Abstract
Social distancing and particularly staying at home are effective public health responses to the COVID-19 pandemic. The sheer scale of behavior changes across a mass population scale is unprecedented and will undoubtedly cause disproportionate hardships for certain vulnerable groups of population and marginalized communities during different periods of the pandemic. However, at the community level, few studies have considered the spatial and temporal variations in such public health behavior changes during this pandemic. We applied a geographically and temporally weighted regression (GTWR) to analyze the spatiotemporal pattern of community stay-at-home behaviors against social vulnerability indicators at the census tract level in New York City from March to August 2020. Our findings are generally supporting the conventional wisdom of social vulnerability yet they also offer new insights. Despite the spatial variations in the effects of social vulnerability on stay-at-home behaviors, people from different vulnerable groups are also exhibiting varying reactions to the pandemic over the duration of this study, thereby highlighting the importance of understanding the spatiotemporal pattern of public health behaviors to develop an effective policy response to avoid the risk of deepening inequalities and to promote a just and sustainable urban future.
Keywords: Social vulnerability, Social distancing, Sustainability, COVID-19, GTWR
1. Introduction
The rapid spread of novel coronavirus disease 2019 (COVID-19) has caused devastating impacts and losses to countries worldwide, posing new challenges for achieving sustainability of the health system. In response, many countries adopted strict public health orders to contain the viral transmission and consequently a majority of them have now successfully kept the disease at manageable risk. However, the United States (US) is not among them. As of 8 September 2020, the total numbers of cases and deaths reach 6,287,362 and 188,688, respectively (CDC, 2020b). When considering that the US only has 4 % of the global population, it now alarmingly accounts for 23 % of the global cases and 21 % of the global deaths due to COVID-19 (WHO, 2020). This outcome is arguably due to a lack of coordinated leadership by the government (Leonhardt, 2020). Thus, local and state responses to the virus differ greatly resulting in enormously varying public health consequences across jurisdictions in the US (Fowler, Hill, Obradovich, & Levin, 2020).
Social or physical distancing is at the center of nonpharmacological responses to this pandemic, which aims to reduce person-to-person contacts that minimize public exposure to the virus (Anderson, Heesterbeek, Klinkenberg, & Hollingsworth, 2020; Beria & Lunkar, 2021). Social distancing has been demonstrated to be strongly effective in reducing the viral transmission of COVID-19 in China (Anderson et al., 2020), South Korea (Park, Sun, Viboud, Grenfell, & Dushoff, 2020), the UK (Jacob et al., 2020), and Brazil (Coelho et al., 2020), which social vulnerability plays a critical role in impeding people’s compliance with social distancing in these countries. In the meantime, a lack of consistent and timely social distancing measures at all levels of government is considered a primary reason for the frightening ramifications of this pandemic in the US (Leonhardt, 2020). Nevertheless, no matter whether the public choose to voluntarily engage in social distancing behaviors or to comply with public order, it not only requires significant shifts in behaviors but also a majority, if not all, of the population to engage to be effective (Briscese, Lacetera, Macis, & Tonin, 2020; Lewnard & Lo, 2020). Drawing from the conventional public health literature, such substantial behavior changes at this scale can be influenced by various internal (e.g. poverty) and external (e.g. misinformation) factors and the associated public containment measures can also be very difficult to implement and enforce (Brzezinski, Deiana, Kecht, & Van Dijcke, 2020; Van Bavel et al., 2020).
It is well-documented that the existing gaps in communities such as poverty and inequality will further exacerbate the disproportionate consequences to the so-called socially vulnerable populations internationally (Chen, Cutter, Emrich, & Shi, 2013; Fatemi, Ardalan, Aguirre, Mansouri, & Mohammadfam, 2017; Rufat, Tate, Burton, & Maroof, 2015). In hazardous events like this pandemic, the sociodemographic status of communities could largely determine their ability to prepare for, respond to, and recover from the event, referred to as social vulnerability (Cutter, Boruff, & Shirley, 2003; Flanagan, Gregory, Hallisey, Heitgerd, & Lewis, 2011). Hence, socially vulnerable communities are generally those with a high percentage of the population who are considered particularly vulnerable to hazardous events. For example, low-income and minority people might lack access to critical resources and services during a disaster and thus they are more likely to suffer the most (Kamel, 2012). In fact, several empirical studies around the world have already documented that socially vulnerable communities were disproportionately impacted by the pandemic both in terms of infection and mortality rates (Coelho et al., 2020; Gaynor & Wilson, 2020; Karaye & Horney, 2020; Sannigrahi, Pilla, Basu, Basu, & Molter, 2020). For example, Sannigrahi et al. (2020) identify poverty as a key determinant for COVID-19 cases and deaths in the European region.
However, on the one hand, socially vulnerable population are more susceptible to the pandemic because of unequal treatment such as their inability to access medical care, social support, and transportation services, while on the other hand, they would also be less likely or even unable to practice social distancing, thereby being more likely to be infected by the virus (Egorov, Enikolopov, Makarin, & Petrova, 2020). For example, social distancing is hardly an attainable reality in the urban slum in poor countries such as India without concomitant economic support (Wasdani & Prasad, 2020). In rich countries, socially vulnerable population (e.g. low-income and ethnic/racial minority) are also largely essential workers who are not eligible to work from home, may lack a place to shelter or live in a crowdy room who are unable to practice social distancing, and/or have prior experiences of institutional discriminations rendering them distrust in science and social institutions and more susceptible to misinformation and ‘fake news’ (Bakker & Dekker, 2012; Blendon et al., 2008; Van Bavel et al., 2020). One existing study has already demonstrated that ethnic minorities like African Americans in the US are less likely to comply with the stay-at-home orders during the pandemic (Block, Berg, Lennon, Miller, & Nunez-Smith, 2020).
Studies have proliferated in exploring the relationship between community social vulnerability and the COVID-19 pandemic outcomes. There are many attempts to understand the relationship between sociodemographic characters and infection cases and fatalities (Khazanchi et al., 2020; Kim & Bostwick, 2020; Mansour, Al Kindi, Al-Said, Al-Said, & Atkinson, 2020; Sannigrahi et al., 2020), and to explore how and to what extent these socially vulnerable population struggle during the pandemic such as maintaining social distancing behaviors and complying with the public health orders (Gaynor & Wilson, 2020; Karaye & Horney, 2020). However, existing research generally fails to consider that such effects are both spatial and temporal nonstationary. In other words, since social networks are deeply rooted in communities, the individual’s behaviors can be greatly affected by collective community values and behaviors, which can be further affected by its surrounding communities (Kuebart & Stabler, 2020). Such a spatial interconnection of community behaviors exhibits spatial nonstationarity in the effects of social vulnerability on community public health outcomes that requires spatial modeling treatment.
