Abstract
Objectives
A gluten-free (GF) diet is the primary treatment for celiac disease (CD). Gluten is used in schools, particularly in early childhood, art, and home-economics classrooms. This study aimed to measure gluten transfer from school supplies to GF foods that a child with CD may eat. Also, to measure efficacy of washing techniques to remove gluten from hands and tables.
Methods
Five experiments measured potential gluten cross-contact in classrooms: Play-Doh (n=30); baking project (n=30); paper mâché (n=10); dry pasta in sensory table (n=10); cooked pasta in sensory table (n=10). Thirty participants ages 2 to 18 were enrolled. Following activities, gluten levels were measured on separate slices of GF bread rubbed on participant’s hands and table surfaces. Participants were assigned one of three handwashing methods (soap and water, water alone, or wet wipe). Repeat gluten transfer measurements were taken from hands and tables. Gluten measurements made using R-Biopharm R7001 R5-ELISA Sandwich assay.
Results
Paper mâché, cooked pasta in sensory tables, and baking project resulted in rates of gluten transfer far greater than the 20ppm threshold set by Codex Alimentarius Commission. However, Play-Doh and dry pasta resulted in few gluten transfers to GF bread >20ppm. Soap and water was consistently the most effective method for removing gluten, although other methods proved as effective in certain scenarios.
Conclusions
The potential for gluten exposure at school is high for some materials and low for others. For high-risk materials, schools should provide GF supplies and have a robust strategy to prevent gluten cross-contact with food.
Keywords: celiac disease, gluten-free diet, school, classroom, gluten cross-contact
INTRODUCTION
Celiac disease (CD) is a chronic health condition characterized by an immune response to gluten ingestion(1), with a global prevalence of 1 percent(2) that is treated with a strict gluten-free diet (GFD). There are approximately 74 million school-age children in the United States, thus an estimated 740,000 school children who require a GFD for CD. Although many of these children remain undiagnosed or misdiagnosed, the number of children with CD and other conditions that require avoiding gluten (e.g., some elimination diets for eosinophilic esophagitis, non-celiac gluten sensitivity, and wheat allergy)(3) continues to increase, there is a growing need for learning environments to properly manage students with CD. Gluten is ubiquitous not only in school cafeterias (e.g., cereals, bread, cookies/snacks), but also in classrooms. Many common school supplies, including modeling clay (e.g., Play-Doh), paper mâché, and pasta (cooked and uncooked), contain gluten and gluten-containing flours are commonly used in home-economics classrooms. Understanding how children may be exposed to gluten within the school environment and how this may be mitigated would facilitate safe participation for children who require a GFD in learning activities.
Fear of gluten exposure is common among CD patients and their parents, and often leads to hypervigilance and decreased quality of life(4). The Codex Alimentarius Commission defines GF as less than 20 parts per million (ppm) gluten(5). It is generally believed that the gluten protein is too large to be absorbed through the skin; thus, touching gluten-containing materials should not pose a problem for children with CD unless they have a contact allergy. However, there have been no investigations to date reporting the levels of gluten in school supplies or how much gluten may transfer from those school supplies to foods that a child with CD may eat. Therefore, there is great variation in how CD is managed in the school setting. With limited data regarding the potential for gluten exposure in the classroom environment, parents of children with CD often fear that their child will be exposed to gluten at school and experience painful or embarrassing symptoms(6, 7). To overcome these concerns and perhaps exaggerated perceived risk of gluten exposure, parents often advocate for precautions that may at times unnecessarily restrict their child’s participation(8). This may lead to confusion, particularly when other parents acknowledge that their child lives in a gluten-filled world and needs to learn to adapt to keep themselves safe in any environment in which they find themselves. As more children are diagnosed with CD and other conditions requiring a GFD, schools are increasingly challenged with managing GFDs in the face of conflicting demands and limited evidence regarding the true risk associated with common classroom activities.
The primary aim of this study was to determine the quantity of gluten transfer from gluten-containing school supplies to GF bread via a child’s hands or table workspaces. A secondary aim was to determine the best method(s) for removing gluten from hands and tables.
