Abstract
Purpose:
This prospective cohort study examined the association between specific leisure-time activity and mortality risk.
Methods:
Data are from 1999 to 2006 U.S. National Health and Nutrition Examination Surveys and included adults followed through December 31, 2015 (n = 17,938, representing 191,463,892 U.S. adults). Participants reported specific leisure-time activities performed at moderate-to-vigorous intensity. Walking, bicycling, running, dance, golf, stretching, and weightlifting were examined. Cox proportional hazards models (adjusted hazard ratios [aHRs]; 95% confidence intervals [CIs]) assessed the association of individual activities with the risk of all-cause mortality, CVD mortality, and cancer mortality.
Results:
Over a median follow-up of 11.9 years, 3799 deaths occurred. Any leisure-time walking ([aHR], 0.73; 95% CI, 0.66–0.82), bicycling (aHR, 0.73, 95% CI, 0.59–0.91), and running (aHR, 0.70; 95% CI, 0.59–0.84) were associated with lower all-cause mortality compared with no participation in the specific activity. Dance, golf, stretching, and weightlifting were not associated with mortality. Comparable results were observed when activities were categorized as none, less than 60 min/wk, or 60 minutes or more/wk. Walking and running were similarly associated with the risk of CVD mortality.
Conclusions:
Participating in moderate-to-vigorous walking, bicycling, or running may be particularly beneficial for health and longevity.
Keywords: Bicycling, Cardiovascular disease, Neoplasms, Physical activity, Running, Sport, Walking
Introduction
Physical activity is associated with lower risk of morbidity and mortality, including cardiovascular disease (CVD) and certain cancers [1,2]. For the promotion of health and longevity, the 2018 Physical Activity Guidelines for Americans recommends at least 150–300 min/wk of moderate aerobic physical activity, 75–150 min/wk of vigorous, or an equivalent combination of the two, as well as strengthening of major muscle groups [3]. Even at participation levels lower than what is recommended in the 2018 Physical Activity Guidelines, it is evident that physical activity is a protective health behavior [4].
Physical activity is performed as specific types of activities, such as walking or bicycling. Evidence of the protective effects of participation in specific leisure-time activities on mortality is sparse. Studies that have examined activity types have a limited breadth of modalities and have primarily focused on all-cause mortality. Walking, the most common type of leisure-time activity reported by U.S. adults [5], has been the most studied and generally been associated with reduced risk of all-cause mortality [6-9]. Other activities such as bicycling and running have also been associated with reduced risk of all-cause mortality [9,10]. Examinations of the association between these and other types of activities and cause-specific mortality, such as CVD and cancer mortality, are limited [11].
The 2018 Physical Activity Guidelines call for more research on specific types of ambulatory and nonambulatory activities to determine if they comparably contribute to health and for a better understanding of how specific physical activities influence health [12]. The purpose of this study was to examine the association between self-reported participation in specific leisure-time activities and risk of all-cause mortality, CVD mortality, and cancer mortality in a nationally representative sample of U.S. adults.
Methods
Study population
Participants from four separate waves of the U.S. National Health and Nutrition Examination Survey (NHANES) were included (1999–2005; n = 41,474). NHANES is a nationally representative sample of children and adults residing in the United States. More information on the NHANES program can be found at www.cdc.com/nchs/nhanes. A prospective cohort study design was used, in which participants’ physical activity and covariates were ascertained during the NHANES in-person visit with follow-up thorough death certificate records.
Leisure-time physical activity
As part of the NHANES 1999–2006 surveys, participants were interviewed about their physical activity. Participants were asked if they did any moderate or vigorous leisure-time activities for at least 10 minutes over the past 30 days. Those who responded “yes” were asked what specific leisure-time activities they performed. A wide variety of activities could be reported, from aerobics to trampoline jumping [13]. For each reported leisure-time activity, participants indicated how many times they did the activity in the past 30 days and the average duration of the activity. In 2007–2008 NHANES and thereafter, the physical activity questionnaire was changed so that participants were no longer asked about the specific types of leisure-time activities they performed, which, therefore, limited these analyses to 1999–2006 data.
For the purposes of this project, the seven most commonly reported leisure-time activities were examined, chosen because they had at least five events per predictor variable in the final adjusted all-cause mortality models (a cut point determined a priori) [14]. These activities included walking, bicycling, running (combined running, jogging, and treadmill), dance, golf, stretching, and weightlifting. Participants were categorized in two ways: (1) two levels for participation in each activity—any versus none; and (2) average reported time per week spent in each activity as none, less than 60 min/wk, or 60 minutes or more per week.
Mortality
Deaths were ascertained by linkage with the National Death Index (NDI). The leading causes of death were identified using the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) guidelines and grouped into nine categories in the public use data file [15]. In this project, three mortality outcomes were examined: all-cause (mortality from any cause other than accidents), CVD (ICD-10 codes I00–I09, I11, I13, and I20–I51), and cancer (ICD-10 codes C00–C97) [16]. Follow-up was through December 31, 2015.
