Abstract
Purpose:
The aim of this study was to compare the incidence of post laser in situ keratomileusis (LASIK) dry eye with and without intraoperative extended duration temporary punctal plug placement.
Methods:
This retrospective study included myopicastigmatic eyes without a preoperative diagnosis of dry eye disease that underwent LASIK surgery between January 2017, and March 2018. Patients who received punctal plugs during surgery in addition to usual postoperative care were compared to a control group who received usual postoperative care alone. Visual acuity, safety and efficacy indices, as well as predictability and presence of dry eye disease were assessed 3–6 months after surgery.
Results:
A total of 345 eyes of 345 patients were included, 172 eyes received punctal plugs and 173 did not. The mean age was 30.4 ± 10 years (range: 17–60 years) and 46.1% (N = 159) were female. Both groups were similar in terms of preoperative parameters, including age, gender, spherical equivalent, pachymetry or contact lens use. Patients treated with punctal plugs had significantly less postoperative dry eye complaints (N = 37 vs. 58, 21.5% vs. 34.1% respectively, P = 0.001). Patients treated with plugs that did develop dry eye disease did so later (51.2 ± 77.64 days' vs. 20.78 ± 26.9 days, P = 0.009). Postoperative visual acuities were similar between groups (P > 0.05) at all postoperative follow-up visits as were safety (0.95 ± 0.16 vs. 0.99 ± 0.09, P = 0.30) and efficacy (1.01 ± 0.13 vs. 1.00 ± 0.11, P = 0.52) indices.
Conclusion:
Preventative temporary punctal plug placement during LASIK appears to reduce dry eye disease in the short term, without affecting visual acuity outcomes.
Keywords: Dry eye, laser in situ keratomileusis, punctal plugs, visual acuity
Laser refractive surgery is the most common surgical technique for correcting refractive errors.[1] Moreover, there has been an increase in laser assisted in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK) surgery in recent years. However, many patients experience dry eye disease, especially in the early postoperative period.[2,3,4,5]
Several theories exist as to how LASIK contributes to the pathophysiology of dry eye. Some of the reasons for post LASIK dry eye include reduced tear amount or quality[5] and morphologic changes of corneal nerves resulting in damage to corneal sensation.[5,6,7,8,9] Importantly, dry eye is associated with refractive regression after both myopic and hyperopic LASIK,[7] an effect reduced in patients who are treated with an aggressive and scheduled regimen.[10,11]
The purpose of the study was to compare the incidence of post LASIK dry eye with and without intraoperative temporary punctal plug placement, using a retrospective comparative before and after design.
Methods
All data for this study were collected and analyzed in accordance with the policies and procedures of the institutional review board, Barzilai Medical Center and the tenets set forth in the declaration of Helsinki.
Study participants
Patients undergoing LASIK, by a single high-volume surgeon (I.K), in a refractive surgery facility (Care Vision, Tel Aviv, Israel) between January 2017, and March 2018 were included. The patients were divided into two groups, patients who received prophylactic temporary extended duration (3 months) punctal plugs (Oasis Medical, Glendora, California) and patients who did not receive postoperative punctal plugs (control group), except of both groups received the same therapeutic regimen. From January 2017 to August 2017 patients routinely received intraoperative prophylactic punctal plugs. From September 2017 until March 2018 patients no longer received the punctal plugs and served as controls. Plugs were inserted to both eyes, only the right eye of each patient was included in the analysis in order to avoid biases resulting from inter-eye correlation.
Data collection
The following demographic and preoperative data were collected: Age, gender, sphere, cylinder, spherical equivalent (SEQ), mean keratometry and pachymetry. The following postoperative parameters were collected: Uncorrected distance visual acuity (UDVA) at one day, one week and one month, sphere, cylinder. Efficacy and safety indices were calculated. In addition, postoperative dry eye disease was assessed based on clinical findings and patient complaints. Clinical findings routinely documented at our institution include presence of superficial punctate keratitis (SPK), and meibomian gland disease (MGD). In addition, time (days) between surgery and dry eye disease was collected.
The inclusion criteria of the study were adult (over 18 years) and patients undergoing LASIK surgery, operated on by a single high-volume surgeon (I.K). The exclusion criteria of the study were patients with previous ocular surgery, or ocular comorbidities including dry eye syndrome. A flow diagram of the inclusion process is illustrated in Fig. 1.
