Abstract
Purpose:
To estimate the time taken for topometric indices to stabilize in keratoconic corneas following cessation of habitual RGP contact lens wear.
Methods:
A total of 29 eyes of 20 patients, diagnosed with mild to severe keratoconus were included in this prospective observational study. All patients were experienced RGP contact lens wearers (either conventional RGP or Rose K2 lens) with each patient having used these lenses for at least a year. Corneal topography was performed immediately following discontinuation of habitual contact lens wear at baseline and each of four consecutive visits, 1-week apart.
Results:
An overall reduction in the keratometry and thickness values were noted on tomography immediately following cessation of contact lens wear and these indices increased significantly in the 1st week (P < 0.001). Consecutive visits following the first visit did not show any significant change in the topometric parameters (P > 0.05). Subgroup analysis revealed a similar trend in eyes with “severe” keratoconus and in eyes fitted with the “three-point touch” philosophy. However, eyes with “mild-moderate” keratoconus and those fitted with “apical clearance” fitting philosophy showed marginal differences even within the 1-week period of lens cessation.
Conclusion:
Maximum changes in keratometry and pachymetry values following discontinuation of RGP lens wear stabilize within the 1st week of cessation of rigid lens wear in a keratoconic cornea. These changes were more pronounced in patients with severe keratoconus and those with an apical bearing fit. This information would be useful for practitioners to assess the progression of keratoconus in RGP lens users before collagen cross-linking.
Keywords: Apical clearance, contact lens, keratoconus, three-point touch, topography
Keratoconus is a bilateral, progressive, noninflammatory, ectatic corneal degenerative condition with an adverse impact on visual quality.[1] Rigid gas permeable (RGP) lenses are the most preferred nonsurgical modality of correction as they offer maximum potential vision correction by masking the irregular anterior corneal surface.[2] During the disease, the role of RGP lenses become more and more important as patients often become more reliant on these lenses.[3] It has also been reported that RGP contact lens wear has a greater impact on the cornea topometry indices than conventional soft contact lenses.[4] Typically, the cornea regains its shape following a period of contact lens wear, but instances of long-term changes in corneal topography have been reported particularly with polymethyl methacrylate (PMMA) and RGP lenses.[5]
In addition to visual correction with RGP lenses in patients with keratoconus, they require close follow-up to assess disease progression.[6,7] Progression of keratoconus is classically diagnosed by identifying increased steepening of the corneal curvature on corneal topography and reduced central corneal thickness,[7] resulting in a need for collagen cross-linking to arrest the progression.[8] Identification of progression is critical inmaking a decision to crosslink a patient as not all eyes are progressive.[9,10,11,12,13] Currently, collagen cross-linking has become popular as it is minimally invasive and is the only proven method to stop progression, as long as the cornea has adequate thickness. Collagen cross-linking also has an important role in avoiding the need for future corneal transplantation.[14,15,16,17]
During follow-up visits, keratoconus patients typically undergo corneal topography to assess the stability of keratoconus as well as the fitting of contact lenses. Accurate interpretation of corneal topography parameters, however, remains unclear in RGP contact lens wearers due to the impact of lens wear on corneal topography parameters. Hence, a certain duration of abstinence from lens wear is desirable before assessment indices of corneal topography. Since there is no published evidence about the time taken for a keratoconic cornea to regain its original curvature following cessation of habitual contact lens wear, this study will attempt to answer this specific question.
Methods
The study protocol was approved by the Scientific and Ethics Committee of the Institutional Review Board. In this prospective study, 29 eyes of 20 patients diagnosed with mild to severe keratoconus were included for evaluation. All participants were previously diagnosed keratoconus patients and habitually wore RGP contact lenses. Keratoconus was diagnosed by clinical findings such as scissor's reflex on retinoscopy, stromal corneal thinning, corneal ectasia, Vogt's striae, and Fleischer's ring along with topographic changes such as increased keratometric value, increased corneal irregularity, an asymmetric bow-tie pattern on the keratometric map, or significant thinning in the central corneal pachymetry map. All participants were experienced RGP contact lens wearers with a minimum experience of at least a year before inclusion and an average wearing time of at least 8 h per day.
Subjects were wearing either one of two different types of contact lenses, conventional RGP contact lenses or Rose K2 lenses which were chosen based on suitability and fitting. Conventional RGP contact lenses (CLASSIC Company, Bangalore, India) are tri-curve lenses with two additional peripheral curves with one central base curve. They are made of Fluoroperm-90 with a DK value of 90 (cm/s) ([mL O2/mL. mmHg].10-11). Rose K2 lenses (Menicon Co., Ltd; Japan) are multicurve contact lenses that usually possess a central aspheric optic zone which mimics the cone shape of keratoconus and has multiple peripheral curves which flatten progressively from the center of the lens to the periphery. The material of these lenses is Hexafocon A (Fluoro Silicone Acrylate) and the DK value is 100 (cm/s) ([mL O2/mL. mmHg].10-11). Eyes with apical scarring, subjects with lens wearing experience of less than a year and average wear time of fewer than 8 h per day, and eyes that had undergone any form of ocular surgery were excluded from the study. Signed informed consent was collected from subjects who voluntarily expressed their interest in participating in the study.
