Abstract
Objectives
A valid measurement of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) incubation period is needed for case definitions and for adapting appropriate isolation measures but is challenging in an emergency context. Our objective was to systematically review recent literature reporting estimates of the distribution of the incubation period of SARS-CoV-2 and describe the distribution and its variability and dispersion through a meta-analysis.
Methods
A systematic review was carried out on studies published from 1 January 2020 to 10 January 2021 reporting the SARS-CoV-2 incubation period. Individual mean and standard deviation were used to produce the pooled estimate. Sources of heterogeneity were explored by age, gender and study design using a meta-regression.
Results
In total, 99 studies were eligible for analysis in our meta-analysis. The pooled estimate of the mean incubation period across the studies was 6.38 days, 95% CI (5.79; 6.97).
Conclusion
Calculation of the mean incubation period will help with the identification of time of exposure, however, determinants of its variations/range might be explored for potential links with the clinical outcome or pathogenic steps at the early stage of infection. A real-time meta-analysis, named the InCoVid Lyon, is proposed following this initial analysis.
Keywords: COVID-19, Incubation, Infection Control, Meta-analysis, SARS-CoV-2
Introduction
COVID-19 is an infectious disease associated with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which causes lower respiratory tract infections; to date, it is responsible for more than 2 million deaths worldwide (Gisanddata map, 2020).
The incubation period is the interval between the moment a person is infected and the onset of the disease. Knowledge of the duration of the incubation period is essential for the case definition, management of emerging threats, estimation of the duration of follow-up for contact tracing and secondary case detection, and the establishment of public health programs aimed at reducing local transmission (Nishiura et al., 2012).
According to the World Health Organization (WHO), SARS-CoV-2 incubation periods ranging from 1 to 14 days have been reported (WHO, 2020). The distribution of the incubation period may vary between individuals as a result of certain determinants, including host factors.
There is a need to increase our knowledge on the incubation period distribution of SARS-CoV-2 to support effective outbreak investigations.
The objective of this study was to conduct a meta-analysis on summary estimates of the distribution of the incubation period of SARS-CoV-2 as reported in the literature.
Methods
A systematic literature search of peer-reviewed publications was conducted to identify studies reporting the incubation period of SARS-CoV-2. The following terms were used to select papers: ‘Novel Coronavirus’ OR ‘COVID*’ OR ‘Coronavirus’ OR ‘2019-nCoV’ OR ‘SARS-CoV-2′ OR ‘MERS-CoV’ OR ‘SARS’ OR ‘Severe Acute Respiratory Syndrome’ AND ‘incubation’ OR ‘incubation period’.
The search covered literature published from 1 January 2020 to 10 January 2021.
Articles or abstracts in languages other than English were excluded.
Data on the published article, the study characteristics, and summary measures of the incubation period were gathered. Measures of dispersion, as well as data on age and gender distribution, were collected where available. All studies reported at least 1 summary statistic of the incubation period distribution as a mean, median or range. The unit of measurement was days.
Individual mean and standard deviation were used to produce the pooled estimate. Inverse variance weighting was used for pooling individual estimation of mean, median, and 95th and 97.5th percentile of the incubation period. Heterogeneity between studies was assessed using the I2 statistic (Higgins and Thompson, 2002). Age, gender and study design were considered as candidate explicative covariables. All data analyses were done using R (version 3.6.3). Results of this meta-analysis are shared on the following site: InCoVid-Lyon (Incovid, 2020).
Results
In total, 99 articles were selected for analysis (.Supplementary appendix). The majority of the studies reported on cases in Asian countries. In total, 23 (23.2%) cohort, 61 (61.6%) case series, and 15 (15.2%) modeling studies were gathered, with a median age of 45 years, and a sex ratio >1. The median sample size was estimated at 52 individuals (IQR 20; 161).
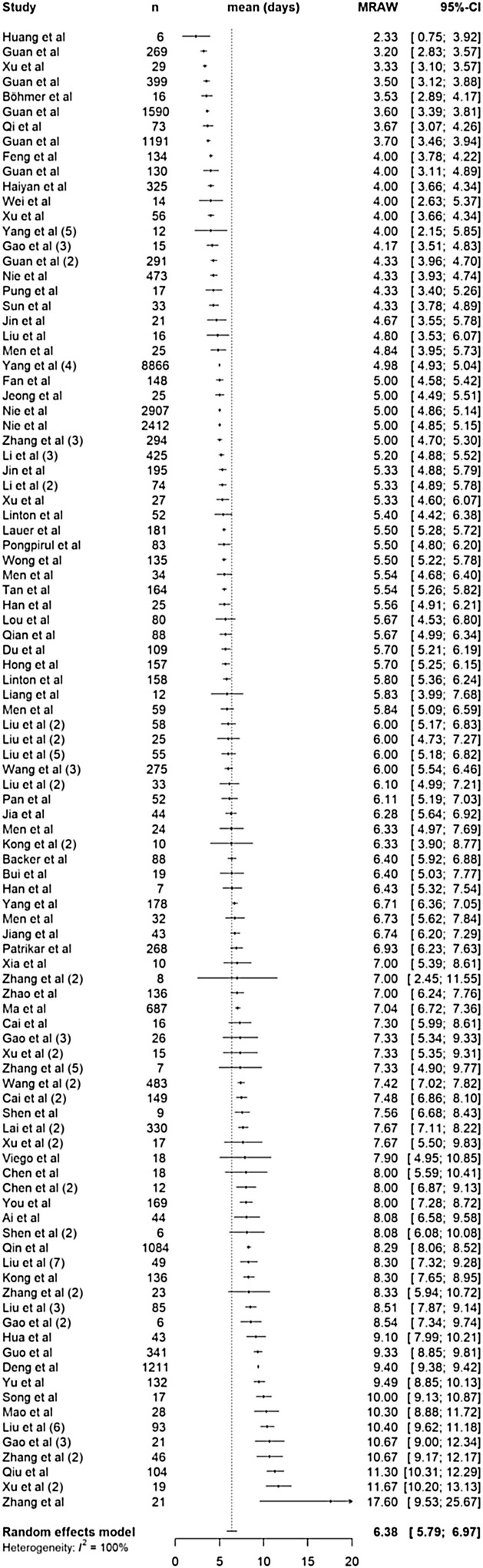
Figure 1 shows that the mean incubation period was 6.38 days 95% CI (5.79; 6.97) ranging from 2.33 to 17.60 days. A range of 15.27 days was described among the studies analyzed. The median incubation period was estimated at 5.41 days 95% CI (4.74; 6.07). There was substantial heterogeneity between the studies (I 2 = 95%).
