Abstract
A 42-year-old female presented with pain, photophobia, and superficial corneal infiltrates in mid-periphery in the left eye, after 2 days of uneventful bilateral SMILE procedure. Inspite of the medical treatment with fortified antibiotics, the infection spread to the interface, close to visual axis reducing UDVA from 20/16 to 20/80. Immediate surgical intervention in the form of scraping of interface lesions with 26G needle, interface wash with antibiotics and photoactivated chromophore for keratitis (PACK-CXL) was performed. After 24 h of bacterial culture Staphylococcus aureus was yielded. Interface wash and PACK-CXL was repeated after 48 h by which infiltrates reduced and early scarring was observed by 10th post-op day. Subsequent topical steroids helped in limiting scar formation and UDVA improved to 20/30 at the final visit. Combined approach of interface wash with antibiotics and PACK-CXL may be a safe and effective modality in treating early onset infectious keratitis following SMILE surgery.
Keywords: Infectious keratitis, interface wash, PACK-CXL, SMILE
Infectious keratitis after laser vision correction (LVC)[1,2,3] warrants aggressive treatment to preserve useful vision. In context of infection after small incision lenticule extraction (SMILE) procedure, the management involves either interface wash[4] or PACK-CXL,[5] but not a combination of the two due to fear of spread of infection. We report aunique case of early onset infectious keratitis after an uneventful SMILE procedure, which was aggressively managed using a multimodal approach, resulting in favorable clinical outcomes.
Case Report
A 42 year old, systemically healthy female underwent uneventful SMILE for simple myopia of -4.00 D in both eyes, following which she achieved 20/16 UDVA in each eye on first post-op day. However, she returned after 24 h with complains of pain, redness, and lid swelling in the left eye, following a foreign body going into the eye. On examination, UDVA in the left eye was 20/16, and ocular evaluation did not reveal foreign body. However, mild lid oedema, circum-corneal congestion, a small superficial infiltrate measuring 0.5 × 0.5 mm in the temporal mid-peripheral cornea at the edge of the side cut of the lasered area and 2+ reaction in the anterior chamber was observed [Fig. 1]. Corneal scrapings were sent for Gram staining and culture in blood agar only, as the sample was not sufficient for KOH preparation and fungal culture. Gram staining revealed Gram positive cocci, based on which a combination therapy of fortified cefotaxime: 50mg/mL and vancomycin: 50mg/mL topical drops (Q 1 hourly alternately) was started along with topical homatropine (2%) for cycloplegia. Topical steroids, which were prescribed postoperatively were stopped.
Figure 1.
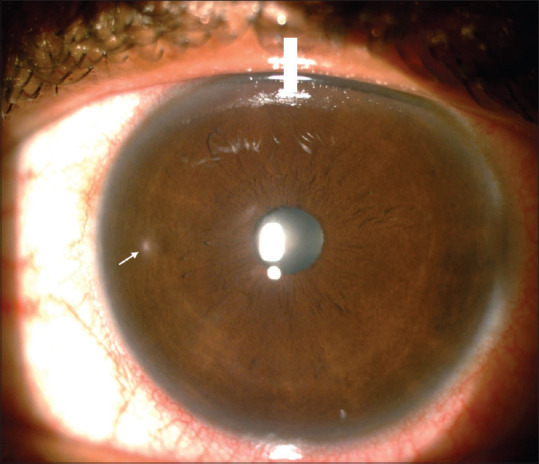
Small infiltrate in mid peripheral cornea (arrow) on 2nd post-operative day in the left eye following uneventful bilateral SMILE procedure
On the next day, the left eye developed 4 new and distinct, white, circular infiltrates of variable sizes (0.5–2mm), and involving the interface, as demonstrated by the AS-OCT [Fig. 2a and b]. UDVA had dropped to 20/80. After 24 h, culture did not reveal any growth.
Figure 2.
