1. Introduction
Coronavirus disease 2019 (COVID-19), which was initially reported in Wuhan, China in December 2019, is a novel respiratory disease that was considered a pandemic in March 2020 [1,2]. By October 2020, the disease infected over 39 million people and led to over 1 million deaths in 189 countries, with a case fatality rate of 2.8% [3]. According to the Centers for Disease Control and Prevention (CDC), elderly patients or those with underlying diseases are more seriously affected [4]. In this situation, management of hip fractures, which are common in the elderly, is expected to be difficult. Although much higher early mortality rates of hip fractures in COVID-19 patients have been reported from Europe and the United States [[5], [6], [7], [8], [9]], as of October 11, 2020, there has been no report specifically examining outcomes in patients with hip fractures and COVID-19 infection undergoing surgical intervention in Japan.
There are regional variations in infection and mortality rates associated with COVID-19. Additionally, there are regional variations in early mortality and postoperative care, and other health care systems associated with hip fractures. To develop the management of hip fractures in COVID-19 patients, a large number of cases reported from different regions is needed. We herein report the first case of hip fracture with COVID-19 infection in Japan.
2. Report of the case
An 83-year-old woman experienced left hip pain after a fall from a standing height. She was transferred to the previous hospital by ambulance, and after examinations, left hip fracture was detected. She had severe comorbidities including chronic heart failure, history of cardiac surgery owing to acute myocardial infarction, breast cancer, hypertension, and diabetes mellitus. Although she was planned to undergo surgery at the previous hospital, following a positive preoperative polymerase chain reaction (PCR) test result for COVID-19 (the sample was collected from her nostril), she was transferred to our hospital, which is a facility with an intensive care unit for COVID-19 patients, 3 days after the injury.
After transfer to our hospital, the patient was reassessed carefully. There were no complaints of cough, dyspnea, or taste disorder. However, mild dementia was noted. Before the injury, she was able to walk with a cane. On physical examination, a shortened externally rotated left lower extremity with no peripheral neurovascular deficit was evident. Her vital signs on admission were as follows: blood pressure, 136/88 mmHg; heart rate, 84 beats/min; body temperature, 37.1 °C; respiratory rate, 18 breaths/min; and oxygen saturation with room air, 90%. A chest radiograph did not demonstrate any lung abnormalities except for a cable at the site of the previous cardiac surgery and marked cardiac enlargement. Computed tomography (CT) revealed diffuse trivial pulmonary edema in both lungs (Fig. 1 ). There were no ground grass opacities, crazy-paving patterns, or any other findings that assumed COVID-19 [10]. Radiographs of the left hip revealed a pertrochanteric fracture with features consistent with three-part fragments (AO 31A2.2, Fig. 2 ). Three-dimensional CT showed a large oblique fragment consisting of the greater trochanter and the lesser trochanter (Shoda classification [11]; three-part G-L) (Fig. 3 ). PCR analysis for COVID-19 was again performed on admission, and the test result was positive.
Fig. 1.
Chest computed tomography at the time of admission to the previous hospital shows diffuse trivial pulmonary edema in both lungs.
Fig. 2.
Radiographs of the left hip reveal a trochanteric fracture. (a) Anteroposterior view, (b) lateral view.
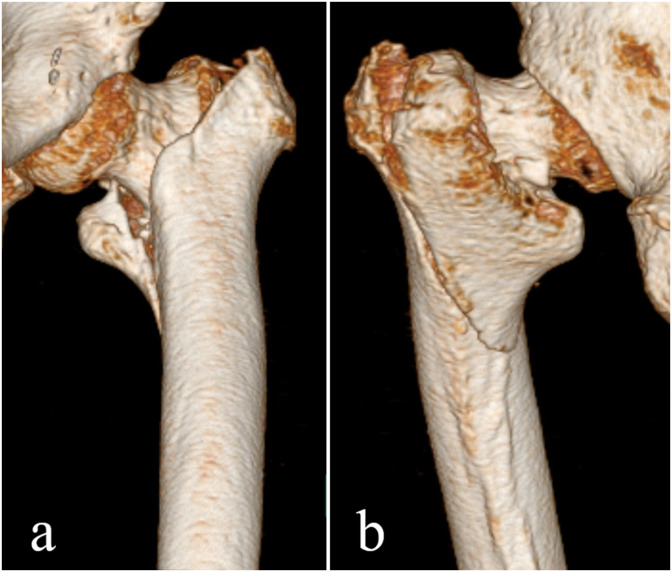
Fig. 3.