Additionally, the health behaviors of individuals and communities are also sensitive to time because the current behaviors will be greatly influenced by previous behaviors and the temporal change of containment policies. Hence, to investigate the effects of social vulnerability on community public health behaviors requires a spatiotemporal analysis, but few studies to our best knowledge have implemented this approach. In addition, existing studies focused primarily on the ex-post effects of social vulnerability to the community pandemic consequences (e.g. Anderson et al., 2020), while limited studies have systematically explored how these socially vulnerable communities responded to the pandemic. To fill these gaps, we applied the geographically and temporally weighted regression (GTWR; Huang, Wu, & Barry, 2010) to examine the spatial and temporal effects of social vulnerability factors on communities’ staying-at-home behaviors. This study will aim to first reexamine the conventional social vulnerability factors on public health behaviors over space and time in the context of this pandemic. It also aims to disentangle the key inequality challenges facing communities to offer policy implications not only for effective and flexible public health measures amid a pandemic but also for building a more just and sustainable future in the post-pandemic world.
2. Conceptual framework
Our theoretical framework builds on the existing literature on sustainability, disaster management, and social and behavior science. The consequences of COVID-19 are complicated and have challenged the sustainability of the health system of different countries (Cutler, 2020). The health system sustainability during the public health crisis is often associated with the quality of the whole system and its capacity to meet needs without compromising extra cost. However, inequality could further exacerbate the spread of COVID-19 and add extra burdens to the health system (Ahmed, Ahmed, Pissarides, & Stiglitz, 2020; Ahmed, Ahmad, Rodrigues, Jeon, & Din, 2021). In the context of social vulnerability, we suggest that addressing inequality should be the first step to opening up space for new approaches to sustainability during COVID-19.
We conceptualize that socially vulnerable communities are less likely to practice social distancing behaviors because they are unable or unwilling to engage in such prosocial behaviors. Our framework is mainly informed by the Social Vulnerability Index (SVI) developed by the Center for Disease Control and Prevention (CDC) to help public health officials to prioritize and implement effective strategies for communities that are the neediest for help before, during, and after a hazardous event (CDC, 2020a). Four domains were adopted to construct the SVI: 1) socioeconomic status, 2) household composition & disability, 3) minority status & language, and 4) housing & transportation. Each domain has several variables and a total of 15 variables are included to construct the overall SVI. In the following, we will introduce the factors that define social vulnerability and hypothesize how each of the factors will potentially hinder social distancing in a pandemic context.
Socioeconomic status represents the inherently disadvantaged population that would be likely to bear the disproportionate public health outcomes. The existing studies have already shown that income is a key factor in social distancing responses during this pandemic (Weill, Stigler, Deschenes, & Springborn, 2020; Zhai, Liu, & Peng, 2020). Specifically, the poor are less likely to have adequate financial resources to support their stay-at-home behaviors (Wright, Sonin, Driscoll, & Wilson, 2020). For example, people who live below the poverty line, are unemployed, and/or low-income would not be able to sustain their stay-at-home behaviors and thus they would have to go outside their homes to seek income (Martin, Markhvida, Hallegatte, & Walsh, 2020). A higher percentage of the poor might also be those who lack a shelter to stay in place or even homeless (Pirtle, 2020). In addition, less educated people (i.e., no high school diploma) are less likely to trust science and institutions, to make rational decisions, and/or to have access to consistent and reliable public health information (Achterberg, De Koster, & Van der Waal, 2017).
Household composition and disability identifies those who are dependent and require additional support so that they might be particularly sensitive to social distancing behaviors during a lockdown. Children (i.e. aged 17 or younger), for instance, are generally dependent on their parents and they lack the resource or knowledge to practice social distancing behaviors without parental guidance (Brody & Shaffer, 1982). Hence, we assume that the presence of children would require more care from their parents, which might consequently encourage stay-at-home behaviors during the closure of schools. Elderly (i.e. aged 65 or older) and disabled people require the assistance of others, which would encourage out-of-home activities of other people to help them, although not necessarily from the same neighborhoods. To this end, we still assume that more elderly and disabled populations in communities would generally reduce social distancing behaviors. Lastly in this domain, single-parent households are considered to be less resourceful or at a lower socioeconomic status, thereby increasing their burden and need to go out of their homes for work and daily care (Alon, Doepke, Olmstead-Rumsey, & Tertilt, 2020).
Minority status & language describes the social and economic marginalization of population who have experienced unequal treatment and discriminations that would have consequently made them unable to engage in social-distancing behaviors. The minority groups (i.e. all persons except white, non-Hispanic) are well-documented to be discriminated against by inequitable allocation of resources (Quinn et al., 2011; Wright & Merritt, 2020). As a result, these marginalized groups of population are more likely to be lower-income, unemployed, and homeless, which would reduce their social-distancing behaviors. They are also more likely to distrust science and social institutions and are more susceptible to misinformation and “fake news” (Van Bavel et al., 2020). Immigrants with limited English proficiency (i.e., speak English “less than well” in our case) might lack the local social roots and networks to support their social-distancing behaviors and they also might not have the ability to access or understand reliable public health guidance (Clark, Fredricks, Woc-Colburn, Bottazzi, & Weatherhead, 2020).
Housing and transportation denote housing quality and accessibility that might limit the people’s ability to shelter in place. Multi-unit housing suggests higher density. Such housing projects can be either low-income public housings or high-rise luxury apartment buildings so that it is highly contextual. Thus, its presence might not necessarily cause more or less social-distancing behaviors. We assume that the effect of multi-unit housing might be reinforcing, which means that wealthy communities are more likely to execute social distancing behaviors because of the peer pressure while the poor are less likely to execute social distancing and thus less likely to form a social norm or to create peer pressures (Borgonovi & Andrieu, 2020). However, crowding within housing units is an indicator of low-income communities, which would reduce the social distancing behaviors similarly to what we have discussed previously (Poole, Escudero, Gostin, Leblang, & Talbot, 2020), especially considering that housing inequality has been exacerbated during COVID-19 (Zhai & Peng, 2020). Mobile homes are commonly found outside of urban areas with limited accessibility to interstate highways or public transit systems (Kusenbach, Simms, & Tobin, 2010; Prasad & Stoler, 2016). In addition to that people who live in mobile homes are more likely to be low-income, their remote location also increases their possibility of going outside for jobs and essential supplies. Population without automobile ownership is not only an indicator of poverty but it also suggests that they cannot easily obtain food supplies in bulk to support such long-lasting stay-at-home behaviors and they would rely primarily on public transit (Wilbur et al., 2020), which would increase their out-of-home trips. Group quarters (e.g. college dormitories and nursing homes) might not be able to sustain social-distancing behaviors because many of these institutions are either underprepared or understaffed to quickly respond to this pandemic (Flanagan et al., 2011).