Slit-lamp biomicroscopy (Carl Zeiss, Germany) was conducted to assess the fitting of the subject's habitual contact lenses. Sodium fluorescein was used to check the lens-cornea relationship. Patients were divided into two groups based on lens fitting characteristics – “apical clearance” or “three-point touch.” Lens fitting that resulted in a clear space between the lens and the cornea filled by fluorescein with a fine layer of fluorescein at the mid-periphery of the lens were graded as “apical clearance [Fig. 1].” Lens fitting that resulted in a mild touch in the center of the cornea with minimal touch in the mid-peripheral zone identified by a “no-fluorescein zone” were graded as “three-point touch [Fig. 2].” In the “apical clearance” group, the mid-peripheral region was examined more carefully to avoid a heavy bearing in that zone. In the “three-point touch” technique, more emphasis was given to keeping the central bearing of the contact lens as minimal as possible.
Figure 1.
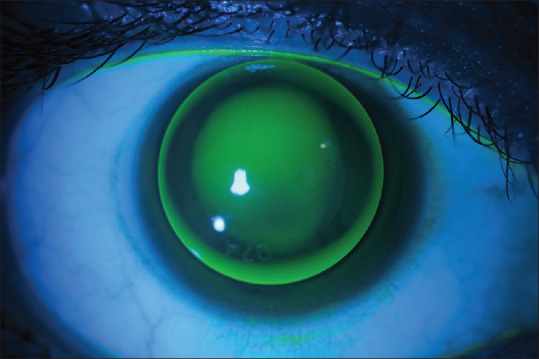
Shows a representative clinical image of a contact lens fitting with the “Apical clearance” philosophy. This was typically characterized by clear space between the lens and the cornea at the center, marked by pooling of fluorescein
Figure 2.
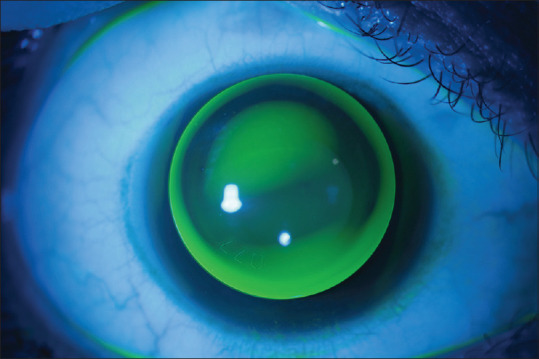
Shows a representative clinical image of a contact lens fitting with a “Three-point touch” philosophy. This was typically characterized by mild touch between the lens and the cornea at the center, marked by a space with a “no-fluorescein zone” at the apex
The Orbscan IIz (Bausch & Lomb, Rochester, NY) topographer was used for corneal topography. This instrument works on a combined Placido-disc and slit-scanning technology with an infrared light source as a target and measures the cornea by scanning more than 9,000 data points within 1.5 s with an added advantage of measuring the elevation and curvature indices from both the anterior and posterior surfaces of the cornea. Scans were acquired in Zyoptix mode and the severity of keratoconus was graded as: moderate (mean keratometry value 45D–52D) or severe (mean keratometry value >52D) according to the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) study group's criteria.[18]
At the baseline visit, subjects were requested to visit the clinic with their habitual lenses on. A routine examination was performed with the lenses in place and the type of lens fitting was noted by a single experienced practitioner. The lenses were then removed from the eyes and corneal topography was performed within 5 min of removal to retain the maximum molding effect of the contact lens on the cornea. The practitioner who assessed contact lens fitting was masked to the corneal topography assessment. Topographic indices such as simulated keratometry (Sim K) astigmatism, maximum and minimum keratometry (Max and Min K) values, mean power at the central 3 mm and 5 mm zones, thinnest pachymetry, and anterior chamber depth were recorded. Patients were advised to discontinue their habitual lenses and were advised to continue spectacle wear. Patients were reviewed in the clinic weekly for the next 3 weeks and underwent corneal topography and the same topographic indices were measured at every visit.
The Shapiro-Wilk normality test was used to examine the distribution of the data. All statistical analyses were performed using the “R” software (version 2.12). The mean difference between the consecutive scans of the corneal topography was compared by multiple comparisons of means from a mixed-effect model; an adjusted P value was obtained by the Bonferroni method. A P value of ≤ 0.05 was considered as being statistically significant to compare the two groups.
Results
Corneal topographic maps of 29 eyes from 20 keratoconus patients were analyzed; 10 were male. Depending on the two different fitting philosophies, 23 out of the 29 eyes (79.3%) were fitted with the “three-point touch” technique, and 6 out of 29 eyes (20.7%) were fitted with the “apical clearance” technique. The mean period of habitual contact lens wear before the assessment was 3.3 years. The demographic distribution and topographic representation at the baseline visit for the overall population and different subgroups were analyzed [Table 1]. Eighteen out of 29 eyes had mild to moderate keratoconus (Mean K value 45D–52D) and 11 out of 29 eyes had severe keratoconus (Mean K value >52D); 22 eyes were fitted with conventional RGP contact lenses while the rest were fitted with Rose K2 contact lenses.
Table 1.
