Abstract
Purpose:
The aim of this study was to compare the visual outcome of participants undergoing toric intraocular lens (IOL) implantation after cataract extraction using manual marking versus digital marking for intraoperative guidance.
Methods:
Randomized controlled trial of participants with cataract and corneal astigmatism of 1.00 D-4.50 D. The eyes were grouped into manual marking (Group 1) and digital marking (Group 2). Preoperative Uncorrected distance visual acuity (UDVA), Corrected distance visual acuity (CDVA), and corneal astigmatism were determined. IOL power and axis of alignment were determined using Barrett toric calculator. Eyes were marked by bubble marker and Mendez ring in group 1 and by VERION (Alcon, Fort Worth, Texas) digital overlay in Group 2. Postoperatively, UDVA, CDVA, residual refractive cylinder and IOL misalignment were determined (iTrace system, Tracey technologies) at 1 week, 6 weeks, and 3 months.
Results:
A total of 61 eyes of 50 participants, 31 in Group 1 and 30 in Group 2, were studied. The mean postoperative cylindrical error was 0.50 ± 0.39 D in Group 1 and 0.29 ± 0.34 D in Group 2 (P = 0.03). 67.74% (n = 21) and 93.55% (n = 29) eyes achieved a residual astigmatism of ≤0.50 D and ≤1.00 D, respectively, in Group 1, whereas 83.33% (n = 25) and 100% (n = 30) eyes achieved a residual astigmatism of ≤0.50 D and ≤1.00 D, respectively, in Group 2 at 3 months postoperatively. Toric IOL misalignment was 4.71 ± 3.12° in Group 1 and 4.03 ± 2.99° in Group 2 (P = 0.39).
Conclusion:
Accurate manual marking and digital marking are equally effective guides for toric IOL alignment, intraoperatively.
Keywords: Astigmatism, IOL misalignment, marking, toric IOL, VERION
Toric IOLs offer patients with higher degrees of corneal astigmatism, spectacle independence after cataract surgery. One degree error in IOL alignment results in 3.3% decrease in the correction of astigmatism.[1,2,3]
Marking aims at improving the accuracy of incision location and IOL alignment. Accuracy in manual marking methods is affected by head position, errors on marking and smearing of ink. Digital marking methods are aimed at reducing intraoperative IOL misalignment using images captured in the sitting position which are used as overlay for IOL alignment intraoperatively.[3]
This study compares the outcome of Toric IOL implantation guided by manual or digital marking techniques.
Methods
This study was a prospective randomized controlled trial conducted at a tertiary eye care superspeciality eye hospital in South India between September 2017 and January 2019. The study was in accordance with the institutional ethics committee and the Helsinki Declaration of 1975. Institutional ethics committee approval was obtained before commencing the study.
Eyes of participants with cataract and regular corneal astigmatism, undergoing cataract extraction with toric monofocal IOL implantation were included in the study. Eyes with irregular corneal astigmatism, previous intraocular or corneal surgeries, intraoperative complications compromising Toric IOL position such as zonular damage, vitreous loss, capsulorrhexis tear, posterior capsular rupture or any condition which could interfere with the visual outcome or with the postoperative assessment of the outcome such as high myopia, glaucoma, retinal disease, postoperative miosis, prolonged postoperative iritis, etc., were excluded. The surgeries were performed by five surgeons.
Preoperatively, UDVA and CDVA were determined by Snellen's chart and converted to logMAR. Preoperative astigmatism was determined by refraction, manual keratometry using Bausch and Lomb manual keratometer (Bausch and Lomb, U.S.A) and automated keratometry using IOL Master 700 (Carl Zeiss Meditec.). Preoperative biometry was done using IOL Master 700. In cases of discrepancy between the manual and automated keratometry values, the automated keratometry values were used. IOL power was determined using the AcrySof Toric calculator available online, which incorporates the Barrett Toric Calculator, incorporating the estimated posterior corneal astigmatism. Here, a mathematical model is used to estimate the posterior corneal astigmatism instead of direct measurement. However, the Barrett Toric mathematical model has been found to be exceedingly accurate and comparable to direct measurement methods.[4,5] Surgically induced astigmatism was pre-calculated to be 0.10 D by analysing the centroid for all the surgeons. Schirmer test, specular microscopy with EM-3000 (Tomey, U.S.A) and Optical Coherence Tomography with Avanti widefield OCT (Optovue, U.S.A) were done to rule out other ocular pathology. Participants were randomly assigned to Group 1 or Group 2 using random number table. Preoperative workup was done by an optometrist. Manual marking was done by the surgeon using Nuijts Solomon bubble marker (ASICO LLC) for Group 1. Limbal marking was done in sitting position. Digital marking was done using VERION for Group 2. Reference images of the participants' eyes were captured and exported to the operating microscope.