Figure 1.
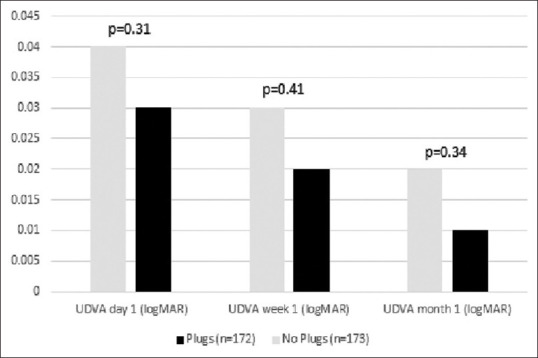
Comparison between UDVA (logMAR) between groups
Dry eye disease diagnosis
Patient with any complaints or signs of dry eye disease following LASIK are routinely evaluated with the OSDI questionnaire and if the score is above 12 they are considered to have dry eye disease.
Main outcome measures
The main outcome was the presence of dry eye disease. Secondary outcomes were visual acuity, safety and efficacy indices.
Surgical technique
All patients underwent microkeratome assisted LASIK using a technique as previously described by us 12. A Moria SBK, 90 microkeratome (Moria, Antony, France) was used to create the nasal-hinge flap and the stromal bed was ablated using the Allegretto EX500 excimer laser (Alcon WaveLight AG, Erlangen, Germany).
An extended duration collagen punctal plug (Oasis Medical, Glendora, California, USA), with length of 2 mm was used. It is designed to be inserted into the punctal opening in order to provide partial occlusion of the puncta and limited tear drainage through the canaliculus. Two plugs were inserted in the inferior punctum in both eyelids at the beginning of the LASIK procedure.
Postoperative care of both groups included moxifloxacin 0.5%, dexamethasone 0.1% and nonpreserved artificial tears. Artificial tears containing hyaluronic acid were used 5 times a day by both groups. Patients were routinely examined at one day, one week and three months postoperatively and thereafter as necessary. In addition, patients were encouraged to return for examinations if vision deteriorated or dryness symptoms were felt at any time after surgery and offered additional treatments free of charge.
Statistical analysis
Data were analyzed using Minitab software (version 17, Minitab, Paris, France). Normal distribution was assessed by the Shapiro–Wilk test. For continuous variables with a normal distribution an independent test was used and the Mann–Whitney U test for non-normally distributing variables. For categorical variables the χ2 or Fisher's tests were used. Visual outcomes were converted to LogMAR for statistical analysis. The values of P < 0.05 on a two-sided test were considered statistically significant. Unless otherwise specified values are given as mean ± standard deviation.
Results
A total of 345 right eyes (173 without plugs and 172 with plugs) were included. Mean patient age was 30.4 ± 10 years (range: 18-60 years) and 46.1% (N = 159) were female. Mean spherical equivalence was –2.72 ± 1.77 D.
Demographic and preoperative data
Table 1 details a comparison of preoperative parameters between the study and control groups. Briefly, both groups were similar in terms of age (30.45 ± 9.8 vs. 30.38 ± 10.3 respectively, P = 0.95), gender (N = 78 vs. 81, 45.3% vs. 46.8% females, respectively, P = 0.78), sphere (–2.45 ± 1.81 D vs. -2.24 ± 1.78 D, P = 0.29), cylinder (–0.74 ± 0.79 D vs. –0.76 ± 0.65 D, P = 0.79), UDVA (LogMAR) (1.15 ± 0.58 vs. 1.21 ± 0.62 (20/282 vs. 20/324 Snellen), P = 0.38) and CDVA (logMAR) (0.016 ± 0.04 vs. 0.016 ± 0.03 (20/20.46 vs. 20/20.46 Snellen), P = 0.98).
Table 1.
