Abstract
PresbyLASIK is one of the most commonly used modalities of surgical correction in presbyopes with no cataract. Unlike monovision procedures, both the eyes are adjusted for near and distance, providing a good stereopsis. This works by creating a corneal multifocality and increasing the depth of focus. Most techniques of presbyLASIK currently employ hybrid methods, i.e., a component of monovision added on to a multifocal corneal ablation. Choosing an appropriate proportion of these two components according to the patients' requirements and meticulous patient selection are key to obtaining desirable outcomes. Being corneal-based procedures, presbyLASIK has shown to be reversible. Thorough updated knowledge of the different presbyLASIK procedures, their principles and outcomes based on previous studies is required before a refractive surgeon plans to start providing presbyLASIK services. We performed a comprehensive search on PubMed with the keywords “Presbyopia surgery,” “PresbyLASIK” “PresbyMAX,” “Supracor,” and “Custom-Q.” In this review article, we have explained the principles of the various presbyLASIK procedures, appropriate patient selection and planning on the devices with examples, and summarized the previously published outcomes of these techniques.
Keywords: Laser blended vision, PresbyLASIK, PresbyMAX, Supracor
Presbyopia, an age-related condition due to the diminishing accommodative power of the lens, is a growing problem across the world. When untreated, it affects productivity and performance significantly.[1] By 2020, 1.37 billion people are estimated to be affected by this condition globally.[2] While spectacles have been the most common form of treatment, with advancement in technology and availability of surgical options, there is a growing demand for the treatment of presbyopia with spectacle independence. 'PresbyLASIK', as commonly known, is gaining popularity among patients and refractive surgeons as a refractive surgical option for presbyopia. We performed a comprehensive search on PUBMED with the keywords 'Presbyopia surgery', 'PresbyLASIK', 'PresbyMAX', 'Supracor', and 'Custom-Q'. We have explained the principles, patient selection, planning, and published outcomes of PresbyMAX, Supracor, Presbyond, and Custom-Q methods of presbyLASIK along with examples from our practice.
I. Approaches to management
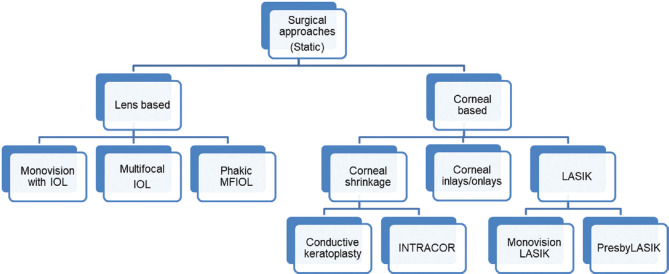
Presbyopia can be addressed either by static or dynamic approaches and are predominantly based on cornea or lens. Dynamic approaches like accommodative IOLs, scleral expansion or electrostimulation try to utilize or restore the remnant accommodative ability of the eye. Static approaches as PresbyLASIK, multifocal IOLs, monovision LASIK, or corneal inlays increase the depth of focus, thereby aiding near vision[3,4] (Fig. 1 shows a broad classification of the static approaches).
Figure 1.
A broad classification of static surgical approaches in the management of presbyopia
Corneal-based procedures offer the advantage of reversibility.[5,6] Options are available postoperatively, in the form of laser-based recorrection, if the patient is unhappy either due to the induced ametropia or corneal multifocality. The latter can cause dysphotopsia and reports of successful reversal of the induced multifocality are available.[5,6] Monovision LASIK[7,8] or PRK[9] is performed by adjusting the residual refractive error to create a low myopia in the nondominant eye to aid near vision. By this, one eye is utilized for distance vision and the other for near vision.[10] Though it is easier to plan and perform, loss of fusion and stereo acuity are the main limitations of LASIK/PRK monovision.[11] This limits the use of monovision in patients requiring good stereoacuity like professional drivers or pilots. Intermediate vision is also not possible with this technique, unless distance or near vision is compromised. Overall, myopes are better satisfied with monovision LASIK/PRK than the hyperopes and a lot of surgeons continue to use monovision technique for the treatment of presbyopia.[12]
PresbyLASIK, in contrast to monovision LASIK, is a technique where cornea is ablated using multifocal ablation profiles to correct ametropia and presbyopia.[13] With this approach, the same eye is utilized for both distance and near vision and is more physiological. Among corneal procedures, presbyLASIK has been gaining popularity. Based on how the multifocality is created, it is classified into three major types [Fig. 2].
Figure 2.
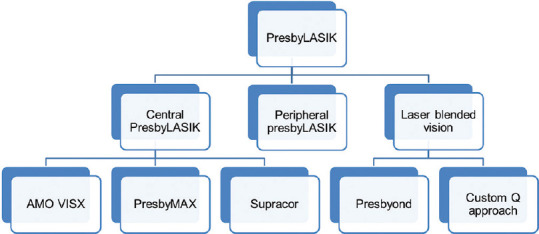
A broad classification of PresbyLASIK approaches
-
1)
Central PresbyLASIK
-
2)
Peripheral PresbyLASIK
-
3)
Laser Blended Vision (LBV).
I A) Central PresbyLASIK
Central PresbyLASIK utilizes the central zone of the cornea for near vision and surrounding peripheral zone for distance vision.[14] It is a pupil-dependent procedure and the central zone for near is considered more physiological, as during a near response, the pupil normally constricts along with accommodation. An advantage of this procedure is the minimal ablation of tissue at the center of the cornea even in myopes. Central presbyLASIK is the most commonly performed laser procedure for the correction of presbyopia[15] and includes the following.
-
A)
AMO VISX hyperopia-presbyopia multifocal approach
-
B)
SCHWIND PresbyMAX®
- PresbyMAX® symmetric
- PresbyMAX® μ-Monovision
- PresbyMAX® hybrid
-
C)
Technolas SUPRACOR.
I B) Peripheral presbyLASIK
Peripheral presbyLASIK involves using the central region for distance vision and treating the peripheral cornea to increase the depth of focus.[16] Since the normal pupillary reflex would lead to an entrance pupil which may not cover this peripheral zone, the results may not be as physiological as central presbyLASIK. The amount of tissue that is to be ablated in the center for myopia is much higher.[13]
I C) Laser Blended Vision (LBV)
This technique works by an increase in depth of focus that can be achieved by the controlled alteration of spherical aberrations (SA) in both eyes (Presbyond) or the adjustment of asphericity in nondominant eye alone (Custom Q).[12] This change in SA is small enough to avoid the degradation of visual quality but enough to increase the depth of focus for a greater range of clear vision. This procedure is suitable for myopic, hyperopic, and emmetropic patients.[17,18,19] PRESBYOND is commercially available as the PRESBYOND module of the CRS Master software, the custom ablation profile software for the MEL 80 and MEL 90 excimer lasers (Carl Zeiss Meditec, Jena, Germany) and is performed as a bilateral simultaneous LASIK treatment.[19]
Among the presbyLASIK methods mentioned above, we will be discussing the principles, patient selection, planning, and outcomes based on various published studies, for PresbyMAX®, Supracor, and Presbyond as these are the most commonly used presbyLASIK techniques in India.