Distribution of the variables in the overall population and the two subgroups: “Three-point touch” and “Apical clearance.” P value indicates the significance level of the comparison between the two subgroups
| Overall (n=29) | “Three-point touch” group (n=23) | “Apical clearance” group (n=6) | P | |
|---|---|---|---|---|
| Age (years), Mean±SD | 21.71±5.26 | 20.45±4.73 | 26.33±4.76 | 0.01* |
| Max K (D), Mean±SD | 54.33±6.01 | 56.16±5.38 | 47.35±1.1 | <0.001* |
| Min K (D), Mean±SD | 48.29±4.02 | 49.39±3.8 | 44.07±0.5 | <0.001* |
| Sim K astigmatism (D), Mean±SD | -5.67±4.3 | -6.29±4.6 | -3.28±1.3 | 0.02* |
| Mean power 3 mm (D), Mean±SD | 49.73±4.07 | 50.78±3.9 | 45.73±0.64 | 0.01* |
| Mean power 5 mm (D), Mean±SD | 46.97±2.6 | 47.43±2.7 | 45.18±1.08 | 0.6 |
| Thinnest pachymetry (µm), Mean±SD | 391.28±46.2 | 380.87±42.9 | 431.17±37.2 | 0.01* |
| Duration of lens wear (years), Mean±SD | 3.3±2.4 | 3.08±2.24 | 4.1±2.62 | 0.74 |
The *sign on the P value indicates a statistically significant difference between the subgroups
Table 2 shows the difference in the mean values of all the variables at each visit in the overall population and the two subgroups (based on lens fitting philosophy). The negative sign in the mean difference indicates a decrease in the mean values of a particular index in the topographic map and a positive sign indicates an increase. In the” three-point touch” cohort, the max K, min K, sim K astigmatism, and mean power at the central 3 mm showed a significant difference between baseline and the first consecutive scan (P < 0.05). Among the keratometry values, max K values showed the maximum changes within this period (2.13 D, P < 0.001). The thinnest pachymetry and anterior chamber depth showed a marginally significant difference between the baseline and the first consecutive scan (9.3 μ and 0.03 mm, respectively, P = 0.04). However, the subsequent scans did not show any significant differences between them (P > 0.05). Mean power in the central 5 mm zone did not show any significant changes between any of the consecutive topographies. In the “apical clearance” cohort, only sim K astigmatism (0.83 D, P < 0.001) and min K value (-0.62 D, P = 0.008) showed a significant difference between the baseline and first consecutive scan. The rest of the variables did not show any significant differences between the visits (P > 0.05). Interestingly, all the significant changes in the topography were restricted to the 1st week of contact lens discontinuation across the groups. Fig. 3 shows the changes in the maximum and minimum keratometric values in both the primary subgroups across visits. Fig. 4 shows corneal topography at various timelines following contact lens removal in a representative patient.
Table 2.
Descriptive report and mean the difference between consecutive scans in the overall population and the two subgroups: “Three-point touch” and “Apical clearance” with a P
| Overall population (n=29) | Three-point touch (n=23) | Apical Clearance (n=6) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scan | Mean±SD | Mean Difference | P | Scan | Mean±SD | Mean Difference | P | Scan | Mean±SD | Mean Difference | P | ||||
| Max K (D) | Baseline | 53.38±5.71 | Baseline | 54.97±5.33 | Baseline | 47.3±1.15 | |||||||||
| 1st week | 55.11±6.45 | 1st week-BL | 1.72 | <0.001* | 1st week | 57.09±5.7 | 1st week-BL | 2.13 | <0.001* | 1st week | 47.5±1.47 | 1st week-BL | 0.2 | 0.72 | |
| 2nd week | 55.03±6.49 | 2nd week-1st week | -0.07 | 1 | 2nd week | 57.08±5.66 | 2nd week-1st week | -0.02 | 1 | 2nd week | 47.18±1.44 | 2nd week-1st week | -0.32 | 0.19 | |
| 3rd week | 55.12±6.48 | 3rd week-2nd week | 0.09 | 1 | 3rd week | 57.19±5.62 | 3rd week-2nd week | 0.11 | 1 | 3rd week | 47.22±1.23 | 3rd week-2nd week | 0.03 | 1 | |
| Min K (D) | Baseline | 48.06±3.88 | Mean Difference | P | Baseline | 48.99±3.84 | Mean Difference | P | Baseline | 44.48±0.41 | Mean Difference | P | |||
