Abstract
Purpose:
The purpose of this study was to evaluate wound healing abilities and efficacy of topical Vitamin C, Vitamin E, and acetylcysteine for their possible clinical use.
Methods:
The study was conducted on 36 eyes of 18 single-breed rabbits, Oryctolagus cuniculus, of both sexes. A 7.5 mm calibrated vacuum corneal trephine was used to induce a defect of 100 micron depth in center of both the corneas. The right eye of rabbits was selected as the control eye and the left eye as the trial eye, which received eyedrops as Group 1–10% Vitamin C eyedrops, Group 2–3% acetylcysteine eye drops, and Group 3–1% Vitamin E eye drops. Control eyes received ringer lactate. Evaluation was done for fluorescein stain positivity, epithelial defect size, and corneal haze on Day 2, Day 7, and Day 14 post induction of the epithelial defect.
Results:
On day 14, three eyes of control group, all Vitamin C and acetylcysteine treated eyes, and four Vitamin E treated eyes were fluorescein stain negative. The mean defect area on day 14 was 0, 0, 0.13, and 1.86 mm2 in Vitamin C, Vitamin E, acetylcysteine, and control eyes, respectively. Vitamin C and Vitamin E control corneal haze better than acetylcysteine in experimentally induced corneal wounds in rabbits.
Conclusion:
The three trial drugs with different mechanism of action showed similar effect on healing of the experimentally created corneal wounds in rabbits, with comparison showing statistical insignificance.
Keywords: Acetylcysteine, corneal wound healing, corneal ulcer, Vitamin C, Vitamin E
A better understanding of the process of corneal wound healing is necessary to guide us towards more effective strategies in order to regain the original anatomical and functional abilities of the cornea in the fastest and the perfect way. Modulation of wound healing processes by the application of topical therapeutic agents is an expanding field of study likely to produce clinically significant improvements in the management of patients with corneal defects. The judicious use of topical compounds has a place in the clinician's armamentarium integrated into a therapeutic plan that decreases the mechanical stresses imposed on the wound bed as well as removal of any underlying inciting causes.
Corneal wound healing promoting substances have a vital role in various eye disorders like stromal corneal dystrophy: lattice, granular and macular dystrophies, keratorefractive surgery, corneal transplantation, cataract surgery, traumatic corneal abrasions, and filamentous keratitis. This study was planned to evaluate and compare topical use of Vitamin C, acetylcysteine, and Vitamin E as healing promoting substances in experimentally produced corneal wounds in rabbit models.
Acetylcysteine was first used by Webb et al. as a mucolytic agent for the liquefaction of tenacious bronchial secretions.[1] Vitamin C is a powerful antioxidant and provides a protective effect against several diseases including oxidative imbalances arising from various causes in the cornea. Vitamin E is a free radical scavenger and protects the cells from reactive oxygen species. It is considered first line of defense against lipid peroxidation and free radicals. Tappel et al. in his work “Vitamin E and Free Radical Peroxidation of Lipids” showed that vitamin E protected cell by breaking the chains of reactive oxygen species.[2]
Methods
The present study was conducted after obtaining the ethical clearance from Institutional Animal Ethical Committee {Certificate no. 8332/CAH dated 16.04.2013}. Single-breed rabbits, Oryctolagus cuniculus, of both sexes were used. The animals were housed under light controlled at a dim level for comfort, at the animal house. Each rabbit was handled with care and precautions and was transferred to the laboratory in plastic boxes for the experiment to be carried out.
All rabbits were anesthetized by intramuscular injection of 5% ketamine hydrochloride (35 mg/kg). Eye drape was applied over the eye to be operated. Proparacaine hydrochloride 0.5% was topically applied to each eye before the procedure. A pediatric eyelid speculum was placed under the lids to open the eyelids and expose the cornea. A 7.5 mm calibrated vacuum corneal trephine was used to induce a defect in the center of the cornea. The trephine depth was set to 100 microns. The trephined area was separated from the cornea by a crescent bevel-up blade. This procedure was performed on both eyes of all the rabbits.
The right eyes of all the rabbits were selected to act as experimental control, and the left eyes were selected to receive the trial drug. All eyes were administered the drugs four times per day (once every four hours from 8 am to 8 pm) for 14 days after the surgery. Rabbits were randomly divided into three groups: Control eyes of rabbits of all three groups received sterile Ringer Lactate solution; Group 1 received 10% Vitamin C eye drops. Group 2 received 3% Acetylcysteine eye drops; Group 3 received 1% Vitamin E eye drops [Fig. 1].