Covariates
Potential covariates were selected a priori based on previous literature [7,17]. The following characteristics, measured at baseline, were used to describe the population and included as covariates in multivariable models: age in years, gender (male and female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Mexican American, other Hispanic, or other race), education (less than high school diploma, high school graduate, and post-high school), cigarette use (never [smoked fewer than 100 cigarettes in one's life], former [smoked at least 100 cigarettes in one's life but stopped], or current [smoked at least 100 cigarettes in one's life and still smoking]), heavy alcohol consumption (having an average of >2 drinks per day in men and >1 drink per day in women during the previous 12 months—yes, no, or missing [categorized as missing]), and body mass index (calculated from measured weight and height). Self-reported history of pre-existing conditions, including diabetes (no, yes, and borderline [glucose levels are higher than normal but not high enough to be diabetes]), arthritis (no, yes), cancer (no, yes), disability (no, yes), and CVD (no, yes), were also included. Cancer was defined as any reported history of cancer or other malignancy of any kind. Disability was defined as any reported functional limitations because of long-term physical, mental, or emotional problems, such as limitations that prevent working or the amount of work, requiring special equipment to walk, or confusion/memory problems. CVD was defined as reported history of angina/angina pectoris, heart attack, or stroke.
The goal for these analyses was to examine the independent association of each type of leisure-time activity with mortality outcomes; to accomplish this, we controlled for all other activity not under examination operationalized as metabolic equivalent of task (MET) × minutes/week. The control variable for other leisure-time activity was total leisure-time activity MET × minutes/week minus the MET × minutes/week spent in the specific activity under study. Household physical activity was reported as the number of times in the past 30 days and average length of time in minutes that the participant did any tasks around the home or yard for at least 10 minutes that required moderate or greater physical effort. Similarly, transportation physical activity was reported as the number of times and average length of time in minutes that the participant walked or bicycled as part of getting to and from work, school, or to do errands in the past 30 days. Leisure-time, household, and transportation activities were assigned MET scores as recommended by the NHANES Physical Activity Codebook (Supplemental Table 1) [18]. For descriptive purposes, total physical activity MET × hours/week was also calculated as the summed leisure-time, household, and transportation MET × minutes/week divided by 60.
Statistical analyses
Analyses were limited to adults aged 20 years or older at the time of screening. Women who were pregnant at the time of the assessment, and those with missing data for any variables other than heavy alcohol consumption were excluded. To help account for reverse causality, individuals with less than 13 months of follow-up were also excluded [19]. Survey sample weights combined across survey cycles (1999–2006) were used for all analyses, accounting for the complex survey design. Descriptive characteristics of the study population were examined using weighted mean and SD or median and interquartile range for continuous variables, whereas counts and weighted percentages were used for categorical variables.
Poisson regression models were used to estimate the age-adjusted all-cause and cause-specific mortality rate per 1000 person-years for participation in each leisure-time activity examined. Multivariable weighted Cox proportional hazard models were used to estimate the association of the seven leisure-time activities with mortality. First, for each of the leisure-time activities operationalized as none versus any activity, hazard ratios with 95% confidence intervals (CIs) for all-cause mortality, CVD mortality, and cancer mortality were estimated. Second, for each of the leisure-time activities operationalized as none, less than 60 min/wk, and 60 minutes or more per week, hazard ratios with 95% CI for all-cause mortality were estimated. All models were first adjusted for leisure-time MET × minutes/week minus the MET × minutes/week spent in the specific activity under examination (model 1). This was used as model 1 under the assumption that all types of activity will be associated with reduced risk of mortality because they provide physical activity generally. Adjusting for all other activity would, therefore, establish a baseline estimate of the association between participation in each specific activity and mortality. Models were then further adjusted for the aforementioned covariates (model 2). Proportional hazard assumptions were checked by examining log-minus-log plots in the multivariable models; all models were satisfactorily proportional.
For a sensitivity analysis, participants with pre-existing conditions were excluded rather than using pre-existing conditions as a covariate. As such, individuals with pre-existing CVD were excluded in CVD mortality models, whereas individuals with a history of cancer were excluded in cancer mortality models. Data were analyzed in 2019 using STATA 15.1 (College Station, TX). This study was deemed exempt from review by the University of Southern Mississippi Institutional Review Board.
Results
Study population
After excluding participants with missing mortality status (n = 21), women pregnant at baseline (n = 1168), individuals with less than 13 months of follow-up (n = 274), and those with missing data for covariates (n = 910), the final sample was 17,938, representing 191,463,892 U.S. adults aged 20 years or older. Compared with those in the final analytic sample, excluded participants were similarly aged but proportionally more female, less Mexican American or other race, and less educated (data not shown). The median time of follow-up was 11.9 years (range: 1.1–16.75 years). A total of 3799 deaths were recorded over the follow-up period for any cause other than unintentional injuries; 688 were recorded CVD as the underlying cause of death and 815 were recorded malignant neoplasms.
At baseline, the population average age was 46.3 years (SE = 0.27). The majority were female (51%), White (72%), and had a post-high school education (55%; Table 1). In the U.S. population, a median of 17 MET × hours/week of total physical activity was reported (combined leisure-time, household, and transportation METs); participants who were alive at the end of the NDI follow-up period reported a median of 18 MET × hours/week of total physical activity, compared with 5 MET × hours/week among those who died before the end of the NDI follow-up period. Almost two-thirds of the population reported any leisure-time activity. The most commonly reported activity was walking, followed by running and bicycling. Those who were alive at the end of follow-up more commonly reported baseline participation in any leisure-time activity, compared with those who were deceased (67.7% vs. 42.1%, respectively). Each specific leisure-time activity examined was also more commonly reported at baseline among those who were alive at the end of follow-up, compared with those who were deceased. Across leisure-time activities and mortality, the age-adjusted mortality rate was lower for those who participated in the activity compared with those who did not participate (Table 2).