| 1st week | 48.73±4.65 | 1st week-BL | 0.7 | <0.001* | 1st week | 50±4.4 | 1st week-BL | 1.01 | <0.001* | 1st week | 43.87±0.28 | 1st week-BL | -0.62 | 0.008* | |
| 2nd week | 48.55±4.33 | 2nd week-1st week | -0.17 | 0.9 | 2nd week | 49.8±3.99 | 2nd week-1st week | -0.21 | 0.84 | 2nd week | 43.78±0.66 | 2nd week-1st week | -0.08 | 1 | |
| 3rd week | 48.59±4.37 | 3rd week-2nd week | 0.04 | 1 | 3rd week | 49.83±4.06 | 3rd week-2nd week | 0.04 | 1 | 3rd week | 43.85±0.53 | 3rd week-2nd week | 0.07 | 1 | |
| Sim K Astigmatism (D) | Baseline | 5.32±3.53 | Mean Difference | P | Baseline | 5.98±3.64 | Mean Difference | P | Baseline | 2.8±1.31 | Mean Difference | P | |||
| 1st week | 6.39±3.72 | 1st week-BL | 1.06 | <0.001* | 1st week | 7.11±3.81 | 1st week-BL | 1.13 | <0.001* | 1st week | 3.63±1.47 | 1st week-BL | 0.83 | <0.001* | |
| 2nd week | 6.4±3.68 | 2nd week-1st week | 0.01 | 1 | 2nd week | 7.18±3.71 | 2nd week-1st week | 0.07 | 1 | 2nd week | 3.42±1.36 | 2nd week-1st week | -0.22 | 0.16 | |
| 3rd week | 6.53±3.62 | 3rd week-2nd week | 0.13 | 0.9 | 3rd week | 7.36±3.59 | 3rd week-2nd week | 0.18 | 0.74 | 3rd week | 3.38±1.4 | 3rd week-2nd week | -0.03 | 1 | |
| Mean Power 3 mm (D) | Baseline | 49.44±3.73 | Mean Difference | P | Baseline | 50.37±3.64 | Mean Difference | P | Baseline | 45.9±0.77 | Mean Difference | P | |||
| 1st week | 50.08±4.15 | 1st week-BL | 0.63 | <0.001* | 1st week | 51.2±3.93 | 1st week-BL | 0.83 | <0.001* | 1st week | 45.8±0.86 | 1st week-BL | -0.1 | 1 | |
| 2nd week | 49.99±4.03 | 2nd week-1st week | -0.08 | 1 | 2nd week | 51.13±3.73 | 2nd week-1st week | -0.07 | 1 | 2nd week | 45.63±0.92 | 2nd week-1st week | -0.17 | 0.7 | |
| 3rd week | 50.13±4.15 | 3rd week-2nd week | 0.13 | 0.7 | 3rd week | 51.29±3.87 | 3rd week-2nd week | 0.16 | 0.59 | 3rd week | 45.68±0.85 | 3rd week-2nd week | 0.05 | 1 | |
| Mean Power 5 mm (D) | Baseline | 46.93±2.48 | Mean Difference | P | Baseline | 47.4±2.54 | Mean Difference | P | Baseline | 45.13±1.08 | Mean Difference | P | |||
| 1st week | 47.03±2.58 | 1st week-BL | 0.09 | 0.4 | 1st week | 47.52±2.64 | 1st week-BL | 0.12 | 0.35 | 1st week | 45.15±1.11 | 1st week-BL | 0.02 | 1 | |
| 2nd week | 47±2.56 | 2nd week-1st week | -0.02 | 1 | 2nd week | 47.5±2.61 | 2nd week-1st week | -0.02 | 1 | 2nd week | 45.08±1.1 | 2nd week-1st week | -0.07 | 1 | |
| 3rd week | 47±2.6 | 3rd week-2nd week | -0.01 | 1 | 3rd week | 47.49±2.66 | 3rd week-2nd week | -0.02 | 1 | 3rd week | 45.1±1.15 | 3rd week-2nd week | 0.02 | 1 | |
| Thinnest Pachymetry (µm) | Baseline | 380.86±52.4 | Mean Difference | P | Baseline | 369.7±50.1 | Mean Difference | P | Baseline | 423.5±39.8 | Mean Difference | P | |||
| 1st week | 388.07±41.8 | 1st week-BL | 7.2 | 0.06 | 1st week | 379.1±38.2 | 1st week-BL | 9.3 | 0.04* | 1st week | 422.5±39.4 | 1st week-BL | -1 | 1 | |
| 2nd week | 389.93±46.1 | 2nd week-1st week | 1.86 | 0.34 | 2nd week | 379.1±42.4 | 2nd week-1st week | <0.001 | 1 | 2nd week | 431.5±37.2 | 2nd week-1st week | 9 | 0.17 | |
| 3rd week | 389.59±44.9 | 3rd week-2nd week | -0.34 | 1 | 3rd week | 378.6±41.4 | 3rd week-2nd week | <0.001 | 1 | 3rd week | 431.8±33.1 | 3rd week-2nd week | 0.33 | 1 | |
| Anterior chamber depth (mm) | Baseline | 3.29±0.34 | Mean Difference | P | Baseline | 3.3±0.36 | Mean Difference | P | Baseline | 3.23±0.26 | Mean Difference | P | |||
| 1st week | 3.31±0.33 | 1st week-BL | 0.02 | 0.01* | 1st week | 3.33±0.35 | 1st week-BL | 0.03 | 0.04* | 1st week | 3.23±0.25 | 1st week-BL | -0.01 | 1 | |
| 2nd week | 3.29±0.34 | 2nd week-1st week | -0.01 | 0.07 | 2nd week | 3.31±0.36 | 2nd week-1st week | -0.02 | 0.175 | 2nd week | 3.21±0.27 | 2nd week-1st week | -0.02 | 0.2 | |
| 3rd week | 3.3±0.34 | 3rd week-2nd week | 0.01 | 0.62 | 3rd week | 3.32±0.36 | 3rd week-2nd week | 0.01 | 0.674 | 3rd week | 3.21±0.25 | 3rd week-2nd week | 0.01 | 1 | |
Note: The *sign on the P indicates a statistically significant difference between the scans
Figure 3.