Three-dimensional computed tomography shows a large oblique fragment of the greater trochanter including the lesser trochanter. (a) Anterior side, (b) posterior side.
After much consultation with the anesthesiologist, the emergency physician, and the internist, the patient was assessed to be able to tolerate the surgical procedure despite her potential risk factors, such as age, American Society of Anesthesiologists (ASA) grade 3, and diabetes. On the day of admission to our hospital, the patient was taken to the negative-pressure operating room for surgical fixation of her left pertrochanteric fracture. This was undertaken under spinal anesthesia on a fracture table with foot traction applied to the ipsilateral leg and in the lithotomy position of the contralateral lower extremity. Considering the mechanism of spread of the virus, high-level personal protective equipment (PPE) was used according to our institutional guidelines (N95 respirator, goggles, face shield, and plastic gown in addition to standard operating room PPE, Fig. 4 ). A surgical mask was also placed on the patient's face to prevent pathogen transmission. To minimize surgical invasion and the number of people in contact with the patient, the operation was performed by one expert surgeon and one nurse (Fig. 5 ). The operating room was isolated, and the red zone was preloaded with minimal surgical equipment. The implants were brought into the room after communicating with the nurse in the green zone. The posterior bone fragments from the greater trochanter to the lesser trochanter were reduced with a finger, and a nail was inserted. The proximal bone fragment, which was displaced into the medulla, was also reduced to the anatomical position (Fig. 6 ). The surgery time was 26 min, and the blood loss was only 10 ml. Postoperative care was provided in the COVID-19 unit. Weight bearing as tolerated was allowed immediately after the surgery.
Fig. 4.
Personal protective equipment used in this case (N95 respirator, goggles, face shield, and plastic gown).
Fig. 5.
Scene during the surgery. Dr., doctor; Ns., nurse.
Fig. 6.
Postoperative radiographs. (a) Anteroposterior view, (b) lateral view.
The pain at the fracture site resolved immediately. In the treatment time course, a gradual worsening of the respiratory status associated with COVID-19 was observed. Bilateral crazy-paving patterns were observed in the chest CT image during the time course (Fig. 7 ). The serum white blood cell (WBC) count, C-reactive protein (CRP) level, and O2 requirement level peaked on day 7 and then declined (Fig. 8 ). From days 35–42, there was a temporary increase in inflammatory response and poor oxygenation with concomitant illness unrelated to COVID-19, which improved quickly (Fig. 8). The patient survived with no further worsening in her systemic condition resulting from the underlying comorbidities or COVID-19. However, active gait training could not be performed in the COVID-19 unit because there was no rehabilitation room and the physiotherapist's entry was limited to a short period of time. Regulations required a negative PCR test for COVID-19 to be transferred to a rehabilitation hospital, but the PCR test result remained positive for over 1 month postoperatively. She finally tested negative on PCR at 7 weeks postoperatively and was transferred to the next hospital (Fig. 8). The Parker Mobility Score [12] was only 1 point (able to get about the house with help from another person) at the time of discharge from our institution.
Fig. 7.
Five weeks after the surgery, chest computed tomography shows bilateral crazy-paving patterns (black arrows).
Fig. 8.
Treatment progress chart and time course of inflammation markers. PCR, polymerase chain reaction; WBC, white blood cell; CRP, C-reactive protein. ∗required over 2 L/min oxygen, †+ indicates positive; - indicates negative.
The patient and her family were informed that the data, including images from the case, would be submitted for publication, and they provided consent. This case report was approved by the institutional review board.
3. Discussion
COVID-19 has led to a great reduction in the load of fracture patients globally, though the incidence of fragility fractures continues to be unaffected [13]. The establishment of guidelines for the management of hip fractures, which represent fragility fractures under the COVID-19 pandemic, is an urgent concern. However, reports of fracture cases in COVID-19-positive patients remain limited. According to Kumar et al. a total of only 10 studies with 112 patients who were positive for COVID-19 and had fractures were detected in their systematic review at that time [13]. Additionally, information from small studies may not provide clear guidance for fracture treatment during the COVID-19 pandemic. To contribute to the accumulation of information from all over the world, we reported in detail the first case of a COVID-19-positive patient with hip fracture in Japan.