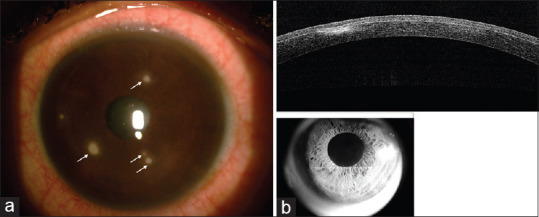
(a) Appearance of four new lesions (arrows) on 3rd post-operative day (b) Corresponding AS-OCT showing infiltrates in interface and stromal bed with largely undisturbed cap
In view of the progression and failure of medical therapy, surgical intervention was contemplated. Interface was carefully opened with blunt dissection followed by which, a 26G needle was used to scrape the lesions from the undersurface of the cap. Samples were obtained for both bacterial and fungal culture in blood agar and Sabouraud's dextrose agar respectively. The interface was then washed using vancomycin (1 mg in 0.1 ml solution) and moxifloxacin (0.05 ml of Vigamox 0.5%, Alcon, Fort Worth, Texas, USA). Subsequently, photoactivated chromophore for keratitis or PACK-CXL[4] was performed by using 2.5% riboflavin reconstituted in normal saline, applied in the interface for 1 min, followed by UV-A exposure at a fluence of 30 mW for 3 min, delivering a total energy of 5.4 J/cm2 (Avedro KXL system, Waltham). Topical therapy with fortified antibiotics was continued.
On postoperative day 1 following intervention, the cornea was hazy and edematous, however, the infiltrates had reduced, and no fresh lesions were noticed [Fig. 3]. After 24 h, bacterial culture showed the growth of Staphylococcus aureus, sensitive to vancomycin, cefotaxime, and moxifloxacin. Fungal culture did not reveal any growth. Interface wash with the same antibiotics was repeated after 48 h in order to consolidate the results, and as it was a case of infection post a refractive surgery, we were being extra cautious.
Figure 3.
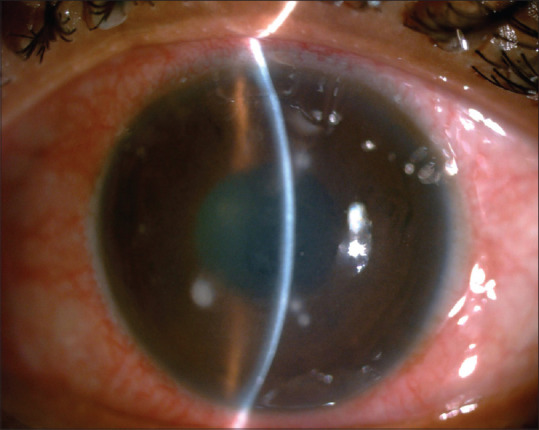
Post-operative day 1 clinical picture following PACK-CXL and interface irrigation showing reduction of infiltrates and mild stromal edema
By 10th post-op day, when infiltrates had reduced, and early scarring was seen, topical steroid (fluoromethalone 0.1%) was started and tapered over 3 weeks. At 3 months, scars had reduced in size, corneal oedema had resolved [Fig. 4a], and the patient recovered a UDVA of 20/30 in the affected eye, which improved to 20/20 with spectacle correction of 0.75D cyl at 140°. Fig. 4b shows the AS-OCT of the left eye at 3-months, showing hyper-reflective areas in the interface, suggestive of post CXL haze and healed keratitis scars.
Figure 4.
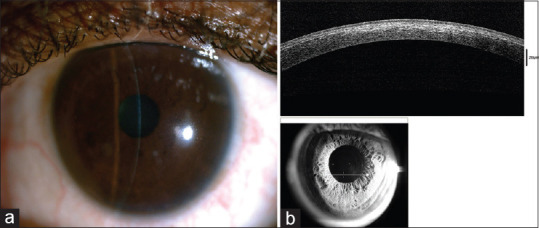
Three month post clinical picture showing (a) Complete resolution of infection with minimal scar and (b) PACK-CXL associated mild anterior stromal haze
Discussion
Infectious keratitis post SMILE may be more challenging to manage, as the infection may spread rapidly within the closed interface, which is relatively difficult to access, compared with flap in LASIK. In these cases, one should not hesitate to open the interface for corneal scrapings, which help in targeted treatment against infectious agent. While obtaining scrapings, however, care must be taken while using sharp needle in the interface, as perforation of cap may lead to scarring and decrease in visual acuity.
