Abstract
Background: Young people is a vulnerable period of the emergence of various problems that may occur especially to those who are pregnant. The study was aimed to analyze the determinants of healthcare childbirth among young people in Indonesia in 2017.
Design and Methods: The samples of this study were young people (15-24 yo.) who labored in the last 5 years, and there were 3,235 female young people involved. The study analyzed some variables, such as childbirth healthcare, a type of residence, age, education, employment, marital, parity, wealth, insurance, the autonomy of family finances, the autonomy of health, knowledge of pregnancy danger signs, and ANC. The data were analyzed by binary logistic regression.
Results: Young people in urban were 2.23 times more likely to attend healthcare childbirth than those in rural (95%CI 1.84-2.70). Young people who completed secondary education were 4.12 times more likely to undergo delivery care than no education (95% CI 1.51-11.23). The richest were 5.60 times more likely to experience delivery care than the poorest (95%CI 3.52-8.93). Health insurance gave 1.44 possibilities for undergoing labor and delivery care (95%CI 1.22-1.70). Besides, knowing the danger signs of pregnancy allowed 1.50 times the possibilities for them to access labor and delivery care (95%CI 1.27-1.78). Young people with ANC visits of ≥4 times had more 1.68 times possibilities for taking healthcare childbirth compared to those with that of <4 times (95%CI 1.38-2.06).
Conclusions: The study concluded that the determinants of healthcare childbirth among female adolescents in Indonesia included a residence, education, wealth, insurance, knowledge of pregnancy danger signs, and ANC.
Significance for public health.
We demonstrated the potential for the determinants of healthcare childbirth among female adolescents in Indonesia. We assume that a type of residence, age, education, employment, marital status, parity, wealth, insurance, the autonomy of family finances, the autonomy of health, knowledge of pregnancy danger signs, and antenatal care are predictors of healthcare childbirth among female adolescents. In this article, we show that residence, education, wealth, insurance, knowledge of pregnancy danger signs, and ANC were determinants of healthcare childbirth among female adolescents in Indonesia.
Key words: Adolescent, pregnant, maternal health, childbirth
Introduction
Adolescence is a transitional phase from childhood to adulthood. An adolescent experiences complex life phases, which include biological growth and the transition of major social roles. The previous puberty period accelerated the onset of adolescence in almost all populations, while the understanding of sustainable growth has raised in the late twenties.1
According to the World Health Organization, an adolescent is an individual aged 10-19 years old, while and youth is an individual in the age group of 15-24 years old. However, another reference argued young people are those aged 10-24 years old.2,3 More inclusive definition of adolescence is crucial for the development of laws, social policies, and service systems. The age range of 10-24 years old is more related to young people’s growth and comprehensive understanding of life phases and facilitates a long-term investment in a wider range of settings. That young people are those in the age group of 10-24 years is more in line with the current development of young people.1
Most problems in young people are reproductive health problems. Young people are attributed to strong emotional upheaval due to puberty that always challenges teens to try new things. Data of the 2017 IDHS showed that teenagers in the 15-19 age group have engaged in risky behavior. For example, around 30.2% of teen girls and 33.6% of teen boys started dating when they were less than 15 years old, and about 0.9% of women and 3.6% of men have premarital sex.4 The consequences of pregnancy and childbirth in young people have an impact on the individual, social, and global levels. Individually, young people fertility is associated with adverse maternal and child health problems, including labor problems, low birth weight, delayed fetal growth, and maternal mortality. At the social level, there is a strong relationship between teenage childbirth and a low level of education which negatively intervene in female young people’s social position in the community. Globally, the population will rapidly grow when a woman experiences the first pregnancy in adolescence which can prolong the reproductive period increasing their fertility.5
In developing countries such as Indonesia, one of the cultural characteristics in its society is being tolerant of young people’s marriages. The child marriage rate was still quite high at more than 20.0%, caused by several factors including cultural factors, religious factors, poverty factors, and promiscuity factors.6 Promiscuity factors dominate child marriages in Indonesia. West Sulawesi has the highest rate of early marriages above 19.0%, and the lowest is in Jakarta at 4.0%.6 Trends for marriage dispensation in religious courts have caused the rise of teenage pregnancy.7 Early marriage may occur before the age of 19 years, which is the minimum age of marriage based on Law 16 of 2019 concerning Amendments to Law 1 of 1974 concerning marriage.8
Pregnant young people are one of the vulnerable groups because apart from low knowledge of reproductive health,9 also because their reproductive organs are not ready.10 This reason is sufficient to encourage their deliveries to health care facilities to ensure better delivery output. On the other hand, young people’s knowledge of pregnancy and the danger signs of pregnancy is still low,11 so it is necessary to monitor pregnancy through antenatal care (ANC). This monitoring is needed to monitor the development of young people’s pregnancy. ANC in pregnant young people is also necessary for early detection of problems in pregnancy.12 Based on the background description, this research is aimed to analyze the determinants of healthcare childbirth in Indonesian young people.