METHODS
Study Design
Healthy children aged 2 to 18 without CD or another health condition necessitating gluten avoidance participated in simulated classroom activities using gluten-containing materials. Trained observers used a rating sheet to document each participant’s interaction with school materials for each activity (e.g., enthusiasm, duration, and messiness), to ensure adherence to the planned experimental design and to account for potential outliers in the data. Results are reported as 95% confidence intervals based upon binomial distribution. This approach explicitly accounts for both the range of possible estimates compatible with the data and the lack of precision inherent in small samples. This study was approved by Children’s National Medical Center IRB.
Play-Doh:
Each participant played with a three-ounce container of wheat-based modeling clay/dough (Play-Doh, Hasbro, Pawtucket, RI) on a table for five minutes. The concentration of gluten in Play-Doh was also determined.
Home-Economics Baking Project:
Each participant used a rolling pin to roll out wheat flour-based cookie dough (Toll House® refrigerated chocolate chip cookie dough, Nestlé®, Arlington, VA) on a table dusted with wheat flour, then cut the dough with cookie cutters and transferred the cookies to a baking sheet.
Paper Mâché Art Project:
Participants used newspaper and adhesive made from wheat flour, salt, and water to create a balloon bowl. Strips of newspaper were dipped into the paper mâché and wrapped around one end of the balloon. The activity was completed once participant hands appeared dry (approximately 2 to 5 minutes).
Dry Pasta Sensory Table:
Participants played with dry wheat spaghetti (Barilla USA, Northbrook IL) in a sensory table for 5 minutes.
Cooked and Dyed Pasted in a Sensory Table:
Wheat spaghetti (Barilla USA, Northbrook IL) prepared according to manufacturer instructions was tossed with GF food coloring. Participants played with the dyed pasta in a sensory table for 5 minutes.
Hand and table surface washing scenarios:
Participants in the Play-Doh and home-economics baking scenarios were randomly assigned one of three hand and table washing methods (soap and water, water alone, or wet wipe (Wet Ones Antibacterial Hand Wipe, Edgewell, North Bergen, NJ). Those assigned to soap and water or water alone were observed washing their hands for the length of time it took them to sing the song “Happy Birthday.” Children who used water dried their hands on a paper towel. Children in the wet wipe group were instructed to wipe the palm and dorsum of both hands and all fingers with the wet wipe, but no time was assigned to this method of washing. Cleaning was supervised and documented by study staff. To simulate an adult cleaning tables in a classroom environment, study staff washed the table surfaces using the assigned washing method, then rubbed the table with a slice of GF bread.
Gluten transfer from hands assay:
Upon completing each timed classroom activity or washing activity, children rubbed their hands with a fresh slice of GF bread (Artisan White Bread, Schar, Lyndhurst, NJ). Both sides of each slice of bread were rubbed on the palm and fingers of both hands. The entire slice of bread was homogenized and assayed for gluten.
Environmental gluten transfer assay:
After each participant completed the activity, study staff with clean and gloved hands rubbed a fresh slice of GF bread (Artisan White Bread, Schar, Lyndhurst, NJ) on the table surface used by the participant. The entire slice of bread was homogenized and assayed for gluten.
Complete Clean Technique Between Activities
To ensure gluten was completely removed from participant hands prior to each scenario, children washed their hands with soap and water while singing “Happy Birthday,” dried them with clean paper towel, rinsed their hands under running tap water while singing an encore of “Happy Birthday,” then dried their hands again with a clean paper towel. Tables were thoroughly cleaned by study staff using a laboratory-grade cleaning solution containing 70% ethanol (Ethanol Pure 200 Proof, Decon Labs). The efficacy of these cleaning methods was verified using GF bread rubbed on children’s hands and surfaces. None of the control samples contained detectable amounts of gluten.
Determination of Gluten Content
For the Play-Doh and baking activities, all samples were individually packaged in clear plastic bags with random sample numbers. Gluten was extracted from homogenized samples using a cocktail solution. Gluten concentration was determined using the R5 sandwich ELISA (R7001, R-Biopharm, Darmstadt, Germany), which has a limit of detection of 5 ppm gluten. The R5 Mendez ELISA method is endorsed by the Codex Alimentarius Commission as a type 1 method for the detection of gluten in foods(5). The assay was performed by Bia Diagnostics laboratories (Colchester, Vermont) for the Play-Doh and baking activities and by the Children’s National Medical Center Research Laboratory for the paper mâché, dry pasta, and cooked and dyed pasta activities. The latter samples were run in in duplicate according to manufacturer instructions.