The postoperative mortality rate for hip fracture in COVID-19 pandemic has been reported to be as high as 30% [5,6,9]. However, it remains unclear whether this high mortality rate is caused by COVID-19 itself or by the impact of the fracture or surgical incursion on COVID-19. A report from Spain showed a mortality rate of 10.3% (4/39 cases), even in COVID-19-negative patients with hip fracture [6]. In a multicenter cohort study in the UK, Kayani et al. demonstrated a mortality rate of 10.3% (35/340 cases) in COVID-19-negative patients with hip fracture [9]. In the situation before the COVID-19 pandemic, the 30-day in-hospital mortality rate in Japan was approximately 1% [14], which was much lower than that reported in the United States and Europe [15,16]. In addition, mortality rates for COVID-19-positive patients currently vary by country and region [3]. Even taking into account the differences in the number of COVID-19 tests performed in different countries and in the health care system, the mortality rates reported in Europe and the United States cannot be directly applied to Japan.
Currently, there is no evidence-based effective treatment for COVID-19. The only thing we can control in hip fracture patients with COVID-19 is the management of the fracture. Whether surgical or conservative management is more suitable is still controversial. Although nonoperative management is optional [17], nonoperative management of frail elderly patients with a hip fracture is associated with a poor prognosis [18]. In general, conservative treatment is often selected for patients with a severe general condition that makes surgery impossible, resulting in a high mortality rate [18]. In hip fracture with COVID-19 patients reported from Europe, conservative management is selected only in patients who cannot tolerate the operation [6,19]. Kumar et al. mentioned in their systematic review, that hip fractures in COVID-19 patients was emergency for surgery unless the patient's health condition was very poor, the patient could not tolerate the operation, the risk of death during the operation was very high or postoperative nursing would be very difficult [13]. Actually, according to the multicenter cohort study reported by Kayani et al. the timing of surgery for hip fractures has not changed with or without COVID-19 [9]. Moreover, several reports suggested that surgery for hip fracture in COVID-19 patient improved O2 saturation and assisted respiratory support [5,7,20]. Therefore, urgent surgical management for hip fractures is preferable, even in a patient with COVID-19, if the general condition permits. Kayani et al. reported that the risk factors for increased mortality in patients with COVID-19 undergoing hip fracture surgery included positive smoking status and multiple (greater than three) comorbidities including hypertension, ischemic heart disease, chronic obstructive pulmonary disease, diabetes, and cancer [9]. According to a recent multicenter cohort study referring to predictors of early mortality in patients undergoing surgery with COVID-19, the 30-day mortality rate was 23.8% (higher risk for ASA grades 3–5) [21]. Shang et al. revealed in their systematic review of 31,067 patients with COVID-19 that patients with diabetes mellitus had significantly higher severe infection and mortality rates compared to those without diabetes mellitus (21.4% vs. 10.6% and 28.5% vs. 13.3%, respectively) [22]. In the presented case, despite the risk factors (high age, ASA grade 3, and diabetes mellitus), the patient survived and was discharged.
In the present case, a large oblique fragment of the greater trochanter, including the lesser trochanter, was shown. Unstable trochanteric fractures may exhibit (1) posteromedial large separate fragmentation, (2) a basicervical pattern, (3) a reverse obliquity pattern, (4) a displaced greater trochanter (lateral wall fracture), or (5) the inability to be reduced before internal fixation [11]. Of the above characteristics, three-part G-L-type fracture is considered to have posteromedial large separate fragmentation. For this type of unstable fracture, we have corrected to a positive anterior-posterior cortical position combined with a positive/neutral lateral position on fluoroscopy to obtain cortical support [23]. Although surgical invasion should be minimized in COVID-19 patients, optimal surgical reduction should be performed. Even in the short term, the fracture was stable and there were no symptoms associated with the fracture.
The rehabilitation system is a major issue. In this case, the patient's activity of walking had not recovered owing to the unavailability of a regular rehabilitation room and limited rehabilitation interventions by a physiotherapist in a short period of time. At present, the establishment of a postoperative rehabilitation system for fracture patients with COVID-19 has not been discussed much and remains a major problem. There have been various protocols implemented across individual institutions to both minimize the spread of COVID-19 and protect the workforce. Owing to the mechanism of spread of the virus, there is concern for virus transmission to rehabilitation room personnel. Careful management for each case should be performed with a streamlined team of only essential personnel.
