Abstract
Laser refractive surgery (LRS) is one of the most demanding areas of ophthalmic surgery and high level of precision is required to meet outcome expectations of patients. Post-operative recovery is of vital importance. Keratitis occurring after LRS can delay visual recovery. Both surface ablations [Photorefractive keratectomy (PRK)] as well as flap procedures [Laser in-situ keratomileusis (LASIK)/Small incision lenticule extraction] are prone to this complication. Reported incidence of post-LRS infectious keratitis is between 0% and 1.5%. The rate of infections after PRK seems to be higher than that after LASIK. Staphylococci, streptococci, and mycobacteria are the common etiological organisms. About 50–60% of patients present within the first week of surgery. Of the non-infectious keratitis, diffuse lamellar keratitis (DLK) is the most common with reported rates between 0.4% and 4.38%. The incidence of DLK seems to be higher with femtosecond LASIK than with microkeratome LASIK. A lot of stress is laid on prevention of this complication through proper case selection, asepsis, and use of improved protocols. Once keratitis develops, the right approach can help resolve this condition quickly. In cases of suspected microbial keratitis, laboratory identification of the organism is important. Most lesions resolve with medical management alone. Interface irrigation, flap amputation, collagen cross-linking and therapeutic penetrating keratoplasty (TPK) are reserved for severe/non-resolving cases. About 50–75% of all infectious keratitis cases post LRS resolve with a final vision of 20/40 or greater. Improved awareness, early diagnosis, and appropriate intervention can help limit the damage to cornea and preserve vision.
Keywords: Infections, keratitis, refractive surgery
Laser vision correction is a rapidly evolving area of ophthalmic surgery that demands a high level of precision. Being a surgery that is elective and not urgent, it is all the more important that the outcomes are satisfactory and that every surgery must be free from complications. Since most of these procedures are done for cosmetic reasons and the candidates are young in the most productive age group, the outcome expectations are high.[1] In this context; any untoward affection of the cornea postoperatively is of grave concern to both patients and clinicians. Many of these complications can result in a loss of best spectacle-corrected visual acuity.[2,3] Therefore, a lot of stress is laid on prevention of these complications through proper case selection, asepsis, and use of improved technology and protocols. All of these measures have enhanced the safety index of refractive surgery procedures.[4] But complications do occur. In such situation, awareness of these complications, early diagnosis, and appropriate intervention will help limiting the damage to cornea and preserve vision.[4] In this review article we will discuss one such complication associated with refractive surgery– Keratitis.
Epidemiology
Keratitis occurring post-laser refractive surgery can be divided into two broad groups of infectious and non-infectious etiology.[5] The reported infectious agents include bacteria, fungi, herpes simplex viruses, and acanthamoeba. The non-infectious group includes diffuse lamellar keratitis (DLK) and staphylococcal marginal hypersensitivity (SMH).[5,6]
Risk factors
Various epidemiological studies suggest that the risk of corneal inflammation in refractive surgery is high in patients with predisposing factors. Pre-existing dry eyes, blepharitis, meibomian gland dysfunction (MGD), history of previous healed keratitis, and previous corneal surgery have been recognized as risk factors.[7] Meticulous treatment of these conditions is essential before surgery. Enough time should be given for ocular surface stabilization prior to refractive surgery. Intraoperative contamination can occur due to poor adnexal preparation, contamination of the surgical area or contaminated instruments.[4] Hence a povidone–iodine solution (Betadine 10%) preparation (painting of the eyelids and periocular region, and cleaning of eye lashes) before surgery is recommended, similar to that prior to cataract surgery.[4] The practice of utilizing re-usable blades, same instruments for bilateral surgery and same surgical gowns/gloves for consecutive patients are risk factors predisposing to infection. Several infectious outbreaks have been associated with the use of contaminated instruments and supplies including unsterile saline.[8,9] The guidelines for cleaning and sterilization of intraocular surgical instruments have been described in detail by the 2018 report of the Ophthalmic Instrument Cleaning and Sterilization (OICS) Task Force. This report recommends standard techniques to follow for multiple aspects like instrument cleaning, instrument transportation, utilization of water type for cleansing, sterilizer maintenance, and usage of sterilization cycle type.[10] Excessive intraoperative tissue handling and epithelial defects also increase infection risk. Post-operatively, delayed epithelialization, use of excessive corticosteroids, improper use of antibiotics, exposure to impure water or a traumatic event can predispose to infection and inflammation.[11] Table 1 describes different measures to reduce the occurrence of post-refractive surgery keratitis.
Table 1.