Design and Methods
Data source
The study analysis utilized secondary data from the 2017 Indonesian Demographic Data Survey (IDHS). The IDHS was part of an international survey in the series of Demographic and Health Survey (DHS) program conducted by the Inner City Fund (ICF). This survey used stratification and multistage random sampling to select the required samples. The unit of analysis in this study was young people1 in childbearing age (15-24 years), whoever delivered in the last 5 years in Indonesia. The sample size was 3,235 female young people.
Data analysis
Healthcare childbirth referred to the respondents’ acknowledgment of delivery locations in the past five years. Healthcare childbirth if childbirth is carried out at healthcare centers, clinics or maternity hospitals, practices of health workers, and general hospitals. 13 Conversely, it is categorized as non-healthcare childbirth if it does childbirth outside that location.
Independent variables involved a type of residence, age groups, education level, employment status, marital status, parity, wealth status, ownership of health insurance, the autonomy of family finance, the autonomy of health, knowledge of pregnancy danger, and antenatal care (ANC). The residence was divided into 2 categories, which are urban and rural. The age group was categorized into groups of 15-19 years and 20-24 years. Meanwhile, education level consisted of 4 categories, including no education, primary, secondary, and higher. Regarding employment status, there were two categories, such as no employment and employment. Parity status involved primipara (≤1), multipara (2-4), and grand multipara (>4).
Wealth status was determined based on the wealth index calculation. The wealth index was a composite measure of a household’s cumulative living standard, calculated from data of household ownership of selected assets, such as televisions and bicycles; materials used for housing construction; and water and sanitation facilities. This index divides the community into 5 groups: the poorest, poorer, middle, richer, and the richest. Health insurance ownership was categorized as not owning and owning. The autonomy of family finance describes respondents’ independency to allocate money on family financial resources. It was categorized as not having autonomy and having autonomy. The autonomy of health referred to respondents’ independency to determine required health services. The autonomy of health was assessed based on two categories: not having autonomy and having.
Respondents’ knowledge of pregnancy danger signs were measured from some conditions, including prolonged labor, vaginal bleeding, fever, convulsions, wrong fetal position, swollen limbs, faint, breathlessness, tiredness, and others. In this variable, the respondents’ knowledge was categorized as not knowing and knowing. ANC was measured from the frequency of visits to antenatal care during pregnancy in a healthcare facility rated from <4 to ≥4 visits.
At the initial stage of the analysis, all variables were tested using a collinearity test to ensure there was no collinearity between variables. These variables included dichotomous variables so that the chi-square test could determine whether there were significant differences in the utilization of healthcare facilities for delivery. At the final stage binary logistic regression was used because of the nature of the dependent variable. All statistical analyses were performed in SPSS 22 software.
Results
Table 1 displays the results of the collinearity test of all variables in analyzing determinants of labor and delivery care utilization among pregnant young people in Indonesia. Collinearity test results showed that there was no co-linearity between the dependent and independent variables.
The tolerance value of all variables is greater than 0.10, while the variance inflation factor (VIF) value for all variables is less than 10.00. Based on concluding the multicollinearity test, there were no symptoms of multicollinearity in the regression model.
Descriptive results
Table 2 is a descriptive statistic of labor and delivery care among young people in the last five years in Indonesia. Teen respondents who chose non-healthcare facilities for labor and delivery dominantly lived in rural areas, while urban were dominated by those who utilize healthcare facilities. Table 2 informs that regarding the locations of labor and delivery in healthcare facilities or not, young people were mostly in the age group of 20-24 years. Young people with secondary education levels dominated the group of pregnant young people in this study. Mostly, the young people were unemployed, although the number did not differ significantly from the employed category. The number of marriages in the past five years also proved to be statistically insignificant.