Phacoemulsification was performed by a 2.2 mm temporal clear corneal incision at the incision site determined by the Toric calculator. The target capsulorhexis diameter was 5.0-5.5 mm to ensure overlap of the IOL border. Centration of the capsulorrhexis was achieved in group 1 by the aid of a ring calliper and in group 2 by the digital image guidance offered by VERION overlay. After cataract extraction, all patients received an AcrySof Toric IOL monofocal implant. Gross alignment was done by placing the IOL horizontally or 20-30 degrees short of intended axis counter-clockwise. Viscoelastic was removed and the IOL was then finally rotated to align the cylinder axis with the marked corneal meridian. For participants in Group 1, Mendez ring (Geuder AG) was used to determine the incision site and identify the axis of toric IOL alignment. For participants in Group 2, VERION digital overlay was used to guide the procedure.
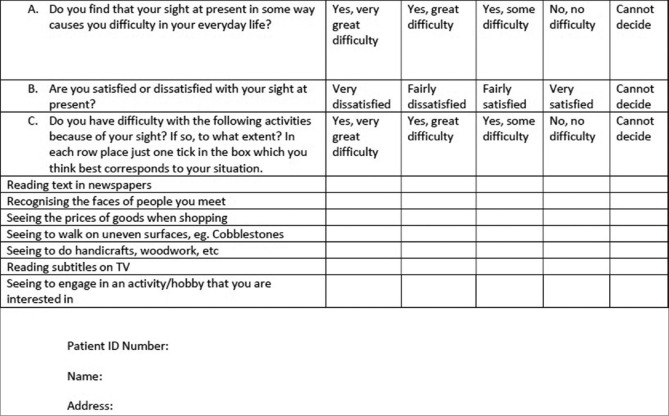
Postoperative follow up included assessment of visual acuity in terms of UDVA and CDVA, residual cylindrical error by subjective refraction and Toric IOL alignment by slit-lamp examination and ray-tracing aberrometer/topographer with iTrace (Tracey Technologies) at 1 week, 6 weeks, and 3 months postprocedure. Assesment of IOL position by Itrace and slit-lamp examination is shown in Figs. 1 and 2. Postoperative manual keratometry or optical biometry was not done. Patient satisfaction was assessed by the Catquest-9SF 2011 questionnaire, at the end of 3 months. The questionnaire used is given in Fig. 3. The cut-off for IOL re-rotation in case of misalignment was 10 degrees.
Figure 1.

Assessment of IOL position by Itrace (Tracey technologies)
Figure 2.
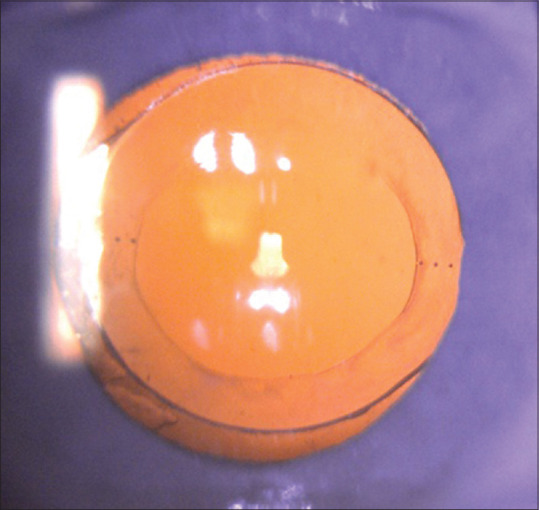
Assessment of IOL position by slit-lamp examination
Figure 3.