Measures to reduce occurrence of keratitis post laser refractive surgery
| Before surgery | During surgery | Post surgery | |||
|---|---|---|---|---|---|
| Aspect | Management | Aspect | Prevention/Management | Aspect | Management |
| Dry eyes: Foreign body sensation/light sensitivity/discomfort/TFBUT <10 sec/Schirmer’s <10 mm | - Lubricating eye drops and gels (CMC/HPMC/PEG + PG/Sodium Hyaluronate) | Tissue handling | - Adequate surgical training/supervised surgeries for new surgeons | Epithelial defects | Bandage contact lens/4th generation fluoroquinolone (moxifloxacin eye drops)/restrict use of topical corticosteroids till the epithelial defect heals |
| - Rule out Sjogren’s syndrome/neurotrophic conditions/ocular surface diseases/vitamin deficiencies/lacrimal disorders | - Careful flap lifting (LASIK) and stromal dissection (SMILE) techniques | ||||
| - Avoiding high-energy ablations | |||||
| Blepharitis/MGD: Irritation/itching/blocked meibomian orifices/frothy secretions/eyelid crusts | Warm compresses/lid massage, antibiotic ointment (chloramphenicol/azithromycin), systemic doxycycline in severe cases | Sterility | - Adequate preparation of ocular adnexa with 10% povidone iodine solution at least 10 minutes prior to surgery | Follow-up and care | - Regular follow-up; at least a minimum of 3 in the first month on post- operative day 1, day 7 and day 30 |
| - Disposable gloves/gowns/surgical drapes | - At each visit, look for persistent epithelial defects/corneal infiltration/any visual loss | ||||
| - A 3 monthly quality check of autoclave units | - Reinforce importance of eye drop administration/avoiding exposure to dust/contaminated water/irritants | ||||
| - Pure and contaminant free water to clean instruments | |||||
| - Avoiding re-usable blades | |||||
| - Different set of instruments for each eye | |||||
TFBUT=Tear film break up time, MGD=Meibomian gland dysfunction, CMC=Carboxymethylcellulose, HPMC=Hydroxypropylmethylcellulose, PEG=Polyethylene glycol, PG=Propylene glycol, LASIK=Laser in-situ keratomileusis, SMILE=Small incision lenticule extraction
Infectious keratitis
The reported incidence of infectious keratitis is between 0.02% and 0.8% after photorefractive keratectomy (PRK) and between 0% and 1.5% after laser in-situ keratomileusis (LASIK).[7,12,13,14,15] Different sources of data, different time periods of studies conducted as well as use of different antibiotics attribute to this wide range of incidence. A group from Spain demonstrated rates of 0.031% in the largest series (more than 200000 eyes) of infectious keratitis after LASIK reported till 2010.[15] This rate was reduced to 0.011% after the introduction of topical moxifloxacin in addition to tobramycin in their post-operative protocol.[16] The American society of cataract and refractive surgery (ASCRS) conducted a survery of post-refractive surgery infectious keratitis in 2008 that calculated an overall incidence of about 0.001%.[4] In a recent report by Schallhorn et al., for all procedures the incidence of suspected or confirmed infectious keratitis after laser vision correction surgery was 0.0057% per procedure. Definite or probable microbial keratitis occurred in 26/564165 eyes and 11/81792 eyes after LASIK and PRK respectively, i.e., an overall incidence of 0.0046% and 0.013% after LASIK and PRK respectively. PRK had a significantly higher incidence of microbial keratitis than LASIK with a hazard ratio of 2.92.[14] Previous studies also report the rate of infectious keratitis after PRK to be five to six times higher than that after LASIK.[12,16] The association between PRK and the increased risk for infectious keratitis is due to the large epithelial defect that the procedure creates and the use of a post-operative bandage contact lens. Reports after small incision lenticule extraction (SMILE) surgery are not many. Few case series suggest an incidence of 0.003% and 0.004% respectively.[17,18]