In Japan, most patients with hip fracture are transferred to a hospital specializing in rehabilitation after completing the acute phase [24]. However, there are currently difficulties in transferring patients who are COVID-19 positive, and our neighboring hospitals require a negative PCR test prior to transfer. In the present case, it took 7 weeks for the PCR test result to come back negative, which may have prevented the patient from receiving rehabilitation at a time when intensive rehabilitation was needed. Interhospital consultation and coordination is important for the transfer of COVID-19-positive patients.
At this time, there are no signs that the situation is being brought under control, and it is impossible to predict when the COVID-19 pandemic will subside. Although the development of a vaccine and the discovery of an effective treatment is expected, it may take several years to overcome the crisis. Surgical strategies for hip fractures during the COVID-19 pandemic need to be established, and it will be important to accumulate more cases from various regions of the world.
In summary, we performed surgery for a COVID-19 patient with a hip fracture, which has not been reported in Japan. Although it was a high-risk case, the patient survived. Establishing guidelines for the management of COVID-19-positive patients in terms of surgery, postoperative management, rehabilitation, and transfer is urgently required in Japan. To prepare for future COVID-19 pandemics, it is necessary to accumulate more cases.
Declaration of competing interest
No conflicts of interest were declared by the authors.
Acknowledgements
The authors wish to thank Sachiyo Iwata (Department of Cardiovascular Medicine, Hyogo Prefectural Kakogawa Medical Center), Yoshiki Tohma (Department of Emergency and Critical Care Medicine, Hyogo Prefectural Kakogawa Medical Center), and Yuko Inayama (Division of Diabetes and Endocrinology, Hyogo Prefectural Kakogawa Medical Center) for their excellent supports on the patient. The authors would also like to thank Enago (www.enago.jp/) for the English language review.
References
- 1.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (covid-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020 Apr;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in wuhan, China. Lancet. 2020 Feb;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Covid-19 dashboard. The center for systems science and engineering at Johns Hopkins University (US) https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 [cited 2020 Oct 12]. Available from:
- 4.Coronavirus disease 2019 (covid-19). Centers for Disease Control and Prevention (US) https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html [cited 2020 Oct 12]. Available from:
- 5.Catellani F., Coscione A., D'Ambrosi R., Usai L., Roscitano C., Fiorentino G. Treatment of proximal femoral fragility fractures in patients with covid-19 during the sars-cov-2 outbreak in northern Italy. J Bone Jt Surg Am. 2020 Jun;102(12):e58. doi: 10.2106/JBJS.20.00617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muñoz Vives J.M., Jornet-Gibert M., Cámara-Cabrera J., Esteban P.L., Brunet L., Delgado-Flores L., Camacho-Carrasco P., Torner P., Marcano-Fernández F. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic: preliminary results of the Spanish hip-covid observational study. J Bone Jt Surg Am. 2020 Jul;102(13):e69. doi: 10.2106/JBJS.20.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheung Z.B., Forsh D.A. Early outcomes after hip fracture surgery in covid-19 patients in New York city. J Orthop. 2020 6-JUN;21:291–296. doi: 10.1016/j.jor.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LeBrun D.G., Konnaris M.A., Ghahramani G.C., Premkumar A., DeFrancesco C.J., Gruskay J.A., Dvorzhinskiy A., Sandhu M.S., Goldwyn E.M., Mendias C.L., Ricci W.M. Hip fracture outcomes during the covid-19 pandemic: early results from New York. J Orthop Trauma. 2020 Aug;34(8):403–410. doi: 10.1097/BOT.0000000000001849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kayani B., Onochie E., Patil V., Begum F., Cuthbert R., Ferguson D., Bhamra J.S., Sharma A., Bates P., Haddad F.S. The effects of covid-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Joint Lett J. 2020 Sep;102-B(9):1136–1145. doi: 10.1302/0301-620X.102B9.BJJ-2020-1127.R1. [DOI] [PubMed] [Google Scholar]