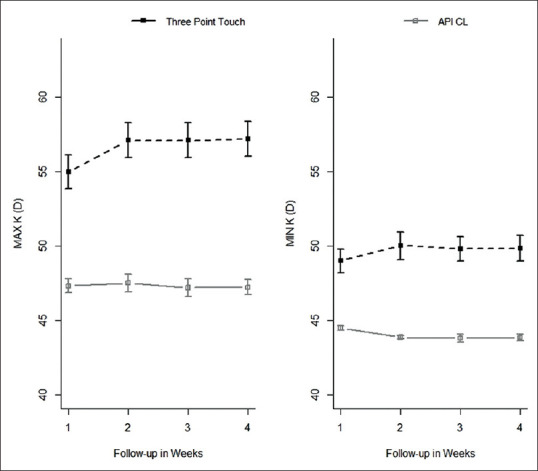
Shows the changes in the maximum and minimum simulated keratometry values in “Three-point touch” and “Apical clearance” groups across the visits
Figure 4.
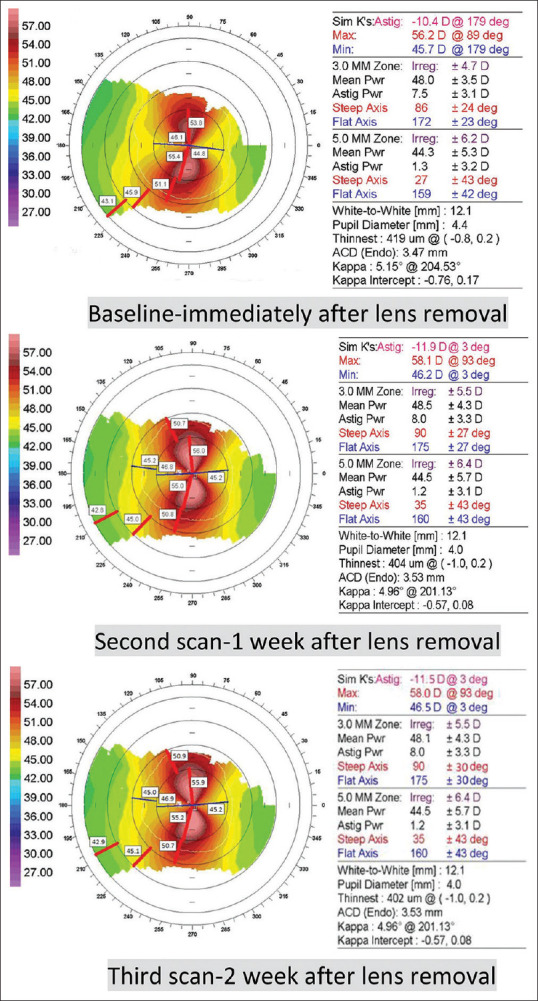
Shows documentation of serial topographic images from the representative subject pool. The uppermost panel shows the scan taken at baseline (immediately after removal of a contact lens); followed by the scans that were taken after 1 week (middle panel) and 2 weeks (lower panel) of lens removal
A similar comparison was carried out for all the variables in the two subgroups divided based on the severity of keratoconus, “mild-moderate” keratoconus versus “severe” keratoconus [Table 3]. Only sim K astigmatism values (0.74 D, P < 0.001) and the max K values (0.59 D, P = 0.03) showed a statistically significant difference from the baseline to that of the first visit in “mild-moderate” keratoconus. In contrast, the “severe” keratoconus cohort showed a statistically significant difference within the first consecutive scans for all parameters except for the anterior chamber depth. Differences in all the variables beyond the 1st week of discontinuation of lenses were insignificant across the groups.
Table 3.