Table 1.
Descriptive characteristics of the study sample by mortality status, NHANES 1999–2006*
| Variable | Alive (n = 14,139) | Deceased (n = 3799) | Total (n = 17,938) |
|---|---|---|---|
| Age (y), mean (SE) | 43.3 (0.25) | 65.7 (0.40) | 46.3 (0.27) |
| Gender, n (%) | |||
| Male | 6970 (48.6) | 2106 (52.4) | 9076 (49.2) |
| Female | 7169 (51.4) | 1693 (47.6) | 8862 (50.8) |
| Race/ethnicity, n (%) | |||
| Non-Hispanic White | 6949 (71.5) | 2322 (77.3) | 9271 (72.3) |
| Non-Hispanic Black | 3.023 (11.0) | 681 (10.9) | 3704 (11.0) |
| Mexican American | 2956 (7.0) | 621 (5.0) | 3577 (6.8) |
| Other Hispanic or other race | 1211 (10.4) | 175 (6.8) | 1386 (9.9) |
| Education, n (%) | |||
| Less than high school diploma | 3783 (16.6) | 1673 (35.1) | 5456 (19.1) |
| High school graduate | 3427 (25.7) | 913 (27.7) | 4340 (26.0) |
| Post-high school | 6929 (57.6) | 1213 (37.1) | 8142 (54.9) |
| Cigarette use, n (%) | |||
| Never | 7538 (52.0) | 1579 (38.3) | 9117 (50.1) |
| Former | 3309 (23.1) | 1438 (36.2) | 4747 (24.9) |
| Current | 3292 (25.0) | 782 (25.6) | 4074 (25.0) |
| Heavy alcohol consumption,† n (%) | |||
| No | 10,414 (74.3) | 2247 (59.4) | 12,661 (72.3) |
| Yes | 918 (7.6) | 197 (6.9) | 1115 (7.5) |
| Missing | 2807 (18.1) | 1355 (33.7) | 4162 (20.2) |
| Body mass index (kg/m2), mean (SE) | 27.6 (0.10) | 27.6 (0.13) | 27.6 (0.09) |
| Pre-existing conditions | |||
| Diabetes, n (%)] | |||
| Yes | 1057 (5.3) | 793 (18.8) | 1850 (7.1) |
| Borderline | 169 (1.0) | 83 (2.2) | 252 (1.2) |
| Arthritis, n (%) | 3026 (19.4) | 1770 (47.2) | 4796 (23.1) |
| Cancer, n (%) | 855 (6.2) | 779 (20.7) | 1634 (8.1) |
| Disability, n (%) | 2849 (18.2) | 1798 (46.3) | 4647 (22.0) |
| CVD, n (%) | 864 (4.8) | 1104 (27.2) | 1968 (7.8) |
| Physical activity measures | |||
| Walking, n (%) | 4561 (36.3) | 788 (23.5) | 5349 (34.6) |
| Walking minute per week among those who reported walking, median (IQR) | 98 (170) | 146 (160) | 98 (180) |
| Bicycling, n (%) | 1520 (13.0) | 177 (5.5) | 1697 (12.0) |
| Bicycling minutes per week among those who reported bicycling, median (IQR) | 60 (90) | 75 (165) | 60 (90) |
| Running, n (%) | 2287 (18.7) | 164 (5.4) | 2451 (16.9) |
| Running minutes per week among those who reported running, median (IQR) | 68 (105) | 65 (88) | 68 (105) |
| Dance, n (%) | 1250 (8.6) | 111 (3.7) | 1361 (8.0) |
| Dance minutes per week among those who reported dance, median (IQR) | 45 (100) | 49 (98) | 45 (98) |
| Golf, n (%) | 648 (6.3) | 112 (4.1) | 760 (6.0) |
| Golf minutes per week among those who reported golf, median (IQR) | 135 (240) | 240 (510) | 135 (240) |
| Stretching, n (%) | 728 (5.6) | 102 (2.8) | 830 (5.2) |
| Stretching minutes per week among those who reported stretching, median (IQR) | 60 (53) | 75 (75) | 63 (61) |
| Weightlifting, n (%) | 1171 (9.95) | 90 (3.3) | 1261 (9.06) |
| Weightlifting minute per week among those who reported weightlifting, median (IQR) | 85 (143) | 79 (101) | 85 (140) |
| Leisure time, n (%) | 8766 (67.7) | 1407 (42.1) | 10,173 (64.3) |
| Leisure-time MET × minutes/week among those who reported leisure-time activity, median (IQR) | 998 (1832) | 788 (1418) | 975 (1815) |
| Household, n (%) | 8687 (68.2) | 1517 (45.4) | 10,204 (65.2) |
| Household MET × minutes/week among those who reported household activity, median (IQR) | 439 (810) | 439 (996) | 439 (810) |
| Transportation, n (%) | 3533 (24.7) | 676 (17.8) | 4209 (23.7) |
| Transportation MET × minutes/week among those who reported transportation activity, median (IQR) | 280 (680) | 420 (780) | 300 (720) |
| Total physical activity MET × hour/week, median (IQR) | 18 (39) | 5 (26) | 17 (38) |
IQR = interquartile range.
Weighted.
Heavy alcohol consumption defined as having an average of >2 drinks per day in men and >1 drink per day in women during the previous 12 months.
Table 2.