RESULTS
A total of 30 children (50% female) without CD or gluten intolerance were recruited. The median age was 8 years (range 2.5–18 years). All children participated in the Play-Doh and home economics-baking activities. Based upon interim data analysis, only 10 children participated in the paper mâché and sensory table activities. One sample from the home-economics project hand transfer was unable to be analyzed. Table 1 shows the range of gluten levels detected on the GF bread samples during each classroom activity. Table 2 shows the range of gluten levels detected on the GF bread samples after hand or surface washing.
Table 1.
Range of gluten levels detected on GF bread samples immediately following each classroom activity. Samples containing less than 20ppm gluten are eligible for a GF label under the Codex Alimentarius Commission standard.
| Classroom Activity | No Gluten <5ppm |
Gluten Detected 5–10 ppm |
Gluten Detected 10–20 ppm |
Gluten Detected >20ppm |
||||
|---|---|---|---|---|---|---|---|---|
| N (%) | 95% CI | N (%) | 95% CI | N (%) | 95% CI | N (%) | 95% CI | |
| Play-Doh | ||||||||
| Transfer from Hands (n=30) |
27 (90%) | 72–97% | 1a (3%) | 0.1–19% | 2b (7%) | 1–24% | 0 (0%) | 0–14% |
| Transfer from Table (n=30) |
24 (80%) | 61–92% | 3c (10%) | 3–28% | 1d (3%) | 0.1–19% | 2e (7%) | 0.1–19% |
| Home Economics Baking Project | ||||||||
| Transfer from Hands (n=29) |
0 (0%) | 0–15% | 0 (0%) | 0–15% | 0 (0%) | 0–15% | 29f (100%) | 85–100% |
| Transfer from Table (n=30) |
0 (0%) | 0–14% | 0 (0%) | 0–14% | 0 (0%) | 0–14% | 30g (100%) | 86–100% |
| Paper Mâché | ||||||||
| Transfer from Hands (n=10) |
0 (0%) | 0–34% | 0 (0%) | 0–34% | 0 (0%) | 0–34% | 10h (100%) | 66–100% |
| Dry GC Pasta | ||||||||
| Transfer from Hands (n=10) |
9 (90%) | 54–99% | 0 (0%) | 0–34% | 1i (10%) | 0.5–46% | 0 (0%) | 0–34% |
| Cooked and Dyed GC Pasta | ||||||||
| Transfer from Hands (n=10) |
0 (0%) | 0–34% | 0 (0%) | 0–34% | 1j (10%) | 0.5–46%% | 9k (90%) | 54–99% |
7.8ppm;
10.1ppm, 13.3ppm;
5.2ppm, 5.5ppm, 5.8ppm;
10.7ppm;
75.6ppm, >84ppm;
21.1ppm, 59ppm, 76.2ppm, 80.1ppm, remainder >84ppm;
all >84ppm;
all >84ppm;
10.2ppm;
13ppm;
26ppm, remainder >84ppm
Table 2.
Range of gluten levels detected on the GF bread samples after washing. Samples containing <20ppm gluten are eligible for a GF label under the Codex Alimentarius Commission standard.