II. Principles of presbyopia laser vision correction
II A) PresbyMAX®
PresbyMAX® is a module available on SCHWIND AMARIS (SCHWIND eye-tech-solutions GmbH, Kleinostheim, Germany) platform. PresbyMAX® works on the principle of central presbyLASIK by the creation of a bi-aspheric profile. The central zone is hyperpositive to provide near vision and gradual aspheric taper at the periphery for distance. Peripheral distance zone is targeted for -0.4D whereas central near add region is targeted for -1.9D of myopia.[20] In PresbyMAX-symmetric module, both the eyes are treated symmetrically with the abovementioned targets to achieve a depth of focus of 1.5D. PresbyMAX μ-Monovision involves the asymmetric correction of eyes with a difference of 0.8D between the eyes. Dominant eye is aimed for a distance target of 0 D and near target of -1.5D and the nondominant eye is targeted for a distant target of -0.8D and a near target of -2.3D. PresbyMAX hybrid is the latest addition in the PresbyMAX module which offers a differential induction of DOF in dominant and nondominant eyes along with differences in targets. Dominant eye is treated for a distance target of -0.1D and a near target of -0.9D while the nondominant eye is treated for a distance target of -0.8D and a near target of -2.3D.[21] Hence, the dominant eye has a DOF of 0.8D while the nondominant eye has a DOF of 1.5D. An overlap of binocular vision and the level of stereoacuity is highest in PresbyMAX-symmetric as compared to PresbyMAX μ-Monovision and PresbyMAX-hybrid. Figs. 3 and 4 show an example of a patient planned for PresbyMAX.
Figure 3.
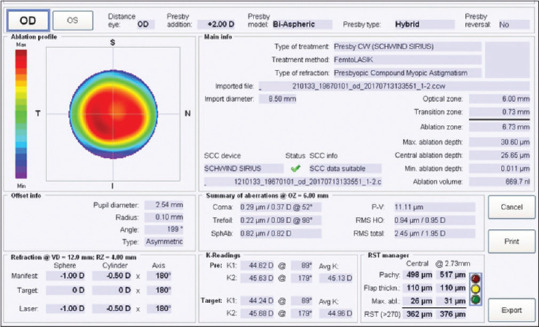
PresbyMAX hybrid planning in the dominant eye. OD is the dominant eye. Note that OD is corrected for distance with an additional paracentral corneal ablation, creating a central hyperprolate area enhancing the depth of focus
Figure 4.
PresbyMAX hybrid planning in the nondominant eye. OS is targeted to -0.89D target refraction with an additional paracentral corneal ablation, creating a central hyperprolate area enhancing the depth of focus
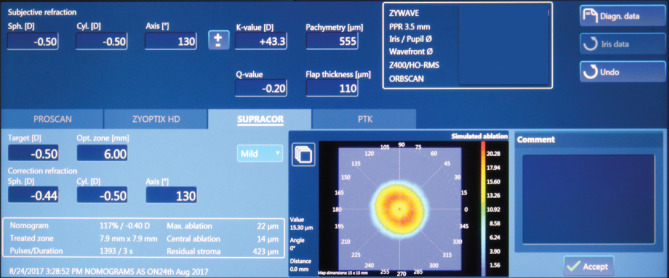
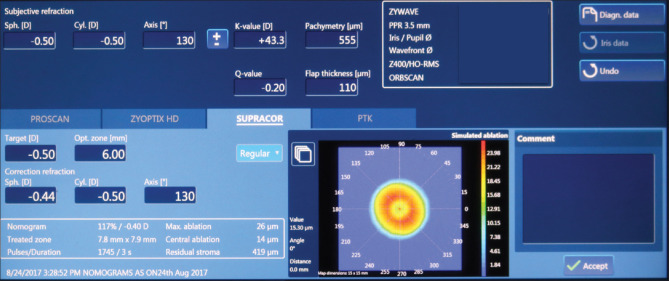
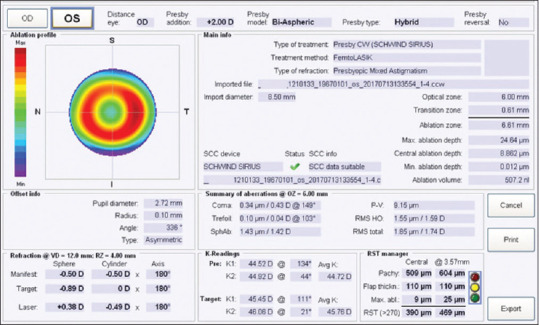
II B) SUPRACOR
Supracor is a central presbyLASIK treatment method from Technolas Perfect Vision GmbH, Munich, Germany. It is based on the principle of central presbyLASIK. Correction of distance vision is done as per the ametropic condition with a distance target of either -0.5D or emmetropia along with a central 3 mm ablation profile for a near add of about 1.75D or 1.5D.[22] Normal or regular mode of presbyopia correction on supracor would have an additional distance target of -0.5D and a near target of -1.75 D while mild correction would have a distance correction of -0.5D and a near target of -1.5D in addition. For patients who demand good distance vision, it is preferable to keep the distance target as 0D in either the dominant eye (micro monovision) or both eyes. An example of a patient planned for Supracor is explained in Figs. 5 and 6.
Figure 5.
Supracor planning. OD, the dominant eye is aimed for -0.5D myopia along with mild supracor which causes additional paracentral ablation to create an intermediate-near zone
Figure 6.