Association of participation in specific leisure-time activities with all-cause, CVD, and cancer mortality (n = 17,938),* NHANES 1999–2006
| Activity† | Number of deaths | Mortality rate (95% CI)‡ | Model 1§ HR (95%CI) | Model 2ǁ HR (95% CI) |
|---|---|---|---|---|
| All-cause mortality | ||||
| Walking | ||||
| No | 3011 | 11.52 (10.99, 12.05) | 1.00 | 1.00 |
| Yes | 788 | 6.97 (6.35, 7.58) | 0.60 (0.55, 0.66) | 0.73 (0.66, 0.82) |
| Bicycling | ||||
| No | 3622 | 10.33 (9.86, 10.80) | 1.00 | 1.00 |
| Yes | 177 | 6.44 (5.13, 7.75) | 0.48 (0.39, 0.59) | 0.73 (0.59, 0.91) |
| Running | ||||
| No | 4293 | 10.44 (9.95, 10.94) | 1.00 | 1.00 |
| Yes | 191 | 5.54 (4.72, 6.37) | 0.30 (0.25, 0.36) | 0.70 (0.59, 0.84) |
| Dance | ||||
| No | 3688 | 10.09 (9.63, 10.55) | 1.00 | 1.00 |
| Yes | 111 | 8.39 (6.46, 10.32) | 0.46 (0.35, 0.60) | 0.92 (0.71, 1.20) |
| Golf | ||||
| No | 3687 | 10.17 (9.72, 10.62) | 1.00 | 1.00 |
| Yes | 112 | 7.43 (5.69, 9.16) | 0.71 (0.56, 0.90) | 0.86 (0.66, 1.10) |
| Stretching | ||||
| No | 3697 | 10.19 (9.72, 10.65) | 1.00 | 1.00 |
| Yes | 102 | 6.38 (4.76, 8.00) | 0.67 (0.51, 0.88) | 0.83 (0.62, 1.11) |
| Weightlifting | ||||
| No | 3709 | 10.16 (9.68, 10.65) | 1.00 | 1.00 |
| Yes | 90 | 6.88 (5.17, 8.58) | 0.41 (0.31, 0.53) | 0.89 (0.67, 1.17) |
| CVD mortality | ||||
| Walking | ||||
| No | 684 | 1.99 (1.75, 2.22) | 1.00 | 1.00 |
| Yes | 143 | 1.16 (0.92, 1.39) | 0.57 (0.45, 0.73) | 0.72 (0.55, 0.93) |
| Bicycling | ||||
| No | 788 | 1.76 (1.58, 1.95) | 1.00 | 1.00 |
| Yes | 39 | 1.18 (0.71, 1.65) | 0.50 (0.32, 0.75) | 0.76 (0.50, 1.16) |
| Running | ||||
| No | 802 | 1.80 (1.61, 1.99) | 1.00 | 1.00 |
| Yes | 25 | 0.75 (0.39, 1.12) | 0.22 (0.13, 0.36) | 0.55 (0.33, 0.92) |
| Dance | ||||
| No | 801 | 1.72 (1.55, 1.90) | 1.00 | 1.00 |
| Yes | 26 | 1.68 (0.66, 2.70) | 0.50 (0.27, 0.92) | 1.29 (0.69, 2.39) |
| Golf | ||||
| No | 807 | 1.74 (1.56, 1.92) | 1.00 | 1.00 |
| Yes | 20 | 1.40 (0.68, 2.11) | 0.78 (0.47, 1.29) | 0.92 (0.54, 1.58) |
| Stretching | ||||
| No | 812 | 1.77 (1.59, 1.95) | 1.00 | 1.00 |
| Yes | 15 | 0.67 (1.18, 1.16) | 0.42 (0.19, 0.91) | 0.53 (0.25, 1.12) |
| Weightlifting | ||||
| No | 816 | 1.76 (1.58, 1.94) | 1.00 | 1.00 |
| Yes | 11 | 0.71 (0.10, 1.32) | 0.22 (0.09, 0.55) | 0.53 (0.21, 1.29) |
| Cancer mortality | ||||
| Walking | ||||
| No | 727 | 2.49 (2.22, 2.76) | 1.00 | 1.00 |
| Yes | 218 | 1.81 (1.49, 2.14) | 0.73 (0.60, 0.88) | 0.86 (0.71, 1.05) |
| Bicycling | ||||
| No | 895 | 2.32 (2.08, 2.56) | 1.00 | 1.00 |
| Yes | 50 | 1.64 (1.05, 2.22) | 0.55 (0.39, 0.79) | 0.78 (0.55, 1.11) |
| Running | ||||
| No | 897 | 2.36 (2.12, 2.59) | 1.00 | 1.00 |
| Yes | 48 | 1.37 (0.89, 1.85) | 0.35 (0.24, 0.50) | 0.72 (0.51, 1.02) |
| Dance | ||||
| No | 912 | 2.28 (2.04, 2.52) | 1.00 | 1.00 |
| Yes | 33 | 1.93 (1.23, 2.63) | 0.49 (0.33, 0.73) | 0.98 (0.66, 1.45) |
| Golf | ||||
| No | 909 | 2.26 (2.03, 2.50) | 1.00 | 1.00 |
| Yes | 36 | 2.31 (1.22, 3.39) | 1.00 (0.62, 1.61) | 1.05 (0.65, 1.69) |
| Stretching | ||||
| No | 918 | 2.30 (2.05, 2.54) | 1.00 | 1.00 |
| Yes | 27 | 1.54 (0.72, 2.36) | 0.68 (0.38, 1.20) | 0.83 (0.48, 1.46) |
| Weightlifting | ||||
| No | 922 | 2.30 (2.06, 2.54) | 1.00 | 1.00 |
| Yes | 23 | 1.57 (0.70, 2.44) | 0.42 (0.24, 0.73) | 0.81 (0.46, 1.42) |
Weighted estimates.