The time of onset of keratitis is an important determinant of its type. It can be divided into early onset (within one week of surgery) and late-onset (beyond one week). About 50–60% of patients present within the first week of surgery.[15,19] Hence carefully monitoring the postoperative course in the first week is important. Early-onset cases are usually caused by staphylococci/streptococci while late-onset cases are usually caused by slow-growing organisms like mycobacteria, nocardia, acanthamoeba, and fungi.[5] Staphylococci and atypical mycobacteria have been the most commonly isolated organisms till date.[5,7,14,15,20] Non-tuberculous mycobacteria (NTM) are known to cause outbreaks of infectious keratitis.[9,21,22] NTM induced post-LASIK keratitis may be caused due to suboptimal pre-surgical preparation of patients/multiple uses of microkeratome blades/use of contaminated water or inefficient techniques to sterilize surgical instruments.[7,20] Intraoperative NTM contamination owing to the ice that was used to chill syringes for saline solution (for intraoperative lavage) has been reported post LASIK.[23] Cases of MRSA (Methicillin-resisitant staphylococcus aureus) have also been reported. Solomon et al. reported 12 patients with infectious keratitis caused by MRSA in which 9/12 patients were exposed to a health care setting.[24] In tropical regions, uncommon organisms such as fungi, nocardia and acanthamoeba have been incriminated as causes of keratitis post LASIK.[25]
Non-infectious keratitis
Staphylococcal marginal hypersensitivity is usually associated with PRK rather than LASIK; a history of rosacea and/or blepharitis is usually present.[5] Cases of diffuse lamellar keratitis (DLK) usually occur in the initial 24-72-hour post-operative period. Although rare, late cases have also been reported.[26] The rates of DLK range from 0.4% to 4.38% in various studies.[27] In the study by Moshirfar et al., the overall occurrence of post-LASIK keratitis was 2.66%, with DLK being most common. The occurrence of non-infectious keratitis (2.34%) was 7.5 times greater than infectious keratitis (0.31%).[5] Epithelial defects have a significant association with DLK.[28,29] Major epithelial defects (larger than 4 mm and located in the center of the cornea) usually cause DLK progression to grade three or four, while minor ones (smaller than 2 mm located outside the central optical zone), idiopathic, blood-interface reactions etc., usually do not cause DLK beyond grade one.[5] Outbreaks of DLK have been associated with surgical glove contamination and cassette sterilization systems with reservoirs.[27,30] The incidence of DLK seems to be higher with femtosecond LASIK than with conventional microkeratome LASIK, possibly due to the higher amount of laser energy delivered in the former procedure.[31] This is in contrast with infectious keratitis that is more common with microkeratome LASIK than with Femtosecond LASIK.[4] Newer data does suggest that the over all incidence of post-LASIK infectious keratitis is declining over the years.[3]
Clinical Features
Infectious keratitis
The clinical presentation of an infectious keratitis is based on the type of causative organism as well as location of the infection. Staphylococci, streptococci and mycobacteria are some of the common organisms. Herpes simplex viruses, acanthamoeba, pseudomonas, nocardia and fungi are among the other pathogens. Polymicrobial infections have also been reported.[4] Herpetic keratitis can present as a primary infection or reactivation of a previous episode.[32]