escriptive report and mean the difference between consecutive scans in the two subgroups: “Mild-moderate” and “Severe” keratoconus along with P
| “Mild-moderate” KC (n=18) | “Severe” KC (n=11) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Scan | Mean±SD | Mean Difference | P | Scan | Mean±SD | Mean Difference | P | |||
| Max K (D) | Baseline | 48.16±1.91 | Baseline | 56.57±4.81 | ||||||
| 1st week | 48.75±2.37 | 1st week-BL | 0.59 | 0.03* | 1st week | 58.99±4.8 | 1st week-BL | 2.42 | <0.001* | |
| 2nd week | 48.59±2.52 | 2nd week-1st week | -0.16 | 1 | 2nd week | 58.97±4.74 | 2nd week-1st week | -0.02 | 1 | |
| 3rd week | 48.59±2.4 | 3rd week-2nd week | <0.001 | 1 | 3rd week | 59.12±4.61 | 3rd week-2nd week | 0.15 | 1 | |
| Min K (D) | Baseline | 44.84±1.12 | Mean Difference | P | Baseline | 50.03±3.63 | Mean Difference | P | ||
| 1st week | 44.68±1.5 | 1st week-BL | -0.15 | 1 | 1st week | 51.21±4.15 | 1st week-BL | 1.18 | <0.001* | |
| 2nd week | 44.64±1.58 | 2nd week-1st week | -0.05 | 1 | 2nd week | 50.94±3.66 | 2nd week-1st week | -0.26 | 0.78 | |
| 3rd week | 44.68±1.52 | 3rd week-2nd week | 0.05 | 1 | 3rd week | 50.98±3.76 | 3rd week-2nd week | 0.04 | 1 | |
| Sim K Astigmatism (D) | Baseline | 3.33±1.47 | Mean Difference | P | Baseline | 6.54±3.88 | Mean Difference | P | ||
| 1st week | 4.06±1.53 | 1st week-BL | 0.74 | <0.001* | 1st week | 7.81±3.97 | 1st week-BL | 1.27 | <0.001* | |
| 2nd week | 3.94±1.52 | 2nd week-1st week | -0.13 | 0.67 | 2nd week | 7.91±3.83 | 2nd week-1st week | 0.09 | 1 | |
| 3rd week | 3.92±1.56 | 3rd week-2nd week | -0.02 | 1 | 3rd week | 8.13±3.62 | 3rd week-2nd week | 0.23 | 0.62 | |
| Mean Power 3 mm (D) | Baseline | 46.16±1.35 | Mean Difference | P | Baseline | 51.45±3.26 | Mean Difference | P | ||
| 1st week | 46.27±1.45 | 1st week-BL | 0.11 | 1 | 1st week | 52.41±3.46 | 1st week-BL | 0.96 | <0.001* | |
| 2nd week | 46.2±1.46 | 2nd week-1st week | -0.07 | 1 | 2nd week | 52.31±3.23 | 2nd week-1st week | -0.09 | 1 | |
| 3rd week | 46.25±1.38 | 3rd week-2nd week | 0.05 | 1 | 3rd week | 52.5±3.41 | 3rd week-2nd week | 0.19 | 0.54 | |
| Mean Power 5 mm (D) | Baseline | 45.01±1.28 | Mean Difference | P | Baseline | 48.11±2.3 | Mean Difference | P | ||
| 1st week | 45±1.25 | 1st week-BL | -0.01 | 1 | 1st week | 48.27±2.4 | 1st week-BL | 0.16 | 0.23 | |
| 2nd week | 44.95±1.24 | 2nd week-1st week | -0.05 | 1 | 2nd week | 48.26±2.34 | 2nd week-1st week | -0.01 | 1 | |
| 3rd week | 44.96±1.28 | 3rd week-2nd week | 0.02 | 1 | 3rd week | 48.24±2.42 | 3rd week-2nd week | -0.02 | 1 | |
| Thinnest Pachymetry (µm) | Baseline | 426.1±35.3 | Mean Difference | P | Baseline | 353.2±40.7 | Mean Difference | P | ||
| 1st week | 422.9±32.3 | 1st week-BL | -3.18 | 1 | 1st week | 366.8±31.5 | 1st week-BL | 13.56 | 0.004* | |
| 2nd week | 429±33.02 | 2nd week-1st week | 6.09 | 0.34 | 2nd week | 366.1±35.6 | 2nd week-1st week | -0.72 | 1 | |
| 3rd week | 430.1±28.5 | 3rd week-2nd week | 1.09 | 1 | 3rd week | 364.8±33.8 | 3rd week-2nd week | -1.22 | 1 | |
| Anterior chamber depth (mm) | Baseline | 3.17±0.28 | Mean Difference | P | Baseline | 3.36±0.35 | Mean Difference | P | ||
| 1st week | 3.19±0.26 | 1st week-BL | 0.02 | 0.14 | 1st week | 3.38±0.36 | 1st week-BL | 0.02 | 0.09 | |
| 2nd week | 3.15±0.28 | 2nd week-1st week | -0.03 | 0.008 | 2nd week | 3.37±0.35 | 2nd week-1st week | -0.01 | 1 | |
| 3rd week | 3.17±0.27 | 3rd week-2nd week | 0.01 | 0.62 | 3rd week | 3.38±0.35 | 3rd week-2nd week | 0.01 | 1 | |
Note: The * sign on the P indicates a statistically significant difference between the scans
Discussion
This study reports the effect of the RGP contact lens on corneal topography and estimates the minimum duration required for discontinuation of lenses to achieve a reliable and repeatable corneal topography in patients with keratoconus. Recommendations from previous reports suggest discontinuation of RGP lenses in normal patients before refractive surgery for 2 weeks at the very least to achieve a stable topography,[19,20,21] There is no previous report of the time required for corneas to regain their native topography values in the eyes with keratoconus. In our practice, emphasis on achieving a “three-point touch” fitting philosophy was apparent from the fewer number of eyes that fitted with the other philosophy. The group of eyes fitted with the “three-point touch” philosophy resembled the characteristics of those with “severe” keratoconus. In comparison, the group fitted with the “apical clearance” philosophy revealed characteristics of “mild-moderate” keratoconus [Table 1]. This is understandable as apical bearing lenses become unavoidable as the condition progresses.[22]
A case study report by Jinabhai and colleagues had followed the changes in refraction, topography, and ocular aberrations in a case of early pellucid marginal corneal degeneration and moderate keratoconus for 1 week. The changes in all the parameters appeared insignificant during this period in both cases.[23] Subsequently, another report from the same group revealed significant changes in ocular parameters in a group of 15 patients with moderate to severe keratoconus after suspending their habitual contact lenses for 7 days.[24] While the primary aim of looking at the changes in corneal parameters could be established, longer duration changes were not apparent. In the present study, all topometric values showed a significant change within the 1st week of cessation of the RGP contact lens. Interestingly, the rest of the consecutive scans did not reveal any statistical as well as clinically significant variation in these parameters. The trend was similar in both of the subgroups divided based on fitting philosophy, i.e., in the “three-point touch” or in the “apical clearance” cohort [Table 2].