3. Methodology
3.1. Data and variables
We used all the census tracts in New York City as our study area. We chose New York City because it was the earliest epicenter during the outbreak of the COVID-19 pandemic in the US. Census tracts were utilized as the spatial units for this analysis because they are a sufficient geographic scale with adequate demographic differences and, generally, a suitable spatial unit to represent local neighborhoods. The human mobility data from 1 March 2020 through 31 August 2020 was collected from anonymized mobile phone data made available by SafeGraph COVID-19 Data Consortium (https://www.safegraph.com/COVID-19-data-consortium). By excluding the 53 census tracts with missing data, a research sample of 2113 census tracts was finalized. The daily human mobility data were spatially aggregated into the census tracts and we chose the stay-at-home percentage, which was calculated by the ratio of people that were completely at home to the sampled population, in each census tract to be the dependent variable. The dataset was later temporally aggregated into six monthly time steps for the feasibility of computation and ease of presentations. It was achieved by averaging the daily data of every month in each census tract since March 1st and consequently, we obtained a reduced spatial panel dataset with time 1 (March), time 2 (April), time 3 (May), time 4 (June), time 5 (July), and time 6 (August).
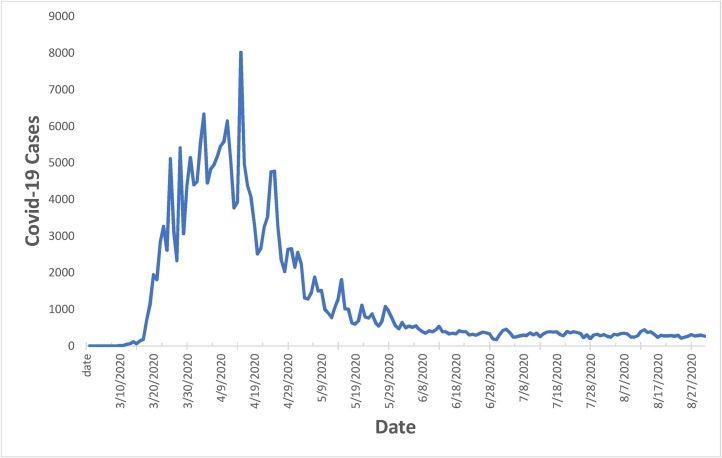
It should also be noted that the six-month study duration can be divided into two time periods: during and after the lockdown, which allows us to further compare the public behaviors of the socially vulnerable communities between these varying times. Specifically, in New York, the first COVID-19 case was reported on 1 March 2020, and a state of emergency was later declared on 7 March 2020, followed by the lockdown order soon after. The lockdown lasted for over three months and the New York City began reopening on 8 June 2020. Hence, we considered our time steps 1 (March), 2 (April), and 3 (May) as the lockdown period, and 4–5 (June–August) as the post-lockdown period. We contend that this time frame provides an ideal coverage not only for comparing the periods during and after the lockdown but also for considering the duration of the first surge of coronavirus cases and flattening the curves as shown in Fig. 1 below. The new confirmed cases increased rapidly since mid-March (in our time step 1) and later peaked at around early to mid-April (time step 2). Thereafter, the number of cases started to decrease in May (time step 3) and stabilized from June to August (i.e. time step 4–5, also as post-lockdown periods).
Fig. 1.
Covid-19 Cases in New York City from March to August.
Source: New York Times at https://github.com/nytimes/covid-19-data.
The independent variables were mainly based on the Center for Disease Control and Prevention (CDC)’s social vulnerability index (SVI). This index is developed to describe a community’s inherent social vulnerability representing their inability or lack of ability to prepare for and respond to hazardous events including a disease outbreak like this COVID-19 pandemic (Flanagan et al., 2011). We chose to include all the 15 individual social vulnerability factors to empirically test each of the variables and to avoid building our models using the reductive indexes. See Table 1 below for a summary of the variables.
Table 1.
Variable Summary.
| Variable | Obs. | Min | Max | Mean | Std. Dev. | |
|---|---|---|---|---|---|---|
| Dependent Variable | ||||||
| SAH | Stay-at-home (%) | 12678 | 5.9 | 76.3 | 43.5 | 9.4 |
| Independent Variablea | ||||||
| POV | Persons in poverty (%) | 12678 | 0.0 | 100.0 | 18.1 | 12.6 |
| UNEM | Civilian (age 16+) unemployment (%) | 12678 | 0.0 | 34.2 | 7.1 | 4.4 |
| PCI | Per capita income (in thousands) | 12678 | 5.6 | 227.1 | 36.5 | 27.6 |
| NOHS | Persons (age 25+) with no high school diploma (%) | 12678 | 0.0 | 62.3 | 18.5 | 11.5 |
| AGE65 | Persons aged 65 or older (%) | 12678 | 0.0 | 87.8 | 14.3 | 6.8 |
| AGE17 | Persons aged 17 and younger (%) | 12678 | 0.0 | 65.1 | 20.8 | 7.3 |
| DISAB | Civilian noninstitutionalized population with a disability (%) | 12678 | 0.0 | 71.6 | 10.7 | 5.2 |
| SNGP | Single parent household with children under 18 (%) | 12678 | 0.0 | 100.0 | 9.9 | 7.8 |
| MINR | Minority (all persons except white, non-Hispanic; %) | 12678 | 0.0 | 100.0 | 67.7 | 29.3 |
| LIME | Persons aged 5 or older who speak English “less than well” (%) | 12678 | 0.0 | 56.6 | 11.8 | 10.6 |
| MUNI | Housing in structures with 10 or more units (%) | 12678 | 0.0 | 100.0 | 41.8 | 35.5 |
| MOBI | Mobile homes (%) | 12678 | 0.0 | 24.9 | 0.2 | 0.7 |
| CROW | At household level (occupied housing units), more people than rooms (%) | 12678 | 0.0 | 55.5 | 9.4 | 7.3 |
| NOVE | Households with no vehicle (%) | 12678 | 0.0 | 100.0 | 48.3 | 23.8 |
| GROU | Persons in institutionalized group quarters (%) | 12678 | 0.0 | 100.0 | 2.2 | 7.5 |
All independent variables, except PCI in thousands, are percentage to the total population in the census tracts. They were retrieved from the CDC Data Repository (https://svi.cdc.gov/SVIDataToolsDownload.html) based on American Community Survey (ACS), 2014–2018 (5-year) data.