Self-reported participation in the specific leisure-time activity at a moderate-to-vigorous intensity for at least 10 min in the past 30 days.
Age-adjusted, per 1000 person-years.
Model 1: adjusted for leisure-time MET × minutes/week minus the MET × minutes/week spent in the specific activity under study.
Model 2: adjusted as in Model 1 and further adjusted age, gender, race, education, cigarette use, heavy alcohol consumption, body mass index, household MET × minutes/week and transportation MET × minutes/week, and history of pre-existing conditions including diabetes, arthritis, cancer, disability, and CVD.
All-cause mortality
Participation in each type of leisure-time activity was associated with a lower risk of death in minimally adjusted models (Model 1; Table 2). Once models were adjusted for other covariates (Model 2), walking, bicycling, and running remained associated with a lower risk of all-cause mortality. When specific leisure-time activities were categorized as none, less than 60 min/wk, or 60 minutes or more per week, mortality risk was lower for walking at both levels of participation compared with no participation, whereas bicycling was associated with lower mortality risk for participation less than 60 minutes, and running was associated with lower mortality risk for participation greater than 60 minutes (Fig. 1, Supplemental Table 2). For walking and bicycling, there was no evidence that participating in 60 minutes or more per week of any type of activity provided a lower risk compared with participating in less than 60 min/wk of said activity. For running, the estimate was lower for less than 60-minute category, but the CIs overlapped for both the less than 60-minute and 60-minute or more categories.
Fig. 1.
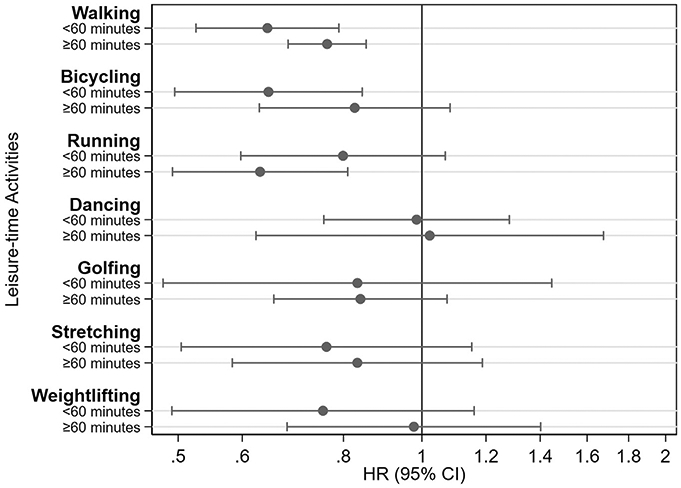
Associations of participating in <60 min/wk or ≥60 min/wk compared with no leisure-time activities with all-cause mortality (n = 17,938)a, NHANES 1999–2006. aAverage reported time spent in each leisure-time activity <60 min/wk or ≥60 min/wk compared with no participation in the activity. Death from any cause other than accidents (unintentional injuries). Weighted estimates, adjusted for age, gender, race, education, cigarette use, heavy alcohol consumption, body mass index, leisure-time MET × minutes/week minus the MET × minutes/week spent in the specific activity under study, household MET × minutes/week and transportation MET × minutes/week, and history of pre-existing conditions including diabetes, arthritis, cancer, disability, and CVD.
CVD mortality
All activities examined, other than golf, were associated with a reduced risk of CVD mortality in minimally adjusted models (Model 1; Table 2). After further adjustment for covariates (Model 2), participation in walking and running remained associated with a lower risk of CVD mortality. Lower CVD mortality risk was observed but not statistically significant for those who bicycled (HR, 0.78; 95% CI, 0.55–1.11), as well as for stretching (HR, 0.53; 95% CI, 0.25–1.12) and weightlifting (HR, 0.53; 95% CI, 0.21–1.29). When individuals with a history of CVD were excluded rather than adjusting for history of CVD, walking was similarly associated with reduced risk of CVD mortality, whereas the association between running and CVD mortality was attenuated (Supplemental Table 3).
Cancer mortality
All activities examined, other than golf and stretching, were associated with a reduced risk of cancer mortality in minimally adjusted models (Model 1; Table 2). After further adjustment for covariates (Model 2), none of the activities examined remained associated with a lower risk of cancer mortality. When individuals with a history of cancer were excluded rather than adjusting for history of cancer, similar results were observed (Supplemental Table 3).
Discussion
In U.S. adults, evidence suggests that participation in walking, bicycling, or running for at least 10 minutes in the past 30 days is associated with a reduced risk of all-cause mortality (excluding injury), whereas walking and running are associated with a reduced risk of CVD mortality. Other activities examined, including dance, golf, stretching, and weightlifting, were not independently associated with the risk of mortality after adjustment for sociodemographic characteristics, history of pre-existing conditions, and other physical activity. This association is evident for walking, regardless of the reported amount of time spent in the activity, but for bicycling and running, time spent in the activity modified the association.