Table 1.
Results for the co-linearity test of place of childbirth among young people in Indonesia (n=3,235).
| Variables | Collinearity statistics | |
|---|---|---|
| Tolerance | VIF | |
| Type of residence | 0.808 | 1.238 |
| Age | 0.930 | 1.076 |
| Education level | 0.882 | 1.134 |
| Employment status | 0.973 | 1.028 |
| Marital status | 0.827 | 1.209 |
| Parity | 0.777 | 1.287 |
| Wealth status | 0.741 | 1.350 |
| Health insurance | 0.987 | 1.013 |
| The autonomy of family finances | 0.778 | 1.286 |
| The autonomy of Health | 0.711 | 1.406 |
| Know the dangers of the pregnancy | 0.914 | 1.094 |
| ANC | 0.799 | 1.251 |
VIF, variance inflation factor; ANC, antenatal care; dependent variable: the use of healthcare facilities for delivery.
Table 2 shows that most of the respondents who whether chose to give birth in healthcare facilities or not had primiparous parity. From the perspective of wealth status, the poorest group mostly chose to give birth in non-healthcare facilities, while the poorer groups utilized healthcare facilities for labor and delivery. Young people who utilized non-healthcare facilities had no insurance, but those who gave birth in healthcare facilities were covered by health insurance. In Table 2, the variables of family finance and health autonomy are dominated by autonomous young people who whether utilized healthcare facilities or non-healthcare facilities for labor and delivery. The variables of family finance and health autonomy proved to be not statistically different. Finally, Table 2 shows that those who gave birth in non-healthcare facilities mostly lacked knowledge of pregnancy danger signs. While young people who had adequate knowledge of pregnancy danger signs chose to give birth in healthcare facilities. In both categories of utilizing or not utilizing healthcare facilities for labor and delivery, most of the respondents attended ANC visits of ≥4 times. The variable selection in Table 2 shows that eight variables were tested to find determinants of healthcare childbirth among young people in Indonesia. These variables included a type of residence, age groups, education level, parity, wealth status, health insurance ownership, knowledge of pregnancy danger signs, and ANC visits.
Table 2.
Descriptive statistic of place of childbirth among young people in Indonesia (n=3,235).
| Characteristics | Place of childbirth | p | |||
|---|---|---|---|---|---|
| Non-healthcare facilities | Healthcare facilities | ||||
| n | % | n | % | ||
| Type of residence | <0.001 | ||||
| - Urban | 223 | 21.8% | 1133 | 51.2% | |
| - Rural (ref.) | 798 | 78.2% | 1081 | 48.8% | |
| Age groups | 0.010 | ||||
| - 15-19 (ref.) | 161 | 15.8% | 275 | 12.4% | |
| - 20-24 | 860 | 84.2% | 1939 | 87.6% | |
| Education level | <0.001 | ||||
| - No education (ref.) | 25 | 2.4% | 5 | 0.2% | |
| - Primary | 308 | 30.2% | 337 | 15.2% | |
| - Secondary | 636 | 62.3% | 1688 | 76.2% | |
| - Higher | 52 | 5.1% | 184 | 8.3% | |
| Employment status | 0.834 | ||||
| - No Employed | 707 | 69.2% | 1525 | 68.9% | |
| - Employed | 314 | 30.8% | 689 | 31.1% | |
| Marital status | 0.897 | ||||
| - Never married | 8 | 0.8% | 15 | 0.7% | |
| - Married | 961 | 94.1% | 2092 | 94.5% | |
| - Divorced | 52 | 5.1% | 107 | 4.8% | |
| Parity | <0.001 | ||||
| - Primipara | 585 | 57.3% | 1616 | 73.0% | |
| - Multipara | 434 | 42.5% | 596 | 26.9% | |
| - Grandemultipara (ref.) | 2 | 0.2% | 2 | 0.1% | |
| Wealth status | <0.001 | ||||
| - Poorest (ref.) | 592 | 58.0% | 521 | 23.5% | |
| - Poorer | 216 | 21.2% | 535 | 24.2% | |
| - Middle | 122 | 11.9% | 510 | 23.0% | |
| - Richer | 68 | 6.7% | 397 | 17.9% | |
| - Richest | 23 | 2.3% | 251 | 11.3% | |
| Covered by health insurance | <0.001 | ||||
| - No (ref.) | 517 | 50.6% | 883 | 39.9% | |
| - Yes | 504 | 49.4% | 1331 | 60.1% | |
| The autonomy of family finances | 0.981 | ||||
| - No | 315 | 30.9% | 684 | 30.9% | |
| - Yes | 706 | 69.1% | 1530 | 69.1% | |
| The autonomy of health | 0.223 | ||||
| - No | 198 | 19.4% | 390 | 17.6% | |
| - Yes | 823 | 80.6% | 1824 | 82.4% | |
| Know the danger signs of pregnancy | <0.001 | ||||
| - No (ref.) | 541 | 53.0% | 746 | 33.7% | |
| - Yes | 480 | 47.0% | 1468 | 66.3% | |
| ANC visits | < 0.001 | ||||
| - < 4 times (ref.) | 389 | 38.1% | 427 | 19.3% | |
| - ≥ 4 times | 632 | 61.9% | 1787 | 80.7% | |
Figure 1 shows the distribution of labor and delivery care among young people based on the categories of health insurance ownership and wealth status in Indonesia. Young people who experienced labor and delivery care had health insurance that was more evenly distributed in all levels of wealth status.