Supracor planning. OS, the nondominant eye is aimed for -0.5D myopia along with regular supracor (greater paracentral ablation compared to OD) for better near vision
II C) PRESBYOND LBV
PRESBYOND LBV is a presbyopia treatment option from Zeiss (Carl Zeiss Meditec, Germany) which uses a combination of monovision and induction of spherical aberration which leads to an increase in the depth of focus. Proprietary nonlinear aspheric ablation profiles are used which incorporate a precompensation factor to control the induction of spherical aberration (SA) without compromising visual quality, contrast sensitivity, or night vision. This range is based on studies to understand the SA levels needed to increase the depth of field[23,24] and the SA limit above which the quality of vision might be subjectively affected as reported by Reinstein at al.[25] The change in SA of 0.253 microns induces an increase in depth of focus of 0.5D to 0.65D in myopic eyes, while in hyperopic eyes, a change in SA by -0.281 microns increases DOF by 0.56 to 0.73D.[26] This combined with micro-monovision facilitates the brain to merge the two images, creating a blend zone that allows the patient to see near, intermediate, and far without glasses.
The standard micro-monovision protocol corrects the dominant eye to plano and the nondominant eye to -1.50 D irrespective of age. CRS-Master is used to plan the treatment considering the manifest refraction and spherical aberration component for both the eyes [Fig. 7]. The treatment is then imported to the laser, following which a standard bilateral simultaneous LASIK (Microkeratome/Femto) is performed.
Figure 7.
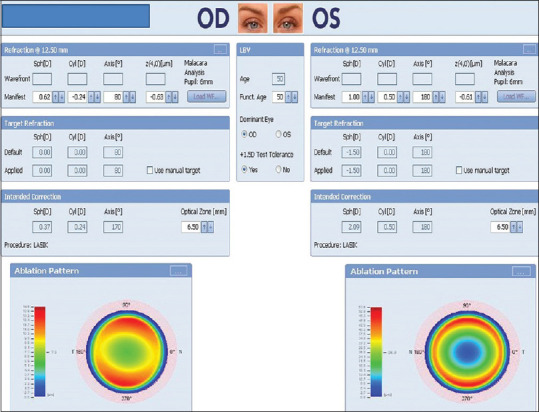
PRESBYOND treatment planning with CRS-Master for a 50-year old male. OD is the dominant eye and the patient had full tolerance to the +1.5 D test. OD was targeted to emmetropia and OS to a myopia of -1.50 D. The software automatically calculates the desired correction by adding the spherical aberration values required to adequately increase the depth of focus of each eye
III. Patient selection
There are some general considerations that are important when planning for laser vision correction for presbyopia. The criteria for good patient selection are similar to that of LASIK. In addition, creation of a multifocal profile in the cornea is associated with decrease in contrast, just like multifocal IOL insertion. Therefore, a thorough preoperative evaluation is mandatory. It is important to objectively look for lenticular changes. Aberrometers can be used to look for increased internal aberrations, especially negative spherical aberrations and schiempflug devices for changes in scatter at the level of the lens to grade dysfunctional lens syndrome.[27,28] In cases where there is an early cataractous change, it is best to go for lens-based procedures.
Pupil evaluation is very important while considering central presbyLASIK as the distance vision is obtained from mid-peripheral cornea. Preoperative pupillography[29] can help understand the pupil response. Those with poor or sluggish pupil dilation are poor candidates for central or peripheral presbyLASIK.
Dry eye evaluation needs to be done thoroughly as these patients tend to have greater prevalence of both evaporative and aqueous deficiency dry eyes. The prevalence of meibomian gland dysfunction is also higher in this age group.[30] Older patients tend to have slower wound healing. A poor quality of tear film postoperatively can worsen the quality of vision in these patients.[31] Increase in depth of focus is usually associated with a loss in contrast and preoperative conditions that can exaggerate contrast loss like higher corneal aberrations can be evaluated using a ray tracing aberrometer or a schiempflug device. It is best to avoid presbyLASIK in patients with conditions like age-related macular degeneration, diabetic retinopathy, and optic nerve pathologies where the contrast is poor. Assessment for strabismus or use of prisms preoperatively is important as patients can sometimes experience diplopia after these procedures.[12]
Judging patient expectations is of utmost importance in presbyopia management. Those with realistic expectations and willingness to adapt are preferred. The amount of near vision correction, which can be a combination of monovision and depth of focus change has to be customized as per patients' profession and requirement of near activity. It should always be explained to the patient that presbyopia is a dynamic condition and the treatment is static (suitable to their current situation). They should be explained not to compare both eyes after surgery and expect an adaptation period (up to 3 months), while the brain adjusts to process the images from the two eyes. Some of the procedures are reversible and can bring back the patient's vision status close to previous condition,[6] but its accuracy is not known. It is always better to underpromise the patients. There may be a decrease in UDVA (uncorrected distance visual acuity) for one or both the eyes. There will be situations when the patient will see better with correction even after the surgery. Since most patients are nearing the age of development of senile cataract there may be need for surgery for the same. Patient's ability to tolerate anisometropia has to be checked preoperatively using a contact lens trial when deciding upon treatments which utilize monovision.
IV. Outcomes of PresbyLASIK
Only one study has been reported utilizing an AMO VISX for central presbyLASIK by Jackson et al.[32] The study done only on hyperopic presbyopes, reported an outcome of binocular UDVA of 20/25 or better and an UNVA of J3 or better in all the 25 patients studied at one-year postoperative time point. Two lines of CDVA loss were noted in 10%.
IV A) PresbyMAX
PresbyMAX-symmetrical was the initial presbyopia treatment module developed by Schwind. Uthoff et al.[33] evaluated the outcomes of PresbyMAX symmetrical in cases of hyperopia, emmetropia, and myopia with presbyopia (+1.5D). They found that 83% patients had good UNVA (Unaided Near Visual Acuity) and were able to read regular newspaper and magazine prints. A UNVA of better than 0.3 LogRAD was found in 80% of hyperopic and myopic patients, while 90% with emmetropia had such vision. Eighty three percent of the patients had (Unaided Distance Visual Acuity) UDVA of 0.1 LogMAR or better, with 100%, 80%, and 70% of hyperopic, emmetropic, and myopic patients, respectively, having UDVA of 0.1LogMAR. Fifty percent of hyperopic and emmetropic patients and 30% or myopic patients lost at least 1 line of CDVA (Corrected Distance Visual Acuity). Two or more lines of CDVA was lost in 10%, 10%, and 20% of hyperopic, emmetropic, and myopic patients, respectively.[33]
Baudu et al.[20] studied 358 presbyopic patients with myopia and hyperopia using PresbyMAX. At 6 months, in the myopic and hyperopic groups, they found binocular UDVA >20/25 in 70% and 74%, respectively, and UNVA >J3 in 94% and 87%, respectively. They also reported a retreatment of 19% in both the groups.