Figure 1.
Forest plot showing mean incubation period of COVID-19 from included studies.
In meta-regression or by subgroup analysis, this heterogeneity across the studies could be explained by the difference in study design. Shorter incubation periods were reported in cohort compared to case series or modeling studies (P < 0.01). No significant variation was identified by age or by gender. To our knowledge, no study reported infection with the English or South African variant of SARS-CoV-2.
Discussion
The results suggested that the mean incubation period of SARS-CoV-2 is 6.38 days, ranging from 2.33 to 17.60 days. Except for Zhang et al. who reported a longer incubation period, the range was within that quoted by the WHO, i.e. 1–14 days.
Longer incubation periods were observed with case-series compared to cohort studies. The incubation period should be carefully interpreted since the level of evidence differs between study designs. Estimating the range of the incubation time is challenging as it is difficult to pinpoint the exact source of infection and hence the exact timing.
The incubation period might be discussed as an epidemiological parameter and as a link with the early pathogenic process.
With no curative treatment available for SARS-CoV-2 understanding incubation time is paramount for isolating infected cases and quarantining case contacts (Wilder-Smith and Freedman, 2020, Kucharski et al., 2020). SARS-CoV-2 appears to be most contagious around the time of symptom onset; infectivity rapidly decreases thereafter to near-zero after approximately 10 days in mild-moderately ill patients and 15 days in severely-critically ill and immunocompromised patients (Rhee et al., 2020). A quarantine period of at least 10 days would be necessary to limit the transmission of the virus from the exposed cases. In the context of nosocomial cases or confined environments (i.e. classrooms in schools or cruise ships), knowing the incubation period will help to identify exposed individuals.
The incubation time is important for non-pharmaceutical public health interventions such as timely isolation and tracing and quarantining contacts.
The precise estimation of the incubation period is also relevant for exploring early pathogenetic mechanisms with potential links to clinical outcome (Vanhems et al., 2000).
Promptly after its emergence, SARS-CoV-2 was identified to be responsible for human transmission during the incubation period (Jin et al., 2020). Previous studies have suggested that a short incubation period could have an impact on the severity of infection caused by the coronavirus species (Virlogeux et al., 2016). More knowledge about the link between the incubation period and the viral load is essential to tailor clinical decision making and assess COVID-19 severity.
The need for an accurate definition of the incubation period has become urgent to better define cases and the duration of isolation measures. Applying different definitions may hamper case detection and the effectiveness of infection control measures.
Conflict of interest/disclosures
None declared.
Funding/Support
None declared.
Authors’ contribution
CE and PV conceived and designed the study. PV coordinated the study. CE, AS and PL collected the data. MC and CE conducted data analyses. MC designed the Incovid-Lyon website. All authors contributed to data interpretation, the manuscript draft and approved the final version of the manuscript.
Ethical approval
Not applicable.
Acknowledgments
The authors thank Michelle Grange for editing the manuscript.
References
- https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 [accessed 24.01.21].
- Higgins J.P.T., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- https://incovidlyon.shinyapps.io/incubationPeriod/ [accessed 24.01.21].
- Jin Y.H., Cai L., Cheng Z.S., Cheng H., Deng T., Fan Y.P. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Mil Med Res. 2020;7(1):4. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kucharski A.J., Klepac P., Conlan A.J.K., Kissler S.M., Tang M.L., Fry H. Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study CMMID COVID-19 working group. Lancet Infect Dis. 2020;20(10):1151–1160. doi: 10.1016/S1473-3099(20)30457-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishiura H., Mizumoto K., Ejima K., Zhong Y., Cowling B., Omori R. Incubation period as part of the case definition of severe respiratory illness caused by a novel coronavirus. Euro Surveill. 2012;17(42):20296. [Published 18.10.12] [PMC free article] [PubMed] [Google Scholar]
- Rhee C., Kanjilal S., Baker M., Klompas M. Duration of SARS-CoV-2 infectivity: when is it safe to discontinue isolation? Clin Infect Dis. 2020:ciaa344. doi: 10.1093/cid/ciaa1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanhems P., Hirschel B., Phillips A.N. Incubation time of acute human immunodeficiency virus (HIV) infection and duration of acute HIV infection are independent prognostic factors of progression to AIDS. J Infect Dis. 2000;182:334–337. doi: 10.1086/315687. [DOI] [PubMed] [Google Scholar]
- Virlogeux V., Park M., Wu J.T., Cowling B.J. Association between Severity of MERS-CoV Infection and Incubation Period. Emerg Infect Dis. 2016;22(3):526–528. doi: 10.3201/eid2203.151437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- https://www.who.int/news-room/q-a-detail/q-a-coronaviruses [accessed 24.01.21].
- Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020:taaa020. doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]