Multivariate regression analysis
Table 3 is the result of the binary logistic regression test for finding determinants of labor and delivery care among young people in Indonesia. The test chose the “non-healthcare facilities” category as a reference.
The binary logistic regression test found six variables as the determinants of healthcare childbirth among young people in Indonesia, such as a type of residence, education level, wealth status, health insurance ownership, knowledge of pregnancy danger signs, and ANC visits. Young people in urban areas were 2.23 times more likely to utilize labor and delivery care in healthcare facilities than those in rural areas (OR 2.23; 95%CI 1.84-2.70). Based on education level, those who completed secondary education had more 4.12 times the possibilities to utilize healthcare facilities for delivery than those with no education (OR 4.12; 95%CI 1.51-11.23). Meanwhile, the higher education was 3.95 times more likely to experience labor and delivery care in healthcare facilities than no education (OR 3.95; 95%CI 1.37-11.36). Young people with poorer wealth status had 2.044 times the possibilities of utilizing labor and delivery care in healthcare facilities compared to the poorest (OR 2.04; 95%CI 1.66-2.52). Moreover, young people with middle wealth status were 2.91 times the possibility to give birth in healthcare facilities compared to the poorest (OR 2.91; 95%CI 2.28-3.73). There were 3.41 times possibilities for young people to utilize healthcare facilities for labor and delivery case than the poorest (OR 3.41; 95%CI 2.51-4.64). In comparison, the richest had 5.60 times the possibilities to give birth in healthcare facilities than the poorest (OR 5.60; 95%CI 3.52-8.93). Furthermore, young people whose healthcare needs are covered by health insurance had more 1.44 times possibilities of labor and delivery in healthcare facilities than uninsured young people (OR 1.44; 95%CI 1.22-1.70). Knowing pregnancy danger signs gave young people 1.50 times possibilities of labor and delivery in healthcare facilities compared to young people who lacked the knowledge (OR 1.50; 95%CI 1.27-1.78). Young people who visited ANC for ≥4 times were 1.68 times more likely to labor and deliver in healthcare facilities compared to those who participated in ANC less than 4 times (OR 1.68; 95%CI 1.38-2.06).
Figure 1.
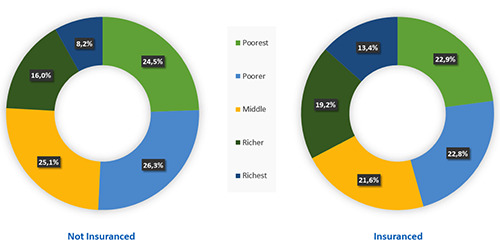
Distribution of healthcare childbirth among young people by health insurance ownership and wealth status in Indonesia, 2017.
Table 3.