In a study by Luger et al.,[34] with 1 year follow up of patients treated for ametropia ranging from -7D to +3.25D and astigmatism of 3D and presbyopia of up to +2.75D, at the end of one year 70% of patients had binocular UDVA of 0.1LogMAR or better and 84% had binocular UNVA of 0.1 Log RAD or better. 33% patients had a drop in CDVA of at least one line and 3% lost more than a line, whereas 23% patients lost a line or more of CNVA (Corrected Near Visual Acuity) and 8% lost more than a line.[34] However, PresbyMAX hybrid showed better results than PresbyMAX symmetric by the same group.[21] A binocular UDVA of 20/20 or better at one year was found in 93% of patients and all the patients had a UDVA of 20/25 or better in the myopic group. Binocular UDVA was 20/20 or better in 94% patients in the hyperopic group. Binocular UNVA of J2 or better was found in 93% of myopic and 88% of hyperopic group. Seven percent of patients in myopic and 6% of hyperopic group lost two or more lines of CDVA. Retreatment was needed in 19% of patients and 3% patients needed reversal of treatment. Postr-retreatment all patients achieved a UDVA of 20/25 or better.[21]
Chan et al.[35] studied monoocular PresbyMAX treatment for hyperopia and presbyopia with contralateral eye undergoing monofocal LASIK. Loss of CDVA of one line was seen in 10% patients while none of the patients lost more than a line of CDVA. Simultaneous binocular UDVA of 20/25 was achieved in 87% patients and a UNVA of J2 or better was achieved in 83%. Retreatment was needed in 14% of patients for improvement of UNVA. These results were comparable to previous presbyopia and hyperopia correction studies.[35]
Recently, Villanueva et al.[36] studied the long-term stability of myopic or hyperopic PresbyMAX in 24 eyes using a light propagation algorithm using MATLAB software. They reported good stability of the multifocal ablation profile created on these corneas at 3 years from the time of the surgery. This is the first study to show the stability of outcomes of any presbyLASIK procedure at 3 years. A summary of outcomes of PresbyMAX procedures are tabulated in Table 1.
Table 1.
Outcomes of PresbyMAX procedures
| Author | Refractive error (Sample size, Follow-up) | Distance vision results* | Near vision results* | % within±0.5D of target refraction (Accuracy) | Loss of CDVA* (denotes safety) | Retreatment or reversal |
|---|---|---|---|---|---|---|
| UTHOFF et al.[33] | Hyperopia (20 eyes, 6 months) | 20/25 or better in 100% | J3 or better in 80% | 60% | 1 line 40% 2 lines 10% | Up to 10% might have required further optimization, but not performed |
| LUGER M H et al.[21] | Hyperopia (PresbyMAX hybrid-µmono) (17 patients, 1-yr) | 20/25 or better in 94% | J2 or better in 88% | 76% for distance eyes, 59% for near eyes | 2 lines in 6%, 1-line in 31% | 14.7% Retreatment and 3% reversal (3% in overall cohort) |
| CHAN et al.[35] | Hyperopia Mono-ocular PresbyMAX (72 eyes, 1-yr) | 20/25 or better in 87% | J3 or better in 90% | NA | 1-line loss in 10%, no 2-line loss | 14% retreatment |
| BAUDU et al.[20] | Hyperopia (552 eyes, 6 months) | 20/25 or better in 74% | J3 or better in 87% | 91% | 25% post-op UDVA, 2 lines <pre-op CDVA | 19% retreatment |
| UTHOFF et al.[33] | Emmetropia (20 eyes, 6 months) | 20/25 or better in 80% | J3 or better in 90% | 90% | 1-line in 40%, 2-lines in 10% | Up to 10% might have required further optimization, but not performed |
| LUGER M[34] H et al. | All (-7 to + 3.25DS and up to 3DC) (62 eyes, 1-yr) | 20/25 or better in 70% | J3 or better in 94% | 73% | 1 line 33% 2-lines 3% | NA |
| LUGER M H et al.[21] | Myopia (PresbyMAX hybrid-µmono) (15 patients, 1-yr) | Better than 20/25 in 100% | J2 or better in 93% | 100% for distance eyes, 67% for near eyes | 2-lines in 7%, 1-line in 14% | 23.3% re-treatment and 3% reversal (3% in overall cohort) |
| UTHOFF et al.[33] | Myopia (20 eyes, 6 months) | Better than 20/25 in 70% | J3 or better in 80% | 70% | 1-line only 10% At least 2-lines 20% | Up to 10% might have required further optimization, but not performed |
| BAUDU et al.[20] | Myopia (164 eyes, 6 months) | 20/25 or better in 70% | J3 or better in 94% | 77% | 26% post-op UDVA, 2 lines <pre-op CDVA | 19% retreatment |
*Denotes binocular results; CDVA - Corrected distance visual acuity; NA- Not available
IV B) Supracor
The first prospective study on hyperopic presbyopia with Supracor was done by Ryan et al.[37] in 2013. This included patients with hyperopia less than +3.25 D and presbyopia of within +1.75D. UDVA was 6/6 or better in 48% patients whereas 91% had UDVA greater than 6/9.5. 89% of patients with post op MRSE 0 D had UNVA of N8 and 67% patients had N5. In patients with MRSE of <-0.50D, 76% and 88% patients could read N5 and N8, respectively. A binocular CDVA of more than 2 lines was lost in 4% of patients. Ninety one percent of patients reported that they were independent of reading glasses all the time.[37]
Cosar and Sener[38] in 2014 evaluated the results of Supracor in patients with hyperopia and presbyopia. A UDVA of 20/20 was achieved only in 22% and 20/25 in 36% patients. The loss of CDVA of one line was seen in 28.5% and two lines in 10.6% patients. A UNVA of 20/20 was seen in 77% while in 89.4% patients it was 20/25 or better. There was loss of one line of CNVA in 4.9% of patients.[38]
Saib et al.[14] studied the correction of hyperopia and presbyopia (+1.75D to 2.5D) with Supracor with micro-monovision. Using a nomogram amount of correction for distance determined the dominant and nondominant eye. Binocularly, all patients at one year achieved a UDVA of 20/25 or better. The dominant and nondominant eyes had a UDVA of 20/25 in 90% and 80% eyes, respectively. UNVA binocularly was better than J1 in 84.21% and better than J2 in 94.73% patients. Simultaneous UDVA of >20/25 and UNVA of >J2 was achieved in 86.2% patients. CDVA of 1 line was lost in 9.45% patients while 4.05% patients lost 2 or 3 lines of CDVA. 83% of patients reported that they were independent of glasses all the time.[14]
Soler et al.[39] in 2015 did a comparative study between symmetrical vs asymmetrical Supracor treatment in patients with presbyopia of less than 2D with hyperopia (MRSE +1 to +2.5D). Binocular mean UDVA was 1 ± 0.007 and 1 ± 0.0 in symmetric and asymmetric, respectively. The need for laser enhancement in the dominant eye of symmetrical Supracor was 41% and asymmetrical was 25%. None of the patients had any loss of CDVA at 18 months. Mean binocular CNVA was 0.8 ± 0.3 and 0.8 ± 0.2 in symmetric and asymmetric treatments.[39]
Ang et al.[22] reported the outcomes of Supracor in 69 hyperopic eyes of 58 patients. They were divided into three groups, wherein group A underwent Supracor in both eyes, group B underwent Supracor in one eye and hyperopic LASIK in other, and group C underwent supracor in one eye and no treatment in the other. Cumulatively, they found 100% of patients attained binocular UDVA >20/25 and 93% with UNVA >J2. They also did not find any significant differences in the outcomes between the three groups.