Figure 1.
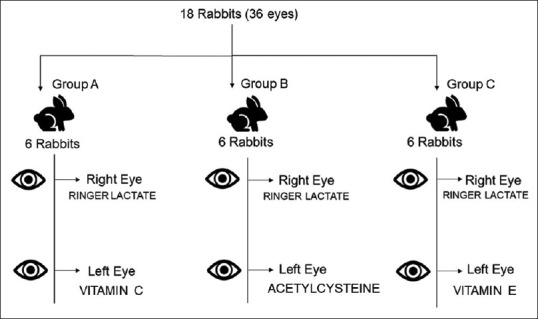
The layout of experimental design
All rabbits were administered one drop of Moxifloxacin ophthalmic solution (0.5%) topically in both eyes at least 10 min before receiving drugs or Ringer Lactate solution. Moxifloxacin treatment was started immediately after surgery and continued for 14 days to prevent infection. Examination of rabbit eyes was done to evaluate corneal epithelial wound healing and corneal haze. All observations were recorded on post wound induction day 2, day 7, and day 14.
To examine the corneal defect, fluorescein staining was done and visualized under cobalt blue light. It was defined as positive or negative. Healing was considered to be complete when no fluorescein stain uptake was visible with a cobalt blue light source. However, drops were continued till day 14 in all eyes, irrespective of whether the lesions had healed or not.
The longest horizontal (Lh) and longest vertical (Lv) lengths of the defect was measured and the area of corneal epithelial defect was approximately calculated as [longest horizontal (Lh) × longest vertical (Lv)].[3]
Corneal haze was graded as the following:
Grade 1 → haze not interfering with visibility of iris details
Grade 2 → mild obscuration of details of iris and lens
Grade 3 → moderate obscuration of details of iris and lens
Grade 4 → completely opaque stroma in the area of defect.[3]
Conjunctival swab (Both control and treated eye) was assessed for microbiological examination and culture on post surgery day 7 and day 14. The obtained data were statistically analyzed comparing the results of control with trial drugs and among the trial drugs themselves.
Statistical Package for the Social Sciences software version 23 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Mean and standard deviation were calculated for continuous variables. For continuous variables, independent t-test was used to determine the difference between the two groups. Fisher's exact test was used to compare categorical variables between the two groups. A probability (P) of 0.05 or less was considered statistically significant.
Results
Fluorescein stain
On day 2 and 7, fluorescein staining of defect area was positive in all the 18 eyes of experimental control group and drug groups. On day 14, 3 eyes out of 18 eyes of control group were fluorescein stain negative. In Vitamin C-treated eyes and acetylcysteine-treated eyes, all eyes were now fluorescein stain negative on Day 14, while 2 out of 6 eyes of vitamin E group remained fluorescein stain positive. The difference in results of fluorescein staining on Day 14 between Vitamin C-treated eyes and control group was statistically significant. (Fisher's Exact Test: P value = 0.001). It was also significant when acetylcysteine-treated eyes were compared with control group (Fisher's Exact Test: P value = 0.001) and Vitamin E-treated eyes with control group (Fisher's Exact Test: P value = 0.038). This analysis showed that all the trial drugs were better in epithelial wound healing when compared to control group on Day 14. When comparison was made among the trial drugs, all the three drugs were equally effective in treating the epithelial defect till day 14.
Corneal defect area measurement
Mean defect area in 18 experimental control eyes, on day 2 was 36.17 mm2, which reduced to a mean area of 1.86 mm2 on day 14 [Fig. 2]. In Vitamin C-treated eyes, the mean defect area on day 2 in was 34.13 mm2, which reduced to 0 mm2, as all the defects had healed by day 14. In acetylcysteine-treated eyes, mean defect area on day 2 was 19.17 mm2, which reduced to a mean area of 0 mm2 on day 14. The mean defect area on day 2 in six eyes of Vitamin E group was 37.04 mm2, which reduced to 0.013 mm2 on day 14.
Figure 2.