Walking was the most commonly reported type of leisure-time activity and was consistently associated with reduced risk of all-cause mortality and CVD mortality, but not cancer mortality. Walking has previously been examined in association with all-cause and CVD mortality using a smaller sample of the NHANES linked-mortality dataset, with similar findings [7]. Another study using a large U.S. cohort of older adults also found consistent association between walking and all-cause mortality, CVD mortality, and cancer mortality [6]. However, the results from the Whitehall II study found no significant association between walking and mortality after adjusting for covariates [20]. Notable differences between this and the Whitehall II study are the population (London civil servants vs. representative U.S. population) and their inclusion of mortality caused by accidents, which were excluded in the present analysis. In the present study, the estimated risk reduction was comparable with other activities studied, such as bicycling and running, indicating that walking at a moderate-to-vigorous pace may provide similar health benefits compared with other activities that may be considered “more” active or rigorous and less approachable because of physical limitations or equipment requirements.
Running was also consistently associated with reduced risk of all-cause and CVD mortality, but not with cancer mortality. Previous studies have shown mixed results. Lee et al [21]. found that running was associated with a lower risk of both all-cause mortality and CVD mortality, whereas another study using the UK Biobank found running was not associated with all-cause mortality and CVD mortality [10]. Running has been less studied in relation to cancer, but one previous study found no association between jogging and cancer [22], whereas another observed an association between running and reduced risk of brain cancer [23]. A recent meta-analysis indicated that running was associated with lower risk of all-cause, cardiovascular, and cancer mortality [24].
Leisure-time bicycling was associated with reduced risk of all-cause mortality, and similar effect sizes were observed for CVD mortality and cancer mortality. This is in contrast to previous studies that have found no association between recreational bicycling and mortality [10,25]. One study using the UK Biobank examined active commuting by bicycle and the risk of CVD mortality, cancer mortality, and all-cause mortality and found significantly lower risk for all outcomes [26]. However, although the physical activity itself may be similar, other lifestyle factors that contribute to this relationship may differ substantially for active commuting compared with leisure-time bicycling.
Other activities, including dance, golf, stretching, and weightlifting, were not found to be associated with reduced risk of mortality in this study, although there was a suggestion of an association with the risk of CVD for weightlifting and stretching. Few of these activities have previously been examined in relation to mortality risk in cohort studies. Participation in moderate-intensity dancing has previously been found to be associated with lower CVD mortality in a population-based British cohort [27]. One study of Swedish golf club members found that being a member was associated with reduced all-cause mortality compared with non-members [28]. There are numerous differences between the Swedish study and the present study to explain these differing results, including very different populations and unmeasured confounding. The findings of the present study regarding weightlifting are most readily compared with previous findings on strength training. Strength training has been associated with reduced risk of all-cause mortality, but there is limited evidence for reducing the risk for CVD or cancer mortality [29]. Weightlifting is a strength training activity, although how weightlifting was defined in NHANES is unclear—individuals who did participate in strength training exercises may not have reported that activity specifically as weightlifting.
It is unclear why leisure-time walking, bicycling, and running may be associated with reduced risk of mortality above other types of aerobic activity examined here. One explanation is selection bias, in that individuals who are physically able to participate in aerobic activities are more likely to, whereas individuals with limited mobility and associated morbidities may be more likely to report activities such as golf or stretching. Another explanation is that it is plausible that the activities not found to be associated with mortality risk, that is, golfing, dance, and stretching, provide less aerobic activity. In the measurement of golfing cart use was not specified, so it is plausible that the majority of golfers were using a cart and not engaging in consistent aerobic activity. Similarly, dance and stretching may not be as clearly defined to individuals as walking, bicycling, and running might be, so that participation is less straightforward and possibly less consistent in terms of aerobic activity. Finally, it is evident that analyses were underpowered for these other activities, as indicated by the smaller sample sizes.
This study examined specific types of leisure-time activities individually to assess their association with mortality outcomes. However, 67% of this population reported more than one activity, and one participant reported 31 different activities that they engaged in (data not shown). Therefore, for most of the sample, any one activity would not necessarily contribute to their total volume of leisure-time activity, and for this reason, the analyses controlled for all other reported leisure-time activities (Table 3). In some cases, the activity being examined may have contributed a small percentage toward the total leisure-time activity. This may be cause for concern, in that the time participants spent in these activities may not have been sufficient to produce a health benefit. Yet, these activities may by their nature or by the nature of those participating, demand less time. Therefore, we do not think this is a limitation of the study, but rather may be a limitation of the activities themselves.
Table 3.
Number of participants who reported participating in any one or a combination of at least two leisure-time activities examined, NHANES 1999–2006
| Activity* | Walking (n = 5349), n (%) |
Bicycling (n = 1697), n (%) |
Running (n = 2451), n (%) |
Dance (n = 1361), n (%) |
Golf (n = 760), n (%) |
Stretching (n = 830), n (%) |
Weightlifting (n = 1261), n (%) |
Median number of activities reported (IQR) |
|---|---|---|---|---|---|---|---|---|
| Walking | 2013 (32.8) | 735 (45.5) | 1047 (45.3) | 581 (45.4) | 329 (43.9) | 482 (61.3) | 518 (42.1) | 2 (3) |
| Bicycling | 735 (15.7) | 243 (2.26) | 593 (25.8) | 172 (14.7) | 156 (21.7) | 187 (23.2) | 358 (30.7) | 3 (3) |
| Running | 1047 (22.2) | 593 (36.6) | 294 (10.5) | 360 (27.5) | 196 (28.1) | 308 (40.5) | 671 (55.8) | 4 (4) |
| Dance | 581 (10.4) | 172 (9.8) | 360 (12.9) | 286 (2.36) | 56 (8.1) | 179 (20.5) | 186 (13.5) | 3 (3) |
| Golf | 329 (7.62) | 156 (10.9) | 196 (9.9) | 56 (6.11) | 123 (1.43) | 52 (8.4) | 122 (11.6) | 3 (3) |
| Stretching | 482 (9.2) | 187 (10.1) | 308 (12.4) | 179 (13.4) | 52 (7.2) | 67 (0.4) | 259 (19.8) | 4 (3) |
| Weightlifting | 518 (11.0) | 358 (23.3) | 671 (29.8) | 186 (15.3) | 122 (17.5) | 259 (34.5) | 86 (0.8) | 4 (3) |
| Total† | 1 (2) |
Reported percentages are weighted column percentages.