A comparison of the baseline parameters between the punctal plug and control groups of the 345 eyes included in this study
| No Plugs (n=173) Mean±SD | Plugs (n=172) Mean±SD | P | |
|---|---|---|---|
| Age (years) | 30.38±10.3 | 30.45±9.8 | 0.95 |
| Gender (F) | 81 (46.8%) | 78 (45.3%) | 0.78 |
| Sphere (D) | -2.24±1.78 | -2.45±1.81 | 0.29 |
| Cylinder (D) | -0.76±0.65 | -0.74±0.79 | 0.79 |
| Spherical equivalent (D) | -2.62±1.79 | -2.82±1.74 | 0.30 |
| Mean keratometry (D) | 43.87±1.27 | 43.98±1.18 | 0.41 |
| Pachymetry (µm) | 545.03±27.55 | 548.98±28.54 | 0.19 |
| Contact lens use | 68 (39.3%) | 74 (43.0%) | 0.48 |
| Preoperative UDVA (logMAR) | 1.21±0.62 | 1.15±0.58 | 0.38 |
| Preoperative BDVA (logMAR) | 0.016±0.03 | 0.016±0.04 | 0.98 |
D: Diopter, F: Female, SD: Standard deviation, UDVA: Uncorrected distance visual acuity, BDVA: Best corrected distance visual acuity
Postoperative dry eye
In patients treated with punctal plugs, there was significantly less superficial punctate keratitis (SPK's) during follow-up (N = 15 vs. 36, 8.7% vs. 20.8%, P = 0.002) and a significant reduction in subjective dryness complaints (N = 37 vs. 59, 21.5% vs. 34.1%, P = 0.01) postoperatively, as illustrated in Fig. 2. The length of time from surgery to first complaint of dry eye was longer in the group treated with punctal plugs, (51.2 ± 77.64 days vs. 20.78 ± 26.9 days, P = 0.009). The presence of moderate to severe meibomian gland dysfunction (MGD) was not significantly different between groups (N = 16 vs. 10, 9.7% vs. 5.8%, P = 0.16), as illustrated in Fig. 3. All those results are detailed in Table 2.
Figure 2.
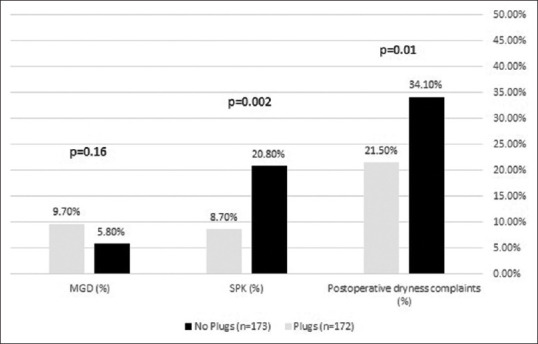
Comparison between different types of dryness between groups
Figure 3.
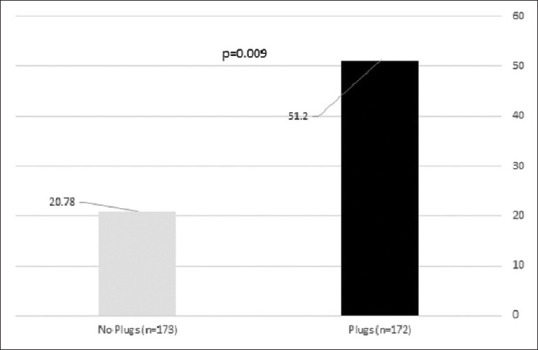
Comparison in time to dryness (days) between groups
Table 2.