Binary Logistic Regression of healthcare childbirth among young people in Indonesia (n=3,235).
| Predictor | Healthcare facilities | |||
|---|---|---|---|---|
| p | OR | Lower bound | Upper bound | |
| Type of residence: Urban | <0.001 | 2.228 | 1.838 | 2.702 |
| Type of residence: Rural | - | - | - | - |
| Age group: 15-19 | - | - | - | - |
| Age group: 20-24 | 0.159 | 1.193 | 0.933 | 1.524 |
| Education level: No Education | - | - | - | - |
| Education level: Primary | 0.085 | 2.429 | 0.885 | 6.662 |
| Education level: Secondary | 0.006 | 4.123 | 1.514 | 11.225 |
| Education level: Higher | 0.011 | 3.948 | 1.372 | 11.356 |
| Parity: Primipara | 0.371 | 0.403 | 0.055 | 2.953 |
| Parity: Multipara | 0.204 | 0.275 | 0.037 | 2.014 |
| Parity: Grande multipara | - | - | - | - |
| Wealth status: Poorest | - | - | - | - |
| Wealth status: Poorer | <0.001 | 2.044 | 1.656 | 2.523 |
| Wealth status: Middle | <0.001 | 2.914 | 2.275 | 3.731 |
| Wealth status: Richer | <0.001 | 3.411 | 2.508 | 4.640 |
| Wealth status: Richest | <0.001 | 5.602 | 3.515 | 8.928 |
| Covered by health insurance: No | - | - | - | - |
| Covered by health insurance: Yes | <0.001 | 1.441 | 1.220 | 1.704 |
| Know the danger signs of pregnancy: No | - | - | - | - |
| Know the danger signs of pregnancy: Yes | <0.001 | 1.502 | 1.266 | 1.783 |
| ANC visits: <4 times | - | - | - | - |
| ANC visits: ≥4 times | <0.001 | 1.684 | 1.379 | 2.056 |
ANC, antenatal care.
Discussion
Premarital sexual relations for the first time are mostly due to mutual love, of which 46.1% and 53.8% occur to men and women respectively. Women (15.8%) rarely had a premarital sexual relation, and 16.3% of them were forced to do it. The data also showed that 16.4% of female adolescents had unwanted pregnancies, around 7% of those aged 15-19 became mothers, 5.0% gave birth, and 2.0% got pregnant for the first time.4 This shows the lack of understanding about reproductive health and the risk of sexual relations in young people. Meanwhile, young people, especially female ones who still attend schools, hardly reject unwanted relationships which resulted in many unwanted pregnancies, leading to unsafe abortion and teenage pregnancy which would increase the risk of maternal and infant mortality.
The analysis showed that young people in urban areas had a better opportunity to labor and deliver in healthcare facilities than those in rural areas. This result corresponded with that of other studies in Indonesia which found that community access to healthcare facilities in urban areas was better. Urban areas provide better public facilities and more massive development for better physical access.14,15
This study also discovered a better education level gave better possibilities of utilizing healthcare facilities for labor and delivery care. Better education level makes individuals better understand their needs.16-18 Several research findings explained education level is one of the determinants for improving public access to healthcare facilities.19,20 Not only for women but also does this condition apply to men and the whole family.21
Regarding wealth status, the higher wealth status gave more proportion for young people to utilize labor and delivery care in healthcare facilities. Research in Guinea-Bissau,22 Ethiopia,23 and India24 also showed consistent results. The better individual’s wealth status, the better access to healthcare facilities.22,25 Better wealth status reduces the barrier to paying for health care costs, including costs for transportation to health care facilities.14
Health insurance ownership became a determinant of labor and delivery care in healthcare facilities. Young people who had health insurance had a better opportunity to utilize healthcare facilities. Similarly, the government has a goal to issue a policy for achieving gradually universal health coverage in Indonesia, which was expected to reduce barriers to service access, especially health costs.26 It remains as a challenge of physical access since Indonesia has archipelagic characteristics.12,27 Previous studies have informed the difficulty of accessing health services in border areas and islands in Indonesia.28,29
This current study pointed out that young people who had enough knowledge of pregnancy danger signs had a better possibility of utilizing healthcare facilities. A study in Myanmar found that women over 35 years old and who received training on maternal health last year had better knowledge of pregnancy danger signs.30 It means training on maternal health is necessary for pregnant female young people. Teenage pregnancy results in a lack of knowledge. In Indonesia, pregnant classes have been conducted to reduce the impact of young people’s pregnancy.11,31 The knowledge of danger signs make pregnant young people more aware of what can happen during childbirth so that it can encourage them to deliver to healthcare facilities.11
The results of this present study prove that young people who made ANC visits ≥4 times had a higher chance of utilizing labor and delivery care in healthcare facilities. ANC provides maternal health services that ensure the best pregnancy outcomes for women and their babies.32 The more frequently pregnant women interact with health workers during the ANC, the greater the possibility of childbirth in healthcare facilities.25 Additionally, full participation of ANC and safe delivery care were associated with the increased use of postnatal care.33 In ANC, pregnant women can receive nutritional interventions, assessment of the condition of the mother and fetus, preventive measures, and interventions for general psychological symptoms, as well as health system interventions to improve the function and quality of the ANC. In Indonesia, pregnant women are required to have a Maternal and Child Health book, and always carry them every time they make an ANC visit.12
Among all findings that corresponded with other studies, this study had a limitation in the data analysis which was only based on the survey data, so we cannot dig deeper into the reasons young people do not do healthcare childbirth. Further qualitative studies are required to further verify the findings based on the quantitative measurement in this study.