3.2. Spatiotemporal regression
Given the dynamically changing public health behaviors amid the pandemic, conventional regression models can only capture the average effect yet fail to account for the spatial and temporal heterogeneity. Geographically and temporally weighted regression (GTWR), a modified version of geographically weighted regression (GWR) that also considers temporal nonstationarity, addresses this shortcoming by allowing parameters to vary over time and space. Hence, GTWR can not only offer important spatiotemporal implications that traditional regression cannot, but also provide a better understanding of how public health behaviors change over time and space, which is of particular significance to inform public health policy. A growing number of studies have applied GTWR, such as on housing (Fotheringham, Crespo, & Yao, 2015; Huang et al., 2010; Shim & Hwang, 2018), air pollution (Chu & Bilal, 2019; Mirzaei, Amanollahi, & Tzanis, 2019), and transportation (Ma, Zhang, Ding, & Wang, 2018), but since the model is extremely computationally intensive its application is constrained to small size datasets and thus remains sparse. However, these studies consistently found that the GTWR model produced an overall better model fit and offered a valuable alternative to explore the spatiotemporal heterogeneity. A typical GTWR model can be written as follows:
where is the dependent variable percentage of stay-at-home in a census tract neighborhood i; denotes the spatial location ( as coordinates) of census tract i at time ; is the intercept value; represents a vector of parameter value for the independent variable k at the census tract i and is the respective independent variable; and denotes error term for census tract i. What is distinct about the GTWR model is that it allows the parameters to vary across the model to measure both the spatial and temporal variations in a spatiotemporal dataset. To calibrate this model, a space-time weight matrix , a diagonal matrix with elements representing the spatial and temporal weights of each census tract i, is required. The optimal spatiotemporal weight matrix is calculated by a cross-validation (CV) approach that aims to achieve the best goodness-of-fit. Given the matrix, the model is estimated using the local weighted least squares approach. See Huang et al. (2010) and Fotheringham et al. (2015) for a detailed technical discussion for the GTWR model and its calibration. The data preparation was conducted in R and the model was calibrated using a GTWR Add-in in the ArcGIS environment.
First, Moran’s I was computed for the dataset and its value was 0.171 (p < 0.001) that demonstrated strong spatial autocorrelation necessitating a spatial regression approach. Further, a test for spatial nonstationarity was also conducted by comparing the interquartile from GTWR with twice the standard errors from the OLS model (appendix 1 in the Supplementary Materials). Since the majority of the variables exhibit extra local variations, the GTWR model is preferred to explore the spatiotemporal heterogeneity (Fotheringham et al., 2015). Three of the fifteen social vulnerability variables, namely multi-unit housing (MUNI), mobile homes (MOBI), and crowded housing (CROW), do not show spatial nonstationarity and they were thus excluded from further analyses and discussions. In addition, the GTWR model has a higher adjusted R squared of 0.66 as compared to 0.13 of the OLS model (appendix 2), thereby suggesting that the GTWR model has significantly improved the overall model performance to reflect the spatial and temporal variations in the research sample.
4. Results and discussions
4.1. Overall model
The GTWR model allows the estimated parameter coefficients to vary across spatial and temporal dimensions and thus the model outputs are presented in Table 2 for the total duration of the study to demonstrate the ranges of estimates using averages, minimum values, lower quartiles, medians, upper quartiles, and maximum values. On average, poverty, per capita income, no high school diploma, aged 17 or younger, population with disability, single parent, mobile homes, no automobile ownership, and group quarters are all showing a negative sign, which suggests that increases in the variables will generally reduce stay-at-home behaviors in the communities. Similarly, the positive sign of the other variables implies greater community stay-at-home behaviors. Table 3 compares the average coefficients between the lockdown and the post-lockdown periods to further support our analysis. The results are generally aligning with our prior hypotheses based on the existing literature but there are a few exceptions. Although the coefficient averages only denote the general patterns across the study area, we are still surprised to find that some of the results are against our hypotheses.
Table 2.
GTWR Model Summary.
| Variable | AVG | MIN | LQ | MED | UQ | MAX |
|---|---|---|---|---|---|---|
| POV | −0.06 | −0.11 | −0.09 | −0.05 | −0.05 | 0.01 |
| UNEM | 0.02 | −0.03 | −0.01 | 0.02 | 0.05 | 0.07 |
| PCI | −0.05 | −0.12 | −0.08 | −0.04 | −0.03 | −0.02 |
| NOHS | −0.03 | −0.07 | −0.03 | −0.03 | −0.01 | 0.02 |
| AGE65 | 0.01 | −0.02 | −0.01 | 0.01 | 0.03 | 0.06 |
| AGE17 | −0.02 | −0.13 | −0.07 | −0.01 | 0.01 | 0.05 |
| DISAB | −0.05 | −0.13 | −0.10 | −0.08 | −0.01 | 0.07 |
| SNGP | −0.10 | −0.17 | −0.14 | −0.12 | −0.07 | 0.00 |
| MINR | 0.07 | 0.02 | 0.04 | 0.07 | 0.09 | 0.10 |
| LIME | 0.15 | 0.07 | 0.09 | 0.13 | 0.21 | 0.24 |
| NOVE | −0.02 | −0.08 | −0.03 | −0.01 | 0.01 | 0.02 |
| GROU | −0.12 | −0.28 | −0.19 | −0.11 | −0.04 | −0.01 |
| Adjusted R2 | 0.66 | |||||
Table 3.
Average Coefficients in Different Time Periods.
| Variable | During Lockdown (March, April, May) | After Lockdown (June, July, August) | All Time (March–August) |
|---|---|---|---|
| POV | −0.09 | −0.04 | −0.06 |
| UNEM | 0.05 | 0.00 | 0.02 |
| PCI | −0.08 | −0.03 | −0.05 |
| NOHS | −0.03 | −0.02 | −0.03 |
| AGE65 | 0.03 | 0.00 | 0.01 |
| AGE17 | 0.01 | −0.05 | −0.02 |
| DISAB | −0.02 | −0.09 | −0.05 |
| SNGP | −0.09 | −0.12 | −0.10 |
| MINR | 0.05 | 0.09 | 0.07 |
| LIME | 0.19 | 0.11 | 0.15 |
| NOVE | −0.03 | −0.01 | −0.02 |
| GROU | −0.19 | −0.04 | −0.12 |
Specifically, we assumed that communities with higher unemployment rates will exhibit less stay-at-home behaviors but our results suggest otherwise. We contend that this might be due to the climbing unemployment rate at the early stage of the pandemic (Fairlie, Couch, & Xu, 2020; The Federal Reserve System, 2020) causing increased stay-at-home behaviors because more people had lost their jobs and thus must stay at home or was able to afford such behaviors with some savings. The average coefficient of unemployment does drop from 0.05 during the lockdown to approximately zero after the lockdown, suggesting as the unemployment rate reduces and stabilizes after reopening the economy the effect of unemployment on the stay-at-home behaviors starts to reduce and fade away.