Main Outcomes
| A comparison of outcomes between the punctual plug and control groups | |||
|---|---|---|---|
| No Plugs (n=173) Mean±SD | Plugs (n=172) Mean±SD | P | |
| UDVA day 1 (logMAR) | 0.04±0.08 | 0.03±0.08 | 0.31 |
| UDVA week 1 (logMAR) | 0.03±0.09 | 0.02±0.06 | 0.41 |
| UDVA month 1 (logMAR) | 0.02±0.078 | 0.01±0.41 | 0.34 |
| Efficacy index | 1.00±0.11 | 1.01±0.13 | 0.52 |
| Safety index | 0.99±0.09 | 0.95±0.16 | 0.3 |
| Post-operative Spherical equivalent (D) | -0.03±0.18 | -0.03±0.17 | 0.9 |
| Postoperative dryness complaints (%) | 34.1% | 21.5% | 0.01 |
| SPK (%) | 20.8% | 8.7% | 0.002 |
| MGD (%) | 5.8% | 9.7% | 0.16 |
| Time to dryness (days) | 20.78±26.9 | 51.2±77.64 | 0.009 |
F: Female, SD: Standard Deviation, K: Keratometry, UDVA: Uncorrected distance visual acuity, BCVA: Best-corrected visual acuity, SPK: Superficial punctate keratitis, MGD: Meibomian gland dysfunction. D: Diopter
Refractive outcomes
The visual and refractive outcomes were not statistically significant differences between the groups. UDVA (LogMAR) was similar in both groups at 1 day (0.03 ± 0.08 vs. 0.04 ± 0.08, P = 0.31), 1 week (0.02 ± 0.06 vs. 0.03 ± 0.09, P = 0.41), and 1 month (0.01 ± 0.41 vs. 0.02 ± 0.07, P = 0.34) following surgery. Spherical equivalent was also similar (–0.03 ± 0.17 vs. -0.03 ± 0.18, P = 0.9), as were safety and efficacy indices (safety: 0.95 ± 0.16 vs. 0.99 ± 0.09, P = 0.3 and efficacy: 1.01 ± 0.13 vs. 1.00 ± 0.11, P = 0.52) as illustrated in Fig. 4.
Figure 4.
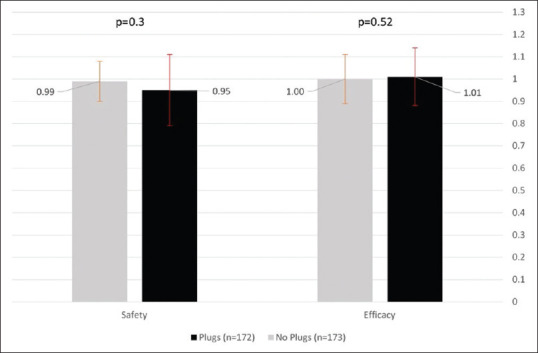
Comparison between efficacy and safety between groups
Complications and side effects
No complications following insertion of the plugs were reported throughout the short and long-term follow-up period.
Discussion
This study evaluated post LASIK dry eye disease with and without temporary lower punctal occlusion. Punctal plugs reduced dry eye symptoms by approximately 13%, reduced SPK by 12% and delayed dry eye disease by more than 30 days. As expected visual outcomes including CDVA, safety and efficacy indices were unaffected in the short term, and no adverse events were reported.
Dry eye is a common side effect after LASIK, affecting up to 40% of patients during the first 3–6 months following the procedure.[1,2,3] The mechanism of post-LASIK dry eye is multifactorial, including loss of corneal neurotrophic effect, reduced blinking rate, mucin deficiency and changes in the corneal curvature.[6,7,8,9,12,13] Dry eyes following LASIK have been implicated in various adverse outcomes including lower patient satisfaction,[9,10] ocular surface staining, and delayed recovery of corneal sensation.[11,14,15,16] In addition, visual acuity might also be adversely affected by postoperative dry eye.[15] Tanaka et al. reported decreased visual acuity during the recovery period,[17] while other studies indicate no significant difference in refractive outcomes.[18,19] Post-LASIK dry eye can usually be managed by conventional dry-eye treatment and artificial tears. However, these treatments are not always sufficient.[15]
Punctal plugs have become a common procedure for treatment of various types of dry eye, they enable to retain both patients own natural tears and artificial tears for a longer period, enhancing their effect.[14,16,20] Dry eye post LASIK can be managed effectively in most of the patients by medications alone, only those who continue to have symptoms despite this may be candidates for plugs and this can be decided to post operatively. s patients can enter a “vicious cycle” of dry eye we assessed whether prophylactic plugs would be beneficial.
In this study there was no statistically significant difference between patients with or without punctal plugs in terms of visual or refractive outcomes. However, there were statistically and clinically significant differences between the groups in terms of dry eye disease. In addition, there was a significant difference in the time to development of complaints. Patients that received punctal plugs postoperatively experienced dry eye symptoms about a month later than the control group.