A post-laser refractive surgery infection may initially present as a single dense white infiltrate or multiple patchy infiltrates that progressively increase in size. For flap procedures, when the source of the infection is intrasurgical contamination, the infiltrate is usually located in the interface to begin with. Chang et al., in their review of post-LASIK infectious keratitis, found that interface infiltrates was the post common form of presentation of the infection.[7] The other types of presentations included infiltrates restricted only to the lamellar flap or stroma/involvement of flap margin and adjacent stroma, surface ulceration, anterior chamber infiltrates and rarely endophthalmitis.[7]
Non-infectious keratitis
Diffuse lamellar keratitis (DLK) is the commonest variant. Clinically resembling the “Sands of Sahara”, DLK is an interface inflammation. Numerous factors predisposing to DLK include bacterial cell wall endotoxins built up in wet autoclave reservoirs, epithelial defects, interface blood, trauma, reaction to cleaning solutions/blade debris/iodine skin cleaners/meibomian secretions and many times idiopathic.[33,34] The clinical presentation typically begins in the periphery and is confined to the flap interface without extension into adjacent stroma. The four grades of DLK are characterized by progressive central spread of the granular infiltration in the interface and progressive dimunition of vision due to flap striae and induced hyperopia.[35]
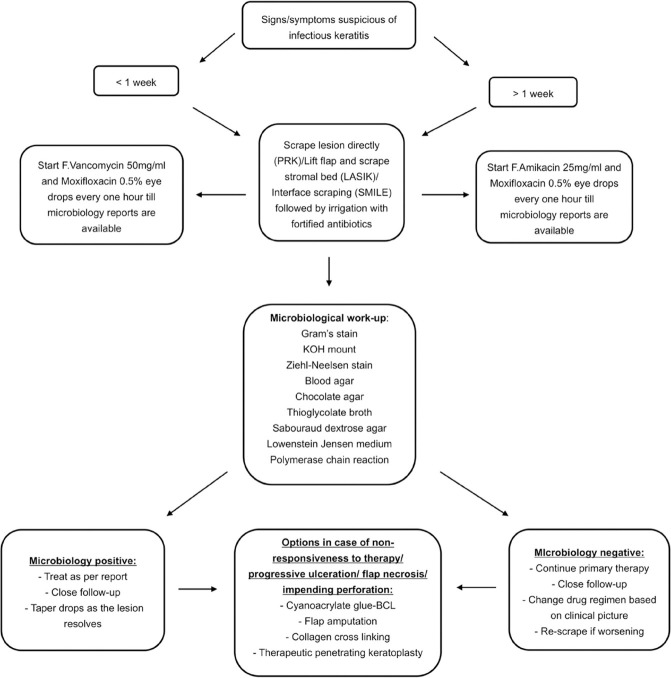
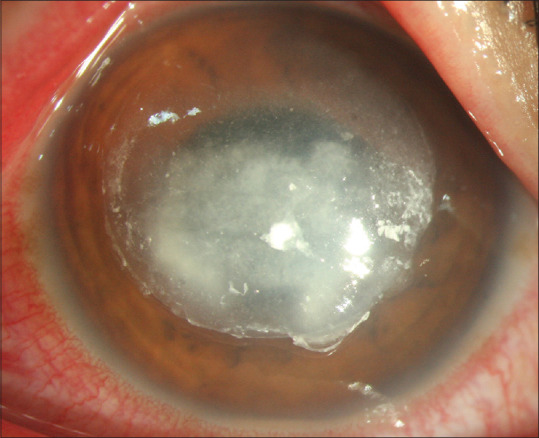
Focal debris between lamellar flaps and underlying stroma can also cause localized reaction confined to one to two millimeters. The non-progressive and self limiting nature of this mild condition generally does not warrant any treatment.[5] Staphylococcal marginal hypersensitivity presents as marginal corneal infiltrates with no or minimum overlying epithelial defect and no anterior chamber reaction. It is usually associated with a history of rosacea/blepharitis. It represents a type three hypersensitivity reaction to bacteria usually staphylococciin the eyelids. The bacterial antigens trigger an immune response with deposition of immune complexes in peripheral cornea, activating the complement pathway.[36] Table 2 describes the different presentations of keratitis post laser refractive surgery (these should not be considered as a gold standard). Figs. 1 and 2 are clinical photographs of different types of keratitis occurring post LASIK.
Table 2.
Keratitis post laser refractive surgery - When to suspect what?
| Signs | Presentation | Type of keratitis |
|---|---|---|
| White infiltrate with rounded margins/stromal edema/overlying epithelial defect | <1 week | Staphylococcus/streptococcus/pseudomonas |
| Yellow white dense infiltrate with irregular margins/satellite lesions/endoexudates | >1 week | Fungus |
| Grayish white ring infiltrate/linear/patchy/irregular infiltrates | >1 week | Acanthamoeba/mycobacteria/nocardia |
| Dendritic/geographic epithelial defect/grayish white stromal infiltrate with edema/endothelial KPs/AC reaction | >1 week | Herpes viral disease |
| Granular infiltration in the interface starting at the periphery and spreading centrally | <1 week | Diffuse lamellar keratitis |
| Marginal corneal infiltrates with no or minimum overlying epithelial defect | <1 week | Staphylococcal marginal hypersensitivity |
KP=Keratic precipitates, AC=Anterior chamber
Figure 1.
A case of infectious keratitis post Laser in-situ keratomileusis, caused by filamentous fungi, presenting with multiple patchy irregular infiltrates in the flap interface. [Original image]
Figure 2.
A case of grade 2 Diffuse lamellar keratitis post Laser in-situ keratomileusis; giving a grey, granular appearance to the flap interface. [Original image]
Management
Careful approach to a case of post-refractive surgery keratitis is vital for a successful outcome. Clinicians handling these cases must perform a thorough clinical examination to distinguish inflammatory from infective keratitis. This distinction is important as the line of management of the two conditions is very different. Avoid denial specially if the case is handled by operating surgeon.