Additionally, communities with higher per capita income, or wealthier communities, are staying less at home. Since we controlled for a variety of socioeconomic variables, this might indicate the additional influences that income has on social distancing behaviors, thereby suggesting that higher income would generally discourage sheltering in place. The reason might simply be that people with higher income would go out more but in a safer way such as driving their own vehicles, staying within their own social bubbles, and exercising good public health measures such as maintaining social distancing and wearing masks in the public.
Another surprising finding is that the marginalized population like the ethnic minority and people with limited English proficiency are shown to increase community stay-at-home behaviors. Although the majority of empirical studies have shown that the marginalized communities are less likely to exercise social distancing behaviors (Block et al., 2020; Coven & Gupta, 2020), they are focusing primarily on the African American communities. Our minority and English proficiency variables, however, are much more inclusive and thus they could represent communities with higher diversity. To this end, our findings are consistent with those of Egorov et al. (2020) that ethnic fractionalization (diversity) would contribute to more prosocial behaviors because of stronger in-group networks and greater out-group distrust.
4.2. Spatial dimension
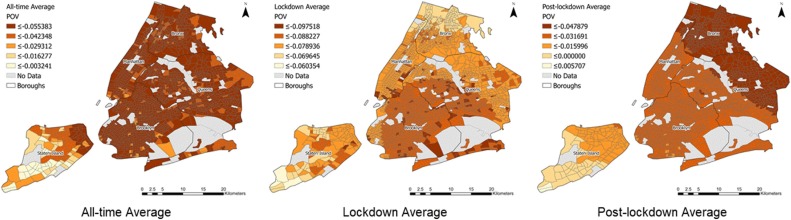
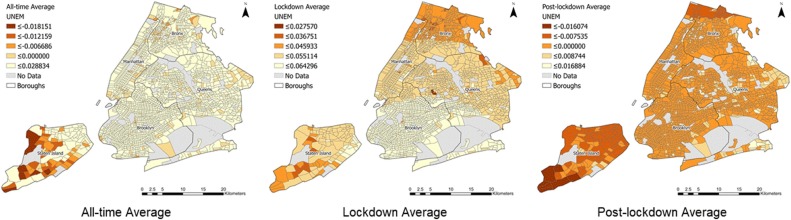
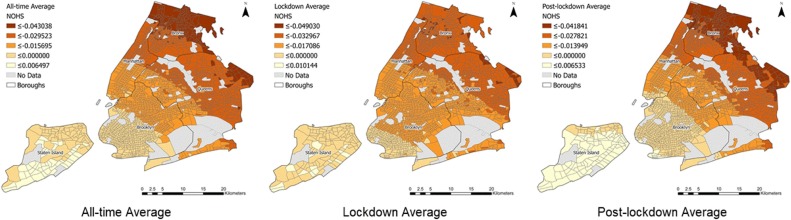
A principal feature of GWR-based models is that the model coefficients are mappable (Ma et al., 2018). For GTWR model, not only each of the spatial units, census tracts in this case, has a vector of coefficients corresponding to the different variables, but also one coefficient for each of the time steps. We will use the average values for each census tract with respect to time in this section to explore the spatial variations, thereby leaving the discussions of temporal variations for the subsequent section. The spatial patterns of the average coefficients of three selected variables were visualized in Fig. 2, Fig. 3, Fig. 4 due to space limitation, illustrating the varying effects of each variable on the stay-at-home behaviors over space. Table 4 provides a contextual backdrop of the five New York Boroughs for our spatial discussions. In brief, Bronx and Brooklyn are the poorest Boroughs with the highest percentage of African Americans. In contrast, Manhattan, the central business district, has the highest per capita income and population density. Queens and Staten Islands are in between, where Queens leans towards the poverty side and Staten Island otherwise.
Fig. 2.
Spatial Pattern of the Average Coefficients for Poverty in all time, during lockdown, and after the lockdown periods.
Fig. 3.
Spatial Pattern of the Average Coefficients for Unemployment in all time, during lockdown, and after the lockdown periods.
Fig. 4.
Spatial Pattern of the Average Coefficients for No High School Diploma in all time, during lockdown, and after the lockdown periods.
Table 4.
Basic Characteristics of New York Boroughs.
| Jurisdiction | Population | Black (%) | Income (median household) | Per capita Income | Poverty (%) | Unemployment (%, average from March to August 2020) |
|---|---|---|---|---|---|---|
| Bronx | 1,418,207 | 43.60 | $38,085 | $20,850 | 27.30 | 19.13 |
| Brooklyn | 2,559,903 | 33.80 | $56,015 | $31,984 | 18.90 | 15.10 |
| Manhattan | 1,628,706 | 17.80 | $82,459 | $72,832 | 15.60 | 12.20 |
| Queens | 2,253,858 | 20.70 | $64,987 | $30,289 | 11.60 | 16.62 |
| Staten Island | 476,143 | 11.60 | $79,267 | $34,987 | 11.70 | 13.92 |
| New York City | 8,336,817 | 24.30 | $60,762 | $37,693 | 18.90 | 15.58 |
Source: US Census QuickFacts 2019 & New York State Department of Labor.
The average effects of poverty are generally significant across the city for the duration of this study (Fig. 2). During the lockdown, the effects of poverty are the strongest in Brooklyn, spreading over to the surrounding communities. This might be due to that Brooklyn not only has the highest total population but also the most African Americans. Hence, communities in these neighborhoods are particularly suffering from poverty exacerbated by the Pandemic, which limited their ability to shelter in place. Surprisingly, the effects are somehow small in Bronx, which might be due to the diminishing marginal effect of greater poverty in these areas. However, after the lockdown, the effects in Bronx and Northeastern Queens become the strongest which implies that people in extreme poverty have greatly suffered from the lockdown. Thus, since the reopening of the economy, people in these communities are most likely to exhaust their savings during the prolonged lockdown and, therefore, they are the least likely to continue staying at home.