Vastardis et al.[40] evaluated a multifocal ablation profile with mini-monovision in patients with hyperopia <4D and presbyopia >2D. A CDVA loss of one or more line was seen in 58% patients with 10% showing loss of CNVA at 6 months. The UDVA in dominant eyes at 6 months was 0 LogMAR in 32% cases of nondominant eyes and 21% of dominant eyes. Eighty four percent of dominant eyes and 74% of nondominant eyes had a visual acuity of 0.1 LogMAR or better.
A UNVA of 0.0 LogMAR was seen in 79% of both dominant and nondominant eyes, while 0.1 LogMAR or better was seen in 100% of dominant eyes and 95% of non-dominant eyes at 6 months. Six present of patients needed re-correction in non-dominant eyes.[40]
Pajic et al.[41] conducted a prospective single surgeon study of myopia with presbyopia with micro-monovision along with multifocal ablation of cornea. They found equally good results in myopic patients with 78% of the subjects having a UNVA of 20/20 and 92% with UIVA (Unaided Intermediate Visual acuity) of 20/20 and 86% reaching a UDVA of 20/20 at 6 months. Furthermore, 36% of dominant and 64% of nondominant eyes had a UNVA of 20/20 which was similar to the results of studies on hyperopia with presbyopia.[41]
Sanchez et al.[42] have recently reported the 24-month outcomes of Supracor in 80 eyes of 40 hyperopes. They performed regular proscan (wavefront optimized) aspheric ablation on distant-dominant eye and mild supracor in the near-dominant eye. At 24 months, they reported a binocular UDVA of 20/25 or better in 100% patients and a UNVA of J1.5 or better in 90%. Two and half percent eyes lost two lines of CDVA and two eyes needed enhancement for near. A summary of outcomes of Supracor procedures are tabulated in Table 2.
Table 2.
Outcomes of Supracor procedures
| Author | Refractive error (Sample size,follow-up) | Distance vision results* | Near vision results* | % within±0.5D of target refraction (Accuracy) | Loss of CDVA* (denotes safety) | Re-treatment or reversal |
|---|---|---|---|---|---|---|
| RYAN et al.[37] | Hyperopia (46 eyes, 6 months) | 20/25 or better in 78% | N8 or better in 89% N5 or better in 67% | 54% | 2-line loss in 4% | 22% retreatment |
| COSAR et al.[38] | Hyperopia (123 eyes, 6 months) | 20/25 or better in 36.6% | 20/25 (J2) or better in 89.4% | NA | 1-line 28.5% 2-lines 10.6% | NA |
| SAIB et al.[14] | Hyperopia (74 eyes, 1-year) | 20/25 or better in 100% | J2 or better in 94.73% | NA | 1-line in 9.45% 2-lines in 4.05% | 13.51% patients needed retreatment |
| SANCHEZ et al.[42] | Hyperopia (Proscan dominant eye, Mild Supracor non-dominant eye) (80 eyes, 2-years) | 20/25 or better in 100% | J3 or better in 98% | 65% | 2-line loss in 2.5% | 2 eyes needed enhancement |
| ANG et al.[22] | Hyperopia (69 eyes, 6 months) | 20/25 or better in 100% | J2 or better in 93% | 68% | 2-line loss in 6% | 6% retreatment |
| PAJIC et al.[41] | Myopia (Supracor with micro-monovision) (72 eyes, 6 months) | 20/25 or better in 100% | J1+or better in 78% | 100% for distance, 97% for near | NA | NA |
*Denotes binocular results; CDVA - Corrected distance visual acuity; NA- Not available
IV C) Laser Blended Vision
1. PRESBYOND
This has been studied in hyperopes, emmetropes, and myopes by Reinstein et al.[17,18,19] The Presbyond treatment for hyperopes showed a CDVA of 20/20 in 86% of patients and a binocular CDVA of 20/40 or better in 100% patients. Eighty one percent patients could read J2 and all had a UNVA of J5 or better. None of the patients lost CDVA of two lines or more and 22% patients needed retreatment.[19] Emmetropic patients after Presbyond showed 20/20 UDVA in 95% and a UNVA of J2 or better in 96% and none of the eyes lost two or more lines of CDVA, retreatment was needed in 11.8% cases and 60% of them were for the near eyes.[18] Myopic patients with presbyopia (-0.20 to -8.30D) attained a binocular UDVA of 20/20 and a UNVA of J5 or better in 99% patients, with 96% having UNVA of J2 or better.[17]
2. Custom-Q ablation
Custom-Q ablation is planned in such a way that a negative asphericity (Q) is created in the nondominant eye along with a -0.5DS postoperative target, while correcting the dominant eye for distance. This negative asphericity in the nondominant eye behaves as a hyperprolate zone and aids near vision. Some classify this as a central presbyLASIK,[12] while some consider it laser blended vision.[13] In essence, Presbyond targets a certain level of SA, whereas custom-Q targets a certain range of negative asphericity.
Yin et al.[15] studied the custom-Q protocol in 138 hyperopes of median age 53.84 ± 4.2 years and reported the outcomes at the end of one year. They reported the ability to attain the targeted Q value in the nondominant eyes and those with a Δ Q of -0.8 had a binocular UDVA of 20/16 and a near vision of J2. On an average, 100% of patients were reported to have a UDVA of 20/25 or better and a UNVA of J3 or better.