Conclusions
This study concluded six determinants of healthcare childbirth among young people in Indonesia. These determinants included a type of residence, education level, wealth status, health insurance ownership, knowledge of pregnancy danger signs, and ANC visits. The results of this study provide specific targets for the government to intervene in rural areas in young people with low education, low wealth status, uninsured, and do not know the danger signs of pregnancy. This intervention needs to be done to be able to encourage the coverage of pregnant young people who deliver in healthcare facilities. The government also needs to provide a mobile unit for maternal health services in peripheral areas with poor access.
Acknowledgments
The author would like to thank the Inner City Fund for allowing the use of the 2017 IDHS.
References
- 1.Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. Lancet Child Adolesc Health 2018;2:223–8. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Adolescent health in the South- East Asia Region. 2019. [cited 2020 Feb 7]. Available from: https://www.who.int/southeastasia/health-topics/adolescenthealth [Google Scholar]
- 3.World Health Organization. Regional Office for South-East Asia. Strategic Guidance on Accelerating Actions for Adolescent Health in South-East Asia Region (2018–2022). New Delhi; 2018. p. 13. [Google Scholar]
- 4.BKKBN. Indonesia Demographic and Health Survey 2017: Adolescent Reproductive Health. Jakarta; 2018. [Google Scholar]
- 5.Raharja M. Adolescent fertility in Indonesia (Fertilitas remaja di Indonesia). Kesmas J Kesehat Masy Nas 2014;9:6–13. [Google Scholar]
- 6.Harianja AJ.. Early marriage rates in indonesia are still high (Angka Pernikahan Dini di Indonesia Masih Tinggi) [in Indonesian]. 2019. [cited 2020 Feb 4]. p. 1. Available from: https://www.idntimes.com/news/indonesia/axel-harianja/bkkbn-angka-pernikahan-dini-di-indonesia-masihtinggi/full [Google Scholar]
- 7.Ahyani S.. [Religious court considerations for early marriage marriage dispensation due to pregnancy outside marriage].[Article in Indonesian]. J Wawasan Huk 2016;34:1-7. [Google Scholar]
- 8.Republic of Indonesia. Law Number 16 of 2019 concerning Amendments to Law 1 of 1974 concerning Marriage [in Indonesian]. 2019. p. 1–30. [Google Scholar]
- 9.Wulandari RD, Laksono AD. Education as predictor of the knowledge of pregnancy danger signs in Rural Indonesia. Int J Innov Creat Chang 2020;13:1037–51. [Google Scholar]
- 10.Handayani OWK, Wiranti I, Raharjo BB, Nugroho E. The reproduction health behavior of high school teenagers in Semarang, Indonesia. Open Public Health J 2019;12:309-14. [Google Scholar]
- 11.Wulandari RD, Laksono AD. Determinants of knowledge of pregnancy danger signs in Indonesia. PLoS One 2020;15: e0232550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laksono AD, Rukmini R, Wulandari RD. Regional disparities in antenatal care utilization in Indonesia. PLoS One 2020;15:e0224006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ministry of Health of the Republic of Indonesia. Republic of Indonesia Minister of Health Regulation Number 99/2015 concerning Health Services at National Health Insurance. Indonesia; 2015. [Google Scholar]
- 14.Laksono AD, Wulandari RD, Soedirham O. Urban and rural disparities in hospital utilization among Indonesian adults. Iran J Public Health 2019;48:247–55. [PMC free article] [PubMed] [Google Scholar]
- 15.Wulandari RD, Laksono AD. Urban-rural disparity: The utilization of primary health care center among elderly in East Java, Indonesia. Indones J Health Adm 2019;7:147–54. [Google Scholar]
- 16.Tille F, Rottger J, Gibis B, et al. Patients’ perceptions of health system responsiveness in ambulatory care in Germany. Patient Educ Couns 2019;102:162–71. [DOI] [PubMed] [Google Scholar]