The average effects of unemployment are only shown to reduce stay-at-home behaviors in some part of Staten Island and Bronx for the all-time duration (Fig. 3). Interestingly, during the lockdown, unemployment increases stay-at-home behaviors across the city, while after the lockdown unemployment reduces such behaviors, yet at a lower degree given the small coefficients, in most parts of the city. Note that the reason why we observe a zero coefficient for variable unemployment in the post-lockdown period is because the coefficient evens out when we sum up the positive and negative coefficients of all the census tracts in the city. This result further supports that the unemployed population during the lockdown are forced to stay at home when there are few job opportunities while after the lockdown these people are the most desperate to go outside seeking income. Additionally, the spatial distributions of effects of lack of education (i.e. no high school diploma) are self-explanatory (Fig. 4). The undereducated populations are primarily concentrating in Bronx and Queens, where the effects on reducing social-distancing behaviors were the strongest and spreading over to Brooklyn and Manhattan. The effects of education are generally consistent during and after the lockdown period.
4.3. Temporal dimension
The GTWR model also allows obtaining a time series of the coefficients over the study time steps. Fig. 5 illustrates a time series of average coefficients of all the variables for the entire study area. We could observe a common pattern that the effects of most variables were the greatest from the beginning of the pandemic (i.e. during the lockdown and surging cases in March and April) and their effects were attenuated afterward when people gradually adapted to the impacts and changes due to the pandemic. It is also obvious that not all the conventional socially vulnerable variables appear to adversely impact the social distancing behaviors in the context of this pandemic, many of which we have already discussed in the previous sections. Here, we would like to highlight a number of key exceptions that we have not focused on yet. Firstly, more people with limited English proficiency interestingly seem to increase stay-at-home behaviors in the communities. This pattern can be probably explained by that these people are primarily first-generation immigrants who have little social trust with the greater community that renders them extremely cautious when it comes to self-protection behaviors like social distancing amid pandemic (Hagan, 1998; Kumlin & Rothstein, 2010). Secondly, single parents are showing alarmingly significant vulnerability during this pandemic as they are under the extra burden to support their families so that throughout the pandemic periods in this study they appear to not be able to shelter in place that we think is because they have to go outside to work and shop. Since they are the only dependent in the family, unable to comply with the stay-at-home orders greatly exposes them to the virus and if they were indeed infected the consequences for the family would be catastrophic. Lastly, people with disability require additional support from other people so that at the beginning of the lockdown they appear to be mostly staying at home but as the pandemic worsens and considering the citywide lockdown, they would need to take care of themselves or require support from other community members, which all would increase outside trips.
Fig. 5.
Temporal Variation of the Parameter Coefficients.
5. Policy implications and conclusions
It is imperative to understand public health behaviors that vary over space and time to inform effective policy making during a pandemic. This study applies the GTWR model to investigate the relationship between conventional social vulnerability indicators and social-distancing behaviors (i.e. stay-at-home) at the census tract neighborhood levels in New York City. The model results offer new and timely insights into spatial and temporal variations in the socially vulnerable communities’ responses to the continuing pandemic. Admittedly, there is no one-fits-all policy that can address the pandemic uniformly across communities and over time, but we contend that public health officials should consider developing a continuum of effective evidenced-based and flexible policies that are designed to target the groups of socially vulnerable populations that suffered the greatest and to allow rapid changes to meet new needs along with the evolving ramifications of the pandemic. For instance, in June, New York State Governor approved a $100 million rental assistance funding that will offer emergency vouchers for vulnerable individuals or families during COVID-19. Our results generally imply at what time period the bill should be paid to vulnerable households in what places. Moreover, our results are timely for New York City's Recovery Agenda, which aims to center service and action in communities that have undertaken the most burden of economic and health inequities during the pandemic.
A key contribution is that our results suggest that public reactions to the pandemic vary and change dynamically over space and time. One obvious policy implication from it is to continuously identify and monitor the vulnerable groups of population amid the pandemic to develop targeted policy response for them to avoid the risk of deepening inequalities. It is because control measures must be equitable and inclusive, particularly considering the hardships for our most vulnerable communities (Berger, Evans, Phelan, & Silverman, 2020). The government can establish collaboration with private enterprises to take advantage of the big data (e.g., mobile phone data, Google navigation data, Yelp sign-ins, or geotagged tweets) to monitor public mobility patterns and social distancing behaviors to jointly inform policy making (Zhou et al., 2020), particularly in socially vulnerable communities. In practice, the city of Los Angeles and RMDS Lab have partnered up to host an open competition for data scientists and analysts to involving in monitoring and combating the pandemic. Several attempts have been made to propose a new approach for such endeavors, such as that Ahmed, Ahmed, Pissarides et al. (2020) and Ahmed, Ahmad, Rodrigues, Jeon, & Din, 2021 developed a deep learning-based monitoring framework to detect social distancing behaviors using videos from the closed-circuit television cameras. This pandemic offers unprecedented challenges for governments to overcome but at the same time it provides a unique opportunity to reexamine our policies, to improve, and to innovate.