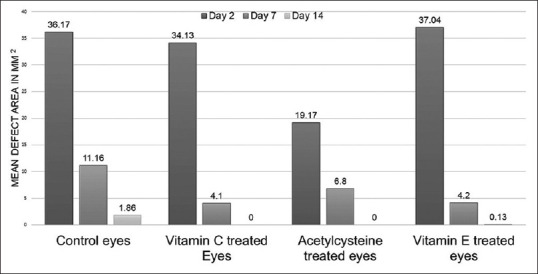
Corneal defect area (mm2) healing over 14 days
Statistical significance was seen on Day 2, when comparison of change in defect area was done between acetylcysteine and control group (Independent t-test: P value = 0.009).
On Day 7, it was significant in comparison between Vitamin C and control group (Independent t-test: P value = 0.030) and Vitamin E with control group (Independent t-test: P value = 0.027).
On Day 14, it was significant in comparison between Vitamin C and control group (Independent t-test: P value = 0.008), Acetylcysteine with control group (Independent t-test: P value = 0.008) and Vitamin E with control group (Independent t-test: P value = 0.013).
When comparison is made among the trial drugs, the only statistical significance was seen between acetylcysteine and Vitamin E (Independent t-test: P value = 0.005) on Day 2.
Conjunctival swabs (Both control and treated eye) assessed for microbiological examination on post surgery day 7 and day 14 revealed no bacteriological growth in all cases under study. Thus, prophylactic instillation of antibiotic drops seemed to be helpful in preventing any microbial infection in rabbit eyes.
Corneal haze
As shown in Fig. 3, on day 2, majority of eyes (61.11%) in experimental control group which received Ringer lactate had corneal haze of grade 3. In Vitamin C-treated eyes, five out of six eyes had corneal haze of grade 3. In majority of acetylcysteine-treated eyes (66.67%) and Vitamin E-treated eyes (83.33%), corneal haze of grade 2 was present. On day 2, statistical significance was seen only when comparison was made between Vitamin E-treated eyes and experimental control group, which received Ringer lactate (Likelihood ratio: P value 0.023).
Figure 3.
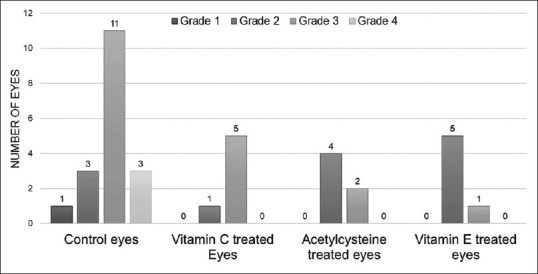
Grading of corneal haze on day 2
As shown in Fig. 4, on day 7, majority of eyes (55.56%) in experimental control group which received Ringer lactate had corneal haze of grade 3. In Vitamin C-treated eyes and acetylcysteine-treated eyes, all eyes had corneal haze of grade 2, while five out of six Vitamin E-treated eyes had corneal haze of grade 2. There was statistical significance when comparison was made between experimental control eyes and eyes which received Vitamin C (P-value = 0.011), acetylcysteine (P-value = 0.011), and Vitamin E (P-value = 0.019) respectively.
Figure 4.
Grading of corneal haze on day 7
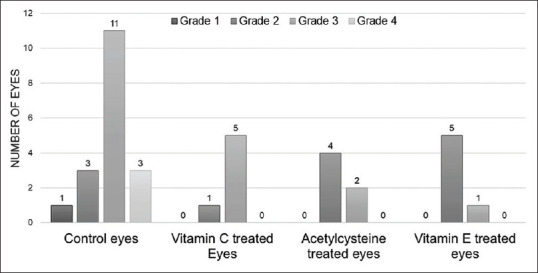
On day 14, [Fig. 5] majority of eyes (55.56%) in experimental control group which received Ringer lactate had corneal haze of grade 2. In both, Vitamin C-treated eyes and Vitamin E-treated eyes, four out of six eyes had corneal haze of grade 1, while five out of six acetylcysteine-treated eyes corneal haze of grade 2. There was statistical significance when comparison was made between experimental control eyes and eyes, which received Vitamin C (P-value = 0.004) and Vitamin E (P-value = 0.004). These results show that both Vitamin C and Vitamin E are better than the control group in terms of grade of corneal haze, whereas acetylcysteine shows a response similar to control group by day 14.
Figure 5.