| Classroom Activity | Gluten Undetectable <5ppm |
Gluten Detected 5ppm–10ppm |
Gluten Detected 10–20 ppm |
Gluten Detected >20ppm |
||||
|---|---|---|---|---|---|---|---|---|
| N (%) | 95% CI | N (%) | 95% CI | N (%) | 95% CI | N (%) | 95% CI | |
| Play-Doh | ||||||||
| (Hands) N (%) | 30 (100%) | 86–100% | 0 (0%) | 0–14% | 0 (0%) | 0–14% | 0 (0%) | 0–14% |
| Soap and Water | 10 | 0 | 0 | 0 | ||||
| Water Alone | 10 | 0 | 0 | 0 | ||||
| Wet Wipes | 10 | 0 | 0 | 0 | ||||
| (Table) | 30 (100%) | 86–100% | 0 (0%) | 0–14% | 0 (0%) | 0–14% | 0 (0%) | 0–14% |
| Soap and Water | 10 | 0 | 0 | 0 | ||||
| Water Alone | 10 | 0 | 0 | 0 | ||||
| Wet Wipes | 10 | 0 | 0 | 0 | ||||
| Home Economics Baking Project | ||||||||
| Hands | 19 (63%) | 44–79% | 7a (23%) | 11–43% | 3b (10%) | 3–28% | 1c (3%) | 0.2–19% |
| Soap and Water | 9 | 0 (0%) | 0 (0%) | 1 (10%) | ||||
| Water Alone | 7 | 1 (10%) | 2 (20%) | 0 (0%) | ||||
| Wet Wipes | 3 | 6(60%) | 1 (10%) | 0 (0%) | ||||
| (Table) | 8 (27%) | 13–46% | 5d (17%) | 6–35% | 7e (23%) | 11–43% | 10f (33%) | 18–53% |
| Soap and Water | 6 | 1 (10%) | 2 (20%) | 1 (10%) | ||||
| Water Alone | 0 | 0 (0%) | 2 (20%) | 8 (80%) | ||||
| Wet Wipes | 2 | 4 (40%) | 3 (30%) | 1 (10%) | ||||
6.3ppm, 8ppm, 8ppm, 8.1ppm, 8.5ppm, 8.6ppm, 10ppm;
12.3ppm, 12.5ppm, 19.2ppm;
30.7ppm;
6ppm, 6ppm, 6.6ppm, 7.3ppm,7.5ppm;
10.1ppm,10.9ppm, 11ppm, 13.6ppm, 16.5; 17.6ppm, 18.4ppm;
21.1ppm, 22.1ppm, 36.3ppm, 80.7ppm, remainder >84ppm
Play-Doh:
The concentration of gluten in a three-ounce container of Play-Doh was 32,253 ppm gluten. Nevertheless, all 30 bread samples rubbed on the participants hands after the five-minute play activity tested below 20 ppm gluten. Only 2 of the 30 bread slices rubbed on the