Several other studies have explored this approach. Huang and associates report that punctal occlusion in post-LASIK dry eye patients reduced total, lower, and higher-order wavefront aberrations. They emphasize that reduction of wavefront aberrations resulted in a significant improvement of subjective qualitative vision and better visual acuity.[11] In a retrospective study by Khalil et al. 18 patients with low refractive errors showed improvement in visual acuity after punctal plug placement.[19]
In the current study although there was no advantage in terms of visual or refractive outcomes, there was a clear advantage in terms of dry eye disease. This is supported by the findings of Alfawaz et al. who found that a higher percentage of eyes with punctal plugs were negative for ocular surface disease parameters (Schirmer 1 test, tear breakup time and punctate epithelial keratitis score), however such differences were not statistically significant.[21] They concluded that punctal plug insertion after LASIK surgery may minimize the need for frequent lubricant application and hence improve patient satisfaction. Recently, Yang et al. found that punctal plugs can improve quality of vision and suggested that punctal occlusion for both puncta is effective for patients with post-LASIK dry eye that cannot be controlled by artificial tears alone.[22]
In this study, in the group of patients without plugs placement, complaining of dry eye following surgery was 34%, and those with evidence of SPK was 20.8%. These proportions are similar to the reported literature at 30% -to 60%.[3,5,23] The study group had reduced rates of 34.1% and 21.5% respectively, which represent a 12.6% reduction. These proportions correspond to a reduction of 126 patients out of every 1000 that would have suffered from dry eye postoperatively otherwise.
This study has several limitations. First, is its retrospective nature, however, the routine use of punctal plugs, that was momentarily ceased, allowed for a before-and-after design. Secondly, potential additional costs of this prophylactic treatment should be outweighed against the benefits. In addition, the physician assessing of dry eye diagnosis based on clinical examination which was made by various doctors.
Conclusion
In conclusion, in this study, patients that received temporary post-LASIK punctal plug placement had less dry eye disease in the short term. In addition, when dry eye disease did develop it developed later than those that did not receive the plugs. We thus recommend to consider temporary prophylactic punctal plugs in patients at risk for dry eye disease following LASIK.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sutton G, Lawless M, Hodge C. Laser in situ keratomileusis in 2012: A review. Clin Exp Optom. 2014;97:18–29. doi: 10.1111/cxo.12075. [DOI] [PubMed] [Google Scholar]
- 2.Melki SA, Azar DT. LASIK complications: Etiology, management, and prevention. Surv Ophthalmol. 2001;46:95–116. doi: 10.1016/s0039-6257(01)00254-5. [DOI] [PubMed] [Google Scholar]
- 3.Hovanesian JA, Shah SS, Maloney RK. Symptoms of dry eye and recurrent erosion syndrome after refractive surgery. J Cataract Refract Surg. 2001;27:577–84. doi: 10.1016/s0886-3350(00)00835-x. [DOI] [PubMed] [Google Scholar]
- 4.Raoof D, Pineda R. Dry eye after laser in-situ Keratomileusis. Semin Ophthalmol. 2001;132:1–7. doi: 10.3109/08820538.2014.962663. [DOI] [PubMed] [Google Scholar]
- 5.Yu EY, Leung A, Rao S, Lam DS. Effect of laser in situ keratomileusis on tear stability. Ophthalmology. 2000;107:2131–5. doi: 10.1016/s0161-6420(00)00388-2. [DOI] [PubMed] [Google Scholar]
- 6.Linna TU, Vesaluoma MH, Pérez-Santonja JJ, Petroll WM, Alió JL, Tervo TMT. Effect of myopic LASIK on corneal sensitivity and morphology of subbasal nerves. Investig Ophthalmol Vis Sci. 2000;41:393–7. [PubMed] [Google Scholar]
