Abstract
A young lady presented with very high vault and fixed dilated pupil along with optic capture of the implantable collamer lens (ICL). After thorough evaluation and ruling out the ICL sizing error, the optic capture was relieved and the ICL was rotated into vertical position. Single-pass four throw pupilloplasty was performed for the fixed dilated pupil. Postoperatively the ICL vault and the pupil size decreased and patient was asymptomatic. This case highlights a successful outcome of rotation of a nontoric ICL to reduce the high vaulting and optic capture along with single-pass four throw pupilloplasty.
Keywords: Implantable collamer lens, pupilloplasty, Urrets-Zavalia syndrome
Fixed and dilated pupil after an intraocular surgery is a rare complication which is termed as Urrets Zavalia Syndrome (UZS).[1] There have been a few case reports of fixed and dilated pupil after Implantable collamer lens (ICL) implanation.[2]
We describe for the first time, an interesting case of anisocoria secondary to the optic capture of ICL and a high vault, which was managed by rotation of the ICL and single pass four throw pupilloplasty.
Case Report
A 27-year-old female presented to our clinic with the complaints of glare and intolerance to light in her left eye (LE) after an ICL (STAAR V4C model) implantation in both eyes (BE) done 3 months back, elsewhere. The preoperative refractive error was -5 D in BE. The preoperative reports showed that BE had a similar white-to-white (WTW) measurement of 11.8 mm and anterior chamber depth (ACD) of 3.1 mm in BE. Hence, a similar-sized nontoric ICL of 13.2 mm size was implanted in BE by the referring primary surgeon. At presentation, uncorrected visual acuity (UCVA) in her right eye (RE) was 20/20, N6 and that of (LE) was 20/30, N6. Slit-lamp evaluation of RE showed clear cornea with peripheral anterior chamber depth (PACD) of ½ corneal thickness (CT). Pupil was 3 mm, round, regular and reactive [Fig. 1a]. ICL was in place with a slit lamp vault of 1 CT. In the LE, cornea was clear, AC was quiet with PACD of ¼ CT. Pupil was 8 mm dilated and fixed [Fig. 1b]. ICL was in place with optic capture at the pupillary border at 4 o'clock [Fig. 2a]. Slit lamp vault of the ICL was approximately 2 times CT. Lens was clear with 16 mm Hg IOP. At presentation, patient was on topical Pilocarpine Hydrochloride 2%, Brimonidine tartarate 0.2%, Timolol maleate 0.5% combination in LE. Gonioscopy showed open angles up to scleral spur in the RE and LE showed 2700 peripheral anterior synechiae. Anterior segment optical coherence tomography (AS-OCT, Optovue) showed ICL vault of 675μ in the RE and 998μ in the LE [Fig. 3a]. Fundus evaluation showed a healthy disc with cup disc ratio of 0.3:1 in BE.
Figure 1.
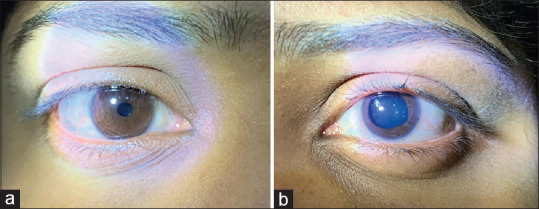
(a) Right eye after ICL surgery showing a round 3 mm sized pupil. (b) Left eye after ICL surgery showing a fixed dilated pupil of size 8 mm
Figure 2.
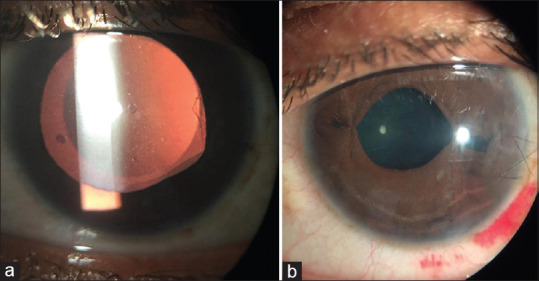
(a) Retroillumination of the left eye showing a fixed dilated pupil and Pupillary capture of the ICL at 4 o clock position. (b) A Smaller pupil after pupilloplasty
Figure 3.