Analyzing subgroups based on the severity of keratoconus, all parameters except the anterior chamber depth in the “severe” keratoconus group showed a clear increase from the baseline scan to that of the scans on the 1st-week visit, while those with “mild-moderate” keratoconus only showed a marginal increase during the same time in max K values and sim K astigmatism values. No significant difference was found in the other parameters. Also interesting was the course of the changes in these parameters over the subsequent visits in each of the groups which appeared to follow the same trend as the previous subgroups. While a greater impact was expected in cases of severe keratoconus, as greater ectasia would result in a larger area of contact with the lens at the apex, the insignificant change in the subsequent visits appeared to be of greater interest for the clinicians.
A recent study by Romero-Jimenez and colleagues has compared the short-term impact of RGP contact lenses on the cornea where the two different fitting techniques have been described as “apical touch” and “three-point touch.” While in our study, a marked flattening of the keratometric parameters was seen in the “three-point touch” group immediately after cessation of contact lens, no such changes were to be seen in the aforementioned study.[25] This could be simply because experienced contact lens wearers were considered for the present study and an increased impact could be expected than in a short-term lens user. While the numbers in our study are small, this is mainly due to the difficulty we encountered in asking contact lens wearers to discontinue their lenses and go back to wearing glasses for a significant duration of time during the study period. Besides, corneas with apical corneal scars and a previous episode of hydrops were excluded from the measurements due to questionable repeatability with a Placido disc-based topographer. This too had an impact on limiting the sample size for this report. Besides, the conclusion drawn from the subgroup analysis over a smaller sample size warrants further validation and could be a potential subject for future research work.
As corneal topography is currently used as the most common method for assessing the progression of keratoconus, it is essential to obtain reliable and repeatable measurements on follow-up visits. Keratoconus patients might find it challenging to perform daily activities without their habitual contact lenses and practitioners need to be sensitive about asking for a significant duration of discontinuation of contact lens wear. Besides, the ability to determine progression, necessitating a surgical intervention such as collagen cross-linking becomes even more important in eyes with mild to moderate keratoconus where adequate corneal thickness allows for the procedure. Hence, it is fundamentally important to be able to recognize a change in corneal topography indices independent of the effect of the contact lens wear in this subgroup of patients.
Conclusion
From our results, it appears that an eye with mild to moderate keratoconus or an eye wearing RGP contact lenses with an “apical clearance” fitting philosophy could be reviewed in the clinic within a week of discontinuation of their habitual lenses. In contrast, an eye with advanced keratoconus or wearing RGP lenses following the “three-point touch” philosophy could be called back to the clinic at least after a week of discontinuation of their habitual contact lenses. This might provide for more reliable and repeatable topography measurements and a more accurate estimation of progression in these patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Krachmer JH, Feder RS, Belin MW. Keratoconus and related non-inflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28:293–322. doi: 10.1016/0039-6257(84)90094-8. [DOI] [PubMed] [Google Scholar]
- 2.Zhou AJ, Kitamura K, Weissman BA. Contact lens care in keratoconus. Cont Lens Anterior Eye. 2003;26:171–4. doi: 10.1016/S1367-0484(03)00042-0. [DOI] [PubMed] [Google Scholar]
- 3.Cesneková T, Skorkovská K, Petrová S, Cermáková S. Visual functions and quality of life in patients with keratoconus. Cesk Slov Oftalmol. 2011;67:51–4. [PubMed] [Google Scholar]
- 4.Lin MC, Yeh TN, Graham AD, Truong T, Hsiao C, Wei G, et al. Ocular surface health during 30-day continuous wear: Rigid gas-permeable versus silicone hydrogel hyper-O2 transmitted contact lenses. Invest Ophthalmol Vis Sci. 2011;52:3530–8. doi: 10.1167/iovs.10-6025. [DOI] [PubMed] [Google Scholar]
- 5.Wilson SE, Lin DT, Klyce SD, Reidy JJ, Insler MS. Topographic changes in contact lens-induced corneal warpage. Ophthalmology. 1990;97:734–44. doi: 10.1016/s0161-6420(90)32516-2. [DOI] [PubMed] [Google Scholar]