As it is evident that socially vulnerable populations will be disproportionately impacted by almost all stressors, how to reduce such inequalities is not only a priority for local communities but also a global agenda as identified by the United Nations Sustainable Development goals (https://sdgs.un.org/goals). Hence, in a post-pandemic era, it is also imperative to reevaluate our community inequalities and find new ways to improve them in our plans, policies, and decision makings to make our cities more resilient in case of a second or even a third wave of the pandemic or another major disaster. By resilient, we mean that the cities should avoid the mere engineering notion of bouncing back but undertake transformative reform to bounce forward because the COVID-19 can be continuing and could be worsening before the mass vaccination. As large infusions of money will be required for recovery (Olshansky and Johnson, 2014), the governments would need to align such investments to long-term sustainable development goals, aiming to reduce the inequality gap, rather than going down the same old path by focusing on immediate job creation and income growth.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgement
This work was supported by University of Waikato Covid-19 Research Recovery Fund, New Zealand.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.scs.2021.102757.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Achterberg P., De Koster W., Van der Waal J. A science confidence gap: Education, trust in scientific methods, and trust in scientific institutions in the United States, 2014. Public Understanding of Science. 2017;26(6):704–720. doi: 10.1177/0963662515617367. [DOI] [PubMed] [Google Scholar]
- Ahmed F., Ahmed N.E., Pissarides C., Stiglitz J. Why inequality could spread COVID-19. The Lancet Public Health. 2020;5(5):e240. doi: 10.1016/S2468-2667(20)30085-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed I., Ahmad M., Rodrigues J.J., Jeon G., Din S. A deep learning-based social distance monitoring framework for COVID-19. Sustainable Cities and Society. 2021;65:1–12. doi: 10.1016/j.scs.2020.102571. 102571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alon T.M., Doepke M., Olmstead-Rumsey J., Tertilt M. National Bureau of Economic Research; 2020. The impact of COVID-19 on gender equality (No. w26947) [Google Scholar]
- Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? The Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker L., Dekker K. Social trust in urban neighbourhoods: The effect of relative ethnic group position. Urban Studies. 2012;49(10):2031–2047. [Google Scholar]
- Berger Z.D., Evans N.G., Phelan A.L., Silverman R.D. 2020. Covid-19: Control measures must be equitable and inclusive. [DOI] [PubMed] [Google Scholar]
- Beria P., Lunkar V. Presence and mobility of the population during the first wave of COVID-19 outbreak and lockdown in Italy. Sustainable Cities and Society. 2021;65:1–15. doi: 10.1016/j.scs.2020.102616. 102616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blendon R.J., Koonin L.M., Benson J.M., Cetron M.S., Pollard W.E., Mitchell E.W.…Herrmann M.J. Public response to community mitigation measures for pandemic influenza. Emerging Infectious Diseases. 2008;14(5):778. doi: 10.3201/eid1405.071437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block R., Berg A., Lennon R.P., Miller E.L., Nunez-Smith M. African american adherence to COVID-19 public health recommendations. HLRP: Health Literacy Research and Practice. 2020;4(3):e166–e170. doi: 10.3928/24748307-20200707-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgonovi F., Andrieu E. Bowling together by bowling alone: Social capital and COVID-19. COVID Economics. 2020;17:73–96. doi: 10.1016/j.socscimed.2020.113501. [DOI] [PubMed] [Google Scholar]
- Briscese G., Lacetera N., Macis M., Tonin M. National Bureau of Economic Research; 2020. Compliance with COVID-19 social-distancing measures in italy: The role of expectations and duration (No. w26916) [Google Scholar]
- Brody G.H., Shaffer D.R. Contributions of parents and peers to children’s moral socialization. Developmental Review. 1982;2(1):31–75. [Google Scholar]
- Brzezinski A., Deiana G., Kecht V., Van Dijcke D. The COVID-19 pandemic: Government vs. community action across the united states. COVID Economics: Vetted and Real-Time Papers. 2020;7:115–156. [Google Scholar]
- CDC . 2020. CDC SVI 2018 documentation.https://svi.cdc.gov/Documents/Data/2018_SVI_Data/SVI2018Documentation-508.pdf [Google Scholar]
- CDC . 2020. CDC COVID data tracker.https://COVID.cdc.gov/COVID-data-tracker/#cases [Google Scholar]
- Chen W., Cutter S.L., Emrich C.T., Shi P. Measuring social vulnerability to natural hazards in the Yangtze River Delta region, China. International Journal of Disaster Risk Science. 2013;4(4):169–181. [Google Scholar]
- Chu H.J., Bilal M. PM 2.5 mapping using integrated geographically temporally weighted regression (GTWR) and random sample consensus (RANSAC) models. Environmental Science and Pollution Research. 2019;26(2):1902–1910. doi: 10.1007/s11356-018-3763-7. [DOI] [PubMed] [Google Scholar]
- Clark E., Fredricks K., Woc-Colburn L., Bottazzi M.E., Weatherhead J. Disproportionate impact of the COVID-19 pandemic on immigrant communities in the United States. PLoS Neglected Tropical Diseases. 2020;14(7) doi: 10.1371/journal.pntd.0008484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coelho F.C., Lana R.M., Cruz O.G., Villela D.A., Bastos L.S., Pastore y Piontti A.…Gomes M.F. Assessing the spread of COVID-19 in Brazil: Mobility, morbidity and social vulnerability. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0238214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coven J., Gupta A. 2020. Disparities in mobility responses to COVID-19. NYU Stern Working Paper. [Google Scholar]
- Cutler D. How Will COVID-19 Affect the Health Care Economy? JAMA. 2020;323(22):2237–2238. doi: 10.1001/jama.2020.7308. [DOI] [PubMed] [Google Scholar]
- Cutter S.L., Boruff B.J., Shirley W.L. Social vulnerability to environmental hazards. Social Science Quarterly. 2003;84(2):242–261. [Google Scholar]
- Egorov G., Enikolopov R., Makarin A., Petrova M. National Bureau of Economic Research; 2020. Divided we stay home: Social distancing and ethnic diversity (No. w27277) [Google Scholar]
- Fairlie R.W., Couch K., Xu H. National Bureau of Economic Research; 2020. The impacts of COVID-19 on minority unemployment: First evidence from April 2020 cps microdata (No. w27246) [Google Scholar]
- Fatemi F., Ardalan A., Aguirre B., Mansouri N., Mohammadfam I. Social vulnerability indicators in disasters: Findings from a systematic review. International Journal of Disaster Risk Reduction. 2017;22:219–227. [Google Scholar]
- Flanagan B.E., Gregory E.W., Hallisey E.J., Heitgerd J.L., Lewis B. A social vulnerability index for disaster management. Journal of Homeland Security and Emergency Management. 2011;8(1) [Google Scholar]
- Fotheringham A.S., Crespo R., Yao J. Geographical and temporal weighted regression (GTWR) Geographical Analysis. 2015;47:431–452. [Google Scholar]
- Fowler J.H., Hill S.J., Obradovich N., Levin R. 2020. The effect of stay-at-home orders on COVID-19 cases and fatalities in the United States. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaynor T.S., Wilson M.E. Social vulnerability and equity: The disproportionate impact of COVID‐19. Public Administration Review. 2020;80(5):832–838. doi: 10.1111/puar.13264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan J.M. Social networks, gender, and immigrant incorporation: Resources and constraints. American Sociological Review. 1998:55–67. [Google Scholar]
- Huang B., Wu B., Barry M. Geographically and temporally weighted regression for modeling spatio-temporal variation in house prices. International Journal of Geographical Information Science. 2010;24(3):383–401. [Google Scholar]