Catquest-9SF 2011 questionnaire
Statistical analysis
Sample size was calculated to be 56, 28 in each group and increased to 59 considering contingencies such as nonresponse or recording error. It was then rounded off to 60, 30 in each group.
Statistical analysis of the obtained data was done using Excel 2007 (Microsoft) and SPSS software, version 26.0 (SPSS, Chicago, Illinois).
Student's t test was used for statistical analysis. Intragroup analysis was done using Independent sample t-test and paired sample t test was used for intergroup analysis. A value of P < 0.05 was considered significant.
Results
A total of 61 eyes of 50 participants, 22 female (44%) and 28 male (56%), were studied. The mean age of the participants enrolled was 63.50 ± 7.79 years (range 37–80 years). The demographic and preoperative details of the participants in both the groups are summarized in Table 1. There were no eyes with traumatic or congenital cataract. None of the eyes had pseudoexfoliation. In Group 1, 25 eyes had against-the-rule astigmatism, 5 eyes had with-the-rule astigmatism, and 1 eye had oblique astigmatism. In Group 2, it was 21 eyes, 7 eyes, and 2 eyes, respectively.
Table 1.
Demographic details of participants in the manual and digital marking groups
| Demographic details | Group 1 | Group 2 | P |
|---|---|---|---|
| Number of eyes | 31 | 30 | |
| Number of patients | 25 | 25 | |
| Mean age (years) | 63.04 ± 9.77 | 62.68 ± 5.50 | |
| Gender (male:female) | 14:11 | 14:11 | |
| Laterality (right eye:left eye) | 15:16 | 14:16 | |
| Mean UDVA (logMAR) | 0.63 ± 0.26 | 0.54 ± 0.24 | 0.23 |
| Mean CDVA (logMAR) | 0.28 ± 0.21 | 0.29 ± 0.22 | 0.81 |
| Mean Refractive cylinder (dioptres) | 1.44 ± 1.25 | 1.47 ± 1.02 | 0.94 |
| Mean astigmatism on manual keratometry (dioptres) | 1.94 ± 0.81 | 1.49 ± 0.02 | 0.02 |
| Mean astigmatism on automated keratometry (dioptres) | 2.01 ± 0.83 | 1.72 ± 0.55 | 0.11 |
| Mean IOL cylindrical power (dioptres) | 3.19 ± 1.04 | 2.70 ± 0.94 | 0.06 |
The visual outcomes after Toric IOL implantation in both the groups are given in Tables 2 and 3 and the residual astigmatism in the two groups is depicted in Table 4. No significant difference was observed between the outcomes of the two groups in terms of UDVA (P = 0.85) and CDVA (P = 0.74). In both groups, there was a significant improvement in UDVA and CDVA from preoperative period to postoperative period at 1 week, 6 weeks, and 3 months (P < 0.00001 for both groups at all postoperative visits). 41.94% (n = 13) and 43.33% (n = 13) eyes in Groups 1 and 2, respectively, had a postoperative UDVA of 20/20. 96.77% (n = 30) and 96.67% (n = 29) eyes in Groups 1 and 2, respectively, had a postoperative UDVA of 20/40 or better.
Table 2.
Postoperative UDVA (in logMAR) of eyes in the two groups
| Postoperative duration | Group 1 | Group 2 | P |
|---|---|---|---|
| 1 week | 0.16 ± 0.19 logMAR | 0.11 ± 0.12 logMAR | 0.29 |
| 6 weeks | 0.15 ± 0.20 logMAR | 0.10 ± 0.12 logMAR | 0.28 |
| 3 months | 0.09 ± 0.10 logMAR | 0.10 ± 0.11 logMAR | 0.85 |
Table 3.
Postoperative CDVA (in logMAR) of eyes in the two groups
| Postoperative duration | Group 1 | Group 2 | P |
|---|---|---|---|
| 1 week | 0.04 ± 0.08 logMAR | 0.04 ± 0.08 logMAR | 0.88 |
| 6 weeks | 0.03 ± 0.07 logMAR | 0.02 ± 0.04 logMAR | 0.43 |
| 3 months | 0.01 ± 0.03 logMAR | 0.01 ± 0.04 logMAR | 0.74 |
Table 4.