Infectious keratitis
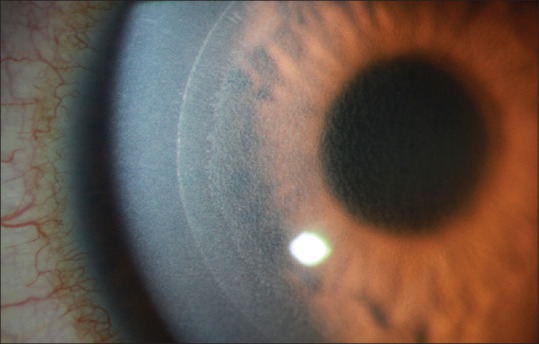
In cases of suspected microbial keratitis, laboratory identification of the organism is important especially when the clinical features overlap. One must try to collect samples for microbiology work-up in every case. This may involve entering the interface in flapped surgical procedures. The guidelines suggested by the ASCRS white paper of 2005 is the approach that has been followed by most physicians for post-LASIK cases.[19]
Sample Collection And Laboratory Work Up: In case of PRK, the infiltrate is easily accessible for sample collection. A blade/spatula can be used for scraping the lesions. For a LASIK flap lift, often a chopper or a flap lifter is used. The stromal bed and at times the undersurface of the flap is then scraped. In SMILE cases, the interface can be scraped using a hydrodissection cannula or a spatula. The flap interface should be irrigated with fortified antibiotics in all cases after sample collection.[3] Fig. 3 depicts a recommended algorithm to follow in a case of infectious keratitis post-laser refractive surgery. Most organisms are identified on Gram's stain and Blood agar. However, if the presentation is late (beyond one week), it is recommended to additionally use Ziehl Neelsen stain, Lowenstein-Jensen media and Sabouraud dextrose agar for mycobateria and fungi respectively. Initially broad-spectrum antibiotics (fourth-generation fluoroquinolones) are preferable, followed by customization based on culture and sensitivity results.[3] Fortified preparations of drugs such as vancomycin/cefazolin/tobramycin/ceftazidime are effective against most gram-positive and gram-negative bacteria. Treatment regimen should be changed to anti-fungals like natamycin/voriconazole/amphotericin B in case of fungal growth. Acanthamoeba cases are treated with PHMB (polyhexamethylene biguanide) and chlorhexidine eye drops. Steroids should be stopped immediately in all cases. HSV (herpes simplex viral) keratitis cases have a typical appearance and should be treated with topical and systemic acyclovir/valacyclovir along with topical steroids in consensus with the HEDS (Herpetic eye disease study) recommendations.[37]
Figure 3.
Management algorithm for a case of infectious keratitis post laser refractive surgery [PRK = Photorefractive keratectomy, LASIK = Laser in-situ keratomileusis, SMILE = Small incision lenticule extraction, KOH = Potassium hydroxide, BCL = Bandage contact lens]. [Original image]
Most lesions resolve with medical management alone over few weeks.[3] In case of non-responding infection, corneal biospy or polymerase chain reaction may also be required to isolate the organisms.[38] Repeated interface irrigation, flap amputation, tissue adhesive-bandage contact lens, collagen cross-linking and therapeutic penetrating keratoplasty (TPK) are reserved for the severe/non-resolving cases.[3,7] Cases with flap necrosis warrant a flap amputaion while those with thinning/impending perforation/frank perforation require a tissue adhesive-bandage contact lens (cyanoacrylate glue).[3] Corneal collagen cross-linking has been emerging as an alternative therapeutic option for early-stage post-LASIK infectious keratitis.[3] TPK is indicated for large/non-resolving infiltrates, limbal involvement and/or intraocular spread. In the study by Moshirfar et al. of 10477 post-LASIK eyes, most cases resolved with appropriate medical treatment. Flap lifting and irrigation were required in 4/33 (12.1%) infectious cases and 3/246 (1.2%) non-infectious cases. Flap amputation and penetrating keratoplasty were performed in 2/33 (6.1%) infectious cases.[5]
Non-infectious keratitis
Staphylococcal marginal keratitis is a self limiting condition.[36] The lesions usually resolve in two to three weeks with topical corticosteroids.[36] Resolution of the epithelial defect, reduced cellularity and rounding of the infiltrate margins are signs of healing.[36] Lid hygiene and antibiotics for blepharitis/rosacea prevent recurrences.[36] Systemic doxycycline has been used in cases with meibomian gland dysfunction associated with peripheral corneal infiltrates post refractive surgery.[39] Doxycycline is known to inhibit collagenolysis as well as inhibit staphylococcal exotoxin-induced cytokines and has an anti- inflammatory effect.[40]
With respect to diffuse lamellar keratitis, grades one and two resolve with topical corticosteroids alone. Hourly prednisolone acetate is the drug regimen of choice. Grades three and four require a flap lift, irrigation with balanced salt solution and flap ironing, along with the topical corticosteroids.[41] A prophylactic antibiotic should be given in all cases that require a high dosage of corticosteroids. Oral prednisolone/intravenous methylprednisolone are useful and have been given in some cases of severe DLK.[5]
Outcomes
Following meticulous treatment, the eventual resolution of infiltrates can take a couple of weeks or months. About 50–75% of all infectious keratitis cases post LASIK resolve with a final best-corrected visual acuity (BCVA) of 20/40 or greater.[5,4,15] Infections with gram-positive bacteria seem to fair better than the rest.[7,15] About 80-90% of patients gain a visual acuity of 20/40 or better and about 50-60% of patients gain a final vision of 20/20 or better.[7,5,15] As reported in two large cohort studies, greater than 50% and 90% of infections post PRK resolve with a BCVA of 20/20 and 20/40 or better, respectively.[33,42] Although few case reports on SMILE do suggest severe infection causing a reduction of final BCVA, in a large study of 1500 SMILE cases that had 5 cases of infectious keratitis, none had a loss of BCVA and all 5 of them had a final vision of 20/20.[18] Most cases of DLK resolve with complete restoration of vision post treatment.
