcomes.
Table 2.
The effect of sex on clinical outcome at three months.
| Outcome | Sex | n/N (%) | OR (95% CI) | P value | Adjusted OR (95% CI)a | P value |
|---|---|---|---|---|---|---|
| Death | F | 126/1187 (10.6) | Reference | |||
| M | 256/2030 (12.6) | 1.22 (0.97–1.52) | 0.092 | 1.38 (1.05–1.83) | 0.022 | |
| Major disabilityb | F | 520/1053 (49.4) | Reference | |||
| M | 792/1752 (45.2) | 0.85 (0.73–0.99) | 0.032 | 0.93 (0.78–1.13) | 0.471 | |
| Death or major disabilityc | F | 646/1179 (54.8) | Reference | |||
| M | 1048/2008 (52.2) | 0.90 (0.78–1.04) | 0.156 | 1.00 (0.83–1.19) | 0.980 | |
| Shift on range of mRS scores | M versus F | 1.09(0.96–1.23) | 0.208 | 1.02 (0.88–1.17) | 0.837 |
CI: confidence interval; F: female; M: male; mRS: modified Rankin scale; OR: odds ratio.
aAdjusted for age, region of recruitment (China versus non-China), history of ischaemic stroke or other undifferentiated stroke, baseline blood glucose (>6.5 versus ≤6.5) and prior use of antihypertension agent(s), National Institutes of Health stroke scale score (<15 versus ≥15), haematoma volume, and randomised BP lowering treatment.
bmRS scores 3–5.
cmRS scores 3–6.
Baseline haematoma volumes were smaller in women (9.9 versus 11.3 ml; P = 0.004), but haematoma location and intraventricular extension were similar in both sexes. Similarly, there was no sex difference in haematoma growth (2.6 versus 3.8 ml; P = 0.164) or perihaematomal oedema growth (3.8 versus 3.9 ml; P = 0.821) at 24 h (Table 3).
Table 3.
Radiological outcomes at 24 h.
| Outcomes | Sex | Mean (95%CI) | P value | Adjusted P valuea |
|---|---|---|---|---|
| Haematoma growth | F | 2.6 (1.7–3.6) | ||
| M | 3.8 (2.7–4.9) | 0.164 | 0.122 | |
| Perihaematomal growth | F | 3.8 (3.0–4.5) | ||
| M | 3.9 (3.3–4.5) | 0.821 | 0.819 |
F: female; M: male.
aAdjusted for age, region of recruitment (China versus non-China), history of ischaemic or other undifferentiated stroke, baseline blood glucose (>6.5 versus ≤6.5), prior use of antihypertensive(s), National Institutes of Health stroke scale score (<15 versus ≥15), haematoma volume and randomised BP lowering treatment.
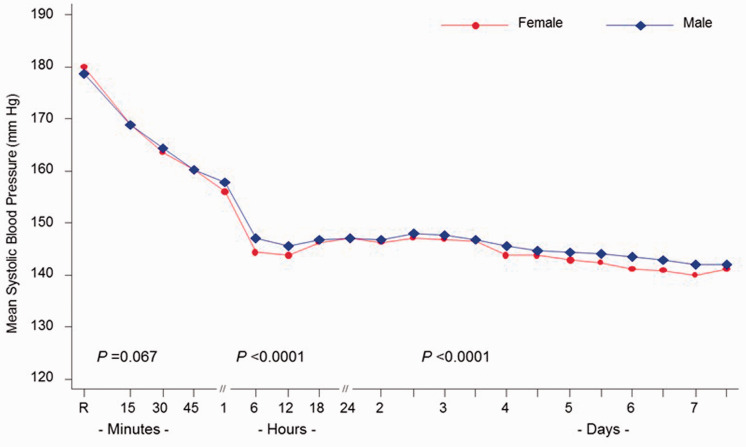
Although there was no significant sex difference in baseline SBP and at 1 h, SBP was marginally lower in women through 24 h (mean difference 1.6 mmHg; P < 0.0001) and seven days (mean difference 1.5 mmHg; P < 0.0001) (Figure 1). There was no heterogeneity in the effect of degree of BP lowering control between the sexes (Supplemental Table 1), nor of significant interactions between treatment and sex for any of the clinical endpoints (Table 2, Supplemental Tables 2–4).
Figure 1.
BP in women and men over seven days.