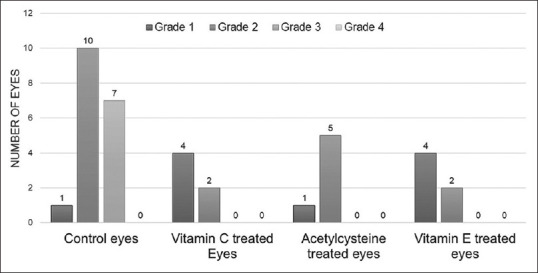
Grading corneal haze on day 14
Discussion
Acetylcysteine is a derivative of cysteine, which inhibits collagenase irreversibly by reducing disulphide bonds and by chelating calcium or zinc.[4] Florence et al., demonstrated a dose-related effect of acetylcysteine on the mucus layer; a 0.1 M solution of acetylcysteine was adequate to dissolve the mucus deposited on the conjunctival and corneal surfaces by blinking.[5] Their results demonstrated the mucolytic effect of acetylcysteine on this conjunctival mucus layer. The presence of free sulfahydryl groups were found necessary to reduce the viscosity of mucoprotein solutions, and increasing the concentration of acetylcysteine decreased the viscosity of the mucus. A lower mucus viscosity therefore would lead to a more rapid removal from precorneal and preconjunctival areas. In this study, no visible signs of intolerance to acetylcysteine were observed, except with the 20% acetylcysteine solution; the latter induced marked ocular irritation after instillation. In our study, the concentration of topical acetylcysteine used was 3%. Obenberger and Cejkov found that the hyperosmotic solution of acetylcysteine drew fluid into the corneal stroma, which caused mechanical damage.[6] Isosmolar acetylcysteine (3%) was essentially nontoxic; hyperosmolar acetylcysteine (20%) caused severe corneal destruction. Matrix metalloproteinases are secreted by corneal epithelial cells and stromal keratocytes and have a role in there modelling of extracellular matrix and migration of corneal epithelial cells on the underlying stroma. The results of study by Ramaesh et al., demonstrated that that acetylcysteine is effective at reducing matrix metalloproteinases-9 (MMP-9) secretion in human corneal epithelial cell cultures in a concentration-dependent manner (significant for 20 mmol and a nonsignificant trend for10 mmol).[7] The inhibitory properties of acetylcysteine on inflammation has been shown to act through nuclear factor-kB, which has a pivotal role in inducing the expression of multiple genes in immune and inflammatory responses. In the present study, all the six rabbit eyes that received topical acetylcysteine were fluorescein stain negative by day 14. This showed that all epithelial defects healed by day 14, which was significantly better result than the experimental control group, in which only 3 out of 18 rabbit eyes had turned fluorescein stain negative. In acetylcysteine-treated eyes, mean defect area on day 2 was 19.17 mm2, which reduced to a mean area of 0 mm2 on day 14.
Vitamin C is a powerful antioxidant, acts both outside and within the cell, and provides a protective effect against several diseases including oxidative imbalances arising from various causes in the cornea. L-ascorbic acid is a six-carbon lactone ring structure with 2, 3-enediol moiety. The antioxidant activity of ascorbic acid comes from 2, 3-enediol structure. After a corneal injury is sustained, there is activation of keratocytes (corneal fibroblasts). Proline and lysine must be taken up into the fibroblasts and then incorporated into the collagen peptide chain formed during ribosomal collagen protein synthesis. Impaired hydroxylation of proline and lysine, a reaction mediated by ascorbic acid, results in unassociated pro-α-chains lacking the protection of the triple helical structure. Such unstable collagen molecules are very vulnerable to the action of proteolytic enzymes. Kimoto et al., investigated the mechanisms by which L-ascorbic acid 2-phosphate (Asc-2P) increased the proliferation of human corneal endothelial cells (HCECs).[8] The growth of cultured HCECs was examined in the presence of various antioxidants, including Asc-2P, retinyl acetate (vitamin A), reduced glutathione, oxidized glutathione, and carnosine. Synthesis of type I, III, and IV collagen by HCECs cultured with or without Asc-2P was evaluated by measuring cell lysates and conditioned medium with Western blotting, immunocytochemistry, or enzyme-linked immunosorbent assay. They found that among the antioxidants tested, only L-ascorbic acid 2-phosphate (Asc-2P) promoted the growth of HCECs. Asc-2P did not promote deposition of type I, III, or IV collagen.