Postoperative residual refractive cylinder (in dioptres) in the two groups
| Postoperative duration | Group 1 | Group 2 | P |
|---|---|---|---|
| 1 week | 0.49 ± 0.75 D | 0.29 ± 0.35 D | 0.19 |
| 6 weeks | 0.58 ± 0.80 D | 0.29 ± 0.34 D | 0.07 |
| 3 months | 0.50 ± 0.39 D | 0.29 ± 0.34 D | 0.03 |
There was a significant difference in the residual refractive cylinder between the two groups 3 months postoperatively (P = 0.03), but not at 1 week (P = 0.19) or 6 weeks (P = 0.07). Table 4 gives the details of the postoperative cylinder of the two groups at 1 week, 6 weeks, and 3 months. 67.74% (n = 21) and 83.33% (n = 25) eyes in groups 1 and 2, respectively, had a residual refractive cylinder of ≤0.50 D. 93.55% (n = 29) and 100% eyes in Groups 1 and 2, respectively, had a residual refractive cylinder of ≤1.00 D.
Toric IOL misalignment was similar in both the groups and was not found to be statistically significant. The Toric IOL misalignment in both the groups is given below in Table 5. The target capsulorrhexis size of 5.0 mm to 5.50 mm was achieved in all eyes. The maximum misalignment obtained was 12° in an eye in Group 2. The residual astigmatism in that eye was 0.50 D and the preoperative refractive astigmatism was 2.00D. However, the patient was happy with the refractive outcome in the postoperative period and no surgical intervention was carried out.
Table 5.
Toric IOL misalignment (in degrees) in the two groups
| Postoperative duration | Group 1 | Group 2 | P |
|---|---|---|---|
| 1 week | 4.71 ± 2.89° | 4.10 ± 2.94° | 0.41 |
| 6 weeks | 4.81 ± 3.00° | 4.03 ± 2.99° | 0.32 |
| 3 months | 4.71 ± 3.12° | 4.03 ± 2.99° | 0.39 |
6.4% (n = 2) participants in Group 1 and 6.6% (n = 2) in Group 2 had difficulty in everyday life due to visual problems postoperatively. 6.4% (n = 2) in Group 1 and none in Group 2 were dissatisfied with the postoperative visual outcome in the operated eye. 16.12% (n = 5) in Group 1 and 10% (n = 3) in Group 2 had difficulty in reading newspapers with the operated eye. None of them had difficulty in recognising faces, walking on uneven ground, or pursuing their hobbies. 12.9% (n = 4) in Group 1 and 10% (n = 3) in Group 2 had difficulty in reading prices of items while shopping, using the operated eye. 12.9% (n = 4) in Group 1 and 6.6% (n = 2) in Group 2 experienced difficulty in doing fine handwork using the operated eye. 3.2% (n = 1) in Group 1 and none in Group 2 had difficulty in reading text on the television with the operated eye.
Discussion
Toric IOL implantation provides correction of corneal astigmatism without any significant additional procedures different from routine cataract surgery. Successful outcome with Toric IOL implantation depends on various factors including IOL alignment. Factors affecting the outcome of toric IOL implantation include anterior and posterior corneal astigmatism, surgically induced astigmatism and accurate toric lens alignment along the calculated meridian.[6] Apart from the surgical technique, intraoperative IOL alignment depends on accurate preoperative marking of the horizontal axis of the eye to compensate for the cyclotorsion that occurs in the supine position on the operating table. IOL rotation in the early postoperative period may occur due to residual viscoelastic between the IOL and the posterior capsule, axial length of the eye, postoperative hypotony that destabilizes the anterior chamber, design and material of the IOL, capsular bag size and capsulorrhexis size and centring.[3] This can compromise postoperative visual outcomes for the patient and may induce higher order aberrations. Eyes with a longer axial length have a larger capsular bag size which may decrease the equatorial friction on the lens. This reduces rotational stability of the IOL.[7] High myopia is also associated with weak zonules.[3] IOL diameter also correlates with their rotational stability. IOLs with smaller diameter tend to rotate more.[2,3]
Elhofi et al.[8] did not obtain any statistically significant difference between manual marking and digital marking in terms of postoperative UDVA or CDVA. Jain et al.,[9] Elhofi et al.,[8] Trinh et al.,[10] and Mayer et al.,[11] studied Toric IOL misalignment with manual marking versus that with digital marking in eyes with significant preoperative astigmatism. In the studies by Jain et al.,[9] and Trinh et al.,[10] no significant difference was shown between the two groups. However, in the studies by Elhofi et al.,[8] and Mayer et al.,[11] significant difference was noted between the two groups with better results with digital marking. Mayer et al.,[11] also obtained favourable results with regard to mean deviation from the target induced astigmatism and mean toric IOL alignment time in the digital group.