- 7.Konomi K, Chen LL, Tarko RS, Scally A, Schaumberg DA, Azar D, et al. Preoperative characteristics and a potential mechanism of chronic dry eye after LASIK. Investig Ophthalmol Vis Sci. 2008;49:168–74. doi: 10.1167/iovs.07-0337. [DOI] [PubMed] [Google Scholar]
- 8.Shoja MR, Besharati MR. Dry eye after LASIK for myopia: Incidence and risk factors. Eur J Ophthalmol. 2007;17:1–6. doi: 10.1177/112067210701700101. [DOI] [PubMed] [Google Scholar]
- 9.Pérez-Santonja JJ, Sakla HF, Cardona C, Chipont E, Alió JL. Corneal sensitivity after photorefractive keratectomy and laser in situ keratomileusis for low myopia. Am J Ophthalmol. 1999;127:497–504. doi: 10.1016/s0002-9394(98)00444-9. [DOI] [PubMed] [Google Scholar]
- 10.Salib GM, McDonald MB, Smolek M. Safety and efficacy of cyclosporine 0.05% drops versus unpreserved artificial tears in dry-eye patients having laser in situ keratomileusis. J Cataract Refract Surg. 2006;32:772–8. doi: 10.1016/j.jcrs.2005.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Huang B, Mirza MA, Qazi MA, Pepose JS. The effect of punctal occlusion on wavefront aberrations in dry eye patients after laser in situ keratomileusis. Am J Ophthalmol. 2004;137:52–61. doi: 10.1016/s0002-9394(03)00903-6. [DOI] [PubMed] [Google Scholar]
- 12.Toda I, Asano-Kato N, Komai-Hori Y, Tsubota K. Dry eye after laser in situ keratomileusis. Am J Ophthalmol. 2001;132:1–7. doi: 10.1016/s0002-9394(01)00959-x. [DOI] [PubMed] [Google Scholar]
- 13.Yu EY, Leung A, Rao S, Lam DS. Effect of laser in situ keratomileusis on tear stability. Ophthalmology. 2000;107:2131–5. doi: 10.1016/s0161-6420(00)00388-2. [DOI] [PubMed] [Google Scholar]
- 14.Kaido M, Ishida R, Dogru M, Tsubota K. A new punctal plug insertion technique to prevent intracanalicular plug migration. Am J Ophthalmol. 2009;147:178–182e1. doi: 10.1016/j.ajo.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 15.Shtein RM. Post-LASIK dry eye. Expert Rev Ophthalmol. 2011;6:575–82. doi: 10.1586/eop.11.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freeman JM. The punctum plug: Evaluation of a new treatment for the dry eye. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1975;79:OP874–9. [PubMed] [Google Scholar]
- 17.Tanaka M, Takano Y, Dogru M, Toda I, Asano-Kato N, Komai-Hori Y, et al. Effect of preoperative tear function on early functional visual acuity after laser in situ keratomileusis. J Cataract Refract Surg. 2004;30:2311–5. doi: 10.1016/j.jcrs.2004.02.086. [DOI] [PubMed] [Google Scholar]
- 18.Chalita MR, Chavala S, Xu M, Krueger RR. Wavefront analysis in post-LASIK eyes and its correlation with visual symptoms, refraction, and topography. Ophthalmology. 2004;111:447–53. doi: 10.1016/j.ophtha.2003.06.022. [DOI] [PubMed] [Google Scholar]
- 19.Khalil MB, Latkany RA, Speaker MG, Yu G. Effect of punctal plugs in patients with low refractive errors considering refractive surgery. J Refract Surg. 2007;23:467–71. doi: 10.3928/1081-597X-20070501-08. [DOI] [PubMed] [Google Scholar]
- 20.Tuberville AW, Frederick WR, Wood TO. Punctal Occlusion in Tear Deficiency Syndromes. Ophthalmology. 1982;89:1170–2. doi: 10.1016/s0161-6420(82)34659-x. [DOI] [PubMed] [Google Scholar]
- 21.Alfawaz AM, Algehedan S, Jastaneiah SS, Al-Mansouri S, Mousa A, Al-Assiri A. Efficacy of punctal occlusion in management of dry eyes after laser in situ keratomileusis for myopia. Curr Eye Res. 2014;39:257–62. doi: 10.3109/02713683.2013.841258. [DOI] [PubMed] [Google Scholar]
- 22.Yung YH, Toda I, Sakai C, Yoshida A, Tsubota K. Punctal plugs for treatment of post-LASIK dry eye. Jpn J Ophthalmol. 2012;56:208–13. doi: 10.1007/s10384-012-0125-8. [DOI] [PubMed] [Google Scholar]
- 23.Levinson BA, Rapuano CJ, Cohen EJ, Hammersmith KM, Ayres BD, Laibson PR. Referrals to the Wills eye institute cornea service after laser in situ keratomileusis: Reasons for patient dissatisfaction. J Cataract Refract Surg. 2008;34:32–9. doi: 10.1016/j.jcrs.2007.08.028. [DOI] [PubMed] [Google Scholar]