- 10.Li J., Yan R., Zhai Y., Qi X., Lei J. Chest ct findings in patients with coronavirus disease 2019 (covid-19): a comprehensive review. Diagn Interv Radiol. 2020 Nov 2 doi: 10.5152/dir.2020.20212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shoda E., Kitada S., Sasaki Y., Hirase H., Niikura T., Lee S.Y., Sakurai A., Oe K., Sasaki T. Proposal of new classification of femoral trochanteric fracture by three-dimensional computed tomography and relationship to usual plain x-ray classification. J Orthop Surg (Hong Kong) 2017 Jan;25(1) doi: 10.1177/2309499017692700. 2309499017692700. [DOI] [PubMed] [Google Scholar]
- 12.Parker M.J., Palmer C.R. A new mobility score for predicting mortality after hip fracture. J Bone Jt Surg Br. 1993 Sep;75(5):797–798. doi: 10.1302/0301-620X.75B5.8376443. [DOI] [PubMed] [Google Scholar]
- 13.Kumar Jain V., Lal H., Kumar Patralekh M., Vaishya R. Fracture management during covid-19 pandemic: a systematic review. J Clin Orthop Trauma. 2020 Jul;11(Suppl 4):S431–S441. doi: 10.1016/j.jcot.2020.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sasabuchi Y., Matsui H., Lefor A.K., Fushimi K., Yasunaga H. Timing of surgery for hip fractures in the elderly: a retrospective cohort study. Injury. 2018 Oct;49(10):1848–1854. doi: 10.1016/j.injury.2018.07.026. [DOI] [PubMed] [Google Scholar]
- 15.Parker M., Johansen A. Hip fracture. BMJ. 2006 Jul 1;333(7557):27–30. doi: 10.1136/bmj.333.7557.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grimes J.P., Gregory P.M., Noveck H., Butler M.S., Carson J.L. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002 Jun 15;112(9):702–709. doi: 10.1016/s0002-9343(02)01119-1. [DOI] [PubMed] [Google Scholar]
- 17.Suzuki Y., Kasashima T., Hontani K., Yamamoto Y., Ito K., Xu L. Conservatively treated femoral intertrochanteric fracture with early asymptomatic novel coronavirus disease 2019 (covid-19): a case report. Geriatr Orthop Surg Rehabil. 2020 28-OCT;11 doi: 10.1177/2151459320969380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loggers S.A.I., Van Lieshout E.M.M., Joosse P., Verhofstad M.H.J., Willems H.C. Prognosis of nonoperative treatment in elderly patients with a hip fracture: a systematic review and meta-analysis. Injury. 2020 Nov;51:2407–2413. doi: 10.1016/j.injury.2020.08.027. [DOI] [PubMed] [Google Scholar]
- 19.Hall A.J., Clement N.D., Farrow L., MacLullich A.M.J., Dall G.F., Scott C.E.H., Jenkins P.J., White T.O., Duckworth A.D. Impact-scot report on covid-19 and hip fractures. Bone Joint Lett J. 2020 Sep;102-B(9):1219–1228. doi: 10.1302/0301-620X.102B9.BJJ-2020-1100.R1. [DOI] [PubMed] [Google Scholar]
- 20.Morelli I., Luceri F., Giorgino R., Accetta R., Perazzo P., Mangiavini L., Maffulli N., Peretti G.M. Covid-19: not a contraindication for surgery in patients with proximal femur fragility fractures. J Orthop Surg Res. 2020 Jul 28;15(1):285. doi: 10.1186/s13018-020-01800-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mortality and pulmonary complications in patients undergoing surgery with perioperative sars-cov-2 infection: an international cohort study. Lancet. 2020 Jul 4;396(10243):27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shang L., Shao M., Guo Q., Shi J., Zhao Y., Xiaokereti J. Diabetes mellitus is associated with severe infection and mortality in patients with covid-19: a systematic review and meta-analysis. Arch Med Res. 2020 Oct;51:700–708. doi: 10.1016/j.arcmed.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chang S.M., Zhang Y.Q., Du S.C., Ma Z., Hu S.J., Yao X.Z., Xiong W.F. Anteromedial cortical support reduction in unstable pertrochanteric fractures: a comparison of intra-operative fluoroscopy and post-operative three dimensional computerised tomography reconstruction. Int Orthop. 2018 Jan;42(1):183–189. doi: 10.1007/s00264-017-3623-y. [DOI] [PubMed] [Google Scholar]
- 24.Hagino H., Endo N., Harada A., Iwamoto J., Mashiba T., Mori S., Ohtori S., Sakai A., Takada J., Yamamoto T. Survey of hip fractures in Japan: recent trends in prevalence and treatment. J Orthop Sci. 2017 Sep;22(5):909–914. doi: 10.1016/j.jos.2017.06.003. [DOI] [PubMed] [Google Scholar]