Courtin et al.[43] studied the results of custom-Q protocol in 65 patients with a mean age of 56.5 ± 5.7 years. They were able to attain a postoperative mean refraction of -1.07D and 0.32D in the near and the distance-corrected eyes and the reported outcomes of UDVA 20/20 or better in 91% and UNVA J3 or better in 81% patients. Studies[15,43,44] on custom-Q have shown the sweet spot or acceptable change in Q between -0.6 and -0.8 within which the near vision improves with no significant change in optical quality. Beyond this, the quality of vision decreases. A summary of outcomes of laser-blended vision procedures are tabulated in Table 3.
Table 3.
Outcomes of Laser-blended vision procedures
| Author | Refractive error (Sample size, follow-up) | Distance vision results* | Near vision results* | % within±0.5D of target refraction (Accuracy) | Loss OF CDVA* (denotes safety) | Re-treatment or reversal |
|---|---|---|---|---|---|---|
| REINSTEIN et al.[19] | Presbyond Hyperopia (258 eyes, 1-year) | 20/20 or better in 86% | J2 or better in 81% | 79% | 2-lines loss in 0% | 22% needed retreatment |
| REINSTEIN et al.[18] | Presbyond Emmetropia (296 eyes, 1-year) | 20/20 or better in 95% | J2 or better in 96% | 95% | 2-lines loss in 0% | 11.8% needed retreatment |
| REINSTEIN et al.[17] | Presbyond Myopia (310 eyes, 1-year) | 20/20 or better in 99% | J2 or better in 96% | 92% | 2-lines loss in 0% | 19% needed retreatment |
| WANG YIN et al.[15] | Custom-Q Hyperopia (138 eyes, 1-year) | 20/25 or better in 100% | Better than J3 in 100% | NA | 2-lines loss in 1.2%, 1-line loss in 6% | 13% needed retreatment |
| COURTIN et al.[43] | Custom-Q Hyperopia (98 eyes, 6 months) | Better than 20/25 in 99% | Better than J3 in 93% | NA | 2-lines loss in 0% | 10.8% needed retreatment |
*denotes binocular results; CDVA- Corrected distance visual acuity
Discussion
In general, the outcomes and satisfaction from presbyLASIK procedures vary according to the patients' age, occupation, requirement of near activity, patients' personality, and type of procedure done. Most presbyLASIK procedures are nowadays performed as a hybrid method, i.e., with a combination of a certain degree of monovision. Hence, improvement in the depth of focus is a combination of the actual principle of presbyLASIK and monovision. A binocular UDVA of 20/25 or better and a UNVA of J3 or better can be expected if the patient and procedure selection are meticulous.
Common problems after presbyLASIK include glare, halos, loss of contrast, and decrease in UDVA. Most of these symptoms decrease with time and when persistent they can be managed by a reversal of correction.[5,6] PresbyLASIK has even been tried in pseudophakic patients who wish to be free of glasses.[45] For patients requiring cataract surgery following presbyLASIK, although IOL power calculation has been described in a few reports, the accuracy of these in larger cohorts are yet to be studied.[46] The importance of the ability to choose appropriate IOL power cannot be overemphasized as patients with presbyopia will need cataract surgery in near future and the inability to provide spectacle freedom after cataract surgery is unacceptable.
Summarizing the reported outcomes of the different presbyLASIK techniques, Supracor has mostly been studied in hyperopes and has reported good outcomes, with asymmetrical supracor having better outcomes than symmetrical procedure.[14,22,38,42] Only one study has been done in myopes using Supracor with micro-monovision, reporting good outcomes.[41] Custom-Q ablation has also been studied only in hyperopes, with good outcomes.[15,43] While PresbyMAX symmetric has had better outcomes with hyperopes and emmetropes, PresbyMAX hybrid provides better outcomes with myopes than hyperopes.[20,21,33,34,35] Presbyond LBV has better outcomes in emmetropes and myopes than hyperopes.[17,18,19]
Conclusion
Understanding of accommodation and presbyopia and the available approaches to treatment is a rapidly evolving field with newer modalities coming up very often. Newer pharmacologic therapies in the form of eye drops are also being explored, but require further research.[47] These could in future be used along with other existing procedures to enhance outcomes.
All the different presbyLASIK approaches discussed have their own advantages and disadvantages in different subgroups of presbyopes, viz., myopes or hyperopes or emmetropes. Most of them are currently performed as a hybrid procedure by utilizing a component of monovision. In short, for myopes and emmetropes, the preferred approaches would be PresbyMAX hybrid, Presbyond, and monovision LASIK, while for hyperopes, Supracor, PresbyMAX symmetric, Custom-Q, and Presbyond would be preferable.
Irrespective of the procedure planned, meticulous preoperative evaluation assessing the patients' need and customizing the planning appropriately based on the patients' tolerance of monovision is of utmost importance. Invariably, a small percentage of patients tend to lose a line or two of corrected distance vision (as mentioned in the tables), experience postoperative glare or haloes, and may require recorrection. These have to be adequately explained to the patient preoperatively. In the event of persistent unsatisfactory outcomes below our expectation, recorrection or reversal can be offered, at least 3 months after the surgery.
The long-term outcomes, in the form of maintenance of corneal multifocality and recorrection rate, and detailed outcomes when these patients require cataract surgery in the future including difficulties in IOL power calculation need further research, in order to develop a more thorough understanding of these procedures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Dr. Rohit Shetty receives research grant from Alcon and Carl Zeiss Meditec and Dr. Sheetal Brar is a consultant for Carl Zeiss Meditec. Other authors have no financial disclosures.