No statistically significant difference was observed in the preoperative UDVA, BDVA or astigmatism between the two groups. We obtained a significant improvement in UDVA and BDVA in both manual and digital marking groups postoperatively. At the end of three months, 70.97% of eyes in the manual marking group and 66.67% in the digital marking group had UDVA of 20/25 or better. CDVA was 20/20 or better in 90.32% of eyes implanted with Toric IOL in both the manual and digital marking groups. 100% of eyes in the manual marking group and 96.67% (n = 29) of eyes in the digital marking group had a CDVA of 20/25 or better at the end of 3 months. The one eye in the digital marking group that did not achieve CDVA of 20/25 was noted to have mild posterior capsular opacity.
There was a significant reduction in astigmatism postoperatively in both groups. There was also a significant difference between the two groups in regard to the astigmatism at the end of 3 months postoperatively. Group 1 had significantly more residual cylinder in comparison with Group 2, though the difference was very small in magnitude. This may be attributed to a single eye in Group 1 with an axial length of 27.26 mm where Toric IOL power calculation could have been erroneous. However, the difference between the residual refractive cylinders in the two groups did not result in a significant difference in the UDVA. The mean change in UDVA per dioptre of astigmatism was found to be 0.16 logMAR in a study by Berdahl et al.[12] We did not obtain a statistically significant difference in mean IOL misalignment between the two groups.
Visser et al.,[13] obtained toric IOL misalignment of 4.9° ± 2.1° with manual marking using bubble marker and Mendez ring which is comparable to the values in this study. Elhofi et al.,[8] and Nuijts et al.,[14] compared manual marking using pendulum attached marker and Nuijts/Lane marker, Mendez ring and Nuijts toric axis marker, respectively, with digital marking using VERION and obtained significantly better toric IOL alignment in eyes which had undergone digital marking. Trinh et al.,[11] compared ZEISS Cataract Suite and traditional marking with a pendular marker and Mendez ring and also obtained better alignment with eyes marked digitally. However, we obtained similar outcomes with regard to toric IOL alignment in both the groups. Titiyal et al.,[15] also obtained significantly lesser misalignment with the Callisto eye and Z align as compared with bubble marker. IOL position was not assessed on the first postoperative day due to mild corneal edema, small air bubble in anterior chamber, and anterior chamber reaction in some patients, thus rendering it difficult. Also, other software for assessment of postoperative IOL rotation weren't used. Additionally, it was a multiple surgeon study, thus rendering some ambiguity to the results obtained.