soiled, unwashed table workspaces resulted in transfer levels above 20 ppm (Figure 1). Both of these samples had visible pea-sized pieces of Play-Doh adhered to the GF bread. All samples tested after washing (30 hand samples and 30 table samples) resulted in GF bread slices with less than 5 ppm gluten, regardless of the washing method (Figure 2).
Figure 1.
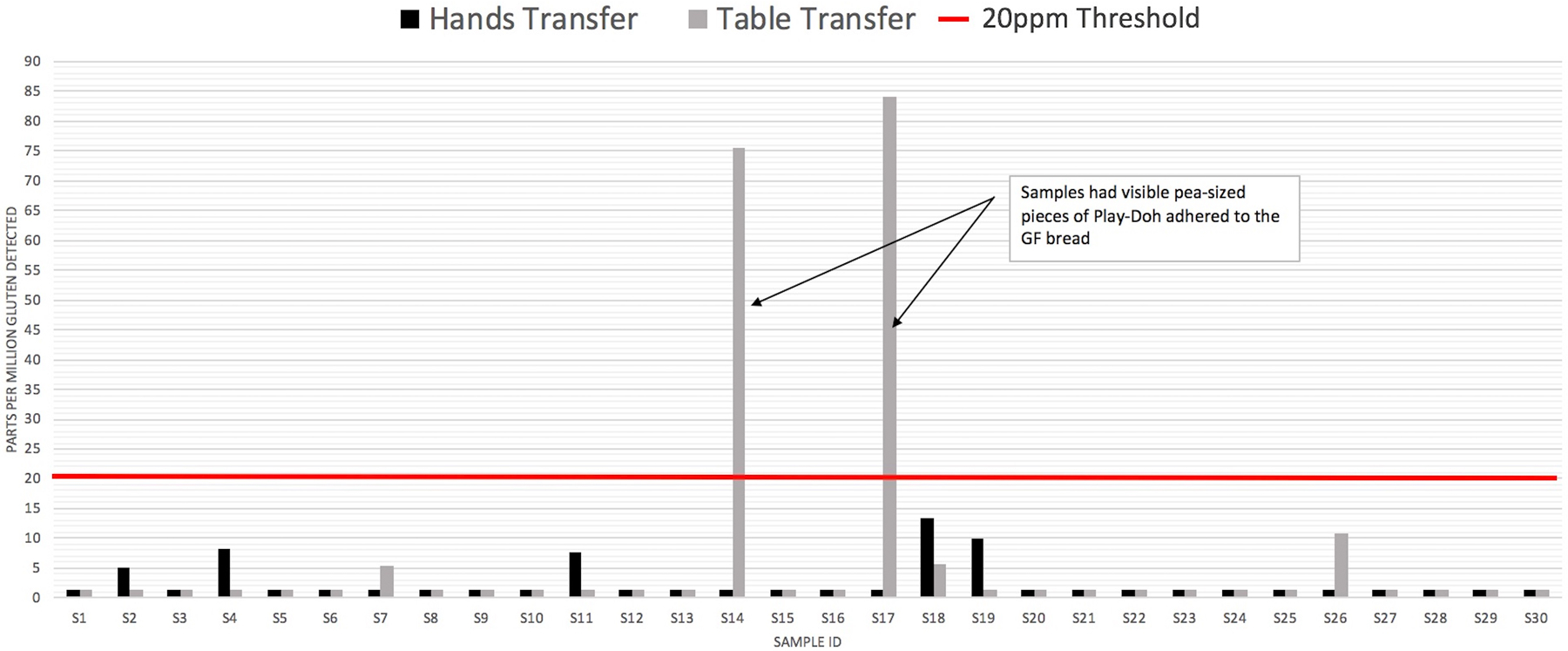
Play-Doh: Transfer from Hands and Table to Gluten-Free Bread
Figure 2.
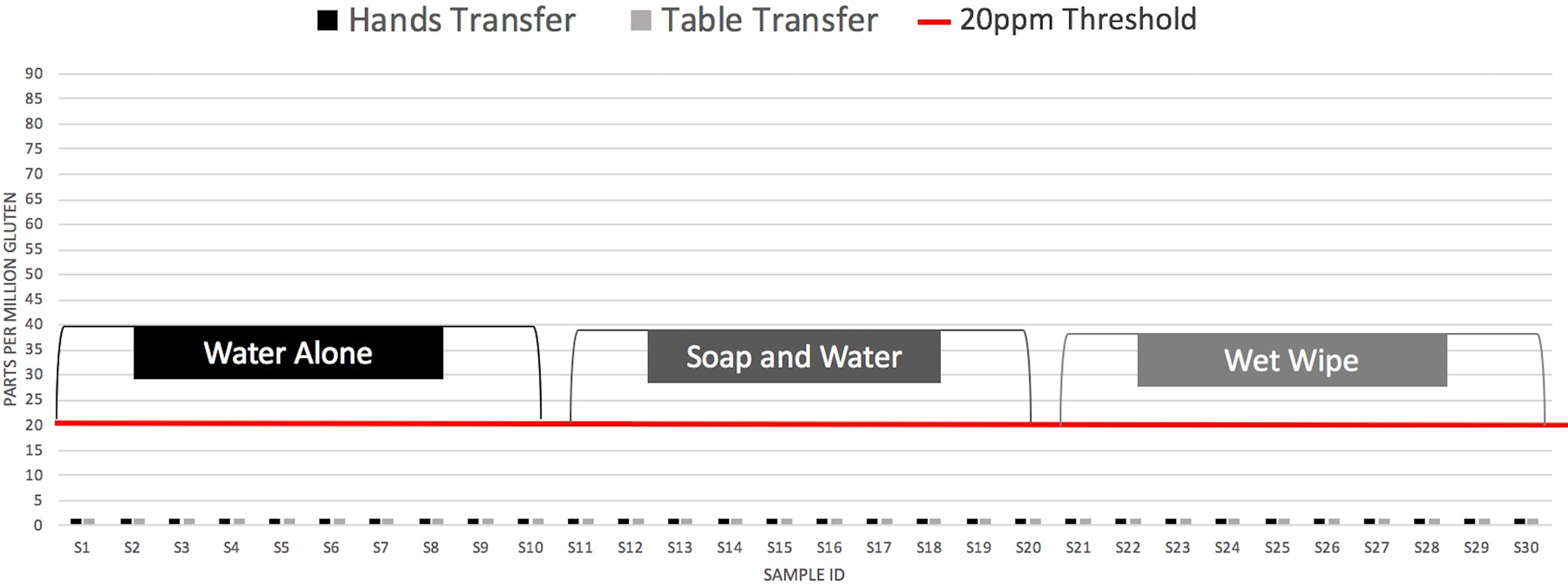
Play-Doh Transfer from Hands and Table After Washing
Home Economics Baking Project:
In contrast to the Play-Doh activity, all 29 GF bread slices (one sample was lost during processing) rubbed on participant hands after the home economics cooking activity resulted in gluten transfers of greater than 20 ppm, with most of the samples exceeding the upper limit of quantification of greater than 84 ppm. The same was true for all 30 bread samples rubbed on the soiled, unwashed cooking workspaces. Nevertheless, all three washing methods effectively removed gluten from participant hands, with the exception of one piece of bread that contained 30.7 ppm gluten after being rubbed on the hands of a 4-year-old who washed their hands with soap and water. Observation notes indicated that this child had visibly more flour adhered to their body, including on clothing, face, and both forearms. Variable amounts of gluten were transferred from the tables after washing, with 10 of the 30 slices of bread rubbed on the cleaned surface containing greater than 20 ppm gluten. Eight of the 10 gluten transfers occurred when water alone was used, while just one transfer occurred in each of the soap and water and wet wipe groups (Table 2).