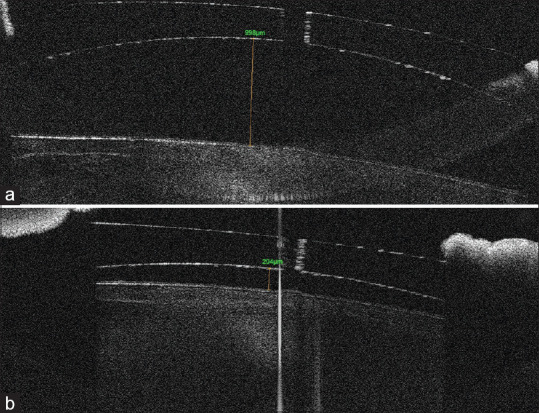
(a) Preoperative ASOCT showing a high vault of around 998 microns. (b) Immediate postoperative ASOCT showing reduced vault of around 204 microns
A diagnosis of high ICL vault in LE with secondary angle closure and anisocoria was made. Under peribulbar anesthesia, after forming the AC with viscoelastic, the ICL was gently manipulated by ICL manipulator from the side port incision and rotated from horizontal to vertical meridian under the iris, without getting it into the AC. After relieving the pupillary capture, intracameral pilocarpine was injected to constrict the pupil. As the pupil did not constrict, a pupilloplasty was performed. The previous temporal clear corneal incision was opened with a sharp keratome. A needle of the 10-0 prolene suture was passed from superior side port. A microforceps was passed from the main temporal incision to grasp the superior iris through which the needle was passed. A 26-G needle was passed through the inferior side port into the AC and then pierced through the inferior part of the iris. The needle of the prolene suture was then passed into the barrel of the 26 G needle and the needle was pulled out of the AC through the inferior side port [Fig. 4a]. The suture at the inferior side was brought out through the superior sideport as a loop using an IOL dialer. A single-pass four throw technique was used to create a helical loop. Later, the superior and inferior ends of the suture were pulled to create a knot at the iris plane, in the AC approximating the iris [Fig. 4b]. A similar procedure was repeated on the other side. At the end of the procedure the pupil size was reduced to 4 mm. After thorough viscoelastic removal, the eye was patched.
Figure 4.
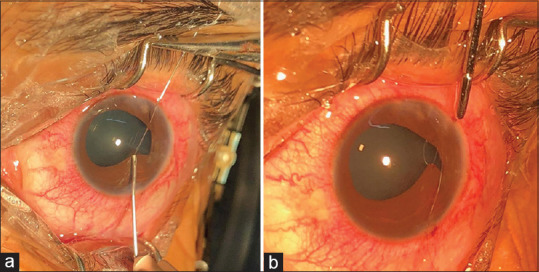
(a and b) Intra-operative photographs showing single pass four throw pupilloplasty with a 10-0 prolene suture
On postoperative day 1, UCVA was 20/25, cornea was clear with IOP 12 mm Hg in the LE. The pupil size was around 4 mm [Fig. 2b]. The ICL vault reduced to 204 microns on AS-OCT [Fig. 3b]. She was prescribed topical prednisolone acetate 1%, moxifloxacin 0.5% every 2 hourly.
At the last follow up of 12 months, the patient was asymptomatic the UCVA in LE remained at 20/25 and near vision of N6 with an IOP of 11 mm Hg and a ICL vault of 270 microns.
Discussion
The mechanism of UZS is due to ischemia of the iris, acute rise in IOP, and presence of iris abnormalities.[3] In our case, the cause for fixed, dilated pupil after an ICL surgery was due to optic capture of ICL in the immediate postoperative period. The reason for optic capture of ICL could not be ascertained. The primary operating surgeon did not try to relieve the pupillary capture and instead the patient was prescribed topical miotics to constrict the pupil. This pupillary capture resulted in a very high vault and synechial angle closure. When there is high vault due to oversizing of ICL, nontoric ICL can be rotated vertically as the sulcus diameter is larger in vertical meridian as compared to horizontal meridian.[4] As the preoperative WTW measurements and the implanted ICL size were similar in both the eyes, the reason for the higher vault in the LE was not explainable due to oversizing of ICL. Even though there was no sizing error, vertical rotation of ICL was planned to reduce the vault. Also, rotation of the ICL without getting into the anterior chamber would involve less manipulation and is less traumatic than explantation and replacing the ICL. The pros and cons of both the options of rotation vis-a-vis explantation was discussed in detail with the patient preoperatively. A single-pass four throw pupilloplasty as described by Narang et al. was performed.[5] This pupilloplasty technique improves the cosmetic appearance of a fixed dilated pupil, reduces the glare and also improves the aqueous drainage from the trabecular meshwork by opening the synechial angle closure. Review of literature mention only conservative managements for dilated pupil following ICL surgery.
Conclusion
For the first time this case describes single four throw pupilloplasty for fixed, dilated pupil in an eye with ICL.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Spierer O, Lazar M. UrretsZavalia syndrome (fixed and dilated pupil following penetrating keratoplasty for keratoconus) and its variants. Surv Ophthalmol. 2014;59:304–10. doi: 10.1016/j.survophthal.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Park SH, Kim SY, Kim HI, Yang SW. Urrets-Zavalia syndrome following iris-claw phakic intraocular lens implantation. J Refract Surg. 2008;24:959–61. doi: 10.3928/1081597X-20081101-18. [DOI] [PubMed] [Google Scholar]
- 3.Nizamani NB, Bhutto IA, Talpur KI. Cluster of Urrets-Zavalia syndrome: A sequel of toxic anterior segment syndrome. Br J Ophthalmol. 2013;97:976–9. doi: 10.1136/bjophthalmol-2012-302319. [DOI] [PubMed] [Google Scholar]
- 4.Matarazzo F, Day AC, Cueto LF, Maurino V. Vertical implantable collamer lens (ICL) rotation for the management of high vault due to lens oversizing. Int Ophthalmol. 2018;38:2689–92. doi: 10.1007/s10792-017-0757-2. [DOI] [PubMed] [Google Scholar]
- 5.Narang P, Agarwal A. Single-pass four-throw technique for pupilloplasty. Eur J Ophthalmol. 2017;27:506–8. doi: 10.5301/ejo.5000922. [DOI] [PubMed] [Google Scholar]