- 17.Laksono AD, Wulandari RD. The barrier to maternity care in rural Indonesia. J Public Health (Berl.) 2020. doi: 10.1007/s10389-020-01274-3 [Google Scholar]
- 18.Laksono AD, Wulandari RD, Efendi F. Determinants of hospital utilisation among urban poor societies in Indonesia. Int J Innov Creat Chang 2020;12:375–87. [Google Scholar]
- 19.Izudi J, Akwang DG, McCoy SI, et al. Effect of health education on birth preparedness and complication readiness on the use of maternal health services: A propensity score-matched analysis. Midwifery 2019;78:78–84. [DOI] [PubMed] [Google Scholar]
- 20.Luy M, Zannella M, Wegner-Siegmundt C, et al. The impact of increasing education levels on rising life expectancy: a decomposition analysis for Italy, Denmark, and the USA. Genus 2019;75:11. [Google Scholar]
- 21.Gize A, Eyassu A, Nigatu B, et al. Men’s knowledge and involvement on obstetric danger signs, birth preparedness and complication readiness in Burayu town, Oromia region, Ethiopia. BMC Pregnancy Childbirth 2019;19:515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yaya S, Bishwajit G, Gunawardena N. Socioeconomic factors associated with choice of delivery place among mothers: A population-based cross-sectional study in Guinea-Bissau. BMJ Glob Health 2019;4:e001341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woldeamanuel BT, Gelebo KK. Statistical analysis of socioeconomic and demographic correlates of perinatal mortality in Tigray region, Ethiopia: A cross sectional study. BMC Public Health 2019;19:1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barman B, Saha J, Chouhan P. Impact of education on the utilization of maternal health care services: An investigation from National Family Health Survey (2015–16) in India. Child Youth Serv Rev 2020;108:104642. [Google Scholar]
- 25.Tsawe M, Sathiya Susuman A. Factors associated with the upsurge in the use of delivery care services in Sierra Leone. Public Health 2020;180:74–81. [DOI] [PubMed] [Google Scholar]
- 26.Dewi A, Mukti AG. The strategy to achieve universal health coverage membership in Indonesia. Res J Pharm Technol 2018;11:1774–7. [Google Scholar]
- 27.Laksono AD, Wulandari RD, Soedirham O. Regional disparities of health center utilization in rural Indonesia. Malaysian J Public Heal Med 2019;19:158-66. [Google Scholar]
- 28.Suharmiati S, Laksono AD, Astuti WD. [Policy review on health services in primary health center in the border and remote area].[Article in Indonesian]. Bull Heal Syst Res 2013;16:109-16. [Google Scholar]
- 29.Senewe FP, Elsi E. Descriptive Analysis to environment health in less development, borderlands, archipelagoes and remote areas (DTPK-T). Media Litbangkes 2014;24:153–60. [Google Scholar]
- 30.Than KK, Morgan A, Pham MD, et al. Determinants of knowledge of critical danger signs, safe childbirth and immediate newborn care practices among auxiliary midwives: A cross sectional survey in Myanmar. BMJ Open 2017;7:e017180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Puspita Y, Susanti E. [Counseling for pregnant women classes about P4K].[Article in Indonesian]. J Media Kesehat 2017;10:78–83. [Google Scholar]
- 32.Jinga N, Mongwenyana C, Moolla A, et al. Reasons for late presentation for antenatal care, healthcare providers’ perspective. BMC Health Serv Res 2019;19:1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Iacoella F, Tirivayi N. Determinants of maternal healthcare utilization among married adolescents: Evidence from 13 Sub- Saharan African countries. Public Health 2019;177:1-9. [DOI] [PubMed] [Google Scholar]
- 34.Indonesian Ministry of Health Data and Information Center. Guidelines for National Standards for Adolescent Health Care Services (Pedoman Standar Nasional Pelayanan Kesehatan Peduli Remaja) [in Indonesian]. Jakarta: Indonesian Ministry of Health; 2018. 1–40 p. Available from: http://kesga.kemkes.go.id/images/pedoman/BukuSNPKPR2018.pdf [Google Scholar]