Paper Mâché Balloon Art Project:
Similar to the baking project, gluten transfer from participants dried hands after the paper mâché balloon art project activity resulted in gluten transfer to the slices of GF bread of greater than 20 ppm gluten, with most of the samples testing greater than 84ppm.
Dry Pasta in a Sensory Table:
All 10 GF bread samples rubbed on participant hands after the five-minute play with dry pasta in a sensory table contained less than 20 ppm gluten, with 9 out of 10 samples testing below 5 ppm.
Cooked and Dyed Pasta in a Sensory Table:
Nine of the 10 bread samples rubbed on participant hands after the five-minute play with cooked and dyed pasta in a sensory table contained greater than 20 ppm gluten, with 8 out of 10 exceeding the upper limit of quantification of greater than 84 ppm gluten. The one sample that tested below the 20 ppm threshold was from a 4-year-old participant who described the pasta material as “feeling like gross worms.” There was a visibly less pasta residue on this child’s hands compared to the other participants.
DISCUSSION
Quantification of gluten transferred from school supplies to GF foods provides empiric evidence to guide strategies to provide a safe and inclusive learning environment for children with CD and others who require a GFD. In this novel study of gluten transfer from school supplies during common classroom activities, we found that school supplies that are dry had very low gluten transfers while materials that were wet and/or sticky tended to cling to the hands of children and table surfaces. Specifically, Play-Doh and dry pasta were associated with the lowest risk of gluten exposure. When gluten transfer to GF bread was detected, the levels were less than the 20 ppm threshold so long as there was no visible Play-Doh. In contrast, there was substantial gluten transfer resulting in levels greater than 20 ppm after the baking, paper mâché, and cooked pasta activities, all of which utilized wheat flour-based materials. Furthermore, a child who vigorously or exuberantly interacts with gluten-containing materials may experience a greater risk of gluten transfer, as we observed during the baking and cooked pasta activities.
Going to school should be an exciting time for children as they are immersed in learning new academic skills and developing social relationships. A recent study by Shull et al(9) found that school functioning is impacted by untreated CD, with over half of patients in the study experiencing significant impairment in school performance, such as missing school or being unable to concentrate or keep up with schoolwork. Children diagnosed with CD early (between ages of 0–15) who maintain a strict GFD may experience no effect on academic performance(10), whereas those with undiagnosed, untreated CD may have lower educational attainment(11). Nevertheless, there may be a social and emotional toll of CD and following a GFD. Children and adolescents frequently report feeling left out and feeling different from their peers because they had to eat something they brought from home or they had to “say no”(12, 13) and that they often felt isolated because adults did not know the appropriate strategy to manage a child with CD. Thus, effective management of a GFD at school requires not only avoiding gluten ingestion, but also considering the social and emotional needs of the child.