- Jacob L., Tully M.A., Barnett Y., Lopez-Sanchez G.F., Butler L., Schuch F.…Yakkundi A. The relationship between physical activity and mental health in a sample of the UK public: A cross-sectional study during the implementation of COVID-19 social distancing measures. Mental Health and Physical Activity. 2020;19 doi: 10.1016/j.mhpa.2020.100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamel N. Social marginalisation, federal assistance and repopulation patterns in the New Orleans metropolitan area following Hurricane Katrina. Urban Studies. 2012;49(14):3211–3231. [Google Scholar]
- Karaye I.M., Horney J.A. The impact of social vulnerability on COVID-19 in the US: An analysis of spatially varying relationships. American Journal of Preventive Medicine. 2020;59(3):317–325. doi: 10.1016/j.amepre.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khazanchi R., Beiter E.R., Gondi S., Beckman A.L., Bilinski A., Ganguli I. County-level association of social vulnerability with COVID-19 cases and deaths in the USA. Journal of General Internal Medicine. 2020;35(9):2784–2787. doi: 10.1007/s11606-020-05882-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.J., Bostwick W. Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Education & Behavior. 2020;47(4) doi: 10.1177/1090198120929677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuebart A., Stabler M. Infectious diseases as socio‐spatial processes: The Covid‐19 outbreak in Germany. Tijdschrift voor economische en sociale geografie. 2020;111(3):482–496. doi: 10.1111/tesg.12429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumlin S., Rothstein B. Questioning the new liberal dilemma: Immigrants, social networks, and institutional fairness. Comparative Politics. 2010;43(1):63–80. [Google Scholar]
- Kusenbach M., Simms J.L., Tobin G.A. Disaster vulnerability and evacuation readiness: Coastal mobile home residents in Florida. Natural Hazards. 2010;52(1):79. [Google Scholar]
- Leonhardt D. 2020. The unique U.S. Failure to control the virus.https://www.nytimes.com/2020/08/06/us/coronavirus-us.html [Google Scholar]
- Lewnard J.A., Lo N.C. Scientific and ethical basis for social-distancing interventions against COVID-19. The Lancet Infectious Diseases. 2020;20(6):631. doi: 10.1016/S1473-3099(20)30190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma X., Zhang J., Ding C., Wang Y. A geographically and temporally weighted regression model to explore the spatiotemporal influence of built environment on transit ridership. Computers, Environment and Urban Systems. 2018;70:113–124. [Google Scholar]
- Mansour S., Al Kindi A., Al-Said A., Al-Said A., Atkinson P. Sociodemographic determinants of COVID-19 incidence rates in Oman: Geospatial modelling using multiscale geographically weighted regression (MGWR) Sustainable Cities and Society. 2020;65:1–13. doi: 10.1016/j.scs.2020.102627. 102627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin A., Markhvida M., Hallegatte S., Walsh B. Socio-economic impacts of COVID-19 on household consumption and poverty. Economics of Disasters and Climate Change. 2020:1–27. doi: 10.1007/s41885-020-00070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirzaei M., Amanollahi J., Tzanis C.G. Evaluation of linear, nonlinear, and hybrid models for predicting PM 2.5 based on a GTWR model and MODIS AOD data. Air Quality, Atmosphere & Health. 2019;12(10):1215–1224. [Google Scholar]
- Olshansky R.B., Johnson L.A. The evolution of the federal role in supporting community recovery after US disasters. Journal of the American Planning Association. 2014;80(4):293–304. [Google Scholar]
- Park S.W., Sun K., Viboud C., Grenfell B.T., Dushoff J. Potential role of social distancing in mitigating spread of coronavirus disease, South Korea. Emerging Infectious Diseases. 2020;26(11):2697. doi: 10.3201/eid2611.201099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirtle W.N.L. Racial capitalism: A fundamental cause of novel coronavirus (COVID-19) pandemic inequities in the United States. Health Education & Behavior. 2020;47(7):504–508. doi: 10.1177/1090198120922942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole D.N., Escudero D.J., Gostin L.O., Leblang D., Talbot E.A. Responding to the COVID-19 pandemic in complex humanitarian crises. International Journal for Equity in Health. 2020;19(1):1–2. doi: 10.1186/s12939-020-01162-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad S., Stoler J. Mobile home residents and hurricane vulnerability in South Florida: Research gaps and challenges. International Journal of Disaster Risk Science. 2016;7(4):436–439. [Google Scholar]
- Quinn S.C., Kumar S., Freimuth V.S., Musa D., Casteneda-Angarita N., Kidwell K. Racial disparities in exposure, susceptibility, and access to health care in the US H1N1 influenza pandemic. American Journal of Public Health. 2011;101(2):285–293. doi: 10.2105/AJPH.2009.188029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rufat S., Tate E., Burton C.G., Maroof A.S. Social vulnerability to floods: Review of case studies and implications for measurement. International Journal of Disaster Risk Reduction. 2015;14:470–486. [Google Scholar]
- Sannigrahi S., Pilla F., Basu B., Basu A.S., Molter A. Examining the association between socio-demographic composition and COVID-19 fatalities in the European region using spatial regression approach. Sustainable Cities and Society. 2020;62 doi: 10.1016/j.scs.2020.102418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim J., Hwang C. Kernel-based geographically and temporally weighted autoregressive model for house price estimation. PLoS One. 2018;13(10) doi: 10.1371/journal.pone.0205063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Federal Reserve System . 2020. Perspectives from main street: The impact of COVID-19 on communities and the entities serving them.https://www.frbatlanta.org/-/media/documents/community-development/publications/federal-reserve-system-resources/05/04/perspectives-from-main-street-the-impact-of-COVID-19-on-communities.pdf [Google Scholar]
- Van Bavel J.J., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M.…Drury J. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour. 2020:1–12. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Wasdani K.P., Prasad A. The impossibility of social distancing among the urban poor: The case of an Indian slum in the times of COVID-19. Local Environment. 2020;25(5):414–418. [Google Scholar]
- Weill J.A., Stigler M., Deschenes O., Springborn M.R. Social distancing responses to COVID-19 emergency declarations strongly differentiated by income. Proceedings of the National Academy of Sciences. 2020;117(33):19658–19660. doi: 10.1073/pnas.2009412117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. WHO coronavirus disease (COVID-19) dashboard.https://COVID19.who.int/ [Google Scholar]
- Wilbur M., Ayman A., Ouyang A., Poon V., Kabir R., Vadali A.…Dubey A. 2020. Impact of COVID-19 on public transit accessibility and ridership. arXiv preprint arXiv:2008.02413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright J.E., Merritt C.C. Social equity and COVID‐19: The case of african americans. Public Administration Review. 2020;80(5):820–826. doi: 10.1111/puar.13251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright A.L., Sonin K., Driscoll J., Wilson J. University of Chicago, Becker Friedman Institute for Economics Working Paper; 2020. Poverty and economic dislocation reduce compliance with COVID-19 shelter-in-place protocols. (2020-40) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai W., Peng Z.R. Where to buy a house in the United States amid COVID-19? Environment and Planning A: Economy and Space. 2020;53(1):9–11. 0308518X20946041. [Google Scholar]
- Zhai W., Liu M., Peng Z.R. Social distancing and inequality in the United States amid COVID-19 outbreak. Environment and Planning A: Economy and Space. 2020;53(1):3–5. 0308518X20932576. [Google Scholar]
- Zhou C., Su F., Pei T., Zhang A., Du Y., Luo B.…Song C. COVID-19: Challenges to GIS with big data. Geography and Sustainability. 2020;1(1):77–87. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.