Conclusion
In conclusion, accurate alignment by the use of manual as well as digital methods which are comparable is crucial in achieving appropriate outcomes with Toric IOL implantation. Further studies with a larger sample size and both immediate postoperative and longer term follow up are required to assess the accuracy of marking techniques and determine the long-term outcome of eyes that have undergone Toric IOL implantation guided by these techniques. Also, other software for assessment of postoperative toric IOL alignment such as computerized analysis of digitally scanned retroilluminated photographs, camera-enabled cellular phone, using episcleral vessels as reference and usage of a specially designed grid and software and anterior segment optical coherence tomography require further study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chang DF. Early rotational stability of the longer Staar toric intraocular lens: Fifty consecutive cases. J Cataract Refract Surg. 2003;29:935–40. doi: 10.1016/s0886-3350(02)01843-6. [DOI] [PubMed] [Google Scholar]
- 2.Ventura BV, Wang L, Weikert MP, Robinson SB, Koch DD. Surgical management of astigmatism with toric intraocular lenses. Arq Bras Oftalmol. 2014;77:125–31. doi: 10.5935/0004-2749.20140032. [DOI] [PubMed] [Google Scholar]
- 3.Nunez MX, Henriquez MA, Escaf LJ, Ventura BV, Srur M, Newball L, et al. Consensus on the management of astigmatism in cataract surgery. Clin Ophthalmol. 2019;13:311–24. doi: 10.2147/OPTH.S178277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skrzypecki J, Patel MS, Suh LH. Performance of the Barrett Toric calculator with and without measurements of posterior corneal curvature. Eye. 2019;33:1762–7. doi: 10.1038/s41433-019-0489-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ferreira TB, Ribeiro P, Ribeiro FJ, O'Neill JG. Comparison of methodologies using estimated or measured values of total corneal astigmatism for Toric intraocular lens power calculation. J Refract Surg. 2017;33:794–800. doi: 10.3928/1081597X-20171004-03. [DOI] [PubMed] [Google Scholar]
- 6.Shah GD, Praveen MR, Vasavada AR, Vasavada VA, Rampal G, Shastry LR. Rotational stability of a toric intraocular lens: Influence of axial length and alignment in the capsular bag. J Cataract Refract Surg. 2012;38:54–9. doi: 10.1016/j.jcrs.2011.08.028. [DOI] [PubMed] [Google Scholar]
- 7.Zhu X, He W, Zhang K, Lu Y. Factors influencing 1-year rotational stability of Acrysof toric intraocular lenses. Br J Ophthalmol. 2016;100:263–8. doi: 10.1136/bjophthalmol-2015-306656. [DOI] [PubMed] [Google Scholar]
- 8.Elhofi AH, Helaly HA. Comparison between digital and manual marking for toric intraocular lenses: A randomized trial. Medicine (Baltimore) 2015;94:e1618. doi: 10.1097/MD.0000000000001618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jain R, Aggarwal S, Dokania A. A clinical study to compare the accuracy of digital and manual marking for toric IOL alignment. Intl J Contemp Med Res. 2017;4:25–7. [Google Scholar]
- 10.Trinh L, Villette V, Dupont Monod S, Auclin F, Baudouin C. Zeiss: Astigmatism, Paris, France; 2013. Dec, [Last accessed on 2020 Jan 12]. Marker based versus markerlesstoric IOL alignment: Demonstrated benefit of an automated markerless system. Available online: https://wwwsemanticscholarorg/paper/ MARKER-BASED-VERSUS-MARKERLESS-TORIC-IOL-ALIGNMENT-Trinh-Villette/62e5402dc0499d06622bcf3b08b17eb317f02661 . [Google Scholar]
- 11.Mayer WJ, Keutzer T, Dirisamer M, Kern C, Kortuem K, Vounotrypidis E, et al. Comparison of visual outcomes, alignment accuracy, and surgical time between two methods of corneal marking for toric intraocular lens implantation. J Cataract Refract Surg. 2017;43:1281–6. doi: 10.1016/j.jcrs.2017.07.030. [DOI] [PubMed] [Google Scholar]
- 12.Berdahl JP, Hardten DR, Kramer BA, Potvin R. Effect of astigmatism on visual acuity after multifocal versus monofocal intraocular lens implantation. J Cataract Refract Surg. 2018;44:1192–7. doi: 10.1016/j.jcrs.2018.06.048. [DOI] [PubMed] [Google Scholar]
- 13.Visser N, Bauer NJ, Nuijts RM. Toric intraocular lenses: Historical overview, patient selection, IOL calculation, surgical techniques, clinical outcomes, and complications. J Cataract Refract Surg. 2013;39:624–37. doi: 10.1016/j.jcrs.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Rudy Nuijts. Netherlands: 2015. Feb, [Last accessed on 2020 Jan 27]. VERION Versus Conventional, Manual Ink marking in Toric IOL Implantation Maatricht University Medical Centre. Available online: http://clinicaltrials gov/ct2/show/NCT02370953 . [Google Scholar]
- 15.Titiyal JS, Kaur M, Jose CP, Falera R, Kinkar A, Bageshwar LMS. Comparative evaluation of toric intraocular lens alignment and visual quality with image-guided surgery and conventional three-step manual marking. Clin Ophthalmol. 2018;12:747–53. doi: 10.2147/OPTH.S164175. [DOI] [PMC free article] [PubMed] [Google Scholar]