IQR = interquartile range.
Participants reporting only one activity are represented in the junction of the activity column and row. Activity groupings are not mutually exclusive—participants who reported more than two activities are represented in multiple cells.
Entire analytic sample (n = 17,938).
The strengths of this study include the use of a large sample representative of the U.S. adult population, which allowed for examination of specific activities not previously explored, and further allowed for examination of the association of these activities with all-cause and cause-specific mortality. This study also has limitations. Physical activity was assessed in NHANES in bouts of 10 minutes or more, as was recommended in the 2008 Physical Activity Guidelines for Americans [30]. This bout requirement may have led to underreporting of moderate-to-vigorous leisure-time activity. The 2018 guidelines have removed the bout recommendation, in recognition that any length of moderate-to-vigorous activity can provide health benefits [3]. The leisure-time activities examined were chosen a priori to provide sufficient sample size for hazard models of all-cause mortality events with activities categorized as yes/no. Other analyses may have small sample size for some models, producing imprecise estimates. Furthermore, the possibility remains that the sample size for some activities was insufficient to detect a difference in the mortality models. Larger sample sizes are needed to further elucidate the association between different types of leisure-time activity and morbidity and mortality risks.
There is a risk of residual confounding from not having complete information about specific leisure-time activity participation over the lifespan, particularly for individuals who may have taken up or stopped participation after the NHANES physical activity assessment. Over adjustment is an additional concern because prevalent conditions that may be on the causal pathway were controlled for in multivariable models. There is also the possibility of reverse causality, in that individuals who engage in specific types of physical activity may be healthier than those who do not. In an attempt to address this, we excluded participants with less than 13 months of follow-up, but exclusion of longer follow-up times may have been needed to fully account for the potential bias.
Conclusions
Participating in moderate-to-vigorous walking, bicycling, and running showed an inverse association with the risk of all-cause mortality, whereas walking and running were inversely associated with CVD mortality. Participation in other activities examined here, including dance, golf, stretching, and weightlifting, did not show a significant association with mortality risk, but we cannot rule out the lack of association because of the small number of events. Longer follow-up time of this cohort will allow more precision and greater insight into the association between types of activities and mortality risk, as well as allow for stratification by sociodemographic variables. Studies in large and diverse populations should consider measuring physical activity by activity type to fully understand how specific types of physical activity influence health and to explore these activities in relation to incident health events.
Supplementary Material
Acknowledgments
C.C.C. was supported by a National Research Service Award postdoctoral research fellowship (T32-HL007055), funded by the National Institutes of Health National Heart, Lung, and Blood Institute.
References
- [1].Lear SA, Hu W, Rangarajan S, Gasevic D, Leong D, Iqbal R, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet 2017;390(10113):2643–54. [DOI] [PubMed] [Google Scholar]
- [2].Li T, Wei S, Shi Y, Pang S, Qin Q, Yin J, et al. The dose-response effect of physical activity on cancer mortality: findings from 71 prospective cohort studies. Br J Sports Med 2016;50(6):339–45. [DOI] [PubMed] [Google Scholar]
- [3].U.S. Department of Health and Human Services. Physical activity guidelines for Americans. 2nd ed. Washington, DC: US Department of Health and Human Services; 2018. https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf. [Accessed 23 March 2020]. [Google Scholar]
- [4].Arem H, Moore SC, Patel A, Hartge P, Berrington de Gonzalez A, Visvanathan K, et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med 2015;175(6):959–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ham SA, Kruger J, Tudor-Locke C. Participation by US adults in sports, exercise, and recreational physical activities. J Phys Act Health 2009;6(1):6–14. [DOI] [PubMed] [Google Scholar]
- [6].Patel AV, Hildebrand JS, Leach CR, Campbell PT, Doyle C, Shuval K, et al. Walking in relation to mortality in a large prospective cohort of older U.S. adults. Am J Prev Med 2018;54(1):10–9. [DOI] [PubMed] [Google Scholar]
- [7].Evenson KR, Wen F, Herring AH. Associations of accelerometry-assessed and self-reported physical activity and sedentary behavior with all-cause and cardiovascular mortality among US adults. Am J Epidemiol 2016;184(9):621–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Hamer M, Chida Y. Walking and primary prevention: a meta-analysis of prospective cohort studies. Br J Sports Med 2008;42(4):238–43. [DOI] [PubMed] [Google Scholar]
- [9].Kelly P, Kahlmeier S, Götschi T, Orsini N, Richards J, Roberts N, et al. Systematic review and meta-analysis of reduction in all-cause mortality from walking and cycling and shape of dose response relationship. Int J Behav Nutr Phys Act 2014;11:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Oja P, Kelly P, Pedisic Z, Titze S, Bauman A, Foster C, et al. Associations of specific types of sports and exercise with all-cause and cardiovascular-disease mortality: a cohort study of 80 306 British adults. Br J Sports Med 2017;51(10):812–7. [DOI] [PubMed] [Google Scholar]
- [11].Oja P, Titze S, Kokko S, Kujala UM, Heinonen A, Kelly P, et al. Health benefits of different sport disciplines for adults: systematic review of observational and intervention studies with meta-analysis. Br J Sports Med 2015;49(7):434–40. [DOI] [PubMed] [Google Scholar]
- [12].2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S. Department of Health and Human Services; 2018. [Google Scholar]
- [13].Centers for Disease Control and Prevention. NHANES 1999-2000: physical activity - individual activity data documentation, codebook, and frequencies. https://wwwn.cdc.gov/Nchs/Nhanes/1999-2000/PAQIAF.htm#Appendix_1:_Physical_Activity_Codes. [Accessed 19 July 2019].