Discussion
This study, derived from a large international clinical trial database, identified several sex-related differences in demography, risk profile and severity of acute ICH. Although women were older, the results suggest that men have a higher odds of dying compared to women after adjustment for age.
Previous studies are conflicting regarding sex disparities in the outcome from ICH. Some studies have reported increased mortality in men, whereas others report no differences or even higher deaths in women.15 As most such data have been derived from single centres, there are multiple explanations for the differences covering change, bias, confounding and real differences in the biology, sociocultural factors and aspects of management.15 While comorbid factors, such as vascular risk factors,16 may contribute to higher case fatality after ICH in men than women, it may be that women are under-represented in stroke trials.17 As women contributed to only about one-third of the data in the INTERACT studies, it is possible that frailer sicker women were excluded from participation.17 While it has been proposed that men have a greater predisposition to haematoma expansion,18 this was not confirmed in our analyses although men had slightly larger baseline haematoma volumes. Contrary to other studies, we found no differences in haematoma location.
Although more women than men were on prior antihypertensive therapy, men and women had comparable baseline SBP, but women were less likely to be treated with intravenous BP lowering medication which was reflected in significant, albeit small, differences in SBP between men and women in the first 24 h, and over the subsequent 7 days. These findings may reflect more treatment resistant BP or more severe ICH in women, where the natural decline in BP after ICH is less prominent in those with less severe illness.19 Finally, despite greater BP control, there was higher case fatality in men than in women7; however, there was no heterogeneity in the effects of intensive versus guideline BP lowering on clinical outcomes.
Despite several strengths including the large and heterogeneous population, and systematic evaluation of outcomes, our study is limited by being post-hoc and selection bias related to a clinical trial population where the majority of participants were Chinese with mild ICH defined by small haematoma volumes and mild-moderate neurological deficits.
In summary, in our review of a large international clinical trial population, we have shown that men have a greater odds of dying after ICH than women, which could not be readily explained by differing casemix or patterns of BP management.
Supplemental Material
Supplemental material, sj-pdf-1-eso-10.1177_2396987320957513 for Sex differences in treatment, radiological features and outcome after intracerebral haemorrhage: Pooled analysis of Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage trials 1 and 2 by Else Charlotte Sandset, Xia Wang, Cheryl Carcel, Shoichiro Sato, Candice Delcourt, Hisatomi Arima, Christian Stapf, Thompson Robinson, Pablo Lavados, John Chalmers, Mark Woodward and Craig S Anderson in European Stroke Journal
Acknowledgements
We thank all INTERACT participants, investigators and project staff.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: ECS has received speaker fees from Bayer and Novartis. JC has received research grants from Servier, administered through the University of Sydney, as principal investigator for the ADVANCE trial and ADVANCE-ON post-trial study, and also received honoraria from Servier for speaking about those studies at scientific meetings. CSA holds a Senior Investigator Fellowship and grants from the National Health and Medical Research Council (NHMRC), and reports grants and honorarium travel reimbursement from Takeda China.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: The INTERACT studies were funded by Program (358395, 571281) and Project (512402 and 1004170) grants from the NHMRC of Australia.
Ethical approval: The INTERACT1 and INTERACT2 studies were approved centrally by the Ethics Review Committee of Royal Prince Alfred Hospital Zone in Sydney Local Health District, Sydney, Australia and Peking University Health Science Center, Beijing, PR China; and by the ethics committee at each participating hospital site.
Informed consent: Written informed consent was obtained from all patients or appropriate surrogates.
Guarantor: CSA.
Contributorship: CSA developed the concept and rationale for the study; ECS, CC and XW contributed to analyses, SS and CD undertook CT imaging analysis, and XW undertook analyses. All authors contributed to interpretation of the results, drafting and approval of the final manuscript, and take responsibility for the content and interpretation of this article.
Supplemental material: Supplemental material for this article is available online.