This case reiterates that early onset keratitis after refractive surgery is predominantly caused by Gram positive bacteria,[1] and when nature of organism and its antibiotic sensitivity is not available, vancomycin and moxifloxacin appear to be good choice for interface irrigation as recommended by Soloman, et al. to cover Methicillin resistant S. aureus.[4]
There are very few reported cases of culture proven infectious keratitis after SMILE surgery.[4,5,6,7,8] These were treated either with antibiotics interface wash[4] or PACK-CXL,[5] but not with the combination of the two. Chan, et al. reported the successful use of PACK-CXL in treatment of Staphylococcal keratitis after SMILE.[6] However, they did not perform interface irrigation fearing an iatrogenic spread of infection. We performed both interface irrigation with antibiotics and PACK-CXL in the same sitting, as the former would reduce the infective load and enhance the bactericidal effect of PACK-CXL. Interface irrigation was repeated after 48 hs for continued response. As, the role of steroids is controversial and they did not make a difference in scar size and final visual outcome,[9] we were cautious in starting steroids early and used milder steroids, only when early scarring was noted.
Conclusion
To the best of our knowledge, we described the first case of bacterial keratitis after SMILE, which was treated successfully with corneal scraping, interface wash and PACK-CXL, without additional complications.
However, further data are required to establish this, and early recognition and treatment, along with close follow-up, remains the key to successful management in these challenging cases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Llovet F, de Rojas V, Interlandi E, Martín C, Cobo-Soriano R, Ortega-Usobiaga J, et al. Infectious keratitis in 204 586 LASIK procedures. Ophthalmology. 2010;117:232–8e1-4. doi: 10.1016/j.ophtha.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 2.De Rojas V, Llovet F, Martinez M, Cobo-Soriano R, Ortega-Usobiaga J, Beltran J, et al. Infectious keratitis in 18651 laser surface ablation procedures. J Cataract Refract Surg. 2011;37:1822–31. doi: 10.1016/j.jcrs.2011.04.037. [DOI] [PubMed] [Google Scholar]
- 3.Ivarsen A, Asp S, Hjortdal J. Safety and complications of more than 1500 small-incision lenticule extraction procedures. Ophthalmology. 2014;121:822–8. doi: 10.1016/j.ophtha.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 4.Chehaibou I, Sandali O, Ameline B, Bouheraoua N, Borderie V, Laroche L. Bilateral infectious keratitis after small-incision lenticule extraction. J Cataract Refract Surg. 2016;42:626–30. doi: 10.1016/j.jcrs.2016.03.024. [DOI] [PubMed] [Google Scholar]
- 5.Chan TC, Chow VW, Jhanji V. Collagen cross-linking with photoactivated riboflavin (PACK-CXL) for bacterial keratitis after small incision lenticule extraction (SMILE) J Refract Surg. 2017;33:278–80. doi: 10.3928/1081597X-20170126-01. [DOI] [PubMed] [Google Scholar]
- 6.Solomon R, Donnenfeld ED, Holland EJ, Yoo SH, Daya S, Güell JL, et al. Microbial keratitis trends following refractive surgery: Results of the ASCRS Infectious keratitis survey and comparisons with prior ASCRS surveys of infectious keratitis following keratorefractive procedures. J Cataract Refract Surg. 2011;37:1343–50. doi: 10.1016/j.jcrs.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Liu HY, Chu HS, Chen WL, Hu FR, Wang IJ. Bilateral non-tuberculous mycobacterial keratitis after small incision lenticule extraction. J Refract Surg. 2018;34:633–6. doi: 10.3928/1081597X-20180827-01. [DOI] [PubMed] [Google Scholar]
- 8.Sachdev GS, Diwan S, Sachdev M. Unilateral fungal keratitis after small-incision lenticule extraction. JCRS Online Case Rep. 2019;7:11–3. [Google Scholar]
- 9.Srinivasan M, Mascarenhas J, Rajaraman R, Ravindran M, Lalitha P, O'Brien KS, et al. For the Steroids for Corneal Ulcers Trial Group. The Steroids for corneal ulcers trial (SCUT): Secondary 12-month clinical outcomes of a randomized controlled trial. Am J Ophthalmol. 2014;157:327–333. doi: 10.1016/j.ajo.2013.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]