The concentration of topical Vitamin C used in the present study was 10%. The study by Pfister et al., showed that topical 10% ascorbate administered 14 times per day to alkali-burned eyes significantly reduced the incidence of corneal ulceration in the rabbit eye.[9] All ascorbate solutions of 10% or less, in distilled water or Adsorbo tear, instilled topically into rabbit eyes caused mild conjunctival injection, and mild blepharospasm for less than 2 min. The 20% ascorbate solutions caused moderate conjunctival reaction and moderate to marked blepharospasm for about 5 min.
In the present study, all the six rabbit eyes that received topical Vitamin C were fluorescein stain negative by day 14. This showed that all epithelial defects healed by day 14, which was significantly better result than the experimental control group, in which only 3 out of 18 rabbit eyes had turned fluorescein stain negative. In Vitamin C-treated eyes, mean defect area on day 2 was 34.13 mm2, which reduced to a mean area of 0 mm2 on day 14. Kasetsuwan et al., demonstrated that the acute corneal changes following excimer laser surgery in rabbits were favorably modified by ascorbate treatment.[10] Oxygen free radical-induced tissue damage in form of lipid peroxidation was demonstrated by the presence of positive fluorescent napthoic acid hydrazide carbonyl compounds. A statistically significant decrease of fluorescence was found in the corneal stroma of ascorbic acid-treated eyes compared with control eyes.
In the present study, on examination of the Vitamin C-treated eyes, five out of six eyes had corneal haze of grade 3 on day 2. On the final day of examination, day 14, four out of six eyes had corneal haze of grade 1. There was marked improvement in the corneal haze of Vitamin C-treated eyes by day 14, which was also significantly better than the control group.
Vitamin E is a free radical scavenger and protects the cells from reactive oxygen species. It is considered first line of defense against lipid peroxidation and free radicals. Tappel et al. in his work “Vitamin E and free radical peroxidation of lipids” showed that Vitamin E protected cell by breaking the chains of reactive oxygen species.[2]
In the present study, the concentration of Vitamin E used was 1%. Nagata et al., studied the aqueous humor and lens dynamics of 1% deuterium-labeled α-tocopherol acetate (D3-VEA) solution.[11] The concentrations of deuterium-labeled α-tocopherol acetate (D3-VEA) and D3-α-tocopherol (D3-VE), derived D3-VEA, in the aqueous humor and lens were measured after continuous instillation of 1% D3-VEA into the cul-de-sac of rat eyes for 1 or 3 weeks. In the aqueous humor, α-tocopherol acetate (VEA) and a-tocopherol (VE) concentrations increased more in the 3-week treatment group than in the 1-week treatment group. The increase in concentration was in proportion to the length of the treatment period.
In the present study, four out of the six rabbit eyes that received topical Vitamin E were fluorescein stain negative by day 14. This showed that majority of the epithelial defects healed by day 14, which was significantly better result than the experimental control group, in which only 3 out of 18 rabbit eyes had turned fluorescein stain negative. In Vitamin E-treated eyes, mean defect area on day 2 was 34.13 mm2, which reduced to a mean area of 0.013 mm2 on day 14. On examination of the Vitamin E-treated eyes, five out of six eyes had corneal haze of grade 2 on day 2. On the final day of examination, day 14, four out of six eyes had corneal haze of grade 1. There was marked improvement in the corneal haze of Vitamin E-treated eyes by day 14, which was also significantly better than the control group.
The beneficial effect of topical Vitamin E after photorefractive keratectomy (PRK) was shown by Bilgihan et al.[12] They investigated the effects of topical vitamin E and hydrocortisone acetate treatment on corneal healing response after 10.0 D PRK in rabbits. They concluded that deep corneal photoablation induces an aggressive healing response, and topical hydrocortisone acetate reduces this corneal wound healing effectively. The effect of topical Vitamin E on corneal wound healing seemed to be less than that of hydrocortisone acetate; Vitamin E treatment alone may have a limited effect on corneal wound healing after PRK, but combined treatment with these two drugs may have an additive effect in controlling corneal wound healing after PRK.