Conclusion
Keratitis post laser refractive surgery is a complicaton that deters early as well as adequate visual recovery in patients. Although the incidence of infectious keratitis is not as high as that due to non-infectious etiology; it can be severe in nature and needs meticulous treatment to salvage vision. Taking preventive steps pre, intra and post-operatively can help reduce its occurrence.
Greater understanding of the complication, use of better technology, and attention to sterilization; all these have resulted in progressive reduction in the incidence of this complication over the years. High index of clinical suspicion, early recognition and treatment with sensitive drugs aid in effective management and preservation of good vision in cases that develop it.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Alexander JK, Davidson RS. Managing expectations in refractive surgery. Int Ophthalmol Clin. 2016;56:1–17. doi: 10.1097/IIO.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 2.Spadea L, Giovannetti F. Main complications of photorefractive keratectomy and their management. Clin Ophthalmol. 2019;13:2305–15. doi: 10.2147/OPTH.S233125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haq Z, Farooq AV, Huang AJW. Infections after refractive surgery. Curr Opin Ophthalmol. 2016;27:367–72. doi: 10.1097/ICU.0000000000000275. [DOI] [PubMed] [Google Scholar]
- 4.Solomon R, Donnenfeld ED, Holland EJ, Yoo SH, Daya S, Güell JL, et al. Microbial keratitis trends following refractive surgery: Results of the ASCRS infectious keratitis survey and comparisons with prior ASCRS surveys of infectious keratitis following keratorefractive procedures. J Cataract Refr Surg. 2011;37:1343–50. doi: 10.1016/j.jcrs.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 5.Moshirfar M, Welling JD, Feiz V, Holz H, Clinch TE. Infectious and noninfectious keratitis after laser in situ keratomileusis.Occurrence, management, and visual outcomes. J Cataract Refract Surg. 2007;33:474–83. doi: 10.1016/j.jcrs.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Smith RJ, Maloney RK. Diffuse lamellar keratitis: A new syndrome in lamellar refractive surgery. Ophthalmology. 1998;105:1721–26. doi: 10.1016/S0161-6420(98)99044-3. [DOI] [PubMed] [Google Scholar]
- 7.Chang MA, Jain S, Azar DT. Infections following laser in situ keratomileusis: An integration of the published literature. Surv Ophthalmol. 2004;49:269–80. doi: 10.1016/j.survophthal.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Freitas D, Alvarenga L, Sampaio J, Mannis M, Sato E, Sousa L, et al. An outbreak of Mycobacterium chelonae infection after LASIK. Ophthalmology. 2003;110:276–85. doi: 10.1016/S0161-6420(02)01643-3. [DOI] [PubMed] [Google Scholar]
- 9.Winthrop KL, Steinberg EB, Holmes G, Kainer MA, Werner SB, Winquist A, et al. Epidemic and sporadic cases of nontuberculous mycobacterial keratitis associated with laser in situ keratomileusis. Am J Ophthalmol. 2003;135:223–4. doi: 10.1016/s0002-9394(02)01955-4. [DOI] [PubMed] [Google Scholar]
- 10.Guidelines for the Cleaning and Sterilization of Intraocular Surgical Instruments. Ophthalmic Instrument Cleaning and Sterilization (OICS) Task Force ASCRS, AAO and OOSS. 2018. Apr, [Last accessed on 2020 Oct 06]. Available from: https://wwwaaoorg/clinical-statement/guidelines-cleaning-sterilization-intraocular .