- 6.Kanellopoulos AJ, Asimellis G. Revisiting keratoconus diagnosis and progression classification based on evaluation of corneal asymmetry indices, derived from Scheimpflug imaging in keratoconic and suspect cases. Clin Ophthalmol. 2013;7:1539–48. doi: 10.2147/OPTH.S44741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi JA, Kim MS. Progression of keratoconus by longitudinal assessment with corneal topography. Invest Ophthalmol Vis Sci. 2012;53:927–35. doi: 10.1167/iovs.11-8118. [DOI] [PubMed] [Google Scholar]
- 8.Sharif KW, Casey TA. Penetrating keratoplasty for keratoconus: Complications and long-term success. Br J Ophthalmol. 1991;75:142–6. doi: 10.1136/bjo.75.3.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620–7. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 10.Brown SE, Simmasalam R, Antonova N, Gadaria N, Asbell PA. Progression in keratoconus and the effect of corneal cross-linking on progression. Eye Contact Lens. 2014;40:331–8. doi: 10.1097/ICL.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 11.Ganesh S, Shetty R, D'Souza S, Ramachandran S, Kurian M. Intra-stromal corneal ring segments for management of keratoconus. Indian J Ophthalmol. 2013;61:451–5. doi: 10.4103/0301-4738.116065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coskunseven E, Jankov MR, 2nd, Grentzelos MA, Plaka AD, Limnopoulou AN, Kymionis GD. Topography-guided Trans epithelial PRK after intra corneal ring segments implantation and corneal collagen CXL in a three-step procedure for keratoconus. J Refract Surg. 2013;29:54–8. doi: 10.3928/1081597X-20121217-01. [DOI] [PubMed] [Google Scholar]
- 13.Kymionis GD, Grentzelos MA, Kounis GA, Diakonis VF, Limnopoulou AN, Panagopoulou SI. Combined Trans epithelial phototherapeutic keratectomy and corneal collagen cross-linking for progressive keratoconus. Ophthalmology. 2012;119:1777–84. doi: 10.1016/j.ophtha.2012.03.038. [DOI] [PubMed] [Google Scholar]
- 14.Spoerl E, Mrochen M, Sliney D, Trokel S, Seiler T. Safety of UVA-riboflavin cross-linking of the cornea. Cornea. 2007;26:385–9. doi: 10.1097/ICO.0b013e3180334f78. [DOI] [PubMed] [Google Scholar]
- 15.Caporossi A, Mazzotta C, Baiocchi S, Caporossi T. Long-term results of riboflavin ultraviolet a corneal collagen cross-linking for keratoconus in Italy: The Siena eye-cross study. Am J Ophthalmol. 2010;149:585–93. doi: 10.1016/j.ajo.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 16.Lam FC, Georgoudis P, Nanavaty MA, Khan S, Lake D. Sterile keratitis after combined riboflavin-UVA corneal collagen cross-linking for keratoconus. Eye (Lond) 2014;28:1297–303. doi: 10.1038/eye.2014.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gumus K. Acute idiopathic endothelitis early after corneal cross-linking with riboflavin and Ultraviolet-A. Cornea. 2014;33:630–3. doi: 10.1097/ICO.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 18.Zadnik K, Barr JT, Gordon MO, Edrington TB. Bio microscopic signs and disease severity in keratoconus. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study Group. Cornea. 1996;15:139–46. doi: 10.1097/00003226-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Budak K, Hamed AM, Friedman NJ, Koch DD. Pre-operative screening of contact lens wearers before refractive surgery. J Cataract Refract Surg. 1999;25:1080–6. doi: 10.1016/s0886-3350(99)00122-4. [DOI] [PubMed] [Google Scholar]
- 20.Wang X, McCulley JP, Bowman RW, Cavanagh HD. Time to resolution of contact lens-induced corneal warpage prior to refractive surgery. CLAO J. 2002;28:169–71. doi: 10.1097/01.ICL.0000018042.02034.AB. [DOI] [PubMed] [Google Scholar]
- 21.Tsai PS, Dowidar A, Naseri A, McLeod SD. Predicting time to refractive stability after discontinuation of rigid contact lens wear before refractive surgery. J Cataract Refract Surg. 2004;30:2290–4. doi: 10.1016/j.jcrs.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 22.Edrington TB, Szczotka LB, Barr JT, Achtenberg JF, Burger DS, Janoff AM, et al. Rigid contact lens fitting relationships in keratoconus. Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study Group. Optom Vis Sci. 1999;76:692–9. [PubMed] [Google Scholar]
- 23.Jinabhai A, Radhakrishnan H, O'Donnell C. Corneal changes after suspending contact lens wears in early pellucid marginal corneal degeneration and moderate keratoconus. Eye Contact Lens. 2011;37:99–105. doi: 10.1097/ICL.0b013e31820592b1. [DOI] [PubMed] [Google Scholar]
- 24.Jinabhai A, O'Donnell C, Radhakrishnan H. Changes in refraction, ocular aberrations, and corneal structure after suspending rigid gas-permeable contact lens wear in keratoconus. Cornea. 2012;31:500–8. doi: 10.1097/ICO.0b013e31820f777b. [DOI] [PubMed] [Google Scholar]
- 25.Romero-Jiménez M, Santodomingo-Rubido J, Flores-Rodríguez P, González-Méijome JM. Short-term corneal changes with gas-permeable contact lens wear in keratoconus subjects: A comparison of two fitting approaches. J Optom. 2015;8:48–55. doi: 10.1016/j.optom.2014.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