Acetylcysteine used topically on cornea is reported as a promising agent in the treatment of a range of ophthalmic disorders with oxidative stress component. Inhibitory effect of acetylcysteine on MMP-9 secretion and the reports on the inflammatory responses suggest that acetylcysteine may be useful to treat destructive corneal conditions in which MMP-9 activity and inflammatory cytokines are upregulated. Vitamin C is a powerful antioxidant and is helpful in regeneration of intracellular compounds such as glutathione, NADH, and NADPH. Vitamin C also removes hydrogen peroxidase and other free radicals, thereby adjusting the activity of glutathione peroxidase and catalase. Vitamin E is a free radical scavenger and protects the cells from reactive oxygen species. It is considered the first line of defense against lipid peroxidation and free radicals.
In the present study, these trial drugs with different mechanisms of action showed similar effect on healing of the experimentally created corneal wounds in rabbits, with comparison showing statistical insignificance.
Conclusion
Vitamin C, E, and acetylcysteine are potent corneal wound healing agents that lead to earlier rehabilitation and better visual prognosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Webb WR. Clinical evaluation of a new mucolytic agent acetylcysteine. J Thorac Cardiovasc Surg. 1962;44:330. [PubMed] [Google Scholar]
- 2.Tappel Al. Vitamin E and free radical peroxidation of lipids. Ann A Y Acad Sci. 1972;203:12–28. doi: 10.1111/j.1749-6632.1972.tb27851.x. [DOI] [PubMed] [Google Scholar]
- 3.Lai YH. Endothelin-1 enhances corneal fibronectin deposition and promotes corneal epithelial wound healing after photorefractive keratectomy in rabbits. Kaohsiung J Med Sci. 2008;24:254–61. doi: 10.1016/S1607-551X(08)70150-5. [DOI] [PubMed] [Google Scholar]
- 4.Brown SI, Weller CA, Wassermann HE. Collagenolytic activity of alkali burned corneas. Arch Ophthal. 1969;81:370–3. doi: 10.1001/archopht.1969.00990010372015. [DOI] [PubMed] [Google Scholar]
- 5.Florence T, Sylvain MN, Grove J. Effects of acetylcysteine on rabbit conjunctival and corneal surfaces a scanning electron microscopy study. Invest Ophthalmol Vis Sci. 1991;32:2958–63. [PubMed] [Google Scholar]
- 6.Obenberger J, Cejkova J. Corneal damage following intracorneal injection of N-acetyl-L-cysteine. Albrecht V Graefes Arch Klin Exp Ophthalmol. 1972;185:171. doi: 10.1007/BF00410060. [DOI] [PubMed] [Google Scholar]
- 7.Ramaesh T, Ramaesh K, Riley SC, West JD, Dhillon B. Effects of N-acetylcysteine on matrix metalloproteinase-9 secretion and cell migration of human corneal epithelial cells. Eye. 2012;26:1138–44. doi: 10.1038/eye.2012.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kimoto M, Shima N, Yamaguchi M, Amano S, Yamagami S. Role of hepatocyte growth factor in promoting the growth of human corneal endothelial cells stimulated by L-ascorbic acid 2-phosphate. Invest Ophthalmol Vis Sci. 2012;53:7583–9. doi: 10.1167/iovs.12-10146. [DOI] [PubMed] [Google Scholar]
- 9.Pfister RR, Paterson CA, Hayes SA. Topical ascorbate decreases the incidence of corneal ulceration after experimental alkali burns. Invest Ophthalmol Vis Sci. 1978;17:1019. [PubMed] [Google Scholar]
- 10.Kasetsuwan N, Heish F, Sanchez D, Macdonnel PJ. Effect of topical ascorbic acid on free radical tissue damage and inflammtory cell influx in the cornea after excimer laser corneal surgery. Arch Ophthalmol. 1999;117:649–52. doi: 10.1001/archopht.117.5.649. [DOI] [PubMed] [Google Scholar]
- 11.Nagata M, Kawazu K, Midori Y, Kojima M, Shirasawa M, Sasaki K. Intracameral and lenticular penetration of locally applied stable isotope labeled Vitamin E. Jpn J Ophthalmol. 2001;45:125–7. doi: 10.1016/s0021-5155(00)00361-0. [DOI] [PubMed] [Google Scholar]
- 12.Bilgihan K, Ozdek S, Ozogul C, Gurelik G, Bilghihan A. Topical Vitamin E and hydrocortisone acetate treatment after PRK. Eye. 2000;14:231–7. doi: 10.1038/eye.2000.60. [DOI] [PubMed] [Google Scholar]


