A 30-year-old female patient underwent bilateral photorefractive keratectomy (PRK) with mitomycin C (MMC) application to correct compound myopic astigmatism of -8.50,-0.50@60, and -2.25, 1.00@70 in her right eye (RE) and left eye (LE), respectively. RE pachymetry was 513 μm and the anterior chamber depth was 2.57 mm and hence PRK with MMC application was considered. MMC 0.02% was applied for 90 s in RE and 30 s in LE. At 1 month, uncorrected visual acuity (UCVA) was 20/20 in both eyes. However, at 2 months, her RE UCVA dropped to 20/80. Examination showed dense reticular haze (grade 3)[1] [Fig. 1]. The central corneal thickness was 382 μm in the RE [Fig. 2]. Anterior segment optical coherence tomography (OCT) showed intense hyperreflectivity at the level of the epithelial basement membrane corresponding to the haze and undulation of the anterior edge of this scar tissue [Fig. 3]. After an initial failed course of topical corticosteroids, she underwent phototherapeutic keratectomy (PTK) + PRK 6 months after PRK, using the trans-PTK mode for ablation of 50 μ and PRK for 40 μ ablation and MMC was applied for 30 s. At 3 months post PTK, UCVA was 20/30, (20/20 with-0.50,-0.50@60) [Table 1]. No further regression or increase in the haze was noted 18 months after retreatment.
Figure 1.
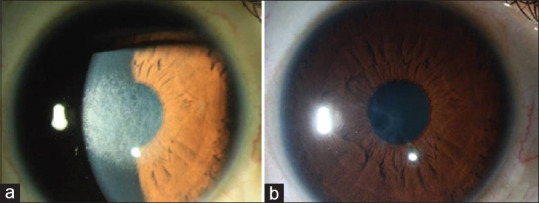
RE slit-lamp photograph with evident grade 4 haze 6 months after PRK (a), and 3 months after PTK + PRK + MMC (b), the corneal opacity is remarkably reduced
Figure 2.
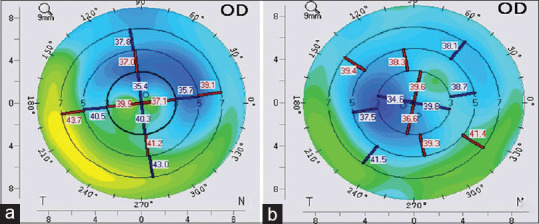
Right eye video keratography maps before (a) and 3 months after (b) PTK + PRK + MMC for treatment of post-PRK haze. The topographic pattern highlights the more regularized corneal profile
Figure 3.
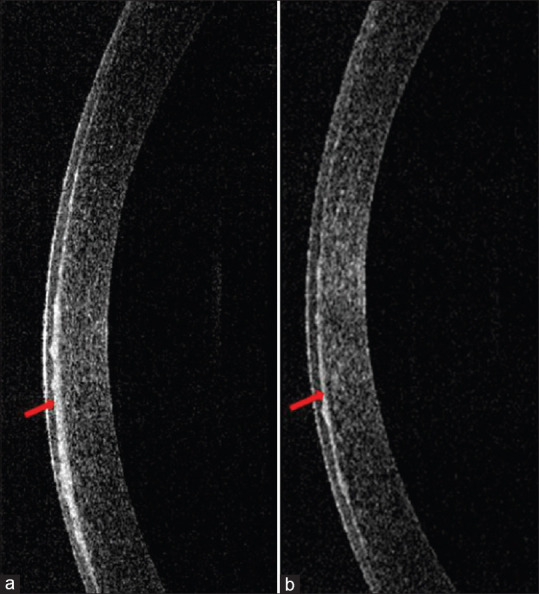
ASOCT pictures before (a) and 3 months after PTK + PRK + MMC (b). The hyperreflectivity at basement membrane level (arrow) is reduced in intensity (arrow) post-laser retreatment
Table 1.
Temporal changes in visual acuity, refractive correction, and slit-lamp haze grading after sequential PRK and PTK + PRK + MMC procedures
| Right eye | UCVA | BCVA | Spherical equivalent | Haze |
|---|---|---|---|---|
| Preoperative | 20/600 | 20/25 | -9.00 | 0 |
| 2 months post PRK | 20/80 | 20/25 | -1.75 | 3 |
| 6 months post PRK | 20/100 | 20/25 | -2.50 | 4 |
| Post PTK + PRK | 20/30 | 20/20 | -0.75 | 2 |
Discussion
PRK is a safe surgical procedure for effectively reducing refractive errors but refractive regression and corneal haze are known complications that can affect the outcome.[2] The risk factors for post-PRK haze include higher degrees of myopia and astigmatism, hyperopic corrections, and younger age.[3] The symptoms associated with haze are disabling glare and impairment of visual acuity. Intraoperative MMC use has a protective role. Post-PRK haze can be treated with topical steroids if mild, but in a dense haze, surgical management is required.[4] The various techniques include either manual debridement or PTK and MMC application.[5] Our case had risk factors of high myopia and deeper ablation, which led to haze but could be successfully treated with PTK, PRK, and intraoperative MMC application.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Hyderabad Eye Research Foundation.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Heitzmann J, Binder PS, Kassar BS, Nordan LT. The correction of high Myopia using the excimer laser. Arch Ophthalmol. 1993;111:1627–34. doi: 10.1001/archopht.1993.01090120049021. [DOI] [PubMed] [Google Scholar]
- 2.Kaiserman I, Sadi N, Mimouni M, Sela T, Munzer G, Levartovsky S. Corneal breakthrough haze after photorefractive keratectomy with Mitomycin C: Incidence and risk factors. Cornea. 2017;36:961–6. doi: 10.1097/ICO.0000000000001231. [DOI] [PubMed] [Google Scholar]
- 3.Ang BC, Foo RC, Lim EW, Tan MM, Nah GK, Thean LS, et al. Risk factors for early-onset corneal haze after photorefractive keratectomy in an Asian population: Outcomes from the Singapore Armed Forces Corneal Refractive Surgery Programme 2006 to 2013. J Cataract Refract Surg. 2016;42:710–6. doi: 10.1016/j.jcrs.2016.01.047. [DOI] [PubMed] [Google Scholar]
- 4.Tengroth B, Epstein D, Fagerholm P, Hamberg-Nystrom H, Fitzsimmons TD. Excimer laser photorefractive keratectomy for myopia. Clinical results in sighted eyes. Ophthalmology. 1993;100:739–45. doi: 10.1016/s0161-6420(93)31581-2. [DOI] [PubMed] [Google Scholar]
- 5.Seiler T, Derse M, Pham T. Repeated excimer laser treatment after photorefractive keratectomy. Arch Ophthalmol. 1992;110:1230–3. doi: 10.1001/archopht.1992.01080210048021. [DOI] [PubMed] [Google Scholar]