References
- 1.Wolffsohn JS, Davies LN. Presbyopia: Effectiveness of correction strategies. Prog Retin Eye Res. 2019;68:124–43. doi: 10.1016/j.preteyeres.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 2.Holden BA, Tahhan N, Jong M, Wilson DA, Fricke TR, Bourne R, et al. Towards better estimates of uncorrected presbyopia. Bull World Health Organ. 2015;93:667. doi: 10.2471/BLT.15.156844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Charman WN. Developments in the correction of presbyopia II: Surgical approaches. Ophthalmic Physiol Opt. 2014;34:397–426. doi: 10.1111/opo.12129. [DOI] [PubMed] [Google Scholar]
- 4.Zare Mehrjerdi MA, Mohebbi M, Zandian M. Review of static approaches to surgical correction of presbyopia. J Ophthalmic Vis Res. 2017;12:413–8. doi: 10.4103/jovr.jovr_162_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ang RE, Reyes RM, Solis ML. Reversal of a presbyopic LASIK treatment. Clin Ophthalmol. 2015;9:115–9. doi: 10.2147/OPTH.S72676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luger MH, Ewering T, Arba-Mosquera S. Nonwavefront-guided Presby reversal treatment targeting a monofocal cornea after bi-aspheric ablation profile in a patient intolerant to multifocality. J Refract Surg. 2014;30:214–6. doi: 10.3928/1081597X-20131223-01. [DOI] [PubMed] [Google Scholar]
- 7.Goldberg DB. Laser in situ keratomileusis monovision. J Cataract Refract Surg. 2001;27:1449–55. doi: 10.1016/s0886-3350(01)01001-x. [DOI] [PubMed] [Google Scholar]
- 8.Miranda D, Krueger RR. Monovision laser in situ keratomileusis for pre-presbyopic and presbyopic patients. J Refract Surg. 2004;20:325–8. doi: 10.3928/1081-597X-20040701-04. [DOI] [PubMed] [Google Scholar]
- 9.Wright KW, Guemes A, Kapadia MS, Wilson SE. Binocular function and patient satisfaction after monovision induced by myopic photorefractive keratectomy. J Cataract Refract Surg. 1999;25:177–82. doi: 10.1016/s0886-3350(99)80123-0. [DOI] [PubMed] [Google Scholar]
- 10.Evans BJ. Monovision: A review. Ophthalmic Physiol Opt. 2007;27:417–39. doi: 10.1111/j.1475-1313.2007.00488.x. [DOI] [PubMed] [Google Scholar]
- 11.Fawcett SL, Herman WK, Alfieri CD, Castleberry KA, Parks MM, Birch EE. Stereoacuity and foveal fusion in adults with long-standing surgical monovision. J AAPOS. 2001;5:342–7. doi: 10.1067/mpa.2001.119785. [DOI] [PubMed] [Google Scholar]
- 12.Stival LR, Figueiredo MN, Santhiago MR. Presbyopic excimer laser ablation: A review. J Refract Surg. 2018;34:698–710. doi: 10.3928/1081597X-20180726-02. [DOI] [PubMed] [Google Scholar]
- 13.Vargas-Fragoso V, Alio JL. Corneal compensation of presbyopia: PresbyLASIK: An updated review. Eye Vis (Lond) 2017;4:11. doi: 10.1186/s40662-017-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saib N, Abrieu-Lacaille M, Berguiga M, Rambaud C, Froussart-Maille F, Rigal-Sastourne J-C. Central PresbyLASIK for hyperopia and presbyopia using micro-monovision with the Technolas 217P platform and SUPRACOR algorithm. J Refract Surg. 2015;31:540–6. doi: 10.3928/1081597X-20150727-04. [DOI] [PubMed] [Google Scholar]
- 15.Wang Yin GH, McAlinden C, Pieri E, Giulardi C, Holweck G, Hoffart L. Surgical treatment of presbyopia with central presbyopic keratomileusis: One-year results. J Cataract Refract Surg. 2016;42:1415–23. doi: 10.1016/j.jcrs.2016.07.031. [DOI] [PubMed] [Google Scholar]
- 16.Epstein RL, Gurgos MA. Presbyopia treatment by monocular peripheral presbyLASIK. J Refract Surg. 2009;25:516–23. doi: 10.3928/1081597X-20090512-05. [DOI] [PubMed] [Google Scholar]
- 17.Reinstein DZ, Archer TJ, Gobbe M. LASIK for Myopic astigmatism and presbyopia using non-linear aspheric micro-monovision with the Carl Zeiss Meditec MEL 80 platform. J Refract Surg. 2011;27:23–37. doi: 10.3928/1081597X-20100212-04. [DOI] [PubMed] [Google Scholar]
- 18.Reinstein DZ, Carp GI, Archer TJ, Gobbe M. LASIK for presbyopia correction in emmetropic patients using aspheric ablation profiles and a micro-monovision protocol with the Carl Zeiss Meditec MEL 80 and VisuMax. J Refract Surg. 2012;28:531–41. doi: 10.3928/1081597X-20120723-01. [DOI] [PubMed] [Google Scholar]
- 19.Reinstein DZ, Couch DG, Archer TJ. LASIK for hyperopic astigmatism and presbyopia using micro-monovision with the Carl Zeiss Meditec MEL80 platform. J Refract Surg. 2009;25:37–58. doi: 10.3928/1081597X-20090101-07. [DOI] [PubMed] [Google Scholar]
- 20.Baudu P, Penin F, Arba Mosquera S. Uncorrected binocular performance after biaspheric ablation profile for presbyopic corneal treatment using AMARIS with the PresbyMAX module. Am J Ophthalmol. 2013;155:636–47. doi: 10.1016/j.ajo.2012.10.023. 647e631. [DOI] [PubMed] [Google Scholar]
- 21.Luger MH, McAlinden C, Buckhurst PJ, Wolffsohn JS, Verma S, Mosquera SA. Presbyopic LASIK using hybrid bi-aspheric micro-monovision ablation profile for presbyopic corneal treatments. Am J Ophthalmol. 2015;160:493–505. doi: 10.1016/j.ajo.2015.05.021. [DOI] [PubMed] [Google Scholar]
- 22.Ang RE, Cruz EM, Pisig AU, Solis MLPC, Reyes RMM, Youssefi G. Safety and effectiveness of the SUPRACOR presbyopic LASIK algorithm on hyperopic patients? Eye Vis (Lond) 2016;3:33. doi: 10.1186/s40662-016-0062-6. doi: 10.1186/s40662-016-0062-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marcos S, Barbero S, Jimenez-Alfaro I. Optical quality and depth-of-field of eyes implanted with spherical and aspheric intraocular lenses. J Refract Surg. 2005;21:223–35. doi: 10.3928/1081-597X-20050501-05. [DOI] [PubMed] [Google Scholar]
- 24.Marcos S, Moreno E, Navarro R. The depth-of-field of the human eye from objective and subjective measurements. Vision Res. 1999;39:2039–49. doi: 10.1016/s0042-6989(98)00317-4. [DOI] [PubMed] [Google Scholar]
- 25.Reinstein DZ, Archer TJ, Couch D, Schroeder E, Wottke M. A new night vision disturbances parameter and contrast sensitivity as indicators of success in wavefront-guided enhancement. J Refract Surg. 2005;21:S535–40. doi: 10.3928/1081-597X-20050901-23. [DOI] [PubMed] [Google Scholar]