ORCID iDs
Else Charlotte Sandset https://orcid.org/0000-0003-4312-4778
Craig S Anderson https://orcid.org/0000-0002-7248-4863
References
- 1.Qureshi AI, Tuhrim S, Broderick JP, et al. Spontaneous intracerebral hemorrhage. N Engl J Med 2001; 344: 1450–1460. [DOI] [PubMed] [Google Scholar]
- 2.Flaherty ML, Haverbusch M, Sekar P, et al. Long-term mortality after intracerebral hemorrhage. Neurology 2006; 66: 1182–1186. [DOI] [PubMed] [Google Scholar]
- 3.Carcel C, Wang X, Sandset EC, et al. Sex differences in treatment and outcome after stroke: pooled analysis including 19,000 participants. Neurology 2019; 93: e2170–e2180. [DOI] [PubMed] [Google Scholar]
- 4.Roquer J, Rodriguez-Campello A, Jimenez-Conde J, et al. Sex-related differences in primary intracerebral hemorrhage. Neurology 2016; 87: 257–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guha R, Boehme A, Demel SL, et al. Aggressiveness of care following intracerebral hemorrhage in women and men. Neurology 2017; 89: 349–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wagner I, Volbers B, Kloska S, et al. Sex differences in perihemorrhagic edema evolution after spontaneous intracerebral hemorrhage. Eur J Neurol 2012; 19: 1477–1481. [DOI] [PubMed] [Google Scholar]
- 7.Qureshi AI, Bliwise DL, Bliwise NG, et al. Rate of 24-hour blood pressure decline and mortality after spontaneous intracerebral hemorrhage: a retrospective analysis with a random effects regression model. Crit Care Med 1999; 27: 480–485. [DOI] [PubMed] [Google Scholar]
- 8.Qureshi AI, Palesch YY, Barsan WG, et al. Intensive blood-pressure lowering in patients with acute cerebral hemorrhage. N Engl J Med 2016; 375: 1033–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson CS, Heeley E, Huang Y, et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med 2013; 368: 2355–2365. [DOI] [PubMed] [Google Scholar]
- 10.Anderson CS, Huang Y, Arima H, et al. Effects of early intensive blood pressure-lowering treatment on the growth of hematoma and perihematomal edema in acute intracerebral hemorrhage: the intensive blood pressure reduction in acute cerebral haemorrhage trial (interact). Stroke 2010; 41: 307–312. [DOI] [PubMed] [Google Scholar]
- 11.Anderson CS, Huang Y, Wang JG, et al. Intensive blood pressure reduction in acute cerebral haemorrhage trial (interact): a randomised pilot trial. Lancet Neurol 2008; 7: 391–399. [DOI] [PubMed] [Google Scholar]
- 12.Delcourt C, Huang Y, Wang J, et al. The second (main) phase of an open, randomised, multicentre study to investigate the effectiveness of an intensive blood pressure reduction in acute cerebral haemorrhage trial (interact2). Int J Stroke 2010; 5: 110–116. [DOI] [PubMed] [Google Scholar]
- 13.Brott T, Adams HP, Jr, Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke 1989; 20: 864–870. [DOI] [PubMed] [Google Scholar]
- 14.Yang J, Arima H, Wu G, et al. Prognostic significance of perihematomal edema in acute intracerebral hemorrhage: pooled analysis from the intensive blood pressure reduction in acute cerebral hemorrhage trial studies. Stroke 2015; 46: 1009–1013. [DOI] [PubMed] [Google Scholar]
- 15.Gokhale S, Caplan LR, James ML. Sex differences in incidence, pathophysiology, and outcome of primary intracerebral hemorrhage. Stroke 2015; 46: 886–892. [DOI] [PubMed] [Google Scholar]
- 16.Xing Y, An Z, Zhang X, et al. Sex differences in the clinical features, risk factors, and outcomes of intracerebral hemorrhage: a large hospital-based stroke registry in China. Sci Rep 2017; 7: 286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carcel C, Woodward M, Balicki G, et al. Trends in recruitment of women and reporting of sex differences in large-scale published randomized controlled trials in stroke. Int J Stroke 2019; 14: 931–938. [DOI] [PubMed] [Google Scholar]
- 18.Marini S, Morotti A, Ayres AM, et al. Sex differences in intracerebral hemorrhage expansion and mortality. J Neurol Sci 2017; 379: 112–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Christensen H, Meden P, Overgaard K, et al. The course of blood pressure in acute stroke is related to the severity of the neurological deficits. Acta Neurol Scand 2002; 106: 142–147. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-eso-10.1177_2396987320957513 for Sex differences in treatment, radiological features and outcome after intracerebral haemorrhage: Pooled analysis of Intensive Blood Pressure Reduction in Acute Cerebral Haemorrhage trials 1 and 2 by Else Charlotte Sandset, Xia Wang, Cheryl Carcel, Shoichiro Sato, Candice Delcourt, Hisatomi Arima, Christian Stapf, Thompson Robinson, Pablo Lavados, John Chalmers, Mark Woodward and Craig S Anderson in European Stroke Journal