There are several strategies that may be implemented in schools to mitigate gluten transfer during high-risk activities such as paper mâché, sensory tables with cooked pasta, and home-economics projects with flour. Traditionally, paper mâché is made from water, white flour, and salt; however, white flour may be replaced with a GF product (e.g., rice flour, cornstarch) to achieve similar results in an environment safe for students with CD. Mainstream companies are producing corn and rice-based GF pastas that can be substituted for gluten-containing pasta and these are increasingly available in grocery stores. Home-economics projects with wheat flour may be more difficult to adapt; however, it can be done. Miller et al(14) found that GF food could be safely prepared concurrently with wheat-based flour in a shared commercial kitchen space provided that proper sanitation methods are followed (clean surfaces, equipment, and utensils) and the GF foods were at least 2 meters (6.56 feet) away from areas where gluten-containing flours were used. A dedicated gluten-free zone may be more important than dedicated equipment as washing kitchen utensils and pots with soap and water or water alone is sufficient to remove gluten(15). Further studies are needed to establish whether these practices can be safely adopted in a classroom setting as well as a commercial kitchen.
Strategies focused upon ensuring adequate hand-washing and cleaning of surfaces may be appropriate when school supplies with a low-risk of gluten transfer are used. Given the consistent data on the very low possibility of significant gluten transfer from Play-Doh and dry pasta to GF food products, students may be able to use them so long as there is no concern that the child will eat the gluten-containing school supplies. Regardless of the low gluten transfer risk, children should be required to wash their hands following use, and workspaces should be cleaned to prevent transfer, especially if food will be consumed later in the same space. Our data showed that soap and water, water alone, or wet wipes were sufficient to create safe surfaces after Play-Doh activities.
Limitations
Acknowledged limitations of our study include subsampling of homogenized foods and relatively small sample size for some scenarios. Nevertheless, even with these small sample sizes, the lower bound of the 95% confidence interval was 85% which allowed for identification of high-risk activities. Furthermore, we did not test the level of gluten possibly transferred from low risk supplies to the hands of children with CD nor how much could be consumed from actions like thumb sucking and nail biting. Similarly, more data is needed regarding hand and surface washing after paper mâché and pasta activities.
CONCLUSIONS
Gluten at school is often a source of anxiety for children with CD and their parents(6, 16). Our data shows that some common school activities pose a higher risk of gluten exposure than others, especially those that utilize wet materials and wheat flour. However, the data also illustrates that the risk of gluten ingestion associated with use of materials like Play-Doh and dry pasta may have been historically overestimated and that children with CD may be able to use these materials safely in the classroom environment, provided that the materials themselves are not consumed. Furthermore, hand washing and cleaning of surfaces are generally effective strategies to mitigate the risk of gluten transfer. It is important for patients with CD and their parents to continue to work closely with school administrators, teachers, and other educators to develop appropriate reasonable accommodations to mitigate the risk of gluten transfer in the classroom so that students can participate fully in all learning and social activities. Additional rigorous studies are needed to evaluate risk of gluten transfer in home-economics and cooking classrooms. Such studies are needed to develop evidence-based practices for students participating in lessons involving food preparation that balance the risk of gluten exposure with the desire for an inclusive learning environment.
| What is Known | What is New |
|---|---|
| • Maintaining a strict gluten-free diet is challenging for children with celiac disease. • Some school supplies are made from gluten-containing materials. • To date, there is no data documenting potential levels of gluten exposure in school classrooms. |
• Paper mâché, cooked pasta, and home-economics baking activities may present a high risk of gluten exposure • Use of Play-Doh and dried pasta may present a very low or negligible risk of gluten exposure. • Based on our data, schools may consider providing gluten-free materials for students with celiac disease in scenarios that present a high-risk of gluten transfer. • Robust cleaning methods may be needed to prevent gluten transfer from common classroom materials. |
Other Acknowledgements:
Patients and families from the Celiac Disease Program at Children’s National Medical Center, most notably the siblings of many celiac patients who participated in the study activities. The many volunteers who helped with the study day activities including: Amy Smith, Rowan Smith, Maureen Basye, Brandon Weisbrod, Eric Weisbrod, Leo Weisbrod, Chloe Lerner, Alexa Lerner, Christopher Latourrette, Owen McMahon, Judith Ross, Sophia Ross, Ella Ross, and Chloe Ross.
Funding Source:
Supported by philanthropic gifts from the Celiac Disease Foundation, Dr. SCHAR USA, and Bia Diagnostics. JAS is supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number K23DK119584. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Clinical Trial Registration: None (not applicable)
Disclosures: JAS has served on an advisory board of Takeda Pharmaceuticals and received research support from Cour Pharma, Glutenostics, and the Celiac Disease Foundation. The other authors have no conflicts of interest to disclose.