- 26.Gifford P, Kang P, Swarbrick H, Versace P. Changes to corneal aberrations and vision after Presbylasik refractive surgery using the MEL 80 platform? J Refract Surg. 2014;30:598–603. doi: 10.3928/1081597X-20140709-01. doi: 10.3928/1081597X-20140709-01. [DOI] [PubMed] [Google Scholar]
- 27.Faria-Correia F, Lopes B, Monteiro T, Franqueira N, Ambrósio R., Jr Scheimpflug lens densitometry and ocular wavefront aberrations in patients with mild nuclear cataract. J Cataract Refract Surg. 2016;42:405–11. doi: 10.1016/j.jcrs.2015.10.069. [DOI] [PubMed] [Google Scholar]
- 28.Fernandez J, Rodriguez-Vallejo M, Martinez J, Tauste A, Piñero DP. From presbyopia to cataracts: A critical review on dysfunctional lens syndrome? J Ophthalmol. 2018;2018:4318405. doi: 10.1155/2018/4318405. doi: 10.1155/2018/4318405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wilhelm H, Wilhelm B. Clinical applications of pupillography. J Neuroophthalmol. 2003;23:42–9. doi: 10.1097/00041327-200303000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Schaumberg DA, Nichols JJ, Papas EB, Tong L, Uchino M, Nichols KK. The international workshop on meibomian gland dysfunction: Report of the subcommittee on the epidemiology of, and associated risk factors for, MGD. Invest Ophthalmol Vis Sci. 2011;52:1994–2005. doi: 10.1167/iovs.10-6997e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herbaut A, Liang H, Denoyer A, Baudouin C, Labbé A. Tear film analysis and evaluation of optical quality: A review of the literature. J Fr Ophtalmol. 2019;42:e21–35. doi: 10.1016/j.jfo.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 32.Jackson WB, Tuan KM, Mintsioulis G. Aspheric wavefront-guided LASIK to treat hyperopic presbyopia: 12-month results with the VISX platform. J Refract Surg. 2011;27:519–29. doi: 10.3928/1081597X-20101110-02. [DOI] [PubMed] [Google Scholar]
- 33.Uthoff D, Polzl M, Hepper D, Holland D. A new method of cornea modulation with excimer laser for simultaneous correction of presbyopia and ametropia. Graefes Arch Clin Exp Ophthalmol. 2012;250:1649–61. doi: 10.1007/s00417-012-1948-1. [DOI] [PubMed] [Google Scholar]
- 34.Luger MH, Ewering T, Arba-Mosquera S. One-year experience in presbyopia correction with biaspheric multifocal central presbyopia laser in situ keratomileusis. Cornea. 2013;32:644–52. doi: 10.1097/ICO.0b013e31825f02f5. [DOI] [PubMed] [Google Scholar]
- 35.Chan TC, Kwok PS, Jhanji V, Woo VCP, Ng ALK. Presbyopic Correction Using Monocular Bi-aspheric Ablation Profile (PresbyMAX) in hyperopic eyes: 1-year outcomes. J Refract Surg. 2017;33:37–43. doi: 10.3928/1081597X-20161006-03. [DOI] [PubMed] [Google Scholar]
- 36.Villanueva A, Vargas V, Mas D, Torky M, Alió JL. Long-term corneal multifocal stability following a presbyLASIK technique analysed by a light propagation algorithm. Clin Exp Optom. 2019;102:496–500. doi: 10.1111/cxo.12883. [DOI] [PubMed] [Google Scholar]
- 37.Ryan A, O'Keefe M. Corneal approach to hyperopic presbyopia treatment: Six-month outcomes of a new multifocal excimer laser in situ keratomileusis procedure. J Cataract Refract Surg. 2013;39:1226–33. doi: 10.1016/j.jcrs.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 38.Cosar CB, Sener AB. Supracor hyperopia and presbyopia correction: 6-month results. Eur J Ophthalmol. 2014;24:325–9. doi: 10.5301/ejo.5000371. [DOI] [PubMed] [Google Scholar]
- 39.Soler Tomas JR, Fuentes-Paez G, Burillo S. Symmetrical versus asymmetrical PresbyLASIK: Results after 18 months and patient satisfaction. Cornea. 2015;34:651–7. doi: 10.1097/ICO.0000000000000339. [DOI] [PubMed] [Google Scholar]
- 40.Vastardis I, Pajic-Eggspuhler B, Muller J, Cvejic Z, Pajic B. Femtosecond laser-assisted in situ keratomileusis multifocal ablation profile using a mini-monovision approach for presbyopic patients with hyperopia. Clin Ophthalmol. 2016;10:1245–56. doi: 10.2147/OPTH.S102008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pajic B, Pajic-Eggspuehler B, Mueller J, Cvejic Z, Studer H. A novel laser refractive surgical treatment for presbyopia: Optics-based customization for improved clinical outcome? Sensors (Basel, Switzerland) 2017;17:1367. doi: 10.3390/s17061367. doi: 10.3390/s1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sanchez-Gonzalez JM, Alonso-Aliste F, Amian-Cordero J, Sánchez-González MC, De-Hita-Cantalejo C. Refractive and visual outcomes of SUPRACOR TENEO 317 LASIK for presbyopia in hyperopic eyes: 24-month follow-up. J Refract Surg. 2019;35:591–8. doi: 10.3928/1081597X-20190815-01. [DOI] [PubMed] [Google Scholar]
- 43.Courtin R, Saad A, Grise-Dulac A, Guilbert E, Gatinel D. Changes to corneal aberrations and vision after monovision in patients with hyperopia after using a customized aspheric ablation profile to increase corneal asphericity (Q-factor) J Refract Surg. 2016;32:734–41. doi: 10.3928/1081597X-20160810-01. [DOI] [PubMed] [Google Scholar]
- 44.Alarcon A, Anera RG, Villa C, del Barco LJ, Gutierrez R. Visual quality after monovision correction by laser in situ keratomileusis in presbyopic patients. J Cataract Refract Surg. 2011;37:1629–35. doi: 10.1016/j.jcrs.2011.03.042. [DOI] [PubMed] [Google Scholar]
- 45.Paley GL, Chuck RS, Tsai LM. Corneal-based surgical presbyopic therapies and their application in pseudophakic patients? J Ophthalmol. 2016;2016:5263870. doi: 10.1155/2016/5263870. doi: 10.1155/2016/5263870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Qu Y, Li F, Li J. Bilateral cataract surgery in a 56-year-old man following presbyopia laser in situ keratomileusis: A case report. Saudi J Ophthalmol. 2016;30:268–71. doi: 10.1016/j.sjopt.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Krader C. Topical drops show promise as treatment for presbyopia. Ophthalmol Times Eur. 2016;12:18–20. [Google Scholar]