- [14].Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol 2007;165(6):710–8. [DOI] [PubMed] [Google Scholar]
- [15].National Center for Health Statistics. Office of analysis and epidemiology, public-use linked mortality file, 2015. Hyattsville, Maryland: https://www.cdc.gov/nchs/data/datalinkage/public-use-2015-linked-mortality-file-description.pdf. [Accessed 22 July 2019]. [Google Scholar]
- [16].National Center for Health Statistics. Codebook for the 2015 public-use linked mortality file (LMF). https://www.cdc.gov/nchs/data/datalinkage/public-use-2015-linked-mortality-files-data-dictionary.pdf. [Accessed 22 July 2019].
- [17].Zhao G, Chaoyang L, Ford ES, Fulton JE, Carlson SA, Okoro CA, et al. Leisure-time aerobic physical activity, muscle-strengthening activity and mortality risks among US adults: the NHANES linked mortality study. Br J Sports Med 2014;48:244–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Centers for Disease Control and Prevention. National Health and Nutrition Survey 1999-2000 data documentation, codebook, and frequencies: physical activity (PAQ). https://wwwn.cdc.gov/Nchs/Nhanes/1999-2000/PAQ.htm. [Accessed 14 November 2019].
- [19].Strain T, Wijndaele K, Sharp SJ, Dempsey PC, Wareham N, Brage S. Impact of follow-up time and analytical approaches to account for reverse causality on the association between physical activity and health outcomes in UK Biobank. Int J Epidemiol 2020;49:162–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Sabia S, Dugravot A, Kivimaki M, Brunner E, Shipley MJ, Singh-Manoux A. Effect of intensity and type of physical activity on mortality: results from the Whitehall II cohort study. Am J Public Health 2012;102(4):698–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lee DC, Pate RR, Lavie CJ, Sui X, Church TS, Blair SN. Leisure-time running reduces all-cause and cardiovascular mortality risk. J Am Coll Cardiol 2014;64(5):472–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Schnohr P, Marott JL, Lange P, Jensen GB. Longevity in male and female joggers: the Copenhagen City Heart Study. Am J Epidemiol 2013;177(7):683–9. [DOI] [PubMed] [Google Scholar]
- [23].Williams PT. Reduced risk of brain cancer mortality from walking and running. Med Sci Sports Exerc 2014;46(5):927–32. [DOI] [PubMed] [Google Scholar]
- [24].Pedisic Z, Shrestha N, Kovalchik S, Stamatakis E, Liangruenrom N, Grgic J, et al. Is running associated with a lower risk of all-cause, cardiovascular and cancer mortality, and is the more the better? A systematic review and meta-analysis. Br J Sports Med 2019. 10.1136/bjsports-2018-100493. [DOI] [PubMed] [Google Scholar]
- [25].Sahlqvist S, Goodman A, Simmons RK, Khaw K, Cavill N, Foster C, et al. The association of cycling with all-cause, cardiovascular and cancer mortality: findings from the population-based EPIC-Norfolk cohort. BMJ Open 2013;3(11):e003797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Celis-Morales CA, Lyall DM, Welsh P, Anderson J, Steell L, Guo Y, et al. Association between active commuting and incident cardiovascular disease, cancer, and mortality: prospective cohort study. BMJ 2017;357:j1456. [DOI] [PubMed] [Google Scholar]
- [27].Merom D, Ding D, Stamatakis E. Dancing participation and cardiovascular disease mortality: a pooled analysis of 11 population-based British cohorts. Am J Prev Med 2016;50(6):756–60. [DOI] [PubMed] [Google Scholar]
- [28].Farahmand B, Broman G, de Faire U, Vågerö D, Ahlbom A. Golf: a game of life and death–reduced mortality in Swedish golf players. Scand J Med Sci Sports 2009;19(3):419–24. [DOI] [PubMed] [Google Scholar]
- [29].Saeidifard F, Medina-Inojosa JR, West CP, Olson TP, Somers VK, Bonikowske AR, et al. The association of resistance training with mortality: a systematic review and meta-analysis. Eur J Prev Cardiol 2019;26(15):1647–65. [DOI] [PubMed] [Google Scholar]
- [30].U.S. Department of Health and Human Services. 2008 Physical activity guidelines for Americans. Washington, DC: US Department of Health and Human Services; 2008. https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf. [Accessed 23 March 2020]. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