References
- 1.Lebwohl B, Sanders DS, Green PHR. Coeliac disease. Lancet (London, England) 2017; 6736:1–12. 10.1016/S0140-6736(17)31796-8 [DOI] [PubMed] [Google Scholar]
- 2.Singh P, Arora A, Strand TA, et al. Global Prevalence of Celiac Disease: Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol 2018. 10.1016/j.cgh.2017.06.037 [DOI] [PubMed]
- 3.Almallouhi E, Absah I. Gluten-free diet among school-age children in Olmsted County, Minnesota. Avicenna J Med 2017; 7:171 10.4103/ajm.ajm_42_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolf RL, Lebwohl B, Lee AR, et al. Hypervigilance to a Gluten-Free Diet and Decreased Quality of Life in Teenagers and Adults with Celiac Disease. Dig Dis Sci 2018; 63:1438–1448. 10.1007/s10620-018-4936-4 [DOI] [PubMed] [Google Scholar]
- 5.Codex Alimentarius Comission. Codex standard for foods for special dietary use for persons intolerant to gluten. Codex stan 2008:3–5.
- 6.Meyer S, Rosenblum S. Daily Experiences and Challenges Among Children and Adolescents with Celiac Disease: Focus Group Results. J Pediatr Gastroenterol Nutr 2017:1 10.1097/MPG.0000000000001635 [DOI] [PubMed]
- 7.Cederborg A-C, Hultman E, Magnusson KF. Living with children who have coeliac disease: a parental perspective. Child Care Health Dev 2011:1–6. 10.1111/j.1365-2214.2011.01273.x [DOI] [PubMed] [Google Scholar]
- 8.Roma E, Roubani A, Kolia E, et al. Dietary compliance and life style of children with coeliac disease. J Hum Nutr Diet 2010; 23:176–82. 10.1111/j.1365-277X.2009.01036.x [DOI] [PubMed] [Google Scholar]
- 9.Shull MH, Ediger TR, Hill ID, et al. Health-related Quality of Life in Newly Diagnosed Pediatric Celiac Disease Patients. J Pediatr Gastroenterol Nutr 2019:1 10.1097/MPG.0000000000002465 [DOI] [PubMed] [Google Scholar]
- 10.Namatovu F, Strandh M, Ivarsson A, et al. Effect of childhood coeliac disease on ninth grade school performance: Evidence from a population-based study. Arch Dis Child 2018; 103:143–148. 10.1136/archdischild-2017-312830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Verkasalo M a, Raitakari OT, Viikari J, et al. Undiagnosed silent coeliac disease: a risk for underachievement? Scand J Gastroenterol 2005; 40:1407–12. 10.1080/00365520510023792 [DOI] [PubMed] [Google Scholar]
- 12.Olsson C, Lyon P, Hörnell A, et al. Food that makes you different: the stigma experienced by adolescents with celiac disease. Qual Health Res 2009; 19:976–84. 10.1177/1049732309338722 [DOI] [PubMed] [Google Scholar]
- 13.Olsson C, Hörnell A, Ivarsson A, et al. The everyday life of adolescent coeliacs: issues of importance for compliance with the gluten-free diet. J Hum Nutr Diet 2008; 21:359–67. [DOI] [PubMed] [Google Scholar]
- 14.Miller K, McGough N, Urwin H. Catering Gluten-Free When Simultaneously Using Wheat Flour. J Food Prot 2016; 79:282–287. 10.4315/0362-028x.jfp-15-213 [DOI] [PubMed] [Google Scholar]
- 15.Weisbrod VM, Silvester JA, Raber C, et al. Preparation of Gluten-Free Foods Alongside Gluten-Containing Food May Not Always Be as Risky for Celiac Patients as Diet Guides Suggest. Gastroenterology 2019. 10.1053/j.gastro.2019.09.007 [DOI] [PMC free article] [PubMed]
- 16.Erickson K, Freeborn D, Roper SO, et al. Parent Experiences Raising Young People with Type 1 Diabetes and Celiac Disease. J Pediatr Nurs 2015; 30:353–363. 10.1016/j.pedn.2014.09.011 [DOI] [PubMed] [Google Scholar]