- 11.Linke SJ, Richard G, Katz T. Infectious keratitis after LASIK: Update and survey of the literature. Klin Monbl Augenheilkd. 2011;228:531–6. doi: 10.1055/s-0029-1245549. [DOI] [PubMed] [Google Scholar]
- 12.de Rojas V, Llovet F, Martínez M, Cobo-Soriano R, Ortega-Usobiaga J, Beltrán J, et al. Infectious keratitis in 18,651 laser surface ablation procedures. J Cataract Refract Surg. 2011;37:1822–31. doi: 10.1016/j.jcrs.2011.04.037. [DOI] [PubMed] [Google Scholar]
- 13.de Oliveira GC, Solari HP, Ciola FB, Lima ALH, Campos MS. Corneal infiltrates after excimer laser photorefractive keratectomy and LASIK. J Refract Surg. 2006;22:159–65. doi: 10.3928/1081-597X-20060201-14. [DOI] [PubMed] [Google Scholar]
- 14.Schallhorn JM, Schallhorn SC, Hettinger K, Hannan S. Infectious keratitis after laser vision correction: Incidence and risk factors. J Cataract Refract Surg. 2017;43:473–9. doi: 10.1016/j.jcrs.2017.01.017. [DOI] [PubMed] [Google Scholar]
- 15.Llovet F, de Rojas V, Interlandi E, Martín C, Cobo-Soriano R, Ortega-Usobiaga J, et al. Infectious keratitis in 204 586 LASIK procedures. Ophthalmology. 2010;117:232–e1-4. doi: 10.1016/j.ophtha.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Ortega-Usobiaga J, Llovet-Osuna F, Djodeyre MR, Llovet-Rausell A, Beltran J, Baviera J. Incidence of corneal infections after laser in situ keratomileusis and surface ablation when moxifloxacin and tobramycin are used as postoperative treatment. J Cataract Refract Surg. 2015;41:1210–6. doi: 10.1016/j.jcrs.2014.09.041. [DOI] [PubMed] [Google Scholar]
- 17.Vestergaard A, Ivarsen AR, Asp S, Hjortdal J. Small-incision lenticule extraction for moderate to high myopia: Predictability, safety, and patient satisfaction. J Cataract Refract Surg. 2012;38:2003–10. doi: 10.1016/j.jcrs.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 18.Ivarsen A, Asp S, Hjortdal J. Safety and complications of more than 1500 small-incision lenticule extraction procedures. Ophthalmology. 2014;121:822–8. doi: 10.1016/j.ophtha.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 19.Donnenfeld ED, Kim T, Holland EJ, Azar DT, Palmon FR, Rubenstein JB, et al. ASCRS white paper: Management of infectious keratitis following laser in situ keratomileusis. J Cataract Refract Surg. 2005;31:2008–11. doi: 10.1016/j.jcrs.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 20.Solomon R, Donnenfeld ED, Azar DT, Holland EJ, Palmon FR, Pflugfelder SC, et al. Infectious keratitis after laser in situ keratomileusis: Results of an ASCRS survey. J Cataract Refract Surg. 2003;29:2001–6. doi: 10.1016/s0886-3350(03)00512-1. [DOI] [PubMed] [Google Scholar]
- 21.Yamaguchi T, Bissen-Miyajima H, Hori-Komai Y, Matsumoto Y, Ebihara N, Takahashi H, et al. Infectious keratitis outbreak after laser in situ keratomileusis at a single laser center in Japan. J Cataract Refract Surg. 2011;37:894–900. doi: 10.1016/j.jcrs.2010.11.034. [DOI] [PubMed] [Google Scholar]
- 22.John T, Velotta E. Nontuberculous (atypical) mycobacterial keratitis after LASIK: Current status and clinical implications. Cornea. 2005;24:245–55. doi: 10.1097/01.ico.0000151565.63107.64. [DOI] [PubMed] [Google Scholar]
- 23.Holmes GP, Bond GB, Fader RC, Fulcher SF. A cluster of Mycobacterium szulgai keratitis that occurred after laser-assisted in situ keratomileusis. Clin Infect Dis. 2002;34:1039–46. doi: 10.1086/339487. [DOI] [PubMed] [Google Scholar]
- 24.Solomon R, Donnenfeld ED, Perry HD, Rubinfeld RS, Ehrenhaus M, Wittpenn JR, Jr, et al. Methicillinresistant staphylococcus aureus infectious keratitis following refractive surgery. Am J Ophthalmol. 2007;143:629–34. doi: 10.1016/j.ajo.2006.12.029. [DOI] [PubMed] [Google Scholar]
- 25.Garg P, Chaurasia S, Vaddavalli PK, Muralidhar R, Mittal V, Gopinathan U. Microbial keratitis after LASIK. J Refract Surg. 2010;26:209–16. doi: 10.3928/1081597X-20100224-07. [DOI] [PubMed] [Google Scholar]
- 26.Probst LE, Foley L. Late-onset interface keratitis after uneventful laser in situ keratomileusis. J Cataract Refract Surg. 2001;27:1124–5. doi: 10.1016/s0886-3350(00)00879-8. [DOI] [PubMed] [Google Scholar]
- 27.Stulting RD, Randleman JB, Couser JM, Thompson KP. The epidemiology of diffuse lamellar keratitis. Cornea. 2004;23:680–8. doi: 10.1097/01.ico.0000127477.14304.de. [DOI] [PubMed] [Google Scholar]
- 28.Shah MN, Misra M, Wilhelmus KR, Koch DD. Diffuse lamellar keratitis associated with epithelial defects after laser in situ keratomileusis. J Cataract Refract Surg. 2000;26:1312–8. doi: 10.1016/s0886-3350(00)00570-8. [DOI] [PubMed] [Google Scholar]
- 29.Esquenazi S, Bui V. Long-term refractive results of myopic LASIK complicated with intraoperative epithelial defects. J Refract Surg. 2006;22:54–60. doi: 10.3928/1081-597X-20060101-12. [DOI] [PubMed] [Google Scholar]
- 30.Hoffman RS, Fine IH, Packer M, Reynolds TP, Van Bebber C. Surgical glove-associated diffuse lamellar keratitis. Cornea. 2005;24:699–704. doi: 10.1097/01.ico.0000154379.75119.ba. [DOI] [PubMed] [Google Scholar]
- 31.Chen S, Feng Y, Stojanovic A, Jankov 2nd MR, Wang Q. IntraLase femtosecond laser vs mechanical microkeratomes in LASIK for myopia: A systematic review and meta-analysis. J Refract Surg. 2012;28:15–24. doi: 10.3928/1081597X-20111228-02. [DOI] [PubMed] [Google Scholar]
- 32.Lu C-K, Chen K-H, Lee S-M, Hsu W-M, Lai J-Y, Li Y-S. Herpes simplex keratitis following excimer laser application. J Refract Surg. 2006;22:509–11. doi: 10.3928/1081-597X-20060501-15. [DOI] [PubMed] [Google Scholar]
- 33.Holland SP, Mathias RG, Morck DW, Chiu J, Slade SG. DLK related to endotoxins released from sterilizer reservoir biofilms. Ophthalmology. 2000;107:1227–33. doi: 10.1016/s0161-6420(00)00246-3. [DOI] [PubMed] [Google Scholar]
- 34.Nakano EM, Nakano K, Oliveira MC, Portellinha W, Simonelli R, Alvarenga LS. Cleaning solutions as a cause of diffuse lamellar keratitis. J Refract Surg. 2002;18(3 suppl):S361–3. doi: 10.3928/1081-597X-20020502-16. [DOI] [PubMed] [Google Scholar]
- 35.Saldanha MJ, Chan CC, Probst LE. LASIK complications. In: Mannis MJ, Holland EJ, editors. Cornea: Fundamentals, Diagnosis, Management. New York: Elsevier; 2016. [Google Scholar]
- 36.Chung G, Iuorno JD. Immunologic disorders of the cornea. In: Mannis MJ, Holland EJ, editors. Cornea: Fundamentals, Diagnosis, Management. New York: Elsevier; 2016. [Google Scholar]
- 37.Kalezic T, Mazen M, Kuklinski E, Asbell P. Herpetic eye disease study: Lessons learned. Curr Opin Ophthalmol. 2018;29:340–46. doi: 10.1097/ICU.0000000000000482. [DOI] [PubMed] [Google Scholar]
- 38.Arnalich-Montiel F, Almendral A, Arnalich F, Valladares B, Lorenzo-Morales J. Mixed acanthamoeba and multidrug-resistant Achromobacter xyloxidans in late-onset keratitis after laser in situ keratomileusis. J Cataract Refract Surg. 2012;38:1853–6. doi: 10.1016/j.jcrs.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 39.Lifshitz T, Levy J, Mahler O, Levinger S. Peripheral sterile corneal infiltrates after refractive surgery. J Cataract Refract Surg. 2005;31:1392–5. doi: 10.1016/j.jcrs.2004.12.057. [DOI] [PubMed] [Google Scholar]
- 40.Krakauer T, Buckley M. Doxycycline is anti-inflammatory and inhibits staphylococcal exotoxin-induced cytokines and chemokines. Antimicrob Agents Chemother. 2003;47:3630–3. doi: 10.1128/AAC.47.11.3630-3633.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Linebarger EJ, Hardten DR, Lindstrom RL. DLK: Diagnosis and management. J Cataract Refract Surg. 2000;26:1072–7. doi: 10.1016/s0886-3350(00)00468-5. [DOI] [PubMed] [Google Scholar]
- 42.Wroblewski KJ, Pasternak JF, Bower KS, Schallhorn SC, Hubickey WJ, Harrison CE, et al. Infectious keratitis after PRK in the United States army and navy. Ophthalmology. 2006;113:520–5. doi: 10.1016/j.ophtha.2005.09.038. [DOI] [PubMed] [Google Scholar]